Key Points
Question
How can lymph node metastasis in early gastric cancer be accurately assessed?
Finding
In this study of 375 patients with early gastric cancer, collagen signature was statistically significantly associated with lymph node metastasis. A newly developed lymph node metastasis prediction model based on the collagen signature showed good discrimination in the primary cohort and was externally validated.
Meaning
The new prediction model appears to be useful in decision making associated with tailored surgical interventions in patients with early gastric cancer.
Abstract
Importance
Lymph node status is the primary determinant in treatment decision making in early gastric cancer (EGC). Current evaluation methods are not adequate for estimating lymph node metastasis (LNM) in EGC.
Objective
To develop and validate a prediction model based on a fully quantitative collagen signature in the tumor microenvironment to estimate the individual risk of LNM in EGC.
Design, Setting, and Participants
This retrospective study was conducted from August 1, 2016, to May 10, 2018, at 2 medical centers in China (Nanfang Hospital and Fujian Provincial Hospital). Participants included a primary cohort (n = 232) of consecutive patients with histologically confirmed gastric cancer who underwent radical gastrectomy and received a T1 gastric cancer diagnosis from January 1, 2008, to December 31, 2012. Patients with neoadjuvant radiotherapy, chemotherapy, or chemoradiotherapy were excluded. An additional consecutive cohort (n = 143) who received the same diagnosis from January 1, 2011, to December 31, 2013, was enrolled to provide validation. Baseline clinicopathologic data of each patient were collected. Collagen features were extracted in specimens using multiphoton imaging, and the collagen signature was constructed. An LNM prediction model based on the collagen signature was developed and was internally and externally validated.
Main Outcomes and Measures
The area under the receiver operating characteristic curve (AUROC) of the prediction model and decision curve were analyzed for estimating LNM.
Results
In total, 375 patients were included. The primary cohort comprised 232 consecutive patients, in whom the LNM rate was 16.4% (n = 38; 25 men [65.8%] with a mean [SD] age of 57.82 [10.17] years). The validation cohort consisted of 143 consecutive patients, in whom the LNM rate was 20.9% (n = 30; 20 men [66.7%] with a mean [SD] age of 54.10 [13.19] years). The collagen signature was statistically significantly associated with LNM (odds ratio, 5.470; 95% CI, 3.315-9.026; P < .001). Multivariate analysis revealed that the depth of tumor invasion, tumor differentiation, and the collagen signature were independent predictors of LNM. These 3 predictors were incorporated into the new prediction model, and a nomogram was established. The model showed good discrimination in the primary cohort (AUROC, 0.955; 95% CI, 0.919-0.991) and validation cohort (AUROC, 0.938; 95% CI, 0.897-0.981). An optimal cutoff value was selected in the primary cohort, which had a sensitivity of 86.8%, a specificity of 93.3%, an accuracy of 92.2%, a positive predictive value of 71.7%, and a negative predictive value of 97.3%. The validation cohort had a sensitivity of 90.0%, a specificity of 90.3%, an accuracy of 90.2%, a positive predictive value of 71.1%, and a negative predictive value of 97.1%. Among the 375 patients, a sensitivity of 87.3%, a specificity of 92.1%, an accuracy of 91.2%, a positive predictive value of 72.1%, and a negative predictive value of 96.9% were found.
Conclusions and Relevance
This study’s findings suggest that the collagen signature in the tumor microenvironment is an independent indicator of LNM in EGC, and the prediction model based on this collagen signature may be useful in treatment decision making for patients with EGC.
This study examines the role of collagen in detecting the risk for lymph node metastasis among patients with early gastric cancer.
Introduction
Early gastric cancer (EGC) is defined as cancer limited to the mucosa or submucosa, regardless of nodal status.1 Currently, endoscopic submucosal dissection (ESD) has become more popular than surgical procedures in treating EGC because it is minimally invasive, preserves function, and results in better quality of life.2,3,4 The principal indication for ESD is a tumor with a low risk of lymph node metastasis (LNM) that can undergo en bloc resection.3 The incidence of LNM is less than 3% when cancer is limited to the mucosa and increases to approximately 20% after cancer invades the submucosa.5 Thus, the accurate assessment of nodal status in EGC is integral to providing tailored surgical procedure.6,7 So far, the diagnostic accuracy of endoscopic ultrasonography and computed tomography for the nodal status of EGC is limited.8,9 Early gastric cancer with undifferentiated histologic result, submucosal invasion, and lymphovascular infiltration is deemed a high risk for LNM, and radical surgical procedure is considered,3,5,10 but a unanimous consensus has not been reached. To estimate the likelihood of LNM for EGC, several studies have developed different prediction models.11,12,13 However, these models focused on the clinical-pathologic characteristics, and the association of the tumor microenvironment with LNM was not investigated.
The extracellular matrix constitutes the scaffold of the tumor microenvironment, which regulates cancer behavior.14 As the main component of the extracellular matrix, collagen accounts for its major functions. The arrangement and orientation of collagen were proven to be indicators of tumor metastasis in breast cancer,15,16 glioblastoma17 and prostate cancer.18 Nevertheless, the role of collagen in the process of LNM in EGC is still unclear.
Multiphoton imaging could provide detailed information about tissue architecture and cell morphology in specimens through a combination of 2-photon excitation fluorescence from cells and second harmonic generation from collagen.19 Because of the underlying physical origin, multiphoton imaging has emerged as a powerful modality for collagen imaging in diverse tissues.20,21 Moreover, multiphoton imaging could be converted into high-dimensional and quantitative components of collagen via automatic extraction of multiple features. Collagen features analysis, including morphologic and textural features extracted from multiphoton imaging, has been applied and demonstrated to be a powerful quantitative indicator for diagnosis in several diseases.22,23,24
Integrating multiple biomarkers into a single signature, rather than performing individual biomarker analysis, is a promising approach that would improve clinical management.25,26 Currently, an appropriate method of integrating multiple collagen features into a single signature has not yet been developed. Hence, we propose the collagen signature, deduced by multiple morphologic and textural features of collagen using multiphoton imaging. The aim of this study was to develop and validate a prediction model based on the collagen signature that can distinguish genuine high-risk EGC with LNM. To our knowledge, this is the first study to investigate the role of collagen in EGC and to develop a prediction model for LNM based on the fully quantitative collagen signature.
Methods
The institutional review board at each participating center in China (Nanfang Hospital, Guangzhou, Guangdong, People's Republic of China and Fujian Provincial Hospital, Fuzhou, Fujian, People's Republic of China) approved this study. Patient informed consent was waived by the institutional review board because of the retrospective design of the study and patients' information was protected. The study was conducted from August 1, 2016, to May 10, 2018.
Patients and Specimens
The primary cohort (n = 232) was retrospectively assembled using the medical database of Nanfang Hospital. Consecutive patients who received a diagnosis from January 1, 2008, to December 31, 2012 (eFigure 1 in the Supplement) comprised the cohort. The inclusion criteria were patients with histologically confirmed gastric cancer who underwent radical gastrectomy and received a T1 gastric cancer diagnosis after surgical intervention. We excluded patients with neoadjuvant radiotherapy, chemotherapy, or chemoradiotherapy. An additional consecutive cohort (n = 143) who received the same diagnosis at the Fujian Provincial Hospital another hospital from January 1, 2011, to December 31, 2013, and who met the same criteria as the primary cohort was enrolled to provide validation. The formalin-fixed paraffin-embedded specimens of all patients were used.
Baseline clinicopathologic data of each patient, including sex, age at surgical intervention, macroscopic classification, tumor location, tumor size, tumor differentiation, lymphovascular infiltration, and depth of invasion, were collected. The tumor differentiation was divided into differentiated and undifferentiated types according to the 2014 Japanese gastric cancer treatment guidelines (version 4).3
Selection of Regions of Interest, Multiphoton Image Acquisition, and Collagen Feature Extraction
All specimens were processed for hematoxylin-eosin staining (original magnification ×200). Two of our independent pathologists (W. L. and J. L.), who were blinded to the nodal status, evaluated the region of the invasive margin of the EGC using a microscope at ×200 magnification. The interrater reliability was evaluated (κ = 0.437; 95% CI, 0.295-0.569) with approximately 87.3% (95% CI, 84.3%-90.1%) agreement. When the 2 pathologists differed in opinion, they consulted with the director (G.C.) of the Department of Pathology, Fujian Provincial Cancer Hospital, to make a decision. Five regions of interest with a field of view of 200 × 200 μm per specimen, which were equidistantly spread throughout the invasive margin, were selected to provide a realistic representation of each EGC sample.
Image acquisition for multiphoton imaging was performed with a 200× original magnification objective on another unstained serial section and then compared with hematoxylin-eosin staining for histologic assessment. The multiphoton imaging system used in this study has been described previously (eMethods in the Supplement).27
The extraction of collagen features was performed using MATLAB 2015b (MathWorks) as previously reported.28,29 A total of 146 features, including 12 morphologic features and 134 textural features, were extracted (eMethods and eTable 1 in the Supplement).
Feature Selection and Collagen Signature Construction
The LASSO (least-absolute shrinkage and selection operator) logistic regression, which has been broadly applied for high-dimensional data, was used to select the most predictive features in the primary cohort.30 The collagen signature construction was calculated through a combination of selected features (eMethods in the Supplement).
Prediction Model Development and Evaluation
Both the 8 clinicopathologic variables and the collagen signature were included in the univariate analysis to explore the association with LNM in the primary cohort, and variables with P < .05 were selected for the multivariate analysis. Backward stepwise regression was applied to select the independent predictors. The multicollinearity of the multivariate model was assessed using the tolerance and variance inflation factor. In addition, the effect modification was evaluated. A nomogram was constructed according to independent predictors. For quantification of the discrimination of the nomogram, the area under the receiver operating characteristic curve (AUROC) was measured. The calibration of the nomogram was evaluated by the calibration curve to assess the goodness of fit, accompanied by the Hosmer-Lemeshow test.
Prediction Model Internal and External Validation
The bootstrap method was applied for internal validation, in which the random samples drawn with a replacement from the original data set were the same size as the primary cohort.31 One thousand bootstrap repetitions were performed.
The prediction model was applied in the validation cohort. Ultimately, the AUROC was calculated, and the calibration curve was plotted.
Clinical Application
To evaluate the clinical application of the nomogram, decision curve analysis was used to assess the net benefits of the prediction model at different threshold probabilities (eMethods in the Supplement).32 The maximum Youden index was selected as the cutoff value to evaluate the sensitivity, specificity, accuracy, positive predictive value, and negative predictive value of the prediction model.
Statistical Analysis
An independent-samples, unpaired, 2-tailed t test or Mann-Whitney H test, where appropriate, was used to assess the differences in continuous variables, and a χ2 test or Fisher exact probability test was used to compare the differences between categorical variables. A multivariate logistic regression was performed to estimate the odds ratio (OR) with a 95% CI and to identify the independent predictors for LNM. Statistical analysis was conducted with R software, version 3.4.2 (R Foundation for Statistical Computing). Differences with a 2-sided P < .05 were considered statistically significant.
Results
Participants
The primary cohort included 232 consecutive patients, in whom the LNM rate was 16.4% (n = 38; 25 men [65.8%] with a mean [SD] age of 57.82 [10.17] years). The validation cohort included 143 consecutive patients, in whom the LNM rate was 20.9% (n = 30; 20 men [66.7%] with a mean [SD] age of 54.10 [13.19] years). Patient characteristics in the primary and validation cohorts are given in Table 1. No statistically significant difference in LNM prevalence was observed between the 2 cohorts (OR, 1.355; 95% CI, 0.796-2.307; P = .26). The clinicopathologic characteristics were similar between the primary and validation cohorts (eTable 2 in the Supplement).
Table 1. Characteristics of Patients in the Primary and Validation Cohorts.
| Variable | Primary Cohort (n = 232) | P Value | Validation Cohort (n = 143) | P Value | ||
|---|---|---|---|---|---|---|
| With LNM | Without LNM | With LNM | Without LNM | |||
| Age, mean (SD), y | 57.82 (10.17) | 58.82 (10.90) | .60 | 54.10 (13.19) | 58.64 (11.09) | .06 |
| Sex, No. (%) | .47 | .76 | ||||
| Male | 25 (65.8) | 139 (71.6) | 20 (66.7) | 72 (63.7) | ||
| Female | 13 (34.2) | 55 (28.4) | 10 (33.3) | 41 (36.3) | ||
| Primary site, No. (%) | .21 | .06 | ||||
| Upper | 3 (7.9) | 28 (14.4) | 3 (10) | 24 (21.2) | ||
| Middle | 6 (15.8) | 47 (24.2) | 4 (13.3) | 30 (26.5) | ||
| Low | 29 (76.3) | 119 (61.3) | 23 (76.7) | 59 (52.2) | ||
| Size, No. (%), cm | .001 | .09 | ||||
| ≤2 | 14 (36.8) | 127 (65.5) | 11 (36.7) | 61(54.0) | ||
| >2 | 24 (63.2) | 67 (34.5) | 19 (63.3) | 52 (46.0) | ||
| Macroscopic, No. (%) | .20 | .14 | ||||
| Elevated | 3 (7.9) | 6 (3.1) | 0 (0) | 2 (1.8) | ||
| Flat | 19 (50.0) | 121 (62.4) | 18 (60.0) | 85(75.2) | ||
| Depressed | 16 (42.1) | 67 (34.5) | 12 (40.0) | 26 (23.0) | ||
| Differentiation, No. (%) | .002 | <.001 | ||||
| Differentiated | 18 (47.4) | 141 (72.7) | 9 (30.0) | 75 (66.4) | ||
| Undifferentiated | 20 (52.6) | 53 (27.3) | 21 (70.0) | 38 (33.6) | ||
| Lymphovascular invasion, No. (%) | <.001 | .002 | ||||
| No | 28 (73.7) | 185 (95.4) | 23 (76.7) | 107 (94.7) | ||
| Yes | 10 (26.3) | 9 (4.6) | 7 (23.3) | 6 (5.3) | ||
| Depth, No. (%) | <.001 | .005 | ||||
| Mucosa | 4 (10.5) | 101 (52.1) | 6 (20.0) | 55 (48.7) | ||
| Submucosa | 34 (89.5) | 93 (47.9) | 24 (80.0) | 58 (51.3) | ||
| Collagen signature, median (IQR) | 0.284 (−0.836 to 0.872) | −2.856 (−3.630 to −2.088) | <.001 | −0.552 (−0.887 to −0.125) | −2.277 (−2.851 to −1.794) | <.001 |
Abbreviations: IQR, interquartile range; LNM, lymph node metastasis.
Collagen Signature Construction
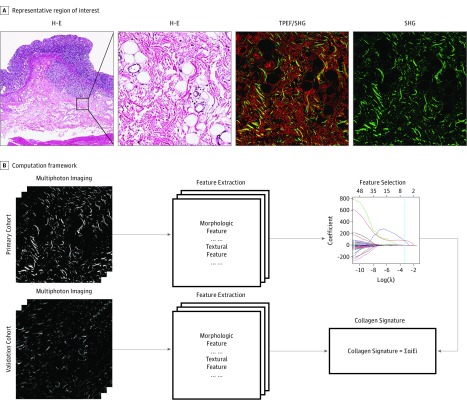
The construction framework of the collagen signature is presented in Figure 1. All collagen features were reduced to the 6 best potential predictors, using LASSO logistic regression (eFigures 2A and 2B in the Supplement; the 6 features are presented in eAppendix 1 in the Supplement). A statistically significant difference in the collagen signature (median [interquartile range (IQR)]) was found between patients with LNM (0.284 [–0.836 to 0.872]) and patients without LNM (–2.856 [–3.630 to –2.088]) in the primary cohort (median difference, 2.059; 95% CI, 1.413 to 2.757; P < .001). This finding was consistent with the patients with LNM (–0.522 [–0.887 to –0.125]) and patients without LNM (–2.277 [–2.851 to –1.794]) in the validation cohort (median difference, 1.793; 95% CI, 1.176 to 2.361; P < .001) (Table 1). The collagen signature indicated a favorable prediction of LNM with an AUROC of 0.944 (95% CI, 0.905-0.982) in the primary cohort and 0.933 (95% CI, 0.889-0.977) in the validation cohort (eFigures 2C and 2D in the Supplement).
Figure 1. Schematic Illustration of Collagen Signature Construction.
A, A representative region of interest with a field of view of 200 × 200 μm was selected in the hematoxylin-eosin (H-E) stain (original magnification ×200). The corresponding multiphoton imaging, including 2-photon excitation fluorescence (TPEF) and second harmonic generation (SHG), was obtained, and the SHG imaging was chosen for collagen feature extraction. B, A computation framework was used to establish the collagen signature. The SHG imaging of multiphoton imaging was chosen for collagen feature extraction, including morphologic features and texture features. Next, the potential predictors were selected using LASSO (least-absolute shrinkage and selection operator) logistic regression. The collagen signature can be calculated by these potential predictors.
Prediction Model Development and Evaluation
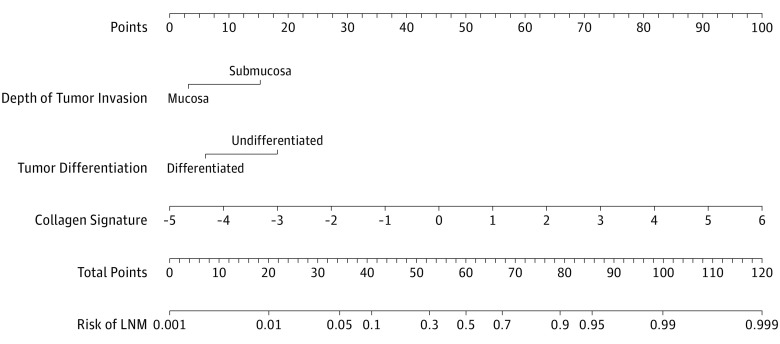
A univariate analysis was performed for each variable in the primary cohort. A tumor size larger than 2 cm (OR, 3.249; 95% CI, 1.578-6.693; P = .001), undifferentiated tumor (OR, 2.956; 95% CI, 1.452-6.017; P = .002), lymphovascular infiltration (OR, 7.341; 95% CI, 2.743-19.646; P < .001), submucosal invasion (OR, 9.231; 95% CI, 3.155-27.010; P < .001), and collagen signature (OR, 5.470; 95% CI, 3.315-9.026; P < .001) were statistically significantly associated with LNM in EGC (Table 2). Furthermore, a multivariate analysis identified that tumor differentiation (OR, 4.585; 95% CI, 1.310-16.041; P = .02), the depth of tumor invasion (OR, 6.773; 95% CI, 1.636-28.039; P = .008), and the collagen signature (OR, 5.335; 95% CI, 3.042-9.358; P < .001) were independent predictors of LNM (Table 2). The variance inflation factor of each predictor was less than 10, and the corresponding tolerance was more than 0.1; therefore, no multicollinearity among these predictors was noted (eTable 3 in the Supplement).33 No effect modification was found in the prediction model (eTables 4 and 5 in the Supplement). The association between the collagen signature and the risk of LNM with different combinations of tumor differentiation states (differentiated or undifferentiated) and depths of tumor invasion (mucosa or submucosa) is presented in eFigure 3 in the Supplement. A nomogram was produced by incorporating these 3 independent predictors (Figure 2).
Table 2. Univariate and Multivariate Logistic Regression of Lymph Node Metastasis in the Primary Cohort.
| Variable | Univariate Logistic Regression | Multivariate Logistic Regression | ||
|---|---|---|---|---|
| OR (95% CI) | P Value | OR (95% CI) | P Value | |
| Age | 0.991 (0.960-1.024) | .60 | NA | NA |
| Sex | ||||
| Male | 1 [Reference] | >.99 | ||
| Female | 1.314 (0.627-2.753) | .47 | NA | NA |
| Primary site of tumor | ||||
| Upper | 1 [Reference] | >.99 | ||
| Middle | 1.191 (0.276-5.145) | .81 | NA | NA |
| Low | 2.275 (0.647-8.002) | .20 | NA | NA |
| Tumor size, cm | ||||
| ≤2 | 1 [Reference] | >.99 | ||
| >2 | 3.249 (1.578-6.693) | .001a | NA | NA |
| Macroscopic tumor view | ||||
| Elevated | 1 [Reference] | >.99 | ||
| Flat | 0.314 (0.072-1.363) | .12 | NA | NA |
| Depressed | 0.478 (0.108-2.118) | .33 | NA | NA |
| Tumor differentiation | ||||
| Differentiated | 1 [Reference] | >.99 | 1 [Reference] | >.99 |
| Undifferentiated | 2.956 (1.452-6.017) | .002 | 4.585 (1.310-16.041) | .02 |
| Lymphovascular invasion | ||||
| No | 1 [Reference] | >.99 | ||
| Yes | 7.341 (2.743-19.646) | <.001 | NA | NA |
| Depth of tumor invasion | ||||
| Mucosa | 1 [Reference] | >.99 | 1 [Reference] | >.99 |
| Submucosa | 9.231 (3.155-27.010) | <.001 | 6.773 (1.636-28.039) | .008 |
| Collagen signature | 5.470 (3.315-9.026) | <.001 | 5.335 (3.042-9.358) | <.001 |
Abbreviations: NA, not available; OR, odds ratio.
Figure 2. Nomogram for Estimating Lymph Node Metastasis (LNM) in Early Gastric Cancer.
The nomogram indicates the risk of LNM in early gastric cancer. For clinical use, tumor differentiation is determined by drawing a line straight up to the point axis to establish the score associated with the differentiation. Next, this process is repeated for the other 2 covariates (depth of tumor invasion and collagen signature). The scores of each covariate are added, and the total score is located on the total score points axis. Last, a line is drawn straight down to the risk of LNM axis to obtain the probability.
The newly developed prediction model showed good discrimination with an AUROC of 0.955 (95% CI, 0.919-0.991), and the calibration curve showed good agreement between the nomogram-estimated probability of LNM and the actual LNM rate in the primary cohort (eFigure 4A and B in the Supplement). The Hosmer-Lemeshow test demonstrated a P = .47, indicating no departure from a good fit.
Internal and External Prediction Model Validation
For internal validation, we used the bootstrap method with 1000 bootstrap repetitions. The results remained largely unchanged between iterations, with a mean concordance index of 0.911.
Good discrimination with an AUROC of 0.938 (95% CI, 0.897-0.981) was externally validated, and the favorable calibration was also confirmed in the validation cohort (eFigure 4C and D in the Supplement). A Hosmer-Lemeshow test demonstrated a nonsignificant P = .15.
Clinical Application
In the decisive curve, the x-axis is a measure of patient or physician preference, and the threshold probability indicates that the expected advantage of treatment is equal to the expected advantage of avoiding treatment.33 The decision curve revealed that if the threshold probability of a patient or physician was greater than 5%, more advantages would be added by using the nomogram to estimate LNM in EGC than the advantage achieved in either the treat-all-patient scheme or the treat-none scheme (eFigure 5 in the Supplement).
In addition, in the primary cohort, the maximum Youden index of 0.301 was selected as the cutoff value, and the cohort had a sensitivity of 86.8%, a specificity of 93.3%, an accuracy of 92.2%, a positive predictive value of 71.7%, and a negative predictive value of 97.3%. The validation cohort had a sensitivity of 90.0%, a specificity of 90.3%, an accuracy of 90.2%, a positive predictive value of 71.1%, and a negative predictive value of 97.1%. Among the 375 patients, a sensitivity of 87.3%, a specificity of 92.1%, an accuracy of 91.2%, a positive predictive value of 72.1%, and a negative predictive value of 96.9% were found (eTable 6 in the Supplement).
Comparison With the Traditional Prediction Model
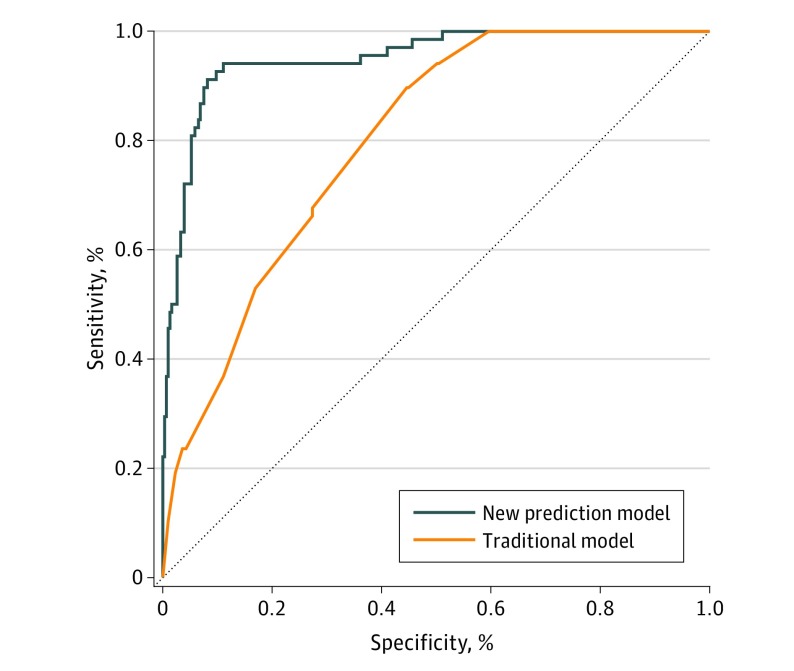
To elucidate the superiority of the model we built over the clinicopathologic characteristic-based model (ie, the traditional model), we eliminated the collagen signature and developed the traditional model on the basis of tumor differentiation (OR, 2.576; 95% CI, 1.167-5.685; P = .02), lymphovascular infiltration (OR, 3.333; 95% CI, 1.145-9.703; P = .03), and the depth of tumor invasion (OR, 9.923; 95% CI, 3.305-29.793; P < .001) (eTable 7 in the Supplement) after univariate and multivariate analyses. No multicollinearity in the traditional model was found (eTable 8 in the Supplement). Sex, age at surgical intervention, macroscopic classification, and tumor location were chosen as variables, but these variables were not statistically significant after univariate analysis. The performance of the traditional model was similar to the performance previously reported, with an AUROC of 0.812 (95% CI, 0.752-0.872) in the primary cohort and 0.768 (95% CI, 0.688-0.849) in the validation cohort (eFigure 6 in the Supplement).11,12 Compared with the traditional model, the new model based on the collagen signature showed a more robust ability to estimate the risk of LNM in EGC in all 375 patients (AUROC comparison, 0.950 [95% CI, 0.923-0.977] vs 0.798 [95% CI, 0.749-0.847]; P < .001) (Figure 3).
Figure 3. Comparison Between the Traditional Model and the New Collagen Signature–Based Prediction Model.
The orange line represents the new model (area under the receiver operating characteristic curve [AUROC], 0.950; 95% CI, 0.923-0.977), including the depth of tumor invasion, tumor differentiation, and the collagen signature. The blue line represents the traditional model (AUROC, 0.798; 95% CI, 0.749-0.847), including the depth of tumor invasion, tumor differentiation, and lymphovascular infiltration.
Discussion
Accurate assessment of the nodal status in EGC is important in the decision making for lymph node dissection. In this study, we developed and validated a nomogram for individual estimation of LNM in EGC, including the depth of tumor invasion, tumor differentiation, and the collagen signature.
Two key factors determine the construction of the collagen signature. The first is the use of a suitable imaging approach to selectively visualize the collagen. In this study, multiphoton imaging was used because of its underlying physical origin.20,21 Previous research indicated that multiphoton imaging can distinguish between the mucosa and submucosa of cancerous gastric tissues, and collagen can be quantified by second harmonic generation in a stain-free section.34 Thus, multiphoton imaging is an ideal method for collagen imaging. The second factor is the quantitative analysis of collagen from multiphoton imaging. For this purpose, we have established a stable framework for achieving precise quantification.28,29
After considering these 2 factors, we constructed the collagen signature. The collagen signature was substantially different in EGC with and without LNM. To develop a clinically practicable prediction tool, we used other clinicopathologic characteristics. We also built a nomogram with good discrimination and calibration. Our findings suggest that LNM is more likely to appear in patients with an undifferentiated histologic result, submucosal invasion, and a high collagen signature.
Compared with the traditional model based on tumor differentiation, the depth of tumor invasion, and lymphovascular infiltration, the prediction model was more powerful in estimating the risk of LNM in EGC. Although a tumor size larger than 2 cm was statistically significantly associated with LNM, it was excluded after backward stepwise multivariate analysis in both the prediction model and the traditional model. The reason for this exclusion was that the depth of tumor invasion was much more important than tumor size in the clinic.
Currently, endoscopic ultrasonography and computed tomography are the 2 most common examination methods for N staging of gastric cancer. Endoscopic ultrasonography for N staging had a sensitivity of 83% and a specificity of 67%.35 Meanwhile, computed tomography for detecting LNM had a sensitivity of 78% and a specificity of 62% in gastric cancer.36 In the prediction model, the sensitivity was 87.3% and the specificity was 92.1%, with the cutoff value of the maximum Youden index. Therefore, the prediction model was adequate for base clinical decisions.
In this study, tumor differentiation and the depth of tumor invasion were categorical variables, and the collagen signature was a continuous variable. The risk of LNM was always contributed to by these 3 predictors. For example, for a patient without LNM with a collagen signature of –2.856, the risk of LNM was less than 1% for differentiated tumors that invaded only the mucosa. When the tumor was undifferentiated, the risk of LNM was approximately 2%, and if the tumor also invaded the submucosa, the risk of LNM increased to 8%. Similarly, for a patient with LNM with a collagen signature of 0.284, the risk of LNM was approximately 30% for differentiated tumors that invaded the mucosa. In the case of undifferentiated tumors, the risk of LNM increased to approximately 70%. Once the tumors invaded the submucosa, the risk of LNM increased to approximately 90%. As tumor differentiation and the depth of tumor invasion are routinely assessed in endoscopic resection specimens, and the collagen signature could be quantified using multiphoton imaging, the individual risk of LNM could be conveniently estimated by the nomogram after ESD. For a low risk of LNM, the nomogram indicates that ESD is adequate. Inversely, for a high risk of LNM, additional lymph node dissection might be needed.
Collagen was identified as a component of cancer metastasis. Local collagen orientations have been shown to play an important role in promoting cell breakage into the basement membrane before entering the circulation systems.15 Kakkad et al24 reported that multiphoton imaging revealed that a substantially increased density of collagen was associated with LNM in breast cancer. In our study, the collagen signature was positively correlated with collagen straightness and cross-link density. This result indicated that the collagen arrangement was far straighter in the invasive margin of EGC with LNM. Straighter collagen in the tumor microenvironment could facilitate invasion.37,38 Meanwhile, increased collagen cross-link density could stiffen the extracellular matrix, enhance growth factor signaling activity, and induce the invasion of an oncogene-initiated epithelium.39 Our data showed the association between the collagen signature and LNM for EGC. Future studies should focus on the underlying molecular mechanisms.
The collagen features in this study were extracted from multiphoton imaging. Because the components of the multiphoton imaging system were fixed, pathologists could conduct multiphoton imaging using a microscope. Finishing multiphoton imaging took approximately 5 to 10 minutes. Multiphoton imaging was good at showing collagen and did not change the tissue architecture and cell morphology. Therefore, pathologists could understand and analyze multiphoton imaging after training. Meanwhile, the ESD of EGC has no special requirements, and specimens can be processed regularly, which would not affect the multiphoton imaging. Multiphoton imaging is a promising method for realizing real-time in vivo optical biopsy, and several groups have reported the possible clinical applications in different organs.40,41,42 We foresee that clinicians could obtain collagen signature in the near future using multiphoton imaging. With the assistance of the prediction model, EGC with a genuine high risk of LNM would be distinguished, and more tailored surgical interventions could be performed.
Limitations
This study has some limitations. First, because it was a retrospective study, it might result in a potential selection bias. Thus, a multicenter prospective clinical trial is required to confirm the prediction model we developed. We are comfortable with the application of this technique in a clinical trial. Second, the clinicopathologic characteristics between the primary and validation cohorts were similar, which made our validation less robust, and the distribution of clinicopathologic characteristics might be different in other countries. Therefore, cohorts from Western countries are needed to further validate our findings. Third, the sample-size calculation for logistic regression analysis is still debated. We used 2 methods to calculate the sample size: one requires at least 10 events per variable,43 and the other is based on the variance inflation factor and does not explicitly require knowledge of the number of variables in the regression model.44 The sample size might not be adequate for the former method but was enough for the latter method (eAppendix 2 in the Supplement). Thus, we hope that this limitation will be solved in our upcoming clinical trial. Fourth, the weak interrater reliability between the 2 pathologists is also a limitation. One pathologist was a senior attending pathologist, and the other was a junior attending pathologist. The weak interrater reliability was the result of the difference in their experiences. In our next trial, we will require 2 senior attending pathologists.
Conclusions
The collagen signature in the tumor microenvironment is an independent risk factor for LNM in EGC. The prediction model we developed and validated is useful for decision making in tailored surgical intervention.
eMethods
eTable 1. List of collagen features
eTable 2. Comparison of clinical-pathological factors in the primary and validation cohorts
eTable 3. Multicollinearity assessment in the prediction model based on the collagen signature
eTable 4. Effect modification assessment between the collagen signature and the depth of tumor invasion
eTable 5. Effect modification assessment between the collagen signature and tumor differentiation
eTable 6. The model performance in estimating the risk of LNM
eTable 7. Univariate and multivariate logistic regression of LNM without the collagen signature
eTable 8. Multicollinearity assessment in the traditional model
eAppendix 1. Collagen signature calculation formula
eAppendix 2. Sample size calculation for logistic regression analysis
eFigure 1. Recruitment pathways for patients in the primary and validation cohorts
eFigure 2. Collagen feature selection using LASSO binary logistic regression and discrimination of the collagen signature
eFigure 3. Association between the collagen signature and the risk of LNM for different types of tumor differentiation and depths of tumor invasion
eFigure 4. The performance of the prediction model based on the collagen signature
eFigure 5. Decision curve analysis of the nomogram
eFigure 6. The ROC curve to predict LNM in the primary and validation cohorts without the collagen signature
References
- 1.Van Cutsem E, Sagaert X, Topal B, Haustermans K, Prenen H. Gastric cancer. Lancet. 2016;388(10060):-. doi: 10.1016/S0140-6736(16)30354-3 [DOI] [PubMed] [Google Scholar]
- 2.Isomoto H, Shikuwa S, Yamaguchi N, et al. Endoscopic submucosal dissection for early gastric cancer: a large-scale feasibility study. Gut. 2009;58(3):331-336. doi: 10.1136/gut.2008.165381 [DOI] [PubMed] [Google Scholar]
- 3.Japanese Gastric Cancer Association Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer. 2017;20(1):1-19. doi: 10.1007/s10120-016-0622-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Choi JH, Kim ES, Lee YJ, et al. Comparison of quality of life and worry of cancer recurrence between endoscopic and surgical treatment for early gastric cancer. Gastrointest Endosc. 2015;82(2):299-307. doi: 10.1016/j.gie.2015.01.019 [DOI] [PubMed] [Google Scholar]
- 5.Hirasawa T, Gotoda T, Miyata S, et al. Incidence of lymph node metastasis and the feasibility of endoscopic resection for undifferentiated-type early gastric cancer. Gastric Cancer. 2009;12(3):148-152. doi: 10.1007/s10120-009-0515-x [DOI] [PubMed] [Google Scholar]
- 6.An JY, Baik YH, Choi MG, Noh JH, Sohn TS, Kim S. Predictive factors for lymph node metastasis in early gastric cancer with submucosal invasion: analysis of a single institutional experience. Ann Surg. 2007;246(5):749-753. doi: 10.1097/SLA.0b013e31811f3fb7 [DOI] [PubMed] [Google Scholar]
- 7.Oh SY, Lee KG, Suh YS, et al. Lymph node metastasis in mucosal gastric cancer: reappraisal of expanded indication of endoscopic submucosal dissection. Ann Surg. 2017;265(1):137-142. doi: 10.1097/SLA.0000000000001649 [DOI] [PubMed] [Google Scholar]
- 8.Spolverato G, Ejaz A, Kim Y, et al. Use of endoscopic ultrasound in the preoperative staging of gastric cancer: a multi-institutional study of the US gastric cancer collaborative. J Am Coll Surg. 2015;220(1):48-56. doi: 10.1016/j.jamcollsurg.2014.06.023 [DOI] [PubMed] [Google Scholar]
- 9.Fujikawa H, Yoshikawa T, Hasegawa S, et al. Diagnostic value of computed tomography for staging of clinical T1 gastric cancer. Ann Surg Oncol. 2014;21(9):3002-3007. doi: 10.1245/s10434-014-3667-9 [DOI] [PubMed] [Google Scholar]
- 10.Park JW, Ahn S, Lee H, et al. Predictive factors for lymph node metastasis in early gastric cancer with lymphatic invasion after endoscopic resection. Surg Endosc. 2017;31(11):4419-4424. doi: 10.1007/s00464-017-5490-4 [DOI] [PubMed] [Google Scholar]
- 11.Pyo JH, Shin CM, Lee H, et al. ; JHP and CMS contributed equally as the first authors of this study. . A risk-prediction model based on lymph-node metastasis for incorporation into a treatment algorithm for signet ring cell-type intramucosal gastric cancer. Ann Surg. 2016;264(6):1038-1043. doi: 10.1097/SLA.0000000000001602 [DOI] [PubMed] [Google Scholar]
- 12.Guo CG, Zhao DB, Liu Q, et al. A nomogram to predict lymph node metastasis in patients with early gastric cancer. Oncotarget. 2017;8(7):12203-12210. doi: 10.18632/oncotarget.14660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jung DH, Huh CW, Kim JH, et al. Risk-stratification model based on lymph node metastasis after noncurative endoscopic resection for early gastric cancer. Ann Surg Oncol. 2017;24(6):1643-1649. doi: 10.1245/s10434-017-5791-9 [DOI] [PubMed] [Google Scholar]
- 14.Buchheit CL, Weigel KJ, Schafer ZT. Cancer cell survival during detachment from the ECM: multiple barriers to tumour progression. Nat Rev Cancer. 2014;14(9):632-641. doi: 10.1038/nrc3789 [DOI] [PubMed] [Google Scholar]
- 15.Han W, Chen S, Yuan W, et al. Oriented collagen fibers direct tumor cell intravasation. Proc Natl Acad Sci U S A. 2016;113(40):11208-11213. doi: 10.1073/pnas.1610347113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Conklin MW, Gangnon RE, Sprague BL, et al. Collagen alignment as a predictor of recurrence after ductal carcinoma in situ. Cancer Epidemiol Biomarkers Prev. 2018;27(2):138-145. doi: 10.1158/1055-9965.EPI-17-0720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pointer KB, Clark PA, Schroeder AB, Salamat MS, Eliceiri KW, Kuo JS. Association of collagen architecture with glioblastoma patient survival. J Neurosurg. 2017;126(6):1812-1821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Penet MF, Kakkad S, Pathak AP, et al. Structure and function of a prostate cancer dissemination-permissive extracellular matrix. Clin Cancer Res. 2017;23(9):2245-2254. doi: 10.1158/1078-0432.CCR-16-1516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zipfel WR, Williams RM, Christie R, Nikitin AY, Hyman BT, Webb WW. Live tissue intrinsic emission microscopy using multiphoton-excited native fluorescence and second harmonic generation. Proc Natl Acad Sci U S A. 2003;100(12):7075-7080. doi: 10.1073/pnas.0832308100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zipfel WR, Williams RM, Webb WW. Nonlinear magic: multiphoton microscopy in the biosciences. Nat Biotechnol. 2003;21(11):1369-1377. doi: 10.1038/nbt899 [DOI] [PubMed] [Google Scholar]
- 21.Campagnola P. Second harmonic generation imaging microscopy: applications to diseases diagnostics. Anal Chem. 2011;83(9):3224-3231. doi: 10.1021/ac1032325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cicchi R, Kapsokalyvas D, De Giorgi V, et al. Scoring of collagen organization in healthy and diseased human dermis by multiphoton microscopy. J Biophotonics. 2010;3(1-2):34-43. doi: 10.1002/jbio.200910062 [DOI] [PubMed] [Google Scholar]
- 23.Wen BL, Brewer MA, Nadiarnykh O, et al. Texture analysis applied to second harmonic generation image data for ovarian cancer classification. J Biomed Opt. 2014;19(9):096007. doi: 10.1117/1.JBO.19.9.096007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kakkad SM, Solaiyappan M, Argani P, et al. Collagen I fiber density increases in lymph node positive breast cancers: pilot study. J Biomed Opt. 2012;17(11):116017. doi: 10.1117/1.JBO.17.11.116017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Huang YQ, Liang CH, He L, et al. Development and validation of a radiomics nomogram for preoperative prediction of lymph node metastasis in colorectal cancer. J Clin Oncol. 2016;34(18):2157-2164. doi: 10.1200/JCO.2015.65.9128 [DOI] [PubMed] [Google Scholar]
- 26.Agesen TH, Sveen A, Merok MA, et al. ColoGuideEx: a robust gene classifier specific for stage II colorectal cancer prognosis. Gut. 2012;61(11):1560-1567. doi: 10.1136/gutjnl-2011-301179 [DOI] [PubMed] [Google Scholar]
- 27.Zhuo S, Chen J, Luo T, Zou D. Multimode nonlinear optical imaging of the dermis in ex vivo human skin based on the combination of multichannel mode and Lambda mode. Opt Express. 2006;14(17):7810-7820. doi: 10.1364/OE.14.007810 [DOI] [PubMed] [Google Scholar]
- 28.Xu S, Wang Y, Tai DCS, et al. qFibrosis: a fully-quantitative innovative method incorporating histological features to facilitate accurate fibrosis scoring in animal model and chronic hepatitis B patients. J Hepatol. 2014;61(2):260-269. doi: 10.1016/j.jhep.2014.02.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Xu S, Kang CH, Gou X, et al. Quantification of liver fibrosis via second harmonic imaging of the Glisson’s capsule from liver surface. J Biophotonics. 2016;9(4):351-363. doi: 10.1002/jbio.201500001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sauerbrei W, Royston P, Binder H. Selection of important variables and determination of functional form for continuous predictors in multivariable model building. Stat Med. 2007;26(30):5512-5528. doi: 10.1002/sim.3148 [DOI] [PubMed] [Google Scholar]
- 31.Iasonos A, Schrag D, Raj GV, Panageas KS. How to build and interpret a nomogram for cancer prognosis. J Clin Oncol. 2008;26(8):1364-1370. doi: 10.1200/JCO.2007.12.9791 [DOI] [PubMed] [Google Scholar]
- 32.Kerr KF, Brown MD, Zhu K, Janes H. Assessing the clinical impact of risk prediction models with decision curves: guidance for correct interpretation and appropriate use. J Clin Oncol. 2016;34(21):2534-2540. doi: 10.1200/JCO.2015.65.5654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dormann CF, Elith J, Bacher S, et al. Collinearity: a review of methods to deal with it and a simulation study evaluating their performance. Ecography. 2013;36(1):27-46. doi: 10.1111/j.1600-0587.2012.07348.x [DOI] [Google Scholar]
- 34.Chen J, Zhuo S, Chen G, et al. Establishing diagnostic features for identifying the mucosa and submucosa of normal and cancerous gastric tissues by multiphoton microscopy. Gastrointest Endosc. 2011;73(4):802-807. doi: 10.1016/j.gie.2010.12.016 [DOI] [PubMed] [Google Scholar]
- 35.Mocellin S, Pasquali S. Diagnostic accuracy of endoscopic ultrasonography (EUS) for the preoperative locoregional staging of primary gastric cancer. Cochrane Database Syst Rev. 2015;(2):CD009944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ajani JA, D’Amico TA, Almhanna K, et al. Gastric Cancer, Version 3.2016, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2016;14(10):1286-1312. doi: 10.6004/jnccn.2016.0137 [DOI] [PubMed] [Google Scholar]
- 37.Provenzano PP, Eliceiri KW, Campbell JM, Inman DR, White JG, Keely PJ. Collagen reorganization at the tumor-stromal interface facilitates local invasion. BMC Med. 2006;4(1):38. doi: 10.1186/1741-7015-4-38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wyckoff JB, Wang Y, Lin EY, et al. Direct visualization of macrophage-assisted tumor cell intravasation in mammary tumors. Cancer Res. 2007;67(6):2649-2656. doi: 10.1158/0008-5472.CAN-06-1823 [DOI] [PubMed] [Google Scholar]
- 39.Levental KR, Yu H, Kass L, et al. Matrix crosslinking forces tumor progression by enhancing integrin signaling. Cell. 2009;139(5):891-906. doi: 10.1016/j.cell.2009.10.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Brown CM, Rivera DR, Pavlova I, et al. In vivo imaging of unstained tissues using a compact and flexible multiphoton microendoscope. J Biomed Opt. 2012;17(4):040505. doi: 10.1117/1.JBO.17.4.040505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Huland DM, Brown CM, Howard SS, et al. In vivo imaging of unstained tissues using long gradient index lens multiphoton endoscopic systems. Biomed Opt Express. 2012;3(5):1077-1085. doi: 10.1364/BOE.3.001077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rivera DR, Brown CM, Ouzounov DG, et al. Compact and flexible raster scanning multiphoton endoscope capable of imaging unstained tissue. Proc Natl Acad Sci U S A. 2011;108(43):17598-17603. doi: 10.1073/pnas.1114746108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Collins GS, Reitsma JB, Altman DG, Moons KG. Transparent Reporting of a multivariable prediction model for Individual Prognosis or Diagnosis (TRIPOD): the TRIPOD statement. Ann Intern Med. 2015;162(1):55-63. doi: 10.7326/M14-0697 [DOI] [PubMed] [Google Scholar]
- 44.Hsieh FY. Sample size tables for logistic regression. Stat Med. 1989;8(7):795-802. doi: 10.1002/sim.4780080704 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods
eTable 1. List of collagen features
eTable 2. Comparison of clinical-pathological factors in the primary and validation cohorts
eTable 3. Multicollinearity assessment in the prediction model based on the collagen signature
eTable 4. Effect modification assessment between the collagen signature and the depth of tumor invasion
eTable 5. Effect modification assessment between the collagen signature and tumor differentiation
eTable 6. The model performance in estimating the risk of LNM
eTable 7. Univariate and multivariate logistic regression of LNM without the collagen signature
eTable 8. Multicollinearity assessment in the traditional model
eAppendix 1. Collagen signature calculation formula
eAppendix 2. Sample size calculation for logistic regression analysis
eFigure 1. Recruitment pathways for patients in the primary and validation cohorts
eFigure 2. Collagen feature selection using LASSO binary logistic regression and discrimination of the collagen signature
eFigure 3. Association between the collagen signature and the risk of LNM for different types of tumor differentiation and depths of tumor invasion
eFigure 4. The performance of the prediction model based on the collagen signature
eFigure 5. Decision curve analysis of the nomogram
eFigure 6. The ROC curve to predict LNM in the primary and validation cohorts without the collagen signature