Abstract
This study examines the appropriate use of percutaneous coronary interventions in New York, Michigan, and Florida using Healthcare Cost and Utilization Project state databases.
Recent health care policy initiatives have focused on reducing misuse or overuse of expensive cardiovascular procedures. The appropriate use criteria (AUC) for coronary revascularization were released in 2009 with the aim of reducing inappropriate percutaneous coronary interventions (PCIs).1 In addition, national efforts to provide hospitals with information about their performance on PCI appropriateness began in 2011.2
Since these initiatives were enacted, the volume of PCIs performed for nonacute indications in the United States has declined, as have rates of PCIs considered inappropriate.3,4 Some have declared this a policy success—that the fewer inappropriate PCIs performed nationally reflect better selection of patients likely to experience improved outcomes. However, it may be that these initiatives incentivized physicians to classify patients with stable chest pain as having unstable angina (UA) to meet AUC. To explore this possibility, we examined trends in PCIs coded for acute indications in the outpatient setting in 3 large and geographically dispersed states.
Methods
Using Healthcare Cost and Utilization Project state databases, we identified all inpatient and outpatient PCIs in New York, Michigan, and Florida from 2010 to 2014. Percutaneous coronary interventions were classified as acute if associated with a primary or secondary diagnosis of UA or acute myocardial infarction (AMI). We then calculated the proportion of outpatient PCIs coded for acute indications relative to total PCIs performed in each state by year. Percutaneous coronary interventions performed for AMI and UA in an outpatient setting should be infrequent and remain stable over time—a significant increase would suggest potential shifts in diagnostic and/or coding patterns. We also characterized the proportion of acute inpatient PCIs relative to total PCIs.
Results
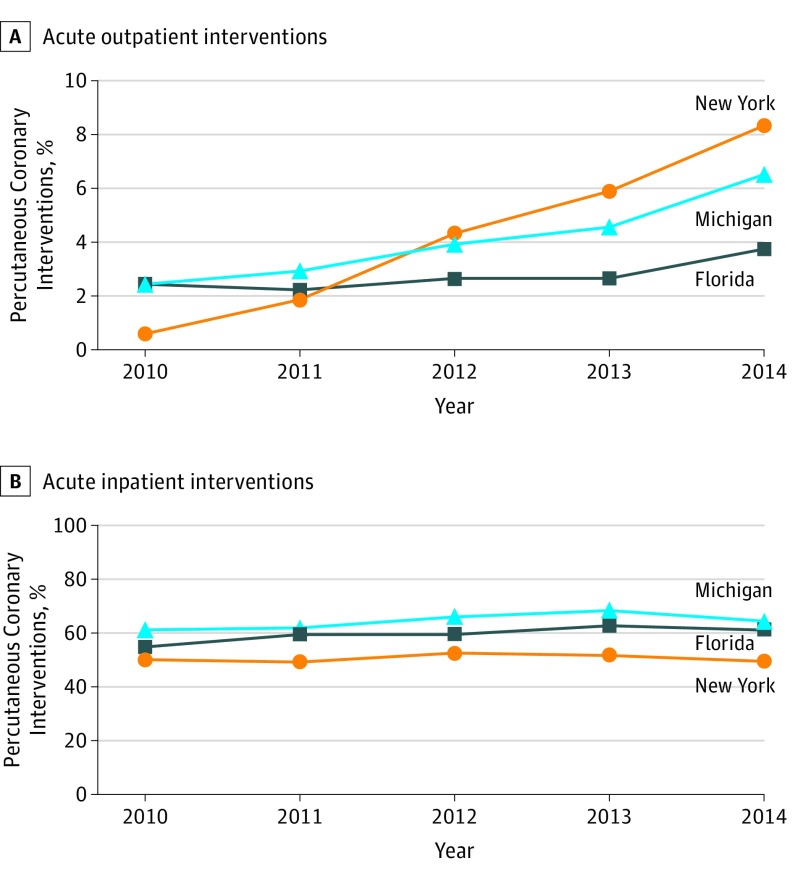
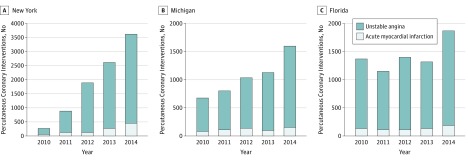
A total of 615 649 PCIs were performed in both the inpatient and outpatient setting from 2010 to 2014. The proportion of outpatient PCIs coded for acute indications increased over time in New York (0.6% to 8.3%), Michigan (2.4% to 6.5%), and Florida (2.4% to 3.8%) (Figure 1A). This increase was driven by a substantial rise in the crude number of outpatient PCIs coded for UA (New York, 242 to 3179; Michigan, 587 to 1426; Florida, 1231 to 1686). The number of outpatient PCIs coded for AMI were lower, but also increased: New York (49 to 435), Michigan (90 to 162), and Florida (134 to 192) (Figure 2). In the inpatient setting, PCIs coded for acute indications increased in 2 states (Figure 1B).
Figure 1. Proportion of Percutaneous Coronary Interventions (PCIs) Coded for Acute Indications in the Outpatient and Inpatient Settings.
A, Acute outpatient PCIs. B, Acute inpatient PCIs. Proportions reflect PCIs coded for acute indications in the outpatient setting, or PCIs coded for acute indications in the inpatient setting, divided by total PCIs (acute and nonacute in both outpatient and inpatient settings) for each state by year.
Figure 2. Number of Percutaneous Coronary Interventions (PCIs) Performed for Unstable Angina or Acute Myocardial Infarction in the Outpatient Setting .
Number of PCIs in New York (A), Michigan (B), and Florida (C).
Discussion
Overall, we found that outpatient PCIs coded for acute indications increased in 3 states in the years following initiatives designed to reduce rates of inappropriate PCIs. In New York, the proportion of PCIs labeled as acute, but performed as outpatient procedures, increased 14-fold, driven largely by a rise in PCIs performed for UA. Similar, but less pronounced, patterns were observed in Michigan and Florida.
The observed rise in outpatient PCIs performed for acute indications is inconsistent with population-level trends.5 Our data raise the possibility that physicians increasingly classified patients with stable chest pain as UA in the outpatient setting, or that hospitals shifted coding patterns, potentially owing to external factors including reporting of appropriateness or differences in reimbursement. The significant increase observed in New York may have been driven by additional state policy initiatives—notably, the 2011 announcement that inappropriate PCIs performed for patients insured by Medicaid would no longer be reimbursed.6 It is also possible, however, that outpatient PCIs were coded more accurately or that PCIs performed for acute indications shifted from the inpatient to outpatient setting over time, though the stable-to-rising rates of acute PCI performed in the inpatient setting make this less likely.
Overall, our findings suggest that observed declines in inappropriate PCIs3,4 may, in part, be related to shifts in diagnostic and/or coding practices. Further study is needed to understand the rise in outpatient PCIs coded for UA. These data also highlight the need for developing mechanisms to more accurately assess PCI appropriateness.
References
- 1.Patel MR, Dehmer GJ, Hirshfeld JW, Smith PK, Spertus JA. ACCF/SCAI/STS/AATS/AHA/ASNC 2009 Appropriateness Criteria for Coronary Revascularization: A Report of the American College of Cardiology Foundation Appropriateness Criteria Task Force, Society for Cardiovascular Angiography and Interventions, Society of Thoracic Surgeons, American Association for Thoracic Surgery, American Heart Association, and the American Society of Nuclear Cardiology: Endorsed by the American Society of Echocardiography, the Heart Failure Society of America, and the Society of Cardiovascular Computed Tomography. Circulation. 2009;119(9):1330-1352. doi: 10.1161/CIRCULATIONAHA.108.191768 [DOI] [PubMed] [Google Scholar]
- 2.Understanding the Reporting of Appropriate Use Criteria in the CathPCI Registry National Cardiovascular Data Registry 2012; https://www.ncdr.com/WebNCDR/docs/default-source/cathpci-auc-documents/auc_companion_guide-2-25-15.pdf?sfvrsn=3. Accessed May 30, 2018.
- 3.Desai NR, Bradley SM, Parzynski CS, et al. Appropriate use criteria for coronary revascularization and trends in utilization, patient selection, and appropriateness of percutaneous coronary intervention. JAMA. 2015;314(19):2045-2053. doi: 10.1001/jama.2015.13764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hannan EL, Samadashvili Z, Cozzens K, et al. Changes in percutaneous coronary interventions deemed “inappropriate” by appropriate use criteria. J Am Coll Cardiol. 2017;69(10):1234-1242. doi: 10.1016/j.jacc.2016.12.025 [DOI] [PubMed] [Google Scholar]
- 5.Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med. 2010;362(23):2155-2165. doi: 10.1056/NEJMoa0908610 [DOI] [PubMed] [Google Scholar]
- 6.Medicaid Redesign Team; Basic Benefit Review Work Group Final Recommendations. New York State Department of Health 2011; https://www.health.ny.gov/health_care/medicaid/redesign/docs/basic_benefit_review_wrk_grp_final_rpt.pdf. Accessed August 8, 2018.