Key Points
Question
What is the prevalence of a false-negative result of intraoperative consultation on surgical margins during curative intent resection of gastric or gastroesophageal adenocarcinoma?
Findings
In this study of 2002 patients with 3171 intraoperative consultations on surgical margins, the prevalence of a false-negative result was 1.7%. Duodenal margins, diffuse or signet ring disease, and not receiving neoadjuvant radiotherapy were associated with less accurate results.
Meaning
The findings suggest that Intraoperative consultations on surgical margins are accurate but select clinical scenarios are at risk for false-negative results, providing a framework for expectations of the utility of intraoperative consultations on surgical margins during curative intent surgery.
Abstract
Importance
Intraoperative consultation (IOC) on surgical margins during curative intent resection of gastric and gastroesophageal adenocarcinoma presents sampling and interpretive challenges. A false-negative (FN) IOC result can affect clinical care. Many factors may be associated with higher risk for an FN result of IOC on surgical margins.
Objective
To assess the prevalence and clinical implications of FN results of IOC on surgical margins during resection of gastric and gastroesophageal adenocarcinoma.
Design, Setting, and Participants
This retrospective study assessed the results of IOC on surgical margins to determine the prevalence of FN results and the accuracy and clinical implications of the results for patients undergoing curative intent resection for gastric or gastroesophageal adenocarcinoma. The study examined patients with gastric or gastroesophageal adenocarcinoma who underwent resection with curative intent at a single-institution referral center from January 1, 1992, to December 31, 2015.
Interventions
Curative intent gastric and/or esophageal resection.
Main Outcomes and Measures
False-negative results of IOC on surgical margins, accuracy of the results, factors associated with decreased accuracy of the results, and clinical implications of FN results.
Results
This study included 2002 patients (median age, 65 years; 1343 [67.1%] male; 1638 [81.8%] white) who received 3171 IOCs on surgical margins. Of the 3171 IOCs, the prevalence of FN results was 1.7%, with an accuracy of 98.1%. The prevalence of an FN IOC result was 1.2% for esophageal margins, 2.0% for gastric margins, and 2.5% for duodenal margins (P = .04). The prevalence of an FN IOC result was higher for patients with diffuse or signet ring disease compared with those without (2.6% vs 1.2%, P = .002) and for those not receiving neoadjuvant radiotherapy compared with those receiving neoadjuvant radiotherapy (1.4% vs 0.7%, P < .001). The prevalence of FN results of IOCs performed by nongastrointestinal pathologists was similar to that of IOCs performed by gastrointestinal pathologists (2.3% vs 1.9%, P = .60). The disease-specific survival was 34 months (95% CI, 20.7-47.2 months) for those with an FN result and 26.9 months (95% CI, 18.3-35.4; P = .72) for those with a true-positive result. Half of the patients with FN IOC results received further margin-directed therapy, including subsequent resection or radiotherapy.
Conclusions and Relevance
This study found that IOC on surgical margins was accurate at a specialty center. Signet ring or diffuse disease, duodenal margins, and not receiving neoadjuvant radiotherapy were challenging scenarios for IOC on surgical margins. The use of IOC on surgical margins may be optimal when it will affect intraoperative decision making framed by the stage of disease, tumor location, and surgical fitness of the patient.
This study assesses the prevalence of false-negative results and the accuracy of intraoperative consultations on surgical margins in patients undergoing curative intent resection for gastric or gastroesophageal adenocarcinoma.
Introduction
Gastric and gastroesophageal junction adenocarcinoma is increasing in incidence, representing the fourth most common cancer worldwide. Patients presenting with locoregional disease have estimated 5-year survival rates of 36% to 75%.1,2 R1 resection is an independent factor associated with decreased survival in patients with T1 to T2 disease who have fewer than 3 positive lymph nodes.3 Conversion from an R1 to R0 resection based on intraoperative consultation (IOC) on surgical margins seems to be associated with a decreased rate of local anastomotic recurrence.4 An IOC on surgical margins requires prolonged operative time adherence by the pathologist to the College of American Pathologists (CAP) benchmarks.5
Spicer et al6 reported that signet ring disease was challenging during IOC on surgical margins for esophageal, gastroesophageal, and gastric tumors at a large university setting. This study had a limited number of patients, with heterogeneous methods for identifying margin involvement with cancer. Squires et al4 noted malignant involvement in 13% of proximal margins evaluated by IOC. They did not comment on any factors or the outcomes in patients who were found to have a false-negative (FN) result of IOC on surgical margins.
We frequently use IOC on surgical margins during curative intent resection of gastroesophageal and gastric adenocarcinoma. We performed a retrospective review of all patients who underwent IOC to ascertain the concordance between frozen section and permanent section margin status to define the prevalence of FN results and accuracy of IOC results. In addition, we sought to define the clinicopathologic and technical factors that are associated with the prevalence of FN results of IOC. Lastly, we sought to define the clinical implications of FN IOC results.
Methods
Consecutive patients undergoing resection with curative intent for gastroesophageal (Seiwert II-III) and gastric adenocarcinoma from January 1, 1992, to December 31, 2015, at Memorial Sloan Kettering Cancer Center (MSKCC) were identified. Data on patient demographics, treatment, and pathologic factors, including stage, histologic subtype, and differentiation, were collected. This study was reviewed and approved by the MSKCC Institutional Review Board. Informed consent was exempt because of the retrospective nature of the study. Data were not deidentified but encrypted to be assessed only by the study investigators.
We collected data on IOC variables, including which margin(s) was used for the IOC, the IOC margin status (positive or negative), the pathologist and his/her specialty, the distance from the gross margin to the tumor, and the preparation method. Any change in patient treatment in response to an FN result of margin IOC was reviewed.
The IOC results were compared with their respective formalin-fixed, permanent results. A single patient may have had multiple IOC results during an operation. Each IOC result was evaluated to determine whether the result was true-negative (TN), true-positive (TP), FN, or false-positive (FP). Three investigators (J.C.M., K.K., and K.L.O.) determined whether the IOC result was true or false. In a masked fashion, one specialized gastrointestinal pathologist (L.H.T.) reviewed all cases with FN and FP results to determine whether sampling or interpretation error occurred. Sampling error was defined as an error in which insufficient, inadequate, or nonrepresentative tissue was examined for IOC analysis. An interpretation error was defined as an error in diagnosis of cells present on the slides evaluated during IOC.
Statistical Analysis
Descriptive statistics, accuracy, sensitivity, specificity, positive predictive value, negative predictive value, and FN rate were calculated for the IOC. The Fisher exact test was used to compare categorical variables. Kaplan-Meier estimates were used for disease-specific survival. Microsoft Excel (Microsoft Inc) and SPSS, version 24 (IBM Corp) were used for all statistical analyses. Two-sided P ≤ .05 was considered to be statistically significant.
Results
Patient, Tumor, and Treatment Characteristics
Of the 2706 patients who underwent resection with curative intent, 2002 (74.0%) (median age, 65 years; 1343 [67.1%] male; 1638 [81.8%] white) had an IOC on surgical margins performed. A total of 843 patients (42%) had IOC of the proximal margin only, 48 (2%) of the distal margin only, and 1111 (56%) of both proximal and distal margins; IOC was not performed for 704 patients (26%). The clinicopathologic data are summarized in Table 1. The treatment of these patients is summarized in Table 2. A total of 902 patients (45.1%) received neoadjuvant chemotherapy and/or radiotherapy. A total of 1211 patients (60.5%) had received a gastric resection for a gastric or gastroesophageal junction tumor, with the remaining 791 (39.5%) undergoing an esophagectomy for gastroesophageal tumors.
Table 1. Baseline Characteristics, Pathologic Stage, and Treatmenta.
| Variable | Findings (N = 2002) |
|---|---|
| Age, median (range), y | 65 (17-96) |
| Sex | |
| Male | 1343 (67.1) |
| Female | 659 (32.9) |
| Race/ethnicity | |
| White | 1638 (81.8) |
| African American | 111 (5.5) |
| Asian | 191 (9.5) |
| Other | 62 (3.1) |
| Pathologic stage | |
| 0 | 112 (5.6) |
| IA | 400 (20.0) |
| IB | 200 (10.0) |
| IIA | 194 (9.7) |
| IIB | 332 (16.6) |
| IIIA | 245 (12.2) |
| IIIB | 219 (10.9) |
| IIIC | 203 (10.1) |
| IV | 97 (4.8) |
| Pathologic T stage | |
| T0 | 120 (6.0) |
| T1 | 529 (26.4) |
| T2 | 272 (13.6) |
| T3 | 676 (33.8) |
| T4 | 405 (20.2) |
| Pathologic N and M stages | |
| N0 | 1014 (50.6) |
| N1 | 367 (18.3) |
| N2 | 300 (15.0) |
| N3 | 321 (16.0) |
| M1 | 97 (4.8) |
| Differentiation | |
| Unknown grade | 20 (1.0) |
| Well | 101 (5.0) |
| Moderate | 661 (33.0) |
| Poor | 1220 (60.9) |
| Lauren classification | |
| Diffuse | 534 (26.7) |
| Intestinal | 1147 (57.3) |
| Mixed | 271 (13.5) |
| Not stated | 50 (2.5) |
| WHO classification | |
| Signet ring | 564 (28.2) |
| Other | 1333 (66.6) |
| Not stated | 105 (5.2) |
| LVI | |
| Yes | 864 (43.2) |
| No | 1111 (55.5) |
| Not stated | 27 (1.3) |
| PNI | |
| Yes | 826 (41.3) |
| No | 1137 (56.8) |
| Not stated | 39 (1.9) |
Abbreviations: LVI, lymphovascular invasion; PNI, perineural invasion; WHO, World Health Organization.
Data are presented as number (percentage) of patients unless otherwise indicated.
Table 2. Treatment of the Cohort With Gastric and Gastroesophageal Adenocarcinomaa.
| Variable | Finding (N = 2002) |
|---|---|
| Neoadjuvant treatment | |
| Chemotherapy | 481 (24.0) |
| Radiation | 421 (21.0) |
| None | 1100 (54.9) |
| Operation | |
| Esophagectomy | 791 (39.5) |
| Proximal gastrectomy | 75 (3.7) |
| Total gastrectomy | 442 (22.1) |
| Distal gastrectomy | 679 (33.9) |
| Wedge resection | 15 (0.7) |
| IOC proximal margin location | |
| Esophagus | 1275 (63.7) |
| Gastric | 679 (33.9) |
| Not stated | 48 (2.4) |
| IOC distal margin location | |
| Gastric | 835 (41.7) |
| Duodenal | 316 (15.8) |
| Not stated | 851 (42.5) |
| Gross margin, median (range), cm | |
| Proximal | 3.5 (0-27) |
| Distal | 4.5 (0-39) |
Abbreviation: IOC, intraoperative consultation.
Data are presented as number (percentage) of patients unless otherwise indicated.
A total of 1275 IOCs (63.7%) on proximal margins were esophageal, including the proximal resection margin for both gastrectomy (total or proximal) and esophagectomy. Among patients who received an IOC on distal margins, most IOCs were for a gastric margin in patients who underwent an esophagectomy or proximal gastrectomy. A total of 1954 patients had a proximal margin evaluated by IOC. A total of 1159 patients had a distal margin evaluated by IOC. The median gross distance from the tumor was 3.5 cm proximally and 4.5 cm distally.
Of the 2002 patients, 1841 (92.0%) had a pathologic R0 resection indicated on the final pathology report. A total of 160 patients (8.0%) in this cohort had an R1 resection indicated on the final pathology report. Of the 160 patients who underwent an R1 resection, the deep margin was the only margin positive in 46 (28.8). Therefore, the final proximal and/or distal margin was positive in 114 patients (5.7%). Seventy-two patients (3.6%) had a TP result on the IOC. Fifty-one (2.5%) of these patients had a TP proximal margin result during total gastrectomy or esophagectomy. Ten patients (0.5%) had a TP distal margin result during a total gastrectomy or distal gastrectomy. Resection to achieve a TN margin result was presumed to be associated with high morbidity or believed not to be beneficial.
Prevalence of FN Results and the Accuracy of IOC Results
A total of 2004 IOCs on proximal margins were performed on 1954 patients. A total of 1167 IOCs on distal margins were performed on 1159 patients. The overall diagnostic accuracy for the IOC was 98.1% (Table 3). Of the 3171 margins evaluated by IOC, 2930 (92.4%) had TN IOC results and 54 (1.7%) had FN IOC results. For the IOC on surgical margins, the overall specificity was 99.8%, the sensitivity was 77.0%, the positive predictive value was 96.3%, the negative predictive value was 98.2%, and the FN rate was 23.0%.
Table 3. Prevalence of False-Negative Results and Accuracy.
| Variable | Prevalence of False-Negative Results, % | Accuracy, % | P Value |
|---|---|---|---|
| Overall | 1.7 | 98.1 | NA |
| Margin | |||
| Esophageal | 1.2 | 98.7 | .05 |
| Gastric | 2.0 | 97.8 | |
| Duodenal | 2.5 | 96.8 | |
| Disease type | |||
| Signet ring | 3.0 | 96.7 | <.001 |
| Non–signet ring | 1.2 | 98.6 | |
| Diffuse | 2.7 | 96.9 | .007 |
| Nondiffuse | 1.4 | 98.4 | |
| Signet ring and diffuse | 2.6 | 97.1 | .002 |
| Non–signet ring and diffuse | 1.2 | 98.7 | |
| Treatment | |||
| Neoadjuvant chemotherapy | 2.9 | 97.1 | .06 |
| No neoadjuvant chemotherapy | 1.4 | 98.3 | |
| Neoadjuvant radiotherapy | 0.7 | 99.3 | <.001 |
| No neoadjuvant radiotherapy | 1.4 | 98.4 | |
| Risk factorsa | |||
| Risk features | 4.7 | 95.3 | <.001 |
| No risk features | 0.8 | 99.0 | |
| Pathologist | |||
| Gastrointestinal | 1.9 | 98.1 | .60 |
| Nongastrointestinal | 2.3 | 97.6 |
Abbreviation: NA, not applicable.
Risk factors include diffuse and signet ring disease, neoadjuvant chemotherapy, and no neoadjuvant radiotherapy.
Distance From the Tumor and Margin
The median gross proximal esophageal margin for those with a positive IOC result (TP or FN) was 1.4 cm (95% CI, 0.5-2.3 cm). The median gross proximal esophageal margin for those with a negative IOC result (TN or FP) was 4.2 cm (95% CI, 3.9-4.4 cm; P < .001). The median gross proximal gastric margin for those with a positive IOC result (TP or FN) was 1.0 cm (95% CI, 0.4-1.5 cm). The median gross proximal gastric margin for those with a negative IOC result (TN or FP) was 3.0 cm (95% CI, 2.6-3.4 cm; P = .003). Twenty-four percent of proximal margin IOCs within 1 cm of gross tumor had TP or FN results, whereas 3.7% had TP or FN results if more than 3 cm from gross tumor (eFigure 1 in the Supplement). The median gross distal gastric or duodenal margin for those undergoing an R0 or R1 resection was 4.5 cm. Nineteen percent of distal margin IOCs within 1 cm of gross tumor had TP or FN results, whereas 3.3% had TP or FN results if more than 3 cm from gross tumor (eFigure 2 in the Supplement).
Table 3 gives the prevalence of FN IOC results according to the location of the margin. The prevalence of FN results of IOCs was 1.2% for esophageal margins, 2.0% for gastric margins, and 2.5% for duodenal margins (P = .04). The overall accuracy was 98.7% for esophageal margins, 97.8% for gastric margins, and 96.8% for duodenal margins. These findings suggest that IOCs of the duodenal margin may be at risk for FN results.
Histologic Subtype
Among the 2296 margins evaluated from patients with non–signet ring adenocarcinoma, 27 IOC results (1.2%) were FN. Among the 876 margins from patients with signet ring adenocarcinoma, 26 IOC results (3.0%) were FN (P < .001). The accuracy of IOC results for non–signet ring disease was 98.6%. The accuracy of IOC results for signet ring disease was 96.7%, suggesting that identification of signet ring disease may be challenging at the time of IOC.
Of the 2246 margins evaluated by IOC from patients with nondiffuse adenocarcinoma, 31 (1.4%) tested FN. Of the 845 margins evaluated by IOC from patients with diffuse adenocarcinoma, 23 (2.7%) tested FN (P = .007). The accuracy of IOC results for nondiffuse disease was 98.4%. The accuracy of IOC results for diffuse disease was 96.9%, suggesting that identification of tumor cells of diffuse disease may be challenging at the time of IOC.
Tumors classified as signet ring or diffuse largely overlapped, and the prevalence of an FN result of IOC and accuracy of the results were similar for these histologic types. The prevalence of an FN IOC result among patients with diffuse and/or signet ring disease was 2.6% compared with 1.2% among those without diffuse or signet ring disease (P = .002). The accuracy of IOC results among patients with diffuse and/or signet ring disease was 97.1%. The accuracy of IOC results among those with nondiffuse and/or non–signet ring disease was 98.7%, suggesting that identification of diffuse or signet ring disease may be associated with difficulty and decreased accuracy during IOC on surgical margins.
Neoadjuvant Therapy
Of 716 margins evaluated from patients who received neoadjuvant chemotherapy, 21 (2.9%) had an FN IOC result. The percentage of FN IOC results was less for those patients who did not receive neoadjuvant chemotherapy (1.4%). However, this difference was not statistically significant (P = .06). The accuracy of the IOC results for those receiving neoadjuvant chemotherapy was 97.1%, whereas the accuracy was 98.3% for those not receiving neoadjuvant chemotherapy, suggesting that neoadjuvant chemotherapy does not affect IOC results.
A total of 421 patients of the 2002 evaluated in this study received neoadjuvant radiotherapy. All of these patients underwent curative intent resection with esophagogastrectomy or total gastrectomy for gastroesophageal tumors. In this subset of patients who received neoadjuvant radiotherapy, 418 proximal margins were evaluated by IOC, whereas 364 distal margins were evaluated by IOC. The prevalence of an FN IOC result among those receiving neoadjuvant radiotherapy was 0.7% compared with 1.4% among those not receiving neoadjuvant radiotherapy (P < .001). The accuracy of IOC results among those receiving neoadjuvant radiotherapy was 99.3% compared with 98.4% among those not receiving neoadjuvant radiotherapy, suggesting that neoadjuvant radiotherapy is associated with a decreased risk of an FN IOC result.
Combined Risk Factors
A total of 213 margins were evaluated by IOC in patients with diffuse and signet ring disease who were treated with neoadjuvant chemotherapy and no neoadjuvant radiotherapy. The prevalence of an FN IOC result was 4.7%, with an accuracy of 95.3%, in this subset of patients compared with a prevalence of 0.8% and an accuracy of 99.0% in the 957 margins of patients without diffuse and signet ring disease who received neoadjuvant chemotherapy and did not receive neoadjuvant radiotherapy (P < .001). This finding suggests that patients with diffuse and signet ring disease treated with neoadjuvant chemotherapy but not neoadjuvant radiotherapy are at a higher risk of an FN IOC result during their curative intent resection.
Pathologist Subspecialization
Subspecialization of the pathologists who performed the final pathology review was instituted at our institution in 2004; however, this review was not universally adopted for IOC. We therefore sought to determine whether pathologist subspecialization at the time of IOC was associated with the prevalence of FN results and the accuracy of the IOC results (Table 3). Of the 1150 patients who underwent resection from 2004 to 2015, a total of 184 (16%) had a gastrointestinal pathologist perform or participate in the IOC. A total of 966 patients (84%) did not have a gastrointestinal pathologist perform the IOC. The prevalence of an FN margin IOC result was 1.9% for a gastrointestinal pathologist compared with 2.3% for a nongastrointestinal pathologist (P = .60). The accuracy of the IOC result for a gastrointestinal pathologist was 98.1% vs 97.6% for nongastrointestinal pathologists. The associations regarding specialization were not statistically significant (P = .60).
Interpretive vs Sampling Errors
Sampling error was determined to be responsible for 50% of FN results. The other 50% were determined to be attributable to an interpretation error. Overall, errors in interpretation occurred in 1% of all margin IOC assessments. The method for handling the margin IOC was not documented in 53% of cases. The entire margin was evaluated by IOC in 23% of cases. For the 36 FN results of IOC on proximal margins, 3 margins (8.3%) were evaluated entirely, 23 (63.9%) were representative sections, and this information was not recorded in 10 cases (27.8%). For the 19 FN results of IOC on distal margins, 2 margins (11.1%) were evaluated entirely, 8 margins (44.4%) were representative sections, and this information was not recorded in 9 cases (50.0%).
Clinical Implications of a False IOC Result
Of the 2002 patients who received an IOC on surgical margins, 61 (3.0%) had an FN or FP result; 54 patients had an FN result, and 7 had an FP result. Of the 7 patients with an FP result, 3 had another margin evaluated during the index operation, which was a TN margin. The other 4 patients ultimately had no margin involvement on the final pathology report and did not receive treatment.
Of the 61 patients, 54 had an FN IOC result. Eleven patients had another margin evaluated that produced a true IOC result. The reason for the evaluation of an additional margin is unknown. The remaining 43 patients underwent an R1 resection at the index operation. Twelve (27.9%) of these 43 patients had no change in their postoperative management. Seven patients (16.3%) underwent another operation (4 completion gastrectomies, 2 subtotal gastrectomies, and 1 pancreaticoduodenectomy). Twenty patients (46.5%) received adjuvant radiotherapy. Four patients (9.3%) had disease progression before planned therapy.
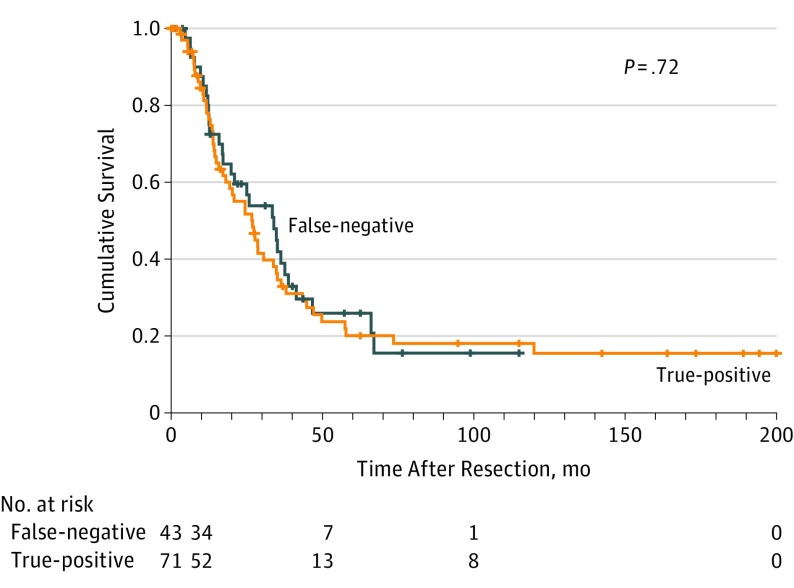
The median disease-specific survival was 34.0 months (95% CI, 20.7-47.2 months) among patients with an FN IOC result (Figure). The median disease-specific survival was 26.9 months (95% CI, 18.3-35.4 months; P = .72) among those with a TP IOC result.
Figure. Disease-Specific Survival Among Patients With False Intraoperative Consultation Results.
Discussion
The purpose of IOC on surgical margins is to assure the surgeon and patient of complete extirpation. False results have significant clinical consequences. Patients, surgeons, and pathologists should share a common understanding of the clinical significance of margin IOC during curative intent resection of gastric and gastroesophageal adenocarcinoma. Our high-volume experience at MSKCC and frequent use of IOC on surgical margins provide a unique opportunity to frame expectations of IOC.
Our study found that the prevalence of an FN IOC result was 1.7%, with an overall accuracy of 98.1%, which is congruent with previously reported series.4,6 The overall discordant rate in this study was 1.9% (1.7% FN and 0.2% FP results). The CAP has established benchmarks for anatomical pathologic error.7 These benchmarks were established on the basis of large studies8,9,10 that evaluated the discordance rate of frozen section consultation and final pathologic diagnoses. These studies8,9,10 found a discordance rate of approximately 2.0% for neoplastic cases. Margin IOCs performed by gastrointestinal and nongastrointestinal pathologists were within the CAP benchmarks.
Better understanding of risk factors associated with an incorrect IOC result might lead to quality control initiatives to improve IOC result accuracy. We found that the accuracy of the results for each subset evaluated was greater than 97%. However, the prevalence of an FN result was variable, from 3.0% for IOCs performed on patients with signet ring disease to 0.7% for IOCs evaluated in those receiving neoadjuvant radiotherapy. Spicer at al6 presented their experience with IOC on surgical margins for gastroesophageal and gastric adenocarcinoma and suggested that signet ring disease presents difficulty in interpretation of results. Of the 6 cases with FN IOC results, 5 were signet ring disease. In our study, the prevalence of FN IOC results was increased among patients with signet ring and diffuse disease. We combined these pathologic risk factors with treatment factors and found a greatly increased prevalence of FN results at 4.7%. Patients with signet ring and diffuse disease treated without neoadjuvant radiotherapy had a higher risk for an FN result.
We expect that specialization in gastrointestinal pathology by the pathologists performing the IOC would improve the accuracy of IOC results. We found that the accuracy of the IOC result was similar between nongastrointestinal pathologists and gastrointestinal pathologists. The percentage of discordant IOC results was 1.9% for gastrointestinal pathologists and 2.4% for nongastrointestinal pathologists. This finding may have important implications on surgical pathologic call structures, but these results should be interpreted with caution. The sampling error was 50%, meaning that overall, only 1% of discordance was related to interpretation error, which is well within the CAP guidelines.
Another aim of our study was to evaluate the clinical implications of an FN IOC result. In our series, 43 patients had an FN status after the primary surgery. A previous study3 found that an R1 resection was clinically important for those with T3 disease with fewer than 3 positive lymph nodes. This subset represented 43% of the entire cohort in our study. In another study,4 which specifically evaluated the utility of margin IOC during curative resection for gastroesophageal cancer, conversion from an R1 to an R0 resection based on margin IOC was associated with a decrease in local recurrence but not overall survival. In the context of aggressive pathologic factors, margin status associated with survival. These data indicate that survival is determined more by the biological mechanisms of the disease than by margin status alone. This concept is further supported by our data indicating similar survival among patients with FN or TP margin results.
Limitations
Our study is limited in important ways. We did not examine the cases in which IOC on surgical margins was not performed (704 cases [26.0%] of the entire experience). The prevailing reason why IOCs are not being performed in this subset of patients is unclear. Our current approach is to perform margin IOC when it would affect an intraoperative decision. We recognize that margins are not indicators of survival in patients with T2 disease with less than 3 positive lymph nodes.3 We would probably not use IOC on surgical margins in a patient with advanced disease if a negative margin would require pancreatic resection or thoracotomy. Moreover, on the basis of our results, curative intent resection in which the margin is within 3 cm of gross tumor may benefit from IOC.
For practical reasons, the entire margin was not evaluated in most of the documented gastric margin IOCs. Representative sectioning for IOC on surgical margins may contribute to false IOC results. Evaluation of the entire margin during IOC may improve the quality of IOC.
Despite technical and interpretive difficulties, the results of IOC on surgical margins for gastroesophageal and gastric adenocarcinoma are accurate at a specialty center. In our experience, the clinical implications of an FN IOC result are varied. The consequences of an FN IOC result on long-term outcome appear to be minor based on our survival analysis.
Conclusions
The findings of our study suggest that the uncommon FN IOC result should be interpreted in the context of the stage of disease, patient risk factors, and the understanding that there are few data that support survival benefit of additional local therapy. The results of this study may help to provide surgeons, pathologists, and patients with expectations for the role of IOC at the time of resection of gastroesophageal junction and gastric adenocarcinoma.
eFigure 1. Percentage of Negative Margins and Positive Margins by IOC vs Gross Distance From the Tumor at the Proximal Margin
eFigure 2. Percentage of Negative Margins and Positive Margins by IOC vs Gross Distance From the Tumor at the Distal Margin
References
- 1.Cunningham D, Allum WH, Stenning SP, et al. ; MAGIC Trial Participants . Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl J Med. 2006;355(1):11-20. doi: 10.1056/NEJMoa055531 [DOI] [PubMed] [Google Scholar]
- 2.Park SH, Sohn TS, Lee J, et al. Phase III trial to compare adjuvant chemotherapy with capecitabine and cisplatin versus concurrent chemoradiotherapy in gastric cancer: final report of the Adjuvant Chemoradiotherapy in Stomach Tumors Trial, including survival and subset analyses. J Clin Oncol. 2015;33(28):3130-3136. doi: 10.1200/JCO.2014.58.3930 [DOI] [PubMed] [Google Scholar]
- 3.Bickenbach KA, Gonen M, Strong V, Brennan MF, Coit DG. Association of positive transection margins with gastric cancer survival and local recurrence. Ann Surg Oncol. 2013;20(8):2663-2668. doi: 10.1245/s10434-013-2950-5 [DOI] [PubMed] [Google Scholar]
- 4.Squires MH III, Kooby DA, Pawlik TM, et al. Utility of the proximal margin frozen section for resection of gastric adenocarcinoma: a 7-institution study of the US Gastric Cancer Collaborative. Ann Surg Oncol. 2014;21(13):4202-4210. doi: 10.1245/s10434-014-3834-z [DOI] [PubMed] [Google Scholar]
- 5.Tworek JA, Volmar KE, McCall SJ, Bashleben CP, Howanitz PJ. Q-Probes studies in anatomic pathology: quality improvement through targeted benchmarking. Arch Pathol Lab Med. 2014;138(9):1156-1166. doi: 10.5858/arpa.2014-0149-OA [DOI] [PubMed] [Google Scholar]
- 6.Spicer J, Benay C, Lee L, et al. Diagnostic accuracy and utility of intraoperative microscopic margin analysis of gastric and esophageal adenocarcinoma. Ann Surg Oncol. 2014;21(8):2580-2586. doi: 10.1245/s10434-014-3669-7 [DOI] [PubMed] [Google Scholar]
- 7.Nakhleh RE, Nosé V, Colasacco C, et al. Interpretive diagnostic error reduction in surgical pathology and cytology: guideline from the College of American Pathologists Pathology and Laboratory Quality Center and the Association of Directors of Anatomic and Surgical Pathology. Arch Pathol Lab Med. 2016;140(1):29-40. doi: 10.5858/arpa.2014-0511-SA [DOI] [PubMed] [Google Scholar]
- 8.Gephardt GN, Zarbo RJ. Interinstitutional comparison of frozen section consultations: a College of American Pathologists Q-Probes study of 90,538 cases in 461 institutions. Arch Pathol Lab Med. 1996;120(9):804-809. [PubMed] [Google Scholar]
- 9.Novis DA, Gephardt GN, Zarbo RJ; College of American Pathologists . Interinstitutional comparison of frozen section consultation in small hospitals: a College of American Pathologists Q-Probes study of 18,532 frozen section consultation diagnoses in 233 small hospitals. Arch Pathol Lab Med. 1996;120(12):1087-1093. [PubMed] [Google Scholar]
- 10.Raab SS, Tworek JA, Souers R, Zarbo RJ. The value of monitoring frozen section-permanent section correlation data over time. Arch Pathol Lab Med. 2006;130(3):337-342. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. Percentage of Negative Margins and Positive Margins by IOC vs Gross Distance From the Tumor at the Proximal Margin
eFigure 2. Percentage of Negative Margins and Positive Margins by IOC vs Gross Distance From the Tumor at the Distal Margin