Key Points
Question
Is nonoperative management of appendicitis effective in a national retrospective cohort?
Findings
In a national cohort analysis of 58 329 patients with uncomplicated appendicitis, patients treated nonoperatively had higher rates of abscess (2.3% vs 1.3%) and readmission (all-cause, 4.6% vs 2.5%; appendicitis-associated, 2.6% vs 1.2%) and higher overall cost of care ($14 934 vs $14 186). The overall failure rate of nonoperative management was 3.9%.
Meaning
Although the overall failure rate of nonoperative management of appendicitis was very low, nonoperative management was associated with worse short-term outcomes compared with appendectomy.
This cohort study compares the outcomes of nonoperatively managed appendicitis against appendectomy in patients with uncomplicated appendicitis from a private insurance claims database.
Abstract
Importance
Health care professionals have shown significant interest in nonoperative management for uncomplicated appendicitis, but long-term population-level data are lacking.
Objective
To compare the outcomes of nonoperatively managed appendicitis against appendectomy.
Design, Setting, and Participants
This national retrospective cohort study used claims data from a private insurance database to compare patients admitted with uncomplicated appendicitis from January 1, 2008, through December 31, 2014, undergoing appendectomy vs nonoperative management. Coarsened exact matching was applied before multivariate analysis to reduce imbalance between groups. Data were analyzed from February 12 through May 1, 2018.
Exposures
Appendectomy (control arm) or nonoperative management (treatment arm).
Main Outcomes and Measures
Short-term primary clinical outcomes included emergency department visits, hospital readmission, abdominal abscess, and Clostridium difficile infections. Long-term primary clinical outcomes were small-bowel obstructions, incisional hernias, and appendiceal cancers. Nonoperative management failure was defined by hospital readmission with appendicitis diagnosis and an appendicitis-associated operation or procedure. Secondary outcomes included number of follow-up visits, length and cost of index hospitalization, and total cost of appendicitis-associated care. Covariates included age, sex, region, insurance plan type, admission year, and Charlson comorbidity index.
Results
Of 58 329 patients with uncomplicated appendicitis (52.7% men; mean [SD] age, 31.9 [16.5] years), 55 709 (95.5%) underwent appendectomy and 2620 (4.5%) underwent nonoperative management. Patients in the nonoperative management group were more likely to have appendicitis-associated readmissions (adjusted odds ratio, 2.13; 95% CI, 1.63-2.77; P < .001) and to develop an abscess (adjusted odds ratio, 1.42; 95% CI, 1.05-1.92; P = .02). Patients in the nonoperative management group required more follow-up visits in the year after index admission (unadjusted mean [SD], 1.6 [6.3] vs 0.3 [1.4] visits; adjusted +1.11 visits; P < .001) and had lower index hospitalization cost (unadjusted mean [SD], $11 502 [$9287] vs $13 551 [$10 160]; adjusted −$2117, P < .001), but total cost of appendicitis care was higher when follow-up care was considered (unadjusted, $14 934 [$31 122] vs $14 186 [$10 889]; adjusted +$785; P = .003). During a mean (SD) of 3.2 (1.7) years of follow-up, failure of nonoperative management occurred in 101 patients (3.9%); median time to recurrence was 42 days (interquartile range, 8-125 days). Among the patients who experienced treatment failure, 44 did so within 30 days.
Conclusions and Relevance
According to results of this study, nonoperative management failure rates were lower than previously reported. Nonoperative management was associated with higher rates of abscess, readmission, and higher overall cost of care. These data suggest that nonoperative management may not be the preferred first-line therapy for all patients with uncomplicated appendicitis.
Introduction
Traditional surgical teaching states that acute appendicitis invariably progresses to gangrene and perforation if not undergoing surgery in a timely fashion.1,2,3 As such, urgent appendectomy has historically been considered the mainstay of treatment. However, appendectomy is not without risk; reported rates of postoperative complications range from 2% to 23%.4,5,6 In addition, long-term complications may occur, including incisional hernias and small-bowel obstructions.7,8,9 Due to sheer volume, appendectomy is the sixth leading cause of morbidity and mortality owing to emergency general surgery in the United States.10
Given the known risks associated with surgery, several randomized clinical trials have compared appendectomy with nonoperative antibiotic management for uncomplicated appendicitis.11,12,13,14,15,16,17 In the largest and most recent randomized trial, 73% of patients treated nonoperatively did not require appendectomy within 1 year of follow-up.14 For the patients with nonoperative treatment who eventually required surgery, the complication rate was no higher than for patients who initially underwent appendectomy. In combination with other existing randomized clinical trials and concordant with recent consensus guidelines,18 these data indicate that nonoperative management is a viable treatment option in most cases and imply that surgery is overused.
Despite randomization, these trials contain limitations that threaten the generalizability of their findings. Existing randomized clinical trials are relatively small, with a maximum follow-up of 2 years. Among the 2 existing studies that examined long-term outcomes of nonoperative management, one was a nonrandomized single-institution study confined to pediatric patients19; the other was regionally limited, unable to censor patients who left the cohort, and conducted a decade ago.20
To address these issues, we assessed nonoperative management of uncomplicated appendicitis using a large private insurance claims database. We hypothesized that (1) nonoperative management would be selected more often than appendectomy for patients deemed high-risk candidates for surgery; (2) nonoperative management would have comparable outcomes with appendectomy; and (3) the overall cost of nonoperative management would be less than that of appendectomy.
Methods
Study Design
We performed a retrospective cohort analysis of patients admitted with uncomplicated appendicitis using the Truven Health MarketScan database from 2007 through 2015. The database contains deidentified patient-level information from inpatient, outpatient, and pharmaceutical claims on 40 to 50 million privately insured patients per year. Claims originate from more than 150 large employer-sponsored health plans and include patients from all 50 states. The database includes demographic characteristics (ie, age, sex, and geographic region), encounter data (ie, hospital admissions, outpatient visits, and associated procedures), pharmaceutical data (ie, medications, days’ supply, dose dispensed, strength, and administration method), and financial data (ie, total cost, copayment, and deductibles). The institutional review board of Stanford University determined that this project did not meet the definition of human subject research and exempted it from further review and informed consent.
Participants
We identified a cohort of patients who underwent inpatient admission from January 1, 2008, through December 31, 2014, with a primary admission diagnosis of acute appendicitis. The American Association for the Surgery of Trauma has recently developed a grading system for appendicitis.21 Grade I appendicitis was classified as uncomplicated acute appendicitis. We elected to focus on uncomplicated appendicitis to avoid bias introduced during complex clinical scenarios not consistent with those studied in randomized clinical trials of nonoperative management. We used International Classification of Diseases, Ninth Revision (ICD-9) codes 540.9 and 541.0 to classify uncomplicated acute appendicitis.21,22,23,24 Patients with co-occurring diagnosis or procedure codes consistent with complicated appendicitis were excluded (ICD-9 codes 472.0, 540.0, 540.1, 54.91, 567.22, and 569.5; Current Procedural Terminology [CPT] codes 10030, 49021, 49405, 49406, 75989, 76942, 77002, and 77012). Patients were classified as undergoing appendectomy if appendectomy procedure codes were present (ICD-9 codes 47.01 and 47.09; CPT codes 44950 and 44970). Patients lacking appendectomy codes were excluded if they had procedure codes for an operation other than appendectomy. The remaining patients were classified as undergoing nonoperative management. We required patients to be continuously enrolled for at least 12 months before the index appendicitis admission to ensure adequate capture of comorbid disease and for at least 12 months afterward to ensure adequate follow-up time.
Outcomes
Our primary outcomes of interest were the clinical outcomes of appendicitis treatment associated with nonoperative management compared with appendectomy. These outcomes included rates of short-term (<30 days) complications (including emergency department visits, all-cause readmissions, appendicitis-associated readmissions, rates of abdominal abscess, and Clostridium difficile diagnoses) (eTable in the Supplement provides a definition of complications) and rates of long-term (≥30 days) complications (including readmission for small-bowel obstruction, diagnosis of incisional hernia, and diagnosis of appendiceal cancer), consistent with published randomized trials.14,15 Secondary outcomes included length of stay during index hospitalization, cost of index hospitalization, number of follow-up visits required in the following year, and the total cost of appendicitis-associated care in the year after diagnosis. Total cost of appendicitis-associated care was determined by summing the total cost for every inpatient and outpatient encounter associated with appendicitis for the following year, including the index hospitalization. Log transformations of hospital length of stay, index hospitalization cost, and total cost of appendicitis care were calculated given the right skewness of the variables and generated similar results.
In post hoc analyses, we assessed rates of nonoperative management failure (<30 days) and rates of appendicitis recurrence (≥30 days) for patients undergoing nonoperative management as well as timing of failure or recurrence. Failure or recurrence was defined as readmission to the hospital with a diagnosis of appendicitis (ICD-9 codes 540.0, 540.1, 540.9, 541.0, and 542.0; International Statistical Classification of Diseases and Related Health Problems, Tenth Revision codes K35.80, K35.89, and K37) and undergoing an appendicitis-associated operation or procedure (ie, appendectomy, right hemicolectomy, or percutaneous drain placement).
We assessed regional variation in nonoperative management by assessing the percentage of total appendicitis cases managed nonoperatively in each metropolitan statistical area (MSA) with at least 10 cases of appendicitis. Urban vs rural patients were categorized by those living in an MSA vs those not.
Variable Classification
The primary independent variable of interest was appendectomy vs nonoperative management. Covariates included age group (<12, 12-18, 19-30, 31-44, and 45-64 years), geographic region, sex, insurance plan type (exclusive or preferred provider organization, health maintenance organization or capitated point-of-service plan, high-deductible or consumer-driven health plan, point of service, and comprehensive health insurance), year of index admission, and Charlson comorbidity index (calculated using inpatient and outpatient claims from the 12-month lead-in period). Reference groups were appendectomy, age 12 to 18 years, Northeast region, exclusive or preferred provider organization insurance type, and Charlson comorbidity index of 0. Financial variables were adjusted to December 2017 dollars using the Consumer Price Index.25
Statistical Analysis
Data were analyzed from February 12 to May 1, 2018. Level of significance was defined a priori as α = .05, and P values were 2-tailed. We did not adjust for multiple comparisons given the exploratory observational nature of our study and the relatively small number of outcomes and to avoid missing any potentially important unknown outcomes (eg, exaggerating type II error).26 Categorical and demographic variables were compared using χ2 tests. A nonparametric test for trend across ordered groups was performed to assess the association between diagnosis year and the use of nonoperative management, as well as the use of laparoscopy. Categorical variables were compared using χ2 tests, and continuous variables were compared using unpaired 2-tailed t tests.
Given the presumed bias in patient selection for nonoperative management, we applied a coarsened exact matching (CEM) algorithm before multivariate analysis to reduce covariate imbalance between groups. Coarsened exact matching is a form of monotonic imbalance bounding in which the balance between treatment and control groups is chosen ex ante27 by pruning observations so that remaining data have improved covariate distributions between the treatment and control groups. In contrast to the common method of propensity score matching, CEM approximates an efficient, fully blocked randomized experiment, which is a more powerful experimental design than complete randomization. Blocking approaches such as CEM allow for improved balance between treatment and control groups, whereas propensity score matching ignores the potentially large imbalance that full blocking can remove.28,29 We then calculated multivariate linear and logistic regressions to compare cohorts preprocessed with CEM. Covariates included in CEM and adjusted for in regression models included age group, sex, geographic region, insurance plan type, year of index hospitalization, and Charlson comorbidity index. Finally, we determined timing of nonoperative management failure or appendicitis recurrence using Kaplan-Meier time-to-event analysis. Patients were censored at the end of continuous plan enrollment.
Missing or unknown demographic data were considered a separate category within each variable. No patients were missing data regarding primary outcomes. Patients missing data regarding secondary outcomes were considered not to have the outcome during their enrollment. All statistical analyses were completed using Stata software (version 14.2; StataCorp).
Results
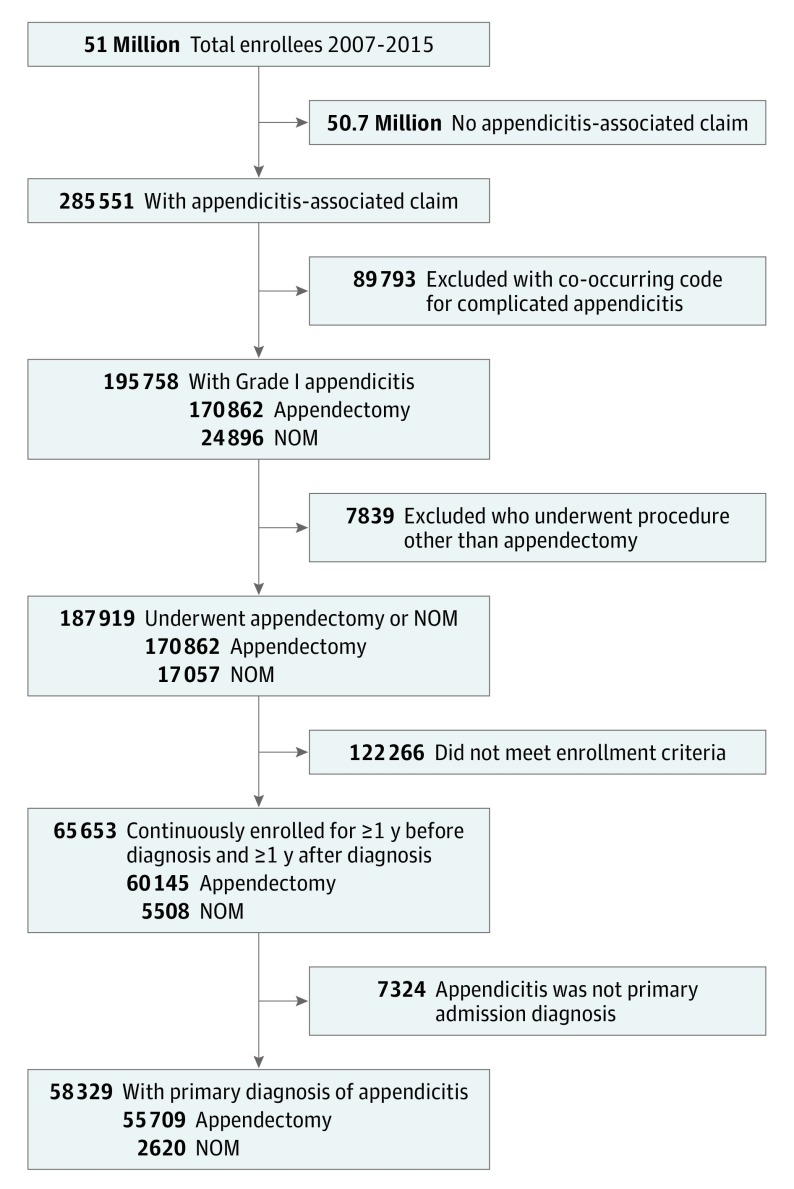
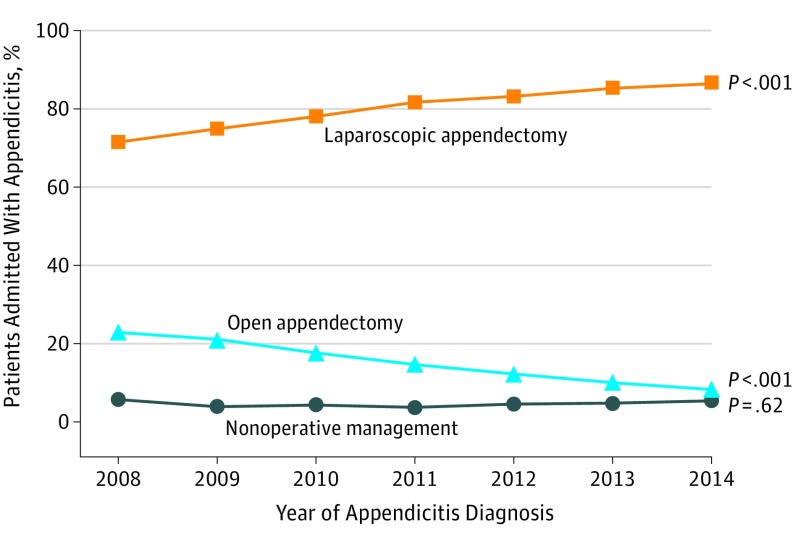
After applying cohort selection criteria, we identified 58 329 patients with a primary admission diagnosis of acute, uncomplicated American Association for the Surgery of Trauma grade I appendicitis (Figure 1) (47.3% women and 52.7% men; mean [SD] age, 31.9 [16.5] years). A total of 55 709 patients underwent appendectomy (95.5%) and 2620 (4.5%) were managed nonoperatively. Although the yearly distribution of appendectomy vs nonoperative management differed (Table 1), we found no significant trend in the percentage of patients who underwent nonoperative management by year (P = .62). Most patients (83.0%) who had an appendectomy underwent a laparoscopic procedure; the percentage of patients who had laparoscopic surgery increased significantly across the study period (6076 [75.8%] in 2008 to 3306 [91.3%] in 2014; P < .001) (Figure 2). Patients who underwent nonoperative management were significantly older (mean [SD] age, 34.2 [16.8] vs 31.8 [16.4] years, P < .001; aged 46-64 years, 824 of 2620 [31.4%] vs 14 362 of 55 709 [25.8%]), had more comorbid conditions (mean [SD] Charlson comorbidity index, 0.37 [1.08] vs 0.26 [0.79], P < .001; Charlson comorbidity index ≥2, 189 of 2620 [7.2%] vs 2613 of 55 709 [4.7%]), and lived in the Northeast (615 of 2620 [23.5%] vs 10 552 of 55 709 [18.9%]) or South (946 of 2620 [36.1%] vs 19 222 of 55 709 [34.5%]) compared with patients who underwent appendectomy (P < .001 for all) (Table 1). We found a significant difference in the type of insurance plans in which the nonoperative and appendectomy groups were enrolled; nonoperative patients were more likely to have high-deductible insurance (235 of 2620 [9.0%] vs 3626 of 55 709 [6.5%]; P < .001). Patients who underwent appendectomy were enrolled in their health plans for a mean (SD) duration of 5 (104) weeks longer than those undergoing nonoperative management, suggesting that patients in the nonoperative group had higher insurance turnover.
Figure 1. Cohort Enrollment Criteria.
NOM indicates nonoperative management.
Table 1. Baseline Demographic Characteristics of Appendicitis Cohort.
| Characteristic | Study Groupa | P Value | |
|---|---|---|---|
| Appendectomy (n = 55 709) | NOM (n = 2620) | ||
| Sex, No. (%) | |||
| Male | 29 358 (52.7) | 1378 (52.6) | .92 |
| Female | 26 351 (47.3) | 1242 (47.4) | |
| Age, mean (SD), y | 31.8 (16.4) | 34.2 (16.8) | <.001 |
| Age group, No. (%) | |||
| <12 y | 5845 (10.5) | 232 (8.8) | <.001 |
| 12-18 y | 10 933 (19.6) | 432 (16.5) | |
| 19-30 y | 10 672 (19.2) | 469 (17.9) | |
| 31-45 y | 13 897 (24.9) | 663 (25.3) | |
| 46-64 y | 14 362 (25.8) | 824 (31.4) | |
| Geographic region, No. (%) | |||
| Northeast | 10 552 (18.9) | 615 (23.5) | <.001 |
| North Central | 10 884 (19.5) | 509 (19.4) | |
| South | 19 222 (34.5) | 946 (36.1) | |
| West | 14 282 (25.6) | 519 (19.8) | |
| Unknown | 769 (1.4) | 31 (1.2) | |
| Insurance type, No. (%) | |||
| EPO or PPO | 35 912 (64.5) | 1647 (62.9) | <.001 |
| HMO or Cap POS | 9529 (17.1) | 416 (15.9) | |
| HDHP or CDHP | 3626 (6.5) | 235 (9.0) | |
| POS | 4357 (7.8) | 217 (8.3) | |
| Comp | 810 (1.4) | 41 (1.6) | |
| Unknown/missing | 1475 (2.6) | 64 (2.4) | |
| Grouped Charlson comorbidity index, No. (%)b | |||
| 0 | 46 286 (83.1) | 2105 (80.3) | <.001 |
| 1 | 6810 (12.2) | 326 (12.4) | |
| ≥2 | 2613 (4.7) | 189 (7.2) | |
| Year of diagnosis, No. (%) | |||
| 2008 | 8016 (14.4) | 486 (18.5) | <.001 |
| 2009 | 9740 (17.5) | 397 (15.2) | |
| 2010 | 10 001 (18.0) | 452 (17.3) | |
| 2011 | 9982 (17.9) | 381 (14.5) | |
| 2012 | 8120 (14.6) | 388 (14.8) | |
| 2013 | 6228 (11.2) | 312 (11.9) | |
| 2014 | 3622 (6.5) | 204 (7.8) | |
| Duration of enrollment, mean (SD), y | 6.0 (2.0) | 5.9 (2.1) | .04 |
| Duration of follow-up, mean (SD), y | 3.2 (1.7) | 3.2 (1.8) | .77 |
Abbreviations: Cap POS, capitated point of service; CDHP, consumer-driven health plan; Comp, comprehensive health insurance; EPO, exclusive provider organization; HDHP, high-deductible health plan; HMO, health maintenance organization; NOM, nonoperative management; POS, point of service; PPO, preferred provider organization.
Percentages have been rounded and may not total 100.
Higher index indicates greater number of comordidities.
Figure 2. Variation in Appendicitis Treatment by Year of Diagnosis.
P values represent the results of a nonparametric test for trend across ordered groups.
After CEM, cohort size was reduced to 44 775 (42 197 in the appendectomy group and 2578 in the nonoperative group). After pruning and weighting by CEM, baseline demographic differences between the 2 cohorts were no longer statistically different.
We determined the rate of short-term complications occurring less than 30 days after the index hospitalization for appendectomy and nonoperative management (Table 2). All-cause readmissions (121 of 2620 [4.6%] vs 1387 of 55 709 [2.5%]; P < .001) and appendicitis-associated readmissions (69 of 2620 [2.6%] vs 652 of 55 709 [1.2%]; P < .001) were significantly higher for patients who underwent nonoperative management. Patients undergoing nonoperative management were significantly more likely to develop an abdominal abscess than those undergoing appendectomy (59 of 2620 [2.3] vs 722 of 55 709 [1.3%; P < .001]; adjusted odds ratio, 1.42 [95% CI, 1.05-1.92; P = .02]). We found no significant differences in rates of emergency department visits or C difficile diagnoses.
Table 2. Complications Following Index Appendicitis Hospitalization.
| Complication | Unadjusted Univariate Analysis | Adjusted Multivariate Analysisa | |||
|---|---|---|---|---|---|
| Study Group, No. (%) | P Value | OR (95% CI) | P Value | ||
| Appendectomy (n = 55 709) | Nonoperative Management (n = 2620) | ||||
| Short-term (<30 d) | |||||
| ED visit | 3299 (5.9) | 169 (6.4) | .26 | 0.96 (0.81-1.14) | .65 |
| All-cause readmission | 1387 (2.5) | 121 (4.6) | <.001 | 1.60 (1.29-1.97) | <.001 |
| Appendicitis-associated readmission | 652 (1.2) | 69 (2.6) | <.001 | 2.13 (1.63-2.77) | <.001 |
| Abscess | 722 (1.3) | 59 (2.3) | <.001 | 1.42 (1.05-1.92) | .02 |
| Clostridium difficile diagnosis | 79 (0.1) | 2 (0.1) | .38 | 0.04 (0-10.32) | .25 |
| Long-term (≥30 d) | |||||
| Admission for SBO | 213 (0.4) | 18 (0.7) | .02 | 1.29 (0.73-2.29) | .38 |
| Incisional hernia | 477 (0.9) | 30 (1.1) | .12 | 1.19 (0.80-1.77) | .39 |
| Appendiceal cancer | 131 (0.2) | 8 (0.3) | .47 | 4.07 (2.56-6.49) | <.001 |
Abbreviations: ED, emergency department; OR, odds ratio; SBO, small-bowel obstruction.
Variables included as covariates in multivariate models were age group, geographic region, sex, insurance plan type, year of index admission, and Charlson comorbidity index.
For long-term complications occurring 30 days or more after the index hospitalization, univariate analysis revealed no statistically significant difference between groups in rates of appendiceal cancer (131 of 55 709 [0.2%] vs 8 of 2620 [0.3%]; P = .47) (Table 2). However, after CEM and multivariate logistic regression, patients treated nonoperatively were more likely to be diagnosed with appendiceal cancer than those who underwent appendectomy (adjusted odds ratio, 4.07; 95% CI, 2.56-6.49; P < .001). Median time to appendiceal cancer diagnosis was 71 days (interquartile range, 41-130 days). No differences occurred in admissions for small-bowel obstruction (adjusted odds ratio, 1.29; 95% CI, 0.73-2.29) or subsequent claims related to incisional hernia (adjusted odds ratio, 1.19; 95% CI, 0.80-1.77).
Patients undergoing nonoperative management experienced statistically significant, albeit small, differences in length of hospital stay compared with patients who underwent appendectomy (unadjusted mean [SD], 1.7 [1.4] vs 1.6 [1.2] days [P < .001]; adjusted +0.15 days, P < .001). Patients who underwent open appendectomy were hospitalized for slightly longer than those treated laparoscopically (unadjusted mean [SD] length of stay, 1.9 [1.6] vs 1.5 [1.1] days [P < .001]; adjusted +0.39 days, P < .001). Patients undergoing nonoperative management had more follow-up visits for appendicitis in the year after hospital discharge compared with those undergoing appendectomy (unadjusted mean [SD], 1.6 [6.3] vs 0.3 [1.4] visits [P < .001]; adjusted, +1.11 visits, P < .001). The mean (SD) cost of the index hospitalization was less for patients undergoing nonoperative management (unadjusted, $11 502 [$9287] vs $13 551 [$10 160] [P < .001]; adjusted −$2117, P < .001). However, when the total cost of appendicitis-associated care was considered (including index hospitalization, outpatient follow-up visits, and readmissions for complications, failure, or recurrence within 1 year after diagnosis), nonoperative management was more expensive (unadjusted mean [SD], $14 934 [$31 122] vs $14 186 [$10 889] [P = .003]; adjusted +$785, P = .003).
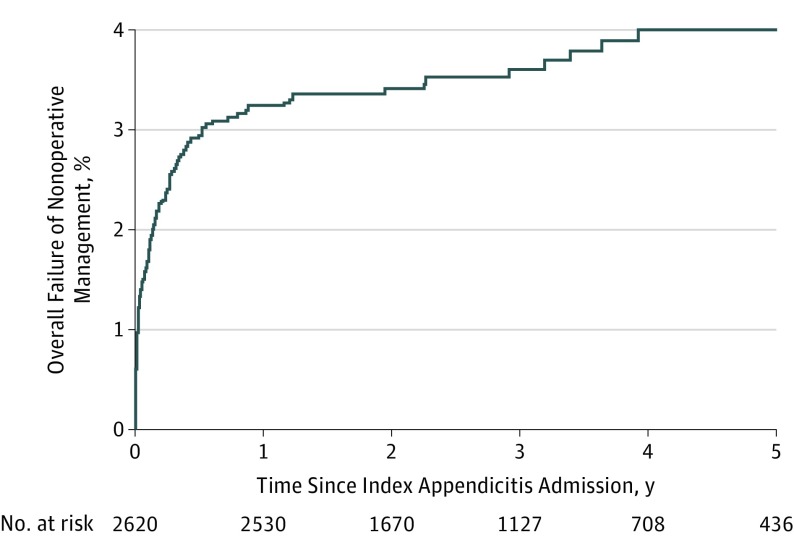
Among patients in whom nonoperative management failed, a total of 44 (1.7% of the nonoperative group) experienced treatment failure within 30 days, resulting in hospital readmission and an appendicitis-associated surgery or procedure. Appendicitis recurred after 30 days in 57 patients (2.2% of patients in the nonoperative management group), who required hospital admission and an appendicitis-associated operation or procedure. Overall, the failure rate of nonoperative management (failure or recurrence leading to operative or procedural intervention) was 3.9% (101 of 2620 patients). Median time from the incident diagnosis to failure or recurrence was 42 days (interquartile range, 8-125 days; mean [SD], 153 [29] days) (Figure 3).
Figure 3. Timing of Overall Failure of Nonoperative Management of Appendicitis by Kaplan-Meier Time-to-Event Analysis.
The overall failure rate of nonoperative management (failure or recurrence leading to operative or procedural intervention) was 3.9%.
We found extensive regional variation in rates of nonoperative management by MSA but no statistically significant difference between urban vs rural areas (2237 of 50 414 [4.4%] vs 383 of 7915 [4.8%]; P = .11) (eFigure in the Supplement). In 69 of the 314 MSAs (22.0%), all cases of uncomplicated appendicitis were managed with appendectomy, whereas the maximum rate of nonoperative management was 20.4% (10 of 49 cases) in 1 MSA.
Discussion
This study is unique in its evaluation of nonoperative management of uncomplicated appendicitis based on its use of a large national cohort, detailed longitudinal cost data, and duration of long-term follow-up (mean [SD], 3.2 [1.7] years, maximum 8 years). We found that patients undergoing nonoperative management had higher rates of readmission and were more likely to develop an abscess. Although the mean index hospitalization cost was less for nonoperative management, the mean total cost of appendicitis-associated care was more expensive for the nonoperative cohort owing to more follow-up visits, readmissions, and additional procedures.
The overall failure rate of nonoperative management, including short-term failures and long-term recurrences, was 3.9%, which is lower than the failure rates reported in existing randomized trials11,12,13,14,15,16,17 but consistent with the failure rate reported in a prior retrospective study.20 The privately insured cohort assessed in this study may have a different failure rate than the general population; alternatively, nonoperative treatment failure may be discovered at higher rates in randomized clinical trials, given careful monitoring for ongoing complications. Although most failures of nonoperative management occurred in the first year, the risk of appendicitis recurrence persisted as long as 4 years after the index hospitalization. This outcome represents a new finding, because no randomized trial, to our knowledge, has followed up patients for longer than 2 years. Furthermore, in the clinical setting, this timeline may exceed a single surgeon’s care, leading to a positively skewed assumption about the success of nonoperative management.
Although overall failure rates were low, those who underwent nonoperative management had an increased risk of abscess, consistent with previous studies of laparoscopic appendectomy30,31,32 and nonoperative management.13,14,15,17 Proponents of nonoperative management note that the crude increase in abscess is only 1%, and many patients may be willing to accept this slight additional risk to avoid surgery. However, this increase in morbidity is also associated with increased costs and the need for additional procedures. Full disclosure for patients considering nonoperative management should include this information.
Patients undergoing nonoperative management also had more all-cause and appendicitis-related readmissions. Our study is nonrandomized and retrospective, so the increased all-cause readmission rate could reflect the worse baseline health of the population undergoing nonoperative management. Higher readmission rates may also reflect a bias by surgeons not comfortable with nonoperative management to readmit patients for observation. Supporting such a possibility is the finding that 25 of 69 patients undergoing appendicitis-related readmission in the nonoperative management group (36%) did not require additional operations or procedures. Despite these potential explanations, differences in readmission rates persisted after CEM and multivariate analysis, suggesting that our findings reflect a true clinical difference. These findings differ from those of prior randomized clinical trials and may indicate that nonoperative management results in worse short-term health when generalized to a broader population.
Higher rates of complications are tied to higher costs. Previous analyses found that nonoperative management is less expensive than appendectomy.13,15,17,33,34,35 Proponents argue that nonoperative management is a cost-effective way to treat appendicitis. However, most studies focus only on the cost of index hospitalization or obtain long-term costs through modeling. The assumptions on which these models are built reference the controlled environment of randomized clinical trials. Our data reflect real-world costs and suggest that, although the index hospitalization is less expensive for nonoperative management, the total cost of appendicitis care is approximately 5.5% higher when managed nonoperatively. Although these data do not account for indirect societal costs, they highlight the importance of considering the total burden of care rather than the index hospitalization alone.
An important consequence of nonoperative management is missed appendiceal cancer. We found that 0.3% of patients undergoing nonoperative management later presented with appendiceal cancer, similar to the cohort that underwent appendectomy (0.2%) and to previous studies that found appendiceal cancer rates ranging from 0.01% to 1.0% in appendectomy specimens after appendicitis.36,37,38,39 However, adjusted analyses suggested that nonoperative management was associated with increased odds of eventual development of appendiceal malignant disease. Given the low rate of appendiceal malignant neoplasms in this cohort, unadjusted analyses suggest that the present study is underpowered to detect a true difference in risk. Any study or clinical pathway involving nonoperative management must consider this potential downstream effect of nonoperative management and use the encounter as an opportunity to counsel patients regarding vigilant future cancer screening.
Although rates of nonoperative management varied across metropolitan areas, broad regional differences were less pronounced. Patients living in the Northeast and South were slightly more likely to undergo nonoperative management compared with those living in the North Central and Western regions. No difference in rates of nonoperative management occurred between urban and rural areas. Previous studies have suggested that patients in rural areas may undergo less surgery than those in urban regions with abundant health care resources40; however, our data do not support a similar regional pattern for appendicitis care.
Limitations
Our study has limitations inherent to administrative claims data, including the ability to accurately identify the nonoperative management cohort. We applied stringent cohort selection criteria to best identify these patients (ie, those requiring a primary diagnosis of uncomplicated appendicitis, excluding those with co-occurring complicated appendicitis codes, and excluding those who underwent procedures other than appendectomy). However, the potential for misclassification remains owing to errors in diagnosis. If these patients instead had another abdominal process, such as gastroenteritis, the outcomes for nonoperative management may appear better than they actually are. We also assumed that all patients who had appendectomies actually had appendicitis, which may not be the case in approximately 10%.41 The privately insured population evaluated in this study may be different than uninsured and government-insured patients; thus, these results may not be generalizable to these populations.
Our data may also have been limited by potential selection bias, because nonoperative management is most commonly used for patients who are poor operative candidates. We therefore corrected for differences between the groups undergoing appendectomy and nonoperative management using a CEM algorithm and multivariate analysis. However, the potential for hidden confounding remains. Patients in the nonoperative group were enrolled in their insurance plans for slightly shorter times than those in the appendectomy group; this small differential loss to follow-up also may contribute to selection bias. Finally, the insurance claims database lacks clinical information that would improve comparisons between patients. Data regarding important clinical characteristics, such as symptom duration on presentation, laboratory data, imaging findings, and presence or absence of appendicolith, would significantly improve patient matching and stratification.
Conclusions
This report is the first national longitudinal study, to our knowledge, assessing the outcomes of nonoperative management of appendicitis. The nonoperative management failure and appendicitis recurrence rates described herein are lower than those reported in previous clinical trials. However, nonoperative management was found to be associated with higher rates of abscess development and readmission and higher overall cost of care. Taken together, these data do not support the use of nonoperative management as first-line therapy for uncomplicated appendicitis until more conclusive randomized clinical trial data become available.
eTable. Definitions of Short- and Long-term Complications
eFigure. Regional Variation in Nonoperative Management of Appendicitis
References
- 1.Ditillo MF, Dziura JD, Rabinovici R. Is it safe to delay appendectomy in adults with acute appendicitis? Ann Surg. 2006;244(5):656-660. doi: 10.1097/01.sla.0000231726.53487.dd [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Eldar S, Nash E, Sabo E, et al. Delay of surgery in acute appendicitis. Am J Surg. 1997;173(3):194-198. doi: 10.1016/S0002-9610(96)00011-6 [DOI] [PubMed] [Google Scholar]
- 3.Temple CL, Huchcroft SA, Temple WJ. The natural history of appendicitis in adults: a prospective study. Ann Surg. 1995;221(3):278-281. doi: 10.1097/00000658-199503000-00010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wilms IM, de Hoog DE, de Visser DC, Janzing HM. Appendectomy versus antibiotic treatment for acute appendicitis. Cochrane Database Syst Rev. 2011;(11):CD008359. [DOI] [PubMed] [Google Scholar]
- 5.Ming PC, Yan TY, Tat LH. Risk factors of postoperative infections in adults with complicated appendicitis. Surg Laparosc Endosc Percutan Tech. 2009;19(3):244-248. doi: 10.1097/SLE.0b013e3181a4cda2 [DOI] [PubMed] [Google Scholar]
- 6.Konstantinidis KM, Anastasakou KA, Vorias MN, Sambalis GH, Georgiou MK, Xiarchos AG. A decade of laparoscopic appendectomy: presentation of 1026 patients with suspected appendicitis treated in a single surgical department. J Laparoendosc Adv Surg Tech A. 2008;18(2):248-258. doi: 10.1089/lap.2006.0209 [DOI] [PubMed] [Google Scholar]
- 7.Leung TT, Dixon E, Gill M, et al. Bowel obstruction following appendectomy: what is the true incidence? Ann Surg. 2009;250(1):51-53. doi: 10.1097/SLA.0b013e3181ad64a7 [DOI] [PubMed] [Google Scholar]
- 8.Parker MC, Ellis H, Moran BJ, et al. Postoperative adhesions: ten-year follow-up of 12 584 patients undergoing lower abdominal surgery. Dis Colon Rectum. 2001;44(6):822-829. doi: 10.1007/BF02234701 [DOI] [PubMed] [Google Scholar]
- 9.Kapischke M, Friedrich F, Hedderich J, Schulz T, Caliebe A. Laparoscopic versus open appendectomy—quality of life 7 years after surgery. Langenbecks Arch Surg. 2011;396(1):69-75. doi: 10.1007/s00423-010-0715-1 [DOI] [PubMed] [Google Scholar]
- 10.Scott JW, Olufajo OA, Brat GA, et al. Use of national burden to define operative emergency general surgery. JAMA Surg. 2016;151(6):e160480. doi: 10.1001/jamasurg.2016.0480 [DOI] [PubMed] [Google Scholar]
- 11.Eriksson S, Granström L. Randomized controlled trial of appendicectomy versus antibiotic therapy for acute appendicitis. Br J Surg. 1995;82(2):166-169. doi: 10.1002/bjs.1800820207 [DOI] [PubMed] [Google Scholar]
- 12.Styrud J, Eriksson S, Nilsson I, et al. Appendectomy versus antibiotic treatment in acute appendicitis: a prospective multicenter randomized controlled trial. World J Surg. 2006;30(6):1033-1037. doi: 10.1007/s00268-005-0304-6 [DOI] [PubMed] [Google Scholar]
- 13.Turhan AN, Kapan S, Kütükçü E, Yiğitbaş H, Hatipoğlu S, Aygün E. Comparison of operative and non operative management of acute appendicitis. Ulus Travma Acil Cerrahi Derg. 2009;15(5):459-462. [PubMed] [Google Scholar]
- 14.Salminen P, Paajanen H, Rautio T, et al. Antibiotic therapy vs appendectomy for treatment of uncomplicated acute appendicitis: the APPAC randomized clinical trial. JAMA. 2015;313(23):2340-2348. doi: 10.1001/jama.2015.6154 [DOI] [PubMed] [Google Scholar]
- 15.Di Saverio S, Sibilio A, Giorgini E, et al. The NOTA Study (Non Operative Treatment for Acute Appendicitis): prospective study on the efficacy and safety of antibiotics (amoxicillin and clavulanic acid) for treating patients with right lower quadrant abdominal pain and long-term follow-up of conservatively treated suspected appendicitis. Ann Surg. 2014;260(1):109-117. doi: 10.1097/SLA.0000000000000560 [DOI] [PubMed] [Google Scholar]
- 16.Vons C, Barry C, Maitre S, et al. Amoxicillin plus clavulanic acid versus appendicectomy for treatment of acute uncomplicated appendicitis: an open-label, non-inferiority, randomised controlled trial. Lancet. 2011;377(9777):1573-1579. doi: 10.1016/S0140-6736(11)60410-8 [DOI] [PubMed] [Google Scholar]
- 17.Hansson J, Körner U, Khorram-Manesh A, Solberg A, Lundholm K. Randomized clinical trial of antibiotic therapy versus appendicectomy as primary treatment of acute appendicitis in unselected patients. Br J Surg. 2009;96(5):473-481. doi: 10.1002/bjs.6482 [DOI] [PubMed] [Google Scholar]
- 18.Di Saverio S, Birindelli A, Kelly MD, et al. WSES Jerusalem guidelines for diagnosis and treatment of acute appendicitis. World J Emerg Surg. 2016;11:34. doi: 10.1186/s13017-016-0090-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tanaka Y, Uchida H, Kawashima H, et al. Long-term outcomes of operative versus nonoperative treatment for uncomplicated appendicitis. J Pediatr Surg. 2015;50(11):1893-1897. doi: 10.1016/j.jpedsurg.2015.07.008 [DOI] [PubMed] [Google Scholar]
- 20.McCutcheon BA, Chang DC, Marcus LP, et al. Long-term outcomes of patients with nonsurgically managed uncomplicated appendicitis. J Am Coll Surg. 2014;218(5):905-913. doi: 10.1016/j.jamcollsurg.2014.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tominaga GT, Staudenmayer KL, Shafi S, et al. ; American Association for the Surgery of Trauma Committee on Patient Assessment . The American Association for the Surgery of Trauma grading scale for 16 emergency general surgery conditions: disease-specific criteria characterizing anatomic severity grading. J Trauma Acute Care Surg. 2016;81(3):593-602. doi: 10.1097/TA.0000000000001127 [DOI] [PubMed] [Google Scholar]
- 22.Shafi S, Aboutanos M, Brown CV, et al. ; American Association for the Surgery of Trauma Committee on Patient Assessment and Outcomes . Measuring anatomic severity of disease in emergency general surgery. J Trauma Acute Care Surg. 2014;76(3):884-887. doi: 10.1097/TA.0b013e3182aafdba [DOI] [PubMed] [Google Scholar]
- 23.Hernandez MC, Aho JM, Habermann EB, Choudhry AJ, Morris DS, Zielinski MD. Increased anatomic severity predicts outcomes: validation of the American Association for the Surgery of Trauma’s Emergency General Surgery score in appendicitis. J Trauma Acute Care Surg. 2017;82(1):73-79. doi: 10.1097/TA.0000000000001274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Utter GH, Miller PR, Mowery NT, et al. ICD-9-CM and ICD-10-CM mapping of the AAST Emergency General Surgery disease severity grading systems: conceptual approach, limitations, and recommendations for the future. J Trauma Acute Care Surg. 2015;78(5):1059-1065. doi: 10.1097/TA.0000000000000608 [DOI] [PubMed] [Google Scholar]
- 25.Bureau of Labor Statistics Consumer price index—all urban consumers, 1956-2018 [time series]. https://data.bls.gov/pdq/SurveyOutputServlet. Accessed October 8, 2018.
- 26.Rothman KJ. No adjustments are needed for multiple comparisons. Epidemiology. 1990;1(1):43-46. doi: 10.1097/00001648-199001000-00010 [DOI] [PubMed] [Google Scholar]
- 27.Blackwell M, Iacus S, King G, Porro G. CEM: coarsened exact matching in Stata. Stata J. 2009;9(4):524-546. [Google Scholar]
- 28.Iacus S, King G, Porro G. Causal inference without balance checking: coarsened exact matching. Polit Anal. 2012;20(1):1-24. doi: 10.1093/pan/mpr013 [DOI] [Google Scholar]
- 29.King G, Nielsen R Why propensity scores should not be used for matching. https://gking.harvard.edu/files/gking/files/psnot.pdf. Updated December 16, 2016. Accessed October 8, 2018.
- 30.Cho J, Park I, Lee D, Sung K, Baek J, Lee J. Risk factors for postoperative intra-abdominal abscess after laparoscopic appendectomy: analysis for consecutive 1817 experiences. Dig Surg. 2015;32(5):375-381. doi: 10.1159/000438707 [DOI] [PubMed] [Google Scholar]
- 31.Katkhouda N, Friedlander MH, Grant SW, et al. Intraabdominal abscess rate after laparoscopic appendectomy. Am J Surg. 2000;180(6):456-459. [DOI] [PubMed] [Google Scholar]
- 32.Asarias JR, Schlussel AT, Cafasso DE, et al. Incidence of postoperative intraabdominal abscesses in open versus laparoscopic appendectomies. Surg Endosc. 2011;25(8):2678-2683. doi: 10.1007/s00464-011-1628-y [DOI] [PubMed] [Google Scholar]
- 33.Sippola S, Grönroos J, Tuominen R, et al. Economic evaluation of antibiotic therapy versus appendicectomy for the treatment of uncomplicated acute appendicitis from the APPAC randomized clinical trial. Br J Surg. 2017;104(10):1355-1361. doi: 10.1002/bjs.10575 [DOI] [PubMed] [Google Scholar]
- 34.Wu JX, Dawes AJ, Sacks GD, Brunicardi FC, Keeler EB. Cost effectiveness of nonoperative management versus laparoscopic appendectomy for acute uncomplicated appendicitis. Surgery. 2015;158(3):712-721. doi: 10.1016/j.surg.2015.06.021 [DOI] [PubMed] [Google Scholar]
- 35.Wu JX, Sacks GD, Dawes AJ, DeUgarte D, Lee SL. The cost-effectiveness of nonoperative management versus laparoscopic appendectomy for the treatment of acute, uncomplicated appendicitis in children. J Pediatr Surg. 2017;52(7):1135-1140. doi: 10.1016/j.jpedsurg.2016.10.009 [DOI] [PubMed] [Google Scholar]
- 36.Arellano M, Gonzalez-Dominguez Y, Molina-Ortiz F, Garceau MH, Cantero R, Rodriguez-Montes J. Primary adenocarcinoma of the appendix: experience at La Paz University Hospital of Madrid (1967-2014). Int J Surg Open. 2016;4:23-26. doi: 10.1016/j.ijso.2016.06.003 [DOI] [Google Scholar]
- 37.Blair NP, Bugis SP, Turner LJ, MacLeod MM. Review of the pathologic diagnoses of 2216 appendectomy specimens. Am J Surg. 1993;165(5):618-620. doi: 10.1016/S0002-9610(05)80446-5 [DOI] [PubMed] [Google Scholar]
- 38.Schwartz JA, Forleiter C, Lee D, Kim GJ. Occult appendiceal neoplasms in acute and chronic appendicitis: a single-institution experience of 1793 appendectomies. Am Surg. 2017;83(12):1381-1385. [PubMed] [Google Scholar]
- 39.Swank HA, Eshuis EJ, Ubbink DT, Bemelman WA. Is routine histopathological examination of appendectomy specimens useful? a systematic review of the literature. Colorectal Dis. 2011;13(11):1214-1221. doi: 10.1111/j.1463-1318.2010.02457.x [DOI] [PubMed] [Google Scholar]
- 40.Birkmeyer JD, Reames BN, McCulloch P, Carr AJ, Campbell WB, Wennberg JE. Understanding of regional variation in the use of surgery. Lancet. 2013;382(9898):1121-1129. doi: 10.1016/S0140-6736(13)61215-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Flum DR, Morris A, Koepsell T, Dellinger EP. Has misdiagnosis of appendicitis decreased over time? a population-based analysis. JAMA. 2001;286(14):1748-1753. doi: 10.1001/jama.286.14.1748 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. Definitions of Short- and Long-term Complications
eFigure. Regional Variation in Nonoperative Management of Appendicitis