Abstract
This study reports 2-year survival outcomes among patients with advanced nonprogressive stage IIA to IV lung cancer randomized to symptom monitoring during chemotherapy via web-based patient-reported outcomes vs standard scheduled imaging after treatment to detect symptomatic recurrence.
Symptom monitoring during chemotherapy via web-based patient-reported outcomes (PROs) was previously demonstrated to lengthen survival in a single-center study.1 A multicenter randomized clinical trial compared web-based monitoring vs standard scheduled imaging to detect symptomatic recurrence in patients with lung cancer following initial treatment. A planned interim analysis (9-month follow-up) found a significant survival benefit (19-month survival in the PRO group vs 12 months in the control group).2 We now present the final overall survival analysis.
Methods
As described previously,2 in this randomized trial, patients with advanced nonprogressive stage IIA (TXN1) to IV lung cancer were randomly assigned within 3 months of previous treatment to receive either web-based symptom monitoring via the Sentinel PRO system (Hyperion) or standard follow-up with scheduled imaging every 3 to 6 months (the trial protocol is available in Supplement 1). Eligible patients were recruited at 5 centers in France from June 2014 to January 2016. Nonprogressive patients treated for metastatic disease by tyrosine kinase inhibitors, maintenance antiangiogenic or chemotherapy, or immunotherapy were eligible. Allocation was generated centrally and concealed from investigators and participants. The study was reviewed and approved by the ethics review board from the University Hospital at Angers (France). All participants provided written informed consent.
In the PRO group, patients were invited to complete weekly self-reports of 13 common symptoms online between visits. The PRO system automatically triggered an alert email to the treating oncologist when patient-reported symptoms matched predefined criteria for severity and worsening. In both groups, additional imaging could be performed at the treating oncologist’s discretion.
The primary outcome was overall survival after 2 years of follow-up, which was selected based on prior pilot research.3 Survival data were gathered from patient follow-up by blinded investigators. After a preplanned interim analysis in January 2016 in which a significant survival improvement was observed, the data and safety monitoring committee mandated cessation of recruitment and crossover of control patients to the intervention. Sixty percent of the prespecified sample size was enrolled when recruitment was halted. The final date of follow-up was December 29, 2017.
Overall survival was estimated via the Kaplan-Meier method and compared between groups with a log-rank test (SAS version 9.3; SAS Institute). A 2-sided P<.05 was considered significant. Analyses were performed on an intention-to-treat basis and with censoring at crossover.4
Results
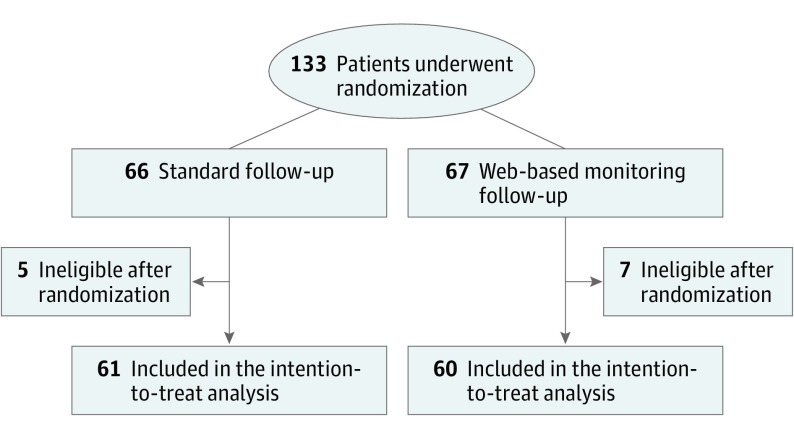
One hundred thirty-three patients were enrolled of whom 12 were ineligible, leaving a study population of 121 (60 in the intervention and 61 in the control group) (Figure 1). Baseline demographic and disease characteristics were well balanced between groups.2 The median age was 65 years (range, 36-88 years), 67% were men, 32% had stage III cancer, 63% had stage IV cancer, and 17% had small cell cancer. Following interim analysis, 10 of 34 living patients in the control group had not relapsed and therefore were eligible to cross over to the intervention. No participants were lost to follow-up.
Figure 1. Assignment, Follow-up, and Analysis of the Study Patients.
At 9 months when recruitment was halted, 10 patients in the intervention group and 27 patients in the control group had died. Of the 34 living patients in the control group, 10 had not relapsed and crossed over to the intervention.
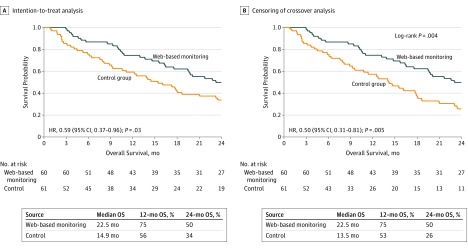
With 2 years of follow-up, 69 deaths were observed: 29 (47.5%) in the intervention group and 40 (66.7%) in the control group. The median overall survival was 22.5 months in the intervention group vs 14.9 months in the control group, without censoring for crossover (hazard ratio, 0.59 [95% CI, 0.37-0.96]; P = .03) (Figure 2A). Censoring crossover resulted in a median overall survival of 22.5 months in the intervention group vs 13.5 months in the control group (hazard ratio, 0.50 [95% CI, 0.31-0.81]; P = .005) (Figure 2B).
Figure 2. Kaplan-Meier Curves for the Overall Survival (OS) Analysis.
A total of 121 patients were included in the intention-to-treat survival analysis. Ten of 34 living patients in the control group were eligible to cross over following the interim analysis. HR indicates hazard ratio.
Discussion
Symptom monitoring via weekly web-based PROs following treatment for lung cancer was associated with increased survival compared with standard imaging surveillance. A potential mechanism of action is that symptoms suggesting adverse events or recurrence were detected earlier.
Limitations of this study include conduct only in France, early stopping of the trial and crossover of control patients, and inclusion of patients receiving maintenance therapy, who may have had increased interactions with care teams.
Section Editor: Jody W. Zylke, MD, Deputy Editor.
Trial Protocol
Data Sharing Statement
References
- 1.Basch E, Deal AM, Dueck AC, et al. Overall survival results of a trial assessing patient-reported outcomes for symptom monitoring during routine cancer treatment. JAMA. 2017;318(2):197-198. doi: 10.1001/jama.2017.7156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Denis F, Lethrosne C, Pourel N, et al. Randomized trial comparing a web-mediated follow-up with routine surveillance in lung cancer patients. J Natl Cancer Inst. 2017;109(9). doi: 10.1093/jnci/djx029 [DOI] [PubMed] [Google Scholar]
- 3.Denis F, Yossi S, Septans AL, et al. Improving survival in patient treated for a lung cancer using self-evaluated symptoms reported through a web application. Am J Clin Oncol. 2017;40(5):464-469. doi: 10.1097/COC.0000000000000189 [DOI] [PubMed] [Google Scholar]
- 4.Robins JM, Tsiatis AA. Correcting for non-compliance in randomized trials using rank preserving structural failure time models. Commun Stat Theory Methods. 1991;20:2609-2631. doi: 10.1080/03610929108830654 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol
Data Sharing Statement