Key Points
Question
How does functional status change in the year after transcatheter and surgical aortic valve replacement?
Findings
In this cohort study of 246 elderly patients (mean age, 78.1 years), the proportions of patients who had excellent, good, fair, poor, and very poor functional trajectories were 14.0%, 23.1%, 37.9%, 14.7%, and 8.4%, respectively, after transcatheter aortic valve replacement, and 36.9%, 37.9%, 19.4%, 2.9%, and 1.0%, respectively, after surgical aortic valve replacement. Preoperative frailty level as well as major complications and delirium were associated with functional decline or lack of improvement.
Meaning
Despite disease-specific benefits of aortic valve replacement, functional decline or lack of functional improvement is common in older patients with severe frailty; information on functional trajectories may be useful for patient-centered decision making and perioperative care to optimize functional outcomes.
Abstract
Importance
Functional status is a patient-centered outcome that is important for a meaningful gain in health-related quality of life after aortic valve replacement.
Objective
To determine functional status trajectories in the year after transcatheter aortic valve replacement (TAVR) and surgical aortic valve replacement (SAVR).
Design, Setting, and Participants
A prospective cohort study with a 12-month follow-up was conducted at a single academic center in 246 patients undergoing TAVR or SAVR for severe aortic stenosis. The study was conducted between February 1, 2014, and June 30, 2017; data analysis was performed from December 27, 2017, to May 7, 2018.
Exposures
Preoperative comprehensive geriatric assessment was performed and a deficit-accumulation frailty index (CGA-FI) (range, 0-1; higher values indicate greater frailty) was calculated.
Main Outcomes and Measures
Telephone interviews were conducted to assess self-reported ability to perform 22 activities and physical tasks at 1, 3, 6, 9, and 12 months after the procedure.
Results
Of the 246 patients included in the study, 143 underwent TAVR (74 [51.7%] women; mean [SD] age, 84.2 [5.9] years), and 103 underwent SAVR (46 [44.7%] women; age, 78.1 [5.3] years). Five trajectories were identified based on functional status at baseline and during the follow-up: from excellent at baseline to improvement at follow-up (excellent baseline-improvement), good (high baseline-full recovery), fair (moderate baseline-minimal decline), poor (low baseline-moderate decline), and very poor (low baseline-large decline). After TAVR, the most common trajectory was fair (54 [37.8%]), followed by good (33 [23.1%]), poor (21 [14.7%]), excellent (20 [14.0%]), and very poor (12 [8.4%]) trajectories. After SAVR, the most common trajectory was good (39 [37.9%]), followed by excellent (38 [36.9%]), fair (20 [19.4%]), poor (3 [2.9%]), and very poor (1 [1.0%]) trajectories. Preoperative frailty level was associated with lower probability of functional improvement and greater probability of functional decline. After TAVR, patients with CGA-FI level of 0.20 or lower had excellent (3 [50.0%]) or good (3 [50.0%]) trajectories, whereas most patients with CGA-FI level of 0.51 or higher had poor (10 [45.5%]) or very poor (5 [22.7%]) trajectories. After SAVR, most patients with CGA-FI level of 0.20 or lower had excellent (24 [58.5%]) or good (15 [36.6%]) trajectories compared with a fair trajectory (5 [71.4%]) in those with CGA-FI levels of 0.41 to 0.50. Postoperative delirium and major complications were associated with functional decline after TAVR (delirium present vs absent: 14 [50.0%] vs 11 [13.4%]; complications present vs absent: 14 [51.9%] vs 19 [16.4%]) or lack of improvement after SAVR (delirium present vs absent: 27 [69.2%] vs 31 [81.6%]; complications present vs absent: 10 [62.5%] vs 69 [79.3%]).
Conclusions and Relevance
The findings suggest that functional decline or lack of improvement is common in older adults with severe frailty undergoing TAVR or SAVR. Although this nonrandomized study does not allow comparison of the effectiveness between TAVR and SAVR, anticipated functional trajectories may inform patient-centered decision making and perioperative care to optimize functional outcomes.
This cohort study examines changes in functional status over time in patients who have undergone transcatheter aortic valve replacement or surgical aortic valve replacement.
Introduction
Aortic stenosis (AS) has a negative association with survival, functional status, and quality of life in older adults.1 With recent advances in surgical techniques, more patients are undergoing transcatheter aortic valve replacement (TAVR)2 or surgical aortic valve replacement (SAVR).3 Although procedural outcomes have improved over time,2,3 functional decline is common owing to high operative risk and frailty.4,5,6,7,8,9,10 Since functional status can be more meaningful than longevity in older adults,11 information on functional status after the procedure is needed for patient-centered decision making and perioperative care to improve functional recovery.
Several clinical trials and observational studies have demonstrated improvement in functional status after TAVR and SAVR.12 However, the evidence based on the population averages may be insufficient to individualize decision making and clinical care in older adults with substantial heterogeneity in health status. These studies assessed functional limitations due to heart failure using disease-specific measures (eg, New York Heart Association [NYHA] class heart failure, Kansas City Cardiomyopathy Questionnaire), rather than adopting generic measures (eg, activities of daily living) oriented toward capturing the overall effect of cardiac and noncardiac conditions.12 Furthermore, studies designed to examine a dichotomous definition of functional decline cannot elucidate transitions in functional status. Examining functional trajectories using a generic measure of functional status may offer useful insights that are not captured by disease-specific measures, yet are relevant for patient selection, preventive care, and rehabilitation.
The objective of our study was to characterize functional status change using data from 5 repeated assessments over 12 months after TAVR and SAVR. We aimed to provide information on clinically meaningful trajectories of functional status according to preoperative frailty level and postoperative complications that can be useful for shared decision making and clinical care.
Methods
Study Design and Participants
The Frailty Assessment Before Cardiac Surgery and Transcatheter Interventions study was a prospective cohort study of 1020 older patients undergoing aortic valve replacement at 14 centers in Canada, the United States, and France.9,13 The researchers at the Beth Israel Deaconess Medical Center, Boston, Massachusetts, designed the Functional Outcomes Study, a single-center substudy, to collect more detailed data to determine the longitudinal change in functional status via interviews at 1, 3, 6, 9, and 12 months after the procedure. This study was approved by the institutional review board at Beth Israel Deaconess Medical Center, and written informed consent was obtained from the patients. The participants received financial compensation.
Eligible patients were adults 70 years or older undergoing TAVR or SAVR for severe AS. Excluded were those who required emergent surgery or surgery involving another valve or aorta, were clinically unstable (eg, hemodynamic instability, decompensated heart failure, or active myocardial ischemia), had a severe neuropsychiatric impairment, or were unable to communicate with the research team owing to language barrier. Because the treatment decision was made by our institution’s heart team without randomization, the study should be considered as 2 independent cohort studies of TAVR and SAVR; outcomes cannot be compared between the 2 procedures.
Preoperative Comprehensive Geriatric Assessment
A research nurse or a trained research assistant (including E.L.) interviewed the patient and reviewed medical records to collect demographic characteristics; cardiac, noncardiac, and geriatric conditions; NYHA class heart failure; and echocardiographic data (aortic valve area, ejection fraction). The Society of Thoracic Surgeons–Predicted Risk of Mortality (STS-PROM) was calculated.14 Depressive symptoms were defined as 2 or more points on the 5-item Geriatric Depression Scale.15 Self-reported functional status, as described below; Mini-Mental State Examination (MMSE) (0-30 points), usual gait speed (meters per second) from a 5-meter walk, and time to complete 5 chair stands (0-60 seconds; 60 seconds was assigned to those who could not complete the task) were measured. Based on these assessments, we calculated a comprehensive geriatric assessment–based frailty index (CGA-FI) (range, 0-1; higher values indicate greater frailty) (eFigure 1 in the Supplement); an online calculator is available.16 According to the standard deficit-accumulation approach,5 a CGA-FI was defined as the proportion of abnormalities present. For example, a patient with 12 deficits out of 48 items assessed has a CGA-FI of 0.25. Although the theoretical maximum CGA-FI is 1.0, several population-based studies demonstrated that few individuals could survive with more than 60% to 70% of the deficits.17 The administration time was approximately 30 to 45 minutes.
Postoperative Complications
Study physicians reviewed medical records to determine the incidence of stroke or transient ischemic attack, myocardial infarction, conduction disturbances, acute kidney injury, bleeding, and vascular access complications according to the Valve Academic Research Consortium–2 end point definitions.18 Data on wound complications, prolonged ventilation, and reoperation were collected. A composite variable of major complications was defined as any occurrence of the STS-PROM major morbidity or mortality (operative mortality, stroke, acute kidney injury, prolonged ventilation, deep sternal wound infection, or reoperation)14 or the Valve Academic Research Consortium–2 early safety end point (mortality, stroke, life-threatening bleeding, acute kidney injury, coronary artery obstruction requiring intervention, major vascular complication, or valve-related dysfunction requiring another procedure).18
Delirium was assessed daily by trained research assistants (including E.L.) using the Confusion Assessment Method algorithm19 after administering the MMSE. Because the delirium assessment was added to the study protocol 8 months after the cohort began,20 delirium data were available in 110 patients with TAVR and 77 patients with SAVR. Although patients for whom delirium data were collected had a lower STS-PROM level than 59 patients who were enrolled prior to delirium assessment (median, 3.5% vs 5.3%), the groups had otherwise similar characteristics, including AS severity (median aortic valve area, 0.7 vs 0.7 cm2) and functional status. Data on hospitalization and skilled nursing facility stay were obtained from medical records and self-report from patients and their proxies at the time of follow-up interview.
Assessment of Functional Status
At 1, 3, 6, 9, and 12 months after the procedure, trained research assistants (E.L.) conducted telephone interviews with patients or their proxy to assess ability to perform 22 daily activities and physical tasks. These activities included 7 activities of daily living, 7 instrumental activities of daily living, and 8 physical tasks (eg, ambulating, transferring, bathing, toileting, feeding, dressing, grooming, doing housework, making telephone calls, using transportation, shopping, cooking, taking medications, managing money, pulling or pushing a large object, lifting 4.5 kg, walking up and down a flight of stairs, walking half a mile, doing heavy work around house, reaching arms above shoulder, writing/handling small objects, stooping/crouching/kneeling) (eFigure 1 in the Supplement).21,22 A composite score (0-22 points) indicates the number of activities that one can perform without help. To explore which types of functional impairment before the procedure were associated with postoperative functional status trajectories, we classified these activities into 9 cognitively demanding tasks (feeding, dressing, grooming, making telephone calls, using transportation, shopping, cooking, taking medications, and managing money) and 13 remaining physically demanding tasks according to the relative cognitive and physical demands to perform each task.23
Statistical Analysis
We imputed missing data on preoperative variables (gait speed had the largest missingness [n = 35]) and functional status scores (for patients who did not respond to follow-up interviews) using a multivariate imputation by chained equations24 based on available information on preoperative characteristics, procedure type, complications, functional status, and mortality.
Group-based trajectory modeling25 was used to identify clusters of patients who followed similar functional status trajectories over 12 months after TAVR or SAVR. The functional status composite scores during follow-up were modeled using censored normal distribution (the score has a restricted range from 0 to 22) after excluding 5 patients who died before the 1-month follow-up. We considered models with 3 to 6 trajectories. We modeled each trajectory with intercept only or linear, quadratic, or cubic terms of time since the procedure to achieve the best fit based on the Bayesian information criterion.26 The number of trajectories was selected after considering the Bayesian information criterion and clinical interpretation. Patients were assigned to a trajectory with the maximum probability. We assessed the proportions of patients with excellent fit (probability >0.9) and poor fit (probability <0.7). A sensitivity analysis that used only observed data before imputation did not affect the final number of trajectories.
According to the final trajectory model, we summarized the distribution of trajectories in patients who underwent TAVR and SAVR. Preoperative characteristics were compared among patients with different trajectories using the Kruskal-Wallis test for continuous variables and Fisher exact test for categorical variables. We also summarized preoperative characteristics of patients with varying CGA-FI levels (≤0.20, 0.21-0.30, 0.31-0.40, 0.41-0.50, ≥0.51). To evaluate the role of preoperative frailty assessment, we examined the proportion of different trajectories in each CGA-FI category. To evaluate the role of postoperative complications, we compared the frequency of complications across trajectories using the Fisher exact test. Owing to low numbers of individual complications, we assessed how trajectories varied by the occurrence of any major complication and delirium.
Analyses were performed from December 27, 2017, to May 7, 2018, with Stata, Release 14 (StataCorp). A 2-sided P value <.05 was considered statistically significant.
Results
Between February 1, 2014, and March 31, 2016, we screened 446 consecutive patients, found 350 patients eligible, and enrolled 143 individuals who underwent TAVR and 103 who underwent SAVR (eFigure 2 in the Supplement). Patients undergoing TAVR were older than those who received SAVR (mean [SD] age, 84.2 [5.9] vs 78.1 [5.3] years) and more likely to be women (74 [51.7%] vs 46 [44.7%]). The final follow-up was completed on June 30, 2017. Response rates for follow-up interviews among surviving patients were 89.2% to 97.9% in the TAVR group and 82.0% to 88.1% in the SAVR group over the 12-month period (eFigure 2 in the Supplement).
Functional Status Trajectories After Aortic Valve Replacement
Five trajectories were identified based on functional status at baseline and during the follow-up: from excellent at baseline to improvement at follow-up (excellent baseline to improvement, 58 [24.1%]), good (high baseline to full recovery, 72 [29.9%]), fair (moderate baseline to minimal decline, 74 [30.7%]), poor (low baseline to moderate decline, 24 [9.9%]), and very poor (low baseline to large decline, 13 [5.4%]) (Figure 1). The median probability of trajectory assignment was 0.94 (interquartile range [IQR], 0.78-0.98), with 58.1% of patients with excellent fit and 15.4% with poor fit. The 12-month mortality rate was high in the group with very poor trajectory (9 of 13 [69.2%]) compared with poor (6 of 24 [25.0%]), fair (7 of 71 [9.9%]), good (2 of 70 [2.9%]), or excellent (2 of 57 [3.5%]) trajectories.
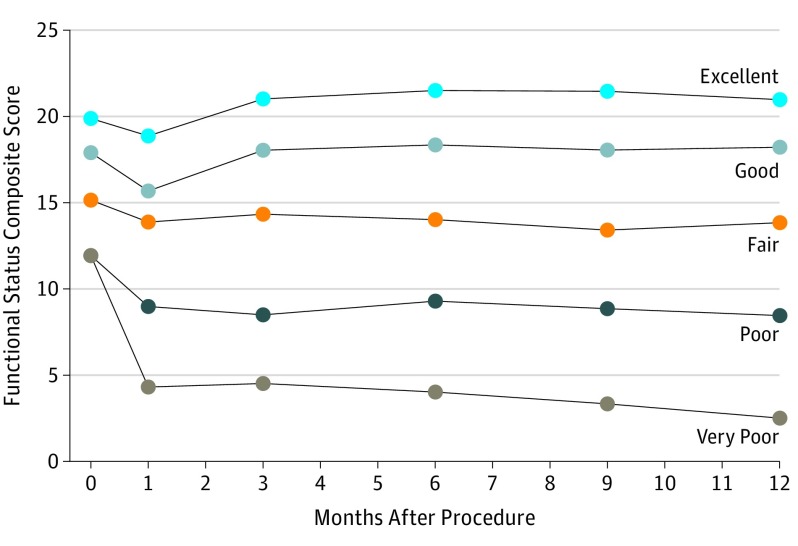
Figure 1. Functional Status Trajectories in the Year After Aortic Valve Replacement.
The functional status composite score represents the number of daily activities and physical tasks that a patient could perform without assistance (range, 0-22). Functional status trajectories were identified using a group-based trajectory model based on functional status at baseline and during the follow-up: excellent (excellent baseline to improvement) (n = 58; mortality, 3.5%), good (high baseline to full recovery) (n = 72; mortality, 2.9%), fair (moderate baseline to minimal decline) (n = 74; mortality, 9.9%), poor (low baseline to moderate decline) (n = 24; mortality, 25.0%), and very poor (low baseline to large decline) (n = 13; mortality, 69.2%).
Patients who followed more favorable trajectories had higher preoperative function than did those with less favorable trajectories (mean [SD] functional status composite score: excellent, 18.9 [2.5]; good, 16.9 [2.9]; fair, 14.2 [2.8]; poor, 10.9 [4.4]; and very poor, 10.9 [4.8] trajectories). Function in those with excellent or good trajectories declined at 1 month but returned to the preoperative level by 3 months with minimal change afterward. Patients with poor or very poor trajectories had a moderate or steep deterioration in function at 1 month and remained impaired. Except for patients with very poor trajectory, disease-specific improvement was achieved in most patients (NYHA class 3 or 4 heart failure at 12 months: excellent, 4.0%; good, 24.1%; fair, 39.0%; poor, 55.6%; and very poor, 100% trajectories).
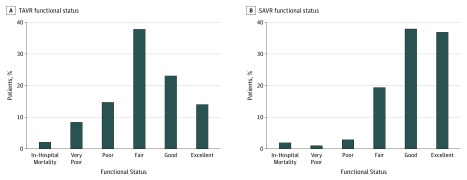
By procedure (Figure 2), the most common trajectory after TAVR was fair (54 [37.8%]), followed by good (33 [23.1%]), poor (21 [14.7%]), excellent (20 [14.0%]), and very poor (12 [8.4%]) trajectories. After SAVR, the most common trajectory was good (39 [37.9%]), followed by excellent (38 [36.9%]), fair (20 [19.4%]), poor (3 [2.9%]), and very poor (1 [1.0%]) trajectories.
Figure 2. Functional Status Trajectories by Procedure.
Functional status trajectories of patients after transcatheter aortic valve replacement (TAVR) in 143 patients (A) and surgical aortic valve replacement (SAVR) in 103 patients (B). In the absence of randomization, these results cannot be used to compare the effectiveness of TAVR vs SAVR on functional status.
Preoperative Characteristics, Frailty, and Functional Status Trajectories
There were statistically significant differences in preoperative characteristics among patients with different trajectories (Table 1). Compared with those who had excellent or good trajectories, patients with poor or very poor trajectories were older and more likely to have NYHA class 3 or 4 heart failure (eg, excellent, 27 [46.6%] vs very poor, 13 [100%]), higher STS-PROM level (eg, excellent, 2.4% [IQR, 1.7%-3.9%] vs very poor, 6.3% [4.4%-7.0%]), atrial fibrillation (eg, excellent, 19 [32.8%] vs very poor, 7 [53.9%]), depressive symptoms (eg, excellent, 11 [19.0%] vs very poor, 6 [46.2%]), lower MMSE scores (eg, excellent, 28 points [IQR, 27-29 points] vs very poor, 23 points [IQR, 20-24 points]), slower gait speed (eg, excellent, 1.0 m/s [IQR, 0.8-1.2 m/s] vs 0.3 m/s [IQR,0.3-0.4 m/s]), more difficulty completing 5 chair stands (eg, excellent, 14.1 seconds [IQR, 10.9-17.2 seconds] vs very poor, 60.0 seconds [IQR, 60.0-60.0 seconds]), greater activities of daily living (eg, excellent, 1 [1.7%] vs very poor, 6 (46.2%]) and instrumental activities of daily living (eg, excellent, 20 [34.5%] vs very poor, 12 [92.3%]) disabilities. Dependence in physical tasks was present in 77.6% to 100% of patients at baseline, regardless of their functional trajectories, whereas dependence in cognitive tasks varied widely in prevalence, from 15.5% to 95.8% across the trajectories.
Table 1. Preoperative Characteristics and Functional Status Trajectory After Transcatheter and Surgical Aortic Valve Replacementa.
| Characteristic | Excellent (n = 58) | Good (n = 72) | Fair (n = 74) | Poor (n = 24) | Very Poor (n = 13) | P Value |
|---|---|---|---|---|---|---|
| Age, median (IQR), y | 77 (73-85) | 81 (76-85) | 84 (80-87) | 85 (84-89) | 85 (82-87) | <.001 |
| Women, No. (%) | 19 (32.8) | 40 (55.6) | 42 (56.8) | 12 (50.0) | 5 (38.5) | .04 |
| White race, No. (%) | 57 (98.3) | 70 (97.2) | 70 (94.6) | 24 (100) | 13 (100) | .76 |
| Aortic valve area, median (IQR), cm2 | 0.7 (0.6-0.9) | 0.8 (0.6-0.9) | 0.7 (0.6-0.8) | 0.8 (0.6-0.8) | 0.8 (0.7-0.8) | .85 |
| Ejection fraction, median (IQR), % | 60 (55-65) | 60 (55-65) | 55 (45-60) | 55 (48-60) | 60 (45-60) | .49 |
| NYHA class 3 or 4, No. (%) | 27 (46.6) | 56 (77.8) | 68 (91.9) | 21 (87.5) | 13 (100) | <.001 |
| STS-PROM, median (IQR), % | 2.4 (1.7-3.9) | 3.4 (2.6-5.8) | 5.0 (3.1-6.0) | 6.2 (4.4-8.7) | 6.3 (4.4-7.0) | <.001 |
| Atrial fibrillation, No. (%) | 19 (32.8) | 18 (25.0) | 32 (43.2) | 15 (62.5) | 7 (53.9) | .006 |
| Chronic kidney disease, No. (%) | 23 (39.7) | 34 (47.2) | 32 (43.2) | 11 (45.8) | 7 (53.9) | .86 |
| COPD, No. (%) | 10 (17.2) | 22 (30.6) | 28 (37.8) | 9 (37.5) | 4 (30.8) | .10 |
| Depressive symptoms, No. (%) | 11 (19.0) | 14 (19.4) | 28 (37.8) | 9 (37.5) | 6 (46.2) | .02 |
| MMSE score median (IQR) | 28 (27-29) | 27 (24-28) | 26 (23-27) | 25 (23-27) | 23 (20-24) | <.001 |
| Gait speed, median (IQR), m/s | 1.0 (0.8-1.2) | 0.8 (0.6-0.9) | 0.5 (0.4-0.6) | 0.4 (0.3-0.6) | 0.3 (0.3-0.4) | <.001 |
| Chair stands, median (IQR), sb | 14.1 (10.9-17.2) | 17.2 (13.4-26.2) | 31.0 (16.9-60.0) | 60.0 (39.9-60.0) | 60.0 (60.0-60.0) | <.001 |
| Grip strength, median (IQR), kg | 27.7 (16.7-34.3) | 18.7 (14.3-26.5) | 15.8 (11.3-22.2) | 12.2 (10.3-17.3) | 11.3 (10.0-17.3) | <.001 |
| ADL dependence, No. (%) | 1 (1.7) | 3 (4.2) | 6 (8.1) | 12 (50.0) | 6 (46.2) | <.001 |
| IADL dependence, No. (%) | 20 (34.5) | 40 (55.6) | 64 (86.5) | 23 (95.8) | 12 (92.3) | <.001 |
| Dependence in physical tasks, No. (%)c | 45 (77.6) | 69 (95.8) | 73 (98.7) | 24 (100) | 13 (100) | <.001 |
| Dependence in cognitive tasks, No. (%)c | 9 (15.5) | 26 (36.1) | 55 (74.3) | 23 (95.8) | 11 (84.6) | <.001 |
Abbreviations: ADL, activities of daily living; COPD, chronic obstructive pulmonary disease; IADL, instrumental ADL; IQR, interquartile range; MMSE, Mini-Mental State Examination; NYHA, New York Heart Association; STS-PROM, Society of Thoracic Surgeons–Predicted Risk of Mortality.
The functional status trajectory could not be determined in 5 patients who died before the 1-month follow-up interview.
Time to complete 5 chair stands was assigned as 60 seconds if the patient was unable to complete them.
Physical tasks include lifting 4.5 kg, pulling/pushing large objects, walking up and down a flight of stairs, walking half a mile, doing heavy work around house, ambulating, transferring, bathing, toileting, doing housework, reaching arms above shoulder, writing/handling small objects, stooping/crouching/kneeling; cognitive tasks include feeding, dressing, grooming, making telephone calls, using transportation, shopping, cooking, taking medications, managing money.
The CGA-FI, which summarizes the total burden of health deficits, was associated with older age (eg, CGA-FI ≥0.51: 84 years [IQR, 82-88 years] vs CGA-FI ≤0.20: 76 years [IQR, 73-81 years]), comorbidities (eg, atrial fibrillation: CGA-FI ≥0.51, 11 [50%] vs CGA-FI ≤0.20, 5 [10.6%]; chronic kidney disease: CGA-FI ≥0.51, 12 [54.6%] vs CGA-FI ≤0.20, 15 [31.9%]), lower cognitive function (eg, MMSE score: CGA-FI ≥0.51, 23 points [IQR, 21-25 points] vs CGA-FI ≤0.20, 28 points [IQR, 26-30 points]), physical function (eg, gait speed: CGA-FI ≥0.51, 0.4 m/s [IQR, 0.3-0.5 m/s] vs CGA-FI ≤0.20, 1.0 m/s [IQR, 0.9-1.2 m/s]), and disabilities (eg, activities of daily living disability: CGA-FI ≥0.51, 17 [77.3%] vs CGA-FI ≤0.20, 1 [2.1%]; instrumental activities of daily living disability: CGA ≥0.51, 22 [100%] vs CGA-FI ≤0.20, 11 [23.4%]) (eTable 1 in the Supplement). Patients with higher CGA-FI levels were more likely to undergo TAVR (6 [12.8%] in CGA-FI ≤0.20 and 22 [100%] in CGA-FI ≥0.51).
To evaluate the role of CGA-FI in predicting functional trajectories, we examined the proportion of different trajectories across the CGA-FI range (Table 2). Increasing CGA-FI levels were associated with lower risk of functional improvement and greater risk of functional decline. After TAVR, patients with CGA-FI levels of 0.20 or lower had excellent (3 [50.0%]) or good (3 [50.0%]) trajectories, whereas most patients with a CGA-FI level of 0.51 or higher had poor (10 [45.5%]) or very poor (5 [22.7%]) trajectories. After SAVR, most patients with a CGA-FI level of 0.20 or lower had excellent (24 patients [58.5%]) or good (15 [36.6%]) trajectories compared with fair trajectory (5 [71.4%]) in those with CGA-FI levels of 0.41 to 0.50.
Table 2. Preoperative Frailty Index and Functional Status Trajectory After Aortic Valve Replacementa.
| CGA-FI | No. (%) | Total (N = 241) | ||||
|---|---|---|---|---|---|---|
| Excellent (n = 58) | Good (n = 72) | Fair (n = 74) | Poor (n = 24) | Very Poor (n = 13) | ||
| TAVR | ||||||
| ≤0.20 | 3 (50.0) | 3 (50.0) | 0 | 0 | 0 | 6 |
| 0.21-0.30 | 12 (35.3) | 11 (32.4) | 10 (29.4) | 1 (2.9) | 0 | 34 |
| 0.31-0.40 | 3 (6.8) | 13 (29.6) | 22 (50.0) | 2 (4.6) | 4 (9.1) | 44 |
| 0.41-0.50 | 2 (5.9) | 6 (17.7) | 15 (44.1) | 8 (23.5) | 3 (8.8) | 34 |
| ≥0.51 | 0 | 0 | 7 (31.8) | 10 (45.5) | 5 (22.7) | 22 |
| SAVR | ||||||
| ≤0.20 | 24 (58.5) | 15 (36.6) | 1 (2.4) | 1 (2.4) | 0 | 41 |
| 0.21-0.30 | 14 (43.8) | 13 (40.6) | 4 (12.5) | 1 (3.1) | 0 | 32 |
| 0.31-0.40 | 0 | 10 (47.6) | 10 (47.6) | 1 (4.8) | 0 | 21 |
| 0.41-0.50 | 0 | 1 (14.3) | 5 (71.4) | 0 | 1 (14.3) | 7 |
| ≥0.51 | 0 | 0 | 0 | 0 | 0 | 0 |
Abbreviations: CGA-FI, comprehensive geriatric assessment–based frailty index; SAVR, surgical aortic valve replacement; TAVR, transcatheter aortic valve replacement.
Five patients whose functional status trajectory could not be determined due to in-hospital mortality were excluded. In the absence of randomization, these results cannot be used to compare the effectiveness of TAVR vs SAVR on functional status.
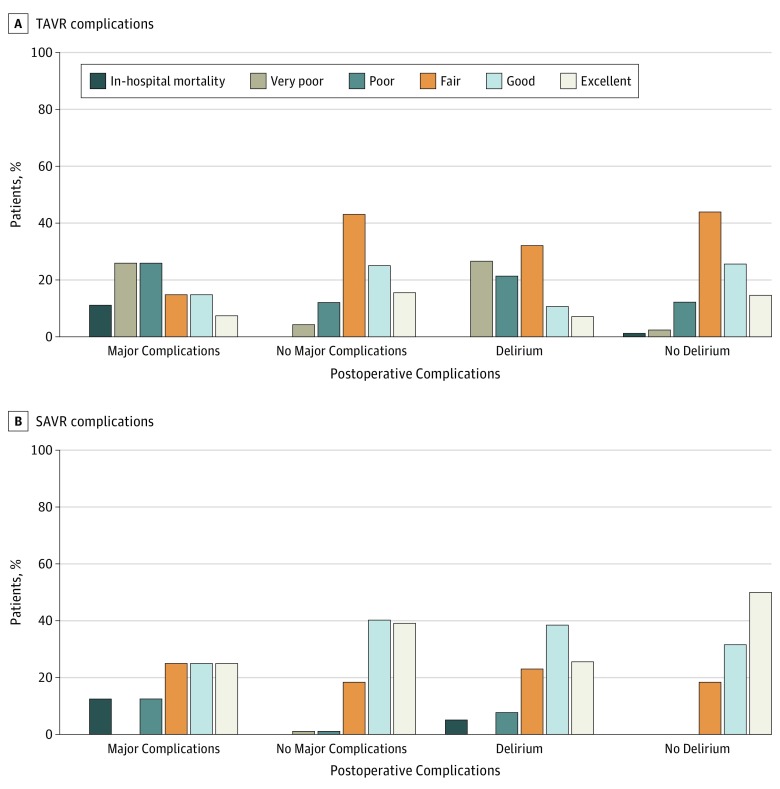
Postoperative Complications and Functional Status Trajectories
Major complications occurred in 24 patients (17.1%) who underwent TAVR and 14 patients (13.9%) who underwent SAVR. The frequency of individual complications and health care use is presented in eTable 2 in the Supplement. Delirium was the most common complication, affecting 28 of 108 (25.9%) patients in the TAVR group and 37 of 75 patients (49.3%) in the SAVR group for whom delirium data were collected. When functional status trajectories were examined according to the occurrence of major complications or delirium (Figure 3), patients in the TAVR group who developed major complications (n = 27) or delirium (n = 28) were more likely to have trajectories of functional decline than their counterparts (major complications present vs absent: 14 [51.9%] vs 19 [16.4%]; delirium present vs absent: 14 [50.0%] vs 11 [13.4%]). Similarly, patients who underwent SAVR and had major complications (n = 16) or delirium (n = 39) were less likely to improve (major complications present vs absent: 10 [62.5%] vs 69 [79.3%] improved; delirium present vs absent: 27 [69.2%] vs 31 [81.6%] improved).
Figure 3. Functional Status Trajectories by Postoperative Complications.
A, Postoperative complications with transcatheter aortic valve replacement (TAVR) in patients with (n = 27) and without (n = 116) major complications and with (n = 28) and without (n = 82) delirium. B, Postoperative complications with surgical aortic valve replacement (SAVR) in patients with (n = 16) and without (n = 87) major complications and with (n = 39) and without (n = 38) delirium. In the absence of randomization, these results cannot be used to compare the effectiveness of TAVR vs SAVR on functional status. A composite end point of major complications was defined as any occurrence of the Society of Thoracic Surgeons major morbidity or mortality (operative mortality, stroke, acute kidney injury, prolonged ventilation, deep sternal wound infection, or reoperation) or the Valve Academic Research Consortium-2 early safety end point (mortality, stroke, life-threatening bleeding, acute kidney injury, coronary artery obstruction requiring intervention, major vascular complication, or valve-related dysfunction requiring repeat procedure). Because delirium assessment was added to the study protocol 8 months after the cohort began, delirium data were available in 110 TAVR and 77 SAVR patients.
Discussion
Functional status is increasingly emphasized as a patient-centered outcome to evaluate the benefit of a medical intervention in older patients, yet little information is available on functional trajectory after AVR. Our study identified 5 clinically meaningful functional trajectories in the year after TAVR and SAVR. Patients who followed more favorable trajectories had higher function before the procedure and recovered their preoperative function within 3 months, whereas those who had poor or very poor trajectories had lower preoperative function and remained persistently impaired. Functional trajectories varied by procedure type, preoperative frailty, and postoperative complications. Given the lack of randomization, these results cannot be used to guide the procedure choice; however, our study suggests a wide range of functional trajectories that patients with different levels of frailty might experience after each procedure.
Previous research measured functional status using a disease-specific measure at limited time points (eTable 3 in the Supplement). In many studies, disease-specific measures improved within a month after transfemoral TAVR.10,27,28,29,30,31,32 The improvement was more gradual yet similar after transapical TAVR28,33 and SAVR.28,29,31,32,33 The change in generic measures of quality of life and functional status was not as impressive,8,27,28,29,30,31,32,33,34 because these measures are less responsive to change in disease severity targeted by the intervention.35,36 It is possible that generic measures are influenced by noncardiac or geriatric conditions, which are important for maintaining independence and quality of life but may not improve with the intervention. Previous studies estimated that 30% to 40% of patients experience poor quality of life or death within 1 year of TAVR.4,5,6,7,8,9,10 Preoperative functional limitations and cognitive impairment were identified as predictors. However, registries had high dropout rates.8,10,34 Moreover, the studies were not designed to explore heterogeneity and time course of functional status change.
Our study contributes to the literature by showing how function changes over time, rather than a dichotomous end point of functional decline. After TAVR, functional ability in about a quarter of the patients declined, while a third improved and the remainder maintained their preoperative level of function. In patients undergoing SAVR, who were relatively healthier and had higher baseline function, functional status improved in three-quarters, remained stable in approximately one-fifth, and declined in very few. Except for those with very poor trajectory, disease-specific benefit (NYHA class 1 or 2 heart failure) was achieved in almost half of the patients with poor trajectory and most of those with fair, good, and excellent trajectories.
Clinicians can calculate CGA-FI level using our online calculator or approximate it based on clinical characteristics (eTable 1 in the Supplement). Based on CGA-FI result, most likely, best-case, and worst-case scenarios of functional status can be communicated to the patient.37,38 For example, a patient with a CGA-FI level of 0.55 is most likely to have a poor trajectory after TAVR (45.5%). There is a nonnegligible chance (22.7%) of a very poor trajectory for which nursing home–level care is needed; functional improvement is unlikely (0%). If the patient’s goal is to achieve disease-specific symptom reduction, there is a 44.4% chance to reach this goal, which may be reasonable to some patients. If the goal is to recover independence, the chance is slim. Although functional limitations primarily caused by severe AS (as opposed to noncardiac comorbidities and frailty) may resolve after TAVR, such distinction is not always straightforward in older adults with multiple comorbidities. Our data suggest that patients with dependence in physical tasks, but not in cognitive tasks, were more likely to have favorable trajectories. These exploratory findings should be confirmed in future research.
For frail patients, interventions can be considered to optimize health status before the procedure. Clinical trials (NCT02219815, NCT02597985, NCT03107897) are under way to evaluate the benefit of prehabilitation in older adults undergoing cardiac surgery. Because major complications and delirium are associated with an unfavorable functional trajectory, efforts to reduce procedure-related complications and delirium through better surgical techniques or devices,39 safer anesthesia methods,40 and prevention of delirium41 may improve functional outcomes. After the procedure, cardiac rehabilitation should be recommended. Despite its functional and quality-of-life benefits,42,43 cardiac rehabilitation is underused in older adults.44 Given that high-risk patients undergoing TAVR have severe frailty, mobility impairment, and cognitive impairment, traditional outpatient center–based rehabilitation may not be feasible. Alternative modalities to increase participation and adherence are needed.
Limitations
There are a few limitations to our study. First, our study was conducted at a large academic center with high procedural volume and expertise. Most patients were white and underwent TAVR with previous-generation transcatheter heart valves. Caution is advised in applying our results to contemporary populations and less-experienced centers that may provide treatment for patients with a different frailty distribution. For widespread clinical applications, our results should be regularly updated using the latest data from a more representative population. Second, as a nonrandomized study, our study precludes comparison of effectiveness between TAVR and SAVR. Third, functional status was self-reported. Nonetheless, we believe that telephone interview was the most feasible modality to achieve high response rates during follow-up in this multimorbid population. Self-reported functional status has been validated against objective measures.45 Fourth, our functional status trajectories represent the experience of surviving patients. Although we imputed functional status scores for a small number of surviving patients without functional status data, the trajectory results did not change in sensitivity analysis using the observed data before imputation.
Conclusions
These limitations notwithstanding, our study offers insight into the role of frailty assessment in predicting heterogeneous functional trajectories. Despite disease-specific benefits of TAVR and SAVR, functional decline or lack of improvement is common in older adults, particularly in those with severe frailty. Anticipated functional trajectories after the procedure should inform patient-centered shared decision making about these procedures and perioperative care to optimize functional outcomes.
eTable 1. Preoperative Characteristics of Patients by the Comprehensive Geriatric Assessment-Based Frailty Index Level
eTable 2. Postoperative Complications, Health Care Utilization, and Functional Status Trajectory After Transcatheter and Surgical Aortic Valve Replacement
eTable 3. Evidence Summary on the Quality of Life and Physical Function from Major Clinical Trials and Registries
eFigure 1. Comprehensive Geriatric Assessment-Based Frailty Index (CGA-FI)
eFigure 2. Patient Enrollment and Follow-Up
References
- 1.Carabello BA, Paulus WJ. Aortic stenosis. Lancet. 2009;373(9667):956-966. doi: 10.1016/S0140-6736(09)60211-7 [DOI] [PubMed] [Google Scholar]
- 2.Grover FL, Vemulapalli S, Carroll JD, et al. ; STS/ACC TVT Registry . 2016 Annual report of the Society of Thoracic Surgeons/American College of Cardiology Transcatheter Valve Therapy Registry. J Am Coll Cardiol. 2017;69(10):1215-1230. doi: 10.1016/j.jacc.2016.11.033 [DOI] [PubMed] [Google Scholar]
- 3.Barreto-Filho JA, Wang Y, Dodson JA, et al. Trends in aortic valve replacement for elderly patients in the United States, 1999-2011. JAMA. 2013;310(19):2078-2085. doi: 10.1001/jama.2013.282437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schoenenberger AW, Stortecky S, Neumann S, et al. Predictors of functional decline in elderly patients undergoing transcatheter aortic valve implantation (TAVI). Eur Heart J. 2013;34(9):684-692. doi: 10.1093/eurheartj/ehs304 [DOI] [PubMed] [Google Scholar]
- 5.Arnold SV, Reynolds MR, Lei Y, et al. ; PARTNER Investigators . Predictors of poor outcomes after transcatheter aortic valve replacement: results from the PARTNER (Placement of Aortic Transcatheter Valve) trial. Circulation. 2014;129(25):2682-2690. doi: 10.1161/CIRCULATIONAHA.113.007477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arnold SV, Afilalo J, Spertus JA, et al. ; US CoreValve Investigators . Prediction of poor outcome after transcatheter aortic valve replacement. J Am Coll Cardiol. 2016;68(17):1868-1877. doi: 10.1016/j.jacc.2016.07.762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim DH, Kim CA, Placide S, Lipsitz LA, Marcantonio ER. Preoperative frailty assessment and outcomes at 6 months or later in older adults undergoing cardiac surgical procedures: a systematic review. Ann Intern Med. 2016;165(9):650-660. doi: 10.7326/M16-0652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lange R, Beckmann A, Neumann T, et al. ; GARY Executive Board . Quality of life after transcatheter aortic valve replacement: prospective data from GARY (German Aortic Valve Registry). JACC Cardiovasc Interv. 2016;9(24):2541-2554. doi: 10.1016/j.jcin.2016.09.050 [DOI] [PubMed] [Google Scholar]
- 9.Afilalo J, Lauck S, Kim DH, et al. Frailty in older adults undergoing aortic valve replacement: the FRAILTY-AVR Study. J Am Coll Cardiol. 2017;70(6):689-700. doi: 10.1016/j.jacc.2017.06.024 [DOI] [PubMed] [Google Scholar]
- 10.Arnold SV, Spertus JA, Vemulapalli S, et al. Quality-of-life outcomes after transcatheter aortic valve replacement in an unselected population: a report from the STS/ACC Transcatheter Valve Therapy Registry. JAMA Cardiol. 2017;2(4):409-416. doi: 10.1001/jamacardio.2016.5302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lewis EF, Johnson PA, Johnson W, Collins C, Griffin L, Stevenson LW. Preferences for quality of life or survival expressed by patients with heart failure. J Heart Lung Transplant. 2001;20(9):1016-1024. doi: 10.1016/S1053-2498(01)00298-4 [DOI] [PubMed] [Google Scholar]
- 12.Kim CA, Rasania SP, Afilalo J, Popma JJ, Lipsitz LA, Kim DH. Functional status and quality of life after transcatheter aortic valve replacement: a systematic review. Ann Intern Med. 2014;160(4):243-254. doi: 10.7326/M13-1316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.ClinicalTrials.gov Frailty Assessment Before Cardiac Surgery & Transcatheter Interventions. NCT01845207. https://clinicaltrials.gov/ct2/show/NCT01845207. Accessed December 17, 2018.
- 14.Online STS Adult Cardiac Surgery Risk Calculator http://riskcalc.sts.org/stswebriskcalc/#/. Accessed December 10, 2015.
- 15.Hoyl MT, Alessi CA, Harker JO, et al. Development and testing of a five-item version of the Geriatric Depression Scale. J Am Geriatr Soc. 1999;47(7):873-878. doi: 10.1111/j.1532-5415.1999.tb03848.x [DOI] [PubMed] [Google Scholar]
- 16.Beth Israel Deaconess Medical Center For providers: online tool to calculate frailty index (FI). https://www.bidmc.org/research/research-by-department/medicine/gerontology/calculator. Accessed December 17, 2018.
- 17.Rockwood K, Mitnitski A. Frailty in relation to the accumulation of deficits. J Gerontol A Biol Sci Med Sci. 2007;62(7):722-727. doi: 10.1093/gerona/62.7.722 [DOI] [PubMed] [Google Scholar]
- 18.Kappetein AP, Head SJ, Généreux P, et al. Updated standardized endpoint definitions for transcatheter aortic valve implantation: the Valve Academic Research Consortium–2 consensus document. J Am Coll Cardiol. 2012;60(15):1438-1454. doi: 10.1016/j.jacc.2012.09.001 [DOI] [PubMed] [Google Scholar]
- 19.Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method: a new method for detection of delirium. Ann Intern Med. 1990;113(12):941-948. doi: 10.7326/0003-4819-113-12-941 [DOI] [PubMed] [Google Scholar]
- 20.Kim DH, Lee J, Kim CA, et al. Evaluation of algorithms to identify delirium in administrative claims and drug utilization database. Pharmacoepidemiol Drug Saf. 2017;26(8):945-953. doi: 10.1002/pds.4226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nagi SZ. An epidemiology of disability among adults in the United States. Milbank Mem Fund Q Health Soc. 1976;54(4):439-467. doi: 10.2307/3349677 [DOI] [PubMed] [Google Scholar]
- 22.Rosow I, Breslau N. A Guttman health scale for the aged. J Gerontol. 1966;21(4):556-559. doi: 10.1093/geronj/21.4.556 [DOI] [PubMed] [Google Scholar]
- 23.Fong TG, Gleason LJ, Wong B, et al. ; Successful Aging after Elective Surgery Functional Measures Working Group . Cognitive and physical demands of activities of daily living in older adults: validation of expert panel ratings. PM R. 2015;7(7):727-735. doi: 10.1016/j.pmrj.2015.01.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Royston P, White IR. Multiple imputation by chained equations (MICE): implementation in Stata. J Stat Softw. 2011;45(4):1-20. doi: 10.18637/jss.v045.i04 [DOI] [Google Scholar]
- 25.Nagin DS, Odgers CL. Group-based trajectory modeling in clinical research. Annu Rev Clin Psychol. 2010;6:109-138. doi: 10.1146/annurev.clinpsy.121208.131413 [DOI] [PubMed] [Google Scholar]
- 26.Jones BL, Nagin DS, Roeder K. A SAS procedure based on mixture models for estimating developmental trajectories. Sociol Methods Res. 2001;29:374-393. doi: 10.1177/0049124101029003005 [DOI] [Google Scholar]
- 27.Reynolds MR, Magnuson EA, Lei Y, et al. ; Placement of Aortic Transcatheter Valves (PARTNER) Investigators . Health-related quality of life after transcatheter aortic valve replacement in inoperable patients with severe aortic stenosis. Circulation. 2011;124(18):1964-1972. doi: 10.1161/CIRCULATIONAHA.111.040022 [DOI] [PubMed] [Google Scholar]
- 28.Reynolds MR, Magnuson EA, Wang K, et al. ; PARTNER Trial Investigators . Health-related quality of life after transcatheter or surgical aortic valve replacement in high-risk patients with severe aortic stenosis: results from the PARTNER (Placement of AoRTic TraNscathetER Valve) Trial (cohort A). J Am Coll Cardiol. 2012;60(6):548-558. doi: 10.1016/j.jacc.2012.03.075 [DOI] [PubMed] [Google Scholar]
- 29.Arnold SV, Reynolds MR, Wang K, et al. ; CoreValve US Pivotal Trial Investigators . Health status after transcatheter or surgical aortic valve replacement in patients with severe aortic stenosis at increased surgical risk: results from the CoreValve US Pivotal Trial. JACC Cardiovasc Interv. 2015;8(9):1207-1217. doi: 10.1016/j.jcin.2015.04.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Osnabrugge RL, Arnold SV, Reynolds MR, et al. ; CoreValve US Trial Investigators . Health status after transcatheter aortic valve replacement in patients at extreme surgical risk: results from the CoreValve US trial. JACC Cardiovasc Interv. 2015;8(2):315-323. doi: 10.1016/j.jcin.2014.08.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Baron SJ, Arnold SV, Wang K, et al. ; PARTNER 2 Investigators . Health status benefits of transcatheter vs surgical aortic valve replacement in patients with severe aortic stenosis at intermediate surgical risk: results from the PARTNER 2 Randomized Clinical Trial. JAMA Cardiol. 2017;2(8):837-845. doi: 10.1001/jamacardio.2017.2039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Reardon MJ, Van Mieghem NM, Popma JJ, et al. ; SURTAVI Investigators . Surgical or transcatheter aortic-valve replacement in intermediate-risk patients. N Engl J Med. 2017;376(14):1321-1331. doi: 10.1056/NEJMoa1700456 [DOI] [PubMed] [Google Scholar]
- 33.Gada H, Kirtane AJ, Wang K, et al. ; PARTNER Investigators . Temporal trends in quality of life outcomes after transapical transcatheter aortic valve replacement: a placement of AoRTic TraNscathetER Valve (PARTNER) Trial substudy. Circ Cardiovasc Qual Outcomes. 2015;8(4):338-346. doi: 10.1161/CIRCOUTCOMES.114.001335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stańska A, Jagielak D, Brzeziński M, et al. Improvement of quality of life following transcatheter aortic valve implantation in the elderly: a multi-centre study based on the Polish national TAVI registry. Kardiol Pol. 2017;75(1):13-20. [DOI] [PubMed] [Google Scholar]
- 35.Eurich DT, Johnson JA, Reid KJ, Spertus JA. Assessing responsiveness of generic and specific health related quality of life measures in heart failure. Health Qual Life Outcomes. 2006;4:89. doi: 10.1186/1477-7525-4-89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wiebe S, Guyatt G, Weaver B, Matijevic S, Sidwell C. Comparative responsiveness of generic and specific quality-of-life instruments. J Clin Epidemiol. 2003;56(1):52-60. doi: 10.1016/S0895-4356(02)00537-1 [DOI] [PubMed] [Google Scholar]
- 37.Kruser JM, Nabozny MJ, Steffens NM, et al. “Best case/worst case”: qualitative evaluation of a novel communication tool for difficult in-the-moment surgical decisions. J Am Geriatr Soc. 2015;63(9):1805-1811. doi: 10.1111/jgs.13615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Taylor LJ, Nabozny MJ, Steffens NM, et al. A framework to improve surgeon communication in high-stakes surgical decisions: best case/worst case. JAMA Surg. 2017;152(6):531-538. doi: 10.1001/jamasurg.2016.5674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Popma JJ, Reardon MJ, Khabbaz K, et al. Early clinical outcomes after transcatheter aortic valve replacement using a novel self-expanding bioprosthesis in patients with severe aortic stenosis who are suboptimal for surgery: results of the Evolut R US Study. JACC Cardiovasc Interv. 2017;10(3):268-275. doi: 10.1016/j.jcin.2016.08.050 [DOI] [PubMed] [Google Scholar]
- 40.Villablanca PA, Mohananey D, Nikolic K, et al. Comparison of local versus general anesthesia in patients undergoing transcatheter aortic valve replacement: a meta-analysis. Catheter Cardiovasc Interv. 2018;91(2):330-342. [DOI] [PubMed] [Google Scholar]
- 41.Hshieh TT, Yue J, Oh E, et al. Effectiveness of multicomponent nonpharmacological delirium interventions: a meta-analysis. JAMA Intern Med. 2015;175(4):512-520. doi: 10.1001/jamainternmed.2014.7779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zanettini R, Gatto G, Mori I, et al. Cardiac rehabilitation and mid-term follow-up after transcatheter aortic valve implantation. J Geriatr Cardiol. 2014;11(4):279-285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sibilitz KL, Berg SK, Tang LH, et al. Exercise-based cardiac rehabilitation for adults after heart valve surgery. Cochrane Database Syst Rev. 2016;3:CD010876. [DOI] [PubMed] [Google Scholar]
- 44.Doll JA, Hellkamp A, Ho PM, et al. Participation in cardiac rehabilitation programs among older patients after acute myocardial infarction. JAMA Intern Med. 2015;175(10):1700-1702. doi: 10.1001/jamainternmed.2015.3819 [DOI] [PubMed] [Google Scholar]
- 45.Young Y, Boyd CM, Guralnik JM, Fried LP. Does self-reported function correspond to objective measures of functional impairment? J Am Med Dir Assoc. 2010;11(9):645-653. doi: 10.1016/j.jamda.2009.12.084 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Preoperative Characteristics of Patients by the Comprehensive Geriatric Assessment-Based Frailty Index Level
eTable 2. Postoperative Complications, Health Care Utilization, and Functional Status Trajectory After Transcatheter and Surgical Aortic Valve Replacement
eTable 3. Evidence Summary on the Quality of Life and Physical Function from Major Clinical Trials and Registries
eFigure 1. Comprehensive Geriatric Assessment-Based Frailty Index (CGA-FI)
eFigure 2. Patient Enrollment and Follow-Up