This cross-sectional study examines the feasibility of implementing an electronic health record–linked, automated reminder system for glaucoma medications and assesses patient satisfaction with the reminder system.
Key Points
Question
What is the performance of an electronic health record–linked telecommunication-based automated reminder system for glaucoma medications?
Findings
In this cross-sectional study in a university-based glaucoma clinic, 100 patients agreed to configure and use electronic health record–linked reminders for 3 months. Most participants found the reminders to be very useful or useful.
Meaning
Electronic health record–linked portals may represent a new and convenient way of allowing patients to link their glaucoma medications to automated reminders; additional longitudinal and glaucoma outcome data would help determine the clinical relevance of such portals.
Abstract
Importance
While dosing reminders for glaucoma medications have been shown to increase drug adherence, an outstanding limitation preventing broad adoption is difficulty linking reminders to medication in each patient’s electronic health record (EHR).
Objective
To examine the feasibility of implementing an EHR-linked, automated reminder system for glaucoma medications and assess patient satisfaction with it.
Design, Setting, and Participants
In this prospective, cross-sectional study, patients receiving glaucoma medications were recruited from a university-based glaucoma clinic from April 2017 to January 2018. Analysis began in February 2018.
Exposures
A web-based application was added to the EHR patient portal, allowing patients to configure telecommunication-based reminders for their glaucoma medications. For all potential participants, basic information was collected to determine risk of nonadherence with glaucoma medications. Those consenting to participate then answered questions on medication adherence, reminders, and their likelihood of using EHR-linked reminders. They then configured reminders using the EHR patient portal. After 3 months, they answered questions about their satisfaction with the system.
Main Outcomes and Measures
Proportions of patients and high-risk patients willing to use the reminders, and patient satisfaction with the system.
Results
Of 147 patients approached, 100 (68%) agreed to participate, of whom the majority were men (54 [54%]) and white (51 [51%]), with a mean (SD) age of 65 (12.4) years. There were no differences between those willing and unwilling to participate, except for a slightly lower self-reported medication adherence rate among those who participated (mean [SD], 91% [13.6%] vs 97% [6.0%]). Based on a previously validated risk assessment score, 9% (9 of 100) of participants were categorized as being at high risk for poor adherence (≥50% probability of nonadherence) compared with 11% (5 of 47) of nonparticipants. Of 100 participants, 94 ultimately configured reminders, of whom 89 (95%) completed follow-up. On follow-up, 74% (n = 66; 95% CI, 65-83) of participants found the reminders to be useful, 15% (n = 13) were neutral, and 11% (n = 10) found them not useful. Most participants (72 [81%]; 95% CI, 77-85) had help configuring reminders.
Conclusions and Relevance
Electronic health records–linked reminders had good uptake and were well received among patients at a tertiary glaucoma clinic. These portals may represent a new and convenient method of allowing patients to link their glaucoma medications to automated reminders, although the generalizability of these results and the effect on glaucoma outcomes remains unknown.
Introduction
Adherence to medications is integral to the management of glaucoma.1 Patient nonadherence with glaucoma medications is a well-documented problem and has been reported to range from 5% to 80%.2 A variety of causes for poor adherence have been identified, including inadequate patient education, complex dosing schedules, difficulty with application, adverse effects, and costs.3,4,5 A factor that has consistently been noted as a major problem is forgetting to use the medications.4,5,6,7
A systematic review of interventions to improve medication adherence noted improved patient adherence and clinical outcomes via increased interaction with patients, including dosing reminders.8 Adherence experts concluded that simple interventions that are feasible in busy clinical practices and are easily workable for clinicians and patients might be promising tools to increase adherence.9 Another systematic review reported that electronic reminders, especially text reminders, improve adherence to long-term medication.10
In a randomized clinical trial, patients receiving personal telephone calls and automated reminders had an improvement in their adherence rate from 54% to 73% compared with no change in the control arm.11 A second study demonstrated that an automated telecommunication-based reminder system could have the same effect on adherence.12
One limitation preventing broad adoption of automated reminders is the difficulty linking reminders to the medications the patient is using. The rapid increase in the adoption of electronic health records (EHRs) in ophthalmology13,14 might be an opportunity in this regard.
We built and evaluated an extension to our EHR patient portal that allows patients to configure reminders for their glaucoma medications. Such a system is likely superior to alarms on a mobile device in that there is the potential for some oversight of reminders by the clinician to make sure they are being applied to current medications.
Methods
Participants were recruited from the glaucoma clinic of the Johns Hopkins Wilmer Eye Institute from April 2017 to January 2018. Analysis began in February 2018. This study was approved by the Johns Hopkins University School of Medicine institutional review board. Informed written consent was obtained from all participants.
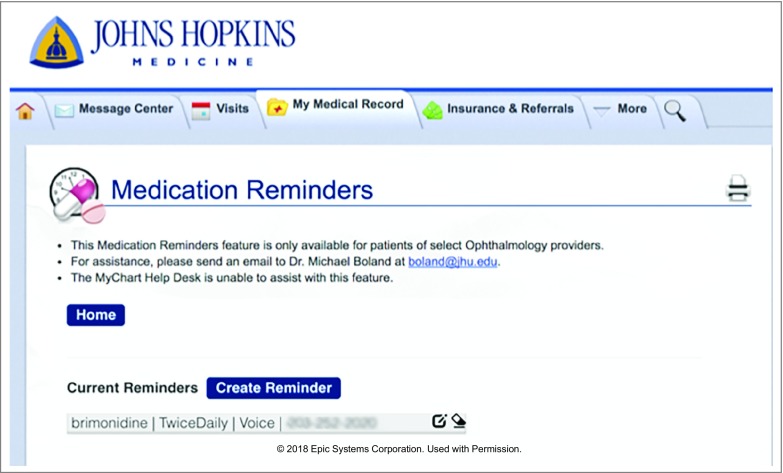
Adding Reminders to the Patient Portal
We designed and built a web-based application to allow configuration of medication reminders using our EHR patient portal that allows patients to access portions of their clinical data (MyChart; Epic Systems). Our application connected to the EHR using existing application programming interfaces. The application allows patients to select a medication from their list in their EHR and then specify how (voice/text) and when they would like to be reminded. After the construction of the patient interface, we built a separate database for storing information needed to deliver the reminders including medication name and the timing and format (ie, text or voice). A third party telecommunication vendor was used to deliver the messages.
Text-based reminders prompted patients to use their eyedrops and requested a response within 30 minutes. If participants did not respond after 30 minutes, they received a second message encouraging them to respond promptly. Participants receiving voice calls received no additional messages.
Study Procedures
Patients using topical glaucoma medications and presenting to the glaucoma clinic with (1) an ability to converse in and read English, (2) the ability to provide written informed consent, and (3) willingness to complete the study were eligible for recruitment. For all potential participants, we collected nonidentifying demographic information to determine factors that predicted enrollment. We used these data to estimate the risk of nonadherence using a previously validated system.15 Briefly, risk factors for nonadherence include younger age, black race, worse general health, shorter duration of medication use, lower self-reported adherence, and admitting to not following physicians’ orders.
Patients consenting to participate were asked a series of questions regarding adherence, reminders, and their likelihood of using a computer-based system to configure medication reminders (eAppendix 1 in the Supplement). Study participants who had not previously enrolled in MyChart were either helped by a research coordinator or received a pamphlet detailing the procedure to set it up on their own at a later time.
Once enrolled in MyChart, study participants were asked to use the custom web interface to configure reminders for some or all of their glaucoma medications (Figure 1). If a participant felt they could not complete this task, it was determined whether a family member could assist. If not, a research coordinator offered to help the participant to configure the reminders. Participants who opted to set up their reminders at a later time were given detailed written instructions on how to configure reminders (eAppendix 2 in the Supplement) and also were provided with the option of calling a research coordinator to get assistance. For the participants who opted to set up the reminders remotely, up to 3 attempts were made to reach them to ensure the reminders were configured, after which they were designated as lost to follow-up.
Figure 1. Automated Reminder Through the MyChart Application.
A research coordinator contacted participants via telephone 3 months after enrollment to collect information on their experience with the system. Up to 6 attempts were made to reach participants via telephone, after which they were designated as lost to follow-up.
Statistical Analysis
Study data were entered into a clinical research data management system (REDCap version 6.5.14; Vanderbilt University). t Test and Fisher exact test were used to summarize continuous and categorical data respectively. A risk assessment score predicting nonadherence to topical glaucoma medications (ranging from 0 to 100) was calculated for both groups based on answers provided to 6 questions as described previously.15 Consistent with prior work, nonadherence was defined as using 75% or fewer of prescribed doses within 4 hours of the dosing time. Based on that definition, participants were categorized as high risk if they had 50% or more probability of nonadherence. The primary study outcome was the proportion of patients willing to configure and use the reminders and the proportion of high-risk patients willing to do the same. Using the demographics collected from all participants and potential participants, we determined the proportion of high-risk patients who were not willing to use such a system of reminders. All analyses were performed using Stata statistical software (version 14, StataCorp).
Results
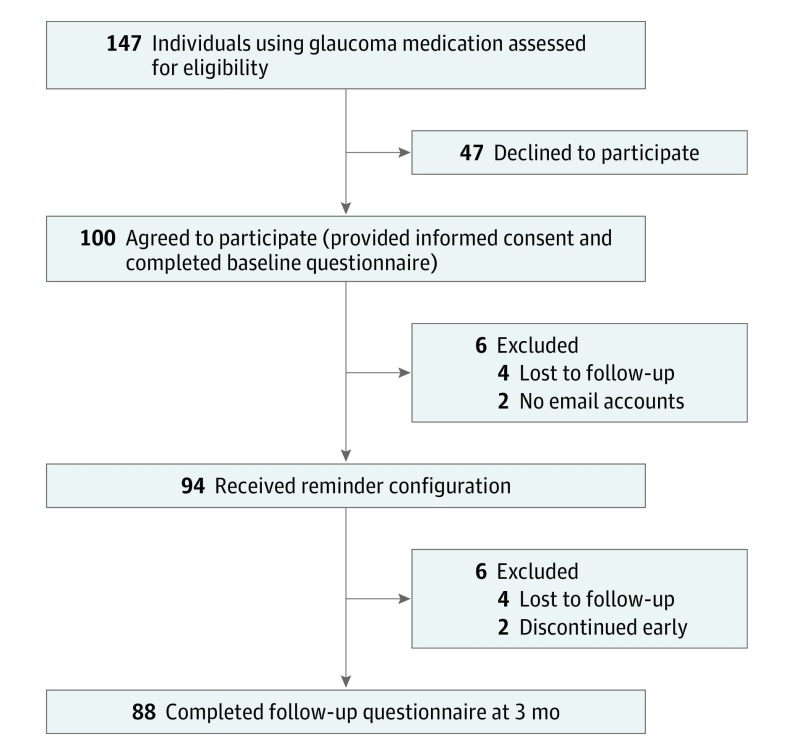
A total of 147 patients were approached and 100 (68%) agreed to participate (Figure 2). The mean (SD) age was 65 (12.4) years, 64 (64%) were men, and 51 (51%) were white (Table 1). Most participants (85 [85%]) reported being in excellent or good health and agreed or strongly agreed that they followed physicians’ orders exactly (94 [94%]). The mean (SD) duration of glaucoma medication use was 11.3 (9.1) years, and participants reported a mean (SD) adherence rate of 91% (13.6%) with their glaucoma medications during the past month. Nonparticipants had similar characteristics to the participant group, except for a higher mean (SD) self-reported treatment adherence rate of 97% (6.0%) (Table 1). However, 9 participants (9%) were categorized as high risk (≥50% probability of nonadherence) compared with 5 nonparticipants (11%).
Figure 2. Flow of Participants Through the Study.
Table 1. Characteristics of Participant and Nonparticipant Groups.
| Characteristic | Nonparticipants (n = 47) |
Participants (n = 100) |
|---|---|---|
| Age, mean (SD), y | 69 (9.9) | 65 (12.4) |
| Men, No. (%) | NA | 64 (64) |
| Race, No. (%) | ||
| White | 17 (37) | 51 (51) |
| Black | 20 (43) | 33 (33) |
| Asian | 8 (17) | 13 (13) |
| Othera | 1 (2) | 3 (3) |
| General health, No. (%) | ||
| Excellent | 8 (17) | 30 (30) |
| Good | 27 (57) | 55 (55) |
| Fair | 11 (23) | 14 (14) |
| Poor | 1 (2) | 1(1) |
| Duration of glaucoma medication use, mean (SD), y | 8.9 (6.7) | 11.3 (9.1) |
| Self-reported glaucoma medication adherence over past month, mean (SD), % | 97 (6.0) | 91 (13.6) |
| Follows physicians’ orders, No. (%) | ||
| Strongly agree | 34 (72) | 57 (57) |
| Agree | 11 (23) | 37 (37) |
| Neutral | 2 (4) | 6 (6) |
| Nonadherence score, mean (SD)b | 35.9 (19.3) | 34.5 (18.8) |
| ≥50% Probability of nonadherence, No. (%)a | 5 (11) | 9 (9) |
Abbreviation: NA, not available.
Included Asian, Native American, and other.
Calculated using a 6-question risk calculator.
Baseline Questionnaire: Assessment of Attitudes About Reminders
A majority of participants (59 [59%]) reported having 1 or more strategies for remembering their eyedrops. Strategies fell into the following categories: (1) timed with waking up/going to bed (20 [20%]); (2) timed with other activities such as brushing teeth, drinking coffee, eating meals, or using oral medications (15 [15%]); (3) eyedrops located where easily visible such as night stand or bathroom sink (14 [14%]); (4) telephone alarm (8 [8%]); (5) help from spouse/partner (4 [4%]); and (6) other strategies such as time tables or sticky notes (7 [7%]). The majority of participants with a strategy reported that theirs worked well or very well (53 of 59 [90%]), 5 participants (8%) said they worked fairly well, and 1 participant (2%) said it worked poorly.
Among the study population, 28 (28%) were very interested in receiving automated EHR-linked reminders, 48 (48%) were interested, 13 (13%) were neutral, 7 (7%) were not interested, and 4 (4%) were not at all interested. Regarding reminders, 67 (67%) preferred text messages; 26 (26%), voice messages; and 7 (7%), email.
In terms of numbers of topical glaucoma medications, 31 (31%) used 1, 48 (48%) used 2, 19 (19%) used 3, and 2 (2%) used 4. Patients using more than 1 type of eyedrop (69 [69%]) were given the option to configure reminders for any or all of them. Most participants (45 [65%]) opted to configure a reminder for a single medication, and the rest configured reminders for each type of eyedrop.
Accessing the Patient Portal
Among all participants, 60 (60%) were not enrolled in the patient portal. The reasons provided for not having activated their account were: (1) did not get around to it (24 [40%]); (2) did not want or need it (15 [25%]); (3) lacked technological skills to set it up (14 [23%]); (4) did not know about it or this was the first clinic visit (6 [10%]); and (5) gave up after technical difficulties (1 [2%]).
Of those without active portal accounts, 5 participants (8%) reported preferring to sign up for it on their own, 2 (3%) preferred help from a family member, and 53 (88%) preferred help from someone in the clinic. Of the 53 who needed help in the clinic, 10 (19%) needed email addresses. Of these, 8 were created by the research coordinator, and 2 participants exited the study at this stage.
Among the 98 remaining study participants, a research coordinator configured the reminders for 75 individuals (77%) at enrollment, and the remainder did so on their own or with help. Of these 23 participants who opted to configure their reminders later, 4 participants were lost to follow-up. It took the research coordinator anywhere between 5 and 20 minutes to complete setup, depending on whether participants had active email and/or MyChart accounts and/or remembered their log in details.
Assessment of Attitudes About the Automated Reminder System
Of the 94 participants who remained in the study, 88 (94%) were successfully followed up through 3 months. Four participants were lost to follow-up, and 2 participants discontinued the study early (1 participant had privacy concerns, and the other found the reminders disruptive/annoying) (Figure 2). The participant who withdrew because of the reminders still completed the follow-up questionnaire.
The majority (66 [74%]; 95% CI, 65-83) of participants found the reminders to be very useful or useful, 15% (n = 13; 95% CI, 7-23) were neutral, and 11% (n = 10; 95% CI, 4-18) found them to be not useful or not at all useful (Table 2). Most participants (72 [81%]; 95% CI, 77-85) had help configuring reminders. Of the 17 participants (95% CI, 11-27) who configured their own reminders, 14 (82%) found it was very easy or easy, while 3 (18%) found it very difficult or difficult.
Table 2. Participant Feedback at 3-Month Follow-up (n = 89)a.
| Variable | No. (%) |
|---|---|
| Usefulness of reminders | |
| Very useful | 28 (31) |
| Useful | 38 (43) |
| Neutral | 13 (15) |
| Not useful | 6 (7) |
| Not at all useful | 4 (4) |
| Ease of configuration | |
| Not applicable | 72 (81) |
| Very difficult | 1 (1) |
| Neutral | 2 (2) |
| Difficult | 8 (9) |
| Easy | 6 (7) |
| Very easy | 72 (81) |
| Likeliness to continue using reminders | |
| Very likely | 18 (20) |
| Likely | 24 (27) |
| Neutral | 10 (11) |
| Unlikely | 24 (27) |
| Very unlikely | 13 (15) |
Includes feedback from 1 participant that discontinued the study after 1 month.
When participants were asked about how likely they were to continue using these reminders, 47% (n = 42; 95% CI, 36-58) reported that they were very likely or likely, 11% (n = 10; 95% CI, 4-18) were neutral, and another 42% (n = 37; 95% CI, 32-53) said they were very unlikely or unlikely. Those wanting to continue using reminders were more likely to have 50% or higher probability of nonadherence (7 of 42 [17%]) compared with 2% (1 of 47) among those not wanting to continue (P = .03; 95% CI for difference, 4%-26%).
In open-ended feedback from participants regarding what they disliked about the reminder system, 10 participants responded that it was of no added benefit to them because they were already compliant or had their own prior reminder strategies; another 10 participants disliked having to respond when they had administered their eyedrops, 4 participants felt that the tone of the reminder message was terse, and 20 participants had complaints about technical glitches encountered with the system, including issues with setting up reminders, receiving extra reminders, receiving reminders at the incorrect time after a change from standard to daylight saving time, and improper acknowledgment of their response confirming that they had used their eyedrops (eAppendix 3 in the Supplement). Participants also suggested enhancements to the reminder system including allowing separate reminder times for weekdays and weekends, receiving voicemails for unanswered voice call reminders, and the ability to have the reminders work during travel across time zones (eAppendix 3 in the Supplement).
In terms of positive feedback, the majority of participants (70 [79%]) liked that the reminders were consistent, reliable, simple, and succinct; 8 participants (9%) felt that the reminders were especially useful on weekends and while traveling when they had a tendency to forget, and 5 participants (6%) liked that they had to respond after using their eyedrops as it demanded more accountability and ensured more timely and consistent use (eAppendix 4 in the Supplement).
Discussion
An EHR-linked telecommunication-based automated reminder system for glaucoma medication was well received by a population in a tertiary glaucoma clinic. Study participation and willingness to configure and use automated reminders were not influenced by risk of medication nonadherence, suggesting that the most at-risk patients would not also opt out of such a system.15 Most participants preferred to have their reminders set up with help from a research coordinator, although the majority of those who configured the reminders on their own found it was easy to use. However, 4 of 17 participants who opted to configure their reminders at home were lost to follow-up, suggesting possible issues with ease of use. Two-thirds of participants also found the reminders to be useful, and about half the participants said they were likely to want to continue using such a system. However, these proportions are likely an overestimate as the 4 participants lost to follow-up might have stopped using the reminders for a number of reasons. Nevertheless, this study showed that an EHR-linked system permitted most patients to configure and receive automated reminders.
While the majority of study participants (91%) had a low (<50%) estimated risk of nonadherence, nonadherence with medications is a problem among patients with glaucoma with myriad reasons for noncompliance ranging from difficulties with affording eyedrops to difficulties instilling them.4,5,6,7 The most common reason reported by patients is simply forgetting to use eyedrops, a cause that is amenable to reminders. Prior studies in glaucoma and other medical fields have shown that increasing patient interaction via dosing reminders improves patient adherence to medications.8,10,11,12 Two prior randomized clinical trials showed that patients with glaucoma with poor adherence and who received automated reminders for glaucoma eyedrops had improved adherence rates of almost 20%.11,12
In terms of subjective feedback, a prior study12 at our institution found 84% of participants who received once-daily voice or text-based dosing reminders felt that they were helpful and that if available, they would continue using them outside the study. In comparison, only 47% of participants in the present study were willing to continue using the reminders after the study ended. The lower proportion willing to continue here may be associated with differences in characteristics of study participants between the studies or owing to changes in the awareness of and approach to adherence in the clinic over time. For example, the majority (59%) of participants who joined the study reported already having a method to help them remember to use their eyedrops. Furthermore, many who signed up for the study may have done so out of an altruistic desire to help us develop new systems to improve patient care and did not feel a personal need for reminders. This may also explain why most participants who were using more than 1 eyedrop opted to configure a reminder for a single medication only.
Despite the wealth of research into electronic dosing reminders for glaucoma medication, studies so far have not attempted to link such reminders to patients’ medication lists in EHRs, to our knowledge. Electronic health records are being increasingly used13,14 to capture and store patient information, and patients are given access to their data via web-based portals. These portals now constitute an obvious channel to allow patients to link their medications to reminders, and this study is the first to explore this option, to our knowledge. However, it is possible that those patients at greatest risk of nonadherence may be least likely to self-actualize and use this tool to potentially improve outcomes. Thus, a tool activated by caregivers concurrent with medication prescription or after identification of missed refills or risk factors for nonadherence may be worthy of further investigation.
Limitations
We encountered some technical issues with reminder setup and implementation including web browser compatibility, changes between daylight saving and standard time, and the behavior of the confirmation messages. Further refinement of the system is required to avoid such errors. Future enhancements might include voicemail reminders when the call is not answered, email-based reminders, and greater flexibility of the reminder scheduling. Second, we acknowledge that this kind of system may not be most appropriate for some patients given it works best with a mobile telephone and requires an active email address. Of note, 2 of 10 patients without email accounts opted out of the study citing unfamiliarity with or mistrust of such systems. Third, our findings reflect acceptance of reminders in a tertiary glaucoma clinic that may not be generalizable to other populations that may not be as compliant with dosing or comfortable with web-based portals. Fourth, we used convenience sampling, which raises the question of selection bias in that our study population may comprise individuals more likely to be approached or willing to participate. Finally, we did not collect data on the reasons behind why one-third of the individuals approached were unwilling to use the reminders, and this deserves further investigation.
Conclusions
In conclusion, given the increasing ubiquity of electronic collection and storage of patient health information, an EHR-linked reminder system for glaucoma medications is likely a convenient way for patients to configure and receive automated reminders pending further longitudinal studies addressing how such portals ultimately address adherence and glaucoma outcomes.
eAppendix 1. Study survey instruments
eAppendix 2. Participant instructions on how to configure reminders
eAppendix 3. Summary of negative feedback & suggestions from participants
eAppendix 4. Summary of positive comments from participants
References
- 1.Lee MD, Fechtner FR, Fiscella RG, Singh K, Stewart WC. Emerging perspectives on glaucoma: highlights of a roundtable discussion. Am J Ophthalmol. 2000;130(4)(suppl):S1-S11. doi: 10.1016/S0002-9394(00)00635-8 [DOI] [PubMed] [Google Scholar]
- 2.Olthoff CM, Schouten JS, van de Borne BW, Webers CA. Noncompliance with ocular hypotensive treatment in patients with glaucoma or ocular hypertension an evidence-based review. Ophthalmology. 2005;112(6):953-961. doi: 10.1016/j.ophtha.2004.12.035 [DOI] [PubMed] [Google Scholar]
- 3.Tsai JC, McClure CA, Ramos SE, Schlundt DG, Pichert JW. Compliance barriers in glaucoma: a systematic classification. J Glaucoma. 2003;12(5):393-398. doi: 10.1097/00061198-200310000-00001 [DOI] [PubMed] [Google Scholar]
- 4.Lacey J, Cate H, Broadway DC. Barriers to adherence with glaucoma medications: a qualitative research study. Eye (Lond). 2009;23(4):924-932. doi: 10.1038/eye.2008.103 [DOI] [PubMed] [Google Scholar]
- 5.Taylor SA, Galbraith SM, Mills RP. Causes of non-compliance with drug regimens in glaucoma patients: a qualitative study. J Ocul Pharmacol Ther. 2002;18(5):401-409. doi: 10.1089/10807680260362687 [DOI] [PubMed] [Google Scholar]
- 6.Reeder CE, Franklin M, Bramley TJ. Managed care and the impact of glaucoma. Am J Manag Care. 2008;14(1)(suppl):S5-S10. [PubMed] [Google Scholar]
- 7.Patel SC, Spaeth GL. Compliance in patients prescribed eyedrops for glaucoma. Ophthalmic Surg. 1995;26(3):233-236. [PubMed] [Google Scholar]
- 8.Haynes RB, Ackloo E, Sahota N, McDonald HP, Yao X. Interventions for enhancing medication adherence. Cochrane Database Syst Rev. 2008;(2):CD000011. [DOI] [PubMed] [Google Scholar]
- 9.van Dulmen S, Sluijs E, van Dijk L, de Ridder D, Heerdink R, Bensing J; International Expert Forum on Patient Adherence . Furthering patient adherence: a position paper of the international expert forum on patient adherence based on an internet forum discussion. BMC Health Serv Res. 2008;8(1):47. doi: 10.1186/1472-6963-8-47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vervloet M, Linn AJ, van Weert JC, de Bakker DH, Bouvy ML, van Dijk L. The effectiveness of interventions using electronic reminders to improve adherence to chronic medication: a systematic review of the literature. J Am Med Inform Assoc. 2012;19(5):696-704. doi: 10.1136/amiajnl-2011-000748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Okeke CO, Quigley HA, Jampel HD, et al. Interventions improve poor adherence with once daily glaucoma medications in electronically monitored patients. Ophthalmology. 2009;116(12):2286-2293. doi: 10.1016/j.ophtha.2009.05.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Boland MV, Chang DS, Frazier T, Plyler R, Jefferys JL, Friedman DS. Automated telecommunication-based reminders and adherence with once-daily glaucoma medication dosing: the automated dosing reminder study. JAMA Ophthalmol. 2014;132(7):845-850. doi: 10.1001/jamaophthalmol.2014.857 [DOI] [PubMed] [Google Scholar]
- 13.Chiang MF, Boland MV, Margolis JW, Lum F, Abramoff MD, Hildebrand PL; American Academy of Ophthalmology Medical Information Technology Committee . Adoption and perceptions of electronic health record systems by ophthalmologists: an American Academy of Ophthalmology survey. Ophthalmology. 2008;115(9):1591-1597. doi: 10.1016/j.ophtha.2008.03.024 [DOI] [PubMed] [Google Scholar]
- 14.Boland MV, Chiang MF, Lim MC, et al. ; American Academy of Ophthalmology Medical Information Technology Committee . Adoption of electronic health records and preparations for demonstrating meaningful use: an American Academy of Ophthalmology survey. Ophthalmology. 2013;120(8):1702-1710. doi: 10.1016/j.ophtha.2013.04.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chang DS, Friedman DS, Frazier T, Plyler R, Boland MV. Development and validation of a predictive model for nonadherence with once-daily glaucoma medications. Ophthalmology. 2013;120(7):1396-1402. doi: 10.1016/j.ophtha.2013.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix 1. Study survey instruments
eAppendix 2. Participant instructions on how to configure reminders
eAppendix 3. Summary of negative feedback & suggestions from participants
eAppendix 4. Summary of positive comments from participants