Key Points
Question
What are the dynamic associations among motor activity, energy, mood, and sleep, as tracked in real time with mobile monitoring technology, in individuals with a history of bipolar disorder or major depression?
Findings
In this case-control study of 242 adults, bidirectional associations were found between motor activity with subjectively rated energy level and sleep duration as well as unidirectional associations between motor activity and mood level. Greater cross-domain reactivity was observed for these associations in people with bipolar I disorder.
Meaning
Interventions that target motor activity and energy may alleviate depressed mood more effectively than could current approaches; simultaneous investigations of multiple regulatory systems in bipolar disorder are important in designing therapeutic targets.
Abstract
Importance
Biologic systems involved in the regulation of motor activity are intricately linked with other homeostatic systems such as sleep, feeding behavior, energy, and mood. Mobile monitoring technology (eg, actigraphy and ecological momentary assessment devices) allows the assessment of these multiple systems in real time. However, most clinical studies of mental disorders that use mobile devices have not focused on the dynamic associations between these systems.
Objectives
To examine the directional associations among motor activity, energy, mood, and sleep using mobile monitoring in a community-identified sample, and to evaluate whether these within-day associations differ between people with a history of bipolar or other mood disorders and controls without mood disorders.
Design, Setting, and Participants
This study used a nested case-control design of 242 adults, a subsample of a community-based sample of adults. Probands were recruited by mail from the greater Washington, DC, metropolitan area from January 2005 to June 2013. Enrichment of the sample for mood disorders was provided by volunteers or referrals from the National Institutes of Health Clinical Center or by participants in the National Institute of Mental Health Mood and Anxiety Disorders Program. The inclusion criteria were the ability to speak English, availability to participate, and consent to contact at least 2 living first-degree relatives. Data analysis was performed from June 2013 through July 2018.
Main Outcomes and Measures
Motor activity and sleep duration data were obtained from minute-to-minute activity counts from an actigraphy device worn on the nondominant wrist for 2 weeks. Mood and energy levels were assessed by subjective analogue ratings on the ecological momentary assessment (using a personal digital assistant) by participants 4 times per day for 2 weeks.
Results
Of the total 242 participants, 92 (38.1%) were men and 150 (61.9%) were women, with a mean (SD) age of 48 (16.9) years. Among the participants, 54 (22.3%) had bipolar disorder (25 with bipolar I; 29 with bipolar II), 91 (37.6%) had major depressive disorder, and 97 (40.1%) were controls with no history of mood disorders. A unidirectional association was found between motor activity and subjective mood level (β = –0.018, P = .04). Bidirectional associations were observed between motor activity (β = 0.176; P = .03) and subjective energy level (β = 0.027; P = .03) as well as between motor activity (β = –0.027; P = .04) and sleep duration (β = –0.154; P = .04). Greater cross-domain reactivity was observed in bipolar disorder across all outcomes, including motor activity, sleep, mood, and energy.
Conclusions and Relevance
These findings suggest that interventions focused on motor activity and energy may have greater efficacy than current approaches that target depressed mood; both active and passive tracking of multiple regulatory systems are important in designing therapeutic targets.
This case-control study examines the real-time changes and associations between physical activity, sleep patterns, and energy and mood levels in people with and those without bipolar or depressive disorder.
Introduction
The role of physical activity in human health has received increasing attention in both medicine and public health. Physical activity is associated with numerous human functional processes, including cognition, sleep, and weight regulation1,2; in contrast, low physical activity is increasingly recognized as a risk factor for diabetes,3 cardiovascular disease,4 cancers,5,6 and mental disorders.7,8 Mobile monitoring, which allows simultaneous, frequent, and reliable assessment of multiple systems in real time, has provided new opportunities for obtaining an objective assessment of physical activity.
Patterns of motor activity are assessed through actigraphy, in which a wrist-worn device provides objective and high-density measurements of physical movement in natural living environments.9 Actigraphy has been used primarily to derive objective measures of sleep characteristics,10,11 but interest in 24-hour patterns of motor activity,12 sedentary behavior,13 physical activity or exercise,14 and weight regulation15 has been increasing. With the recent growth in the use of actigraphy, data are now available from several large population-based studies14,16,17,18 and from studies of specific conditions, such as diabetes3,19 and cardiovascular disease.20,21 In addition, there has been a resurgence of the use of actigraphy to assess physical activity in people with mental disorders, including mood disorders,22,23 schizophrenia,24 attention deficit disorder,25 and posttraumatic stress disorder.26 Consistent evidence now exists for the dysregulation of motor activity in people with bipolar disorder.27,28,29,30,31,32
Basic research has shown that the biologic systems involved in the regulation of motor activity are associated with other homeostatic systems such as sleep, feeding behavior, energy, and mood.32,33 For example, shared circuits have been shown to affect sleep and metabolic systems,34 sleep and feeding behavior,35 and motor activity and metabolism or energy.36,37 However, most clinical research in mental disorders that uses mobile devices has focused on either sleep or motor activity rather than on the associations between them. Moreover, a key challenge lies in associating these objectively measured systems with the subjective psychological states that remain central to mental disorders, particularly mood and cognitive experience. This limitation can be overcome by administering ecological momentary assessment (EMA), which has been widely used to investigate emotional regulation in real time in people with mood and other mental disorders. Furthermore, EMA overcomes the temporal and contextual limitations of traditional clinical measures.38,39,40,41,42,43,44 The concomitant use of both EMA and actigraphy provides a powerful approach to investigating the context of passively acquired data as well as the directional patterns and associations of homeostatic regulatory networks.
The specific aims of this study were to (1) characterize the direction of the associations among activity, energy, mood, and sleep in the natural context of daily life, using a combination of actigraphy and EMA in a community-based sample of adults and youth, and (2) evaluate whether these patterns differ in people with a history of bipolar disorder or major depression compared with controls (people without bipolar or major depression). Our hypothesis was that people with bipolar I disorder have greater sensitivity to changes in homeostatic networks as indexed by greater directional associations among activity, energy, mood, and sleep.
Methods
Study Design and Sample
This study used a nested case-control design and involved a community-based sample of 242 adults. Probands were recruited from the greater Washington, DC, metropolitan area from January 2005 to June 2013. Enrichment of the sample for mood disorders was provided by volunteers or referrals from the National Institutes of Health Clinical Center or participants in the National Institute of Mental Health Mood and Anxiety Disorders Program. The community sample, designed to be a nontreatment or nonclinical group with and without mental health disorders, was ascertained by mail contact; the addresses were obtained from a marketing list of households within a 50-mile radius of Washington, DC. Inclusion criteria were the ability to speak English, availability to participate, and consent to contact at least 2 living first-degree relatives. Additional details of the family study methods are described in Merikangas et al.45 All participants provided written informed consent, and the study was approved by the Combined Neuroscience Institutional Review Board at the National Institutes of Health. Data analysis was performed from June 2013 through July 2018.
The sample included 242 adults, all of whom were evaluated at the National Institutes of Health Clinical Center.45 Other characteristics of the subsample who participated in actigraphy monitoring and EMA rating are presented in previous publications.46,47
Measures
DSM-IV mood disorder diagnoses were based on semistructured diagnostic interviews. The controls (n = 97) had no lifetime history of mood disorders. Actigraphy monitors (Respironics and Actiwatch Score; Philips Respironics), which collect minute-by-minute activity counts, were worn by participants on their nondominant wrist for 2 weeks.
Data on sleep duration (sleep and wake-up times) were obtained from the actigraphy monitor. Wake and sleep periods were defined by a default threshold of fewer than 40 counts per period for more than 10 minutes. This threshold setting has been shown to provide a reliable discrimination between sleep and wake periods, when validated against polysomnography.48
Along with wearing an actigraphy device, participants completed EMAs 4 times per day, with an approximately 4-hour delay between assessments, for 2 weeks. Because the comprehensive superiority of fixed over random assessments has not been established and empirical findings are similar for both approaches,49,50 fixed intervals were chosen for the present study to facilitate the examination of rhythms and routines, which are more accurately characterized when individuals describe their specific behaviors at the same time over a number of days. The EMA included separate 7-point Likert scales to measure the degree to which participants felt very happy (1) to very sad (7) as well as very tired (1) to very energetic (7). These questions were administered through a personal digital assistant (Tungsten E2 PDA; Palm) provided to participants for the duration of the study. Since 2013, the EMA has been administered on an Android platform. Participants were compensated for their completion of the EMA and actigraphy per standard institutional review board procedures.
Statistical Analysis
Outcome Variables
The original 7-level measures of mood and energy were centered around the group median, the median of measures at that same time of the day across all participants and all days; therefore, mood and energy variables indicate deviations from the diurnal sample median. The mean activity counts between each of the EMA assessments were calculated and then transformed using the Box-Cox method to accommodate for skewed data. The transformed mean activity variables were then centered by the group mean across all participants and all days at that same time.
Covariates
Age, sex, body mass index (BMI; calculated as weight in kilograms divided by height in meters squared), and use of medications for mood disorders (antidepressants, mood stabilizers, anxiolytics) that have been associated with physical activity were included as covariates in the models. In the analyses of physical activity and psychological states (mood and energy), we controlled for total sleep duration of the previous night. Weekday and weekend status were also controlled because of the large differences in the key outcome variables. Because no change in the estimates was observed after controlling for medication use, this variable was not included in the final models.
Missing Data
Based on established procedures for EMA data, the start day of mobile monitoring assessments was random to avoid systematic bias in missing data by day of the week. No statistically significant fatigue effect, defined as increases in missing EMA or actigraphy data as a function of day of the study, was observed. No group differences were found in the percentage of missing data for EMA.
Statistical Methods
Generalized estimating equation models were used to make a conditional estimate of the dynamic association among motor activity, sleep, and psychological states while accounting for the lagged associations of various systems. We included the 3 mood disorder subtypes (bipolar I, bipolar II, and major depression) as binary variables in the generalized estimating equation models, and all other covariates (including sex, age, BMI, and medication use) were the independent variables. The reference group for each mood disorder subtype was the control group without a history of mood disorder. We employed deviations from diurnal medians as the primary measure because the population-level diurnal patterns observed in the key study variables violate a key assumption (stationarity) of Granger causality models. The first-order autoregressive working correlation structure was chosen to take into account the within-person correlation over the 2-week observation period. Wald χ2 test was used to test the significance of each variable and their respective 2-sided P values at the α = .05 level. All analyses were conducted using SAS, version 9.3 (SAS Institute Inc).
Results
Of the total 242 participants, 92 (38.1%) were men and 150 (61.9%) were women, with a mean (SD) age of 48 (16.9) years. Among the participants, 54 (22.3%) had bipolar disorder (25 with bipolar I; 29 with bipolar II), 91 (37.6%) had major depressive disorder, and 97 (40.1%) were controls with no lifetime history of mood disorders.
Prospective Association of Motor Activity on Subsequent Mood and Energy
Table 1 presents the prospective association of motor activity with subsequent subjective mood (top) and energy (bottom) levels in the total sample as well as the associations with mood disorder subtype compared with controls. After controlling for sex, age, BMI, weekday vs weekend status, and status of the outcome in the previous assessment, we found a statistically significant inverse association between observed activity in one period and sad mood level in the next period (β = –0.018; P = .04) as well as a positive association between activity and energy level in the next period (β = 0.027; P = .03). Sad mood levels decreased with age and were lower on weekends compared with weekdays (β = 0.10; P < .001). Actigraphy-estimated sleep duration from the previous night was associated with motor activity in the energy-predicting activity model (β = −0.154; P = .04) but not in the mood-predicting motor activity model (β = –0.131; P = .06), or with mood (β = 0.009; P = .51) or energy (β = 0.022; P = .36) level on the next day. Models that tested the interactions between the mood disorder subtypes and activity yielded significant interactions between motor activity and bipolar I disorder on both mood (β = –0.035; P = .03) and energy (β = 0.062; P = .004) levels. Specifically, increased activity was associated with greater changes in mood, energy, and sleep duration among those with bipolar I disorder compared with controls. No interactions emerged for the other 2 mood disorder subtypes.
Table 1. Lagged Associations Between Motor Activity on Mood (Top) and Energy (Bottom).
| Category | Estimate | P Value |
|---|---|---|
| Outcome: Moodta | ||
| Motor activityt-1b | −0.018 | .04c |
| Mood disorder subtype | ||
| Bipolar I | 0.125 | .09 |
| Bipolar II | 0.167 | .03c |
| Major depression | 0.026 | .63 |
| Interactions | ||
| Activityt-1 × bipolar I | −0.035 | .03c |
| Activityt-1 × bipolar II | −0.007 | .67 |
| Activityt-1 × major depression | 0.012 | .41 |
| Model covariates | ||
| Age | −0.003 | .049c |
| Sex (F vs M) | −0.047 | .36 |
| Body mass index | 0.005 | .19 |
| Moodt-1 | 0.675 | <.001c |
| Sleep duration, h | 0.009 | .51 |
| Weekday | 0.100 | <.001c |
| Outcome: Energytd | ||
| Motor activityt-1 | 0.027 | .03c |
| Mood disorder subtype | ||
| Bipolar I | −0.145 | .17 |
| Bipolar II | 0.005 | .97 |
| Major depression | −0.073 | .39 |
| Interactions | ||
| Activityt-1 × bipolar I | 0.062 | .004c |
| Activityt-1 × bipolar II | 0.006 | .82 |
| Activityt-1 × major depression | −0.010 | .64 |
| Model covariates | ||
| Age | 0.002 | .38 |
| Sex (F vs M) | −0.144 | .07 |
| Body mass index | 0.001 | .84 |
| Energyt-1 | 0.411 | <.001c |
| Sleep duration, h | 0.022 | .36 |
| Weekday | −0.030 | .42 |
Abbreviations: F, female; M, male; t, period; t-1, same domain in previous period (Granger model).
Analog mood scale rated by participant 4 times per day for 2 weeks.
Mean counts per minute for each period.
Denotes statistically significant finding.
Analog energy scale rated by participant 4 times per day for 2 weeks.
Prospective Associations of Mood and Energy on Subsequent Motor Activity
Table 2 presents the results of prospective analyses that evaluated the associations of subjective mood and energy with subsequent motor activity. Greater subjective energy (β = 0.176; P = .03) but not mood (β = –0.099; P = .23) level was associated with a subsequent increase in activity. Activity levels did not differ substantially by mood disorder subtype, but they were negatively associated with age; BMI; and, in the models with energy as an outcome, previous night sleep duration and weekday status. There was a trend for an interaction between mood and energy levels and activity in the subsequent period among those with bipolar I disorder, who exhibited a greater decrease in activity after increases in sad mood (β = –0.382; P = .07) and a greater increase in activity after increases in energy level (β = 0.360; P = .056).
Table 2. Lagged Associations Between Mood (Top) and Energy (Bottom) on Motor Activity.
| Category | Estimate | P Value |
|---|---|---|
| Outcome: Motor Activityta | ||
| Moodt-1b | –0.099 | .23 |
| Mood disorder subtype | ||
| Bipolar I | −0.397 | .28 |
| Bipolar II | 0.383 | .28 |
| Major depression | −0.017 | .95 |
| Interactions | ||
| Mood t-1 × bipolar I | −0.382 | .07 |
| Mood t-1 × bipolar II | −0.019 | .91 |
| Mood t-1 × major depression | −0.151 | .33 |
| Model covariates | ||
| Age | −0.041 | <.001c |
| Sex (F vs M) | 0.292 | .29 |
| Body mass index | −0.063 | <.001c |
| Activityt-1 | 0.416 | <.001c |
| Sleep duration, h | −0.131 | .06 |
| Weekday | −0.126 | .25 |
| Outcome: Motor Activityta | ||
| Energyt-1d | 0.176 | .03c |
| Mood disorder subtype | ||
| Bipolar I | −0.295 | .43 |
| Bipolar II | 0.328 | .35 |
| Major depression | 0.021 | .94 |
| Interactions | ||
| Energy t-1 × bipolar I | 0.360 | .056 |
| Energy t-1 × bipolar II | −0.148 | .49 |
| Energy t-1 × major depression | 0.021 | .87 |
| Model covariates | ||
| Age | −0.041 | <.001c |
| Sex (F vs M) | 0.366 | .19 |
| Body mass index | −0.066 | <.001c |
| Activityt-1 | 0.413 | <.001c |
| Sleep duration, h | −0.154 | .04c |
| Weekday | −0.219 | .04c |
Abbreviations: F, female; M, male; t, period; t-1, same domain in previous period (Granger model).
Mean counts per minute for each period.
Analog mood scale rated by participant 4 times per day for 2 weeks.
Denotes statistically significant finding.
Analog energy scale rated by participant 4 times per day for 2 weeks.
Increased activity, but not energy or mood, was associated with less sleep on the subsequent evening (data not shown). Similar to other domains, an interaction was observed between bipolar I disorder and sad mood level and subsequent sleep duration: Higher sad mood level was associated with increased sleep duration in those with bipolar I disorder but decreased sleep duration in controls.
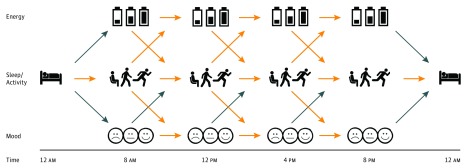
Directional Associations Among Sleep, Energy, Activity, and Mood
The Figure summarizes the directional associations of the time-lagged estimates of energy, activity, mood, and sleep over a 24-hour period in the total sample, based on the analyses presented in Tables 1 and 2. First, strong associations were observed within each domain (energy, activity, mood) over the course of the day. Second, cross-domain, bidirectional associations were found between energy level (β = 0.027; P = .03) and motor activity (β = 0.176; P = .03) as well as between sleep duration (β = –0.154; P = .04) and motor activity (β = –0.027; P = .04). Third, a unidirectional association was seen between motor activity and subsequent changes in mood (β = –0.018; P = .04), but mood levels were not associated with either subsequent activity or sleep level. Increased sleep duration on the previous night was associated with decreased activity on the next day, and decreased activity during the day were associated with increased sleep duration on the next evening. No direct associations were observed between mood or energy level and sleep duration on the next evening or the converse.
Figure. Summary of Within- and Across-Domain Associations of Subjective Mood and Energy, Motor Activity, and Sleep Duration.
Subjective energy and mood were assessed by ecologic momentary sampling and motor activity, and sleep duration was assessed by actigraphy across 2 weeks. Yellow (thicker) arrows indicate statistically significant associations; blue arrows indicate nonsignificant associations.
Discussion
Using mobile monitoring (actigraphy and EMA devices) and traditional clinical methods, we examined the highly dynamic interplay of multiple brain-body systems involved in the homeostatic regulation of human energy, mood, motor activity, and sleep. Results revealed a unidirectional association of motor activity with mood and bidirectional association of motor activity with subjective energy and sleep duration. Findings regarding the central role of motor activity patterns in mood regulation and the salience of subjective energy as a primary factor in motor activity suggest that motor activity may be a more malleable behavioral target of intervention than mood. Our application of fragmentation analysis, a novel statistical technique, to a study of the stability of these domains revealed greater instability of energy and attention, but not mood, in people with bipolar I disorder compared with controls.51 Greater cross-domain reactivity in bipolar I disorder further implicates the lack of central coordination of the network of motor activity, sleep, mood, and energy rather than the dysregulation of any single domain. Failure to consider changes in perturbations of different systems within these networks that drive or maintain set points of equilibrium may actually lead to greater resistance to change in related systems.52 The lack of integration among weight,53 sleep,54 and mood disorders55 may help explain the lack of enduring effectiveness of most intervention programs, which generally focus on only 1 of these domains.
The unidirectional associations of motor activity with depressed mood suggest that novel pharmacologic, physical, and behavioral therapeutic approaches focused on increasing energy and activity (eg, norepinephrine bitartrate, hypocretin/orexin, dopaminergic systems as targets) may be more effective than current treatments that target mood elevation or stabilization in bipolar disorder and major depressive disorder. The success of monoamine oxidase inhibitors in treating low energy in the atypical subtype of depression, which is often associated with bipolar disorder, may be attributable to their stimulating effects on energy and activity rather than mood.56 In addition, consideration of intrinsic rhythms in the timing of interventions,35,57 such as pharmacologic (eg, melatonin-based interventions)58 and/or behavioral interventions designed to enhance circadian rhythmicity,59,60 may be more effective than interventions in one of these domains alone.55,61
Our findings of the central role of motor activity patterns,23,30 the salience of subjective energy as a primary disturbance in motor activity,62 and the increased cross-domain reactivity across regulatory systems in bipolar I disorder also provide a model for translational research. More insight has emerged into the molecular biologic mechanisms underlying rhythms of sleep, activity, and eating63 as well as the role of circadian regulation of human physiologic systems57,64,65,66 and diseases.64,67,68 Basic science research could, therefore, examine whether disturbances in the coordination of hypothalamic regulatory systems, such as regulatory hypocretinergic systems and their catecholaminergic modulation,69,70 may underlie the increased cross-system reactivity observed in people with bipolar I disorder in this study. Greater understanding of the directions and mechanisms for these associations could explain how motor activity; sleep; eating; mood; cognition; and their underlying neural, physiologic, and molecular processes affect energy, interact in more complex networks, and help identify targets for intervention.
Our application of mobile monitoring in a community-based sample with a broad age range illustrates the feasibility of real-time in vivo active and passive assessment techniques.10,71 The joint application of passive data from actigraphy and active responses from EMA to improve the characterization of mental disorders demonstrates the central role of subjective psychological states, such as energy and mood, in bipolar disorder.72 The use of community sampling with clinical enrichment in this investigation extends the approach in previous research, which has generally been restricted to clinical convenience sampling that reflects more severe cases and may not be representative of mood disorders in the general population. Another strength of the present study is its analytic approach: (1) it incorporates covariates, such as BMI, diurnal stationarity, and weekend vs weekday factors, that may have confounded previous analyses, and (2) it employs Granger causality in the context of multilevel models to examine directional cross-domain associations.
Limitations
This study has limitations. First, we initially used 2-week cross-sectional measures of the key study domains. We are now repeating these assessments over longer periods and multiple times per year to study the generalizability of these findings over time. Second, we used actigraphy-based sleep assessment, which is only an index of sleep duration. However, our methods do conform with recommendations for actigraphy procedures recommended by the Society of Behavioral Sleep Medicine.11 Third, we analyzed only a subset of domains involved in these complex homeostatic networks and did not include measures of eating, stress, light, or other extrinsic factors in the core domains evaluated in this study. Future research into these networks could be enhanced by the inclusion of biologic correlates of the daily measures and the use of newer devices that measure light; temperature; and other metabolic correlates of motor activity, sleep, and mood.73 Light exposure is particularly critical because of its association with sleep, mood, and daily rhythms documented in basic science74 and because of the advantages of light treatment for humans shown in early pioneering studies75,76,77,78,79 and more recent applications.80,81 Moreover, low levels of light exposure during early childhood have even been postulated as a potential risk factor for the development of bipolar disorder.82
The simultaneous study of fluctuations in multiple systems that mimic real-life homeostatic regulation will require larger samples than can be collected at any site. For this reason, we have established a collaborative international consortium, the Motor Activity Research Consortium for Health (mMARCH),30 to enhance the ability to examine the generalizability of the present findings (with respect to state vs trait, sex differences, subgroups of mood disorders, and geographic and seasonal variations) and to extend this work to other mental and general health conditions. We are now comparing these earlier data with more recent data from other devices for actigraphy (GENEActiv, www.activinsights.com) and smartphones for EMA on a larger number of participants across collaborating sites.
Conclusions
The cross-domain reactivity in bipolar disorder highlights the importance of identifying potential mechanisms for the lack of synchrony across specific domains as well as the need for tracking multiple regulatory systems in identifying therapeutic targets. The application of real-world mobile technology to track human behavior and physiologic function in real time, coupled with advances in circadian medicine83 and molecular biologic systems research,63 provides unprecedented opportunities for increasing our understanding of the regulation of the core features of mood and other disorders, allowing us to gain insights into their underlying biologic, genetic, and environmental mechanisms and to define novel targets for intervention. Our findings also underscore the importance of both objective and subjective data that provide complementary information needed for fully characterizing these complex systems.
References
- 1.Hillman CH, Erickson KI, Kramer AF. Be smart, exercise your heart: exercise effects on brain and cognition. Nat Rev Neurosci. 2008;9(1):58-65. doi: 10.1038/nrn2298 [DOI] [PubMed] [Google Scholar]
- 2.O’Donoghue G, Perchoux C, Mensah K, et al. ; DEDIPAC Consortium . A systematic review of correlates of sedentary behaviour in adults aged 18-65 years: a socio-ecological approach. BMC Public Health. 2016;16(1):163. doi: 10.1186/s12889-016-2841-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hamilton MT, Hamilton DG, Zderic TW. Sedentary behavior as a mediator of type 2 diabetes. Med Sport Sci. 2014;60:11-26. doi: 10.1159/000357332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Myers J, McAuley P, Lavie CJ, Despres JP, Arena R, Kokkinos P. Physical activity and cardiorespiratory fitness as major markers of cardiovascular risk: their independent and interwoven importance to health status. Prog Cardiovasc Dis. 2015;57(4):306-314. doi: 10.1016/j.pcad.2014.09.011 [DOI] [PubMed] [Google Scholar]
- 5.Moore SC, Lee IM, Weiderpass E, et al. Association of leisure-time physical activity with risk of 26 types of cancer in 1.44 million adults. JAMA Intern Med. 2016;176(6):816-825. doi: 10.1001/jamainternmed.2016.1548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kyu HH, Bachman VF, Alexander LT, et al. Physical activity and risk of breast cancer, colon cancer, diabetes, ischemic heart disease, and ischemic stroke events: systematic review and dose-response meta-analysis for the Global Burden of Disease Study 2013. BMJ. 2016;354:i3857. doi: 10.1136/bmj.i3857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vancampfort D, Firth J, Schuch FB, et al. Sedentary behavior and physical activity levels in people with schizophrenia, bipolar disorder and major depressive disorder: a global systematic review and meta-analysis. World Psychiatry. 2017;16(3):308-315. doi: 10.1002/wps.20458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vancampfort D, Stubbs B, Herring MP, Hallgren M, Koyanagi A. Sedentary behavior and anxiety: association and influential factors among 42,469 community-dwelling adults in six low- and middle-income countries. Gen Hosp Psychiatry. 2018;50:26-32. doi: 10.1016/j.genhosppsych.2017.09.006 [DOI] [PubMed] [Google Scholar]
- 9.Rowlands AV, Fraysse F, Catt M, et al. Comparability of measured acceleration from accelerometry-based activity monitors. Med Sci Sports Exerc. 2015;47(1):201-210. doi: 10.1249/MSS.0000000000000394 [DOI] [PubMed] [Google Scholar]
- 10.Zinkhan M, Kantelhardt JW. Sleep assessment in large cohort studies with high-resolution accelerometers. Sleep Med Clin. 2016;11(4):469-488. doi: 10.1016/j.jsmc.2016.08.006 [DOI] [PubMed] [Google Scholar]
- 11.Ancoli-Israel S, Martin JL, Blackwell T, et al. The SBSM guide to actigraphy monitoring: clinical and research applications. Behav Sleep Med. 2015;13(suppl 1):S4-S38. doi: 10.1080/15402002.2015.1046356 [DOI] [PubMed] [Google Scholar]
- 12.Urbanek JK, Spira AP, Di J, Leroux A, Crainiceanu C, Zipunnikov V. Epidemiology of objectively measured bedtime and chronotype in US adolescents and adults: NHANES 2003-2006. Chronobiol Int. 2018;35(3):416-434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Matthews CE, George SM, Moore SC, et al. Amount of time spent in sedentary behaviors and cause-specific mortality in US adults. Am J Clin Nutr. 2012;95(2):437-445. doi: 10.3945/ajcn.111.019620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Doherty A, Jackson D, Hammerla N, et al. Large scale population assessment of physical activity using wrist worn accelerometers: The UK Biobank Study. PLoS One. 2017;12(2):e0169649. doi: 10.1371/journal.pone.0169649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ekelund U, Kolle E, Steene-Johannessen J, et al. Objectively measured sedentary time and physical activity and associations with body weight gain: does body weight determine a decline in moderate and vigorous intensity physical activity? Int J Obes (Lond). 2017;41(12):1769-1774. [DOI] [PubMed] [Google Scholar]
- 16.Althoff T, Sosič R, Hicks JL, King AC, Delp SL, Leskovec J. Large-scale physical activity data reveal worldwide activity inequality. Nature. 2017;547(7663):336-339. doi: 10.1038/nature23018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yerrakalva D, Cooper AJ, Westgate K, et al. The descriptive epidemiology of the diurnal profile of bouts and breaks in sedentary time in older English adults. Int J Epidemiol. 2017;46(6):1871-1881. doi: 10.1093/ije/dyx123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Varma VR, Dey D, Leroux A, et al. Re-evaluating the effect of age on physical activity over the lifespan. Prev Med. 2017;101:102-108. doi: 10.1016/j.ypmed.2017.05.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rockette-Wagner B, Storti KL, Edelstein S, et al. Measuring physical activity and sedentary behavior in youth with type 2 diabetes. Child Obes. 2017;13(1):72-77. doi: 10.1089/chi.2015.0151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Carson V, Ridgers ND, Howard BJ, et al. Light-intensity physical activity and cardiometabolic biomarkers in US adolescents. PLoS One. 2013;8(8):e71417. doi: 10.1371/journal.pone.0071417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cappuccio FP, Miller MA. Sleep and cardio-metabolic disease. Curr Cardiol Rep. 2017;19(11):110. doi: 10.1007/s11886-017-0916-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Burton C, McKinstry B, Szentagotai Tătar A, Serrano-Blanco A, Pagliari C, Wolters M. Activity monitoring in patients with depression: a systematic review. J Affect Disord. 2013;145(1):21-28. doi: 10.1016/j.jad.2012.07.001 [DOI] [PubMed] [Google Scholar]
- 23.De Crescenzo F, Economou A, Sharpley AL, Gormez A, Quested DJ. Actigraphic features of bipolar disorder: A systematic review and meta-analysis. Sleep Med Rev. 2017;33:58-69. [DOI] [PubMed] [Google Scholar]
- 24.Torous J, Firth J, Mueller N, Onnela JP, Baker JT. Methodology and reporting of mobile health and smartphone application studies for schizophrenia. Harv Rev Psychiatry. 2017;25(3):146-154. doi: 10.1097/HRP.0000000000000133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Faedda GL, Ohashi K, Hernandez M, et al. Actigraph measures discriminate pediatric bipolar disorder from attention-deficit/hyperactivity disorder and typically developing controls. J Child Psychol Psychiatry. 2016;57(6):706-716. doi: 10.1111/jcpp.12520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Slightam C, Petrowski K, Jamison AL, et al. Assessing sleep quality using self-report and actigraphy in PTSD. J Sleep Res. 2018;27(3):e12632. [DOI] [PubMed] [Google Scholar]
- 27.Jones SH, Hare DJ, Evershed K. Actigraphic assessment of circadian activity and sleep patterns in bipolar disorder. Bipolar Disord. 2005;7(2):176-186. doi: 10.1111/j.1399-5618.2005.00187.x [DOI] [PubMed] [Google Scholar]
- 28.Janney CA, Fagiolini A, Swartz HA, Jakicic JM, Holleman RG, Richardson CR. Are adults with bipolar disorder active? objectively measured physical activity and sedentary behavior using accelerometry. J Affect Disord. 2014;152-154:498-504. doi: 10.1016/j.jad.2013.09.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Krane-Gartiser K, Henriksen TE, Morken G, Vaaler A, Fasmer OB. Actigraphic assessment of motor activity in acutely admitted inpatients with bipolar disorder. PLoS One. 2014;9(2):e89574. doi: 10.1371/journal.pone.0089574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Scott J, Murray G, Henry C, et al. Activation in bipolar disorders: a systematic review. JAMA Psychiatry. 2017;74(2):189-196. doi: 10.1001/jamapsychiatry.2016.3459 [DOI] [PubMed] [Google Scholar]
- 31.Pagani L, St Clair PA, Teshiba TM, et al. Genetic contributions to circadian activity rhythm and sleep pattern phenotypes in pedigrees segregating for severe bipolar disorder. Proc Natl Acad Sci U S A. 2016;113(6):E754-E761. doi: 10.1073/pnas.1513525113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Carr O, Saunders KEA, Tsanas A, et al. Variability in phase and amplitude of diurnal rhythms is related to variation of mood in bipolar and borderline personality disorder. Sci Rep. 2018;8(1):1649. doi: 10.1038/s41598-018-19888-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Saper CB. The central circadian timing system. Curr Opin Neurobiol. 2013;23(5):747-751. doi: 10.1016/j.conb.2013.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Adamantidis A, de Lecea L. Sleep and metabolism: shared circuits, new connections. Trends Endocrinol Metab. 2008;19(10):362-370. doi: 10.1016/j.tem.2008.08.007 [DOI] [PubMed] [Google Scholar]
- 35.Bechtold DA, Loudon AS. Hypothalamic clocks and rhythms in feeding behaviour. Trends Neurosci. 2013;36(2):74-82. doi: 10.1016/j.tins.2012.12.007 [DOI] [PubMed] [Google Scholar]
- 36.Brown JA, Woodworth HL, Leinninger GM. To ingest or rest? specialized roles of lateral hypothalamic area neurons in coordinating energy balance. Front Syst Neurosci. 2015;9:9. doi: 10.3389/fnsys.2015.00009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Coppari R, Ichinose M, Lee CE, et al. The hypothalamic arcuate nucleus: a key site for mediating leptin’s effects on glucose homeostasis and locomotor activity. Cell Metab. 2005;1(1):63-72. doi: 10.1016/j.cmet.2004.12.004 [DOI] [PubMed] [Google Scholar]
- 38.Granholm E, Loh C, Swendsen J. Feasibility and validity of computerized ecological momentary assessment in schizophrenia. Schizophr Bull. 2008;34(3):507-514. doi: 10.1093/schbul/sbm113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ebner-Priemer UW, Trull TJ. Ecological momentary assessment of mood disorders and mood dysregulation. Psychol Assess. 2009;21(4):463-475. doi: 10.1037/a0017075 [DOI] [PubMed] [Google Scholar]
- 40.Johnson EI, Grondin O, Barrault M, et al. Computerized ambulatory monitoring in psychiatry: a multi-site collaborative study of acceptability, compliance, and reactivity. Int J Methods Psychiatr Res. 2009;18(1):48-57. doi: 10.1002/mpr.276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Husky MM, Gindre C, Mazure CM, et al. Computerized ambulatory monitoring in mood disorders: feasibility, compliance, and reactivity. Psychiatry Res. 2010;178(2):440-442. doi: 10.1016/j.psychres.2010.04.045 [DOI] [PubMed] [Google Scholar]
- 42.Preston KL, Kowalczyk WJ, Phillips KA, et al. Exacerbated craving in the presence of stress and drug cues in drug-dependent patients. Neuropsychopharmacology. 2018;43(4):859-867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kim J, Nakamura T, Kikuchi H, Sasaki T, Yamamoto Y. Co-variation of depressive mood and locomotor dynamics evaluated by ecological momentary assessment in healthy humans. PLoS One. 2013;8(9):e74979. doi: 10.1371/journal.pone.0074979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Miller MA, Rothenberger SD, Hasler BP, et al. Chronotype predicts positive affect rhythms measured by ecological momentary assessment. Chronobiol Int. 2015;32(3):376-384. doi: 10.3109/07420528.2014.983602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Merikangas KR, Cui L, Heaton L, et al. Independence of familial transmission of mania and depression: results of the NIMH family study of affective spectrum disorders. Mol Psychiatry. 2014;19(2):214-219. doi: 10.1038/mp.2013.116 [DOI] [PubMed] [Google Scholar]
- 46.Shou H, Cui L, Hickie I, et al. Dysregulation of objectively assessed 24-hour motor activity patterns as a potential marker for bipolar I disorder: results of a community-based family study. Transl Psychiatry. 2017;7(8):e1211. doi: 10.1038/tp.2017.136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lamers F, Swendsen J, Cui L, et al. Mood reactivity and affective dynamics in mood and anxiety disorders. J Abnorm Psychol. 2018;127(7):659-669. doi: 10.1037/abn0000378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cellini N, Buman MP, McDevitt EA, Ricker AA, Mednick SC. Direct comparison of two actigraphy devices with polysomnographically recorded naps in healthy young adults. Chronobiol Int. 2013;30(5):691-698. doi: 10.3109/07420528.2013.782312 [DOI] [PubMed] [Google Scholar]
- 49.Swendsen J. Anxiety, depression and their comorbidity: an experience sampling test of helplessness. Cognit Ther Res. 1997;21:97-114. doi: 10.1023/A:1021872410824 [DOI] [Google Scholar]
- 50.Swendsen J. The experience of anxious and depressed moods in daily life: an idiographic and cross-situational test of the Helplessness-Hopelessness Theory. J Pers Soc Psychol. 1998;74:1398-1408. doi: 10.1037/0022-3514.74.5.1398 [DOI] [Google Scholar]
- 51.Johns J, Swendsen J, Cui L, Di J, Zipunnikov V, Merikangas KR. Fragmentation as a novel measure of stability in normalized trajectories of mood and attention measured by ecological momentary assessment [accepted September 30, 2018]. Psychol Assess. [DOI] [PubMed] [Google Scholar]
- 52.Greenway FL. Physiological adaptations to weight loss and factors favouring weight regain. Int J Obes (Lond). 2015;39(8):1188-1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wu T, Gao X, Chen M, van Dam RM. Long-term effectiveness of diet-plus-exercise interventions vs diet-only interventions for weight loss: a meta-analysis. Obes Rev. 2009;10(3):313-323. doi: 10.1111/j.1467-789X.2008.00547.x [DOI] [PubMed] [Google Scholar]
- 54.Riemann D, Nissen C, Palagini L, Otte A, Perlis ML, Spiegelhalder K. The neurobiology, investigation, and treatment of chronic insomnia. Lancet Neurol. 2015;14(5):547-558. doi: 10.1016/S1474-4422(15)00021-6 [DOI] [PubMed] [Google Scholar]
- 55.Thomson D, Turner A, Lauder S, et al. A brief review of exercise, bipolar disorder, and mechanistic pathways. Front Psychol. 2015;6:147. doi: 10.3389/fpsyg.2015.00147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Stewart JW, Thase ME. Treating DSM-IV depression with atypical features. J Clin Psychiatry. 2007;68(4):e10. doi: 10.4088/JCP.0407e10 [DOI] [PubMed] [Google Scholar]
- 57.Baron KG, Reid KJ, Kim T, et al. Circadian timing and alignment in healthy adults: associations with BMI, body fat, caloric intake and physical activity. Int J Obes (Lond). 2017;41(2):203-209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hickie IB, Rogers NL. Novel melatonin-based therapies: potential advances in the treatment of major depression. Lancet. 2011;378(9791):621-631. doi: 10.1016/S0140-6736(11)60095-0 [DOI] [PubMed] [Google Scholar]
- 59.Frank E, Benabou M, Bentzley B, et al. Influencing circadian and sleep-wake regulation for prevention and intervention in mood and anxiety disorders: what makes a good homeostat? Ann N Y Acad Sci. 2014;1334:1-25. doi: 10.1111/nyas.12600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Goldstein TR, Fersch-Podrat R, Axelson DA, et al. Early intervention for adolescents at high risk for the development of bipolar disorder: pilot study of Interpersonal and Social Rhythm Therapy (IPSRT). Psychotherapy (Chic). 2014;51(1):180-189. doi: 10.1037/a0034396 [DOI] [PubMed] [Google Scholar]
- 61.Chalder M, Wiles NJ, Campbell J, et al. Facilitated physical activity as a treatment for depressed adults: randomised controlled trial. BMJ. 2012;344:e2758. doi: 10.1136/bmj.e2758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Johnson SL, Gershon A, Starov V. Is energy a stronger indicator of mood for those with bipolar disorder compared to those without bipolar disorder? Psychiatry Res. 2015;230(1):1-4. doi: 10.1016/j.psychres.2015.06.016 [DOI] [PubMed] [Google Scholar]
- 63.Takahashi JS. Transcriptional architecture of the mammalian circadian clock. Nat Rev Genet. 2017;18(3):164-179. doi: 10.1038/nrg.2016.150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Musiek ES, Holtzman DM. Mechanisms linking circadian clocks, sleep, and neurodegeneration. Science. 2016;354(6315):1004-1008. doi: 10.1126/science.aah4968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Geiger SS, Fagundes CT, Siegel RM. Chrono-immunology: progress and challenges in understanding links between the circadian and immune systems. Immunology. 2015;146(3):349-358. doi: 10.1111/imm.12525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Panda S. Circadian physiology of metabolism. Science. 2016;354(6315):1008-1015. doi: 10.1126/science.aah4967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Arble DM, Bass J, Behn CD, et al. Impact of sleep and circadian disruption on energy balance and diabetes: a summary of workshop discussions. Sleep. 2015;38(12):1849-1860. doi: 10.5665/sleep.5226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Landgraf D, McCarthy MJ, Welsh DK. Circadian clock and stress interactions in the molecular biology of psychiatric disorders. Curr Psychiatry Rep. 2014;16(10):483. doi: 10.1007/s11920-014-0483-7 [DOI] [PubMed] [Google Scholar]
- 69.Elbaz I, Yelin-Bekerman L, Nicenboim J, Vatine G, Appelbaum L. Genetic ablation of hypocretin neurons alters behavioral state transitions in zebrafish. J Neurosci. 2012;32(37):12961-12972. doi: 10.1523/JNEUROSCI.1284-12.2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Singh C, Oikonomou G, Prober DA. Norepinephrine is required to promote wakefulness and for hypocretin-induced arousal in zebrafish. Elife. 2015;4:e07000. doi: 10.7554/eLife.07000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hawkins MS, Storti KL, Richardson CR, et al. Objectively measured physical activity of USA adults by sex, age, and racial/ethnic groups: a cross-sectional study. Int J Behav Nutr Phys Act. 2009;6:31. doi: 10.1186/1479-5868-6-31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Insel TR. Digital phenotyping: technology for a new science of behavior. JAMA. 2017;318(13):1215-1216. doi: 10.1001/jama.2017.11295 [DOI] [PubMed] [Google Scholar]
- 73.Gao W, Emaminejad S, Nyein HYY, et al. Fully integrated wearable sensor arrays for multiplexed in situ perspiration analysis. Nature. 2016;529(7587):509-514. doi: 10.1038/nature16521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.LeGates TA, Fernandez DC, Hattar S. Light as a central modulator of circadian rhythms, sleep and affect. Nat Rev Neurosci. 2014;15(7):443-454. doi: 10.1038/nrn3743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Lewy AJ, Wehr TA, Goodwin FK, Newsome DA, Markey SP. Light suppresses melatonin secretion in humans. Science. 1980;210(4475):1267-1269. doi: 10.1126/science.7434030 [DOI] [PubMed] [Google Scholar]
- 76.Wirz-Justice A. Light therapy for depression: present status, problems, and perspectives. Psychopathology. 1986;19(suppl 2):136-141. doi: 10.1159/000285145 [DOI] [PubMed] [Google Scholar]
- 77.Lewy AJ, Sack RL, Singer CM. Treating phase typed chronobiologic sleep and mood disorders using appropriately timed bright artificial light. Psychopharmacol Bull. 1985;21(3):368-372. [PubMed] [Google Scholar]
- 78.Dijk DJ, Beersma DG, Daan S, Lewy AJ. Bright morning light advances the human circadian system without affecting NREM sleep homeostasis. Am J Physiol. 1989;256(1 Pt 2):R106-R111. [DOI] [PubMed] [Google Scholar]
- 79.Kräuchi K, Wirz-Justice A, Graw P. High intake of sweets late in the day predicts a rapid and persistent response to light therapy in winter depression. Psychiatry Res. 1993;46(2):107-117. doi: 10.1016/0165-1781(93)90013-7 [DOI] [PubMed] [Google Scholar]
- 80.Sit DK, McGowan J, Wiltrout C, et al. Adjunctive bright light therapy for bipolar depression: a randomized double-blind placebo-controlled trial. Am J Psychiatry. 2018;175(2):131-139. doi: 10.1176/appi.ajp.2017.16101200 [DOI] [PubMed] [Google Scholar]
- 81.Wirz-Justice A, Bader A, Frisch U, et al. A randomized, double-blind, placebo-controlled study of light therapy for antepartum depression. J Clin Psychiatry. 2011;72(7):986-993. doi: 10.4088/JCP.10m06188blu [DOI] [PubMed] [Google Scholar]
- 82.Bauer M, Glenn T, Alda M, et al. Influence of light exposure during early life on the age of onset of bipolar disorder. J Psychiatr Res. 2015;64:1-8. doi: 10.1016/j.jpsychires.2015.03.013 [DOI] [PubMed] [Google Scholar]
- 83.Turek FW. Circadian clocks: not your grandfather’s clock. Science. 2016;354(6315):992-993. doi: 10.1126/science.aal2613 [DOI] [PubMed] [Google Scholar]