Key Points
Question
How has the percentage of US adults using outpatient mental health care changed in recent years?
Findings
Among 139 862 adult participants from Medical Expenditure Panel Surveys, the percentage of US adults receiving outpatient mental health services increased from 19.08% (2004-2005) to 23.00% (2014-2015). During this period, there was an increase in outpatient mental health service use among adults with serious psychological distress from 54.17% to 68.40% and among adults with less serious or no psychological distress from 17.26% to 21.08%.
Meaning
Analysis of a recent national increase in outpatient mental health service use shows that adults with less serious psychological distress accounted for most of the absolute increase, while those with serious psychological distress experienced a larger relative increase in service use.
This survey study characterizes US national trends in serious psychological distress and trends in outpatient mental health service use by adults with and without serious psychological distress.
Abstract
Importance
Reports of a recent increase in US outpatient mental health care raise questions about whether it has been driven by rising rates of psychological distress and whether mental health treatment has become either more or less focused on people with higher levels of distress.
Objective
To characterize national trends in serious psychological distress and trends in outpatient mental health service use by adults with and without serious psychological distress.
Design, Setting, and Participants
The 2004-2005, 2009-2010, and 2014-2015 Medical Expenditure Panel Surveys (MEPS) were nationally representative surveys taken in US households. The analysis was limited to participants 18 years or older. Dates of this analysis were February 2018 to April 2018.
Main Outcomes and Measures
Annual national trends in the percentages of adults with serious psychological distress (Kessler 6 scale score ≥13), outpatient mental health service use (outpatient visit with a mental disorder diagnosis, psychotherapy visit, or psychotropic medication), and type of psychotropic medication use (antidepressants, anxiolytics/sedatives, antipsychotics, mood stabilizers, and stimulants). Age- and sex-adjusted odds ratios of the associations of survey period with the odds of serious psychological distress, outpatient mental health service use, and outpatient mental health service use were stratified by level of psychological distress.
Results
The analysis involved 139 862 adult participants from the 2004-2005, 2009-2010, and 2014-2015 MEPS, including 51.67% women, 48.33% men, 67.11% white adults, and 32.89% nonwhite adults, with an overall mean (SE) age of 46.41 (0.14) years. Serious psychological distress declined overall from 4.82% (2004-2005) to 3.71% (2014-2015), including significant declines among young (3.94% to 3.07%), middle-aged (5.52% to 4.36%), and older adults (5.24% to 3.79%); men (3.94% to 3.09%) and women (5.64% to 4.29%); and major racial/ethnic groups (white, 4.52% to 3.82%; African American, 5.12% to 3.64%; Hispanic, 6.03% to 3.55%; and other, 5.22% to 3.26%). Overall, the percentage of adults receiving any outpatient mental health service increased from 19.08% (2004-2005) to 23.00% (2014-2015) (adjusted odds ratio, 1.25; 95% CI, 1.17-1.34). Although the proportionate increase in outpatient mental health service use for adults with serious psychological distress (54.17% to 68.40%) was larger than that for adults with less serious or no psychological distress (17.26% to 21.08%), the absolute increase in outpatient mental health service use was almost completely the result of growth in outpatient mental health service use by individuals with less serious or no psychological distress.
Conclusions and Relevance
The recent increase in outpatient mental health service use occurred during a period of decline in serious psychological distress. Adults with less serious psychological distress accounted for most of the absolute increase in outpatient mental health service use, while adults with serious psychological distress experienced a greater relative increase in outpatient mental health service use.
Introduction
Over the past several years, there have been indications of an increase in the annual percentage of US adults who receive outpatient mental health care. According to the National Survey on Drug Use and Health,1 the percentage of adults using specialty outpatient mental health care increased from 5.0% in 2008-2009 to 5.7% in 2014-2015. Results from the National Health and Nutrition Surveys reveal that the percentage of Americans using antidepressants in the past 30 days increased from 6.4% (2000-2002) to 10.7% (2011-2014), while the corresponding percentage using anxiolytics/hypnotics increased from 3.3% to 5.3%.2 Rising national rates of suicide,3 opioid misuse,4 and opioid-related deaths5 further suggest increasing psychological distress. However, it is not known whether or to what extent an increase in mental health treatment has occurred in response to rising rates of psychological distress.
Concern exists over the extent to which use of mental health services aligns with need for treatment.6 Although the likelihood of receiving mental health treatment is directly associated with clinical severity,7 many adults with serious conditions do not receive treatment, while a substantial proportion of mental health services are provided to individuals with lower levels of distress. Six population surveys fielded in developed countries between 2000 and 2003 reported that approximately one-third to one-half of adults with serious conditions, including 47.7% of those in the United States, received no mental health treatment during the past year.8 At the same time, approximately one-half of adults who received mental health care either had no mental disorders or had mild conditions.8 However, a close examination of US adults who received mental health treatment without a current mental diagnosis revealed that most had either a lifetime history of a mental disorder or other indicators of possible treatment need, such as a recent major stressful life event or a subthreshold mental health condition.9
We examined recent trends in serious psychological distress and trends in outpatient mental health service use by US adults. The trends in use of services were stratified by level of psychological distress to assess how adults with more or less serious distress have reacted to changing patterns of mental health treatment.
Methods
Sources of Data
Data were analyzed from the household component of the 2004-2005, 2009-2010, and 2014-2015 Medical Expenditure Panel Surveys (MEPS) conducted by the Agency for Healthcare Research and Quality. MEPS included a series of 3 in-person interviews with nationally representative adults during each study year. Signed permission forms are required before the first interview. Respondents were asked to record medical events as they occurred in a calendar/diary that was reviewed in person during each interview. Written permission was obtained from selected survey participants to contact medical providers they mentioned during the survey to verify service use. Following Agency for Healthcare Research and Quality recommendations, the 2 annual samples were concatenated to increase sample size.7 Technical information concerning the fielding and nonresponse adjustment of MEPS is provided elsewhere.10,11,12 MEPS oversampled African American, Hispanic, and Asian individuals as well as persons with predicted low income. These analyses, which relied exclusively on deidentified data, were exempted from human participants review by the Institutional Review Board of the New York State Psychiatric Institute.
Study Samples
The analytic sample included all individuals 18 years or older. A common variance structure that treats each response as independent permitted pooling of responses into 3 cross-sections (2004-2005, 2009-2010, and 2014-2015).13 The number of study participants (n = 139 862) included 44 984 (2004-2005), 46 835 (2009-2010), and 48 043 (2014-2015). Among 139 862 participants, 51.67% were women, 48.33% were men, 67.11% were white adults, and 32.89% were nonwhite adults, with an overall mean (SE) age of 46.41 (0.14) years.
Psychological Distress
Psychological distress was measured with the Kessler 6 scale (K-6). Respondents were queried concerning the frequency during the past 30 days of feeling so sad that nothing could cheer them up, nervous, restless or fidgety, hopeless, that everything was an effort, and worthless (all, most, some, a little, or none of the time). Item responses were scored from 0 to 4, with a cumulative score of 13 or higher defining serious psychological distress.14,15 At this cut point, the K-6 has a mean (SE) classification accuracy of 0.92 (0.02) in identifying adults with severe mental illnesses.16 According to receiver operating characteristic curve analyses, the 0.86 area under the curve (AUC) of the K-6 is considerably higher than that of the World Health Organization Composite International Diagnostic Interview Short-Form scales (AUC, 0.76).17 In a separate analysis, the AUC of the K-6 (0.89; 95% CI, 0.88-0.90) was significantly higher than that of the General Health Questionnaire 12 (0.80; 95% CI, 0.78-0.82).18 Serious psychological distress measured with the K-6 is also strongly associated with use of outpatient, inpatient, and emergency health services.19
Outpatient Mental Health Service Use
Outpatient mental health service use was defined by an outpatient visit with a mental disorder diagnosis (International Classification of Diseases, Ninth Revision codes 290-319), use of psychotherapy, or use of psychotropic medications. In some analyses, annual mental health service use was partitioned into 3 mutually exclusive hierarchical groups of treatment from (1) psychiatrists, (2) other mental health professionals (including psychologists and social workers but not psychiatrists), and (3) general medical professionals (only) (including all other health professionals). MEPS asked respondents about the type of care provided during each outpatient visit using response categories that included psychotherapy or mental health counseling. One or more psychotherapy visits defined psychotherapy use. MEPS collected prescription drug use information directly from households on medications obtained by respondents. Psychotropic medications included antidepressants, anxiolytics/sedatives, antipsychotics, mood stabilizers (in the absence of seizure disorder), and stimulants. One or more prescriptions during the survey year defined medication use.
Other Characteristics
Age was considered as 18 to 39 years (younger adults), 40 to 59 years (middle-aged adults), or 60 years or older (older adults); sex and race/ethnicity (white or nonwhite) was as reported by the household respondent. In some analyses, race/ethnicity was defined as white, African American, Hispanic, or other.
Statistical Analysis
For each survey period, the percentage of adults with serious psychological distress was estimated overall and stratified by demographic and outpatient mental health service group. Age- and sex-adjusted logistic regressions tested for change in the odds of people having serious psychological distress over the study period from 2004-2005 to 2014-2015 (ie, period association).
Corresponding age- and sex-adjusted models assessed the period association for outpatient mental health service use. Results are presented as odds ratios (ORs) with 95% CIs. P values for interaction were calculated to test whether changes in outpatient mental health service use over time differed across demographic and psychological distress severity strata. These analyses were performed with the total sample and separately for each psychological distress severity stratum. Similar analyses were performed for outpatient mental health service use provided by psychiatrists, other mental health professionals, and general medical professionals (only). Two-sided α was set at .05.
All statistical analyses were performed with a software program (SAS, version 9.4; SAS Institute Inc); PROC SURVEYFREQ and SURVEYLOGISTIC (SAS Institute Inc) were used to accommodate the complex sample design and weighting of observations.
Results
Serious Psychological Distress
The percentage of adults with serious psychological distress (K-6 score, ≥13) was almost constant from 4.82% (2004-2005) to 4.93% (2009-2010) before declining to 3.71% (2014-2015) (Table 1). Between 2004-2005 and 2014-2015, significant declines in the odds of serious psychological distress were observed for each age group, men, women, and each racial/ethnic group. Among adults who used any outpatient mental health service, the percentage with serious psychological distress also declined although proportionately less than the decline among adults who did not use outpatient mental health services. During all 3 periods, the odds of serious psychological distress were greater for women than for men and for middle-aged and older adults than for younger adults (eTable 1 in the Supplement).
Table 1. Trends in the Percentage of Adults With Serious Psychological Distressa.
| Variable | Serious Psychological Distress, % | Period Association, Adjusted OR (95% CI) | ||
|---|---|---|---|---|
| 2004-2005 (n = 44 984) | 2009-2010 (n = 46 835) | 2014-2015 (n = 48 043) | ||
| Total | 4.82 | 4.93 | 3.71 | 0.77 (0.70-0.84) |
| Age, y | ||||
| 18-39 | 3.94 | 4.07 | 3.07 | 0.78 (0.67-0.90) |
| 40-59 | 5.52 | 5.63 | 4.36 | 0.79 (0.69-0.90) |
| ≥60 | 5.24 | 5.30 | 3.79 | 0.71 (0.61-0.84) |
| Sex | ||||
| Male | 3.94 | 4.30 | 3.09 | 0.78 (0.68-0.89) |
| Female | 5.64 | 5.53 | 4.29 | 0.76 (0.68-0.85) |
| Race/ethnicity | ||||
| White | 4.52 | 4.87 | 3.82 | 0.85 (0.76-0.96) |
| African American | 5.12 | 5.30 | 3.64 | 0.71 (0.58-0.86) |
| Hispanic | 6.03 | 5.29 | 3.55 | 0.55 (0.46-0.65) |
| Other | 5.22 | 4.20 | 3.26 | 0.60 (0.43-0.83) |
| Any outpatient mental health service use | ||||
| Use | 13.71 | 14.23 | 11.11 | 0.80 (0.70-0.91) |
| No use | 2.73 | 2.56 | 1.52 | 0.57 (0.50-0.65) |
| Any psychotherapy use | ||||
| Use | 20.75 | 23.24 | 18.61 | 0.89 (0.73-1.09) |
| No use | 4.04 | 4.06 | 2.95 | 0.72 (0.66-0.80) |
| Any psychotropic medication use | ||||
| Use | 14.30 | 14.72 | 11.46 | 0.79 (0.69-0.90) |
| No use | 2.89 | 2.70 | 1.70 | 0.60 (0.53-0.68) |
Abbreviation: OR, odds ratio.
Data are from the Medical Expenditure Panel Surveys. Adjusted ORs of regressions compare stratified percentages with serious psychological distress in 2014-2015 vs 2004-2005 (reference). Serious psychological distress is based on a Kessler 6 scale score of 13 or higher. The regressions controlled for age and sex except for analyses by age, which controlled only for sex, and analyses by sex, which controlled only for age.
Outpatient Mental Health Service Use
The percentage of adults with any outpatient mental health service use increased between 2004-2005 and 2014-2015. Significant increases were evident among younger, middle-aged, and older adults; men and women; and white and nonwhite adults (Table 2). The relative increase in any outpatient mental health service use was greater among younger adults than among middle-aged adults. Compared with adults with less serious or no psychological distress, those with serious psychological distress experienced a greater relative increase in any outpatient mental health service use, with more than two-thirds (68.40%) accessing services in 2014-2015 (Table 2). In post hoc analyses, the proportionate increase in any outpatient mental health service use from 2004-2005 to 2014-2015 was greater for adults with less serious psychological distress (K-6 scale score, 1-12) (21.40% to 28.57%; OR, 1.46; 95% CI, 1.36-1.57) than for adults with no psychological distress (K-6 scale score, 0) (9.72% to 11.97%; OR, 1.24; 95% CI, 1.11-1.38) (interaction P = .006) (eTable 2 in the Supplement).
Table 2. Trends in Any Outpatient Mental Health Service Use by Adultsa.
| Variable | Any Outpatient Mental Health Service Use, % | Period Association, OR (95% CI)b | P Value for Interactionc | ||
|---|---|---|---|---|---|
| 2004-2005 | 2009-2010 | 2014-2015 | |||
| Total | 19.08 | 20.44 | 23.00 | 1.25 (1.17-1.34) | NA |
| Age, y | |||||
| 18-39 | 12.42 | 14.03 | 15.75 | 1.32 (1.18-1.49) | 1 [Reference] |
| 40-59 | 22.26 | 22.74 | 24.23 | 1.12 (1.02-1.23) | <.001 |
| ≥60 | 25.74 | 27.32 | 31.67 | 1.36 (1.24-1.50) | .05 |
| Sex | |||||
| Male | 13.40 | 15.11 | 17.36 | 1.32 (1.21-1.45) | .08 |
| Female | 24.39 | 25.46 | 28.27 | 1.21 (1.12-1.30) | |
| Race/ethnicity | |||||
| White | 22.56 | 24.46 | 28.34 | 1.35 (1.26-1.45) | .07 |
| Nonwhite | 11.16 | 11.92 | 13.47 | 1.20 (1.08-1.32) | |
| Psychological distress | |||||
| Serious psychological distress | 54.17 | 58.63 | 68.40 | 1.84 (1.53-2.23) | <.001 |
| Less serious or no psychological distress | 17.26 | 18.34 | 21.08 | 1.26 (1.18-1.35) | |
| Less Serious or No Psychological Distress | |||||
| Age, y | |||||
| 18-39 | 11.34 | 12.51 | 14.33 | 1.31 (1.16-1.48) | 1 [Reference] |
| 40-59 | 19.89 | 20.31 | 21.89 | 1.13 (1.03-1.25) | .002 |
| ≥60 | 23.84 | 25.03 | 29.92 | 1.39 (1.26-1.54) | .03 |
| Sex | |||||
| Male | 11.97 | 13.26 | 15.75 | 1.34 (1.22-1.48) | .04 |
| Female | 22.30 | 23.20 | 26.12 | 1.21 (1.12-1.31) | |
| Race/ethnicity | |||||
| White | 20.66 | 22.22 | 26.25 | 1.36 (1.26-1.46) | .34 |
| Nonwhite | 9.31 | 9.97 | 11.79 | 1.26 (1.13-1.39) | |
| Serious Psychological Distress | |||||
| Age, y | |||||
| 18-39 | 39.99 | 48.58 | 61.34 | 2.39 (1.71-3.34) | 1 [Reference] |
| 40-59 | 62.33 | 62.27 | 71.84 | 1.46 (1.13-1.87) | .03 |
| ≥60 | 59.11 | 65.41 | 71.54 | 1.85 (1.35-2.52) | .94 |
| Sex | |||||
| Male | 47.95 | 52.30 | 60.46 | 1.64 (1.26-2.15) | .29 |
| Female | 58.24 | 63.28 | 73.75 | 1.99 (1.58-2.52) | |
| Race/ethnicity | |||||
| White | 60.82 | 64.98 | 75.31 | 1.98 (1.55-2.53) | .38 |
| Nonwhite | 41.60 | 45.49 | 54.85 | 1.71 (1.35-2.17) | |
Abbreviations: NA, not applicable; OR, odds ratio.
Data are from the Medical Expenditure Panel Surveys and are presented as annualized percentages. Serious psychological distress is based on a Kessler 6 scale score of 13 or higher.
Period associations represent the age- and sex-adjusted OR of any outpatient mental health service use in 2014-2015 vs 2004-2005 (reference).
P values for interaction test whether changes in any outpatient mental health service use differed over time across demographic or psychological distress severity strata.
Among adults with less serious or no psychological distress, the relative increase in any outpatient mental health service use was greatest for older adults, followed by younger adults and then middle-aged adults and was greater for men than for women. Among adults with serious psychological distress, the relative increase was greater for younger adults than for middle-aged adults (Table 2).
Between 2004-2005 and 2014-2015, the estimated annual number of US adults who received any outpatient mental health care increased from 41.82 (95% CI, 38.97-44.68) million to 56.00 (95% CI, 52.77-59.20) million (eTable 3 in the Supplement). This absolute increase was largely attributable to the increase in treatment of adults with less serious or no psychological distress from 35.17 (95% CI, 32.64-37.71) million in 2004-2005 to 47.69 (95% CI, 44.80-50.61) million in 2014-2015. Within all 3 periods, the percentages of adults with any outpatient mental health service use were higher for middle-aged or older adults than for younger adults, for women than for men, and for white adults than for nonwhite adults (eTable 4 in the Supplement).
Psychotherapy
Among all adults, use of psychotherapy remained little changed between 2004-2005 (4.62%), 2009-2010 (4.56%), and 2014-2015 (4.87%) (Table 3). However, psychotherapy use increased among adults with serious psychological distress but not among adults with less serious or no psychological distress (Table 3). In each period, psychotherapy was used significantly more frequently by younger adults than by older adults, by women than by men, and by white adults than nonwhite adults (eTable 4 in the Supplement).
Table 3. Trends in Type of Psychotropic Medication Use Classes and Psychotherapy Use by Adultsa.
| Variable | Specific Mental Health Service Use, % | Period Association, OR (95% CI)b | P Value for Interactionc | ||
|---|---|---|---|---|---|
| 2004-2005 | 2009-2010 | 2014-2015 | |||
| Any Psychotropic Medication Use | 16.96 | 18.64 | 20.75 | 1.26 (1.18-1.35) | NA |
| Adults with serious psychological distress | 50.16 | 55.35 | 63.57 | 1.76 (1.46-2.11) | <.001 |
| Adults with less serious or no psychological distress | 15.22 | 16.64 | 18.91 | 1.27 (1.19-1.37) | |
| Antidepressants | 11.81 | 12.45 | 13.73 | 1.18 (1.09-1.28) | NA |
| Adults with serious psychological distress | 38.38 | 42.86 | 47.11 | 1.45 (1.21-1.75) | .06 |
| Adults with less serious or no psychological distress | 10.45 | 10.86 | 12.36 | 1.19 (1.10-1.30) | |
| Anxiolytics/Sedatives | 6.10 | 7.13 | 7.68 | 1.24 (1.15-1.34) | NA |
| Adults with serious psychological distress | 23.09 | 27.06 | 33.51 | 1.70 (1.37-2.12) | .01 |
| Adults with less serious or no psychological distress | 5.17 | 6.02 | 6.61 | 1.25 (1.14-1.36) | |
| Antipsychotics | 1.30 | 1.72 | 1.68 | 1.28 (1.09-1.50) | NA |
| Adults with serious psychological distress | 7.99 | 10.91 | 11.74 | 1.55 (1.20-2.01) | .30 |
| Adults less serious or no psychological distress | 0.95 | 1.23 | 1.25 | 1.29 (1.07-1.56) | |
| Mood Stabilizers | 2.61 | 3.42 | 4.81 | 1.86 (1.66-2.09) | NA |
| Adults with serious psychological distress | 11.94 | 15.19 | 21.49 | 2.05 (1.61-2.61) | .73 |
| Adults with less serious or no psychological distress | 2.13 | 2.76 | 4.09 | 1.94 (1.71-2.20) | |
| Stimulants | 1.55 | 1.87 | 2.29 | 1.48 (1.25-1.76) | NA |
| Adults with serious psychological distress | 4.40 | 5.80 | 7.66 | 1.82 (1.28-2.58) | .31 |
| Adults with less serious or no psychological distress | 1.41 | 1.66 | 2.06 | 1.47 (1.22-1.78) | |
| Any Psychotherapy Use | 4.62 | 4.56 | 4.87 | 1.08 (0.97-1.21) | NA |
| Adults with serious psychological distress | 20.00 | 21.43 | 24.37 | 1.33 (1.09-1.63) | .09 |
| Adults with less serious or no psychological distress | 3.87 | 3.67 | 4.11 | 1.09 (0.96-1.24) | |
Abbreviations: NA, not applicable; OR, odds ratio.
Data are from the Medical Expenditure Panel Surveys and are presented as percentages with any type of psychotropic medication use class. Serious psychological distress is based on a Kessler 6 scale score of 13 or higher.
Period associations represent the age- and sex-adjusted OR of the specific mental health service use in 2014-2015 vs 2004-2005 (reference).
P values for interaction test whether changes in any psychotropic medication use, antidepressants, anxiolytics/sedatives, antipsychotics, mood stabilizers, stimulants, and any psychotherapy use differed over time across psychological distress severity strata.
Psychotropic Medications
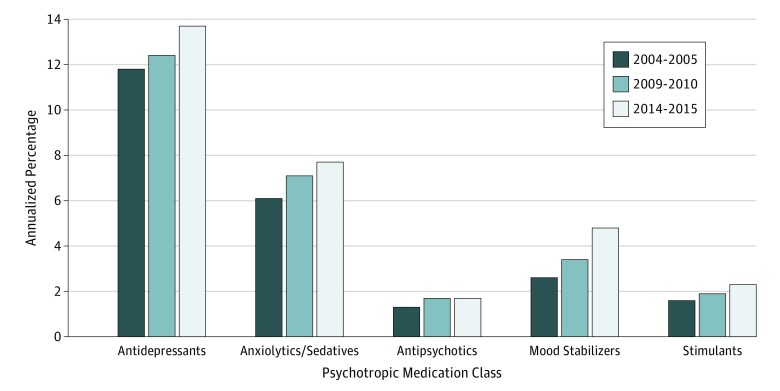
There were significant increases in use of psychotropic medications, including antidepressants, anxiolytics/sedatives, antipsychotics, mood stabilizers, and stimulants (Figure). These increases were observed among adults above and below the serious psychological distress threshold (Table 3). Compared with adults with less serious or no psychological distress, those with serious psychological distress experienced a greater relative increase in use of any psychotropic medication and anxiolytics/sedatives.
Figure. Trends in Use of Antidepressants, Anxiolytics/Sedatives, Antipsychotics, Mood Stabilizers, and Stimulants by Adults, United States.
Data are from the Medical Expenditure Panel Surveys and are presented as annualized percentages. The analysis is limited to persons 18 years or older.
Within each period, the odds of using any psychotropic medication were roughly 2 to 2.5 times greater for middle-aged adults and older adults than for younger adults, for women than for men, and for white adults than for nonwhite adults (eTable 4 in the Supplement). The odds of antidepressant use followed a similar pattern. The odds of anxiolytic/sedative use were markedly higher for older adults than for younger adults in 2004-2005 (4.35; 95% CI, 3.71-5.10), 2009-2010 (2.82; 95% CI, 2.44-3.27), and 2014-2015 (3.13; 95% CI, 2.71-3.62) (eTable 4 in the Supplement).
Service Providers
Most adults with any outpatient mental health service use were treated by general medical professionals (only) (Table 4). Significant relative increases in any outpatient mental health service use by general medical professionals (only) occurred in all demographic groups examined and both psychological distress severity strata. The relative increase was greater among men than among women.
Table 4. Trends in Any Outpatient Mental Health Service Use by Adults by Service Sectora.
| Variable | Use of Outpatient Mental Health Service, % | Period Association, OR (95% CI)b | P Value for Interactionc | ||
|---|---|---|---|---|---|
| 2004-2005 | 2009-2010 | 2014-2015 | |||
| Psychiatrists | |||||
| Total | 2.86 | 3.12 | 3.60 | 1.29 (1.14-1.46) | NA |
| Age, y | |||||
| 18-39 | 2.47 | 3.36 | 3.46 | 1.39 (1.17-1.65) | 1 [Reference] |
| 40-59 | 3.84 | 3.44 | 4.00 | 1.05 (0.87-1.26) | <.001 |
| ≥60 | 1.94 | 2.24 | 3.28 | 1.78 (1.37-2.30) | .007 |
| Sex | |||||
| Male | 2.40 | 2.71 | 2.94 | 1.25 (1.04-1.50) | .55 |
| Female | 3.30 | 3.50 | 4.21 | 1.32 (1.15-1.52) | |
| Race/ethnicity | |||||
| White | 3.17 | 3.56 | 4.16 | 1.36 (1.18-1.58) | .35 |
| Nonwhite | 2.16 | 2.18 | 2.60 | 1.22 (1.00-1.49) | |
| Psychological distress | |||||
| Serious psychological distress | 16.24 | 17.16 | 20.59 | 1.38 (1.11-1.73) | .96 |
| Less serious or no psychological distress | 2.19 | 2.37 | 2.90 | 1.35 (1.17-1.56) | |
| Other Mental Health Professionals | |||||
| Total | 1.37 | 1.35 | 1.81 | 1.39 (1.17-1.66) | NA |
| Age, y | |||||
| 18-39 | 1.56 | 1.50 | 2.14 | 1.42 (1.10-1.83) | 1 [Reference] |
| 40-59 | 1.69 | 1.63 | 1.83 | 1.09 (0.84-1.40) | .001 |
| ≥60 | 0.51 | 0.69 | 1.33 | 2.81 (1.73-4.59) | .005 |
| Sex | |||||
| Male | 0.89 | 1.03 | 1.28 | 1.48 (1.13-1.95) | .45 |
| Female | 1.82 | 1.65 | 2.31 | 1.34 (1.11-1.63) | |
| Race/ethnicity | |||||
| White | 1.66 | 1.63 | 2.27 | 1.47 (1.20-1.79) | .99 |
| Nonwhite | 0.71 | 0.76 | 0.99 | 1.44 (1.05-1.98) | |
| Psychological distress | |||||
| Serious psychological distress | 3.10 | 4.32 | 6.31 | 2.16 (1.48-3.16) | .03 |
| Less serious or no psychological distress | 1.31 | 1.19 | 1.66 | 1.34 (1.10-1.63) | |
| General Medical Professionals (Only) | |||||
| Total | 14.85 | 15.98 | 17.59 | 1.19 (1.11-1.28) | NA |
| Age, y | |||||
| 18-39 | 8.39 | 9.17 | 10.15 | 1.24 (1.08-1.41) | 1 [Reference] |
| 40-59 | 16.73 | 17.67 | 18.40 | 1.12 (1.02-1.24) | .08 |
| ≥60 | 23.29 | 24.39 | 27.06 | 1.24 (1.12-1.37) | .42 |
| Sex | |||||
| Male | 10.11 | 11.37 | 13.13 | 1.29 (1.17-1.43) | .02 |
| Female | 19.27 | 20.31 | 21.76 | 1.13 (1.05-1.23) | |
| Race/ethnicity | |||||
| White | 17.72 | 19.27 | 21.91 | 1.28 (1.19-1.37) | .17 |
| Nonwhite | 8.29 | 8.97 | 9.88 | 1.15 (1.03-1.28) | |
| Psychological distress | |||||
| Serious psychological distress | 34.84 | 37.14 | 41.50 | 1.31 (1.09-1.58) | .32 |
| Less serious or no psychological distress | 13.76 | 14.78 | 16.52 | 1.21 (1.12-1.30) | |
Abbreviations: NA, not applicable; OR, odds ratio.
Data are from the Medical Expenditure Panel Surveys and are presented as annualized percentages. Serious psychological distress is based on a Kessler 6 scale score of 13 or higher.
Period associations represent the age- and sex-adjusted OR of any outpatient mental health service use in 2014-2015 vs 2004-2005 (reference).
P values for interaction test whether changes in any outpatient mental health service use differed over time across demographic or psychological distress severity strata.
The percentage of adults with any outpatient mental health service use from psychiatrists and other mental health professionals also increased between 2004-2005 and 2014-2015 (Table 4). Significant increases in treatment by psychiatrists were evident among younger adults and older adults but not among middle-aged adults, men and women, and white adults. The relative increase in treatment by psychiatrists was greater for older adults than for younger adults or middle-aged adults. Adults with serious psychological distress and adults with less serious or no psychological distress had approximately similar increases in psychiatric treatment. Between 2004-2005 and 2014-2015, treatment by other mental health professionals increased for younger adults and (especially) older adults, for men and women, and for white adults and nonwhite adults. Compared with adults with less serious or no psychological distress, those with serious psychological distress had a greater relative increase in treatment by other mental health professionals.
Discussion
During the study period, there was a decline in the percentage of adults with serious psychological distress. Although this decline coincided with an increase in use of outpatient mental health care, it is unlikely that treatment substantially contributed to the reduction in serious psychological distress because the proportionate decrease in serious psychological distress was smaller among adults using than not using mental health treatment. The factors that led to the decline are not known but may include improving economic conditions after the Great Recession,20 increasing levels of physical activity,21 and declining rates of smoking.22,23 Between 1996-1998 and 2010-2012, an analogous decrease in the percentage of children and adolescents with severe mental health impairment occurred.24
Over the past several years, an increasing percentage of US adults have received outpatient mental health treatment. This occurrence was primarily associated with an increase in treatment of adults without serious psychological distress. However, the increase was proportionately larger for adults with than without serious psychological distress. As seen in the present study, in 2014-2015, more than two-thirds of adults with serious psychological distress accessed outpatient mental health care, an increase of 14.23% from 10 years earlier. In the context of prior epidemiological research documenting extensive unmet need for mental health care,25,26 the present findings suggest that the gap in unmet need for treatment has narrowed.
Several factors may have contributed to the national increase in outpatient mental health care, including improved public attitudes toward seeking mental health treatment,27 changes in clinical diagnostic practices, US Food and Drug Administration approval of new psychotropic medications, increases in psychotropic prescribing by primary care physicians,28 and policy developments that have lowered financial barriers to mental health care. Some major relevant policy developments during this period include enactment in 2006 of the Medicare Part D prescription drug benefit, the Paul Wellstone and Pete Domenici Mental Health Parity and Addiction Equity Act of 2008, the Medicare Improvements for Patients and Providers Act of 2008, and various provisions of the Patient Protection and Affordable Care Act, such as the dependent care provision in 2010 and Medicaid expansion and private insurance subsidies in 2014.
Medicaid acquisition has been associated with gains in depression treatment.29 Because adults with higher compared with lower levels of distress are more likely to be uninsured,30 health insurance reform may have preferentially increased mental health treatment of adults with higher levels of psychological distress. Nevertheless, there was no evidence herein of narrowing in racial/ethnic differences of outpatient mental health service use; mental health service use remained substantially lower in nonwhite adults than in white adults throughout the study period. Lack of progress in reducing racial/ethnic disparities in mental health treatment has important public health and policy implications, especially given the projected changing racial/ethnic composition of the US population.31 Some policy reforms may have contributed to the observed demographic trends in outpatient mental health service use in our study. For example, Medicare Part D may have increased mental health treatment of older adults by expanding their pharmacy coverage,32 and the dependent care provision of the Patient Protection and Affordable Care Act may have increased treatment of young adults by increasing their access to private insurance.33
There was an increase in psychotropic medication use during the study period that is consistent with a greater willingness of US adults to take these medications.27 The largest proportionate increase in our study occurred for mood stabilizers. This outcome may reflect a growing consensus in conceptualizing mood disorders along a continuum from unipolar depression through mixed depressive and manic symptoms to mania34 and treatment of depression and bipolar spectrum features with mood stabilizers.35
Use of antidepressants, anxiolytics/sedatives, antipsychotics, mood stabilizers, and stimulants also increased during the study period. Treatment with anxiolytics/sedatives increased proportionately more for adults above than below the serious psychological distress threshold, suggesting that these medications are becoming more focused on high-need populations, although increases in less distressed populations raise safety concerns, especially in older adults.36 Stimulant use increased among adults above and below the serious psychological distress threshold, which is consistent with increased public and professional attention to adult attention-deficit/hyperactivity disorder.37 Proportionately greater increased antipsychotic use among adults with serious psychological distress than with less serious or no psychological distress may reflect greater caution in prescribing these medications outside of psychotic and other severe psychiatric disorders in light of increased awareness of safety concerns.38
The national increase in outpatient mental health services extended to treatment provided by psychiatrists, other mental health professionals, and general medical professionals. The broad definition herein of outpatient mental health service use, which includes psychotropic medication use without a mental disorder diagnosis, contributes to the high observed proportion of mental health care provided by non–mental health professionals. Different results would have been obtained with a narrower definition that required a mental disorder diagnosis.39
Older adults experienced a disproportionately large increase in outpatient mental health care provided by psychiatrists and other mental health professionals. In view of low use of mental health services by older adults reported from the National Comorbidity Survey Replication (2001-2003),25,40 these trends suggest that this gap is narrowing, although more detailed analyses are needed to evaluate the extent of unmet mental health care needs among older adults.
Limitations
The present analyses have several limitations. First, MEPS relies on respondent recall and calendars/diaries that may underestimate mental health care use, although a medical provider survey supplements and validates reported service use. Second, although the K-6 correlates with several serious mental disorders,16 it is not a diagnostic measure. An AUC of 0.86 indicates that 14% of adults with serious mental illnesses are not detected with the scale. The K-6 includes only depression and anxiety symptoms, and several key dimensions of severe psychopathology, such as psychosis, mania, and substance use, are not represented. Nevertheless, because the K-6 is a dimensional scale, it may better represent a need for mental health services than individual disorders that may vary widely in severity,41 with approximately one-quarter of the adult population meeting criteria for 1 or more DSM-IV disorder at any time point.7 Third, some people who received outpatient mental health care may have reported lower K-6 scores than they would have reported without treatment. Fourth, MEPS does not provide details concerning the types of psychological services used. Fifth, MEPS provides no information on the effectiveness of treatment. This limitation prevents rigorous examination of the association between increasing mental health service use and decreasing serious psychological distress or determination of which adults are overtreated or undertreated.
Conclusions
Between 2004-2005 and 2014-2015, an increasing percentage of US adults received outpatient mental health care. Although increased treatment was found for those with serious psychological distress, the bulk of the increase was driven by greater treatment of adults without serious psychological distress. However, despite increases in outpatient mental health treatment, many adults with serious psychological distress received no mental health care. Compared with adults with less serious or no psychological distress, those with serious psychological distress may have a less favorable view of the effectiveness of mental health treatment.42 Although progress has been made, improvements are still needed in general medical settings in detecting and either treating or referring adults in need of mental health care.
eTable 1. Comparative Odds of Serious Psychological Distress Among Adults Stratified by Age, Sex, and Race/Ethnicity in 2004-05, 2009-10, and 2014-15, United States
eTable 2. Trends in Use of Any Outpatient Mental Health Service by Adults
eTable 3. Estimated Number of Adults in Millions Receiving Any Outpatient Mental Health Services by Serious Psychological Distress
eTable 4. Comparative Odds of Any Mental Health Service Use by Adults Stratified by Age, Sex, and Race/Ethnicity in 2004-05, 2009-10, and 2014-15, United States
References
- 1.Han B, Olfson M, Huang L, Mojtabai R. National trends in specialty outpatient mental health care among adults [published correction appears in Health Aff (Millwood). 2018;37(2):336]. Health Aff (Millwood). 2017;36(12):2062-2068. doi: 10.1377/hlthaff.2017.0922 [DOI] [PubMed] [Google Scholar]
- 2.National Center for Health Statistics , Centers for Disease Control and Prevention. Health, United States, 2016. —individual charts and tables: spreadsheet, PDF, and PowerPoint files. Table 080. https://www.cdc.gov/nchs/hus/contents2016.htm#080 Accessed May 5, 2018.
- 3.Curtin SC, Warner M, Hedegaard H Suicide rates for females and males by race and ethnicity: United States, 1999 and 2014. NCHS health E-stat. National Center for Health Statistics. April 2016.
- 4.Dart RC, Surratt HL, Cicero TJ, et al. Trends in opioid analgesic abuse and mortality in the United States. N Engl J Med. 2015;372(3):241-248. doi: 10.1056/NEJMsa1406143 [DOI] [PubMed] [Google Scholar]
- 5.Rudd RA, Seth P, David F, Scholl L. Increases in drug and opioid overdose deaths—United States, 2010-2015. MMWR Morb Mortal Wkly Rep. 2016;65(50-51):1445-1452. doi: 10.15585/mmwr.mm655051e1 [DOI] [PubMed] [Google Scholar]
- 6.Ten Have M, Nuyen J, Beekman A, de Graaf R. Common mental disorder severity and its association with treatment contact and treatment intensity for mental health problems. Psychol Med. 2013;43(10):2203-2213. doi: 10.1017/S0033291713000135 [DOI] [PubMed] [Google Scholar]
- 7.Kessler RC, Demler O, Frank RG, et al. Prevalence and treatment of mental disorders, 1990 to 2003. N Engl J Med. 2005;352(24):2515-2523. doi: 10.1056/NEJMsa043266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Demyttenaere K, Bruffaerts R, Posada-Villa J, et al. ; WHO World Mental Health Survey Consortium . Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health surveys. JAMA. 2004;291(21):2581-2590. doi: 10.1001/jama.291.21.2581 [DOI] [PubMed] [Google Scholar]
- 9.Druss BG, Wang PS, Sampson NA, et al. Understanding mental health treatment in persons without mental diagnoses: results from the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2007;64(10):1196-1203. doi: 10.1001/archpsyc.64.10.1196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weiss C, Connor S, Ward P, DiGaetano R, Machlin S, Wun LM Report on interim nonresponse subsampling for MEPS Panel 16. Agency for Healthcare Research and Quality Working Paper No. 13001. https://meps.ahrq.gov/data_files/publications/workingpapers/wp_13001.pdf. Published January 11, 2013. Accessed May 20, 2018.
- 11.Wun LM, Ezzati-Rice TM Diaz-Tena N, Greenblatt J. On modeling response propensity for dwelling unit (DU) level non-response adjustment in the Medical Expenditure Panel Survey (MEPS). Stat Med. 2007;26(8):1875-1884. doi: 10.1002/sim.2809 [DOI] [PubMed] [Google Scholar]
- 12.Agency for Healthcare Research and Quality Medical Expenditure Panel Survey, MEPS Survey Questionnaires, Household Questionnaire Sections Rockville, MD: Dept of Health and Human Services. https://meps.ahrq.gov/mepsweb/survey_comp/survey.jsp. Accessed May 20, 2018.
- 13.Agency for Healthcare Research and Quality MEPS HC-036: 1996-2012: pooled linkage variance estimation file. https://meps.ahrq.gov/data_stats/download_data_files_detail.jsp. Published October 2014. Accessed May 20, 2018.
- 14.Kessler RC, Berglund PA, Glantz MD, et al. Estimating the prevalence and correlates of serious mental illness in community epidemiological surveys In: Manderscheid RW, Henderson MJ, eds. Mental Health, United States, 2002 Rockville, MD: Substance Abuse and Mental Health Services Administration; 2004. [Google Scholar]
- 15.Pratt LA. Serious psychological distress, as measured by the K6, and mortality. Ann Epidemiol. 2009;19(3):202-209. doi: 10.1016/j.annepidem.2008.12.005 [DOI] [PubMed] [Google Scholar]
- 16.Kessler RC, Barker PR, Colpe LJ, et al. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003;60(2):184-189. doi: 10.1001/archpsyc.60.2.184 [DOI] [PubMed] [Google Scholar]
- 17.Kessler RC, Andrews G, Mroczek D, Üstün TB, Wittchen HU. The World Health Organization Composite International Diagnostic Interview Short-Form (CIDI-SF). Int J Methods Psychiatr Res. 1998;7:171-185. doi: 10.1002/mpr.47 [DOI] [Google Scholar]
- 18.Furukawa TA, Kessler RC, Slade T, Andrews G. The performance of the K6 and K10 screening scales for psychological distress in the Australian National Survey of Mental Health and Well-Being. Psychol Med. 2003;33(2):357-362. doi: 10.1017/S0033291702006700 [DOI] [PubMed] [Google Scholar]
- 19.Dismuke CE, Egede LE. Association of serious psychological distress with health services expenditures and utilization in a national sample of US adults. Gen Hosp Psychiatry. 2011;33(4):311-317. doi: 10.1016/j.genhosppsych.2011.03.014 [DOI] [PubMed] [Google Scholar]
- 20.Cooper B. Economic recession and mental health: an overview. Neuropsychiatr. 2011;25(3):113-117. [PubMed] [Google Scholar]
- 21.An R, Xiang X, Yang Y, Yan H. Mapping the prevalence of physical inactivity in US states, 1984-2015. PLoS One. 2016;11(12):e0168175. doi: 10.1371/journal.pone.0168175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health 13. Patterns of tobacco use among US youth, young adults, and adults. In: The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General Atlanta, GA: Centers for Disease Control and Prevention; 2014. https://www.ncbi.nlm.nih.gov/books/NBK294302/. Accessed May 10, 2018.
- 23.Patterns of tobacco use among U.S. youth, young adults, and adults. https://www.ncbi.nlm.nih.gov/books/NBK294302/. Accessed May 10, 2018.
- 24.Olfson M, Druss BG, Marcus SC. Trends in mental health care among children and adolescents. N Engl J Med. 2015;372(21):2029-2038. doi: 10.1056/NEJMsa1413512 [DOI] [PubMed] [Google Scholar]
- 25.Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelve-month use of mental health services in the United States: results from the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):629-640. doi: 10.1001/archpsyc.62.6.629 [DOI] [PubMed] [Google Scholar]
- 26.Kessler RC, Zhao S, Katz SJ, et al. Past-year use of outpatient services for psychiatric problems in the National Comorbidity Survey. Am J Psychiatry. 1999;156(1):115-123. doi: 10.1176/ajp.156.1.115 [DOI] [PubMed] [Google Scholar]
- 27.Mojtabai R. Americans’ attitudes toward psychiatric medications: 1998-2006. Psychiatr Serv. 2009;60(8):1015-1023. doi: 10.1176/ps.2009.60.8.1015 [DOI] [PubMed] [Google Scholar]
- 28.Olfson M, Kroenke K, Wang S, Blanco C. Trends in office-based mental health care provided by psychiatrists and primary care physicians. J Clin Psychiatry. 2014;75(3):247-253. doi: 10.4088/JCP.13m08834 [DOI] [PubMed] [Google Scholar]
- 29.Baicker K, Taubman SL, Allen HL, et al. ; Oregon Health Study Group . The Oregon experiment: effects of Medicaid on clinical outcomes. N Engl J Med. 2013;368(18):1713-1722. doi: 10.1056/NEJMsa1212321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pearson WS, Dhingra SS, Strine TW, Liang YW, Berry JT, Mokdad AH. Relationships between serious psychological distress and the use of health services in the United States: findings from the Behavioral Risk Factor Surveillance System. Int J Public Health. 2009;54(suppl 1):23-29. doi: 10.1007/s00038-009-0003-4 [DOI] [PubMed] [Google Scholar]
- 31.Vespa J, Armstrong DM, Medina L. Demographic Turning Points for the United States: Population Projections for 2020 to 2060, Current Population Reports. Washington, DC: US Census Bureau; 2018:25-1144. https://www.census.gov/content/dam/Census/library/publications/2018/demo/P25_1144.pdf. Accessed July 20, 2018. [Google Scholar]
- 32.Donohue JM, Zhang Y, Aiju M, et al. Impact of Medicare Part D on antidepressant treatment, medication choice, and adherence among older adults with depression. Am J Geriatr Psychiatry. 2011;19(12):989-997. doi: 10.1097/JGP.0b013e3182051a9b [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Saloner B, Lê Cook B. An ACA provision increased treatment for young adults with possible mental illnesses relative to comparison group. Health Aff (Millwood). 2014;33(8):1425-1434. doi: 10.1377/hlthaff.2014.0214 [DOI] [PubMed] [Google Scholar]
- 34.Moreno C, Hasin DS, Arango C, et al. Depression in bipolar disorder versus major depressive disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Bipolar Disord. 2012;14(3):271-282. doi: 10.1111/j.1399-5618.2012.01009.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McIntyre RS, Ng-Mak D, Chuang CC, et al. Major depressive disorder with subthreshold hypomanic (mixed) features: a real-world assessment of treatment patterns and economic burden. J Affect Disord. 2017;210:332-337. doi: 10.1016/j.jad.2016.12.033 [DOI] [PubMed] [Google Scholar]
- 36.Markota M, Rummans TA, Bostwick JM, Lapid MI. Benzodiazepine use in older adults: dangers, management, and alternative therapies. Mayo Clin Proc. 2016;91(11):1632-1639. doi: 10.1016/j.mayocp.2016.07.024 [DOI] [PubMed] [Google Scholar]
- 37.Kessler RC, Adler L, Barkley R, et al. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry. 2006;163(4):716-723. doi: 10.1176/ajp.2006.163.4.716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Correll CU, Robinson DG, Schooler NR, et al. Cardiometabolic risk in patients with first-episode schizophrenia spectrum disorders: baseline results from the RAISE-ETP study. JAMA Psychiatry. 2014;71(12):1350-1363. doi: 10.1001/jamapsychiatry.2014.1314 [DOI] [PubMed] [Google Scholar]
- 39.Mojtabai R, Olfson M. Proportion of antidepressants prescribed without a psychiatric diagnosis is growing. Health Aff (Millwood). 2011;30(8):1434-1442. doi: 10.1377/hlthaff.2010.1024 [DOI] [PubMed] [Google Scholar]
- 40.Byers AL, Arean PA, Yaffe K. Low use of mental health services among older Americans with mood and anxiety disorders. Psychiatr Serv. 2012;63(1):66-72. doi: 10.1176/appi.ps.201100121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617-627. doi: 10.1001/archpsyc.62.6.617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kobau R, Zack MM. Attitudes toward mental illness in adults by mental illness–related factors and chronic disease status: 2007 and 2009 Behavioral Risk Factor Surveillance System. Am J Public Health. 2013;103(11):2078-2089. doi: 10.2105/AJPH.2013.301321 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Comparative Odds of Serious Psychological Distress Among Adults Stratified by Age, Sex, and Race/Ethnicity in 2004-05, 2009-10, and 2014-15, United States
eTable 2. Trends in Use of Any Outpatient Mental Health Service by Adults
eTable 3. Estimated Number of Adults in Millions Receiving Any Outpatient Mental Health Services by Serious Psychological Distress
eTable 4. Comparative Odds of Any Mental Health Service Use by Adults Stratified by Age, Sex, and Race/Ethnicity in 2004-05, 2009-10, and 2014-15, United States