This analysis of US nationally representative survey data assessed the financial burdens of patients with head and neck cancer compared with patients with other types of cancer.
Key Points
Questions
How do the financial demographics of patients with head and neck cancer differ from patients with other cancers, and how are these differences associated with their medical expenses?
Findings
In this review of data from 16 771 patients with cancer in the Medical Expenditure Panel Survey, patients with head and neck cancer were more often members of a racial/ethnic minority group, poor, and less educated and had lower health status than patients with other cancers. Patients with head and neck cancer also experienced higher total medical expenses and higher out-of-pocket costs relative to their income, with the highest relative out-of-pocket costs occurring among the poor and publicly insured.
Meaning
Patients with head and neck cancer are uniquely disenfranchised and have higher medical expenses, which cumulatively increases their risk for financial burdens incurred by medical treatments.
Abstract
Importance
Head and neck cancer (HNC) is more common among socioeconomically disenfranchised individuals, making financial burden particularly relevant.
Objective
To assess the financial burdens of HNC compared with other cancers.
Design, Setting, and Participants
In this retrospective review of nationally representative, publicly available survey, data from the Medical Expenditure Panel Survey were extracted from January 1, 1998, to December 31, 2015. A total of 444 867 adults were surveyed, which extrapolates to a population of 221 503 108 based on the weighted survey design. Data analysis was performed from April 18, 2018, to August 20, 2018.
Exposures
Of 16 771 patients with cancer surveyed (weighted count of 10 083 586 patients), 489 reported HNC (weighted count of 261 631).
Main Outcomes and Measures
Patients with HNC were compared with patients with other cancers on demographics, income, employment, and health. Within the HNC group, risk factors for total medical expenses and relative out-of-pocket expenses were assessed with regression modeling. Complex sampling methods were accounted for with weighting using balanced repeated replication.
Results
A total of 16 771 patients (mean [SD] age, 62.3 [18.9] years; 9006 [53.7%] female) with cancer were studied. Compared with patients with other cancers, patients with HNC were more often members of a minority race/ethnicity, male, poor, publicly insured, and less educated, with lower general and mental health status. Median annual medical expenses ($8384 vs $5978; difference, $2406; 95% CI, $795-$4017) and relative out-of-pocket expenses (3.93% vs 3.07%; difference, 0.86%; 95% CI, 0.06%-1.66%) were higher for patients with HNC than for patients with other cancers. Among patients with HNC, median expenses were lower for Asian individuals compared with white individuals ($5359 vs $10 078; difference, $4719; 95% CI, $1481-$7956]), Westerners ($8094) and Midwesterners ($5656) compared with Northwesterners ($10 549), and those with better health status ($16 990 for those with poor health vs $6714 for those with excellent health). Higher relative out-of-pocket expenses were associated with unemployment (5.13% for employed patients vs 2.35% for unemployed patients; difference, 2.78%; 95% CI, 0.6%-4.95%), public insurance (5.35% for those with public insurance vs 2.87% for those with private insurance; difference, 2.48%; 95% CI, −0.6% to 5.55%), poverty (13.07% for poor patients vs 2.06% for high-income patients), and lower health status (10.2% for those with poor health vs 1.58% for those with excellent health).
Conclusions and Relevance
According to this study, HNC adds a substantial, additional burden to an already financially strained population in the form of higher total and relative expenses. The financial strain on individuals, assessed as relative out-of-pocket expenses, appears to be driven more by income than by health factors, and health insurance does not appear to be protective.
Introduction
With increasing survivability of cancer, the number of cancer survivors in the United States is expected to increase to 18 million by 2020.1 The cost of cancer care has also doubled during the past decade, contributing 4.9% of all medical expenditures and continuing to increase.2,3 The financial burden to patients, especially those with cancer, is increasingly recognized. Out-of-pocket cancer expenses often consume up to 27% of income in low-income households,4 and it is the most common cause of medical bankruptcy.5
This financial burden is acutely relevant in head and neck cancer (HNC), which occurs disproportionately in the socioeconomically disenfranchised, is costly to treat, and creates long-term health needs.6,7,8,9 Head and neck cancer encompasses mucosal and salivary gland malignant tumors of the upper aerodigestive tract,10 thus directly affecting vital functions, including voice, swallowing, and cosmesis. Head and neck cancer constitutes 3% of new cancer diagnoses, with 436 060 current survivors,8,11 and its incidence is increasing.12 Survival has slowly improved13 to 64.5% at 5 years,14 largely driven by shifting causes from carcinogen exposures to human papillomavirus–mediated disease.15,16
Most existing literature on HNC expenses is limited to subpopulations defined by the treating institution, payer, age, site, or treatment modality.17,18,19,20 A systematic review21 in 2014 concluded that no studies up to that time had assessed the societal burden of HNC medical cost. The largest study9 used a national sample and established a median treatment cost of $79 151, with variability attributed to payer, treatment modality, and health status. However, that study was restricted to insured patients and did not include income data to contextualize out-of-pocket expenses. Only 2 studies22,23 analyzed a nationally representative sample, but the scopes were limited to defining expenses attributable to HNC. No prior study, to our knowledge, directly compares HNC finances and expenses with those of other patient populations.
The present study used the Medical Expenditure Panel Survey (MEPS) database to assess the societal and individual burden of HNC. Comparisons were made with other cancer survivors, trends were assessed for total and relative expenses, and factors associated with increased total and personal expenses were identified.
Methods
Data Source and Definitions
Data were collected from the MEPS database using household and condition survey files from January 1, 1997, through December 31, 2015.24 Data analysis was performed from April 18, 2018, to August 20, 2018. The survey methods have been previously described in detail.25 Briefly, the survey provides a nationally representative, annual assessment of the nation’s medical expenses and includes data on individual demographics, employment, income, insurance, and medical conditions. Individuals younger than 18 years were excluded. For the years when age at diagnosis was available (2007-2012), length of follow-up was calculated based on age at the time the survey was completed. This study was considered exempt from review and patient consent by the Saint Louis University Institutional Review Board based on use of deidentified, publicly available data. The need for participant informed consent was also waived by the Institutional Review Board for the same reason.
Demographic characteristics included age, sex, race/ethnicity (white, black, Asian, Hispanic, or other), and marital status (married, single, or widowed or separated). Race/ethnicity was self-identified by the survey participants. In addition, educational level was available since 2011 (less than high school, high school graduate, or beyond high school). Economic variables included insurance (any private, public only, or uninsured), employment, total family income, and poverty level. Poverty level was divided into 5 categories based on the percentage of the local poverty level: poor (<100%), near poor (100%-125%), low income (>125%-200%), middle income (>200%-400%), and high income (>400%).
Several metrics of patient health were investigated. Individual self-report of general and mental health was assessed on a 5-point semicontinuous scale, ranging from poor (score of 1) to excellent (score of 5). In addition, 2 comorbidity indexes were calculated from International Classification of Disease, Ninth Revision (ICD-9) codes listed in the condition data files. First, the Charlson Comorbidity Index with Quan modification26 was used to allow comparisons with other oncologic literature. Second, the Elixhauser index with van Walraven modification27 was used because of its stronger correlation with inpatient mortality and medical expenses.28
Total expenses incorporate expenses reported by the household and practitioner survey components. Expenses and income were corrected for inflation to 2014 US dollars using the gross domestic product for total expenses and price index for individual costs and income based on MEPS guidelines. Relative out-of-pocket expenses were calculated as the percentage of total income spent on out-of-pocket medical expenses.
Comparison Between Cancer Groups
Individuals were categorized as having HNC, other cancer, or no cancer based on the MEPS clinical classification system.29 Individual characteristics were compared between patients with HNC, other cancers, and no cancer. Differences between means, medians, and proportions for each variable are reported together with 95% CIs.
Trend Analysis
Annual estimates were calculated for HNC and other cancer groups. Total and relative out-of-pocket expenses were assessed over time, and trends were assessed by linear regression models.
Identifying Factors Associated With Increased Expenses
Among patients with HNC, factors associated with increased total and relative out-of-pocket expenses were assessed using generalized linear models. To select the optimal model, several models were explored to best reflect the data, as summarized by Mihaylova et al.30 Given that less than 1% of individuals within each cancer group had nonzero expenses, a 2-stage model was not required. Instead, to account for the skewed distribution, a log-link was used. To allow inclusion of individuals with no expenses, these values were set nominally to $1. For those with out-of-pocket expenses but no income, the relative out-of-pocket expense would be infinite, so it was set to the 97.5th percentile of all finite values. These transformations were confirmed to normalize the distributions of total and relative expenses and accommodate a gaussian distribution without substantially affecting median values.
Bivariable models were created using demographics, economic factors, health status, age of diagnosis, and time since diagnosis with the outcome variables. Ordinal variables were analyzed as linear and semicontinuous. Variables were eligible for inclusion in the initial multivariable model if the 90% CI excluded 1 and data were available for all study years. A stepwise analysis was then used to maximize the predictive ability of the model. To assess the association of variables available for limited years, a sensitivity analysis was performed using only the data from 2007 to 2012 with all variables available. Results of the linear models are reported as β with 95% CI after inverse log transformation so that β = 1 represents no association between the independent and dependent variables.
Statistical Analysis
Data were downloaded from MEPS publicly available files, then imported into R statistical computing software, version 3.2.3 (R Foundation for Statistical Computing) for analysis using the survey package. Complex sampling techniques were accounted for using sample weights with balanced repeated replication techniques. Comorbidity indexes were calculated with the icd package. Results are presented as weighted estimates with 95% CIs.
Results
Description of the Cohort
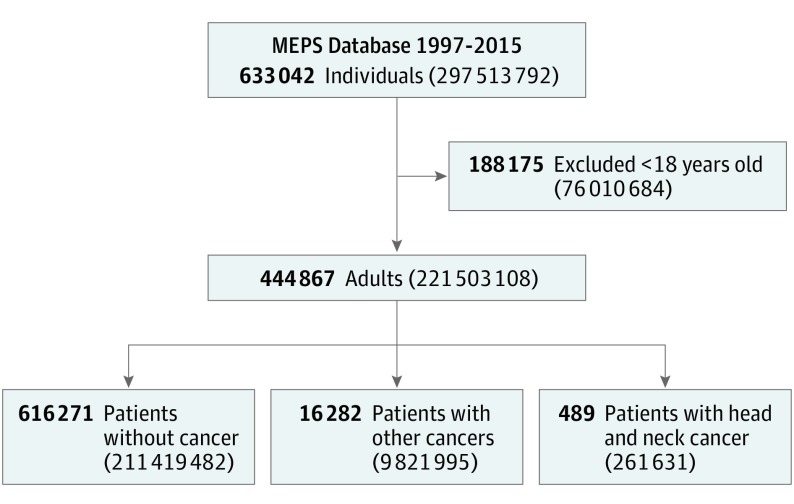
From January 1, 1997, to December 31, 2015, a total of 16 771 surveyed individuals reported a history of cancer (mean [SD] age, 62.3 [18.9] years; 9006 [53.7%] female), including 489 (3.0%) with HNC. This number extrapolates to a national representative weighted sample of 10 083 586 patients with cancer and 261 631 patients (2.7%) with HNC (Figure 1). Of the 131 patients with data from 2007 to 2012 (which includes age of the patient at time of HNC diagnosis), 35 (26.7%) had been diagnosed within the year before the survey.
Figure 1. Cohort Selection.
Number of individuals presented as raw count, with weighted totals given parenthetically. MEPS indicates Medical Expenditure Panel Survey.
Patient characteristics are summarized in Table 1, including individuals without cancer for comparison. Compared with patients with other cancers, patients with HNC were less likely to be female, white, and highly educated and more likely to be poor and publicly insured. The general and mental health status of patients with HNC was rated worse. Patients with HNC also had more comorbidities based on the Charlson comorbidity index and Elixhauser index.
Table 1. Cohort Characteristics by Cancer Diagnosis and Sitea.
| Characteristic | HNC | Other Cancer | Difference (95% CI)b | No Cancer |
|---|---|---|---|---|
| Age, mean (95% CI), y | 65.0 (63.1 to 66.8) | 65.4 (64.9 to 65.8) | −0.37 (−2.23 to 1.49) | 45.1 (44.9 to 45.3) |
| Educational level | ||||
| Less than high school | 41 459 (13.7) | 1 216 400 (9.5) | 4.11 (−5.19 to 13.4) | 30 088 669 (14.4) |
| High school graduate | 122 366 (40.3) | 3 570 902 (28.0) | 12.29 (−1.28 to 25.9) | 58 067 550 (27.9) |
| Beyond high school | 139 671 (46.0) | 7 951 655 (62.4) | −16.4 (−29.4 to −3.45) | 120 304 436 (57.7) |
| Marriage | ||||
| Married | 160 172 (61.2) | 6 217 582 (63.3) | −2.08 (−10.5 to 6.33) | 114 302 813 (54.1) |
| Single | 16 486 (6.30) | 691 278 (7.04) | −0.74 (−4.46 to 2.99) | 56 152 902 (26.6) |
| Widowed or separated | 84 980 (32.5) | 2 913 357 (29.7) | 2.82 (−4.7 to 10.3) | 40 963 539 (19.4) |
| Race/ethnicity | ||||
| White | 167 902 (64.2) | 7 202 115 (73.3) | −9.15 (−16.0 to −2.32) | 108 803 255 (51.5) |
| Black | 25 653 (9.8) | 508 835 (5.2) | 4.62 (0.6 to 8.65) | 24 793 134 (11.7) |
| Asian | 55 225 (21.1) | 1 669 830 (17) | 4.11 (−1.87 to 10.1) | 47 786 796 (22.6) |
| Hispanic | 12 851 (4.9) | 392 875 (4) | 0.91 (−1.62 to 3.44) | 2 8751 347 (13.6) |
| Other | 0 | 48 339 (0.5) | −0.49 (−0.68 to −0.31) | 1 284 949 (0.6) |
| Sex | ||||
| Male | 168 716 (64.5) | 4 622 219 (47.1) | 17.4 (10.1 to 24.7) | 101 923 275 (48.2) |
| Female | 92 916 (35.5) | 5 199 776 (52.9) | −17.4 (−24.7 to −10.1) | 109 496 207 (51.8) |
| Region | ||||
| Northeast | 44 315 (16.9) | 1 871 150 (19.1) | −2.11 (−7.45 to 3.22) | 39528045 (18.7) |
| Midwest | 56 326 (21.5) | 2 112 840 (21.5) | 0.02 (−6.63 to 6.66) | 46 812 323 (22.1) |
| South | 111 327 (42.6) | 3 743 322 (38.1) | 4.44 (−4.46 to 13.3) | 76 575 098 (36.2) |
| West | 49 666 (19) | 2 094 772 (21.3) | −2.34 (−8.44 to 3.75) | 48 503 924 (22.9) |
| Insurance | ||||
| Any private | 162 808 (62.2) | 7 084 104 (72.1) | −9.90 (−17.1 to −2.66) | 149 263 083 (70.6) |
| Public only | 91 952 (35.1) | 2 483 634 (25.3) | 9.86 (3.29 to 16.4) | 32 078 694 (15.2) |
| Uninsured | 6871 (2.6) | 254 256 (2.6) | 0.04 (−2.18 to 2.25) | 30 077 705 (14.2) |
| Health status | ||||
| Poor | 36 906 (14.1) | 744 480 (7.6) | −0.45 (−0.59 to −0.31)c | 6 794 135 (3.2) |
| Fair | 59 611 (22.7) | 1 536 531 (15.6) | 20 594 884 (9.7) | |
| Good | 80 197 (30.6) | 2 971 434 (30.2) | 55 862 747 (26.4) | |
| Very good | 67 862 (25.9) | 2 842 034 (28.9) | 68 962 565 (32.6) | |
| Excellent | 17 696 (6.7) | 1 741 264 (17.7) | 59 190 761 (28) | |
| Mental health status | ||||
| Poor | 5951 (2.3) | 165 708 (1.7) | −0.29 (−0.42 to −0.17)c | 2704 985 (1.3) |
| Fair | 30 896 (11.8) | 690 528 (7) | 10 978 514 (5.2) | |
| Good | 87 492 (33.4) | 2 658 537 (27) | 48 464 901 (22.9) | |
| Very good | 79415 (30.3) | 2 975 554 (30.2) | 62 886 943 (29.7) | |
| Excellent | 58 555 (22.3) | 3 348 996 (34) | 86 366 133 (40.9) | |
| van Walraven Index, mean (95% CI)d | 4.95 (4.46 to 5.43) | 3.41 (3.30 to 3.52) | 1.54 (1.05 to 2.02) | 0.37 (0.35 to 0.38) |
| Charlson Comorbidity Indexe | ||||
| 0 | 22 340 (7.8) | 3 687 823 (34.3) | 0.89 (0.67 to 1.10)c | 169 933 926 (80.7) |
| 1 | 7937 (2.8) | 1 144 979 (10.7) | 32 321 027 (15.4) | |
| 2 | 144 330 (50.4) | 3 547 635 (33) | 5 701 383 (2.7) | |
| ≥3 | 111 683 (39) | 2 367 272 (22) | 2 512 772 (1.2) | |
| Total income, median (95% CI), $f | 24 056 (21 478 to 26 633) | 29 698 (28 724 to 30 672) | −5642 (−7951 to −3334) | 27 979 (27 507 to 28 452) |
| Poverty levelg | ||||
| Poor | 28 824 (11) | 769 803 (7.8) | −0.24(−0.41 to −0.08)c | 24 146 405 (11.4) |
| Near poor | 15 252 (5.8) | 441 435 (4.5) | 8 742 755 (4.1) | |
| Low income | 39 859 (15.2) | 1 291 199 (13.1) | 27 984 171 (13.2) | |
| Middle income | 80 357 (30.7) | 2 667 237 (27.2) | 65 129 261 (30.8) | |
| High income | 97 339 (37.2) | 4 652 320 (47.4) | 8 5416 889 (40.4) | |
| Employment | ||||
| Employed | 97 628 (37.1) | 3 805 528 (38.6) | −1.54 (−7.94 to 4.85) | 144 111 467 (68.2) |
| Unemployed | 165 574 (62.9) | 6 044 143 (61.4) | 1.54 (−4.85 to 7.94) | 67 278 768 (31.8) |
| Total medical expenses, median (95% CI), $f | 8384 (6717 to 10 052) | 5978 (5770 to 6186) | 2407 (795 to 4017) | 1048 (1025 to 1072) |
| Out-of-pocket medical expenses, median (95% CI), $f | 929 (775 to 1084) | 918 (885 to 951) | 11 (−165 to 187) | 238 (231 to 245) |
| Out-of-pocket expenses per income, median (95% CI), % | 3.93 (3.21 to 4.65) | 3.07 (2.91 to 3.22) | 0.86 (0.06 to 1.66) | 0.87 (0.85 to 0.89) |
Abbreviation: HNC, head and neck cancer.
Data are presented as number (percentage) of patients unless otherwise indicated.
Differences are reported between HNC and other cancer groups. Negative differences imply a higher value for the other cancer group.
For ordinal variables, values were converted to numeric values and differences in the mean are reported.
The range of possible scores on the van Walraven Index is −19 to 89; higher scores indicate more comorbidities.
For the Charlson Comorbidity Index, the range of possible scores is 0 to 40; higher scores indicate more comorbidities.
Income and expenses are reported as the median of annualized values.
Poverty levels are defined in the Data Source and Definitions subsection of the Methods section.
Annual medical expenditure varied widely among patients with cancer (range, $0-$797 300). Median expenses were higher for patients with HNC compared with patients with other cancers. The out-of-pocket expenses were similar between groups; however, the out-of-pocket expense constituted a larger percentage of income for patients with HNC.
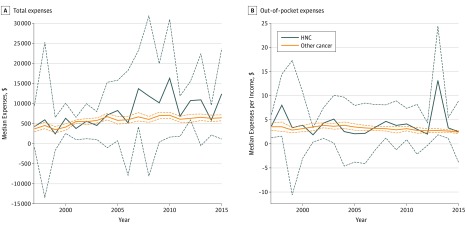
Medical Expenditures Trends for Patients With HNC
Total medical expenditures have increased over time (Figure 2A) for patients with other cancers ($273 per year; 95% CI, $170-$374) and patients with HNC ($252 per year; 95% CI, −$256 to $860); however, the 95% CI for HNC included $0 per year. Relative out-of-pocket expenses were generally stable over time (Figure 2B) for HNC (1.45% per year; 95% CI, −1.73% to 4.65%) and other cancer groups (0.25% per year; 95% CI, 4.67%-4.98%), with the notable exception of 2013, during which there was a substantial increase in relative out-of-pocket expense (13.1%; 95% CI, 1.87%-24.4%) before returning to baseline levels in 2014.
Figure 2. Medical Expense Trends.
Total medical expenses (A) and relative out-of-pocket expenses (B) are shown over time for patients with head and neck cancer (HNC) and all other cancers. Dashed lines represent 95% CIs.
Factors Associated With Total Expenses for Patients With HNC
In the bivariable models, total medical expenses were associated with race/ethnicity, region, educational level, general health status, and mental health status (Table 2). Specifically, Asian individuals had lower expenses than white individuals, and Midwesterners and Westerners had lower expenses than Northeasterners. Better general and mental health status was associated with lower expenses. Higher educational level was associated with higher expenses.
Table 2. Factors Associated With Total Medical Expenses: Results of Generalized Linear Model.
| Factor | Expenses, Median (95% CI), US $ | β (95% CI) | |
|---|---|---|---|
| Bivariable Model | Multivariable Model | ||
| Year of survey | NA | 1.02 (0.99-1.06) | NA |
| Age at diagnosis | NA | 1.01 (0.99-1.04) | NA |
| HNC follow-up, y | |||
| ≤1 | 18 113 (5071-31 155) | 1 [Reference] | NA |
| >1 | 8476 (4069-12 883) | 0.73 (0.47-1.12) | NA |
| Age at survey | NA | 0.99 (0.98-1.01) | NA |
| Marital status | |||
| Married | 8539 (6050-11 029) | 1 [Reference] | NA |
| Single | 6813 (3416-10 210) | 1.17 (0.41-3.34) | NA |
| Widowed or separated | 7982 (4809-11155) | 0.93 (0.65-1.34) | NA |
| Race/ethnicity | |||
| White | 10 078 (7914-12 241) | 1 [Reference] | 1 [Reference] |
| Black | 5313 (1817-8809) | 1.36 (0.60-3.10) | 1.46 (0.58-3.68) |
| Asian | 5359 (2977-7741) | 0.52 (0.36-0.74) | 0.53 (0.34-0.82) |
| Hispanic | 6086 (0-14 839) | 1.44 (0.72-2.89) | 1.28 (0.60-2.74) |
| Sex | |||
| Male | 8379 (6340-10 419) | 1 [Reference] | NA |
| Female | 8152 (5288-11 017) | 0.78 (0.56-1.1) | NA |
| Region | |||
| Northeast | 10 549 (5716-15 382) | 1 [Reference] | 1 [Reference] |
| Midwest | 5656 (2985-8326) | 0.54 (0.33-0.88) | 0.55 (0.30-0.99) |
| South | 8621 (6667-10 574) | 0.81 (0.50-1.33) | 0.83 (0.46-1.50) |
| West | 8094 (4931-11 257) | 0.53 (0.34-0.82) | 0.54 (0.29-1.01) |
| Poverty levela | |||
| Poor | 7101 (4307-9896) | 0.86 (0.56-1.30) | NA |
| Near poor | 8768 (3069-14 468) | ||
| Low income | 9641 (5524-13 759) | ||
| Middle income | 6560 (3689-9432) | ||
| High income | 8347 (4667-12 026) | ||
| Total income, per $1000 | NA | 1.00 (0.996-1.00) | NA |
| Employment | |||
| Employed | 7344 (4247-10 442) | 1 [Reference] | NA |
| Unemployed | 9044 (7103-10 984) | 1.06 (0.69-1.63) | NA |
| Insurance | |||
| Any private | 8305 (5774-10 836) | 1 [Reference] | NA |
| Public only | 9182 (6092-12 271) | 1.11 (0.78-1.59) | NA |
| Uninsured | 5287 (1753-8822) | 0.53 (0.07-4.20) | NA |
| Educational level | |||
| Less than high school | 6220 (1086-11 353) | 1.54 (0.96-2.48) | NA |
| High school graduate | 10 205 (5041-15 368) | ||
| Beyond high school | 9618 (4731-14 505) | ||
| Health status | |||
| Poor | 16 990 (9724-24 257) | 0.59 (0.42-0.84) | 0.65 (0.35-1.24) |
| Fair | 8084 (4895-11 272) | ||
| Good | 6219 (3931-8506) | ||
| Very good | 8062 (4887-11 237) | ||
| Excellent | 6714 (1235-12 193) | ||
| Mental health status | |||
| Poor | 23 227 (6621-39 832) | 0.60 (0.40-0.89) | NA |
| Fair | 8080 (535-15 626) | ||
| Good | 8433 (5680-11 187) | ||
| Very good | 8115 (5491-10 739) | ||
| Excellent | 8189 (4575-11 803) | ||
| van Walraven Index | NA | 0.99 (0.95-1.04) | NA |
| Charlson Comorbidity Index | NA | 1.02 (0.94-1.11) | NA |
Abbreviations: HNC, head and neck cancer; NA, not applicable.
Poverty levels are defined in the Data Source and Definitions subsection of the Methods section.
On the basis of statistical significance in the bivariable models, race/ethnicity and region were incorporated into a multivariable model. Additional models were explored by individually adding variables with potential confounding effects, but each of these led to lack of convergence. In the sensitivity analysis, age at diagnosis and educational level of patients with HNC were included but did not produce different findings or improve the fitting of the model. Therefore, the final model was limited to race, region, and health status. Of these, only Asian race remained independently associated with total expenses. In addition, several categorical variables showed substantial variability of expenses between groups but with wide 95% CIs that included 1. For example, median expenses were less for black individuals ($5313) than white individuals ($10 078), and individuals within 1 year of their HNC diagnosis also had higher median expenses ($18 113 vs $8476).
Individual Factors Associated With the Relative Expenses of Patients With HNC
Relative out-of-pocket expenses varied widely (median, 4.03%; range, 0%-916%). As expected, higher total income and higher income rating on the poverty index were associated with lower relative expenses (Table 3). Other variables associated with higher relative expenses were region, unemployment, public insurance, and lower health status. Relative expenses also varied by education; however, the wide CI reduced the ability to make conclusions regarding the association between educational level on out-of-pocket expenses. A multivariable model was constructed using important variables identified based on our study design; however, insurance and poverty level were removed sequentially because of a lack of convergence. Ultimately, income, sex, employment, and health status were included in the final model, but none were independently associated with relative out-of-pocket expenses.
Table 3. Factors Associated With Out-of-Pocket Medical Expenses Relative to Income: Results of Generalized Linear Model.
| Factor | Median Relative Out-of Pocket Expenses, % (95%CI) | β (95% CI) | |
|---|---|---|---|
| Univariable Model | Multivariable Model | ||
| Year of survey | NA | 0.98 (0.93-1.03) | NA |
| Age at diagnosis | NA | 1.01 (0.97-1.05) | NA |
| HNC follow-up, y | |||
| ≤1 | 3.24 (0.0-9.97) | 1 [Reference] | NA |
| >1 | 3.24 (1.37-5.12) | 0.92 (0.50-1.68) | NA |
| Age at survey | NA | 0.99 (0.97-1.01) | NA |
| Marital status | |||
| Married | 4.09 (3.01-5.17) | 1 [Reference] | NA |
| Single | 3.46 (1.3-5.62) | 0.89 (0.31-2.57) | NA |
| Widowed or separated | 2.71 (1.22-4.2) | 0.67 (0.4-1.12) | NA |
| Race | |||
| White | 4.08 (3.06-5.1) | 1 [Reference] | NA |
| Black | 1.83 (0-4.02) | 0.70 (0.38-1.29) | NA |
| Asian | 4.10 (2.87-5.32) | 1.05 (0.58-1.93) | NA |
| Hispanic | 2.33 (0-5.49) | 1.32 (0.33-5.27) | NA |
| Sex | |||
| Male | 3.18 (2.24-4.11) | 1 [Reference] | 1 [Reference] |
| Female | 5.46 (2.01-8.92) | 1.69 (0.94-3.04) | 1.38 (0.39-4.89) |
| Region | |||
| Northeast | 1.56 (0.27-2.85) | 1 [Reference] | NA |
| Midwest | 3.27 (2.12-4.42) | 1.19 (0.64-2.21) | NA |
| South | 5.66 (3.99-7.34) | 2.82 (1.47-5.43) | NA |
| West | 3.03 (1.99-4.08) | 1.46 (0.67-3.18) | NA |
| Poverty levela | |||
| Poor | 13.07 (2.93-23.22) | 0.43 (0.21-0.85) | NA |
| Near poor | 6.84 (2.99-10.69) | ||
| Low income | 5.66 (0.46-10.86) | ||
| Middle income | 4.07 (2.69-5.45) | ||
| High income | 2.06 (0.96-3.16) | ||
| Total income (per $1000) | NA | 0.88 (0.83-0.94) | 0.89 (0.69-1.14) |
| Employment | |||
| Employed | 2.35 (1.25-3.45) | 1 [Reference] | 1 [Reference] |
| Unemployed | 5.13 (3.42-6.83) | 3.11 (1.79-5.42) | 0.87 (0.25-3.04) |
| Insurance | |||
| Any private | 2.87 (1.81-3.93) | 1 [Reference] | NA |
| Public only | 5.35 (2.76-7.94) | 1.89 (1.10-3.28) | NA |
| Uninsured | 5.12 (-1.28-11.52) | 1.73 (0.34-8.68) | NA |
| Educational level | 0.90 (0.37-2.23) | NA | |
| Less than high school | 6.50 (0-15.75) | NA | NA |
| High school graduate | 3.67 (0-9.48) | NA | NA |
| Beyond high school | 2.15 (0.67-3.63) | NA | NA |
| Health status | |||
| Poor | 10.20 (4.3-16.1) | 0.33 (0.16-0.65) | 0.63 (0.21-1.95) |
| Fair | 5.19 (1.73-8.65) | ||
| Good | 3.70 (2.72-4.68) | ||
| Very good | 2.48 (1.52-3.44) | ||
| Excellent | 1.58 (0.13-3.03) | ||
| Mental health status | |||
| Poor | 13.21 (NA) | 0.75 (0.24-2.34) | NA |
| Fair | 5.15 (0.82-9.47) | ||
| Good | 4.19 (1.95-6.44) | ||
| Very good | 3.30 (2.44-4.15) | ||
| Excellent | 3.50 (2.15-4.84) | ||
| van Walraven Index | NA | 1.01 (0.97-1.05) | NA |
| Charlson Comorbidity Index | NA | 1.04 (0.93-1.17) | NA |
Abbreviations: HNC, head and neck cancer; NA, not applicable.
Poverty levels are defined in the Data Source and Definitions subsection of the Methods section.
Discussion
It is increasingly important for practitioners and the health care system to understand the financial burden on patients and society. Individuals with HNC are expected to be particularly vulnerable to financial strains given the established association with lower socioeconomic status.6,7 This study, which used national data from nearly 2 decades, found that patients with HNC in the United States are uniquely disadvantaged compared with patients with other cancer in terms of poverty, educational level, and overall health. In addition, socioeconomic variables and geographic region were identified as risk factors associated with higher total medical expenditures and individual burden.
Patients with HNC are demographically distinct from patients with other cancers. Compared with the general population, patients with HNC are classically described as male, white, and middle-aged.31,32 This study provides perspective by comparing these patients with patients with other cancers and revealing that patients with HNC are more often of a minority race, less educated, poorer, sicker, and lacking private insurance, all of which can exacerbate existing socioeconomic disenfranchisement.33,34,35 On the basis of the MEPS data, patients with non-HNCs benefit from 23% higher median income compared with patients with HNC. Compounding this discrepancy, patients with HNC have higher medical expenses (median, $8101 vs $5930). This finding expands on prior literature that demonstrates higher HNC treatment costs9 by showing their overall medical expenses remain persistently elevated after the initial treatment period. Compared with the general population, patients with cancer have not only higher medical expenditures but also higher out-of-pocket costs.5,36 For patients with HNC, limited resources and higher expenses manifest as higher mean out-of-pocket expenses as a percentage of their income. In some cases, out-of-pocket medical expenses consume all a household’s income for a given year. Despite substantial changes during the past 2 decades in the treatment of HNC, the economy, and the health care system, these excess financial burdens have remained largely stable. The spike seen in relative out-of-pocket expenses in 2013 represents relatively high expenses and relatively low income among patients with HNC. This outlier year occurred during the initiation of Medicaid expansion in many states in 2014, which led to volatility in some public insurance markets and may explain the observed fluctuation in relative out-of-pocket expenses.37
Within patients with HNC, several demographic factors were associated with higher absolute and relative medical expenses. Some of these findings were expected: medical expenses were higher for those with lower health status and within the first year of HNC diagnosis, and relative expenses were greater among those with lower incomes. However, the observed variation by race, sex, and educational level highlight important disparities and are less readily explainable. Socioeconomic factors, especially race and insurance status, have been correlated with expenses for several disease categories.38,39,40,41 Reduced access to medical services among lower socioeconomic classes may contribute to these disparities.42 In particular, racial differences in access persist even after controlling for income and insurance.43 However, total expenses represent a complex summation of access, disease burden, and care setting, which all vary with demographics.42,44 For cancer populations, expenses may be driven partly by stage, which correlates with treatment costs and long-term rehabilitative needs.19,20 Unfortunately, demographics continue to serve as markers of stage of presentation, treatment, and survival in HNC31,45,46,47,48 and likely affect medical expenses through this mechanism.
Relative out-of-pocket expenses were used to assess the burden of medical expenses on the individual patient and family. Similar to total expenses, variability in this metric was associated with demographic, health, regional, and insurance differences. However, the variability in relative expenses appears to be explained primarily by the differences in income. In other words, the individual’s financial burden from out-of-pocket expenses depends more on income than health, demographics, or even insurance status. The paradoxical finding that insurance status does not protect against out-of-pocket costs may be attributable to less intensive treatments among those with inadequate insurance coverage. This would, unfortunately, also result in worse oncologic outcomes in these groups.49,50,51 These findings are important for practitioners discussing financial burden with patients, yet most oncologists are uncomfortable having these discussions52 despite the recommendations to discuss the financial implications of cancer with patients53 and patients’ desire to hear this information.54
For HNC, regional variation exists for absolute and relative medical expenses. Regional variation in medical costs was brought to public attention in 1973 by the Dartmouth Atlas study.55 Since then, regional differences are often cited as an example of unwarranted variability and are attributed to waste or disparities in care.56 For patients with HNC, MEPS data revealed higher costs in the Northeast followed by the South, West, and Midwest. Meanwhile, the highest relative out-of-pocket expenses were in the South. However, none of this variation remained when controlling for other factors. This finding suggests that variability in this case is attributable to the individual level rather than regional differences in the health care system based on the data available.
Strengths and Limitations
This study uses nationally representative medical expenditures from the MEPS database and benefits from the rigorous methods and quality controls used by the survey. The prevalence and demographic profile in the weighted estimates of the HNC population from the MEPS data are consistent with other national representative cancer databases, which supports the accuracy of the MEPS estimates.32,57 The scope of this survey facilitates comparisons to other cancer sites and could be used in future research to compare with noncancer cohorts. However, these data have limitations inherent to survey studies, such as nonresponse and recall bias. In addition, the breadth of the MEPS survey across disease conditions necessitates practical limitations on disease-specific details. As a result, HNC-specific details are lacking, such as stage, site, and treatment modality, which can affect costs.9 The patients identified in the HNC cohort were limited to survivors available to survey. Therefore, patients at higher risk for HNC mortality may be underrepresented, and the financial burden on their families would not be captured.
Conclusions
Many gaps remain in our understanding of the financial burden of HNC on individual families and society. Previous studies58,59 have estimated expenses directly attributable to an HNC cancer diagnosis, whereas this study focused on overall medical expenses. Further research is needed to assess the indirect financial costs to families and society as a whole. These costs may include rehabilitation, loss of personal and family income, and the inability to obtain future insurance coverage. An improved understanding is needed regarding the association of payer mix with expenses, outcomes, and disparities. This study sets a foundation for future research by establishing burdens unique to HNC and demonstrating variation within the HNC population that may not be justifiable.
References
- 1.de Moor JS, Mariotto AB, Parry C, et al. Cancer survivors in the United States: prevalence across the survivorship trajectory and implications for care. Cancer Epidemiol Biomarkers Prev. 2013;22(4):561-570. doi: 10.1158/1055-9965.EPI-12-1356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tangka FK, Trogdon JG, Richardson LC, Howard D, Sabatino SA, Finkelstein EA. Cancer treatment cost in the United States: has the burden shifted over time? Cancer. 2010;116(14):3477-3484. doi: 10.1002/cncr.25150 [DOI] [PubMed] [Google Scholar]
- 3.Mariotto AB, Yabroff KR, Shao Y, Feuer EJ, Brown ML. Projections of the cost of cancer care in the United States: 2010-2020. J Natl Cancer Inst. 2011;103(2):117-128. doi: 10.1093/jnci/djq495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Langa KM, Fendrick AM, Chernew ME, Kabeto MU, Paisley KL, Hayman JA. Out-of-pocket health-care expenditures among older Americans with cancer. Value Health. 2004;7(2):186-194. doi: 10.1111/j.1524-4733.2004.72334.x [DOI] [PubMed] [Google Scholar]
- 5.Himmelstein DU, Warren E, Thorne D, Woolhandler S. Illness and injury as contributors to bankruptcy. Health Aff (Millwood). 2005;(Suppl Web Exclusives):W5-63-W5-73. doi: 10.1377/hlthaff.W5.63 [DOI] [PubMed] [Google Scholar]
- 6.Johnson S, McDonald JT, Corsten MJ. Socioeconomic factors in head and neck cancer. J Otolaryngol Head Neck Surg. 2008;37(4):597-601. [PubMed] [Google Scholar]
- 7.Hwang E, Johnson-Obaseki S, McDonald JT, Connell C, Corsten M. Incidence of head and neck cancer and socioeconomic status in Canada from 1992 to 2007. Oral Oncol. 2013;49(11):1072-1076. doi: 10.1016/j.oraloncology.2013.08.002 [DOI] [PubMed] [Google Scholar]
- 8.Cohen EEW, LaMonte SJ, Erb NL, et al. American Cancer Society head and neck cancer survivorship care guideline. CA Cancer J Clin. 2016;66(3):203-239. doi: 10.3322/caac.21343 [DOI] [PubMed] [Google Scholar]
- 9.Jacobson JJ, Epstein JB, Eichmiller FC, et al. The cost burden of oral, oral pharyngeal, and salivary gland cancers in three groups: commercial insurance, Medicare, and Medicaid. Head Neck Oncol. 2012;4:15. doi: 10.1186/1758-3284-4-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Head and Neck Cancers. National Cancer Institute. https://www.cancer.gov/types/head-and-neck/head-neck-fact-sheet. Accessed July 13, 2017.
- 11.Cancer Facts & Figures 2017. https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/cancer-facts-figures-2017.html. Accessed February 13, 2017.
- 12.Jemal A, Ward EM, Johnson CJ, et al. Annual report to the nation on the status of cancer, 1975-2014, featuring survival. J Natl Cancer Inst. 2017;109(9). doi: 10.1093/jnci/djx030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lin SS, Massa ST, Varvares MA. Improved overall survival and mortality in head and neck cancer with adjuvant concurrent chemoradiotherapy in national databases. Head Neck. 2016;38(2):208-215. doi: 10.1002/hed.23869 [DOI] [PubMed] [Google Scholar]
- 14.Howlander N, Noone A, Krapcho M, Miller D, Bishop K. SEER Cancer Statistics Review, 1975-2014. Bethesda, MD: National Cancer Institute; 2015. [Google Scholar]
- 15.Lin BM, Wang H, D’Souza G, et al. Long-term prognosis and risk factors among patients with HPV-associated oropharyngeal squamous cell carcinoma. Cancer. 2013;119(19):3462-3471. doi: 10.1002/cncr.28250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ang KK, Harris J, Wheeler R, et al. Human papillomavirus and survival of patients with oropharyngeal cancer. N Engl J Med. 2010;363(1):24-35. doi: 10.1056/NEJMoa0912217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Epstein JD, Knight TK, Epstein JB, Bride MA, Nichol MB. Cost of care for early- and late-stage oral and pharyngeal cancer in the California Medicaid population. Head Neck. 2008;30(2):178-186. doi: 10.1002/hed.20670 [DOI] [PubMed] [Google Scholar]
- 18.Hollenbeak CS, Stack BC Jr, Daley SM, Piccirillo JF. Using comorbidity indexes to predict costs for head and neck cancer. Arch Otolaryngol Head Neck Surg. 2007;133(1):24-27. doi: 10.1001/archotol.133.1.24 [DOI] [PubMed] [Google Scholar]
- 19.Lang K, Menzin J, Earle CC, Jacobson J, Hsu M-A. The economic cost of squamous cell cancer of the head and neck: findings from linked SEER-Medicare data. Arch Otolaryngol Head Neck Surg. 2004;130(11):1269-1275. doi: 10.1001/archotol.130.11.1269 [DOI] [PubMed] [Google Scholar]
- 20.Kim Le T, Winfree KB, Yang H, et al. Treatment patterns and economic burden of metastatic and recurrent locally-advanced head and neck cancer patients. J Med Econ. 2012;15(4):786-795. doi: 10.3111/13696998.2012.682632 [DOI] [PubMed] [Google Scholar]
- 21.Wissinger E, Griebsch I, Lungershausen J, Foster T, Pashos CL. The economic burden of head and neck cancer: a systematic literature review. Pharmacoeconomics. 2014;32(9):865-882. doi: 10.1007/s40273-014-0169-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Coughlan D, Yeh ST, O’Neill C, Frick KD. Evaluating direct medical expenditures estimation methods of adults using the medical expenditure panel survey: an example focusing on head and neck cancer. Value Health. 2014;17(1):90-97. doi: 10.1016/j.jval.2013.10.004 [DOI] [PubMed] [Google Scholar]
- 23.Dwojak SM, Bhattacharyya N. Incremental and comparative health care expenditures for head and neck cancer in the United States. Laryngoscope. 2014;124(10):2305-2308. doi: 10.1002/lary.24795 [DOI] [PubMed] [Google Scholar]
- 24.Medical Expenditure Panel Survey Home page. https://meps.ahrq.gov/mepsweb/. Accessed November 22, 2017.
- 25.Cohen SB. Design strategies and innovations in the Medical Expenditure Panel Survey. Med Care. 2003;41(7)(suppl):III5-III12. doi: 10.1097/01.MLR.0000076048.11549.71 [DOI] [PubMed] [Google Scholar]
- 26.Quan H, Li B, Couris CM, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011;173(6):676-682. doi: 10.1093/aje/kwq433 [DOI] [PubMed] [Google Scholar]
- 27.van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care. 2009;47(6):626-633. doi: 10.1097/MLR.0b013e31819432e5 [DOI] [PubMed] [Google Scholar]
- 28.Sharabiani MTA, Aylin P, Bottle A. Systematic review of comorbidity indices for administrative data. Med Care. 2012;50(12):1109-1118. doi: 10.1097/MLR.0b013e31825f64d0 [DOI] [PubMed] [Google Scholar]
- 29.Fleishman JA, Cohen JW. Using information on clinical conditions to predict high-cost patients. Health Serv Res. 2010;45(2):532-552. doi: 10.1111/j.1475-6773.2009.01080.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mihaylova B, Briggs A, O’Hagan A, Thompson SG. Review of statistical methods for analysing healthcare resources and costs. Health Econ. 2011;20(8):897-916. doi: 10.1002/hec.1653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Choi SH, Terrell JE, Fowler KE, et al. Socioeconomic and other demographic disparities predicting survival among head and neck cancer patients. PLoS One. 2016;11(3):e0149886. doi: 10.1371/journal.pone.0149886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Weatherspoon DJ, Chattopadhyay A, Boroumand S, Garcia I. Oral cavity and oropharyngeal cancer incidence trends and disparities in the United States: 2000-2010. Cancer Epidemiol. 2015;39(4):497-504. doi: 10.1016/j.canep.2015.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Major JM, Doubeni CA, Freedman ND, et al. Neighborhood socioeconomic deprivation and mortality: NIH-AARP diet and health study. PLoS One. 2010;5(11):e15538. doi: 10.1371/journal.pone.0015538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rehkopf DH, Haughton LT, Chen JT, Waterman PD, Subramanian SV, Krieger N. Monitoring socioeconomic disparities in death: comparing individual-level education and area-based socioeconomic measures. Am J Public Health. 2006;96(12):2135-2138. doi: 10.2105/AJPH.2005.075408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fiscella K, Tancredi D. Socioeconomic status and coronary heart disease risk prediction. JAMA. 2008;300(22):2666-2668. doi: 10.1001/jama.2008.792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zafar SY, Peppercorn JM, Schrag D, et al. The financial toxicity of cancer treatment: a pilot study assessing out-of-pocket expenses and the insured cancer patient’s experience. Oncologist. 2013;18(4):381-390. doi: 10.1634/theoncologist.2012-0279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Caswell KJ, Waidmann T, Blumberg LJ. Financial burden of medical out-of-pocket spending by state and the implications of the 2014 Medicaid expansions. Inquiry. 2013;50(3):177-201. doi: 10.1177/0046958013516590 [DOI] [PubMed] [Google Scholar]
- 38.Ma S, Frick KD, Bleich S, Dubay L. Racial disparities in medical expenditures within body weight categories. J Gen Intern Med. 2012;27(7):780-786. doi: 10.1007/s11606-011-1983-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Xu KT, Borders TF. Racial and ethnic disparities in the financial burden of prescription drugs among older Americans. J Health Hum Serv Adm. 2007;30(1):28-49. [PubMed] [Google Scholar]
- 40.Wang J, Dong Z, Hong SH, Suda KJ. A comparison of direct medical costs across racial and ethnic groups among children with cancer. Curr Med Res Opin. 2008;24(3):847-858. doi: 10.1185/030079908X273390 [DOI] [PubMed] [Google Scholar]
- 41.Taylor AK, Larson S, Correa-de-Araujo R. Women’s health care utilization and expenditures. Womens Health Issues. 2006;16(2):66-79. doi: 10.1016/j.whi.2005.11.001 [DOI] [PubMed] [Google Scholar]
- 42.Unequal treatment: confronting racial and ethnic disparities in health care. Institute of Medicine. http://www.nationalacademies.org/hmd/Reports/2002/Unequal-Treatment-Confronting-Racial-and-Ethnic-Disparities-in-Health-Care.aspx. Accessed September 22, 2016.
- 43.Weinick RM, Zuvekas SH, Cohen JW. Racial and ethnic differences in access to and use of health care services, 1977 to 1996. Med Care Res Rev. 2000;57(suppl 1):36-54. doi: 10.1177/1077558700057001S03 [DOI] [PubMed] [Google Scholar]
- 44.Zuvekas SH, Taliaferro GS. Pathways to access: health insurance, the health care delivery system, and racial/ethnic disparities, 1996-1999. Health Aff (Millwood). 2003;22(2):139-153. doi: 10.1377/hlthaff.22.2.139 [DOI] [PubMed] [Google Scholar]
- 45.Osazuwa-Peters N, Christopher KM, Hussaini AS, Behera A, Walker RJ, Varvares MA. Predictors of stage at presentation and outcomes of head and neck cancers in a university hospital setting. Head Neck. 2016;38(suppl 1):E1826-E1832. doi: 10.1002/hed.24327 [DOI] [PubMed] [Google Scholar]
- 46.Daraei P, Moore CE. Racial disparity among the head and neck cancer population. J Cancer Educ. 2015;30(3):546-551. doi: 10.1007/s13187-014-0753-4 [DOI] [PubMed] [Google Scholar]
- 47.Osazuwa-Peters N, Massa ST, Christopher KM, Walker RJ, Varvares MA. Race and sex disparities in long-term survival of oral and oropharyngeal cancer in the United States. J Cancer Res Clin Oncol. 2016;142(2):521-528. doi: 10.1007/s00432-015-2061-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Naghavi AO, Echevarria MI, Strom TJ, et al. Treatment delays, race, and outcomes in head and neck cancer. Cancer Epidemiol. 2016;45:18-25. doi: 10.1016/j.canep.2016.09.005 [DOI] [PubMed] [Google Scholar]
- 49.Abdelsattar ZM, Hendren S, Wong SL. The impact of health insurance on cancer care in disadvantaged communities. Cancer. 2017;123(7):1219-1227. doi: 10.1002/cncr.30431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Halpern MT, Ward EM, Pavluck AL, Schrag NM, Bian J, Chen AY. Association of insurance status and ethnicity with cancer stage at diagnosis for 12 cancer sites: a retrospective analysis. Lancet Oncol. 2008;9(3):222-231. doi: 10.1016/S1470-2045(08)70032-9 [DOI] [PubMed] [Google Scholar]
- 51.Inverso G, Mahal BA, Aizer AA, Donoff RB, Chuang S-K. Health insurance affects head and neck cancer treatment patterns and outcomes. J Oral Maxillofac Surg. 2016;74(6):1241-1247. doi: 10.1016/j.joms.2015.12.023 [DOI] [PubMed] [Google Scholar]
- 52.Schrag D, Hanger M. Medical oncologists’ views on communicating with patients about chemotherapy costs: a pilot survey. J Clin Oncol. 2007;25(2):233-237. doi: 10.1200/JCO.2006.09.2437 [DOI] [PubMed] [Google Scholar]
- 53.Meropol NJ, Schrag D, Smith TJ, et al. ; American Society of Clinical Oncology . American Society of Clinical Oncology guidance statement: the cost of cancer care. J Clin Oncol. 2009;27(23):3868-3874. doi: 10.1200/JCO.2009.23.1183 [DOI] [PubMed] [Google Scholar]
- 54.Bullock AJ, Hofstatter EW, Yushak ML, Buss MK. Understanding patients’ attitudes toward communication about the cost of cancer care. J Oncol Pract. 2012;8(4):e50-e58. doi: 10.1200/JOP.2011.000418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wennberg J, Gittelsohn. Small area variations in health care delivery. Science. 1973;182(4117):1102-1108. doi: 10.1126/science.182.4117.1102 [DOI] [PubMed] [Google Scholar]
- 56.Committee on Geographic Variation in Health Care Spending and Promotion of High-Value Care; Board on Health Care Services; Institute of Medicine; Newhouse JP, Garber AM, Graham RP, McCoy MA, Mancher M, Kibria A, eds. Variation in Health Care Spending: Target Decision Making, Not Geography. Washington, DC: National Academies Press; 2013. doi: 10.17226/18393 [DOI] [PubMed] [Google Scholar]
- 57.Warnakulasuriya S. Global epidemiology of oral and oropharyngeal cancer. Oral Oncol. 2009;45(4-5):309-316. doi: 10.1016/j.oraloncology.2008.06.002 [DOI] [PubMed] [Google Scholar]
- 58.Jo C. Cost-of-illness studies: concepts, scopes, and methods. Clin Mol Hepatol. 2014;20(4):327-337. doi: 10.3350/cmh.2014.20.4.327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.van Baal PHM, Wong A, Slobbe LCJ, Polder JJ, Brouwer WBF, de Wit GA. Standardizing the inclusion of indirect medical costs in economic evaluations. Pharmacoeconomics. 2011;29(3):175-187. doi: 10.2165/11586130-000000000-00000 [DOI] [PubMed] [Google Scholar]