Key Points
Question
What is the association among a county’s economy, clinician supply, and neonatal abstinence syndrome?
Findings
In this retrospective repeated cross-sectional study that included 580 US counties and 6 302 497 births, there was a significant association with county-level rates of neonatal abstinence syndrome and county 10-year unemployment rate (adjusted incidence rate ratio, 1.11) and designation as a mental health clinician shortage area (adjusted incidence rate ratio, 1.17).
Meaning
Long-term unemployment and shortage of mental health clinicians were associated with higher rates of neonatal abstinence syndrome on a county level.
Abstract
Importance
Neonatal abstinence syndrome (NAS) has increased over the last 2 decades, but limited data exist on its association with economic conditions or clinician supply.
Objective
To determine the association among long-term unemployment, clinician supply (as assessed by primary care and mental health clinician shortage areas), and rates of NAS and evaluate how associations differ based on rurality.
Design, Setting, and Participants
Ecological time-series analysis of a retrospective, repeated cross-sectional study using outcome data from all 580 counties in Florida, Kentucky, Massachusetts, Michigan, New York, North Carolina, Tennessee, and Washington from 2009 to 2015 and economic data from 2000 to 2015. Negative binomial models were used with year and county-level fixed effects. Interactions were tested and stratified analyses were conducted by metropolitan counties, rural counties adjacent to metropolitan counties, and rural remote counties.
Exposures
County-level 10-year unemployment rate and mental health and primary care clinician supply obtained from the Health Resources and Services Administration Area Health Resources Files.
Main Outcomes and Measure
Rates of NAS, excluding iatrogenic withdrawal, obtained from state inpatient databases.
Results
The sample included observations from 580 counties over 7 years (1803 county-years from metropolitan counties, 1268 county-years from rural counties adjacent to metropolitan counties, and 927 county-years from rural remote counties). During the study period, there were 6 302 497 births and 47 224 diagnoses of NAS. The median rate of NAS was 7.1 per 1000 hospital births (interquartile range [IQR], 2.2-15.8), the 10-year unemployment rate was 7.6% (IQR, 6.4%-9.0%), and 83.9% of county-years were partial or complete mental health shortage areas. In the adjusted analyses, mental health shortage areas had higher NAS rates (unadjusted rate in shortage areas of 14.0 per 1000 births vs unadjusted rate in nonshortage areas of 10.6 per 1000 births; adjusted incidence rate ratio [IRR], 1.17 [95% CI, 1.07-1.27]), occurring primarily in metropolitan counties (adjusted IRR, 1.28 [95% CI, 1.16-1.40]; P = .02 for test of equivalence between metropolitan counties and rural counties adjacent to metropolitan counties). There was no significant association between primary care shortage areas and rates of NAS. The 10-year unemployment rate was associated with higher rates of NAS (unadjusted rate in highest unemployment quartile of 20.1 per 1000 births vs 7.8 per 1000 births in lowest unemployment quartile; adjusted IRR, 1.11 [95% CI, 1.00-1.23]) occurring primarily in rural remote counties (adjusted IRR, 1.34 [95% CI, 1.05-1.70]; P = .04 for test of equivalence between metropolitan counties and rural remote counties).
Conclusions and Relevance
In this ecological analysis of counties in 8 US states, there was a significant association among higher long-term unemployment, higher mental health clinician shortage areas, and higher county-level rates of neonatal abstinence syndrome.
This population epidemiology study assesses the association of US county-level long-term unemployment, primary care and mental health clinician supply, and urban vs rural status with rates of neonatal abstinence syndrome (NAS).
Introduction
From 1999 to 2014, there was an increase in opioid use in the United States.1,2,3,4 Increased use of opioid analgesics, heroin, and fentanyl was associated with increased rates of opioid overdose deaths.5 Although the crisis affects communities throughout the United States, opioid use disproportionately affects impoverished rural counties.6,7 Rural counties may be particularly at risk for opioid-related complications because residents often have poor access to health care, lack economic opportunity, and have diminished social capital, which are all factors associated with opioid-related mortality.8,9
The effects of the opioid crisis on pregnant women and infants are of increasing concern. Chronic opioid use during pregnancy can result in neonatal abstinence syndrome (NAS), which is a type of neonatal drug withdrawal syndrome. Neonatal abstinence syndrome can occur after illicit opioid use (eg, heroin) or as an expected outcome from opioid agonist treatment (eg, methadone and buprenorphine).10 From 2000 to 2014, the US rate of NAS increased from 1.2 to 8.0 per 1000 hospital births.11,12,13 Similar to overdose deaths, the increases in NAS rates disproportionately occurred in rural, impoverished counties.6
Even though some adult opioid-related outcomes have been associated with adverse economic conditions,14 this association has not been evaluated for opioid-related complications in infants. Furthermore, few studies have evaluated the association between NAS rates and county-level health care infrastructure such as clinician supply. A better understanding of the association among community characteristics such as health care infrastructure and macroeconomic conditions and NAS is needed to inform community-level interventions aimed at improving opioid-related outcomes for these vulnerable populations.
To address this gap in the literature, data were used from 580 diverse counties in 8 states to examine the association among long-term unemployment, clinician supply (measured by primary care and mental health clinician shortage areas and number of obstetricians per population), and rates of NAS and evaluate how these associations may differ based on rurality.
Methods
Study Design
This retrospective time-series analysis of counties in Florida, Kentucky, Massachusetts, Michigan, New York, North Carolina, Tennessee, and Washington used a longitudinal data set created from repeated cross-sectional data for 2009 to 2015 from multiple public sources. The convenience sample of states was chosen to reflect variation in opioid-related outcomes, county characteristics, and macroeconomic conditions. New York data were available through 2014, whereas data for the remaining states were available for all years (2009-2015). The study was determined to be exempt by the institutional review boards of the Tennessee Department of Health and the Vanderbilt University Medical Center and was approved by the RAND institutional review board with a waiver of informed consent.
Data Sources
Outcome data for NAS were obtained using the Healthcare Cost and Utilization Project’s State Inpatient Databases and the Tennessee All-Payer Database. Additional county data were obtained from the Health Resources and Services Administration Area Health Resources Files. Historical county-level economic data were obtained from 2000 to 2015. Data for health professional shortage areas (HPSAs) were not available for 2014. We assumed the estimates in 2014 remained stable if the estimates were the same in 2013 and 2015 (97.8% for primary care HPSAs and 98.4% for mental health HPSAs), otherwise the 2013 estimates were carried forward. There were no other missing data.
Covariates
County-level covariates were chosen a priori with prespecified hypotheses to evaluate the association among rates of NAS, clinician supply, and macroeconomic conditions. To evaluate county clinician supply, we used data from the Area Health Resources Files regarding primary care and mental health HPSAs and the number of obstetricians per 1000 population. We generated separate county indicators for primary care and mental health HPSAs, combining partial and total HPSAs. We hypothesized that higher mental health clinician supply would be associated with decreased rates of NAS.
More mental health clinicians may increase access to medication treatment for opioid use disorder, potentially increasing rates of NAS.15 However, in 2017 an estimated 12% of individuals with substance use disorder received treatment,16 and most clinicians who are waivered from the Drug Addiction Treatment Act of 2000 treat relatively few patients17,18; therefore, any increase in NAS rate from medication treatment of opioid use disorder is likely to be quite modest.
However, individuals with mental health disorders are 3 times as likely to use opioid analgesics as individuals without such disorders,19 and individuals with poorly or untreated mental health disorders are more likely to misuse opioids or develop opioid use disorders.20,21 For these reasons, better access to mental health treatment is likely to reduce opioid misuse and development of comorbid opioid use disorder among individuals with mental health disorders prior to and during pregnancy, thereby decreasing rates of NAS.
In addition, because NAS may result from any opioid use, including misuse of opioid analgesics,22 we hypothesized that lower primary care clinician supply would be associated with lower rates of NAS from less availability of opioid analgesics.23 Obstetrician supply may have 2 counteracting effects: more obstetricians may lead to greater opioid analgesic availability, increasing NAS rates, but may also increase prenatal care access, preventing opioid-related high-risk behaviors and, thus, lowering NAS rates.
To examine the hypotheses based on previous literature8,9,24 that adverse economic conditions, including high unemployment, percentage of residents below the poverty line, and a greater proportion of manufacturing jobs would be associated with higher NAS rates, we used data from the Area Health Resources Files on unemployment and poverty rates and manufacturing employment.
To investigate how these covariates may be modified by rurality, counties were designated using Rural-Urban Continuum Codes (1, 2, or 3 were designated as living in a metropolitan county; 4, 6, or 8, rural county adjacent to metropolitan county; and 5, 7, or 9, rural remote county; eMethods in the Supplement). Because rural county residents may be at risk for opioid-related complications from poorer access to health care, a lack of economic opportunity, and diminished social capital,8,9 we hypothesized that economic and clinician workforce associations with NAS rates would be stronger with a greater degree of rurality.
Outcome
Neonatal abstinence syndrome occurs when maternal chronic opioid use continues until near the time of delivery.25 The annual rate of infants with NAS per 1000 hospital births per county was calculated using inpatient admissions identified with the International Classification of Diseases, Clinical Modification code 779.5 (ICD-9-CM) or P96.1 (ICD-10-CM). Iatrogenic NAS (neonatal withdrawal from medical treatment) was excluded using previously defined criteria.11,12 Hospital births were defined as inpatient admissions identified as “in-hospital.” Birth data were attributed to an infant’s county of residence instead of the county where the hospital delivery occurred.
Data Analysis
Descriptive statistics were calculated and the collinearity among the variables of interest was investigated. We then created multivariable negative binomial models of the county-level number of NAS births as a function of county-level characteristics and economic conditions using the county-level number of all births as the exposure. We chose negative binomial models in favor of Poisson models because of overdispersion.
We first sought to identify the enduring association of adverse economic conditions by evaluating unemployment changes during the prior decade (ie, 2000-2009). Variables that are in the causal pathway (eg, income) were excluded from the estimation for the full association between unemployment and rates of NAS. Our primary analysis included clinician supply (primary care and mental health HPSAs, obstetrician density), 10-year moving average unemployment rate (referred throughout as 10-year unemployment rate), proportion of manufacturing jobs, number of births per county, year, and county fixed effects. Second, because county fixed effects account for county-level characteristics that do not vary from year to year (eg, rurality), we tested interaction terms and conducted a stratified analysis by rurality (metropolitan counties, rural counties adjacent to metropolitan counties, and rural remote counties). The adjusted incidence rate ratios (IRRs) are reported and are based on a 1-unit change for dichotomous variables and a 1-SD change for continuous variables.
A series of sensitivity analyses were conducted to confirm the robustness of the results. First, we added poverty to the primary analysis, and then replaced the 10-year unemployment rate with a 10-year poverty rate. Poverty is correlated both with rates of unemployment and NAS and is on the causal pathway from unemployment to NAS; therefore, we excluded it from the primary analysis. Second, because 2015 New York data were unavailable, an analysis was conducted first excluding New York from the sample, and then another analysis was conducted limiting the study years to 2009-2014.
We also conducted tests for trend analyses on NAS rates, employment characteristics, income, clinician supply, and HPSAs. All testing was 2-sided and conducted using Stata version 15.0 (StataCorp) and R version 3.4.0 (R Core Team).
Results
From 2009 to 2015, the sample included observations from 3998 county-years (6 302 497 births and 47 224 diagnoses of NAS). There were 1803 county-years from metropolitan counties (5 590 647 births and 38 201 diagnoses of NAS), 1268 county-years from rural counties adjacent to metropolitan counties (500 006 births and 4962 diagnoses of NAS), and 927 county-years from rural remote counties (211 844 births and 4061 diagnoses of NAS). During the study period, the overall median NAS rate (per 1000 hospital births) increased from 3.2 to 14.5 in the counties examined (eFigures 1-5 in the Supplement).
From 2009 to 2015, the proportion of counties designated as primary care HPSAs increased from 76.6% to 85.3% and counties designated as mental health HPSAs increased from 79.5% to 88.2%. During this time span, the county-level proportion of manufacturing jobs decreased from 14.0% to 13.7% and the unemployment rate decreased from 11.0% to 6.0%. However, the 10-year unemployment rate increased during this period from 6.5% to 8.2% (P < .001 for trend for all rate changes; Table 1).
Table 1. Neonatal Abstinence Syndrome (NAS), Employment Characteristics, Clinician Supply, and Socioeconomic Characteristics for 580 Counties in 8 States Examined for 2009 to 2015a.
| All Years | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 |
P Value for Trend |
|
|---|---|---|---|---|---|---|---|---|---|
| Total No. of birthsb | 6 302 497 | 965 652 | 934 868 | 927 595 | 922 356 | 916 824 | 928 750 | 706 452 | |
| Total No. of NAS birthsb | 47 224 | 3784 | 4663 | 5831 | 6630 | 7851 | 9015 | 9450 | |
| NAS rate/1000 births, median (IQR)b | 7.1 (2.2-15.8) | 3.2 (0-7.7) | 4.3 (0.6-9.7) | 6.1 (2.0-12.5) | 7.1 (2.4-14.7) | 9.2 (3.9-18.5) | 10.0 (4.8-21.3) | 14.5 (7.0-32.3) | <.001 |
| Unemployment rate, median (IQR)c | |||||||||
| 10-y moving average, % | 7.6 (6.4-9.0) | 6.5 (5.3-7.9) | 7.1 (5.9-8.6) | 7.4 (6.4-9.0) | 7.7 (6.6-9.2) | 7.9 (6.9-9.3) | 8.0 (6.9-9.4) | 8.2 (7.2-9.6) | <.001 |
| Current year, % | 8.9 (7.3-11.0) | 11.0 (9.2-12.9) | 10.9 (9.2-12.7) | 10.2 (8.6-11.6) | 9.0 (7.8-10.4) | 8.4 (7.4-10.0) | 6.9 (6.1-8.2) | 6.0 (5.2-7.3) | <.001 |
| Proportion of manufacturing jobs, median (IQR), %c | 13.4 (8.1-18.7) | 14.0 (8.3-19.7) | 13.5 (8.1-19.0) | 13.3 (8.1-18.6) | 13.1 (7.9-18.3) | 13.2 (7.9-18.2) | 13.2 (7.8-18.1) | 13.7 (8.4-18.9) | <.001 |
| Proportion of population in poverty, median (IQR), %c | 17.2 (14.3-20.5) | 16.4 (13.4-19.7) | 16.9 (14.2-20.3) | 17.8 (14.6-21.2) | 17.6 (14.6-20.8) | 17.7 (14.7-21.0) | 17.2 (14.3-20.3) | 16.8 (14.2-20.0) | .054 |
| No. of obstetricians/1000 population, median (IQR)c | 0.5 (0-0.9) | 0.5 (0-0.9) | 0.5 (0-1.0) | 0.5 (0-0.9) | 0.5 (0-0.09) | 0.5 (0-0.9) | 0.4 (0-0.9) | 0.4 (0-0.9) | .12 |
| Health professional shortage area, mean (SD), %c | |||||||||
| Primary care | 81.7 (38.7) | 76.6 (42.4) | 80.2 (39.9) | 79.8 (40.2) | 82.8 (37.8) | 83.8 (36.9) | 83.8 (36.9) | 85.3 (35.4) | <.001 |
| Mental health | 83.9 (36.8) | 79.5 (40.4) | 80.7 (39.5) | 81.7 (38.7) | 83.8 (36.9) | 86.9 (33.8) | 86.9 (33.8) | 88.2 (32.3) | <.001 |
Abbreviation: IQR, interquartile range.
The total sample was composed of 3998 county observations, 1803 metropolitan counties, 1268 rural counties adjacent to metropolitan counties, and 927 rural remote counties.
Data were obtained from Agency for Healthcare Research and Quality Healthcare Utilization Project’s Statewide Inpatient Database and the Tennessee All-Payer Database.
Data were obtained from Health Resource Services Administration Area Health Resources Files.
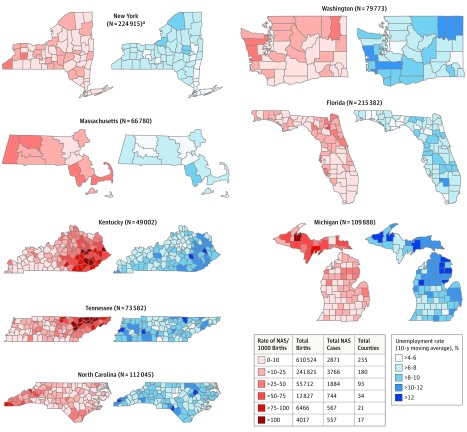
In 2015, there was substantial county-level variation in NAS rates ranging from 0 to greater than 100 per 1000 births (Figure; there was 1 county with a NAS rate of >250 per 1000 births). Similarly, counties varied substantially in 10-year unemployment rate, ranging from 4.1% to 15.8%. The NAS rates and 10-year unemployment rates overlapped (Figure), illustrating clustering of high rates of both in rural Appalachia (parts of the states of Kentucky, New York, North Carolina, and Tennessee), southeastern Massachusetts, northern Michigan, and southwestern Washington. An example of this association is Baraga County, Michigan, which reached a peak unemployment rate of approximately 24% in 2009 that decreased to 14% in 2013. This county’s NAS rate peaked at 113 per 1000 births in 2012, which was 3 years after unemployment peaked.
Figure. County Variation in Neonatal Abstinence Syndrome (NAS) per 1000 Hospital Births and 10-Year Moving Average Unemployment Rate for 2015.
Data are from an analysis of the Healthcare Cost and Utilization Project’s State Inpatient Databases, the Tennessee All-Payer Database, and the Health Resources and Services Administration Area Health Resources Files.
aData from New York are from 2014, which is the most recent year available.
Clinician Supply
Primary care and mental health clinician supply varied by location. There were primary care HPSAs in 79% of metropolitan counties, 84% of rural counties adjacent to metropolitan counties, and 85% of rural remote counties. Similarly, there were mental health HPSAs in 78% of metropolitan counties, 86% of rural counties adjacent to metropolitan counties, and 91% of rural remote counties.
The Pearson correlation coefficient between primary care HPSAs and poverty rates was 0.11 and between primary care HPSAs and 10-year unemployment rates was 0.14. The Pearson correlation coefficient between mental health HPSAs and poverty rates was 0.23 and between mental health HPSAs and 10-year unemployment rates was 0.29. There was no substantial difference when evaluating these relationships stratified by location (metropolitan counties, rural counties adjacent to metropolitan counties, and rural remote counties; eTable 1 in the Supplement).
In the unadjusted analyses, the NAS rates were higher in mental health HPSAs compared with non-HPSAs (overall: 14.0 vs 10.6 per 1000 births, respectively; metropolitan counties: 12.0 vs 9.9 per 1000 births; Table 2). In the multivariable overall model, county mental health HPSAs were associated with higher NAS rates than counties not designated as mental health HPSAs (adjusted IRR, 1.17 [95% CI, 1.07-1.27]).
Table 2. Associations Among Neonatal Abstinence Syndrome (NAS), County-Level Clinician Supply, and Rates for Unemployment and Manufacturing Jobsa.
| Overallb | Metropolitan Countiesc | Rural Counties Adjacent to Metropolitan Countiesc |
Rural Remote Countiesc | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| NAS Rate/ 1000 Births |
Adjusted IRR (95% CI)d |
P Value | NAS Rate/ 1000 Births |
Adjusted IRR (95% CI)d |
P Value | NAS Rate/ 1000 Births |
Adjusted IRR (95% CI)d |
P Value | NAS Rate/ 1000 Births |
Adjusted IRR (95% CI)d |
P Value | |
| Clinician Supply | ||||||||||||
| Primary care HPSAs | ||||||||||||
| Yes | 13.5 | 0.98 (0.89-1.08) | .73 | 10.9 | 0.91 (0.81-1.03) | .14 | 11.3 | 1.08 (0.88-1.33) | .45 | 21.2 | 1.07 (0.84-1.37) | .59 |
| No | 13.1 | 1 [Reference] | 13.8 | 1 [Reference] | 11.1 | 1 [Reference] | 14.4 | 1 [Reference] | ||||
| Mental health HPSAs | ||||||||||||
| Yes | 14.0 | 1.17 (1.07-1.27) | <.001 | 12.0 | 1.28 (1.16-1.40) | <.001e | 11.5 | 0.94 (0.75-1.18) | .59 | 20.6 | 1.01 (0.78-1.31) | .94 |
| No | 10.6 | 1 [Reference] | 9.9 | 1 [Reference] | 9.8 | 1 [Reference] | 15.5 | 1 [Reference] | ||||
| No. of obstetricians/1000 population | 0.32 (0.10-1.06) | .06 | 0.20 (0.04-1.04) | .06 | 1.06 (0.05-24.28) | .97 | 0.60 (0.07-5.51) | .66 | ||||
| Highest quartile | 10.5f | 8.8f | 9.2f | 16.1f | ||||||||
| Lowest quartile | 17.0f | 15.7f | 13.0f | 22.0f | ||||||||
| Employment Characteristics | ||||||||||||
| 10-y moving average unemployment rate | 1.11 (1.00-1.23) | .045 | 1.02 (0.89-1.16) | .82 | 0.96 (0.76-1.22) | .76 | 1.34 (1.05-1.70) | .02g | ||||
| Highest quartile, % | 20.1f | 14.8f | 14.9f | 28.1f | ||||||||
| Lowest quartile, % | 7.8f | 6.4f | 7.8f | 12.0f | ||||||||
| Proportion of manufacturing jobs | 1.01 (0.99-1.03) | .29 | 0.97 (0.95-1.00) | .06 | 1.00 (0.97-1.03) | .97 | 1.06 (1.02-1.10) | <.001 | ||||
| Highest quartile, % | 13.3f | 13.2f | 10.6f | 14.9f | ||||||||
| Lowest quartile, % | 12.0f | 7.7f | 9.2f | 26.1f | ||||||||
Abbreviations: HPSAs, health professional shortage areas; IRR, incidence rate ratio.
Models adjusted for county fixed effects, year fixed effects, and number of county births.
The overall sample includes 3998 county-years (6 302 497 births and 47 224 diagnoses of NAS).
There were 1803 county-years for the metropolitan counties (5 590 647 births and 38 201 diagnoses of NAS), 1268 county-years for the rural counties adjacent to metropolitan counties (500 006 births and 4962 diagnoses of NAS), and 927 county-years for the rural remote counties (211 844 births and 4061 diagnoses of NAS). Rural-Urban Continuum Codes: (1) metropolitan county with population greater than 1 million; (2) metropolitan county with population of 250 000 to 1 million; (3) metropolitan county with population less than 250 000; (4) rural county adjacent to metropolitan county with population greater than 20 000; (5) rural remote county with population greater than 20 000; (6) rural county adjacent to metropolitan county with population of 2500 to 19 999; (7) rural remote county with population of 2500 to 19 999; (8) rural county adjacent to metropolitan county with population less than 2500; and (9) rural remote county with population less than 2500.
The adjusted IRR is the estimated change in the outcome rate for a given change in the exposure variable (a change of 1 for dichotomous exposure variables and 1 SD for continuous variables). For example, the adjusted IRR of 1.11 for the 10-year moving average unemployment rate can be interpreted as follows: a 1 SD higher 10-year moving average unemployment rate (1 SD = 1.91 percentage points) relative to a reference county-year was associated with an 11% higher rate of NAS compared with the reference county.
P = .02 for test of equivalence between metropolitan counties and rural counties adjacent to metropolitan counties (eTable 2 in the Supplement).
Expressed as mean values.
P = .04 for test of equivalence between metropolitan counties and rural remote counties (eTable 2 in the Supplement).
When stratified analyses were conducted by rurality, mental health HPSAs were significantly associated with rates of NAS in metropolitan counties (adjusted IRR, 1.28 [95% CI, 1.16-1.40]; P = .02 for test of equivalence between metropolitan counties and rural counties adjacent to metropolitan counties; eTable 2 in the Supplement). Even though the adjusted IRRs for NAS rate and obstetrician density overall and in metropolitan counties were lower (ie, greater obstetrician density was associated with lower NAS rates) than for any other covariate examined, the NAS rates were not significantly associated with obstetrician density. The NAS rates also were not significantly associated with primary care HPSAs at the county level (Table 2).
County-Level Macroeconomic Factors
In unadjusted analyses, the mean rates of NAS were higher in counties with the highest quartile of unemployment compared with those in the lowest quartile of unemployment (overall rate: 20.1 vs 7.8 per 1000 births, respectively; rural remote counties: 28.1 vs 12.0 per 1000 births). In the adjusted analyses, the 10-year unemployment rate was associated with higher rates of NAS (adjusted IRR, 1.11 [95% CI, 1.00-1.23]; P = .045), but the proportion of manufacturing jobs was not significantly associated with the rates of NAS.
However, these findings differed based on county rurality. In the adjusted models, a higher 10-year unemployment rate was associated with higher rates of NAS in rural remote counties (adjusted IRR, 1.34 [95% CI, 1.05-1.70]; P = .04 for test of equivalence between metropolitan counties and rural remote counties). The association was not significant in metropolitan counties or in rural counties adjacent to metropolitan counties (Table 2 and eTable 2 in the Supplement).
In the unadjusted analyses, counties with a higher proportion of manufacturing jobs had lower mean rates of NAS in rural remote counties (14.9 per 1000 births in highest quartile of manufacturing jobs vs 26.1 per 1000 births in lowest quartile). However, in the adjusted analyses, a higher proportion of manufacturing jobs was associated with higher rates of NAS in rural remote counties (adjusted IRR, 1.06 [95% CI, 1.02-1.10]; P < .001 for equivalence of metropolitan counties and rural remote counties) but not in metropolitan counties or in metropolitan counties adjacent to rural counties (Table 2 and eTable 2 in the Supplement).
The results of the sensitivity analyses replacing the unemployment rate with the poverty rate, excluding New York, and limiting the analytic period to 2009-2014 were not significantly different than the main models (eTables 3-6 in the Supplement).
Discussion
Among 8 US states studied from 2009 to 2015, there was substantial variation across counties in NAS incidence, with rates often highest in rural remote counties. Although the complex contributors of the opioid crisis remain an area of debate in the existing literature,8,9,26 this study found higher rates of NAS to be associated with mental health HPSAs and high rates of long-term unemployment, with substantial differences in these associations between rural and metropolitan counties.
There is a lack of consensus regarding the complex association between the lack of economic opportunity in a county and the county’s drug environment, and how these factors (independently or combined) contribute to the extent of the opioid crisis in a given community.8,9,26 The association between NAS and opioid use is clear22; however, the findings suggest county macroeconomic conditions are also associated with this multifactorial problem, especially in rural counties. In this study, higher long-term unemployment rates were associated with higher rates of NAS, suggesting that both past and present economic conditions contribute to NAS rates.
Case and Deaton9 suggest that recent observed increases in morbidity and mortality, particularly among rural populations, may represent cumulative disadvantage, social isolation, and decline of marriage, resulting in a poor labor market and poor health outcomes. A recent federal report also found that higher county unemployment rates were associated with higher rates of opioid overdose deaths.27 In the adjusted analyses, the current study found that a higher 10-year unemployment rate was associated with a higher county NAS rate; however, this association was not observed in metropolitan counties. These findings are consistent with the thesis of Case and Deaton9 that lack of economic opportunity, particularly in rural counties, is associated with opioid-related complications.
A higher proportion of manufacturing jobs in rural counties was associated with higher rates of NAS, which is consistent with prior research finding higher opioid use in counties with more manufacturing.24 This could be the result of higher rates of injury, chronic pain, and disability experienced by many individuals working in manufacturing, factors that may contribute to greater opioid analgesic use,28,29 coupled with a relative lack of nonmanufacturing employment opportunities in those rural counties compared with less rural counties.
In this study, mental health HPSAs were associated with higher rates of NAS, particularly in metropolitan counties. Mental health disorders are a risk factor for opioid misuse, and opioid use disorder and mental health disorders are frequently comorbid, with a 2-fold increase in the odds of opioid use during pregnancy among women with depressive or anxiety disorders compared with those without these types of diagnoses.30 Untreated and undertreated mental health disorders increase the risk of opioid misuse and abuse16 and potentially help explain the finding of an association between mental health HPSAs and NAS rates. This finding occurred only in metropolitan counties, potentially representing metropolitan counties’ unique needs or the possibility that economic effects dominate workforce issues in rural remote counties. Furthermore, the use of mental health HPSAs as a measurement may be too crude a division to fully capture such workforce issues.
Future research could explore additional relationships between mental health workforce (eg, number of clinicians waivered from the Drug Addiction Treatment Act and the number of psychiatrists) and NAS rates. The contributors to the opioid crisis and NAS rates are complex and multifactorial; thus, the response to address the crisis of opioid-related complications in infants will require comprehensive efforts to address the range of contributors that are sensitive to the individual needs of the local community.
Limitations
This study has several limitations. First, the ecological design of this study and the absence of patient-level data limit the strength of inferences that can be drawn from the associations among the covariates of interest (eg, unemployment) and individual-level patient outcomes (eg, NAS).
Second, the hospital discharge data used to determine the NAS rates may be prone to misclassification bias; however, previous research indicates diagnostic codes for NAS have a high positive predictive value.22
Third, although this analysis attempted to account for multiple county-level factors potentially associated with NAS, it is possible that some important time-varying, county-level confounders were not included. This analysis did not attempt to examine the complex relationship and pathways among economic conditions (eg, loss of social capital, food insecurity, housing), use and misuse of different types of opioids (eg, heroin), and NAS rates. Furthermore, clinician supply is complex and may experience endogeneity due to omitted variables that characterize demand for their services (ie, clinicians may move to areas of high demand), potentially biasing the results toward the null.
Fourth, even though this study examined a diverse cohort of counties across 8 states and over 7 years, the findings may not generalize to other communities or periods.
Fifth, this analysis does not capture factors potentially influencing maternal access to care in local communities, including the availability of hospital-based obstetric services, federally qualified health centers, midwives, and family physicians that provide obstetric services.
Sixth, the study design allows an examination of the associations among the exposures of interest (eg, unemployment, clinician workforce) and NAS rates but cannot prove causation.
Seventh, given some studies suggest that a small proportion of clinicians write a large volume of opioid prescriptions,31 primary care HPSAs may not accurately reflect opioid prescribing.
Eighth, the proportion of counties designated as mental health HPSAs was high for all locations examined (metropolitan counties, rural counties adjacent to metropolitan counties, and rural remote counties), and the limited variability among counties may have affected the estimation of an association with NAS rates.
Conclusions
In this ecological analysis of counties in 8 US states, there was a significant association among higher long-term unemployment, higher mental health clinician shortage areas, and higher county-level rates of neonatal abstinence syndrome.
eMethods. Geographic Definitions
eTable 1. Pearsons Correlations Between 10-Year Moving Average of Unemployment and Poverty with Primary Care and Mental Health Shortage Areas
eTable 2. P-Values for Interaction Terms of Exposures of Interest and Metro, Rural-Adjacent and Rural Remote Counties
eTable 3. Primary model with 10-Year Moving Average of Unemployment Rate & Current Poverty Rate
eTable 4. Primary Model with 10-Year Moving Average of Poverty Rate
eTable 5. Primary model with 10-Year Moving Average of Unemployment Rate, excluding New York State, 2009-2015
eTable 6. Primary model with 10-Year Moving Average of Unemployment Rate, Full Sample of States, 2009-2014
eFigure 1. Rates of Neonatal Abstinence Syndrome per 1000 Hospital Births, Florida 2009-2015
eFigure 2. Rates of Neonatal Abstinence Syndrome per 1000 Hospital Births, Michigan 2009-2015
eFigure 3. Rates of Neonatal Abstinence Syndrome per 1000 Hospital Births, Massachusetts and New York 2009-2015
eFigure 4. Rates of Neonatal Abstinence Syndrome per 1000 Hospital Births, Kentucky, Tennessee, North Carolina 2009-2015
eFigure 5. Rates of Neonatal Abstinesults of quality assessment per study ence Syndrome per 1000 Hospital Births, Washington 2009-2015
References:
- 1.Centers for Disease Control and Prevention (CDC) Vital signs: overdoses of prescription opioid pain relievers—United States, 1999-2008. MMWR Morb Mortal Wkly Rep. 2011;60(43):1487-1492. [PubMed] [Google Scholar]
- 2.Peterson AB, Gladden RM, Delcher C, et al. Increases in fentanyl-related overdose deaths—Florida and Ohio, 2013-2015. MMWR Morb Mortal Wkly Rep. 2016;65(33):844-849. [DOI] [PubMed] [Google Scholar]
- 3.Rudd RA, Paulozzi LJ, Bauer MJ, et al. Increases in heroin overdose deaths—28 states, 2010 to 2012. MMWR Morb Mortal Wkly Rep. 2014;63(39):849-854. [PMC free article] [PubMed] [Google Scholar]
- 4.Rudd RA, Aleshire N, Zibbell JE, Gladden RM. Increases in drug and opioid overdose deaths—United States, 2000-2014. MMWR Morb Mortal Wkly Rep. 2016;64(50-51):1378-1382. [DOI] [PubMed] [Google Scholar]
- 5.Hedegaard H, Warner M, Miniño AM. Drug overdose deaths in the United States, 1999-2016. NCHS Data Brief. 2017;(294):1-8. [PubMed] [Google Scholar]
- 6.Villapiano NL, Winkelman TN, Kozhimannil KB, et al. Rural and urban differences in neonatal abstinence syndrome and maternal opioid use, 2004 to 2013. JAMA Pediatr. 2017;171(2):194-196. [DOI] [PubMed] [Google Scholar]
- 7.Guy GP Jr, Zhang K, Bohm MK, et al. Vital signs: changes in opioid prescribing in the United States, 2006-2015. MMWR Morb Mortal Wkly Rep. 2017;66(26):697-704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Case A, Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc Natl Acad Sci U S A. 2015;112(49):15078-15083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Case A, Deaton A. Mortality and morbidity in the 21st century. Brookings Pap Econ Act. 2017;2017:397-476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jones HE, Kaltenbach K, Heil SH, et al. Neonatal abstinence syndrome after methadone or buprenorphine exposure. N Engl J Med. 2010;363(24):2320-2331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Patrick SW, Schumacher RE, Benneyworth BD, et al. Neonatal abstinence syndrome and associated health care expenditures. JAMA. 2012;307(18):1934-1940. [DOI] [PubMed] [Google Scholar]
- 12.Patrick SW, Davis MM, Lehmann CU, et al. Increasing incidence and geographic distribution of neonatal abstinence syndrome [published correction appears in J Perinatol. 2015;35(8):667]. J Perinatol. 2015;35(8):650-655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Winkelman TNA, Villapiano N, Kozhimannil KB, et al. Incidence and costs of neonatal abstinence syndrome among infants with Medicaid. Pediatrics. 2018;141(4):e20173520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hollingsworth A, Ruhm CJ, Simon K. Macroeconomic conditions and opioid abuse. J Health Econ. 2017;56:222-233. [DOI] [PubMed] [Google Scholar]
- 15.Rosenblatt RA, Andrilla CH, Catlin M, et al. Geographic and specialty distribution of US physicians trained to treat opioid use disorder. Ann Fam Med. 2015;13(1):23-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Substance Abuse and Mental Health Services Administration Results From the 2017 National Survey on Drug Use and Health: Summary of National Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2018. [Google Scholar]
- 17.Stein BD, Sorbero M, Dick AW, et al. Physician capacity to treat opioid use disorder with buprenorphine-assisted treatment. JAMA. 2016;316(11):1211-1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thomas CP, Doyle E, Kreiner PW, et al. Prescribing patterns of buprenorphine waivered physicians. Drug Alcohol Depend. 2017;181:213-218. [DOI] [PubMed] [Google Scholar]
- 19.Davis MA, Lin LA, Liu H, Sites BD. Prescription opioid use among adults with mental health disorders in the United States. J Am Board Fam Med. 2017;30(4):407-417. [DOI] [PubMed] [Google Scholar]
- 20.Martins SS, Keyes KM, Storr CL, et al. Pathways between nonmedical opioid use/dependence and psychiatric disorders. Drug Alcohol Depend. 2009;103(1-2):16-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Boscarino JA, Rukstalis M, Hoffman SN, et al. Risk factors for drug dependence among out-patients on opioid therapy in a large US health-care system. Addiction. 2010;105(10):1776-1782. [DOI] [PubMed] [Google Scholar]
- 22.Patrick SW, Dudley J, Martin PR, et al. Prescription opioid epidemic and infant outcomes. Pediatrics. 2015;135(5):842-850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McDonald DC, Carlson K, Izrael D. Geographic variation in opioid prescribing in the US. J Pain. 2012;13(10):988-996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cerdá M, Gaidus A, Keyes KM, et al. Prescription opioid poisoning across urban and rural areas. Addiction. 2017;112(1):103-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hudak ML, Tan RC; Committee on Fetus and Newborn, American Academy of Pediatrics . Neonatal drug withdrawal. Pediatrics. 2012;129(2):e540-e560. [DOI] [PubMed] [Google Scholar]
- 26.Ruhm CJ. Deaths of despair or drug problems? https://www.nber.org/papers/w24188. Accessed December 14, 2018.
- 27.Ghertner R, Groves L The opioid crisis and economic opportunity: geographic and economic trends. ASPE Research Brief. September 11, 2018;1-22.
- 28.Leff M, Stallones L, Keefe TJ, et al. Comparison of urban and rural non-fatal injury. Inj Prev. 2003;9(4):332-337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ives TJ, Chelminski PR, Hammett-Stabler CA, et al. Predictors of opioid misuse in patients with chronic pain. BMC Health Serv Res. 2006;6:46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Faherty LJ, Matone M, Passarella M, Lorch S. Mental health of mothers of infants with neonatal abstinence syndrome and prenatal opioid exposure. Matern Child Health J. 2018;22(6):841-848. [DOI] [PubMed] [Google Scholar]
- 31.Schneberk T, Raffetto B, Kim D, Schriger DL. The supply of prescription opioids. Ann Emerg Med. 2018;71(6):668-673.e3, e663. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods. Geographic Definitions
eTable 1. Pearsons Correlations Between 10-Year Moving Average of Unemployment and Poverty with Primary Care and Mental Health Shortage Areas
eTable 2. P-Values for Interaction Terms of Exposures of Interest and Metro, Rural-Adjacent and Rural Remote Counties
eTable 3. Primary model with 10-Year Moving Average of Unemployment Rate & Current Poverty Rate
eTable 4. Primary Model with 10-Year Moving Average of Poverty Rate
eTable 5. Primary model with 10-Year Moving Average of Unemployment Rate, excluding New York State, 2009-2015
eTable 6. Primary model with 10-Year Moving Average of Unemployment Rate, Full Sample of States, 2009-2014
eFigure 1. Rates of Neonatal Abstinence Syndrome per 1000 Hospital Births, Florida 2009-2015
eFigure 2. Rates of Neonatal Abstinence Syndrome per 1000 Hospital Births, Michigan 2009-2015
eFigure 3. Rates of Neonatal Abstinence Syndrome per 1000 Hospital Births, Massachusetts and New York 2009-2015
eFigure 4. Rates of Neonatal Abstinence Syndrome per 1000 Hospital Births, Kentucky, Tennessee, North Carolina 2009-2015
eFigure 5. Rates of Neonatal Abstinesults of quality assessment per study ence Syndrome per 1000 Hospital Births, Washington 2009-2015