This cohort study, part of the Transforming Research and Clinical Knowledge in Traumatic Brain Injury (TRACK-TBI) study, ascertains prevalence of and risk factors for posttraumatic stress disorder and major depressive disorder among patients evaluated in the emergency department for mild traumatic brain injury.
Key Points
Question
Who is at greatest risk for developing mental health problems such as posttraumatic stress disorder (PTSD) or major depression after sustaining a mild traumatic brain injury (mTBI)?
Findings
In this cohort study of 1155 patients with mTBI and 230 patients with orthopedic injuries not involving the head, patients with mTBI were more likely to report PTSD and/or major depressive symptoms 3 and 6 months after injury. Among patients with mTBI, a number of preinjury (eg, prior mental health problems) and injury-related (eg, assault or other violent cause of injury in the case of PTSD) characteristics were associated with increased risk of mental health problems.
Meaning
Injury to the brain is associated with new onset or exacerbation of preexisting mental health problems in a substantial minority of patients; knowledge of risk factors can inform efforts at prevention, screening, diagnosis, and improved treatment.
Abstract
Importance
Traumatic brain injury (TBI) has been associated with adverse mental health outcomes, such as posttraumatic stress disorder (PTSD) and major depressive disorder (MDD), but little is known about factors that modify risk for these psychiatric sequelae, particularly in the civilian sector.
Objective
To ascertain prevalence of and risk factors for PTSD and MDD among patients evaluated in the emergency department for mild TBI (mTBI).
Design, Setting, and Participants
Prospective longitudinal cohort study (February 2014 to May 2018). Posttraumatic stress disorder and MDD symptoms were assessed using the PTSD Checklist for DSM-5 and the Patient Health Questionnaire-9 Item. Risk factors evaluated included preinjury and injury characteristics. Propensity score weights-adjusted multivariable logistic regression models were performed to assess associations with PTSD and MDD. A total of 1155 patients with mTBI (Glasgow Coma Scale score, 13-15) and 230 patients with nonhead orthopedic trauma injuries 17 years and older seen in 11 US hospitals with level 1 trauma centers were included in this study.
Main Outcomes and Measures
Probable PTSD (PTSD Checklist for DSM-5 score, ≥33) and MDD (Patient Health Questionnaire-9 Item score, ≥15) at 3, 6, and 12 months postinjury.
Results
Participants were 1155 patients (752 men [65.1%]; mean [SD] age, 40.5 [17.2] years) with mTBI and 230 patients (155 men [67.4%]; mean [SD] age, 40.4 [15.6] years) with nonhead orthopedic trauma injuries. Weights-adjusted prevalence of PTSD and/or MDD in the mTBI vs orthopedic trauma comparison groups at 3 months was 20.0% (SE, 1.4%) vs 8.7% (SE, 2.2%) (P < .001) and at 6 months was 21.2% (SE, 1.5%) vs 12.1% (SE, 3.2%) (P = .03). Risk factors for probable PTSD at 6 months after mTBI included less education (adjusted odds ratio, 0.89; 95% CI, 0.82-0.97 per year), being black (adjusted odds ratio, 5.11; 95% CI, 2.89-9.05), self-reported psychiatric history (adjusted odds ratio, 3.57; 95% CI, 2.09-6.09), and injury resulting from assault or other violence (adjusted odds ratio, 3.43; 95% CI, 1.56-7.54). Risk factors for probable MDD after mTBI were similar with the exception that cause of injury was not associated with increased risk.
Conclusions and Relevance
After mTBI, some individuals, on the basis of education, race/ethnicity, history of mental health problems, and cause of injury were at substantially increased risk of PTSD and/or MDD. These findings should influence recognition of at-risk individuals and inform efforts at surveillance, follow-up, and intervention.
Introduction
It has been commonly assumed, even among many health care professionals, that mild traumatic brain injuries (mTBIs) virtually always resolve without sequelae.1 This assumption may contribute to these patients not receiving education about their injury at the time of injury and not receiving appropriate follow-up care after the acute injury.2,3,4 Whereas it is the case that symptoms in most patients with initial Glasgow Coma Scale (GCS) scores of 13 to 15 and negative computed tomography (CT) scan results do resolve in 1 to 3 months,3 studies show that some patients have symptoms that persist for months beyond the acute injury.5,6 In nearly 25 000 nonmedically evacuated US soldiers returning from Afghanistan or Iraq between 2009 and 2014 and screened for mTBI, a substantial proportion (10%-30%) of those who screened positive had symptoms that persisted for at least 3 months postinjury.7 These and other data in civilians indicate that for many patients with mTBI, their course is not inevitably one of improvement.8,9
Mental health problems may be particularly salient features of nonrecovery from mTBI.1,10 In civilian patients hospitalized for an orthopedic injury, presence of comorbid mTBI was associated with an increased risk for posttraumatic stress disorder (PTSD) and depression 3 to 6 months postinjury.11 Even among healthy young athletes, premorbid psychological factors have been found to be highly relevant to postconcussive recovery.12 Among 50 US soldiers with concussive blast traumatic brain injuries (TBIs) followed up for 1 to 5 years, many had posttraumatic stress (PTS) and depressive symptoms that worsened over time.13 Preexisting mental disorder14 and mental health sequelae have been shown to be important determinants of overall functioning and quality of life after mTBI.15,16,17,18 In US Army soldiers, deployment-related mTBI was associated with an increased risk for subsequent PTSD, as well as for major depressive disorder (MDD).19
Although MDD and PTSD are prevalent after TBI, little is known about which patients are at risk for developing them. In a study of 559 civilians consecutively admitted to a level 1 trauma center with TBI, preinjury history of MDD was associated with an increased risk for MDD.20 A retrospective review of medical records from 276 service members assigned to the United States Army Special Operations Command referred for mTBI evaluation found that premorbid PTS symptoms were associated with an increased risk for PTSD following a subsequent mTBI.21 In a 2017 systematic review of 26 observational studies of TBI, the authors found that female sex and preinjury depressive symptoms were predictive of MDD, whereas memory of the traumatic events and early PTS symptoms were predictive of PTSD.22
Taken together, these observations strongly suggest that mental health problems are common following a “mild” TBI and that there may be individual-specific and injury-specific factors that influence risk for these disorders. We hypothesized that factors (eg, antecedent mental disorder, prior TBI, cause of injury)23,24 observed in prior studies to increase risk for mental health and/or postconcussive symptoms, which are known to overlap with depressive and PTS symptoms,25,26 in patients with TBI would be predictive of PTSD and MDD status at 6 months postinjury, with similar risk factors observed at 3 and 12 months. To our knowledge, few studies have been designed and powered to ascertain prevalence of PTSD and MDD and examine hypothesized risk factors in a large, prospective longitudinal study of nonmilitary personnel. Given substantial differences in the nature and context of the injuries and postinjury circumstances of military and civilian personnel sustaining mTBIs,27 additional focus on these factors in a civilian cohort is needed.
Methods
Overview
Patients were enrolled at 11 academic level 1 trauma centers in the United States within 24 hours of injury, following evaluation in the emergency department (ED) for TBI as part of the prospective study, Transforming Research and Clinical Knowledge in Traumatic Brain Injury (TRACK-TBI).28 Data for this analysis come from the first 1352 adult patients with TBI enrolled between February 26, 2014, and May 4, 2016. Some analysis started in September 2017, and most analysis began in March 2018. The 1155 patients included in this analysis had GCS scores of 13 to 15 on arrival in the ED and received a CT scan per order of the evaluating ED physician. Glasgow Coma Scale scores of 13 to 15 are usually consistent with a diagnosis of mTBI; here we examine whether additional criteria for mTBI (per American Congress of Rehabilitation Medicine criteria for mTBI) including presence and duration of disturbance or loss of consciousness or posttraumatic amnesia are related to mental health outcomes. Other inclusion criteria included injury occurrence within 24 hours of admission, acute brain CT imaging ordered for clinical care purposes, and fluent in English or Spanish. Exclusion criteria included significant multiple trauma that would interfere with follow-up; penetrating TBI; prisoners or patients in custody; pregnancy; patients whose reason for being in the ED was for mandated psychiatric assessment; major debilitating mental (eg, schizophrenia, bipolar disorder) or neurological disorders (eg, stroke, dementia) or any other disorder that would interfere with assessment and follow-up or provision of informed consent; and current participation in a clinical therapeutic trial.
Patients were assessed at baseline (shortly after being seen in the ED) and at 2 weeks and 3, 6, and 12 months postinjury. An orthopedic trauma comparison group (n = 230) was enrolled partway through the study using identical inclusion and exclusion criteria with the exception that none were judged to have had a probable TBI on the basis of clinical history and ED admission GCS score. Follow-up on the orthopedic trauma comparison patients at the time of this report was only complete through the 6-month assessment.
All eligible individuals voluntarily agreed to participate and gave written informed consent. All study protocols were approved by the University of California, San Francisco, institutional review board and by the institutional review boards at all participating sites.
Measures
Glasgow Coma Scale
The GCS is a widely used measure of brain injury severity.29 The GCS score reported here was acquired at the time of presentation to the ED. All patients with mTBI in the analyses reported here had ED admission GCS scores of 13 to 15.
PTSD Checklist for DSM-5
The PTSD Checklist for DSM-5 (PCL-5) is a widely used measure of PTSD symptoms. The range of the scale is 0 to 80. Signal detection analyses against a clinical criterion standard revealed that PCL-5 scores of 31 to 33 were optimally efficient for diagnosing PTSD.30 We used scores of 33 or higher to indicate probable PTSD.
Patient Health Questionnaire–9
The Patient Health Questionnaire–9 (PHQ-9) is a 9-item self-report instrument widely used to measure depressive symptoms in primary care and other medical settings.31 The range of the scale is 0 to 27, and scores of 15 or higher are indicative of moderately severe to severe MDD. The PHQ-9 has been shown to function well as a measure of depression in those with TBI.32
Injury Characteristics and History of Mental Disorder
The TRACK-TBI assessment obtained from the respondent and the medical record information about the characteristics of the injury including (1) cause of injury (eg, motor vehicle collision, fall, other unintentional injury, assault); (2) occurrence and duration of disturbance or loss of consciousness; and (3) occurrence and duration of posttraumatic amnesia. Patients were hospitalized based on clinical indications as determined by the treating physicians and were recorded as (1) not hospitalized (ie discharged from the ED); (2) hospitalized outside of intensive care unit (ICU); or (3) hospitalized in ICU. In this cohort with ED GCS scores of 13 to 15, most ICU hospitalizations were for reasons other than the TBI per se, although at some sites it was common practice to admit patients with mTBI to the ICU solely for observation. The TRACK-TBI interview requested information from the respondent (acquired at baseline and in some cases collected from a patient relative or other suitable informant) about prior TBI(s) and history of mental disorder.
CT Scans
Computed tomography scans obtained within the first 25 hours of injury were available for the majority (missing in 25 of 1155 [2.2%]) of patients with mTBI. These scans were systematically read by an experienced neuroradiologist and for purposes of analysis here were categorized as either positive or negative (ie, no evidence of intracranial injury).
Statistical Analysis
Cross-sectional analyses were performed at each follow-up visit. Propensity weights using generalized boosted regression models33 were developed separately for patients with mTBI and orthopedic trauma and applied to account for missing data at follow-up visits. Weights-adjusted summaries were calculated for the PCL-5 and PHQ-9 outcomes. Comparisons were made between mTBI and orthopedic controls using weights-adjusted t tests for the continuous scores and weights-adjusted χ2 test for the binary diagnosis outcomes. Among patients with mTBI, weights-adjusted logistic regression models were fit to estimate the association of demographics and preinjury and injury characteristics with postinjury PTSD and depression. Multivariable significance was examined using design-based Wald χ2 tests. For the regression analyses, a 2-sided P value less than .005 was considered statistically significant, taking into account the multitude of comparisons made and the magnitude of associations.34 Sensitivity analyses were also performed using linear mixed-effects models to assess the effect of baseline risk factors on PCL-5 and PHQ-9 total scores at 3, 6, and 12 months postinjury. All statistical analyses were conducted in R, version 3.3.2 (R Foundation for Statistical Computing).
Results
A total of 1155 individuals with TBI were evaluated in the ED with an ED arrival GCS score of 13 to 15. The mean (SD) age was 40.5 (17.2) years, and the mean (SD) years of education was 13.6 (2.9). Of 1155 individuals, 752 (65.1%) were men, 881 (77.2%) were white, and 245 (21.4%) were Hispanic. A total of 239 patients (21%) had a psychiatric history. Table 1 summarizes the clinical characteristics of the mTBI sample. Also included in Table 1 are the 230 comparison patients with orthopedic trauma who were similar to the patients with mTBI on all characteristics with the exception of being less likely to report assault or other violence as their cause of injury (1% for orthopedic trauma patients vs 6% for patients with mTBI; P = .001 by Fisher exact test) and less likely to have been admitted to the ICU (7.4% for orthopedic trauma patients vs 24.5% for patients with mTBI; P < .001 by Fisher exact test).
Table 1. TRACK-TBI mTBI and Orthopedic Trauma Cohort Characteristicsa.
| Variable | No. (%) | |
|---|---|---|
| mTBI (n = 1155)b | Orthopedic Trauma (n = 230) | |
| Age, mean (SD), y | 40.5 (17.2) | 40.4 (15.6) |
| Education, mean (SD), y | 13.6 (2.9) | 13.8 (2.8) |
| Sex | ||
| Male | 752 (65.1) | 155 (67.4) |
| Female | 403 (34.9) | 75 (32.6) |
| Race/ethnicity | ||
| White | 881 (77.2) | 180 (80.4) |
| Black | 195 (17.1) | 35 (15.6) |
| Other | 66 (5.8) | 9 (4.0) |
| Hispanic | 245 (21.4) | 60 (26.7) |
| Non-Hispanic | 898 (78.6) | 165 (73.3) |
| Employment status | ||
| Working/homemaker/student | 878 (80.0) | 179 (81.0) |
| Retired | 89 (8.1) | 16 (7.2) |
| Unemployed/sick/disabled | 118 (10.7) | 22 (10.0) |
| Other or unspecified | 13 (1.2) | 4 (1.8) |
| Health insurance | ||
| Uninsured or Medicaid | 361 (32.9) | 75 (35.0) |
| Employer/private/medicare | 699 (63.8) | 129 (60.3) |
| Other | 36 (3.3) | 10 (4.7) |
| Patient type | ||
| ED discharge | 393 (34.0) | 82 (35.7) |
| Hospital admit no ICU | 479 (41.5) | 131 (57.0) |
| Hospital admit with ICU | 283 (24.5) | 17 (7.4) |
| Injury cause | ||
| Motor vehicle collision | 712 (61.8) | 82 (39.2) |
| Fall/other unintentional injury | 337 (29.2) | 102 (48.8) |
| Violence/assault | 70 (6.1) | 2 (1.0) |
| Unspecified | 34 (3.0) | 23 (11.0) |
| Loss of consciousness | ||
| No | 167 (14.5) | 230 (100.0) |
| Yes | 920 (79.6) | NA |
| Unknown | 68 (5.9) | NA |
| Intracranial injury on CT scan | ||
| No | 783 (69.3) | NA |
| Yes | 347 (30.7) | NA |
| Psychiatric history | ||
| No | 903 (79.1) | 166 (74.8) |
| Yes | 239 (20.9) | 56 (25.2) |
| Prior TBI | ||
| No | 802 (69.5) | 174 (75.7) |
| Yes | 352 (30.5) | 56 (24.4) |
Abbreviations: CT, computed tomography; ED, emergency department; ICU, intensive care unit; mTBI, mild traumatic brain injury; NA, not applicable; TRACK-TBI; Transforming Research and Clinical Knowledge in Traumatic Brain Injury; TBI, traumatic brain injury.
Data shown are raw numbers; sample sizes for variables may differ from the total owing to missing data.
Glasgow Coma Scale scores ranged from 13 to 15.
Table 2 summarizes weights-adjusted PCL-5 and PHQ-9 scores and corresponding rates of probable PTSD and probable moderately severe to severe MDD at each of the outcome assessment time points, all of which are significantly different between the mTBI and orthopedic comparison groups, with the exception of probable MDD at 6 months. Weights-adjusted prevalence of either MDD or PTSD in the 2 groups at 3 months was 20.0% (SE, 1.4%) vs 8.7% (SE, 2.2%) (P < .001) and at 6 months was 21.2% (SE, 1.5%) vs 12.1% (SE, 3.2%) (P = .03). Sensitivity analyses using higher and lower thresholds for case definitions yielded similar results (eTables 1 to 6 in the Supplement).
Table 2. Mental Health Outcomes at Follow-up Visitsa,b.
| Variable | 3 mo | 6 mo | 12 mo | |||
|---|---|---|---|---|---|---|
| mTBIc | Orthopedic Trauma | mTBIc | Orthopedic Trauma | mTBIc | Orthopedic Trauma | |
| PCL-5 Totald | ||||||
| No. | 842 | 165 | 809 | 148 | 750 | NA |
| Mean (SE) | 17.6 (0.6) | 12.2 (1.0) | 17.4 (0.6) | 13.7 (1.3) | 17.0 (0.7) | NA |
| Probable PTSD (SE), % | 18.7 (1.4) | 7.6 (2.1) | 19.2 (1.4) | 9.8 (2.8) | 17.2 (1.5) | NA |
| PHQ-9 Totale | ||||||
| No. | 867 | 167 | 823 | 150 | 759 | NA |
| Mean (SE) | 5.4 (0.2) | 4.2 (0.4) | 5.1 (0.2) | 4.0 (0.4) | 4.7 (0.2) | NA |
| Probable MDD (SE), % | 8.8 (1.0) | 3.0 (1.3) | 9.0 (1.0) | 5.5 (2.4) | 6.6 (0.9) | NA |
Abbreviations: MDD, major depressive disorder; mTBI, mild traumatic brain injury; NA, not applicable; PCL-5, PTSD Checklist for DSM-5; PHQ-9, Patient Health Questionnaire–9; PTSD, posttraumatic stress disorder.
All comparisons of mTBI vs orthopedic trauma comparison patient are statistically significant with P values ranging from <.001 to .023, except for comparison of probable MDD at 6 months (P = .26).
Values shown are raw numbers (sample sizes) and propensity weights–adjusted summaries.
Glasgow Coma Scale scores of 13 to 15.
PCL-5 total score was calculated as the sum of 20 individual items. Range was 0 to 80, and higher score indicates worse symptoms. Total score was prorated if less than 25% of the individual items were missing. Probable PTSD diagnosis was defined as PCL-5 total score 33 or higher.
PHQ-9 total score was calculated as the sum of 9 individual items. Range was 0-27, and higher score indicates worse symptoms. Probable MDD (moderately severe to severe depression) was defined as PHQ-9 total score 15 or higher. Data for this report are available for the orthopedic trauma comparison patients only through 6 months.
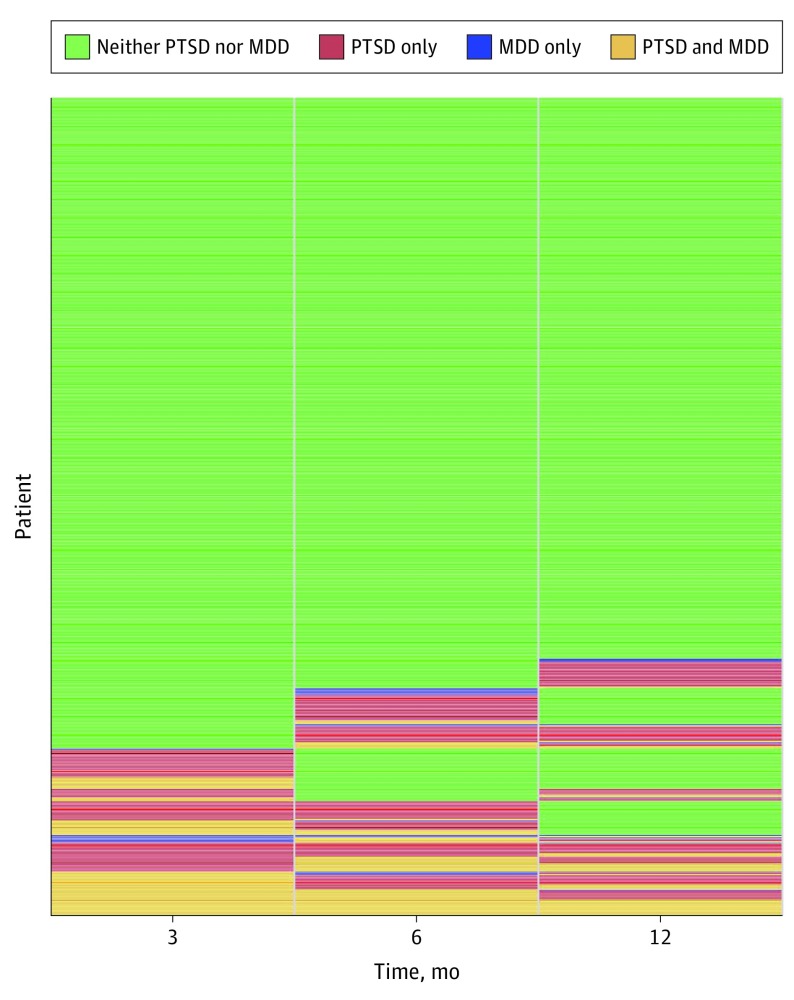
The Figure illustrates the status of patients with mTBI (628 individuals had complete data) over time with respect to meeting criteria for probable PTSD, MDD, both, or neither at 3, 6, and 12 months after mTBI. The most common outcome was having no disorder at any time (n = 431), followed by having both PTSD and MDD at all times (n = 62); all other possible combinations of outcomes were seen but less frequently.
Figure. Status of Individual Patients With Mild Traumatic Brain Injury at Each Outcome Assessment Time Point .
Data shown are for the 628 patients who completed all outcome assessments. MDD indicates major depressive disorder; PTSD, posttraumatic stress disorder.
Risk factors for probable PTSD and probable moderately severe to severe MDD at 6 months postinjury are summarized in Table 3 and Table 4, respectively. Models for 3- and 12-month outcomes were similar and are shown in eTables 7 to 10 in the Supplement. Longitudinal linear mixed-effects models for continuous PCL-5 (eTable 11 in the Supplement) and PHQ-9 scores (eTable 12 in the Supplement) were also consistent in identifying similar sets of predictors.
Table 3. Risk Factors for Probable PTSD at 6 Months Postinjury Among 671 Patients With Mild TBIa .
| Variable | AOR (95% CI) | χ2 | P Value |
|---|---|---|---|
| Age, y | 1.00 (0.98-1.01) | 0.26 | .61 |
| Sex | |||
| Male | 0.60 (0.38-0.96) | 4.64 | .03 |
| Female | 1 [Reference] | ||
| Race | |||
| Not black | 1 [Reference] | 31.28 | <.001 |
| Black | 5.11 (2.89-9.05) | ||
| Hispanic | |||
| No | 1 [Reference] | 3.63 | .06 |
| Yes | 1.95 (0.98-3.88) | ||
| Education, y | 0.89 (0.82-0.97) | 7.86 | .005 |
| Patient type | |||
| ED discharge | 1 [Reference] | 2.45 | .29 |
| Hospital admit no ICU | 1.39 (0.83-2.33) | ||
| Hospital admit with ICU | 1.68 (0.83-3.37) | ||
| Injury cause | |||
| Motor vehicle/fall/other unintentional injury | 1 [Reference] | 9.4 | .002 |
| Violence/assault | 3.43 (1.56-7.54) | ||
| Loss of consciousness | |||
| No | 1 [Reference] | 0.85 | .36 |
| Yes | 0.73 (0.38-1.42) | ||
| Posttraumatic amnesia | |||
| No | 1 [Reference] | 0.21 | .65 |
| Yes | 0.88 (0.50-1.54) | ||
| CT intracranial injury | |||
| No | 1 [Reference] | 2.14 | .14 |
| Yes | 0.65 (0.37-1.16) | ||
| Psychiatric history | |||
| No | 1 [Reference] | 21.64 | <.001 |
| Yes | 3.57 (2.09-6.09) | ||
| Prior TBI | |||
| No | 1 [Reference] | 4.16 | .04 |
| Yes | 1.63 (1.02-2.60) |
Abbreviations: AOR, adjusted odd ratio; CT, computed tomography; ED, emergency department; ICU, intensive care unit; PTSD, posttraumatic stress disorder; TBI, traumatic brain injury.
Using weights-adjusted multivariable logistic regression model.
Table 4. Risk Factors for Probable Moderately Severe to Severe Depression at 6 Months Postinjury Among 679 Patients With Mild TBIa .
| Variable | AOR (95% CI) | χ2 | P Value |
|---|---|---|---|
| Age, y | 1.00 (0.99-1.02) | 0.58 | .45 |
| Sex | |||
| Male | 0.71 (0.40-1.26) | 1.36 | .24 |
| Female | 1 [Reference] | ||
| Race | |||
| Not black | 1 [Reference] | 7.71 | .006 |
| Black | 2.79 (1.35-5.77) | ||
| Hispanic | |||
| No | 1 [Reference] | 1.70 | .19 |
| Yes | 1.82 (0.74-4.48) | ||
| Education, y | 0.91 (0.83-0.99) | 4.86 | .03 |
| Patient type | |||
| ED discharge | 1 [Reference] | 1.22 | .54 |
| Hospital admit no ICU | 0.72 (0.38-1.34) | ||
| Hospital admit with ICU | 0.98 (0.40-2.37) | ||
| Injury cause | |||
| Motor vehicle/fall/other unintentional injury | 1 [Reference] | 0.89 | .34 |
| Violence/assault | 1.63 (0.59-4.45) | ||
| Loss of consciousness | |||
| No | 1 [Reference] | 0.01 | .90 |
| Yes | 1.06 (0.42-2.65) | ||
| Posttraumatic amnesia | |||
| No | 1 [Reference] | 0.53 | .47 |
| Yes | 1.34 (0.61-2.95) | ||
| CT intracranial injury | |||
| No | 1 [Reference] | 0.03 | .87 |
| Yes | 1.06 (0.52-2.16) | ||
| Psychiatric history | |||
| No | 1 [Reference] | 16.24 | <.001 |
| Yes | 3.71 (1.96-7.03) | ||
| Prior TBI | |||
| No | 1 [Reference] | 3.37 | .07 |
| Yes | 1.71 (0.96-3.05) |
Abbreviations: AOR, adjusted odds ratio; CT, computed tomography; ED, emergency department; ICU, intensive care unit; TBI, traumatic brain injury.
Using weights-adjusted multivariable logistic regression model.
Statistically significant risk factors for probable PTSD at 6 months postinjury (Table 3) included less education (adjusted odds ratio [AOR], 0.89; 95% CI, 0.82-0.97 per year), being black (AOR, 5.11; 95% CI, 2.89-9.05), antecedent mental disorder (AOR, 3.57; 95% CI, 2.09-6.09), and injury resulting from assault or other violence (AOR, 3.43; 95% CI, 1.56-7.54). Prior TBI was also nominally associated with increased PTSD risk (AOR, 1.63; 95% CI 1.02-2.60), but this association did not reach our conservative level (ie, P < .005) of statistical significance. Risk factors for probable MDD (Table 4) were similar with the exception that cause of injury was not associated with increased risk. Other injury-related factors, such as duration of loss of consciousness or posttraumatic amnesia, evidence of brain injury on CT scan or hospitalization (± ICU) were not associated with PTSD or MDD risk. Sensitivity analyses that included additional indicators of socioeconomic status (ie, employment status and type of health insurance coverage) did not result in any material change to the strength of any of the above predictors (eTables 13 and 14 in the Supplement).
Discussion
In this study of patients with GCS scores of 13 to 15 seen in the ED at level 1 trauma centers in the United States and triaged to CT imaging, we observed that PTSD and MDD were relatively common, with 6-month rates ranging from 9% to 19%. Benchmarking to prior studies with similar designs, our 3- and 6-month prevalence of PTSD of 19% was somewhat higher than the 3-month and 6-month prevalence estimates of 9% reported in French35 and Dutch17 studies of patients with mTBI seen in the ED. Our 6-month prevalence of MDD of 9% was comparable with that of the Dutch ED study17 (7%) but somewhat lower than the 6-month prevalence of 21% reported in a US study of patients with TBI seen in the ED at a single level 1 trauma center.20 There is great variability in the approach to diagnosis and management of mTBI in the ED in Europe36 and, presumably, in other regions. This variability, along with differences in inclusion and exclusion criteria, assessment tools, and other measurement issues likely underlie the observed differences in prevalence estimates among these studies.
We also observed that patients with mTBI (many of whom also had extracranial injuries) experienced significantly more PTSD and, to a lesser extent, MDD postinjury than did patients with nonhead orthopedic injuries assessed using the same protocol. These findings are congruent with those of other studies that find more mental health problems among patients sustaining TBIs than other bodily injuries.11,37 They are also broadly consistent with other studies of psychological outcomes in patients with TBI, which find pervasive mental health sequelae.1,10 Traumatic brain injury (including mTBI) appears to be a forerunner to a host of neuropsychiatric disorders ranging from MDD to bipolar disorder to neurodegenerative disorders such as dementia38,39,40 and Parkinson disease.41,42 These observations suggest either that TBI is a risk factor for a variety of disparate pathological processes or that TBI increases risk for these disorders through a common mechanistic pathway. Mechanisms posited for the association between TBI and subsequent mental and neurodegenerative disorders include mechanical damage to white matter tracks linking frontocortical regulatory regions to other brain regions, neuroinflammation, and stress-related oxidative damage.25,43,44 Although we are unable to presently address mechanisms underlying the associations between mTBI and the mental health sequelae seen here, we are hopeful that future analyses of TRACK-TBI imaging and blood-based plasma biomarker measures may prove informative in this regard.
Consistent with prior work establishing that a history of MDD increases risk for MDD after TBI,20 we observed that having an antecedent mental health problem prior to TBI was an exceptionally strong risk factor for having PTSD or MDD postinjury. In some cases, this might be the continuation or exacerbation of a preinjury mental disorder, and in others it may be a new episode of mental disorder in someone who was well at the time of injury but had a more remote mental health history. Regrettably, our assessment protocol did not distinguish those 2 eventualities. However, in either case this finding underscores the importance of clinicians being aware of the mental health history of their patients with mTBI, as this information is central to expectations regarding both short-term and long-term outcome.45,46 The neural and behavioral underpinnings of vulnerability to TBI associated with antecedent mental disorders are not well understood, but further investigation may facilitate preventive strategies. In the meantime, awareness of the strong association of TBI involving assault or other violence with risk of PTSD postinjury should also influence decisions about surveillance and treatment planning, as discussed below.
The finding that cause of injury involving assault or violence was specifically associated with risk for PTSD but not MDD after mTBI is a novel finding of our research probably because most other studies have focused on either PTSD or MDD but not both, to our knowledge. This specificity of the association of violence with PTSD likely speaks to the importance of the contextual nature of the injury in determining subsequent psychopathology. Prevalence of mental health symptoms is relatively low following sport concussions12 compared with other sources of concussions, possibly owing to the low likelihood of perceiving the injury as life threatening. Future studies should attempt to obtain more granular information about beliefs and cognitions (eg, “I thought I would die,” or “I thought they would kill me”) associated with the injury,47 as these may help explain the variability in mental health outcomes and may themselves be grist for cognitive behavioral interventions.
Strengths and Limitations
Strengths of our study are the multisite sampling, the prospective longitudinal evaluation, the large sample size, and the standardization of our mental health outcome assessment. However, our study also has a number of limitations that should be considered when contextualizing our results. First, although the patients in this study were seen at 11 academic level 1 trauma centers across the United States, there is no guarantee that our findings are generalizable to other types of medical centers and other communities and countries. For example, patients whose acute injury features did not trigger a CT scan by the examining physician were not eligible for enrollment in this study. Second, although we used propensity score weighting to account for missingness at follow-up, this method accounts only for missingness associated with measured covariates. Third, we relied on patient (or family informant) report about prior TBI(s) and prior mental health problems, and recall or reporting biases may have influenced our results. Fourth, we are uncertain how to understand the finding that black individuals were at increased risk for mental disorders following mTBI, a finding that was not explainable on the basis of socioeconomic status (education, employment status, or health insurance type) or cause of injury. Unmeasured covariates may be part of the explanation; this is a topic needing further study. Fifth, our sample was too small to attempt to replicate population-based findings of an increase in suicide deaths in patients with TBI.48,49 Sixth, although we included a comparison group of patients admitted to the hospital with nonhead orthopedic injuries, nonconsecutive sampling and the nonrepresentative ratio of patients with TBI to non-TBI orthopedic injury weakens conclusions drawn from these comparisons. Furthermore, it is possible that poorly or unmeasured injury characteristics (eg, multiple trauma severity, treatment received for the injury) may materially differ from those of the patients with mTBI. We are therefore cautious about making claims that it is the brain injury, per se, that is driving the higher observed burden of mental illness in the patients with mTBI in our study. This, too, is a question for further research.
Another limitation of this work might be its focus on only 2 (PTSD and MDD) of many possibly consequential mental disorders. For example, insomnia has also been seen as a frequent contributor to functional impairment after TBI.16,50 Future work should delve deeper into a specific role for sleep problems (which are almost inevitably seen in PTSD and MDD) after mTBI. Sleep symptoms are often amenable to pharmacological or psychological interventions such as cognitive behavioral therapy51 and therefore may be a suitable therapeutic target. Such interventions have been developed to target sleep (and related symptoms) following TBI in returning combat veterans52,53 and may be suitable for nonmilitary settings as well.
Our findings may have implications for surveillance and treatment of mental disorders after TBI. The emergence and long-term course of PTSD after TBI is variable,54 and our findings show that PTSD and MDD, although common, occur in only a minority of patients post-mTBI but especially those with prior mental health problems. Consequently, we may want to consider watchful waiting (ie, active vigilance with planned follow-up) of patients with prior mental health problems and intervene when it is apparent that symptoms are persisting or worsening. In such situations, treatment with empirically supported interventions should be promptly initiated. Although some research indicates that selective serotonin reuptake inhibitors are not effective in the treatment of post-TBI major depression,55 the paucity of available evidence for what does work would suggest that selective serotonin reuptake inhibitors or other antidepressants and/or cognitive behavioral therapies would be worth trying on an individual patient-by-patient basis.56 Clearly, more work needs to be done to determine for whom such treatments are effective and to develop more broadly efficacious treatments.
Conclusions
Posttraumatic stress disorder and MDD are common sequelae of mTBI. Some individuals, on the basis of antecedent mental health status and—in the case of PTSD—context of injury (ie, assault or other violence), are at substantially increased risk of mental health problems following mTBI. These findings should influence recognition of at-risk individuals following mTBI and inform efforts at surveillance and intervention.
eTable 1. Sensitivity Analyses at PCL-5 ≥15 vs <15
eTable 2. Sensitivity Analyses at PCL-5 ≥40 vs <40
eTable 3. Sensitivity Analyses at PCL-5 ≥25 vs <25
eTable 4. Sensitivity Analyses at Varying PHQ-9 ≥15 vs <15
eTable 5. Sensitivity Analyses at Varying PHQ-9 ≥20 vs <20
eTable 6. Sensitivity Analyses at Varying PHQ-9 ≥10 vs <10
eTable 7. Risk factors for probable PTSD at 3 months post-injury among patients with mTBI (n=704)
eTable 8. Risk factors for probable PTSD at 12 months post-injury among patients with mTBI (n=619)
eTable 9. Risk factors for probable MDD at 3 months post-injury among patients with mTBI (n=724)
eTable 10. Risk factors for probable MDD at 12 months post-injury among patients with mTBI (n=626)
eTable 11. Longitudinal Model to assess risk factors on PCL-5 Total Score over time
eTable 12. Longitudinal Model to assess risk factors on PHQ-9 Total Score over time
eTable 13. Sensitivity analysis for 6-month PTSD outcome with additional SES predictors
eTable 14. Sensitivity analysis for 6-month MDD outcome with additional SES predictors
References
- 1.Maas AIR, Menon DK, Adelson PD, et al. ; InTBIR Participants and Investigators . Traumatic brain injury: integrated approaches to improve prevention, clinical care, and research. Lancet Neurol. 2017;16(12):987-1048. doi: 10.1016/S1474-4422(17)30371-X [DOI] [PubMed] [Google Scholar]
- 2.McMahon P, Hricik A, Yue JK, et al. ; TRACK-TBI Investigators . Symptomatology and functional outcome in mild traumatic brain injury: results from the prospective TRACK-TBI study. J Neurotrauma. 2014;31(1):26-33. doi: 10.1089/neu.2013.2984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Levin HS, Diaz-Arrastia RR. Diagnosis, prognosis, and clinical management of mild traumatic brain injury. Lancet Neurol. 2015;14(5):506-517. doi: 10.1016/S1474-4422(15)00002-2 [DOI] [PubMed] [Google Scholar]
- 4.Seabury SA, Gaudette É, Goldman DP, et al. Assessment of follow-up care after emergency department presentation for mild traumatic brain injury and concussion: results from the TRACK-TBI study. JAMA Netw Open. 2018;1(1):e180210. doi: 10.1001/jamanetworkopen.2018.0210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rabinowitz AR, Li X, McCauley SR, et al. Prevalence and predictors of poor recovery from mild traumatic brain injury. J Neurotrauma. 2015;32(19):1488-1496. doi: 10.1089/neu.2014.3555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dikmen S, Machamer J, Temkin N. Mild traumatic brain injury: longitudinal study of cognition, functional status, and post-traumatic symptoms. J Neurotrauma. 2017;34(8):1524-1530. doi: 10.1089/neu.2016.4618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schwab K, Terrio HP, Brenner LA, et al. Epidemiology and prognosis of mild traumatic brain injury in returning soldiers: a cohort study. Neurology. 2017;88(16):1571-1579. doi: 10.1212/WNL.0000000000003839 [DOI] [PubMed] [Google Scholar]
- 8.McCrea MA, Nelson LD, Guskiewicz K. Diagnosis and management of acute concussion. Phys Med Rehabil Clin N Am. 2017;28(2):271-286. doi: 10.1016/j.pmr.2016.12.005 [DOI] [PubMed] [Google Scholar]
- 9.Hiploylee C, Dufort PA, Davis HS, et al. Longitudinal study of postconcussion syndrome: not everyone recovers. J Neurotrauma. 2017;34(8):1511-1523. doi: 10.1089/neu.2016.4677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Radhakrishnan R, Garakani A, Gross LS, et al. Neuropsychiatric aspects of concussion. Lancet Psychiatry. 2016;3(12):1166-1175. doi: 10.1016/S2215-0366(16)30266-8 [DOI] [PubMed] [Google Scholar]
- 11.Roden-Foreman K, Solis J, Jones A, et al. Prospective evaluation of posttraumatic stress disorder and depression in orthopaedic injury patients with and without concomitant traumatic brain injury. J Orthop Trauma. 2017;31(9):e275-e280. doi: 10.1097/BOT.0000000000000884 [DOI] [PubMed] [Google Scholar]
- 12.Nelson LD, Tarima S, LaRoche AA, et al. Preinjury somatization symptoms contribute to clinical recovery after sport-related concussion. Neurology. 2016;86(20):1856-1863. doi: 10.1212/WNL.0000000000002679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mac Donald CL, Barber J, Jordan M, et al. Early clinical predictors of 5-year outcome after concussive blast traumatic brain injury. JAMA Neurol. 2017;74(7):821-829. doi: 10.1001/jamaneurol.2017.0143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Silverberg ND, Gardner AJ, Brubacher JR, Panenka WJ, Li JJ, Iverson GL. Systematic review of multivariable prognostic models for mild traumatic brain injury. J Neurotrauma. 2015;32(8):517-526. doi: 10.1089/neu.2014.3600 [DOI] [PubMed] [Google Scholar]
- 15.Pietrzak RH, Johnson DC, Goldstein MB, Malley JC, Southwick SM. Posttraumatic stress disorder mediates the relationship between mild traumatic brain injury and health and psychosocial functioning in veterans of Operations Enduring Freedom and Iraqi Freedom. J Nerv Ment Dis. 2009;197(10):748-753. doi: 10.1097/NMD.0b013e3181b97a75 [DOI] [PubMed] [Google Scholar]
- 16.Schiehser DM, Twamley EW, Liu L, et al. The relationship between postconcussive symptoms and quality of life in veterans with mild to moderate traumatic brain injury. J Head Trauma Rehabil. 2015;30(4):E21-E28. doi: 10.1097/HTR.0000000000000065 [DOI] [PubMed] [Google Scholar]
- 17.Haagsma JA, Scholten AC, Andriessen TM, Vos PE, Van Beeck EF, Polinder S. Impact of depression and post-traumatic stress disorder on functional outcome and health-related quality of life of patients with mild traumatic brain injury. J Neurotrauma. 2015;32(11):853-862. doi: 10.1089/neu.2013.3283 [DOI] [PubMed] [Google Scholar]
- 18.Porter KE, Stein MB, Martis B, et al. Postconcussive symptoms (PCS) following combat-related traumatic brain injury (TBI) in veterans with posttraumatic stress disorder (PTSD): influence of TBI, PTSD, and depression on symptoms measured by the neurobehavioral symptom inventory (NSI). J Psychiatr Res. 2018;102:8-13. doi: 10.1016/j.jpsychires.2018.03.004 [DOI] [PubMed] [Google Scholar]
- 19.Stein MB, Kessler RC, Heeringa SG, et al. ; Army STARRS collaborators . Prospective longitudinal evaluation of the effect of deployment-acquired traumatic brain injury on posttraumatic stress and related disorders: results from the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS). Am J Psychiatry. 2015;172(11):1101-1111. doi: 10.1176/appi.ajp.2015.14121572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bombardier CH, Fann JR, Temkin NR, Esselman PC, Barber J, Dikmen SS. Rates of major depressive disorder and clinical outcomes following traumatic brain injury. JAMA. 2010;303(19):1938-1945. doi: 10.1001/jama.2010.599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Manners JL, Forsten RD, Kotwal RS, Elbin RJ, Collins MW, Kontos AP. Role of pre-morbid factors and exposure to blast mild traumatic brain injury on post-traumatic stress in United States military personnel. J Neurotrauma. 2016;33(19):1796-1801. doi: 10.1089/neu.2015.4245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cnossen MC, Scholten AC, Lingsma HF, et al. Predictors of major depression and posttraumatic stress disorder following traumatic brain injury: a systematic review and meta-analysis. J Neuropsychiatry Clin Neurosci. 2017;29(3):206-224. doi: 10.1176/appi.neuropsych.16090165 [DOI] [PubMed] [Google Scholar]
- 23.Stein MB, Ursano RJ, Campbell-Sills L, et al. Prognostic indicators of persistent post-concussive symptoms after deployment-related mild traumatic brain injury: a prospective longitudinal study in U.S. Army soldiers. J Neurotrauma. 2016;33(23):2125-2132. doi: 10.1089/neu.2015.4320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cnossen MC, Winkler EA, Yue JK, et al. Development of a prediction model for post-concussive symptoms following mild traumatic brain injury: a TRACK-TBI pilot study [published online March 27, 2017]. J Neurotrauma. doi: 10.1089/neu.2017.5486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stein MB, McAllister TW. Exploring the convergence of posttraumatic stress disorder and mild traumatic brain injury. Am J Psychiatry. 2009;166(7):768-776. doi: 10.1176/appi.ajp.2009.08101604 [DOI] [PubMed] [Google Scholar]
- 26.Wilk JE, Herrell RK, Wynn GH, Riviere LA, Hoge CW. Mild traumatic brain injury (concussion), posttraumatic stress disorder, and depression in U.S. soldiers involved in combat deployments: association with postdeployment symptoms. Psychosom Med. 2012;74(3):249-257. doi: 10.1097/PSY.0b013e318244c604 [DOI] [PubMed] [Google Scholar]
- 27.Armistead-Jehle P, Soble JR, Cooper DB, Belanger HG. Unique aspects of traumatic brain injury in military and veteran populations. Phys Med Rehabil Clin N Am. 2017;28(2):323-337. doi: 10.1016/j.pmr.2016.12.008 [DOI] [PubMed] [Google Scholar]
- 28.Yue JK, Vassar MJ, Lingsma HF, et al. ; TRACK-TBI Investigators . Transforming research and clinical knowledge in traumatic brain injury pilot: multicenter implementation of the common data elements for traumatic brain injury. J Neurotrauma. 2013;30(22):1831-1844. doi: 10.1089/neu.2013.2970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Teasdale G, Jennett B. Assessment and prognosis of coma after head injury. Acta Neurochir (Wien). 1976;34(1-4):45-55. doi: 10.1007/BF01405862 [DOI] [PubMed] [Google Scholar]
- 30.Bovin MJ, Marx BP, Weathers FW, et al. Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition (PCL-5) in veterans. Psychol Assess. 2016;28(11):1379-1391. doi: 10.1037/pas0000254 [DOI] [PubMed] [Google Scholar]
- 31.Kroenke K, Spitzer RL, Williams JB, Löwe B. The patient health questionnaire somatic, anxiety, and depressive symptom scales: a systematic review. Gen Hosp Psychiatry. 2010;32(4):345-359. doi: 10.1016/j.genhosppsych.2010.03.006 [DOI] [PubMed] [Google Scholar]
- 32.Dyer JR, Williams R, Bombardier CH, Vannoy S, Fann JR. Evaluating the psychometric properties of 3 depression measures in a sample of persons with traumatic brain injury and major depressive disorder. J Head Trauma Rehabil. 2016;31(3):225-232. doi: 10.1097/HTR.0000000000000177 [DOI] [PubMed] [Google Scholar]
- 33.McCaffrey DF, Ridgeway G, Morral AR. Propensity score estimation with boosted regression for evaluating causal effects in observational studies. Psychol Methods. 2004;9(4):403-425. doi: 10.1037/1082-989X.9.4.403 [DOI] [PubMed] [Google Scholar]
- 34.Ioannidis JPA. The Proposal to Lower P Value Thresholds to. 005. JAMA. 2018;319(14):1429-1430. doi: 10.1001/jama.2018.1536 [DOI] [PubMed] [Google Scholar]
- 35.Lagarde E, Salmi LR, Holm LW, et al. Association of symptoms following mild traumatic brain injury with posttraumatic stress disorder vs postconcussion syndrome. JAMA Psychiatry. 2014;71(9):1032-1040. doi: 10.1001/jamapsychiatry.2014.666 [DOI] [PubMed] [Google Scholar]
- 36.Foks KA, Cnossen MC, Dippel DWJ, et al. Management of mild traumatic brain injury at the emergency department and hospital admission in Europe: a survey of 71 neurotrauma centers participating in the CENTER-TBI study [published online April 11, 2017]. J Neurotrauma. doi: 10.1089/neu.2016.4919 [DOI] [PubMed] [Google Scholar]
- 37.Bryant RA, O’Donnell ML, Creamer M, McFarlane AC, Clark CR, Silove D. The psychiatric sequelae of traumatic injury. Am J Psychiatry. 2010;167(3):312-320. doi: 10.1176/appi.ajp.2009.09050617 [DOI] [PubMed] [Google Scholar]
- 38.Nordström A, Nordström P. Traumatic brain injury and the risk of dementia diagnosis: a nationwide cohort study. PLoS Med. 2018;15(1):e1002496. doi: 10.1371/journal.pmed.1002496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Barnes DE, Kaup A, Kirby KA, Byers AL, Diaz-Arrastia R, Yaffe K. Traumatic brain injury and risk of dementia in older veterans. Neurology. 2014;83(4):312-319. doi: 10.1212/WNL.0000000000000616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fann JR, Ribe AR, Pedersen HS, et al. Long-term risk of dementia among people with traumatic brain injury in Denmark: a population-based observational cohort study. Lancet Psychiatry. 2018;5(5):424-431. doi: 10.1016/S2215-0366(18)30065-8 [DOI] [PubMed] [Google Scholar]
- 41.Perry DC, Sturm VE, Peterson MJ, et al. Association of traumatic brain injury with subsequent neurological and psychiatric disease: a meta-analysis. J Neurosurg. 2016;124(2):511-526. doi: 10.3171/2015.2.JNS14503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gardner RC, Byers AL, Barnes DE, Li Y, Boscardin J, Yaffe K. Mild TBI and risk of Parkinson disease: a chronic effects of neurotrauma consortium study. Neurology. 2018;90(20):e1771-e1779. doi: 10.1212/WNL.0000000000005522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kaplan GB, Leite-Morris KA, Wang L, et al. Pathophysiological bases of comorbidity: traumatic brain injury and post-traumatic stress disorder. J Neurotrauma. 2018;35(2):210-225. doi: 10.1089/neu.2016.4953 [DOI] [PubMed] [Google Scholar]
- 44.Gordon EM, Scheibel RS, Zambrano-Vazquez L, et al. High-fidelity measures of whole-brain functional connectivity and white matter integrity mediate relationships between traumatic brain injury and post-traumatic stress disorder symptoms. J Neurotrauma. 2018;35(5):767-779. doi: 10.1089/neu.2017.5428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.van der Naalt J, Timmerman ME, de Koning ME, et al. Early predictors of outcome after mild traumatic brain injury (UPFRONT): an observational cohort study. Lancet Neurol. 2017;16(7):532-540. doi: 10.1016/S1474-4422(17)30117-5 [DOI] [PubMed] [Google Scholar]
- 46.Cnossen MC, van der Naalt J, Spikman JM, et al. Prediction of persistent post-concussion symptoms after mild traumatic brain injury. J Neurotrauma. 2018;35(22):2691-2698. doi: 10.1089/neu.2017.5486 [DOI] [PubMed] [Google Scholar]
- 47.O’Donnell ML, Creamer M, Bryant RA, Schnyder U, Shalev A. Posttraumatic disorders following injury: an empirical and methodological review. Clin Psychol Rev. 2003;23(4):587-603. doi: 10.1016/S0272-7358(03)00036-9 [DOI] [PubMed] [Google Scholar]
- 48.Fazel S, Wolf A, Pillas D, Lichtenstein P, Långström N. Suicide, fatal injuries, and other causes of premature mortality in patients with traumatic brain injury: a 41-year Swedish population study. JAMA Psychiatry. 2014;71(3):326-333. doi: 10.1001/jamapsychiatry.2013.3935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Madsen T, Erlangsen A, Orlovska S, Mofaddy R, Nordentoft M, Benros ME. Association between traumatic brain injury and risk of suicide. JAMA. 2018;320(6):580-588. doi: 10.1001/jama.2018.10211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Holster JL, Bryan CJ, Heron EA, Seegmiller RA. Traumatic brain injury, sleep, and mental health: a longitudinal study of air force personnel pre- and postdeployment to Iraq. J Head Trauma Rehabil. 2017;32(1):25-33. doi: 10.1097/HTR.0000000000000237 [DOI] [PubMed] [Google Scholar]
- 51.Ritterband LM, Thorndike FP, Ingersoll KS, et al. Effect of a web-based cognitive behavior therapy for insomnia intervention with 1-year follow-up: a randomized clinical trial. JAMA Psychiatry. 2017;74(1):68-75. doi: 10.1001/jamapsychiatry.2016.3249 [DOI] [PubMed] [Google Scholar]
- 52.Vuletic S, Bell KR, Jain S, et al. ; CONTACT Investigators . Telephone problem-solving treatment improves sleep quality in service members with combat-related mild traumatic brain injury: results from a randomized clinical trial. J Head Trauma Rehabil. 2016;31(2):147-157. doi: 10.1097/HTR.0000000000000221 [DOI] [PubMed] [Google Scholar]
- 53.Bell KR, Fann JR, Brockway JA, et al. Telephone problem solving for service members with mild traumatic brain injury: a randomized, clinical trial. J Neurotrauma. 2017;34(2):313-321. doi: 10.1089/neu.2016.4444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bryant RA, Nickerson A, Creamer M, et al. Trajectory of post-traumatic stress following traumatic injury: 6-year follow-up. Br J Psychiatry. 2015;206(5):417-423. doi: 10.1192/bjp.bp.114.145516 [DOI] [PubMed] [Google Scholar]
- 55.Fann JR, Bombardier CH, Temkin N, et al. Sertraline for major depression during the year following traumatic brain injury: a randomized controlled trial. J Head Trauma Rehabil. 2017;32(5):332-342. doi: 10.1097/HTR.0000000000000322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Howlett JR, Stein MB. Post-Traumatic Stress Disorder: Relationship to Traumatic Brain Injury and Approach to Treatment In: Laskowitz D, Grant G, eds. Translational Research in Traumatic Brain Injury. Boca Raton, FL: Taylor & Francis Group, LLC; 2016. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Sensitivity Analyses at PCL-5 ≥15 vs <15
eTable 2. Sensitivity Analyses at PCL-5 ≥40 vs <40
eTable 3. Sensitivity Analyses at PCL-5 ≥25 vs <25
eTable 4. Sensitivity Analyses at Varying PHQ-9 ≥15 vs <15
eTable 5. Sensitivity Analyses at Varying PHQ-9 ≥20 vs <20
eTable 6. Sensitivity Analyses at Varying PHQ-9 ≥10 vs <10
eTable 7. Risk factors for probable PTSD at 3 months post-injury among patients with mTBI (n=704)
eTable 8. Risk factors for probable PTSD at 12 months post-injury among patients with mTBI (n=619)
eTable 9. Risk factors for probable MDD at 3 months post-injury among patients with mTBI (n=724)
eTable 10. Risk factors for probable MDD at 12 months post-injury among patients with mTBI (n=626)
eTable 11. Longitudinal Model to assess risk factors on PCL-5 Total Score over time
eTable 12. Longitudinal Model to assess risk factors on PHQ-9 Total Score over time
eTable 13. Sensitivity analysis for 6-month PTSD outcome with additional SES predictors
eTable 14. Sensitivity analysis for 6-month MDD outcome with additional SES predictors