Key Points
Question
What are the mechanisms of risk transmission from paternal depression during the postnatal period to offspring depression at age 18 years?
Findings
In this cohort study of 3176 father-offspring pairs, paternal depression in the postnatal period was associated with offspring depression at age 18 years and appears to exert its influence on later emotional problems in female children partially through maternal depression. Early conduct disorder in children appears to be a mechanism of risk transmission.
Meaning
Depression in fathers in the postnatal period has potential implications for family and child functioning into late childhood and adolescence; it should be addressed in perinatal services, and both parents should be considered when 1 presents with depression.
This analysis of prospective data from the Avon Longitudinal Study of Parents and Children investigates the association between paternal depression in the postnatal period and offspring depression at age 18 years and identifies potential mediating and moderating factors for this association.
Abstract
Importance
Paternal depression during the postnatal period has been associated with adverse child outcomes. Family environment has been reported as a pathway for risk transmission from fathers to children. The influence of paternal depression during the postnatal period on offspring depression remains to be clarified.
Objective
To investigate the association between paternal depression in the postnatal period and offspring depression and explore potential mediating and moderating factors that influence any association between paternal and offspring depression.
Design, Setting, and Participants
This prospective study of a UK community-based birth cohort (the Avon Longitudinal Study of Parents and Children) of parents and their adolescent offspring investigated associations between paternal depression during the postnatal period and offspring depression at age 18 years. We tested a hypothesized moderator (ie, sex) and conducted path analysis to examine hypothesized mediators (ie, depression in the other parent, couple conflict, and paternal involvement and emotional problems, conduct problems, and hyperactivity in offspring at age 3.5 years) of the associations between both paternal and maternal depression and offspring depression. Data collection for the Avon Longitudinal Study of Parents and Children began in 1991 and is ongoing. Data analysis for this study was conducted from June 2015 to September 2018.
Exposures
Depression symptoms in fathers at 8 weeks after the birth of their children.
Main Outcomes and Measures
Offspring depression symptoms at age 18 years, using International Statistical Classification of Diseases and Related Health Problems, Tenth Revision codes.
Results
A total of 3176 father-offspring pairs were analyzed; of the children, 1764 were girls (55.5%) and 1412 (44.5%) were boys. Paternal mean (SD) age at delivery was 29.6 (9.6) years. The offspring of fathers who had depression during the postnatal period were at increased risk of experiencing depression symptoms at age 18 years (β = 0.053 [95% CI, 0.02-0.09]). The association is mediated by maternal depression at 8 months after birth (β = 0.011 [95% CI, 0.0008-0.02]; 21% [0.011/0.053]) and conduct problems at 42 months after birth (β = 0.004; [95% CI , −0.00004 to 0.009]; 7.5% [0.004/0.053]). Couple conflict and paternal involvement do not mediate this association. The increased risk is seen in girls but not boys (interaction β = 0.095; P = .01).
Conclusions and Relevance
The association between paternal depression in the postnatal period and depression in girls at age 18 years is partially explained by maternal depression. Couple conflict and paternal involvement were not found to play a role in the risk of transmission; this contrasts with the role that couple conflict was found to play in the risk of childhood behavior problems. Conduct problems in childhood appear to be a pathway for risk transmission between paternal depression and subsequent depression in offspring at age 18 years.
Introduction
The prevalence of depression in adolescents is between 4% and 5%. The incidence of depression increases after puberty and is twice as high in girls as boys.1 The rate of depression increases with age from 5.7% among youth aged 12 to 17 years to 7.4% among adults aged 18 to 39 years in the US population.2 A recent review study reported that the strongest risk factors for depression in adolescents are a family history of depression and exposure to psychosocial stress.3
The influence of maternal depression in the postnatal period on adolescent depression has previously been reported.4,5,6 Mechanisms of risk transmission have also been investigated. Some longitudinal studies have suggested that the outcomes associated with early maternal depression are mediated through exposure to later maternal depression or associated psychosocial adversity.5,7,8,9,10,11 Insecure attachment to the mother in infancy was associated with depression in offspring at age 16 years. In addition, marital conflict and ongoing maternal depression have been found to partially mediate the association of maternal postnatal depression with adolescent depression.4
A recent longitudinal study12 using the Avon Longitudinal Study of Parents and Children (ALSPAC) cohort reported that offspring of mothers and fathers with depression in the postnatal period were more likely to develop depression at age 18 years in families with low educational level. Conversely, having parents with depression in the postnatal period did not appear to be a risk factor if parents had a high level of education.12 However, the pathways for risk transmission between paternal depression and subsequent offspring depression still remain to be determined.
The moderating effect of sex on the association between maternal depression and offspring depression at age 18 years has been previously reported.13 Maternal antenatal depression is associated with an increased risk of depression in girls, and maternal postnatal depression was associated with an increased risk of depression in boys.13
There is, to our knowledge, very limited evidence regarding the potential influence of paternal depression in the postnatal period on the development of adolescent depression. However, there is clear evidence that paternal depression in the postnatal period is associated with subsequent child behavioral and emotional problems at ages 4 years14 and 7 years.15 We have previously reported on mechanisms of risk transmission from paternal depression to child behavioral problems. We found that nearly two-thirds of the association between paternal depression and child outcomes were explained by the mediating roles of maternal depression and couple conflicts.16
Using the same cohort, we sought in this study to explore the association between paternal depression in the postnatal period and offspring depression at age 18 years. We also aimed to explore key potential mediating and moderating factors influencing the association between paternal and offspring depression.4 First, we hypothesized that paternal depression symptoms in the postnatal period would be associated with offspring depression symptoms at age 18 years. Second, we hypothesized that pathways for risk transmission from paternal depression to offspring depression at age 18 years would not differ from those seen in children with behavioral difficulties at age 42 months. Furthermore, emotional problems, conduct problems, and hyperactivity at age 42 months would be pathways for risk transmission from paternal depression to offspring depression. Finally, we hypothesized that the influence of paternal depression could be stronger in girls than boys, because there is evidence17 suggesting the influence of a father’s involvement on later mental health problems in girls but not in boys.
Methods
Participants
The sample included participants from ALSPAC.18,19,20 The ALSPAC is an ongoing population-based cohort study in the Southwest of England. The ALSPAC recruited 14 541 pregnant women resident in Avon, United Kingdom, with expected dates of delivery between April 1, 1991, to December 31, 1992. An additional 713 children were enrolled during phases 2 and 3 of the study. The total sample size for analyses was 15 247 pregnancies with 15 458 fetuses. Of this total sample, 14 775 (95.6%) were live births and 14 701 infants (95.1%) were alive at 1 year of age. Questionnaires were sent to mothers and fathers at regular points during and after pregnancy. Detailed information about ALSPAC is available online (http://www.bris.ac.uk/alspac), and the study website also contains details of all data in a fully searchable data dictionary (http://www.bristol.ac.uk/alspac/researchers/access/).
Ethical approval for the study was obtained from the ALSPAC law and ethics committee and local research ethics committees. Written informed consent was obtained from all study participants, including offspring at age 18 years. In this article, we focus on paternal depression during the postnatal period and offspring depression at age 18 years.
Procedures and Measures
Paternal Depression
We used the Edinburgh Postnatal Depression Scale (EPDS) to assess depression symptoms in mothers and fathers at 8 weeks and 8 months after the birth of their infants. The EPDS is a 10-item self-report questionnaire21 with a score range of 0 to 30 points that was initially developed to screen for depression in women within the first 6 to 8 weeks after giving birth. It is also useful in the assessment of mothers through and beyond the first postnatal year and has been validated in men.22,23 Most studies using the EPDS use a cutoff score greater than 12 points,14,24 although other studies have used other cutoffs (eg, 9 points).25 We primarily used the continuous scores to make full use of all variation in symptoms.
Offspring Depression
Depression in the offspring was measured using the computerized version of the Clinical Interview Schedule–Revised (CIS-R).26 The CIS-R is a computerized interview that derives a diagnosis of depression according to International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) criteria, as well as symptom severity score for depression. The interview is fully standardized and equally reliable whether conducted by a clinically trained interviewer or self-administered on the computerized version.26,27,28 The CIS-R is designed for and has been widely used within community samples, including the National Surveys of Psychiatric Morbidity and the 1958 National Child Development Study.28,29,30,31 We used a total depressive symptom score derived by summing scores for depression, depressive ideas, fatigue, sleep, and concentration problems, on a scale of 0 to 4 points (with depressive ideas scaled 0 to 5 points).
Rutter Revised Preschool Scales
Rutter Revised Preschool Scales32 were completed by mothers 42 months after the birth of their children. Each item describes a characteristic or behavior. Individual items combine to form 3 problem scales (emotional problems, conduct problems, and hyperactivity) and a prosocial behaviors scale. All problem behaviors combine to give a total problems scale.
Parental Age and Education
Fathers and mothers reported their age at the time of the infant’s birth. Additionally, in week 32 of pregnancy, mothers were asked about the highest educational qualification of themselves and their partners (who were typically the biological father of the infant). Education up to age 16 years (compulsory education only) was categorized as low education and education past age 16 years as high education.
Couple Conflict
At 8 months after the birth of their infant, mothers were asked about the relationships with their partners (as noted, typically the biological father of the infant). A 9-item scale was used, which included questions such as “Do you get angry with your partner?” and “Does your partner listen when you want to talk about your feelings?” Possible answers range from “almost always” to “never.” The scale was developed specifically for the ALSPAC study and has been used in other research.33 A single factor structure (Cronbach α >.80 for maternal and paternal data) explained the data, generating an overall measure of couple conflict.
Paternal Involvement
At 18 months after birth, mothers were asked how often their partners undertook 10 different activities with their child, including bathing, singing, reading, and putting him or her to bed. Responses were on a 5-point scale, from “never” to “every day.” A sum of all responses was the final score.
Statistical Analysis
Statistical analysis was carried out with Stata version 12.0 (StataCorp) from June 2015 to September 2018. We calculated the prevalence of depression in adolescents, and then we conducted logistic regression analysis to assess the association of paternal depression with offspring depression.
Bivariate correlations analyzed the degree of association between paternal depression at 8 weeks and 8 months after the birth, maternal depression at 8 weeks and 8 months after the birth, couple conflict, and paternal involvement; offspring emotional problems, conduct problems, and hyperactivity at 42 months; and offspring depression at age 18 years.
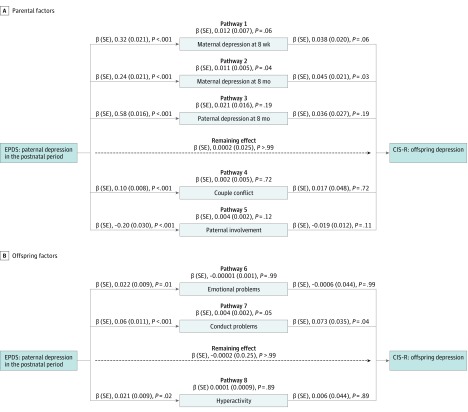
We conducted structural equation modeling to investigate hypothesized mediators between paternal and offspring depression symptoms. The model included paternal depression at 8 weeks after the birth of the infant (independent variable), maternal depression at 8 weeks and 8 months after the birth, paternal depression at 8 months after the birth, couple conflict, and paternal involvement, as well as offspring emotional problems, offspring conduct problems, and offspring hyperactivity at 42 months (mediators) and offspring depression at age 18 years (dependent variable). We controlled for paternal education and age. We examined 2 types of associations between variables: (1) a direct association between paternal depression and offspring depression; (2) an indirect association of paternal depression with offspring depression through each mediator (Figure). Moderate to strong correlations were seen between paternal and maternal education (r = 0.54; P < .001) and paternal and maternal age (r = 0.36; P < .001). Structural equation modeling was performed using maximum likelihood estimation. Indirect associations were calculated using nonlinear combination of parameters (nlcom). To avoid relying on normality assumptions, a nonparametric bootstrap with replacement, with 1000 replicates, was used. To investigate the moderating influence of sex on the association between paternal depression during the postnatal period and offspring depression, we repeated the structural equation modeling, stratifying by sex.
Figure. Hypothesized Pathways in the Association Between Paternal Depression Symptoms at 8 Weeks After the Birth of the Infant and Offspring Depression Symptoms at 18 Years of Age.
The figure shows regression path coefficients, standard errors (SEs), and P values for each direct and indirect association. Model adjusted for paternal education and age. Arrows represent regressions and thus associations between variables. All regression path coefficients are standardized, so all effect sizes are directly comparable. A, Maternal depression was measured at 8 weeks and 8 months after the birth, paternal depression and couple conflict at 8 months after the birth, and paternal involvement at 18 months after the birth. B, Offspring emotional problems, conduct problems, and hyperactivity were measured at age 42 months. CIS-R indicates Clinical Interview Schedule–Revised; EPDS, Edinburgh Postnatal Depression Scale.
We also assessed hypothesized mediators in the association between maternal depression at 8 weeks after the birth (independent variable) and offspring depression at age 18 years (dependent variable). Mediating factors were paternal depression at 8 weeks and 8 months after the birth, maternal depression at 8 months after the birth, couple conflict, and paternal involvement and offspring emotional problems, conduct problems, and hyperactivity at age 42 months. We controlled for maternal education and age. Significance was set at P < .05, 2-sided.
Results
Maternal postnatal depression was assessed in 11 833 of 13 351 mothers (88.6%) and paternal depression in the postnatal period in 8431 of 12 884 fathers (65.4%). At age 18 years, 4566 adolescent offspring completed the CIS-R, and 235 of the 3165 adolescents (7.4%) with information about paternal depression at 8 weeks after their birth had a primary diagnosis of depression: 10 of 93 adolescents (10.8%) of fathers with depression and 225 of 3072 adolescents (7.3%) of fathers without depression (odds ratio, 1.52 [95% CI, 0.78-2.98]). The influence of paternal depression symptoms on offspring depression symptoms is shown in the Table. Bivariate correlations are shown in the eTable in the Supplement. All variables were correlated.
Table. Crude and Adjusted Associations Between Symptoms of Paternal Depression During the Postnatal Period and Symptoms of Offspring Depression at Age 18 Years.
| Offspring Depression Symptoms | Participants, No. (%) | Association With Paternal Depression Symptoms | |
|---|---|---|---|
| Crude β (95% CI) | Adjusted β (95% CI)a | ||
| Total | 3176 (100) | 0.053 (0.02-0.09) | 0.053 (0.02-0.09) |
| Female | 1764 (55.5) | 0.097 (0.05-0.15) | 0.097 (0.04-0.15) |
| Male | 1412 (44.5) | 0.002 (0.05-0.05) | 0.002 (−0.05 to 0.05) |
Adjusted for paternal education and paternal age.
Models of Mediation
A total of 3176 father-adolescent pairs were included in the path analysis. The total association of paternal depression in the postnatal period with offspring depression at age 18 years, after controlling for paternal education and age, was measured as a β value of 0.053 (95% CI, 0.02-0.09; bootstrapped 95% CI, 0.02-0.10; P = .004). This total association was explained by the indirect association of maternal depression at 8 months after the birth (β = 0.011 [bootstrapped 95% CI, 0.0008-0.02]; 21% [0.011/0.053]) and conduct problems in offspring at age 42 months (β = 0.004 [bootstrapped 95% CI, −0.00004 to 0.009]; 7.5% [0.004/0.053]). Couple conflict (β = 0.002 [95% CI, −0.008 to 0.011]; P = .72) and paternal involvement (β = 0.004 [95% CI, −0.001 to 0.009]; P = .12) did not explain this association (Figure).
When stratified by sex, a total of 1764 girls and 1412 boys were included in the path analysis. The association between paternal depression symptoms and total symptoms of depression in adolescents was stronger in girls than boys (paternal depression by sex interaction, β = 0.095; P = .01; girls at age 18 years: β = 0.097 [95% CI, 0.04-0.15; bootstrapped 95% CI, 0.04-0.15]; P < .001; boys at age 18 years: β = −0.002 [95% CI, −0.05 to 0.05]; P = .94). The total association of paternal depression with offspring depression in girls was explained by the indirect association with maternal depression at 8 months (β = 0.017 [bootstrapped 95% CI , 0.003-0.03]; 18% [0.017/0.097]) and conduct problems at age 42 months β = 0.009 [bootstrapped 95% CI, 0.0013-0.016]; 9.3% [0.009/0.097]). The association between paternal and offspring depression was not mediated by couple conflict and paternal involvement (eFigure 1 in the Supplement). Paternal depression during the postnatal period was not associated with offspring depression in boys.
We repeated the analysis using maternal depression at 8 weeks after the birth of the infant as the exposure variable and offspring depression as the dependent variable. A total of 4062 mother-adolescent pairs were included in the analysis. The total association of postnatal maternal depression with offspring depression was defined by a β value of 0.097 (95% CI, 0.07-0.12; P < .001). This was explained by the association with maternal depression at 8 months after the birth (β = 0.048 [95% CI, 0.012-0.084]; P = .009; 50% [0.048/0.097]) and maternal depression at 8 weeks after the birth (β = 0.03 [95% CI, 0.007-0.053]; P = .01; 31% [0.03/0.097]) and minimally explained by the indirect outcome of paternal involvement (β = 0.003 [95% CI, 0.0007-0.006]; P = .02; 3.3% [0.003/0.097]) and conduct problems (β = 0.007 [95% CI, 0.0013-0.013]; P = .02; 7.2% [0.007/0.097]). Paternal depression and couple conflict did not explain this association (eFigure 2 in the Supplement). There was no sex interaction (β = 0.033; P = .21).
Discussion
This study explores the association of paternal depression symptoms at 8 weeks after the birth of an infant and depression symptoms in that offspring at age 18 years in a large community sample. We also explored 8 potential environmental pathways that may explain this association. To conduct pathway analysis, we used continuous measures of depression (ie, symptoms) instead of cases of clinical depression. Responses for a dichotomous variable are heavily skewed toward 1 response and comparison of 2 groups was not possible because too few participants met the threshold for clinical depression.33
Our findings indicate that adolescent offspring of fathers who have depression during the postnatal period are at increased risk of experiencing depression symptoms at age 18 years, even after paternal age and education had been controlled for. The effect size is small, but it is still significant after 18 years of follow-up time. The increased risk is seen in girls but not boys. The mediating effect of maternal depression at 8 months explains one-fifth of the total association of paternal depression in the postnatal period with offspring depression, and conduct problems at age 3.5 years explains almost one-tenth of this association. Conversely, the total association of postnatal maternal depression with subsequent offspring depression is minimally explained by paternal involvement and conduct problems.
Our findings suggest that paternal depression during the postnatal period appears to exert its influence on late emotional problems in girls at least in part through maternal depression. Maternal depression has been previously associated with impaired parenting, particularly sensitive parenting.34 Mothers with depression may show less maternal responsiveness or sensitivity, less verbal and visual interaction, and more intrusiveness during interactions with their infants.35,36
We had previously reported that couple conflict mediated the association between postnatal depression in fathers and child outcomes at 3.5 years after a birth.16,37 However, the role of couple conflict appears to be less important for offspring adolescents with depression than child behavioral problems. Paternal involvement was not found to play a role in the risk of offspring depression, although we did not have suitable data to explore the quality of parent-infant interaction. In addition, mediators were measured early in child life, and we did not measure these variables throughout the time period.
Our group previously reported that boys were more vulnerable to the influence of paternal depression than girls in their early years.14 However, we have found that girls with fathers with depression during the postnatal period are at risk of developing depression after puberty, but such risk is not seen in boys. One study17 has reported an association between parenting father–infant interaction and later emotional development only in girls. The association of paternal depression during the postnatal period through father-infant interaction might affect boys in the short term and girls in the longer term. In this study, we were unable to include this pathway, because this was not assessed.
The association between maternal depression and offspring depression differed from the patterns seen with fathers. Other studies have found these differences are explained by other factors, such as maternal depression,9 mother-child interaction,34 higher genetic loading in mothers,38,39,40 or transmission of cognitive style.41 Additionally, the association between maternal depression during the postnatal period and depression in offspring did not show a sex-specific outcome. A previous meta-analysis reported no differences by sex in the association between maternal depression and internalizing problems.10
In this study, we found that early-onset conduct problems in offspring mediated the association between depression in fathers during the postnatal period and depression in adolescents; however, early emotional problems did not explain such an association. This finding is consistent with previous research that reported conduct problems in early childhood are a strong risk factor for subsequent depression.3,42
Strengths
This study has a number of strengths. The sample size is large and based on a community sample, limiting the possibility of selection bias. This is a long-term follow-up study, with the proposed mediating factors measured at a point between the measured factor and outcome. Paternal depression was first measured 18 years earlier than the measure of offspring depression; as a result, reverse causality is implausible. A clinical interview was used for the offspring outcome.
Limitations
There were a number of limitations of the study. Adolescents who attended the 18-year assessment were more likely to come from families of higher socioeconomic status than those in the original sample. A further limitation was the lack of a measure of paternal depression when the child was 18 years. It is also important to note that the paternal depression measure was a self-report rather than a diagnostic interview. The use of questionnaires to assess father involvement with no directly observed measures did not allow us to assess the influence of paternal depression through parenting interactions. Depression in the adolescents was assessed using a computerized interview. Any form of measurement has some limitations; however, rates of depression diagnoses yielded from the computerized CIS-R assessments are generally similar to those produced by other structured interview assessments.27,30 Finally, the lag time between the mediator and the outcome variable was considerably larger than between the independent variable and the mediator.
Conclusions
This study suggests that there is an association between depression in fathers during the postnatal period and subsequent depression in girls at age 18 years. Such an association is explained predominantly by the influence of maternal depression (21%). In contrast, the association between depression in mothers and adolescent outcome differs from that seen in fathers. Other research suggests that it may be better explained by other factors, including the association of depression with mother-infant interaction, genetic loading, and transmission of negative cognitions. Early conduct disorder in children appears to be a mechanism of risk transmission between depression in fathers and subsequent depression at age 18 years. Overall, these findings highlight the importance of recognizing and treating depression in fathers during the postnatal period and considering both parents when 1 parent presents with depression.
eTable. Bivariate Pearson correlations among paternal depression at 8 weeks and 8 months, maternal depression at 8 weeks and 8 months, couple conflict, paternal involvement, child outcomes at 42 months and offspring depression at 18 years.
eFigure 1. Hypothesized pathways in the association between paternal depression symptoms at 8 weeks after the birth of the child and offspring depression symptoms at 18 years in females. Model adjusted for paternal education and age.
eFigure 2. Hypothesized pathways in the association between maternal depression symptoms at 8 weeks after the birth of the child and offspring depression symptoms at 18 years. Model adjusted for maternal education and age.
References
- 1.Hyde JS, Mezulis AH, Abramson LY. The ABCs of depression: integrating affective, biological, and cognitive models to explain the emergence of the gender difference in depression. Psychol Rev. 2008;115(2):291-313. doi: 10.1037/0033-295X.115.2.291 [DOI] [PubMed] [Google Scholar]
- 2.Pratt LA, Brody DJ. Depression in the U.S. household population, 2009-2012. NCHS Data Brief. 2014;(172):1-8. [PubMed] [Google Scholar]
- 3.Thapar A, Collishaw S, Pine DS, Thapar AK. Depression in adolescence. Lancet. 2012;379(9820):1056-1067. doi: 10.1016/S0140-6736(11)60871-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Murray L, Arteche A, Fearon P, Halligan S, Goodyer I, Cooper P. Maternal postnatal depression and the development of depression in offspring up to 16 years of age. J Am Acad Child Adolesc Psychiatry. 2011;50(5):460-470. doi: 10.1016/j.jaac.2011.02.001 [DOI] [PubMed] [Google Scholar]
- 5.Hay DF, Pawlby S, Waters CS, Sharp D. Antepartum and postpartum exposure to maternal depression: different effects on different adolescent outcomes. J Child Psychol Psychiatry. 2008;49(10):1079-1088. doi: 10.1111/j.1469-7610.2008.01959.x [DOI] [PubMed] [Google Scholar]
- 6.Hammen C, Brennan PA. Severity, chronicity, and timing of maternal depression and risk for adolescent offspring diagnoses in a community sample. Arch Gen Psychiatry. 2003;60(3):253-258. doi: 10.1001/archpsyc.60.3.253 [DOI] [PubMed] [Google Scholar]
- 7.Foster CE, Webster MC, Weissman MM, et al. Remission of maternal depression: relations to family functioning and youth internalizing and externalizing symptoms. J Clin Child Adolesc Psychol. 2008;37(4):714-724. doi: 10.1080/15374410802359726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rice F, Harold GT, Boivin J, van den Bree M, Hay DF, Thapar A. The links between prenatal stress and offspring development and psychopathology: disentangling environmental and inherited influences. Psychol Med. 2010;40(2):335-345. doi: 10.1017/S0033291709005911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: a developmental model for understanding mechanisms of transmission. Psychol Rev. 1999;106(3):458-490. doi: 10.1037/0033-295X.106.3.458 [DOI] [PubMed] [Google Scholar]
- 10.Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, Heyward D. Maternal depression and child psychopathology: a meta-analytic review. Clin Child Fam Psychol Rev. 2011;14(1):1-27. doi: 10.1007/s10567-010-0080-1 [DOI] [PubMed] [Google Scholar]
- 11.Stein A, Malmberg LE, Sylva K, Barnes J, Leach P; FCCC team** . The influence of maternal depression, caregiving, and socioeconomic status in the post-natal year on children’s language development. Child Care Health Dev. 2008;34(5):603-612. doi: 10.1111/j.1365-2214.2008.00837.x [DOI] [PubMed] [Google Scholar]
- 12.Pearson RM, Evans J, Kounali D, et al. Maternal depression during pregnancy and the postnatal period: risks and possible mechanisms for offspring depression at age 18 years. JAMA Psychiatry. 2013;70(12):1312-1319. doi: 10.1001/jamapsychiatry.2013.2163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Quarini C, Pearson RM, Stein A, Ramchandani PG, Lewis G, Evans J. Are female children more vulnerable to the long-term effects of maternal depression during pregnancy? J Affect Disord. 2016;189:329-335. doi: 10.1016/j.jad.2015.09.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ramchandani P, Stein A, Evans J, O’Connor TG; ALSPAC study team . Paternal depression in the postnatal period and child development: a prospective population study. Lancet. 2005;365(9478):2201-2205. doi: 10.1016/S0140-6736(05)66778-5 [DOI] [PubMed] [Google Scholar]
- 15.Ramchandani PG, Stein A, O’Connor TG, Heron J, Murray L, Evans J. Depression in men in the postnatal period and later child psychopathology: a population cohort study. J Am Acad Child Adolesc Psychiatry. 2008;47(4):390-398. doi: 10.1097/CHI.0b013e31816429c2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gutierrez-Galve L, Stein A, Hanington L, Heron J, Ramchandani P. Paternal depression in the postnatal period and child development: mediators and moderators. Pediatrics. 2015;135(2):e339-e347. doi: 10.1542/peds.2014-2411 [DOI] [PubMed] [Google Scholar]
- 17.Flouri E, Buchanan A. The role of father involvement in children’s later mental health. J Adolesc. 2003;26(1):63-78. doi: 10.1016/S0140-1971(02)00116-1 [DOI] [PubMed] [Google Scholar]
- 18.Boyd A, Golding J, Macleod J, et al. Cohort profile: the ‘children of the 90s’—the index offspring of the Avon Longitudinal Study of Parents and Children. Int J Epidemiol. 2013;42(1):111-127. doi: 10.1093/ije/dys064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fraser A, Macdonald-Wallis C, Tilling K, et al. Cohort profile: the Avon Longitudinal Study of Parents and Children. ALSPAC mothers cohort. Int J Epidemiol. 2013;42(1):97-110. doi: 10.1093/ije/dys066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Golding J, Pembrey M, Jones R; ALSPAC Study Team . ALSPAC—the Avon Longitudinal Study of Parents and Children, I: study methodology. Paediatr Perinat Epidemiol. 2001;15(1):74-87. doi: 10.1046/j.1365-3016.2001.00325.x [DOI] [PubMed] [Google Scholar]
- 21.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782-786. doi: 10.1192/bjp.150.6.782 [DOI] [PubMed] [Google Scholar]
- 22.Cox JL, Chapman G, Murray D, Jones P. Validation of the Edinburgh Postnatal Depression Scale (EPDS) in non-postnatal women. J Affect Disord. 1996;39(3):185-189. doi: 10.1016/0165-0327(96)00008-0 [DOI] [PubMed] [Google Scholar]
- 23.Matthey S, Barnett B, Kavanagh DJ, Howie P. Validation of the Edinburgh Postnatal Depression Scale for men, and comparison of item endorsement with their partners. J Affect Disord. 2001;64(2-3):175-184. doi: 10.1016/S0165-0327(00)00236-6 [DOI] [PubMed] [Google Scholar]
- 24.Murray L, Carothers AD. The validation of the Edinburgh Post-natal Depression Scale on a community sample. Br J Psychiatry. 1990;157:288-290. doi: 10.1192/bjp.157.2.288 [DOI] [PubMed] [Google Scholar]
- 25.Areias ME, Kumar R, Barros H, Figueiredo E. Correlates of postnatal depression in mothers and fathers. Br J Psychiatry. 1996;169(1):36-41. doi: 10.1192/bjp.169.1.36 [DOI] [PubMed] [Google Scholar]
- 26.Lewis G, Pelosi AJ, Araya R, Dunn G. Measuring psychiatric disorder in the community: a standardized assessment for use by lay interviewers. Psychol Med. 1992;22(2):465-486. doi: 10.1017/S0033291700030415 [DOI] [PubMed] [Google Scholar]
- 27.Patton GC, Coffey C, Posterino M, Carlin JB, Wolfe R, Bowes G. A computerised screening instrument for adolescent depression: population-based validation and application to a two-phase case-control study. Soc Psychiatry Psychiatr Epidemiol. 1999;34(3):166-172. doi: 10.1007/s001270050129 [DOI] [PubMed] [Google Scholar]
- 28.Bell T, Watson M, Sharp D, Lyons I, Lewis G. Factors associated with being a false positive on the General Health Questionnaire. Soc Psychiatry Psychiatr Epidemiol. 2005;40(5):402-407. doi: 10.1007/s00127-005-0881-6 [DOI] [PubMed] [Google Scholar]
- 29.Brugha TS, Morgan Z, Bebbington P, et al. Social support networks and type of neurotic symptom among adults in British households. Psychol Med. 2003;33(2):307-318. doi: 10.1017/S0033291702006505 [DOI] [PubMed] [Google Scholar]
- 30.Brugha TS, Meltzer H, Jenkins R, Bebbington PE, Taub NA. Comparison of the CIS-R and CIDI lay diagnostic interviews for anxiety and depressive disorders. Psychol Med. 2005;35(7):1089-1091. doi: 10.1017/S0033291705005180 [DOI] [PubMed] [Google Scholar]
- 31.Bebbington P, Dunn G, Jenkins R, et al. The influence of age and sex on the prevalence of depressive conditions: report from the National Survey of Psychiatric Morbidity. Int Rev Psychiatry. 2003;15(1-2):74-83. doi: 10.1080/0954026021000045976 [DOI] [PubMed] [Google Scholar]
- 32.Elander J, Rutter M. Use and development of the Rutter Parents’ and Teachers’ Scales. Int J Methods Psychiatr Res. 1996;6(2):63-78. doi: [DOI] [Google Scholar]
- 33.O’Connor TG, Cheng H, Dunn J, Golding J; ALSPAC Study Team . Factors moderating change in depressive symptoms in women following separation: findings from a community study in England. Psychol Med. 2005;35(5):715-724. doi: 10.1017/S0033291704004015 [DOI] [PubMed] [Google Scholar]
- 34.Lovejoy MC, Graczyk PA, O’Hare E, Neuman G. Maternal depression and parenting behavior: a meta-analytic review. Clin Psychol Rev. 2000;20(5):561-592. doi: 10.1016/S0272-7358(98)00100-7 [DOI] [PubMed] [Google Scholar]
- 35.Campbell SB, Brownell CA, Hungerford A, Spieker SI, Mohan R, Blessing JS. The course of maternal depressive symptoms and maternal sensitivity as predictors of attachment security at 36 months. Dev Psychopathol. 2004;16(2):231-252. doi: 10.1017/S0954579404044499 [DOI] [PubMed] [Google Scholar]
- 36.Foster CJ, Garber J, Durlak JA. Current and past maternal depression, maternal interaction behaviors, and children’s externalizing and internalizing symptoms. J Abnorm Child Psychol. 2008;36(4):527-537. doi: 10.1007/s10802-007-9197-1 [DOI] [PubMed] [Google Scholar]
- 37.Hanington L, Heron J, Stein A, Ramchandani P. Parental depression and child outcomes: is marital conflict the missing link? Child Care Health Dev. 2012;38(4):520-529. doi: 10.1111/j.1365-2214.2011.01270.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Merikangas KR, Risch NJ, Weissman MM. Comorbidity and co-transmission of alcoholism, anxiety and depression. Psychol Med. 1994;24(1):69-80. doi: 10.1017/S0033291700026842 [DOI] [PubMed] [Google Scholar]
- 39.Kendler KS, Davis CG, Kessler RC. The familial aggregation of common psychiatric and substance use disorders in the National Comorbidity Survey: a family history study. Br J Psychiatry. 1997;170:541-548. doi: 10.1192/bjp.170.6.541 [DOI] [PubMed] [Google Scholar]
- 40.O’Connor TG, McGuire S, Reiss D, Hetherington EM, Plomin R. Co-occurrence of depressive symptoms and antisocial behavior in adolescence: a common genetic liability. J Abnorm Psychol. 1998;107(1):27-37. doi: 10.1037/0021-843X.107.1.27 [DOI] [PubMed] [Google Scholar]
- 41.Pearson RM, Fernyhough C, Bentall R, et al. Association between maternal depressogenic cognitive style during pregnancy and offspring cognitive style 18 years later. Am J Psychiatry. 2013;170(4):434-441. doi: 10.1176/appi.ajp.2012.12050673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Stringaris A, Lewis G, Maughan B. Developmental pathways from childhood conduct problems to early adult depression: findings from the ALSPAC cohort. Br J Psychiatry. 2014;205(1):17-23. doi: 10.1192/bjp.bp.113.134221 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. Bivariate Pearson correlations among paternal depression at 8 weeks and 8 months, maternal depression at 8 weeks and 8 months, couple conflict, paternal involvement, child outcomes at 42 months and offspring depression at 18 years.
eFigure 1. Hypothesized pathways in the association between paternal depression symptoms at 8 weeks after the birth of the child and offspring depression symptoms at 18 years in females. Model adjusted for paternal education and age.
eFigure 2. Hypothesized pathways in the association between maternal depression symptoms at 8 weeks after the birth of the child and offspring depression symptoms at 18 years. Model adjusted for maternal education and age.