Abstract
Importance
Individuals with mental disorders often develop comorbidity over time. Past studies of comorbidity have often restricted analyses to a subset of disorders and few studies have provided absolute risks of later comorbidity.
Objectives
To undertake a comprehensive study of comorbidity within mental disorders, by providing temporally ordered age- and sex-specific pairwise estimates between the major groups of mental disorders, and to develop an interactive website to visualize all results and guide future research and clinical practice.
Design, Setting, and Participants
This population-based cohort study included all individuals born in Denmark between January 1, 1900, and December 31, 2015, and living in the country between January 1, 2000, and December 31, 2016. The analyses were conducted between June 2017 and May 2018.
Main Outcomes and Measures
Danish health registers were used to identify mental disorders, which were examined within the broad 10-level International Statistical Classification of Diseases and Related Health Problems, 10th Revision, subchapter groups (eg, codes F00-F09 and F10-F19). For each temporally ordered pair of disorders, overall and lagged hazard ratios and 95% CIs were calculated using Cox proportional hazards regression models. Absolute risks were estimated using competing risks survival analyses. Estimates for each sex were generated.
Results
A total of 5 940 778 persons were included in this study (2 958 293 men and 2 982 485 women; mean [SD] age at beginning of follow-up, 32.1 [25.4] years). They were followed up for 83.9 million person-years. All mental disorders were associated with an increased risk of all other mental disorders when adjusting for sex, age, and calendar time (hazard ratios ranging from 2.0 [95% CI, 1.7-2.4] for prior intellectual disabilities and later eating disorders to 48.6 [95% CI, 46.6-50.7] for prior developmental disorders and later intellectual disabilities). The hazard ratios were temporally patterned, with higher estimates during the first year after the onset of the first disorder, but with persistently elevated rates during the entire observation period. Some disorders were associated with substantial absolute risks of developing specific later disorders (eg, 30.6% [95% CI, 29.3%-32.0%] of men and 38.4% [95% CI, 37.5%-39.4%] of women with a diagnosis of mood disorders before age 20 years developed neurotic disorders within the following 5 years).
Conclusions and Relevance
Comorbidity within mental disorders is pervasive, and the risk persists over time. This study provides disorder-, sex-, and age-specific relative and absolute risks of the comorbidity of mental disorders. Web-based interactive data visualization tools are provided for clinical utility.
This population-based cohort study examines comorbidity within mental disorders, provides temporally ordered age- and sex-specific pairwise estimates between the major groups of mental disorders, and develops an interactive website to visualize all results and guide future research and clinical practice.
Key Points
Question
After an individual receives a diagnosis of a specific mental disorder, does the risk of developing other mental disorders increase?
Findings
This population-based cohort study of 5 940 778 individuals, followed up for 83.9 million person-years, found that comorbidity within mental disorders was pervasive (there was an increased risk of developing all other mental disorders after an index mental disorder) and that the risk of developing comorbidity was most prominent in the first year after the onset of a mental disorder; however, the increased risk persisted over at least 15 years. For some disorders (eg, mood disorders) the absolute risks of developing specific later disorders (eg, anxiety disorders) was substantial (eg, 30%-40% over 5 years).
Meaning
If clinicians and individuals with mental disorders had ready access to diagnosis-, age-, and sex-specific absolute risks of potential future comorbidity, this information could permit more tailored interventions and better education about self-management (ie, personalized medicine).
Introduction
Comorbidity, defined as the presence of 1 or more disorders in relation to an index disorder,1 has been the focus of a substantial body of research during the 5 decades since the term was introduced.2 In the mental health field, it is widely acknowledged that individuals treated for incident mental disorders are at increased risk of subsequently developing other mental disorders.3 Based on a survey of mental health among adolescents 13 to 17 years of age, Kessler et al4 reported that 27.9% of respondents met criteria for 2 or more disorders. Several community surveys have reported that, among respondents with at least 1 mental disorder, 45% to 54% have 1 or more additional lifetime diagnoses.3,5,6
Patterns of concurrent or sequential (cumulative) comorbidity can arise from different factors.7 Diagnosing a mental disorder can be an imprecise science, especially early in the course of the illness. In recognition of the pluripotent nature of mental disorders in young people, the use of clinical staging models has been recommended.8 More importantly, some factors that contribute to comorbidity, such as changes to diagnoses during the first weeks or months after the onset of an index disorder, may reflect good clinical practice. Patterns of comorbidity within mental disorders may also reflect a shared risk architecture underlying different types of disorders. There is a tradition of using symptom-centered or disorder-centered analyses (eg, factor analysis and principal component analysis9) or person-centered analyses (eg, latent class analysis10) to understand the structure of mental disorders.
Estimates of the lifetime prevalence of mental disorders based on cross-sectional surveys are known to underestimate their true prevalence.11 Studies based on national health registers can complement population-based surveys by providing reliable date-stamped timing of the “administrative” onset of treated mental disorders. To date, to our knowledge, register-based studies of comorbidity have been restricted to subsets of mental disorders.12,13 There is a need to examine the comorbidity of mental disorders in a comprehensive fashion.
The main aim of this study was to undertake a comprehensive study of comorbidity within treated mental disorders, by using high-quality Danish registers to provide temporally ordered age- and sex-specific pairwise estimates between the major groups of mental disorders. We also explored patterns of lagged hazard ratios (HRs) over time (ie, examining whether the association between pairs of disorders persists over time).
From a clinical perspective, measures of relative risks should be examined within the context of absolute risks; thus, we have provided detailed age- and sex-specific measures of absolute risk between mental disorders. In the spirit of pragmatic psychiatric epidemiology,14 we have made the findings of our study available on an interactive data visualization webpage (http://www.nbepi.com).
Methods
Study Population and Assessment of Mental Disorders
This population-based cohort study encompassed all individuals born in Denmark between January 1, 1900, and December 31, 2015, who resided in the country during the study period (January 1, 2000–December 31, 2016) (5 940 778; a total of 2 958 293 men and 2 982 485 women). The analyses were conducted between June 2017 and May 2018. Since 1968, the Danish Civil Registration System15 has maintained information on all residents, including sex, date of birth, continuously updated information on vital status, and a unique personal identification number that can be used to link information from various national registries. Information on mental diseases was obtained from the Danish Psychiatric Central Research Register,16 which contains information on all admissions to psychiatric inpatient facilities since 1969 and visits to outpatient psychiatric departments and emergency departments since 1995. The diagnostic system used was the Danish modification of the International Classification of Diseases, Eighth Revision (ICD-8), from 1969 to 1993, and International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10), from 1994 onward. Register-based diagnoses have been validated in Denmark for a range of disorders (eg, affective disorders, schizophrenia, childhood-onset disorders, and dementia) and found to have good validity compared with research criteria.16,17,18,19,20,21,22
To keep the number of analyses tractable, and to ensure comparability with previous publications based on Danish registers,23 we used the 10-level subchapter categories as described in ICD-10 (eg, codes F00-F09, F10-19, F20-29, etc) and corresponding diagnoses in ICD-8. Details of the specific diagnosis included in each group of disorders are presented in the Table. From this point onward, we use disorder to describe each group of specific diagnoses, using the short labels provided in the Table. For each individual in the study, the date of onset for each disorder was defined as the date of first contact (inpatient, outpatient, or emergency department visit).
Table. Diagnostic Classification of Mental Disorders Considered in This Study According to the ICD-10 and Equivalent ICD-8 Diagnoses.
| Mental Disorder; Examples of Diagnoses Included in Each Group | Abbreviated Name Used in This Study | ICD-10 Code(s) | ICD-8 Equivalent Code(s) | Earliest Possible Age at Onset, y | Prevalent Cases Before Follow-up, No. | Persons at Risk at Start of Follow-up, No. | New Cases During Follow-up, No. |
|---|---|---|---|---|---|---|---|
| Organic, including symptomatic, mental disorders; includes dementia in Alzheimer disease, vascular dementia, etc | Organic disorders | F00-F09 | 290.09, 290.10, 290.11, 290.18, 290.19, 292.x9, 293.x9, 294.x9, 309.x9 | 35 | 23 994 | 3 818 123 | 84 813 |
| Mental and behavioral disorders due to psychoactive substance use; includes use of alcohol, cannabis, cocaine, nicotine, opioids, sedatives, hypnotics, anxiolytics, etc | Substance use | F10-F19 | 291.x9, 294.39, 303.x9, 303.20, 303.28, 303.90, 304.x9 | 10 | 66 373 | 5 319 247 | 70 673 |
| Schizophrenia and related disorders; includes schizophrenia, schizotypal disorders, schizoaffective disorders, and other psychotic disorders | Schizophrenia | F20-F29 | 295.x9, 296.89, 297.x9, 298.29-298.99, 299.04, 299.05, 299.09, 301.83 | 10 | 45 617 | 5 340 003 | 42 015 |
| Mood disorders; includes bipolar disorder, depressive disorders, etc | Mood disorders | F30-F39 | 296.x9 (Excluding 296.89), 298.09, 298.19, 300.49, 301.19 | 10 | 73 897 | 5 311 723 | 153 621 |
| Neurotic, stress-related, and somatoform disorders; includes anxiety disorders, phobias, obsessive-compulsive disorders, etc | Neurotic disorders | F40-F48 | 300.x9 (Excluding 300.49), 305.x9, 305.68, 307.99 | 5 | 89 348 | 5 610 596 | 205 241 |
| Eating disorders; includes anorexia nervosa, bulimia nervosa, etc | Eating disorders | F50 | 305.60, 306.50, 306.58, 306.59 | 1 | 4 962 | 5 935 816 | 18 614 |
| Specific personality disorders | Personality disorders | F60 | 301.x9 (Excluding 301.19), 301.80, 301.81, 301.82, 301.84 | 10 | 71 976 | 5 313 644 | 56 779 |
| Intellectual disabilities | Intellectual disabilities | F70-F79 | 311.xx, 312.xx, 313.xx, 314.xx, 315.xx | 1 | 5 564 | 5 935 214 | 17 579 |
| Pervasive developmental disorders; includes autism spectrum disorder | Developmental disorders | F84 | 299.00, 299.01, 299.02, 299.03 | 1 | 3 269 | 5 937 509 | 30 423 |
| Behavioral and emotional disorders with onset usually occurring in childhood and adolescence; includes attention-deficit/hyperactivity disorder, conduct disorders, childhood emotional disorders, etc | Behavioral disorders | F90-F98 | 306.x9, 308.0x | 1 | 13 800 | 5 926 978 | 73 239 |
Abbreviations: ICD-8, International Classification of Diseases, Eighth Revision; ICD-10, International Statistical Classification of Diseases and Related Health Problems, 10th Revision.
The Danish Data Protection Agency and the Danish Health Data Authority approved this study. According to Danish law, informed consent is not required for register-based studies. All data were deidentified and not recognizable at an individual level.
Study Design
We examined the association between all 90 possible pairs of disorders taking the temporal order into consideration (ie, the association between 2 specific disorders was estimated in both directions). Depending on whether individuals had a diagnosis of 1 of the specific disorders (henceforth referred to as prior disorder), we estimated the risk of receiving a diagnosis of an additional disorder (henceforth referred to as later disorder). For each specific pair of disorders, follow-up started on January 1, 2000, or at the earliest age at which a person might develop the later disorder23 (Table), whichever came later. Follow-up was terminated at onset of the later disorder, death, emigration from Denmark, or on December 31, 2016, whichever came first. Our analyses were based on incident cases of the later disorder, diagnosed during the observation period (2000-2016), when disorders were diagnosed according to ICD-10. Individuals with a particular later disorder of interest before the observation period were considered prevalent cases and excluded from the analyses (ie, prevalent cases were washed out). The sample sizes for each later disorder are specified in the Table. For example, for mood disorders as a later disorder, there were 73 897 persons excluded from the analysis because they received a diagnosis before the observation period. Taking into account age thresholds for each disorder, the remaining 5 311 723 individuals were at risk of developing mood disorders and were included in the analysis. All disorders had a sample size larger than 5.3 million persons except organic disorders (3 818 123 persons) because the earliest age at onset was 35 years. When estimating the risk of a later disorder, we considered all individuals to be exposed or unexposed to the each prior disorder depending on whether they had a diagnosis between January 1, 1969, and the end of follow-up. Persons with a prior disorder were considered to be unexposed until the date of the first diagnosis of the prior disorder, and considered to be exposed afterwards (see eAppendix 1 in the Supplement for an overview of the study population and observation period, as well as a simplified “worked example”). We make no assumption that the later disorder is causally related to the prior disorder.
Statistical Analysis
We compared the rate of diagnosis with a specific later disorder between individuals who were exposed and unexposed to each of the other 9 prior disorders using HRs and 95% CIs, obtained via Cox proportional hazards regression models with age as the underlying time scale. All estimates were adjusted for sex and birth date which, in combination with underlying age in the models, also adjusts for calendar time (model A). To adjust for additional preceding comorbidity, we also examined models that adjusted for mental disorder comorbidity with onset before the prior disorder, but not with onset after the prior disorder (model B). This model adjusted for other mental disorders (apart from the specific prior and later disorders) with onset between January 1, 1969, and onset of the prior disorder. We further investigated if the association differed depending on the time since onset of the prior disorder (ie, lagged, or time-dependent, HRs). Finally, we estimated the cumulative incidence proportion of diagnosis with a later disorder after receiving a diagnosis of a prior disorder. Cumulative incidences are absolute risks that can be interpreted as the percentage of individuals among those who received a diagnosis of a prior disorder who develop the later disorder after a specific time. Further details on the statistical analysis can be found in eAppendix 1 in the Supplement. All analyses were performed on the secured platform of Statistics Denmark using R, version 3.2.2 (R Foundation for Statistical Computing), and Stata/MP, version 13.1 (StataCorp). The code used for data management and statistical analysis can be found on https://plana-ripoll.github.io/NB-COMO/ (the pair mood disorders–neurotic disorders is used as example).
We developed an interactive webpage to visualize all results from this study (http://www.nbepi.com). To simplify the presentation of the results, we discuss examples where mood disorders were the prior disorder; however, complete results for every mental disorder pair are available in the Supplement and on the webpage.
Results
This cohort of 5.9 million Danish residents was followed for 83.9 million person-years (mean [SD] age at beginning of follow-up, 32.1 [25.4] years). The longest individual period used to identify incident cases was 17 years (2000-2016). However, the interval between prior disorders and later disorders could range to up to 48 years (1969-2016) in our sampling frame. Overall, 882 730 persons died and 85 356 persons emigrated from Denmark during the observation period. Baseline characteristics of the study population are presented in the eTable in the Supplement.
Pairwise Associations Between Mental Disorders
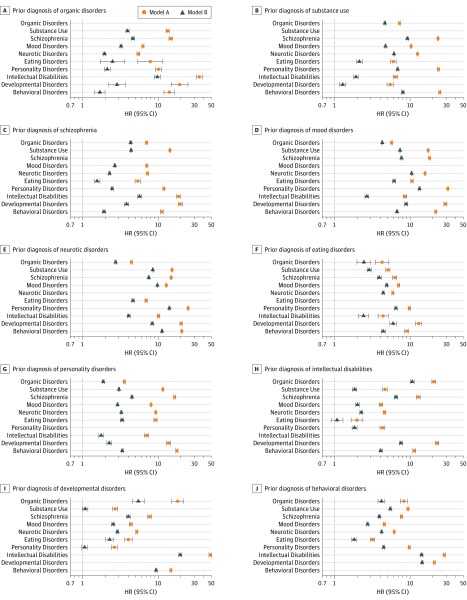
Estimates from the pairwise comparisons of all mental disorders are presented in Figure 1. Overall, receiving a diagnosis of 1 of the disorders increased the risk of a subsequent diagnosis with each of the other disorders. When controlling for age, calendar time, and sex (model A), HRs ranged from 2.0 (95% CI, 1.7-2.4) (prior intellectual disabilities and later eating disorders) to 48.6 (95% CI, 46.6-50.7) (prior developmental disorders and later intellectual disabilities). When further adjusted for previous disorders (model B), the general pattern of findings persisted, but the HRs became smaller. For model A, all HRs were above 1 (and had 95% CIs that excluded 1), indicating that the pairwise patterns of comorbidity were bidirectional. Further details of the bidirectional nature of comorbidity can be found in eFigures 1 to 20 in the Supplement and on the interactive data visualization webpage, and details on the influence of sex on the estimated associations can be found in eAppendix 2 and eFigures 21 to 24 in the Supplement.
Figure 1. Risk of Persons With and Without a Diagnosis of a Prior Disorder Receiving a Diagnosis of Another Disorder.
Each panel shows the pairwise comorbidity between prior disorders and later disorders. Some 95% CIs are obscured by the effect size symbol used to display the hazard ratio (HR). Estimates were obtained via Cox proportional hazards regression models with age as the underlying time scale, adjusting for sex and calendar time (model A) and further adjustment for other mental disorders that had onset before the prior disorder (model B). The line of unity is shown as a dotted line in each panel.
Time-Dependent Associations Between Mental Disorders
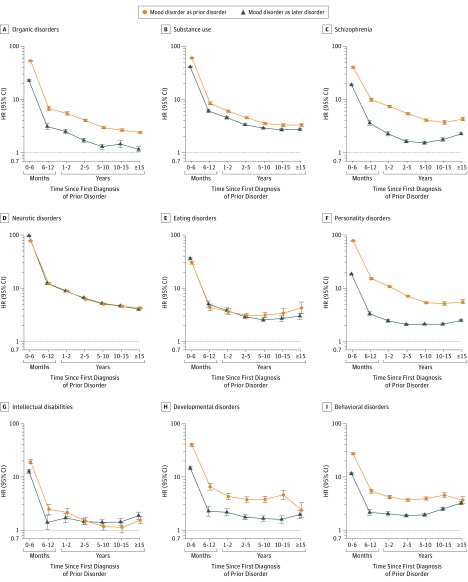
Figure 2 shows the HRs of receiving a diagnosis of each disorder depending on a previous diagnosis of mood disorders, and on the amount of time since this diagnosis. For example, the rate of receiving a diagnosis of neurotic disorders was almost 80 times higher in the first 6 months after receiving a diagnosis of mood disorders, compared with those without a diagnosis of mood disorders (HR, 77.8; 95% CI, 76.5-79.2). This is consistent with these 2 disorders co-occurring at or soon after the index occasion of service. After the first 6 months, the HR decreased considerably, but even after 15 years, affected individuals had a higher rate of receiving a diagnosis of incident neurotic disorders compared with those who had not received a diagnosis of mood disorders (HR, 4.3; 95% CI, 4.1-4.4). For other disorder pairs, we observed a similar pattern, with stronger associations in the first 6 months after an incident diagnosis of the prior disorder, which then diminished (eFigures 25-34 in the Supplement).
Figure 2. Lagged Associations Between Mood Disorders and All Other Disorders.
Hazard ratios (HRs) and 95% CIs are shown of receiving a diagnosis of each disorder comparing those with and without a prior diagnosis of mood disorders, and depending on time since the first diagnosis of mood disorders, and receiving a diagnosis of mood disorders comparing those with and without a prior diagnosis of each other disorder, and depending on time since the first diagnosis of the prior disorder. Estimates were obtained via Cox proportional hazards regression models with age as the underlying time scale, adjusting for sex, calendar time, and all other mental disorders that had onset before the prior disorder (model B). The reference category is persons without a diagnosis of mood disorders or persons without a diagnosis of the specific prior disorder. The line of unity is shown as a dotted line in each panel.
Bidirectional Patterns of Lagged HRs
The lagged HRs between certain groups of disorders were congruent regardless of the order of occurrence. For example, for pairs of disorders such as mood disorders and substance use, mood disorders and neurotic disorders, or mood disorders and eating disorders, the lagged estimates were nearly congruent regardless of the temporal order of the disorders (Figure 2). In contrast, while the lagged HRs for mood disorders and schizophrenia are still bidirectional (significantly increased HRs regardless of the sequence of disorders), the estimates for prior mood disorders and later schizophrenia are larger than the reciprocal pair of disorders. Full details of bidirectional lagged associations are shown in eFigures 35 to 54 in the Supplement.
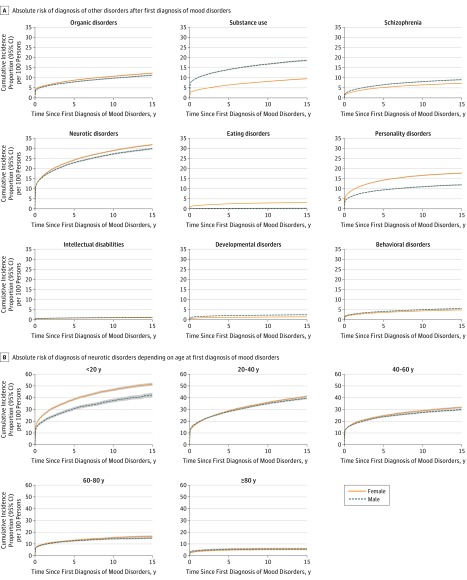
Time-Dependent Absolute Risks Between Mental Disorders
Figure 3A shows the sex- and time-specific absolute risk of receiving a diagnosis of each disorder for individuals who had previously received a diagnosis of a mood disorder. For example, approximately 10% of individuals who received a diagnosis of mood disorders subsequently also received a diagnosis of neurotic disorders within the first month (men, 10.7%; 95% CI, 10.4%-11.0%; women, 10.4%; 95% CI, 10.2%-10.7%). In the first 5 years after receiving a diagnosis of mood disorders, 22.9% (95% CI, 22.5%-23.3%) of men and 24.1% (95% CI, 23.8%-24.5%) of women received a diagnosis of neurotic disorders. These percentages were 27.2% (95% CI, 26.8%-27.7%) for men and 28.9% (95% CI, 28.6%-29.3%) for women after 10 years of a diagnosis of mood disorders. Absolute risks of neurotic disorders depending on age at receiving a diagnosis of mood disorders are presented in Figure 3B, showing higher risks when the diagnosis was received at a younger age. For example, for men and women with a diagnosis of mood disorders before 20 years of age, the absolute risks of developing neurotic disorders within 5 years were 30.6% (95% CI, 29.3%-32.0%) and 38.4% (95% CI, 37.5%-39.4%), respectively. Similar estimates for the other pairs of disorders are presented in eFigures 55 to 154 in the Supplement.
Figure 3. Absolute Risks of Receiving a Diagnosis of Each Disorder After a Prior Diagnosis of Mood Disorders.
A, Cumulative incidence proportions estimated across all ages of receiving a diagnosis of each later disorder after a prior diagnosis of mood disorders. B, Specific details of prior mood disorders and later neurotic disorders, stratified by age at diagnosis of mood disorders.
Discussion
In this population-based comprehensive study based on 5.9 million individuals and 83.9 million person-years, we provide a comprehensive map of pairwise comorbidity within mental disorders. Four key points are noteworthy. First, comorbidity was pervasive. Second, the lagged HRs for the onset of each type of later disorder were temporally patterned. Third, pairwise comorbidity was bidirectional. Fourth, some disorder pairs had appreciable absolute risks.
At the population level, the increased risk of comorbidity was pervasive across pairs of disorders. Our findings are broadly consistent with those of other comprehensive studies of comorbidity within mental disorders.4,10,12,13,24 Our study also allows us to contextualize the many previous register-based studies that have described comorbidity within a subset of disorders of interest: an increased risk of comorbidity between mental disorders is the rule, not the exception. All estimates were attenuated when adjusting for other mental disorders, which suggests that (additional) antecedent mental disorders may account for some of the effect observed for each specific pair of disorders.
We found a consistent pattern when we examined the lagged HRs between pairs of mental disorders. The rate of the later disorder was substantially higher within the first 6 months after the administrative onset of the prior disorder (compared with longer intervals). This rate may reflect appropriate diagnostic uncertainty during the early phase of a disorder, with more than 1 disorder being diagnosed within a short period. Although the size of the HRs between pairs of disorders decreased sharply during the first year after diagnosis, the estimates generally stabilized and then remained persistently elevated during the entire period of observation. Our findings support the pluripotent nature of mental disorders, especially in the early phases of disease progression.8
Significantly increased HRs were found for most pairs of mental disorders regardless of temporal order. Despite variation in the distributions of age of onset by mental disorder type,23 increased HRs were bidirectional. Within pairs of mental disorders with comparable ages of onset (eg, mood disorders and neurotic disorders), the lagged HRs were very similar regardless of the order of onset. This finding suggests that, for some pairs of disorders, the temporal order may be stochastic. The findings related to bidirectionality and persistence of elevated HRs over time support hypotheses that certain mental disorders share risk architectures. There is robust evidence that the structure of mental disorders is better described by underlying latent factors.9,25 This research has taken on added importance in light of the growing body of evidence from genetics indicating that different mental disorders share common gene variants.26
Because of the very large sample size available, we were able to explore absolute risk of developing later disorders, stratified by prior disorders, age, and sex. Certain pairs of disorders were accompanied with substantial absolute risks. For example, among individuals who develop a mood disorder before 20 years of age, 40% of men and 50% of women will subsequently develop an incident neurotic disorder within the next 15 years. To date, to our knowledge, few studies of comorbidity within mental disorders have provided absolute risks between disorders.12,13 To our knowledge, this is the first study to provide a comprehensive set of age- and sex-specific estimates of absolute risks associated with comorbid mental disorders.
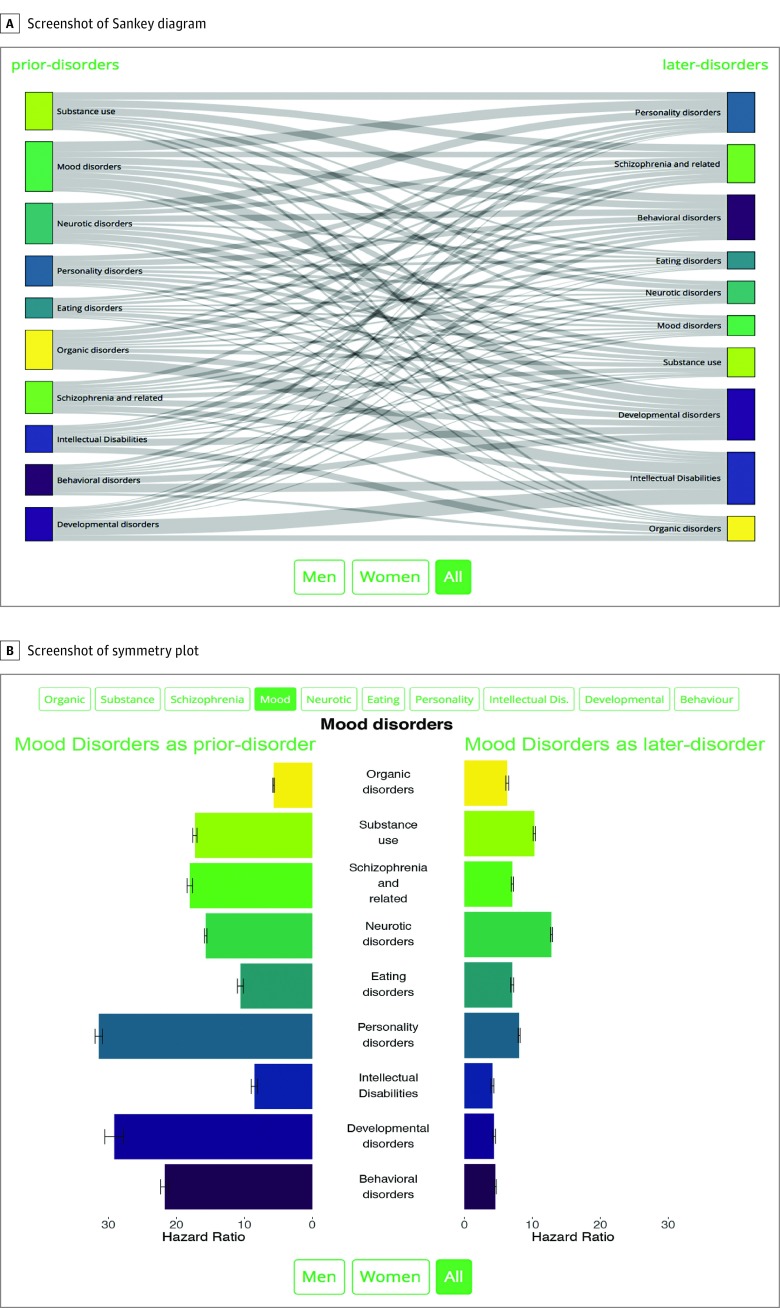
We hope that the provision of an easy-to-use interactive data visualization tool may assist clinicians in monitoring potential emerging comorbidity over time. The website allows data to be interrogated by selecting a range of options related to statistical models, linear or log scale, male and/or female sex, and options related to the mental disorders of interest (Figure 4). For example, the website can provide answers for specific questions such as: for women aged 20 to 30 years who develop an anxiety disorder, what are the absolute risks of developing depression in the next 5 years? Where appropriate, the primary prevention of secondary disorders27 may be indicated (eg, the prevention of subsequent substance use disorders in persons with prior mood or neurotic disorders). If clinicians and individuals with mental disorders had ready access to diagnosis-, age-, and sex-specific absolute risks of potential future comorbidity, this information could permit more tailored interventions and better education about self-management.
Figure 4. Screenshots of Sankey Diagram and Symmetry Plot Available in the Interactive Data Visualization Website.
A, Sankey diagram that shows the significant associations between all possible pairs of mental disorders. The site allows users to select male and/or female sex, or to show associations with a magnitude of effect larger than a certain threshold. B, Symmetry plot for mood disorders. On the left side, the associations in which mood disorders is the prior disorder are displayed; the bars represent the hazard ratio of receiving a diagnosis of each disorder, depending on whether persons have a previous diagnosis of mood disorders. On the right side, the associations in which mood disorders is the later disorder are displayed; the bars represent the hazard ratio of receiving a diagnosis of mood disorders, depending on whether persons have a previous diagnosis of each other disorder. The site allows users to select the main disorder of interest, male and/or female sex, linear or log scale, or different statistical models depending on potential confounders adjusted for. Dis indicates disabilities.
Strengths and Limitations
Our study has several strengths. Apart from its large sample size, the use of population-based registers allows for the inclusion of the entire population. In addition, health care is free in Denmark, further reducing the influence of selection bias. In addition, data are collected prospectively, and the potential for immortal time bias is thus practically negligible.
However, there are 5 important limitations of our study. First, in this initial article, we concentrated on pairs of mental disorders; however, the analyses adjusting for prior additional mental disorders indicate the need to explore more complex types of comorbidity. We will explore patterns of comorbidity in individuals with 3 or more types of disorders in future publications. Second, to make the current analyses tractable, we analyzed groups of disorders, rather than specific disorders. We will provide estimates for specific types of disorders in future publications. Third, we could investigate only mental disorders treated in secondary care; that is, individuals with untreated mental disorders, or those treated by a general practitioner, would not have been recorded. This issue would bias case identification to the more severe end of the clinical spectrum. With respect to understanding the consequence of this bias, access to a community-based survey of mental disorders (as in the World Mental Health Consortium) will allow us to explore these research questions in transnational data. Fourth, we relied on clinical diagnoses rather than structured diagnostic instruments frequently used in research settings. Not all register-based diagnoses have been validated in Denmark, but, where available, they have had good validity compared with research criteria.17,18,19,20,21,22 Fifth, the lifetime prevalence of mental disorders varies between countries28; thus, patterns of comorbidity identified in the Danish population may not generalize to other countries. We plan to undertake comparable studies of comorbidity within mental disorders based on cross-national community-based mental health surveys (which use reliable structured diagnostic interviews) to explore the influences of some of these factors on our findings.
Conclusions
To our knowledge, this is the largest and most detailed examination of comorbidity within mental disorders. Our findings provide new insights into the complex nature of comorbidity and the comprehensive nature of the analysis will provide an important foundation for future research. Our findings indicated that the risk of comorbidity was pervasive across all pairs of disorders and that this risk was temporally patterned. The risk of a later disorder was most prominent in the first year after the prior disorder, but the increased HRs persisted for at least 15 years after the onset of prior disorder. The provision of absolute risk estimates may facilitate the clinical translation of our findings, and lay the groundwork for future studies related to personalized medicine and the primary prevention of comorbidity.
eAppendix 1. Methods
eAppendix 2. Results
eTable. Baseline Characteristics of the Study Population
eFigures 1-154. Supplemental Figures
References
- 1.van den Akker M, Buntinx F, Knottnerus JA. Comorbidity or multimorbidity. Eur J Gen Pract. 1996;2:65-70. doi: 10.3109/13814789609162146 [DOI] [Google Scholar]
- 2.Feinstein AR. The pre-therapeutic classification of co-morbidity in chronic disease. J Chronic Dis. 1970;23(7):455-468. doi: 10.1016/0021-9681(70)90054-8 [DOI] [PubMed] [Google Scholar]
- 3.Andrews G, Slade T, Issakidis C. Deconstructing current comorbidity: data from the Australian National Survey of Mental Health and Well-Being. Br J Psychiatry. 2002;181:306-314. doi: 10.1192/bjp.181.4.306 [DOI] [PubMed] [Google Scholar]
- 4.Kessler RC, Avenevoli S, McLaughlin KA, et al. Lifetime co-morbidity of DSM-IV disorders in the US National Comorbidity Survey Replication Adolescent Supplement (NCS-A). Psychol Med. 2012;42(9):1997-2010. doi: 10.1017/S0033291712000025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Robins LN, Reigier DA. Psychiatric Disorders in America. New York, NY: Free Press; 1991. [Google Scholar]
- 6.Bijl RV, Ravelli A, van Zessen G. Prevalence of psychiatric disorder in the general population: results of The Netherlands Mental Health Survey and Incidence Study (NEMESIS). Soc Psychiatry Psychiatr Epidemiol. 1998;33(12):587-595. doi: 10.1007/s001270050098 [DOI] [PubMed] [Google Scholar]
- 7.Maj M. ‘Psychiatric comorbidity’: an artefact of current diagnostic systems? Br J Psychiatry. 2005;186(3):182-184. doi: 10.1192/bjp.186.3.182 [DOI] [PubMed] [Google Scholar]
- 8.McGorry P, Keshavan M, Goldstone S, et al. Biomarkers and clinical staging in psychiatry. World Psychiatry. 2014;13(3):211-223. doi: 10.1002/wps.20144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.de Jonge P, Wardenaar KJ, Lim CCW, et al. The cross-national structure of mental disorders: results from the World Mental Health Surveys. Psychol Med. 2018;48(12):2073-2084. doi: 10.1017/S0033291717003610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication [published correction appears in Gen Psychiatry. 2005;62(7):709]. Arch Gen Psychiatry. 2005;62(6):617-627. doi: 10.1001/archpsyc.62.6.617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moffitt TE, Caspi A, Taylor A, et al. How common are common mental disorders? evidence that lifetime prevalence rates are doubled by prospective versus retrospective ascertainment. Psychol Med. 2010;40(6):899-909. doi: 10.1017/S0033291709991036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maibing CF, Pedersen CB, Benros ME, Mortensen PB, Dalsgaard S, Nordentoft M. Risk of schizophrenia increases after all child and adolescent psychiatric disorders: a nationwide study. Schizophr Bull. 2015;41(4):963-970. doi: 10.1093/schbul/sbu119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ottosen C, Petersen L, Larsen JT, Dalsgaard S. Gender differences in associations between attention-deficit/hyperactivity disorder and substance use disorder. J Am Acad Child Adolesc Psychiatry. 2016;55(3):227-34.e4. doi: 10.1016/j.jaac.2015.12.010 [DOI] [PubMed] [Google Scholar]
- 14.McGrath JJ, Mortensen PB, Whiteford HA. Pragmatic psychiatric epidemiology—if you can’t count it, it won’t count. JAMA Psychiatry. 2018;75(2):111-112. doi: 10.1001/jamapsychiatry.2017.4184 [DOI] [PubMed] [Google Scholar]
- 15.Pedersen CB. The Danish Civil Registration System. Scand J Public Health. 2011;39(7)(suppl):22-25. doi: 10.1177/1403494810387965 [DOI] [PubMed] [Google Scholar]
- 16.Mors O, Perto GP, Mortensen PB. The Danish Psychiatric Central Research Register. Scand J Public Health. 2011;39(7)(suppl):54-57. doi: 10.1177/1403494810395825 [DOI] [PubMed] [Google Scholar]
- 17.Kessing L. Validity of diagnoses and other clinical register data in patients with affective disorder. Eur Psychiatry. 1998;13(8):392-398. doi: 10.1016/S0924-9338(99)80685-3 [DOI] [PubMed] [Google Scholar]
- 18.Phung TK, Andersen BB, Høgh P, Kessing LV, Mortensen PB, Waldemar G. Validity of dementia diagnoses in the Danish hospital registers. Dement Geriatr Cogn Disord. 2007;24(3):220-228. doi: 10.1159/000107084 [DOI] [PubMed] [Google Scholar]
- 19.Lauritsen MB, Jørgensen M, Madsen KM, et al. Validity of childhood autism in the Danish Psychiatric Central Register: findings from a cohort sample born 1990-1999. J Autism Dev Disord. 2010;40(2):139-148. doi: 10.1007/s10803-009-0818-0 [DOI] [PubMed] [Google Scholar]
- 20.Bock C, Bukh JD, Vinberg M, Gether U, Kessing LV. Validity of the diagnosis of a single depressive episode in a case register. Clin Pract Epidemiol Ment Health. 2009;5:4. doi: 10.1186/1745-0179-5-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mohr-Jensen C, Vinkel Koch S, Briciet Lauritsen M, Steinhausen HC. The validity and reliability of the diagnosis of hyperkinetic disorders in the Danish Psychiatric Central Research Registry. Eur Psychiatry. 2016;35:16-24. doi: 10.1016/j.eurpsy.2016.01.2427 [DOI] [PubMed] [Google Scholar]
- 22.Jakobsen KD, Frederiksen JN, Hansen T, Jansson LB, Parnas J, Werge T. Reliability of clinical ICD-10 schizophrenia diagnoses. Nord J Psychiatry. 2005;59(3):209-212. doi: 10.1080/08039480510027698 [DOI] [PubMed] [Google Scholar]
- 23.Pedersen CB, Mors O, Bertelsen A, et al. A comprehensive nationwide study of the incidence rate and lifetime risk for treated mental disorders. JAMA Psychiatry. 2014;71(5):573-581. doi: 10.1001/jamapsychiatry.2014.16 [DOI] [PubMed] [Google Scholar]
- 24.Kessler RC, Ormel J, Petukhova M, et al. Development of lifetime comorbidity in the World Health Organization world mental health surveys. Arch Gen Psychiatry. 2011;68(1):90-100. doi: 10.1001/archgenpsychiatry.2010.180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kotov R, Krueger RF, Watson D, et al. The Hierarchical Taxonomy of Psychopathology (HiTOP): a dimensional alternative to traditional nosologies. J Abnorm Psychol. 2017;126(4):454-477. doi: 10.1037/abn0000258 [DOI] [PubMed] [Google Scholar]
- 26.Huang J, Perlis RH, Lee PH, et al. Cross-disorder genomewide analysis of schizophrenia, bipolar disorder, and depression. Am J Psychiatry. 2010;167(10):1254-1263. doi: 10.1176/appi.ajp.2010.09091335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kessler RC, Price RH. Primary prevention of secondary disorders: a proposal and agenda. Am J Community Psychol. 1993;21(5):607-633. doi: 10.1007/BF00942174 [DOI] [PubMed] [Google Scholar]
- 28.Kessler RC, Angermeyer M, Anthony JC, et al. Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry. 2007;6(3):168-176. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix 1. Methods
eAppendix 2. Results
eTable. Baseline Characteristics of the Study Population
eFigures 1-154. Supplemental Figures