Abstract
This cohort study examines the incidence of dental caries in children and adolescents of varying income levels living in areas with vs without water fluoridation.
By age 11 years, an American child living in poverty has twice the level of dental caries (tooth decay) as one living at 3 times the poverty threshold.1 To achieve the Healthy People 2020 overarching goal of health equity, interventions must preferentially prevent disease at the lower end of the income distribution. Research conducted in Canada2 suggests that water fluoridation might reduce inequality, but that possibility has not been investigated in the United States. We used 2 nationally representative data sets to investigate whether water fluoridation attenuated income-related inequality in dental caries among US children and adolescents.
Methods
In this cross-sectional epidemiologic investigation, we merged county-level fluoridation data from the Centers for Disease Control and Prevention’s Water Fluoridation Reporting System with dental caries data from 1999-2004 and 2011-2014 cycles of the National Health and Nutrition Examination Survey (NHANES).3 Counties were classified as predominantly fluoridated where 75% or more of the population was served by fluoridated water and otherwise as less fluoridated. Dental caries was quantified as the sum of decayed and filled primary (ie, deciduous) tooth surfaces (dfs) for children aged 2 to 10 years (n = 5835), and the sum of decayed, missing, and filled permanent tooth surfaces (DMFS) for those aged 6 to 17 years (n = 8384). The University of North Carolina's Office of Human Research Ethics determined that this study does not constitute human subjects research. We regressed dental caries on family income to poverty ratio (modeled as a continuous variable), county fluoridation status (dichotomous variable), and the interaction of those variables, adjusting for survey cycle, age, sex, race/ethnicity, rural-urban location, and time since last dental visit. Analysis took account of the NHANES complex survey design, producing estimates for the US child and adolescent populations. Data analysis was conducted between July 2017 and September 2018; SAS, version 9.3 (SAS Institute Inc), software was used. Significance was determined at P < .05.
Results
Children in families with low income—but not those living in poverty—were less likely than other income groups to live in a predominantly fluoridated county (Table). Inverse income gradients in dental caries were most pronounced in the primary dentition.
Table. Characteristics of 11 093 US Children, County Fluoridation Coverage, and Dental Caries Experience for Primary and Permanent Dentitions, National Health and Nutrition Examination Survey 1999 to 2004 and 2011 to 2014a.
| Characteristic | Unweighted No. (Weighted %) | Age 2-10 y (n = 5835) | Age 6-17 y (n = 8384) | ||
|---|---|---|---|---|---|
| Predominantly Fluoridated, % (SE)b | dfs, Mean (SE) | Predominantly Fluoridated, % (SE)b | DMFS, Mean (SE) | ||
| Total | 11 093 (100.0) | 47.7 (4.8) | 3.9 (0.3) | 47.0 (4.5) | 2.0 (0.1) |
| Income to poverty ratio, FPL, % | |||||
| <50c | 1598 (9.4) | 56.9 (5.6) | 5.1 (0.5) | 56.3 (6.0) | 2.5 (0.2) |
| 50 to <100 | 2269 (15.4) | 46.4 (5.5) | 5.8 (0.6) | 47.1 (5.1) | 2.6 (0.3) |
| 100 to <200 | 3001 (24.8) | 41.3 (5.1) | 4.5 (0.3) | 42.8 (5.1) | 2.3 (0.1) |
| 200 to <300 | 1512 (16.2) | 42.5 (5.2) | 3.1 (0.4) | 39.8 (4.4) | 1.9 (0.2) |
| 300 to <400 | 989 (11.4) | 51.2 (6.0) | 3.0 (0.4) | 52.4 (6.0) | 1.6 (0.2) |
| ≥400 | 1724 (22.8) | 54.6 (6.3) | 1.9 (0.2) | 50.3 (5.5) | 1.6 (0.2) |
| Sex | |||||
| Male | 5630 (50.9) | 46.2 (4.8) | 4.3 (0.2) | 47.0 (4.4) | 1.9 (0.1) |
| Female | 5463 (49.1) | 49.2 (4.8) | 3.4 (0.3) | 47.0 (4.6) | 2.2 (0.1) |
| Race/ethnicity | |||||
| Non-Hispanic black | 3400 (14.4) | 73.8 (4.9) | 3.4 (0.3) | 72.0 (5.1) | 2.2 (0.2) |
| Hispanic | 3724 (19.4) | 56.2 (6.0) | 5.2 (0.4) | 54.0 (5.8) | 2.3 (0.1) |
| Other | 933 (7.0) | 48.7 (6.5) | 4.5 (0.6) | 51.5 (6.3) | 2.3 (0.3) |
| Non-Hispanic white | 3036 (59.2) | 37.9 (5.5) | 3.4 (0.3) | 38.3 (5.0) | 1.9 (0.1) |
Abbreviations: dfs, decayed and filled primary tooth surfaces; DMFS, decayed, missing, and filled permanent tooth surfaces; FPL, federal poverty level.
Analysis excluded participants with missing covariate data (n = 1555) as well as those who had lived in the United States for less than 1 y (n = 146) and those in counties in which community water systems became fluoridated during the observation period of 1999 and thereafter (n = 4095).
A total of 75% or more of a county population served by fluoridated community drinking water.
Federal poverty threshold.
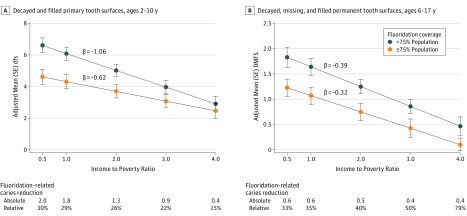
In predominantly fluoridated counties, the income gradient in dfs was attenuated by 41% (estimated slope [β] = –0.62; SE, 0.13) compared with less-fluoridated counties (β = –1.06; SE, 0.18) and the interaction was statistically significant (P = .03) (Figure, A). Absolute and relative fluoridation-related caries reductions were most pronounced for the lowest income level. For permanent teeth, there was 18% attenuation of the income gradient in DMFS in predominantly fluoridated counties (β = –0.32; SE, 0.06) compared with less-fluoridated counties (β = –0.39; SE, 0.08), although the interaction was not significant (P = .49) (Figure, B). The interaction with income was significant (P = .002) under a more restrictive assumption that the percentage of population living in a fluoridated area, when modeled as a continuous variable, has a linear effect on the income gradient in DMFS.
Figure. Predicted Covariate-Adjusted Number of Tooth Surfaces Affected by Dental Caries in the Primary and Permanent Dentitions (National Health and Nutrition Examination Surveys 1999-2004, 2011-2014), Stratified by County Population Coverage of Fluoridated Community Drinking Water.
Decayed and filled primary tooth surfaces in children aged 2 to 10 years (A) and decayed, missing, and filled permanent tooth surfaces in those aged 6 to 17 years (B). The values on the x-axis were selected to represent income to poverty ratio. Living in a predominantly fluoridated county reduced the magnitude of income inequalities in dental caries. This attenuation was statistically significant in the primary dentition (P value for interaction of .03) but failed to reach significance in the permanent dentition of those aged 6 to 17 years (P value for interaction, .49). Values were adjusted for sex, age, race/ethnicity, urban rural classification, and time since last dental visit. Tables below plots report mean fluoridation-related caries reductions as absolute differences (adjusted mean caries for <75% population coverage group minus ≥75% population coverage group) and relative differences (absolute difference divided by adjusted mean caries for <75% population coverage group) for selected values of income to poverty ratio. Data given below the plots report mean fluoridation-related caries reductions as absolute differences (adjusted mean caries for <75% population coverage group minus ≥75% population coverage group) and relative differences (absolute difference divided by adjusted mean caries for <75% population coverage group) for selected values of income to poverty ratio.
Discussion
To our knowledge, this is the first US study to show evidence that water fluoridation attenuates income-related inequalities in dental caries. The degree of attenuation was less pronounced in the permanent dentition, possibly because the level of decay was about half that of primary teeth. Greater attenuation in the permanent dentition might be seen in early adulthood, as the burden of DMFS doubles between adolescence and early adulthood.4
One limitation of this study is its cross-sectional study design, which restricts causal interpretations. Also, in the absence of information about individuals' consumption of water, county of residence was used as a proxy for exposure to fluoridation. The resulting misclassification of exposure likely biases measures of association towards the null.
These findings have public health relevance, as dental caries in the primary dentition affects one-half of children aged 6 to 8 years.3 In 2013, the United States spent $26.9 billion on child and adolescent oral health, exceeding the combined spending on asthma, upper respiratory tract infections, other infectious diseases, and anxiety.5 Economic modeling suggests that fluoridation of currently unfluoridated US communities with populations of 1000 or more would annually save $2.5 billion in costs related to dental caries.6 The current findings provide additional support for water fluoridation as a means toward the Healthy People 2020 goals of achieving health equity, eliminating disparities, and improving the health of all groups.
References
- 1.Slade GD, Sanders AE. Two decades of persisting income-disparities in dental caries among US children and adolescents. J Public Health Dent. 2018;78(3):187-191. doi: 10.1111/jphd.12261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McLaren L, Emery JC. Drinking water fluoridation and oral health inequities in Canadian children. Can J Public Health. 2012;103(7)(suppl 1):eS49-eS56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Slade GD, Grider WB, Maas WR, Sanders AE. Water fluoridation and dental caries in US children and adolescents. J Dent Res. 2018;97(10):1122-1128. doi: 10.1177/0022034518774331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dye BA, Tan S, Smith V, et al. . Trends in oral health status: United States, 1988-1994 and 1999-2004. Vital Health Stat 11. 2007;(248):1-92. [PubMed] [Google Scholar]
- 5.Bui AL, Dieleman JL, Hamavid H, et al. . Spending on children’s personal health care in the United States, 1996-2013. JAMA Pediatr. 2017;171(2):181-189. doi: 10.1001/jamapediatrics.2016.4086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.O’Connell J, Rockell J, Ouellet J, Tomar SL, Maas W. Costs and savings associated with community water fluoridation in the United States. Health Aff (Millwood). 2016;35(12):2224-2232. doi: 10.1377/hlthaff.2016.0881 [DOI] [PubMed] [Google Scholar]