Key Points
Question
What proportion of recommendations in current American College of Cardiology/American Heart Association (ACC/AHA) and European Society of Cardiology (ESC) guidelines are supported by evidence from multiple randomized controlled trials (RCTs), and how has this changed over the past 10 years?
Findings
In this systematic review of 51 current guideline documents that included 6329 recommendations, 8.5% of recommendations in ACC/AHA guidelines and 14.3% of recommendations in ESC guidelines were classified as level of evidence A (supported by evidence from multiple RCTs), compared with 11.5% of recommendations in a systematic review of ACC/AHA guidelines conducted in 2009.
Meaning
Among recommendations in major cardiovascular society guidelines from 2008 to 2018, the proportion supported by evidence from RCTs remains small.
Abstract
Importance
Clinical decisions are ideally based on evidence generated from multiple randomized controlled trials (RCTs) evaluating clinical outcomes, but historically, few clinical guideline recommendations have been based entirely on this type of evidence.
Objective
To determine the class and level of evidence (LOE) supporting current major cardiovascular society guideline recommendations, and changes in LOE over time.
Data Sources
Current American College of Cardiology/American Heart Association (ACC/AHA) and European Society of Cardiology (ESC) clinical guideline documents (2008-2018), as identified on cardiovascular society websites, and immediate predecessors to these guideline documents (1999-2014), as referenced in current guideline documents.
Study Selection
Comprehensive guideline documents including recommendations organized by class and LOE.
Data Extraction and Synthesis
The number of recommendations and the distribution of LOE (A [supported by data from multiple RCTs or a single, large RCT], B [supported by data from observational studies or a single RCT], and C [supported by expert opinion only]) were determined for each guideline document.
Main Outcomes and Measures
The proportion of guideline recommendations supported by evidence from multiple RCTs (LOE A).
Results
Across 26 current ACC/AHA guidelines (2930 recommendations; median, 121 recommendations per guideline [25th-75th percentiles, 76-155]), 248 recommendations (8.5%) were classified as LOE A, 1465 (50.0%) as LOE B, and 1217 (41.5%) as LOE C. The median proportion of LOE A recommendations was 7.9% (25th-75th percentiles, 0.9%-15.2%). Across 25 current ESC guideline documents (3399 recommendations; median, 130 recommendations per guideline [25th-75th percentiles, 111-154]), 484 recommendations (14.2%) were classified as LOE A, 1053 (31.0%) as LOE B, and 1862 (54.8%) as LOE C. When comparing current guidelines with prior versions, the proportion of recommendations that were LOE A did not increase in either ACC/AHA (median, 9.0% [current] vs 11.7% [prior]) or ESC guidelines (median, 15.1% [current] vs 17.6% [prior]).
Conclusions and Relevance
Among recommendations in major cardiovascular society guidelines, only a small percentage were supported by evidence from multiple RCTs or a single, large RCT. This pattern does not appear to have meaningfully improved from 2008 to 2018.
This systematic review of current and prior American College of Cardiology/American Heart Association and European Society of Cardiology guidelines summarizes the class and level of evidence (LOE) supporting guideline recommendations and changes in LOEs over time.
Introduction
In the late 1980s and early 1990s, evidence-based medicine, an approach that stresses the use of evidence from clinical research in clinical decision making, supplanted an older paradigm that valued accumulated wisdom and experience derived from unsystematic observation.1 Randomized controlled trials (RCTs), especially those that evaluate important clinical outcomes, and meta-analyses combining their results, represent the pinnacle of evidence under this framework because the randomization process attempts to equalize the distribution of unmeasured and unknown confounders, enabling investigators to compare competing treatments or strategies with the lowest risk of confounding.
Clinical guidelines for the care of patients with cardiovascular diseases, released by the American College of Cardiology/American Heart Association (ACC/AHA) and European Society of Cardiology (ESC) for more than 30 years, have integrated the evidence-based medicine framework by assigning a level of evidence (LOE) to each recommendation. Each recommendation is assigned an LOE that indicates whether the recommendation is based on multiple RCTs or a single, large RCT (LOE A), observational studies or a single RCT (LOE B), or expert opinion only (LOE C). Across a number of cardiovascular subfields, adherence to guideline recommendations translates the treatment benefits demonstrated in high-quality RCTs to improved patient outcomes.2,3,4
In a review of the ACC/AHA clinical practice guidelines from 2009, only 11% of recommendations were classified as LOE A.5 The authors called for greater collaboration among investigators and funders in identifying key research questions, development of streamlined clinical trial methods, and expansion of funding for clinical research. In the intervening years, some of these steps have been taken,6,7,8 but it is not known whether they have improved the evidence supporting cardiovascular guideline recommendations. This systematic review of current ACC/AHA and ESC guidelines and their immediate precursors was conducted to describe the evidence behind current guideline recommendations and changes in evidence over recent years.
Methods
Current ACC/AHA guidelines were identified as those posted on the ACC (https://www.acc.org/guidelines#doctype=Guidelines) and ESC (https://www.escardio.org/Guidelines/Clinical-Practice-Guidelines) websites as of February 1, 2019. Only comprehensive guideline documents were included in this systematic review; expert consensus documents, performance measures, and appropriateness criteria were not included because they do not report LOE. Focused updates were not included because they are not representative of the evidence base for an entire topic. Only guideline documents that included recommendations organized by class and LOE, clearly highlighted and separated from the rest of the text, were included for this analysis.
Current guideline documents were downloaded, and recommendations were abstracted by a single reviewer (A.C.F.) and validated by another reviewer (R.D.L). The reviewers recorded the number of recommendations included in each document, as well as the LOE (supported by data from multiple RCTs or a single, large RCT [LOE A]; supported by data from observational studies or a single RCT [LOE B]; supported by expert opinion only [LOE C]) and class for each. All recommendations are given a class that synthesizes the opinion of the guideline writing committee regarding the risks and benefits identified by the evidence and expert opinion. Class I recommendations are those for which there is evidence, general agreement, or both, that the treatment is useful or effective. Class IIa recommendations are those for which there is conflicting evidence or opinion, but the weight of evidence/opinion is in favor of the treatment’s usefulness, efficacy, or both; class IIb recommendations are those for which usefulness or efficacy is less well established. Class III recommendations are those for which there is evidence or general agreement that the treatment is not useful or effective and may be harmful.
Current guidelines were also reviewed to identify references to a previous iteration of the same guideline; for example, the 2014 AHA/ACC Guideline for the Management of Patients With Non–ST-Elevation Acute Coronary Syndromes was preceded by the 2007 ACC/AHA Guidelines for the Management of Patients With Unstable Angina/Non–ST-Elevation Myocardial Infarction.9,10 These previous iterations were then downloaded and abstracted, if they otherwise met inclusion criteria.
Recommendations in included guideline documents are clearly displayed statements highlighted and separated from the rest of the document text. Each recommendation has a clearly designated class of recommendation and LOE. Abstraction therefore involved simple reporting of the content of each document and did not require judgment on the part of the abstractors.
Data Presentation
We report the number of recommendations classified as LOE A, B, and C for each current guideline document, as well as the proportion of LOE A, B, and C recommendations by class. Because the number of recommendations included in a guideline document differ substantially by topic, we present the median proportion of recommendations with LOE A, B, and C for ACC/AHA guidelines and for ESC guidelines. We also categorized guideline documents by cardiovascular subspecialty area (electrophysiology, coronary artery disease, heart failure and myocardial disease, congenital and valvular heart disease, vascular medicine, preventive and general outpatient cardiology) and report the proportion of recommendations for each subspecialty area categorized as LOE A overall and by class of recommendation. We further report the median proportion of recommendations with LOE A, B, and C among guideline documents in each subspecialty area.
To identify changes in quality of evidence over time among current guidelines, we report the proportion of recommendations categorized as LOE A by year of guideline document release (2017-2018, 2015-2016, 2013-2014, and before 2014). We also report the proportion of recommendations categorized as LOE A in guideline documents released in the past 2 years (2017-2018) and those released before 2017. To further evaluate whether there has been a change in the evidence underpinning guideline recommendations, we compared the proportion of LOE A, B, and C recommendations in current guidelines with the proportion in prior guidelines. This procedure was performed separately for ACC/AHA and ESC guidelines. For topics that had both a current ACC/AHA and a current ESC guideline, we report the proportion of LOE A recommendations by society producing the guideline overall and by subspecialty area.
Results
Overall, LOEs from 26 current ACC/AHA guidelines (2930 recommendations) published between 2008 and 2018,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35 and from 25 current ESC guidelines (3399 recommendations) published between 2003 and 2018, were abstracted.36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60
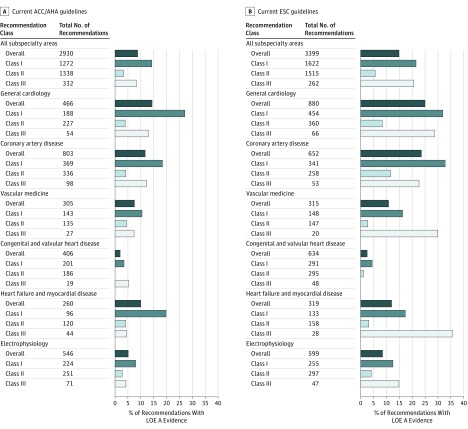
Across the 26 current ACC/AHA guidelines, 248 recommendations (8.5%) were classified as LOE A, 1465 (50.0%) as LOE B, and 1217 (41.5%) as LOE C (eTable 1 in the Supplement). Of 1272 class I recommendations, 180 (14.2%) were classified as LOE A. The median number of recommendations per guideline was 121 (25th-75th percentiles, 76-155), of which 7.9% (25th-75th percentiles, 0.9%-15.2%) were LOE A, 50.1% (25th-75th percentiles, 40.9%-58.4%) were LOE B, and 38.4% (25th-75th percentiles, 31.2%-49.0%) were LOE C. When guidelines were categorized by subspecialty area, the proportion of recommendations characterized as LOE A ranged from 2.0% (valvular and congenital heart disease) to 14.5% (general cardiology) (Figure 1, panel A). Overall, 1604 recommendations were classified as class I (“should do”) or class III (“should not do”). Of these recommendations, 207 (12.9%) were supported by LOE A evidence, 785 (48.9%) by LOE B evidence, and 612 (38.2%) by LOE C evidence.
Figure 1. Proportion of Recommendations Classified as Level of Evidence A Overall and by Class of Recommendation in the ACC/AHA and ESC Guidelines.
Although a greater proportion of class I (“should do”) and class III (“should not do”) recommendations are supported by level of evidence (LOE) A evidence and some subspecialties have a greater proportion of LOE A recommendations than others, less than 15% of guideline recommendations in all subspecialties are supported by LOE A evidence. Missing bars represent subspecialty area/class combinations for which 0% of recommendations are classified as LOE A. ACC/AHA indicates American College of Cardiology/American Heart Association; ESC, European Society of Cardiology.
Since 2015, ACC/AHA guidelines have indicated whether recommendations with LOE B were based on data from RCTs or observational studies. In the 8 guideline documents published since,11,12,13,14,15,16,34,35 there were a total of 543 recommendations with LOE B, and 144 of these recommendations (26.5%) were based on data from RCTs.
Across the 25 current ESC guidelines, 484 recommendations (14.2%) were classified as LOE A, 1053 (31.0%) as LOE B, and 1862 (54.8%) as LOE C. Of 1622 class I recommendations, 349 (21.5%) were LOE A. The median number of guideline recommendations was 130 (25th-75th percentiles, 111-154), of which 9.1% (25th-75th percentiles, 3.8%-23.1%) were LOE A, 32.6% (25th-75th percentiles, 20.5%-38.9%) were LOE B, and 50.0% (25th-75th percentiles, 40.3%-72.7%) were LOE C (eTable 2 in the Supplement). When guidelines were categorized by subspecialty area, the proportion of recommendations characterized as LOE A ranged from 2.5% (valvular and congenital heart disease) to 25.0% (general cardiology) (Figure 1, panel B). ESC guidelines contained 1884 class I and class III recommendations, 402 (21.3%) classified as LOE A, 548 (29.1%) as LOE B, and 934 (49.6%) as LOE C.
To identify trends over time, we compared evidence supporting recommendations from guideline documents written in the past 2 years (2017-2018) with that from other current guideline documents. In ACC/AHA guidelines, 5.7% of recommendations released in the past 2 years were supported by LOE A evidence compared with 9.5% of recommendations released earlier (eFigure in the Supplement). In ESC guidelines, 17.4% of recommendations released in the past 2 years were supported by LOE A evidence, compared with 12.8% of recommendations released earlier.
Changes From Prior to Current Guidelines
ACC/AHA Guidelines
Sixteen current ACC/AHA guideline documents, published between 2008 and 2018, had a prior document for comparison.10,12,14,15,16,17,19,21,23,24,25,26,27,28,33,34 These 16 documents contained a total of 2159 recommendations (median, 130). The 16 prior documents were published between 1999 and 2013 and included 3154 recommendations (median, 135).9,59,61,62,63,64,65,66,67,68,69,70,71,72,73,74
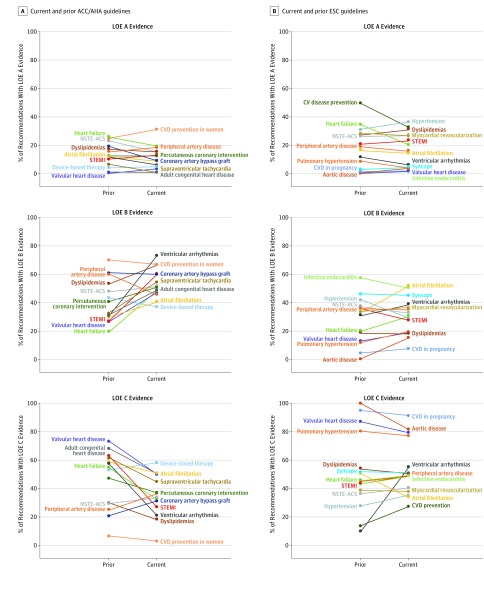
Among the 16 current ACC/AHA guideline documents with available prior guideline documents, the median proportion of LOE A recommendations was 9.0% (25th-75th percentiles, 4.8%-15.1%); the median proportion of LOE A recommendations in prior guidelines was 11.7% (25th-75th percentiles, 5.8%-17.5%) (Figure 2, panel A). Among class I recommendations, there was similarly no meaningful change in the proportion that were LOE A between current and prior guidelines (median, 16.1% in current vs 20.7% in prior). By contrast, when comparing the proportion of LOE B and C recommendations in prior ACC/AHA guidelines and current guidelines, the proportion of LOE B recommendations increased (median, 41.9% vs 51.0%) and the proportion of LOE C recommendations decreased (median, 51.9% vs 36.7%).
Figure 2. Proportion of Recommendations With Level of Evidence A, B, and C in Current and Prior Guideline Documents.
In all cases, a current guideline document is compared with its predecessor covering the same disease or topic area. ACC/AHA indicates American College of Cardiology/American Heart Association; CVD, cardiovascular disease; ESC, European Society of Cardiology; LOE, level of evidence; NSTE-ACS, acute coronary syndrome without ST-segment elevation; STEMI, ST-segment elevation myocardial infarction.
When looking at number rather than proportion of LOE A recommendations, findings were similar: The median number of LOE A recommendations in prior guidelines was 10.5 (25th-75th percentiles, 7.5-28.0) compared with 11.5 (25th-75th percentiles, 6.5-16.0) in current guidelines, and in 10 of 16 current/prior guideline dyads, there were more LOE A recommendations in the prior iteration of the guidelines.
ESC Guidelines
Sixteen current ESC guideline documents, published between 2014 and 2018, had a corresponding prior guideline document for comparison.36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51 These 16 documents included 2447 recommendations (median, 142). The 16 prior documents were published between 2004 and 2014 and included 2112 recommendations (median, 110).42,64,75,76,77,78,79,80,81,82,83,84,85,86,87,88
Among the 16 current ESC guideline documents with available prior guideline documents, the median proportion of LOE A recommendations was 15.1% (25th-75th percentiles, 3.7%-26.4%); the median proportion of LOE A recommendations among prior guidelines was 17.6% (25th-75th percentiles, 2.4%-27.6%) (Figure 2, panel B). Among class I recommendations, there was similarly little change in the proportion that were LOE A between current and prior guidelines (median, 26.9% in current vs 23.6% in prior). There were similarly small differences between current and prior guidelines in the proportion of recommendations that were LOE B (median, 31.7% [current] vs 33.4% [prior]) or LOE C (median, 49.3% [current] vs 48.0% [prior]).
When looking at number of recommendations, the median number of LOE A recommendations in current guideline documents was 21 (25th-75th percentiles, 4.7-37.2), compared with 26 (25th-75th percentiles, 2.5-35.2) in prior guideline documents.
Comparison Between ACC/AHA and ESC Guidelines
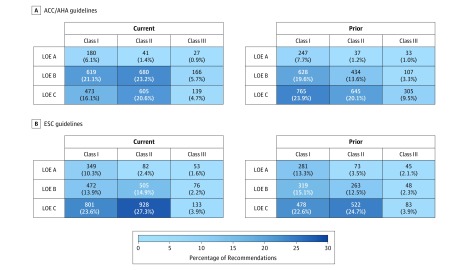
Among current guideline documents, 17 topics had both a current ESC and current ACC/AHA version. Among these guideline documents, 13.3% of recommendations in ESC guidelines and 7.5% of recommendations in ACC/AHA guidelines were supported by LOE A evidence. In 13 cases, the ESC guideline document had a greater proportion of recommendations supported by LOE A evidence. When guideline documents were grouped by subspecialty, ESC guidelines included a greater proportion of recommendations classified as LOE A in every subspecialty area except valvular and congenital heart disease (Figure 3). A greater proportion of recommendations in ESC guidelines, both current and prior, were class I, LOE A than in ACC/AHA guidelines (Figure 4).
Figure 3. Proportion of Recommendations With Level of Evidence A by Subspecialty Area in Topic Areas Covered by Both a Current American College of Cardiology/American Heart Association and European Society of Cardiology Guideline Document.
Numbers within the bars represent the total number of recommendations in each subspecialty area. In most subspecialty areas, a greater proportion of recommendations in European Society of Cardiology guidelines are supported by level of evidence (LOE) A evidence.
Figure 4. Proportion of Recommendations by Class and Level of Evidence in Current and Prior ACC/AHA and ESC Guidelines.
“Heat maps” shown represent 26 current and 16 prior American College of Cardiology/American Heart Association (ACC/AHA) guidelines and 25 current and 16 prior European Society of Cardiology (ESC) guidelines. Light blue squares represent low percentages; darker blue squares, high percentages.
Discussion
In this review of evidence supporting major society cardiovascular guidelines, less than 10% of recommendations from current ACC/AHA guidelines and less than 15% of recommendations from current ESC guidelines were supported by evidence from multiple high-quality RCTs and characterized as LOE A; approximately 80% of strong (class I or III) recommendations were not characterized as LOE A. Furthermore, there was wide variety by subject area—in some guideline documents, more than 33% of recommendations were characterized as LOE A, but others had no LOE A recommendations at all. Among guideline documents that have been updated, there was no meaningful change in the proportion or number of recommendations characterized as LOE A from prior to current guidelines. Taken together, these results demonstrate that efforts over the past decade to simplify and facilitate clinical trials have not yet translated into an evidence base better supported by RCTs.
In 2009, Tricoci et al5 analyzed data from ACC/AHA guidelines published from 1984 to 2008. At that time, 12% of guideline recommendations were classified as LOE A, including 19% of class I recommendations. Because LOEs were included in guidelines starting in 1998, Tricoci et al were only able to assess changes in LOE over time in 6 guideline documents, but in these 6 guideline documents, they found minimal increases in LOE A recommendations compared with LOE B and C. In follow-up to this effort, the evidence underlying guideline recommendations in other medical and surgical subspecialties was systematically reviewed in a number of studies. Overall, very few recommendations were supported by high-quality evidence from multiple RCTs.89,90,91,92,93,94,95,96,97,98,99
In the article by Tricoci et al, the authors pointed out many of the flaws in the clinical trial enterprise, including inefficiency, fragmentation, and reliance on industry funding, resulting in narrowly focused trials in highly selected populations, designed to achieve regulatory approval but not necessarily to provide useful evidence for patients, clinicians, and payers. The authors called for increased funding for practical clinical trials evaluating the comparative effectiveness of existing products, increased collaboration in setting a research agenda, and novel methods of conducting clinical trials with less waste. Over the last decade, public-private partnerships have been developed to fund clinical trials asking patient-centered questions,7 trial designs leveraging administrative data and existing registries to capture baseline characteristics and long-term outcomes have been deployed in service to these questions,6,100,101 and a series of meetings have brought leaders in various cardiovascular subfields together to collaboratively devise research agendas.102,103
The present study shows that, despite these efforts, the proportion of guideline recommendations supported by high-quality evidence did not increase. When directly comparing current guideline documents with prior documents covering the same topic there was similarly not a meaningful increase in recommendations with LOE A classification from the prior version to the current version of guidelines in either the ACC/AHA or ESC guidelines. Although it is possible that RCTs both convincingly answer a single question (leading to a single LOE A recommendation) and raise new questions (leading to multiple non–LOE A recommendations), the absolute number of LOE A recommendations did not meaningfully change from prior to current guideline iterations. In both the ACC/AHA and the ESC guidelines, the large majority of patient care recommendations were based on nonrandomized evidence, even class I (“should do”) and class III (“should not do”) recommendations. The lack of RCT evidence supporting most recommendations in the guidelines was compounded by variability among subspecialties within cardiovascular medicine; some subspecialty guidelines contained almost no LOE A recommendations. Although the ESC and ACC/AHA guidelines use similar evidence to generate recommendations, a greater proportion of recommendations overall in the ESC guidelines were classified as LOE A, highlighting differences in the way that these professional societies interpret data and make guideline recommendations, and/or hesitancy of guideline writing committees to categorize as LOE A recommendations based on evidence from RCTs that enrolled patients entirely in other regions of the world.
In the ACC/AHA guidelines, there was a small increase in the proportion of recommendations that were LOE B and a decrease in the proportion that were LOE C when comparing current and prior guideline documents. LOE B recommendations are supported either by observational studies or single RCTs, so this increase in LOE B recommendations could indicate that the proportion of recommendations supported by randomized evidence is increasing; however, relatively few LOE B recommendations were supported by randomized evidence. More likely, the increase in LOE B recommendations from prior to current ACC/AHA guideline documents can be explained, at least in part, by the elaboration of new observational “big data” sources and application of advanced statistical methods, which have led researchers to ask and answer questions using observational study designs.104 Although evidence generated from such studies is valuable in many circumstances, comparative effectiveness analyses using observational data are limited by residual confounding, and in most circumstances a well-conducted RCT is the only study design that enables a true comparison (and cause-effect relationship assessment) between 2 medications, procedures, or treatment strategies.104 In a review of cardiology guidelines, 19% of class I recommendations supported by 1 RCT or observational evidence only, and more than 25% of class I recommendations supported by expert opinion only, were downgraded or reversed in the next edition of the guidelines, compared with less than 10% of recommendations supported by higher-quality evidence.105
Solid RCT evidence delineates treatments and strategies that lead to better patient outcomes, which can then be implemented in clinical practice.106 By contrast, in the absence of RCT evidence, the association between clinical practices and outcomes is less certain. The decline in cardiovascular mortality has decelerated over the past several years.107 Efforts to bolster the evidence base—eg, pragmatic clinical trials, registry-based clinical trials, and clinical trials conducted within health systems—may help forestall this trend.
Limitations
This study has several limitations. First, the evidence supporting major society guideline recommendations is a surrogate for the totality of the evidence in cardiology, rather than a direct measurement. The quality of evidence supporting each recommendation was not independently assessed, and it is possible that an increasing proportion of LOE B recommendations are supported by RCT evidence that is insufficient to characterize as LOE A. Similarly, the proportion of guideline recommendations supported by LOE A evidence may not be a perfect surrogate for the totality of evidence, because advances in the field may make prior guideline recommendations obsolete and thus removed from the next edition of the guidelines. Alternatively, standards for LOE A designation may have changed over time.
Second, exclusion of focused updates, which are usually undertaken when new RCT evidence is generated, may lead to underestimation of the proportion of LOE A recommendations; however, this limitation should not affect findings regarding changes in LOE over time.
Third, this review describes only evidence supporting cardiology guidelines, rather than across medical and surgical subspecialties; however, prior studies have shown a low level of high-quality evidence in other fields. Moreover, the high global prevalence of cardiovascular disease suggests that efforts to build a higher-quality cardiovascular medicine evidence base might have a large effect on global health.
Conclusions
Among recommendations in major cardiovascular society guidelines, only a small percentage were supported by evidence from multiple RCTs or a single, large RCT. This pattern does not appear to have meaningfully improved from 2008 to 2018.
eTable 1. Levels of Evidence by Guideline and Category of Recommendation (ACC/AHA Guidelines)
eTable 2. Levels of Evidence by Guideline and Category of Recommendation (ESC Guidelines)
eFigure. Proportion of Recommendations Characterized as Level of Evidence A by Year of Guideline Document Release
eReferences
References
- 1.Evidence-Based Medicine Working Group Evidence-based medicine: a new approach to teaching the practice of medicine. JAMA. 1992;268(17):2420-2425. doi: 10.1001/jama.1992.03490170092032 [DOI] [PubMed] [Google Scholar]
- 2.Mehta RH, Chen AY, Alexander KP, Ohman EM, Roe MT, Peterson ED. Doing the right things and doing them the right way: association between hospital guideline adherence, dosing safety, and outcomes among patients with acute coronary syndrome. Circulation. 2015;131(11):980-987. doi: 10.1161/CIRCULATIONAHA.114.013451 [DOI] [PubMed] [Google Scholar]
- 3.Komajda M, Cowie MR, Tavazzi L, Ponikowski P, Anker SD, Filippatos GS; QUALIFY Investigators . Physicians’ guideline adherence is associated with better prognosis in outpatients with heart failure with reduced ejection fraction: the QUALIFY international registry. Eur J Heart Fail. 2017;19(11):1414-1423. doi: 10.1002/ejhf.887 [DOI] [PubMed] [Google Scholar]
- 4.Lip GY, Laroche C, Popescu MI, et al. . Improved outcomes with European Society of Cardiology guideline-adherent antithrombotic treatment in high-risk patients with atrial fibrillation: a report from the EORP-AF General Pilot Registry. Europace. 2015;17(12):1777-1786. doi: 10.1093/europace/euv269 [DOI] [PubMed] [Google Scholar]
- 5.Tricoci P, Allen JM, Kramer JM, Califf RM, Smith SC Jr. Scientific evidence underlying the ACC/AHA clinical practice guidelines. JAMA. 2009;301(8):831-841. doi: 10.1001/jama.2009.205 [DOI] [PubMed] [Google Scholar]
- 6.James S, Rao SV, Granger CB. Registry-based randomized clinical trials—a new clinical trial paradigm. Nat Rev Cardiol. 2015;12(5):312-316. doi: 10.1038/nrcardio.2015.33 [DOI] [PubMed] [Google Scholar]
- 7.Hernandez AF, Fleurence RL, Rothman RL. The ADAPTABLE trial and PCORnet: shining light on a new research paradigm. Ann Intern Med. 2015;163(8):635-636. doi: 10.7326/M15-1460 [DOI] [PubMed] [Google Scholar]
- 8.Psaty BM, Breckenridge AM. Mini-Sentinel and regulatory science—big data rendered fit and functional. N Engl J Med. 2014;370(23):2165-2167. doi: 10.1056/NEJMp1401664 [DOI] [PubMed] [Google Scholar]
- 9.Anderson JL, Adams CD, Antman EM, et al. ; American College of Cardiology; American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction); American College of Emergency Physicians; Society for Cardiovascular Angiography and Interventions; Society of Thoracic Surgeons; American Association of Cardiovascular and Pulmonary Rehabilitation; Society for Academic Emergency Medicine . ACC/AHA 2007 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction. J Am Coll Cardiol. 2007;50(7):e1-e157. doi: 10.1016/j.jacc.2007.02.013 [DOI] [PubMed] [Google Scholar]
- 10.Amsterdam EA, Wenger NK, Brindis RG, et al. . 2014 AHA/ACC Guideline for the Management of Patients With Non-ST-Elevation Acute Coronary Syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;64(24):e139-e228. doi: 10.1016/j.jacc.2014.09.017 [DOI] [PubMed] [Google Scholar]
- 11.Whelton PK, Carey RM, Aronow WS, et al. . 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/Pcna Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71(19):e127-e248. doi: 10.1016/j.jacc.2017.11.006 [DOI] [PubMed] [Google Scholar]
- 12.Stout KK, Daniels CJ, Aboulhosn JA, et al. . AHA/ACC Guideline for the Management of Adults With Congenital Heart Disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines [published online August 10, 2019]. J Am Coll Cardiol. 2018. doi: 10.1161/CIR.0000000000000602 [DOI] [PubMed] [Google Scholar]
- 13.Shen WK, Sheldon RS, Benditt DG, et al. . 2017 ACC/AHA/HRS Guideline for the Evaluation and Management of Patients With Syncope: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2017;70(5):e39-e110. doi: 10.1016/j.jacc.2017.03.003 [DOI] [PubMed] [Google Scholar]
- 14.Gerhard-Herman MD, Gornik HL, Barrett C, et al. . 2016 AHA/ACC Guideline on the Management of Patients With Lower Extremity Peripheral Artery Disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2017;69(11):e71-e126. doi: 10.1016/j.jacc.2016.11.007 [DOI] [PubMed] [Google Scholar]
- 15.Al-Khatib SM, Stevenson WG, Ackerman MJ, et al. . 2017 AHA/ACC/HRS Guideline for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2018;72(14):e91-e220. doi: 10.1016/j.jacc.2017.10.054 [DOI] [PubMed] [Google Scholar]
- 16.Page RL, Joglar JA, Caldwell MA, et al. . 2015 ACC/AHA/HRS Guideline for the Management of Adult Patients With Supraventricular Tachycardia: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2016;67(13):e27-e115. doi: 10.1016/j.jacc.2015.08.856 [DOI] [PubMed] [Google Scholar]
- 17.Nishimura RA, Otto CM, Bonow RO, et al. ; American College of Cardiology/American Heart Association Task Force on Practice Guidelines . 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease. J Am Coll Cardiol. 2014;63(22):e57-e185. doi: 10.1016/j.jacc.2014.02.536 [DOI] [PubMed] [Google Scholar]
- 18.Jensen MD, Ryan DH, Apovian CM, et al. ; American College of Cardiology/American Heart Association Task Force on Practice Guidelines; Obesity Society . 2013 AHA/ACC/TOS Guideline for the Management of Overweight and Obesity in Adults. J Am Coll Cardiol. 2014;63(25, pt B):2985-3023. doi: 10.1016/j.jacc.2013.11.004 [DOI] [PubMed] [Google Scholar]
- 19.January CT, Wann LS, Alpert JS, et al. ; American College of Cardiology/American Heart Association Task Force on Practice Guidelines . 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation. J Am Coll Cardiol. 2014;64(21):e1-e76. doi: 10.1016/j.jacc.2014.03.022 [DOI] [PubMed] [Google Scholar]
- 20.Goff DC Jr, Lloyd-Jones DM, Bennett G, et al. ; American College of Cardiology/American Heart Association Task Force on Practice Guidelines . 2013 ACC/AHA Guideline on the Assessment of Cardiovascular Risk. J Am Coll Cardiol. 2014;63(25, pt B):2935-2959. doi: 10.1016/j.jacc.2013.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fleisher LA, Fleischmann KE, Auerbach AD, et al. ; American College of Cardiology; American Heart Association . 2014 ACC/AHA Guideline on Perioperative Cardiovascular Evaluation and Management of Patients Undergoing Noncardiac Surgery. J Am Coll Cardiol. 2014;64(22):e77-e137. doi: 10.1016/j.jacc.2014.07.944 [DOI] [PubMed] [Google Scholar]
- 22.Eckel RH, Jakicic JM, Ard JD, et al. ; American College of Cardiology/American Heart Association Task Force on Practice Guidelines . 2013 AHA/ACC Guideline on Lifestyle Management to Reduce Cardiovascular Risk. J Am Coll Cardiol. 2014;63(25, pt B):2960-2984. doi: 10.1016/j.jacc.2013.11.003 [DOI] [PubMed] [Google Scholar]
- 23.Yancy CW, Jessup M, Bozkurt B, et al. ; American College of Cardiology Foundation; American Heart Association Task Force on Practice Guidelines . 2013 ACCF/AHA Guideline for the Management of Heart Failure. J Am Coll Cardiol. 2013;62(16):e147-e239. doi: 10.1016/j.jacc.2013.05.019 [DOI] [PubMed] [Google Scholar]
- 24.O’Gara PT, Kushner FG, Ascheim DD, et al. . 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;61(4):e78-e140. doi: 10.1016/j.jacc.2012.11.019 [DOI] [PubMed] [Google Scholar]
- 25.Fihn SD, Gardin JM, Abrams J, et al. ; American College of Cardiology Foundation; American Heart Association Task Force on Practice Guidelines; American College of Physicians; American Association for Thoracic Surgery; Preventive Cardiovascular Nurses Association; Society for Cardiovascular Angiography and Interventions; Society of Thoracic Surgeons . 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the Diagnosis and Management of Patients With Stable Ischemic Heart Disease. J Am Coll Cardiol. 2012;60(24):e44-e164. doi: 10.1016/j.jacc.2012.07.013 [DOI] [PubMed] [Google Scholar]
- 26.Mosca L, Benjamin EJ, Berra K, et al. ; American Heart Association . Effectiveness-based guidelines for the prevention of cardiovascular disease in women—2011 update. J Am Coll Cardiol. 2011;57(12):1404-1423. doi: 10.1016/j.jacc.2011.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Levine GN, Bates ER, Blankenship JC, et al. ; American College of Cardiology Foundation; American Heart Association Task Force on Practice Guidelines; Society for Cardiovascular Angiography and Interventions . 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention. J Am Coll Cardiol. 2011;58(24):e44-e122. doi: 10.1016/j.jacc.2011.08.007 [DOI] [PubMed] [Google Scholar]
- 28.Hillis LD, Smith PK, Anderson JL, et al. ; American College of Cardiology Foundation; American Heart Association Task Force on Practice Guidelines; American Association for Thoracic Surgery; Society of Cardiovascular Anesthesiologists; Society of Thoracic Surgeons . 2011 ACCF/AHA Guideline for Coronary Artery Bypass Graft Surgery. J Am Coll Cardiol. 2011;58(24):e123-e210. doi: 10.1016/j.jacc.2011.08.009 [DOI] [PubMed] [Google Scholar]
- 29.Gersh BJ, Maron BJ, Bonow RO, et al. ; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines . 2011 ACCF/AHA Guideline for the Diagnosis and Treatment of Hypertrophic Cardiomyopathy. J Am Coll Cardiol. 2011;58(25):e212-e260. doi: 10.1016/j.jacc.2011.06.011 [DOI] [PubMed] [Google Scholar]
- 30.Brott TG, Halperin JL, Abbara S, et al. . 2011 ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/SCAI/SIR/SNIS/SVM/SVS Guideline on the Management of Patients With Extracranial Carotid and Vertebral Artery Disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American Stroke Association, American Association of Neuroscience Nurses, American Association of Neurological Surgeons, American College of Radiology, American Society of Neuroradiology, Congress of Neurological Surgeons, Society of Atherosclerosis Imaging and Prevention, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of NeuroInterventional Surgery, Society for Vascular Medicine, and Society for Vascular Surgery. J Am Coll Cardiol. 2011;57(8):e16-e94. doi: 10.1016/j.jacc.2010.11.006 [DOI] [PubMed] [Google Scholar]
- 31.Hiratzka LF, Bakris GL, Beckman JA, et al. ; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines; American Association for Thoracic Surgery; American College of Radiology; American Stroke Association; Society of Cardiovascular Anesthesiologists; Society for Cardiovascular Angiography and Interventions; Society of Interventional Radiology; Society of Thoracic Surgeons; Society for Vascular Medicine . 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM Guidelines for the Diagnosis and Management of Patients With Thoracic Aortic Disease. J Am Coll Cardiol. 2010;55(14):e27-e129. doi: 10.1016/j.jacc.2010.02.015 [DOI] [PubMed] [Google Scholar]
- 32.Greenland P, Alpert JS, Beller GA, et al. ; American College of Cardiology Foundation; American Heart Association . 2010 ACCF/AHA Guideline for Assessment of Cardiovascular Risk in Asymptomatic Adults. J Am Coll Cardiol. 2010;56(25):e50-e103. doi: 10.1016/j.jacc.2010.09.001 [DOI] [PubMed] [Google Scholar]
- 33.Epstein AE, DiMarco JP, Ellenbogen KA, et al. ; American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices); American Association for Thoracic Surgery; Society of Thoracic Surgeons . ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities. J Am Coll Cardiol. 2008;51(21):e1-e62. doi: 10.1016/j.jacc.2008.02.032 [DOI] [PubMed] [Google Scholar]
- 34.Grundy SM, Stone NJ, Bailey AL, et al. . AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol [published online November 10, 2018]. J Am Coll Cardiol. 2018. doi: 10.1016/j.jacc.2018.11.003 [DOI] [Google Scholar]
- 35.Kusumoto FM, Schoenfeld MH, Barrett C, et al. . ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay [published online November 6, 2018]. J Am Coll Cardiol. 2018. doi: 10.1016/j.jacc.2018.10.044 [DOI] [Google Scholar]
- 36.Williams B, Mancia G, Spiering W, et al. ; ESC Scientific Document Group . 2018 ESC/ESH Guidelines for the Management of Arterial Hypertension. Eur Heart J. 2018;39(33):3021-3104. doi: 10.1093/eurheartj/ehy339 [DOI] [PubMed] [Google Scholar]
- 37.Regitz-Zagrosek V, Roos-Hesselink JW, Bauersachs J, et al. ; ESC Scientific Document Group . 2018 ESC Guidelines for the Management of Cardiovascular Diseases During Pregnancy. Eur Heart J. 2018;39(34):3165-3241. doi: 10.1093/eurheartj/ehy340 [DOI] [PubMed] [Google Scholar]
- 38.Neumann FJ, Sousa-Uva M, Ahlsson A, et al. ; ESC Scientific Document Group . 2018 ESC/EACTS Guidelines on Myocardial Revascularization. Eur Heart J. 2019;40(2):87-165. doi: 10.1093/eurheartj/ehy855 [DOI] [PubMed] [Google Scholar]
- 39.Ibanez B, James S, Agewall S, et al. ; ESC Scientific Document Group . 2017 ESC Guidelines for the Management of Acute Myocardial Infarction in Patients Presenting With ST-Segment Elevation. Eur Heart J. 2018;39(2):119-177. doi: 10.1093/eurheartj/ehx393 [DOI] [PubMed] [Google Scholar]
- 40.Brignole M, Moya A, de Lange FJ, et al. ; ESC Scientific Document Group . 2018 ESC Guidelines for the Diagnosis and Management of Syncope. Eur Heart J. 2018;39(21):1883-1948. doi: 10.1093/eurheartj/ehy037 [DOI] [PubMed] [Google Scholar]
- 41.Aboyans V, Ricco JB, Bartelink MEL, et al. ; ESC Scientific Document Group . 2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in collaboration with the European Society for Vascular Surgery (ESVS). Eur Heart J. 2018;39(9):763-816. doi: 10.1093/eurheartj/ehx095 [DOI] [PubMed] [Google Scholar]
- 42.Baumgartner H, Falk V, Bax JJ, et al. ; ESC Scientific Document Group . 2017 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J. 2017;38(36):2739-2791. doi: 10.1093/eurheartj/ehx391 [DOI] [PubMed] [Google Scholar]
- 43.Roffi M, Patrono C, Collet JP, et al. ; ESC Scientific Document Group . 2015 ESC Guidelines for the Management of Acute Coronary Syndromes in Patients Presenting Without Persistent ST-Segment Elevation. Eur Heart J. 2016;37(3):267-315. doi: 10.1093/eurheartj/ehv320 [DOI] [PubMed] [Google Scholar]
- 44.Ponikowski P, Voors AA, Anker SD, et al. ; ESC Scientific Document Group . 2016 ESC Guidelines for the Diagnosis and Treatment of Acute and Chronic Heart Failure. Eur Heart J. 2016;37(27):2129-2200. doi: 10.1093/eurheartj/ehw128 [DOI] [PubMed] [Google Scholar]
- 45.Piepoli MF, Hoes AW, Agewall S, et al. ; ESC Scientific Document Group . 2016 European Guidelines on Cardiovascular Disease Prevention in Clinical Practice. Eur Heart J. 2016;37(29):2315-2381. doi: 10.1093/eurheartj/ehw106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kirchhof P, Benussi S, Kotecha D, et al. ; ESC Scientific Document Group . 2016 ESC Guidelines for the Management of Atrial Fibrillation developed in collaboration with EACTS. Eur Heart J. 2016;37(38):2893-2962. doi: 10.1093/eurheartj/ehw210 [DOI] [PubMed] [Google Scholar]
- 47.Galiè N, Humbert M, Vachiery JL, et al. ; ESC Scientific Document Group . 2015 ESC/ERS Guidelines for the Diagnosis and Treatment of Pulmonary Hypertension. Eur Heart J. 2016;37(1):67-119. doi: 10.1093/eurheartj/ehv317 [DOI] [PubMed] [Google Scholar]
- 48.Catapano AL, Graham I, De Backer G, et al. ; ESC Scientific Document Group . 2016 ESC/EAS Guidelines for the Management of Dyslipidaemias. Eur Heart J. 2016;37(39):2999-3058. doi: 10.1093/eurheartj/ehw272 [DOI] [PubMed] [Google Scholar]
- 49.Priori SG, Blomström-Lundqvist C, Mazzanti A, et al. ; ESC Scientific Document Group . 2015 ESC Guidelines for the Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death. Eur Heart J. 2015;36(41):2793-2867. doi: 10.1093/eurheartj/ehv316 [DOI] [PubMed] [Google Scholar]
- 50.Habib G, Lancellotti P, Antunes MJ, et al. ; ESC Scientific Document Group . 2015 ESC Guidelines for the Management of Infective Endocarditis. Eur Heart J. 2015;36(44):3075-3128. doi: 10.1093/eurheartj/ehv319 [DOI] [PubMed] [Google Scholar]
- 51.Adler Y, Charron P, Imazio M, et al. ; ESC Scientific Document Group . 2015 ESC Guidelines for the Diagnosis and Management of Pericardial Diseases. Eur Heart J. 2015;36(42):2921-2964. doi: 10.1093/eurheartj/ehv318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kristensen SD, Knuuti J, Saraste A, et al. . 2014 ESC/ESA Guidelines on Non-Cardiac Surgery: cardiovascular assessment and management: the Joint Task Force on Non-cardiac Surgery: Cardiovascular Assessment and Management of the European Society of Cardiology (ESC) and the European Society of Anaesthesiology (ESA). Eur Heart J. 2014;35(35):2383-2431. doi: 10.1093/eurheartj/ehu282 [DOI] [PubMed] [Google Scholar]
- 53.Konstantinides SV, Torbicki A, Agnelli G, et al. ; Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC) . 2014 ESC Guidelines on the Diagnosis and Management of Acute Pulmonary Embolism. Eur Heart J. 2014;35(43):3033-3069. doi: 10.1093/eurheartj/ehu283 [DOI] [PubMed] [Google Scholar]
- 54.Erbel R, Aboyans V, Boileau C, et al. ; ESC Committee for Practice Guidelines; Task Force for the Diagnosis and Treatment of Aortic Diseases of the European Society of Cardiology (ESC) . 2014 ESC Guidelines on the Diagnosis and Treatment of Aortic Diseases: document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. Eur Heart J. 2014;35(41):2873-2926. doi: 10.1093/eurheartj/ehu281 [DOI] [PubMed] [Google Scholar]
- 55.Montalescot G, Sechtem U, Achenbach S, et al. . 2013 ESC Guidelines on the Management of Stable Coronary Artery Disease: the Task Force on the Management of Stable Coronary Artery Disease of the European Society of Cardiology. Eur Heart J. 2013;34(38):2949-3003. doi: 10.1093/eurheartj/eht296 [DOI] [PubMed] [Google Scholar]
- 56.Brignole M, Auricchio A, Baron-Esquivias G, et al. . 2013 ESC Guidelines on Cardiac Pacing and Cardiac Resynchronization Therapy: the Task Force on Cardiac Pacing and Resynchronization Therapy of the European Society of Cardiology (ESC) developed in collaboration with the European Heart Rhythm Association (EHRA). Eur Heart J. 2013;34(29):2281-2329. doi: 10.1093/eurheartj/eht150 [DOI] [PubMed] [Google Scholar]
- 57.Rydén L, Grant PJ, Anker SD, et al. . ESC Guidelines on Diabetes, Pre-diabetes, and Cardiovascular Diseases developed in collaboration with the EASD: the Task Force on Diabetes, Pre-diabetes, and Cardiovascular Diseases of the European Society of Cardiology (ESC) and developed in collaboration with the European Association for the Study of Diabetes (EASD). Eur Heart J. 2013;34(39):3035-3087. doi: 10.1093/eurheartj/eht108 [DOI] [PubMed] [Google Scholar]
- 58.Baumgartner H, Bonhoeffer P, De Groot NM, et al. ; Task Force on the Management of Grown-up Congenital Heart Disease of the European Society of Cardiology (ESC); Association for European Paediatric Cardiology (AEPC); ESC Committee for Practice Guidelines (CPG) . ESC guidelines for the management of grown-up congenital heart disease (new version 2010). Eur Heart J. 2010;31(23):2915-2957. doi: 10.1093/eurheartj/ehq249 [DOI] [PubMed] [Google Scholar]
- 59.Blomström-Lundqvist C, Scheinman MM, Aliot EM, et al. ; European Society of Cardiology Committee, NASPE-Heart Rhythm Society . ACC/AHA/ESC Guidelines for the Management of Patients With Supraventricular Arrhythmias—executive summary. J Am Coll Cardiol. 2003;42(8):1493-1531. [DOI] [PubMed] [Google Scholar]
- 60.Elliott PM, Anastasakis A, Borger MA, et al. . 2014 ESC Guidelines on Diagnosis and Management of Hypertrophic Cardiomyopathy: the Task Force for the Diagnosis and Management of Hypertrophic Cardiomyopathy of the European Society of Cardiology (ESC). Eur Heart J. 2014;35(39):2733-2779. doi: 10.1093/eurheartj/ehu284 [DOI] [PubMed] [Google Scholar]
- 61.Warnes CA, Williams RG, Bashore TM, et al. . ACC/AHA 2008 Guidelines for the Management of Adults With Congenital Heart Disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Develop Guidelines on the Management of Adults With Congenital Heart Disease) developed in collaboration with the American Society of Echocardiography, Heart Rhythm Society, International Society for Adult Congenital Heart Disease, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2008;52(23):e143-e263. doi: 10.1016/j.jacc.2008.10.001 [DOI] [PubMed] [Google Scholar]
- 62.Mosca L, Banka CL, Benjamin EJ, et al. ; Expert Panel/Writing Group; American Heart Association; American Academy of Family Physicians; American College of Obstetricians and Gynecologists; American College of Cardiology Foundation; Society of Thoracic Surgeons; American Medical Women’s Association; Centers for Disease Control and Prevention; Office of Research on Women’s Health; Association of Black Cardiologists; American College of Physicians; World Heart Federation; National Heart, Lung, and Blood Institute; American College of Nurse Practitioners . Evidence-based guidelines for cardiovascular disease prevention in women: 2007 update. Circulation. 2007;115(11):1481-1501. doi: 10.1161/CIRCULATIONAHA.107.181546 [DOI] [PubMed] [Google Scholar]
- 63.Fleisher LA, Beckman JA, Brown KA, et al. ; American College of Cardiology; American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery); American Society of Echocardiography; American Society of Nuclear Cardiology; Heart Rhythm Society; Society of Cardiovascular Anesthesiologists; Society for Cardiovascular Angiography and Interventions; Society for Vascular Medicine and Biology; Society for Vascular Surgery . ACC/AHA 2007 Guidelines on Perioperative Cardiovascular Evaluation and Care for Noncardiac Surgery [published correction appears in J Am Coll Cardiol. 2008;52(9):793-794]. J Am Coll Cardiol. 2007;50(17):e159-e241. doi: 10.1016/j.jacc.2007.09.003 [DOI] [PubMed] [Google Scholar]
- 64.Zipes DP, Camm AJ, Borggrefe M, et al. ; American College of Cardiology/American Heart Association Task Force; European Society of Cardiology Committee for Practice Guidelines; European Heart Rhythm Association; Heart Rhythm Society . ACC/AHA/ESC 2006 Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death. Circulation. 2006;114(10):e385-e484. doi: 10.1161/CIRCULATIONAHA.106.178233 [DOI] [PubMed] [Google Scholar]
- 65.Smith SC Jr, Feldman TE, Hirshfeld JW Jr, et al. ; American College of Cardiology/American Heart Association Task Force on Practice Guidelines; ACC/AHA/SCAI Writing Committee to Update the 2001 Guidelines for Percutaneous Coronary Intervention . ACC/AHA/SCAI 2005 Guideline Update for Percutaneous Coronary Intervention: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/SCAI Writing Committee to Update the 2001 Guidelines for Percutaneous Coronary Intervention). J Am Coll Cardiol. 2006;47(1):e1-e121. doi: 10.1016/j.jacc.2005.12.001 [DOI] [PubMed] [Google Scholar]
- 66.Fuster V, Rydén LE, Cannom DS, et al. ; European Heart Rhythm Association; Heart Rhythm Society; American College of Cardiology; American Heart Association Task Force on Practice Guidelines; European Society of Cardiology Committee for Practice Guidelines; Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation . ACC/AHA/ESC 2006 Guidelines for the Management of Patients With Atrial Fibrillation—executive summary. J Am Coll Cardiol. 2006;48(4):854-906. doi: 10.1016/j.jacc.2006.07.009 [DOI] [PubMed] [Google Scholar]
- 67.Bonow RO, Carabello BA, Chatterjee K, et al. ; American College of Cardiology; American Heart Association Task Force on Practice Guidelines (Writing Committee to revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease); Society of Cardiovascular Anesthesiologists . ACC/AHA 2006 Guidelines for the Management of Patients With Valvular Heart Disease. J Am Coll Cardiol. 2006;48(3):e1-e148. doi: 10.1016/j.jacc.2006.05.021 [DOI] [PubMed] [Google Scholar]
- 68.Hunt SA; American College of Cardiology; American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure) . ACC/AHA 2005 Guideline Update for the Diagnosis and Management of Chronic Heart Failure in the Adult. J Am Coll Cardiol. 2005;46(6):e1-e82. doi: 10.1016/j.jacc.2005.08.022 [DOI] [PubMed] [Google Scholar]
- 69.Eagle KA, Guyton RA, Davidoff R, et al. ; American College of Cardiology; American Heart Association . ACC/AHA 2004 Guideline Update for Coronary Artery Bypass Graft Surgery. Circulation. 2004;110(14):e340-e437. [PubMed] [Google Scholar]
- 70.Antman EM, Anbe DT, Armstrong PW, et al. . ACC/AHA Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of Patients With Acute Myocardial Infarction). J Am Coll Cardiol. 2004;44(3):E1-E211. doi: 10.1016/j.jacc.2004.07.014 [DOI] [PubMed] [Google Scholar]
- 71.Gregoratos G, Abrams J, Epstein AE, et al. . ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices—summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/NASPE Committee to Update the 1998 Pacemaker Guidelines). J Am Coll Cardiol. 2002;40(9):1703-1719. doi: 10.1016/S0735-1097(02)02528-7 [DOI] [PubMed] [Google Scholar]
- 72.Gibbons RJ, Chatterjee K, Daley J, et al. . ACC/AHA/ACP-ASIM Guidelines for the Management of Patients With Chronic Stable Angina: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Patients With Chronic Stable Angina). J Am Coll Cardiol. 1999;33(7):2092-2197. doi: 10.1016/S0735-1097(99)00150-3 [DOI] [PubMed] [Google Scholar]
- 73.Hirsch AT, Haskal ZJ, Hertzer NR, et al. ; American Association for Vascular Surgery; Society for Vascular Surgery; Society for Cardiovascular Angiography and Interventions; Society for Vascular Medicine and Biology; Society of Interventional Radiology; ACC/AHA Task Force on Practice Guidelines Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease; American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; Vascular Disease Foundation . ACC/AHA 2005 Practice Guidelines for the Management of Patients With Peripheral Arterial Disease (Lower Extremity, Renal, Mesenteric, and Abdominal Aortic). Circulation. 2006;113(11):e463-e654. [DOI] [PubMed] [Google Scholar]
- 74.Stone NJ, Robinson JG, Lichtenstein AH, et al. ; American College of Cardiology/American Heart Association Task Force on Practice Guidelines . 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. J Am Coll Cardiol. 2014;63(25, pt B):2889-2934. doi: 10.1016/j.jacc.2013.11.002 [DOI] [PubMed] [Google Scholar]
- 75.Windecker S, Kolh P, Alfonso F, et al. . 2014 ESC/EACTS Guidelines on Myocardial Revascularization: the Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J. 2014;35(37):2541-2619. doi: 10.1093/eurheartj/ehu278 [DOI] [PubMed] [Google Scholar]
- 76.Mancia G, Fagard R, Narkiewicz K, et al. . 2013 ESH/ESC Guidelines for the Management of Arterial Hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2013;34(28):2159-2219. doi: 10.1093/eurheartj/eht151 [DOI] [PubMed] [Google Scholar]
- 77.Steg PG, James SK, Atar D, et al. ; Task Force on the Management of ST-Segment Elevation Acute Myocardial Infarction of the European Society of Cardiology (ESC) . ESC Guidelines for the Management of Acute Myocardial Infarction in Patients Presenting With ST-Segment Elevation. Eur Heart J. 2012;33(20):2569-2619. doi: 10.1093/eurheartj/ehs215 [DOI] [PubMed] [Google Scholar]
- 78.Perk J, De Backer G, Gohlke H, et al. ; European Association for Cardiovascular Prevention & Rehabilitation (EACPR); ESC Committee for Practice Guidelines (CPG) . European Guidelines on Cardiovascular Disease Prevention in Clinical Practice (version 2012). Eur Heart J. 2012;33(13):1635-1701. doi: 10.1093/eurheartj/ehs092 [DOI] [PubMed] [Google Scholar]
- 79.McMurray JJ, Adamopoulos S, Anker SD, et al. ; ESC Committee for Practice Guidelines . ESC Guidelines for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012. Eur Heart J. 2012;33(14):1787-1847. doi: 10.1093/eurheartj/ehs104 [DOI] [PubMed] [Google Scholar]
- 80.Vahanian A, Alfieri O, Andreotti F, et al. ; Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC); European Association for Cardio-Thoracic Surgery (EACTS) . Guidelines on the management of valvular heart disease (version 2012). Eur Heart J. 2012;33(19):2451-2496. doi: 10.1093/eurheartj/ehs109 [DOI] [PubMed] [Google Scholar]
- 81.Hamm CW, Bassand JP, Agewall S, et al. ; ESC Committee for Practice Guidelines . ESC Guidelines for the Management of Acute Coronary Syndromes in Patients Presenting Without Persistent ST-Segment Elevation. Eur Heart J. 2011;32(23):2999-3054. doi: 10.1093/eurheartj/ehr236 [DOI] [PubMed] [Google Scholar]
- 82.Tendera M, Aboyans V, Bartelink ML, et al. ; European Stroke Organisation; ESC Committee for Practice Guidelines . ESC Guidelines on the Diagnosis and Treatment of Peripheral Artery Diseases: document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteries. Eur Heart J. 2011;32(22):2851-2906. doi: 10.1093/eurheartj/ehr211 [DOI] [PubMed] [Google Scholar]
- 83.Regitz-Zagrosek V, Blomstrom Lundqvist C, Borghi C, et al. ; European Society of Gynecology (ESG); Association for European Paediatric Cardiology (AEPC); German Society for Gender Medicine (DGesGM); ESC Committee for Practice Guidelines . ESC Guidelines on the Management of Cardiovascular Diseases During Pregnancy. Eur Heart J. 2011;32(24):3147-3197. doi: 10.1093/eurheartj/ehr218 [DOI] [PubMed] [Google Scholar]
- 84.Reiner Z, Catapano AL, De Backer G, et al. ; European Association for Cardiovascular Prevention and Rehabilitation; ESC Committee for Practice Guidelines (CPG) 2008-2010 and 2010-2012 Committees . ESC/EAS Guidelines for the Management of Dyslipidaemias. Eur Heart J. 2011;32(14):1769-1818. doi: 10.1093/eurheartj/ehr158 [DOI] [PubMed] [Google Scholar]
- 85.Moya A, Sutton R, Ammirati F, et al. ; Task Force for the Diagnosis and Management of Syncope; European Society of Cardiology (ESC); European Heart Rhythm Association (EHRA); Heart Failure Association (HFA); Heart Rhythm Society (HRS) . Guidelines for the Diagnosis and Management of Syncope (version 2009). Eur Heart J. 2009;30(21):2631-2671. doi: 10.1093/eurheartj/ehp298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Habib G, Hoen B, Tornos P, et al. ; ESC Committee for Practice Guidelines; Endorsed by the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) and the International Society of Chemotherapy (ISC) for Infection and Cancer . Guidelines on the Prevention, Diagnosis, and Treatment of Infective Endocarditis (new version 2009). Eur Heart J. 2009;30(19):2369-2413. doi: 10.1093/eurheartj/ehp285 [DOI] [PubMed] [Google Scholar]
- 87.Galiè N, Hoeper MM, Humbert M, et al. ; ESC Committee for Practice Guidelines (CPG) . Guidelines for the Diagnosis and Treatment of Pulmonary Hypertension. Eur Heart J. 2009;30(20):2493-2537. doi: 10.1093/eurheartj/ehp297 [DOI] [PubMed] [Google Scholar]
- 88.Maisch B, Seferović PM, Ristić AD, et al. ; Task Force on the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology . Guidelines on the Diagnosis and Management of Pericardial Diseases executive summary. Eur Heart J. 2004;25(7):587-610. doi: 10.1016/j.ehj.2004.02.002 [DOI] [PubMed] [Google Scholar]
- 89.Meyer C, Bowers A, Wayant C, et al. . Scientific evidence underlying the American College of Gastroenterology’s clinical practice guidelines. PLoS One. 2018;13(10):e0204720. doi: 10.1371/journal.pone.0204720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Duarte-García A, Zamore R, Wong JB. The evidence basis for the American College of Rheumatology practice guidelines. JAMA Intern Med. 2018;178(1):146-148. doi: 10.1001/jamainternmed.2017.6680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Venkatesh AK, Savage D, Sandefur B, Bernard KR, Rothenberg C, Schuur JD. Systematic review of emergency medicine clinical practice guidelines: implications for research and policy. PLoS One. 2017;12(6):e0178456. doi: 10.1371/journal.pone.0178456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Lee DH, Vielemeyer O. Analysis of overall level of evidence behind Infectious Diseases Society of America practice guidelines. Arch Intern Med. 2011;171(1):18-22. doi: 10.1001/archinternmed.2010.482 [DOI] [PubMed] [Google Scholar]
- 93.Poonacha TK, Go RS. Level of scientific evidence underlying recommendations arising from the National Comprehensive Cancer Network clinical practice guidelines. J Clin Oncol. 2011;29(2):186-191. doi: 10.1200/JCO.2010.31.6414 [DOI] [PubMed] [Google Scholar]
- 94.Wright JD, Pawar N, Gonzalez JS, et al. . Scientific evidence underlying the American College of Obstetricians and Gynecologists’ practice bulletins. Obstet Gynecol. 2011;118(3):505-512. doi: 10.1097/AOG.0b013e3182267f43 [DOI] [PubMed] [Google Scholar]
- 95.Koh C, Zhao X, Samala N, Sakiani S, Liang TJ, Talwalkar JA. AASLD clinical practice guidelines: a critical review of scientific evidence and evolving recommendations. Hepatology. 2013;58(6):2142-2152. doi: 10.1002/hep.26578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Brito JP, Domecq JP, Murad MH, Guyatt GH, Montori VM. The Endocrine Society guidelines: when the confidence cart goes before the evidence horse. J Clin Endocrinol Metab. 2013;98(8):3246-3252. doi: 10.1210/jc.2013-1814 [DOI] [PubMed] [Google Scholar]
- 97.Feuerstein JD, Akbari M, Gifford AE, et al. . Systematic review: the quality of the scientific evidence and conflicts of interest in international inflammatory bowel disease practice guidelines. Aliment Pharmacol Ther. 2013;37(10):937-946. doi: 10.1111/apt.12290 [DOI] [PubMed] [Google Scholar]
- 98.Feuerstein JD, Akbari M, Gifford AE, et al. . Systematic analysis underlying the quality of the scientific evidence and conflicts of interest in interventional medicine subspecialty guidelines. Mayo Clin Proc. 2014;89(1):16-24. doi: 10.1016/j.mayocp.2013.09.013 [DOI] [PubMed] [Google Scholar]
- 99.Alseiari M, Meyer KB, Wong JB. Evidence underlying KDIGO (Kidney Disease: Improving Global Outcomes) guideline recommendations: a systematic review. Am J Kidney Dis. 2016;67(3):417-422. doi: 10.1053/j.ajkd.2015.09.016 [DOI] [PubMed] [Google Scholar]
- 100.Lauer MS, D’Agostino RBS Sr. The randomized registry trial—the next disruptive technology in clinical research? N Engl J Med. 2013;369(17):1579-1581. doi: 10.1056/NEJMp1310102 [DOI] [PubMed] [Google Scholar]
- 101.Harvard Pilgrim Health Care IMplementation of an RCT to imProve Treatment With Oral AntiCoagulanTs in Patients With Atrial Fibrillation (IMPACT-AFib). ClinicalTrials.gov website. https://clinicaltrials.gov/ct2/show/NCT03259373. 2018. Accessed March 9, 2018.
- 102.Povsic TJ, Scott R, Mahaffey KW, et al. . Navigating the future of cardiovascular drug development—leveraging novel approaches to drive innovation and drug discovery: summary of findings from the Novel Cardiovascular Therapeutics Conference. Cardiovasc Drugs Ther. 2017;31(4):445-458. doi: 10.1007/s10557-017-6739-9 [DOI] [PubMed] [Google Scholar]
- 103.Fanaroff AC, Morrow V, Krucoff MW, et al. . A path forward for regenerative medicine. Circ Res. 2018;123(4):495-505. doi: 10.1161/CIRCRESAHA.118.313261 [DOI] [PubMed] [Google Scholar]
- 104.Fanaroff AC, Steffel J, Alexander JH, Lip GYH, Califf RM, Lopes RD. Stroke prevention in atrial fibrillation: re-defining “real-world data” within the broader data universe. Eur Heart J. 2018;39(32):2932-2941. doi: 10.1093/eurheartj/ehy236 [DOI] [PubMed] [Google Scholar]
- 105.Neuman MD, Goldstein JN, Cirullo MA, Schwartz JS. Durability of class I American College of Cardiology/American Heart Association clinical practice guideline recommendations. JAMA. 2014;311(20):2092-2100. doi: 10.1001/jama.2014.4949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Shortell SM, Rundall TG, Hsu J. Improving patient care by linking evidence-based medicine and evidence-based management. JAMA. 2007;298(6):673-676. doi: 10.1001/jama.298.6.673 [DOI] [PubMed] [Google Scholar]
- 107.Sidney S, Quesenberry CP Jr, Jaffe MG, et al. . Recent trends in cardiovascular mortality in the United States and public health goals. JAMA Cardiol. 2016;1(5):594-599. doi: 10.1001/jamacardio.2016.1326 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Levels of Evidence by Guideline and Category of Recommendation (ACC/AHA Guidelines)
eTable 2. Levels of Evidence by Guideline and Category of Recommendation (ESC Guidelines)
eFigure. Proportion of Recommendations Characterized as Level of Evidence A by Year of Guideline Document Release
eReferences