Key Points
Question
Is concussion and/or mild traumatic brain injury (TBI) associated with a higher risk of suicide?
Findings
This systematic review and meta-analysis found a 2-fold higher risk of subsequent suicide among more than 700 000 patients diagnosed with concussion and/or mild TBI, compared with more than 6.2 million individuals who had not been so diagnosed. Experiencing concussion and/or mild TBI was also associated with a higher risk of suicide attempt and suicidal ideation.
Meaning
These results suggest that experiencing concussion and/or mild TBI is associated with an increased risk of suicide.
This systematic review and meta-analysis assesses the risk of suicide after concussion and/or mild traumatic brain injury in a cohort of more than 700 000 individuals diagnosed with these conditions, compared with a cohort of more than 6.2 million individuals who had not been so diagnosed.
Abstract
Importance
Concussion is the most common form of traumatic brain injury (TBI). While most patients fully recover within 1 week of injury, a subset of patients might be at a higher risk of suicide.
Objective
To assess the risk of suicide after concussion.
Data Sources
We performed a systematic search of Medline (PubMed), Embase, PsycINFO, and Published International Literature on Traumatic Stress (PILOTS) from 1963 to May 1, 2017. We also searched Google Scholar and conference proceedings and contacted experts in the field to seek additional studies.
Study Selection
Studies that quantified the risk of suicide, suicide attempt, or suicidal ideation after a concussion and/or mild TBI were included. Studies that included children and adults, including military and nonmilitary personnel, were included. Two authors independently reviewed all titles and abstracts to determine study eligibility.
Data Extraction and Synthesis
Study characteristics were extracted independently by 2 trained investigators. Study quality was assessed using the Newcastle-Ottawa Scale. Study data were pooled using random-effects meta-analysis.
Main Outcomes and Measures
The primary exposure was concussion and/or mild TBI, and the primary outcome was suicide. Secondary outcomes were suicide attempt and suicidal ideation.
Results
Data were extracted from 10 cohort studies (n = 713 706 individuals diagnosed and 6 236 010 individuals not diagnosed with concussion and/or mild TBI), 5 cross-sectional studies (n = 4420 individuals diagnosed and 11 275 individuals not diagnosed with concussion and/or mild TBI), and 2 case-control studies (n = 446 individuals diagnosed and 8267 individuals not diagnosed with concussion and/or mild TBI). Experiencing concussion and/or mild TBI was associated with a 2-fold higher risk of suicide (relative risk, 2.03 [95% CI, 1.47-2.80]; I2 = 96%; P < .001). In 2 studies that provided estimates with a median follow-up of approximately 4 years, 1664 of 333 118 individuals (0.50%) and 750 of 126 114 individuals (0.59%) diagnosed with concussion and/or mild TBI died by suicide. Concussion was also associated with a higher risk of suicide attempt and suicide ideation. The heightened risk of suicide outcomes after concussion was evident in studies with and without military personnel.
Conclusions and Relevance
Experiencing concussion and/or mild TBI was associated with a higher risk of suicide. Future studies are needed to identify and develop strategies to decrease this risk.
Introduction
Concussion is defined as a transient disturbance of neurologic function caused by acute trauma.1 Concussion is the most common form of traumatic brain injury (TBI), with approximately 4 million concussions occurring each year in the United States.1 It is increasingly recognized as an injury affecting military personnel.2,3 For approximately 80% of affected individuals, neurologic symptoms resolve within 7 days of injury.1 However, up to 25% of patients experience chronic neuropsychiatric symptoms, including anxiety and depression, that may last years after the initial injury.4
High-profile cases of professional athletes (eg, Junior Seau, Ken Stabler, and Mike Webster) and military personnel who sustained concussions and subsequently died from suicide have received widespread media attention.5 Although there has been anecdotal evidence reported in newspaper reports, movies, and documentaries suggesting a link between concussion and/or mild TBI and subsequent suicide, past studies on the topic have been limited by small sample sizes and conflicting results.6,7,8
Systematic reviews have demonstrated that severe TBI is associated with a higher risk of suicide.9,10 Severe TBI may involve diffuse axonal injury, intracranial hemorrhage, and/or coma,10 which may cause more severe health consequences than a concussion. Therefore, results of systematic reviews of severe TBI may not apply to concussions.
Evaluating the potential association between concussion and/or mild TBI and suicide is important, because concussion and mild TBI are common, affect individuals of every age, and are often preventable. Furthermore, even if the absolute risk of suicide is low, evidence of an association between concussion and mild TBI and suicide across a range of populations is important because of the seriousness of the outcome. The objective of this systematic review and meta-analysis was to assess the risk of suicide after concussion.
Methods
Protocol and Registration
We conducted a systematic review and meta-analysis, according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.11 Before initiation, we registered our study on Prospero (CRD 42016049388; eMethods in the Supplement).
Information Sources
PubMed (Medline), Embase, Published International Literature on Traumatic Stress (PILOTS), PsycINFO, and Google Scholar were searched from 1963 until May 1, 2017. Conference abstracts, including unpublished studies, from the Annual Academy of Neurology from 2012 to 2017 were also reviewed. (Abstracts prior to 2012 were not readily accessible.) Additional articles were identified by screening reference lists of articles and contacting study investigators.
Search Strategy and Eligibility
Our search strategy, which was created with the help of a librarian with expertise in meta-analysis, is summarized in the eMethods in the Supplement. Keywords included suicide, suicide attempt, suicidal ideation, concussion, and traumatic brain injury. For each database, we used keywords to identify the appropriate controlled vocabulary terms (eg, MeSH headings). We included observational studies that quantified the risk of suicide, suicide attempt, and/or suicidal ideation after a concussion and/or mild TBI, compared with an unexposed comparator. Only studies written in English, French, or Italian were included.
Study Selection
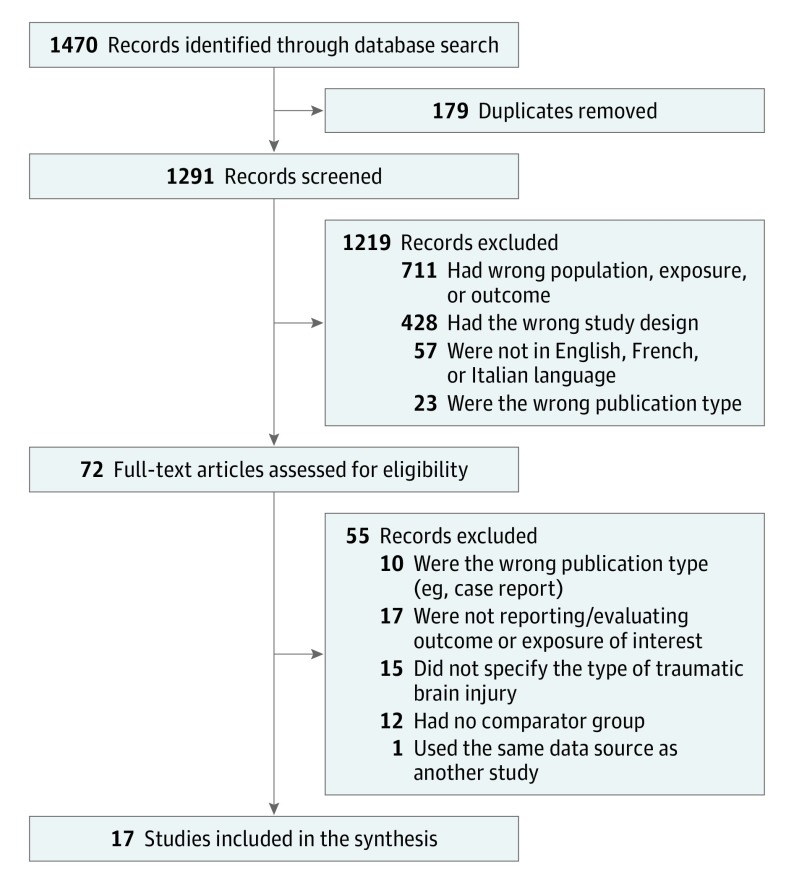
The study selection process is outlined in Figure 1. Two authors (E.S. and A.H.) independently reviewed all titles and abstracts to determine eligibility; the full text of the article was evaluated if the content was not clear from the abstract. Disagreements in study inclusion were resolved through consensus, and when no consensus was reached (<1% of studies) it was resolved by a third author (M.F.).
Figure 1. Flow Diagram of Included Studies.
Data Collection and Quality Assessment
An initial data collection tool was piloted using 5 articles and revised thereafter based on mutual consensus (M.F. and T.K.). The following information was independently extracted from each article by 2 trained investigators (M.F. and T.K.): study authorship, year of publication, study period, country, language, study design (ie, cohort, case-control, or cross-sectional), inclusion and exclusion criteria, population type (ie, military, athletes, students, children, and/or general population), sample size, data source, primary objective, and study conclusion. We also extracted patient demographics, including age, sex, and psychiatric history (ie, depression, anxiety, and substance use disorder). We collected the following concussion-associated information: method of diagnosis (ie, International Classification of Diseases, Eighth, Ninth, or Tenth Revision [ICD-8, ICD-9, or ICD-10] diagnosis, physician diagnosis, concussion scale, survey information, or self-report), the definition used (ie, concussion or mild TBI), and number of concussions or mild TBIs. We collected the following suicide-associated information: ascertainment of outcome (ie, death certificate, database or registry information, family interview, or questionnaire/survey for details on suicide attempt or ideation). We extracted unadjusted and adjusted crude measures of association for suicide, suicide attempt, and suicidal ideation. When neither were reported, we recorded the frequency counts required to calculate unadjusted measures of association. When relevant information was not included in a publication, we contacted the authors of included papers to obtain the data needed to quantify the measures of association.
Quality Assessment
All studies were independently assessed by 2 investigators (M.F. and T.K.) for risk of bias using the Newcastle-Ottawa Scale for cohort and case-control studies.12 A modification of the Newcastle-Ottawa Scale was used for assessment of cross-sectional studies. This scale assesses quality in terms of sample representativeness and size, comparability between respondents and nonrespondents, ascertainment of suicide, and statistical quality. Disagreements in quality assessment were resolved by consensus.
Summary Measures
We extracted count data, unadjusted and adjusted estimates of absolute risk and relative risk, and the respective 95% CIs for suicide, suicide attempt, and suicidal ideation. When both unadjusted and adjusted estimates were provided, adjusted estimates were used. When only count data were provided, we calculated unadjusted measures of association.
All statistical analyses were performed using Stata IC version 14.2 (StataCorp LP) and RevMan Version 5.3 (the Nordic Cochrane Centre, the Cochrane Collaboration). We used random-effects models using the method of DerSimonian and Laird.13 We analyzed suicide, suicide attempt, and suicidal ideation separately.
We calculated pooled estimates presented as relative risks (RRs) with 95% CIs and presented these in forest plots. Different studies calculated different ratio measures of association (eg, rate ratio, odds ratio, incidence ratio). However, since the occurrence of suicide was rare, these estimates should be fairly similar for the different ratio measures. We have referred to these effect estimates using the umbrella term of RRs.
We quantified statistical heterogeneity using the I2 test statistic. An I2 of less than 25% is considered no statistical heterogeneity, 25% to 50% as low statistical heterogeneity, 50% to 75% as medium statistical heterogeneity, and more than 75% as high statistical heterogeneity.14 We evaluated the potential for publication bias with funnel plots for the outcomes and the Egger test.
Sensitivity Analyses
To assess the robustness of our results, we planned to perform an additional analysis stratified by the Newcastle-Ottawa Scale score (lower quality [≤4 points] vs higher quality [>4 points]) and an analysis stratified by population type (military vs nonmilitary personnel). We also performed 2 post hoc analyses of the risk of suicide, restricted to (1) studies that adjusted for potential relevant confounders and (2) cohort studies that reported an odds ratio or hazard ratio.
Results
Study Selection and Characteristics
We identified 1470 abstracts, and 17 studies met our inclusion criteria (Figure 1). These consisted of 10 cohort studies2,3,8,15,16,17,18,19,20,21 (n = 713 706 patients diagnosed and 6 236 010 participants not diagnosed with concussion and/or mild TBI), 5 cross-sectional studies7,22,23,24,25 (n = 4420 patients diagnosed and 11 275 not diagnosed with concussion and/or mild TBI), and 2 case-control studies6,26 (n = 446 patients diagnosed and 8267 not diagnosed with concussion and/or mild TBI; Table 1). Fourteen studies2,3,6,7,8,17,18,19,21,22,23,24,25,26 included patients in North America, 2 studies15,16 were conducted in Scandinavian countries, and 1 study20 was conducted in Australia. Seven studies2,3,6,19,21,25,26 included military personnel, and 3 studies7,17,23 primarily included children or students from the general population.
Table 1. Characteristics of Included Studies.
| Source | Country | Study Period | Design | Study Sample | Participants With Concussion or Mild TBI, No. | Unaffected Participants, No. | Suicides, Suicide Attempts, and/or Suicidal Ideation Among Participants With Concussion or Mild TBI, No. | Suicides, Suicide Attempts, and/or Suicidal Ideation Among Unaffected Participants, No. | Ascertainment Method and Injury Type | Relevant Adjustment Factors | Value (95% CI) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Suicide | |||||||||||
| Teasdale and Engberg,15 2001 | Denmark | 1979-1993 | Retrospective cohort | Patients hospitalized with TBI | 126 114 | NA | 750 | NA | ICD-8 codes, concussion | Age, sex | SMR, 3.02 (2.82-3.25) |
| Brenner et al,2 2011 | US | 2001-2006 | Retrospective cohort | Military VHA | 12 159 | 7 800 846a | 33 | 11 279 | ICD-9 codes, concussion | Age, sex, psychiatric comorbidities, geographic region | HR,1.98 (1.39-2.82) |
| Skopp et al,26 2012 | US | 2001-2009 | Case-control | Military | 420 | 8221 | 97 | NA | ICD-9 codes, mild TBI | Age, sex, race, psychiatric comorbidities, date of service, service type | OR, 1.10 (0.88-1.42) |
| Fazel et al,16 2014 | Sweden | 1969-2009 | Retrospective cohort | General population | 333 118 | 3 331 180 | 1664 | 5962 | ICD codes (unspecified edition), concussion | Age, sex, income, marital status, immigration status | OR, 2.75 (2.08-3.65)b |
| Richard et al,17 2015 | Canada | 1987-2008 | Retrospective cohort | Children | 5314 | 113 582 | 31 | 390 | ICD-9 codes, mild TBI | Age, sex, psychiatric disease, socioeconomic status, musculoskeletal disease | HR, 2.18 (1.63-2.91) |
| Fralick et al,18 2016 | Canada | 1992-2012 | Retrospective cohort | General population | 235 110 | 2 397 192 | 667 | 3934 | ICD-9 and ICD-10 codes, concussion | None | OR, 1.73 (1.59-1.88) |
| Suicide attempt | |||||||||||
| Oquendo et al,8 2004 | US | Unknown | Retrospective cohort | Patients admitted to research unit with depression | 143 | 182 | 86 | 86 | Survey, mild TBI | None | OR, 1.68 (1.08-2.62)c |
| Barnes et al,6 2012 | US | 2006-2010 | Case-control | Military personnel in VHA PTSD Clinic | 44 | NR | 2 | 3 | Physician, mild TBI | Ethnicity, age | OR, 0.65 (0.10-4.10) |
| Mackelprang et al,22 2014 | US | 2006-2009 | Cross-sectional | Homeless individuals | 1145 | 1549 | 383 | 209 | Survey, mild TBI | Age, sex, race, education level | PR, 1.22 (1.01-1.47) |
| Ilie et al,7 2014 | Canada | 2011 | Cross-sectional | Students, grades 7-12 | 882 | 3803 | 52 | 76 | Survey, mild TBI | Grade of school, sex, survey design | OR, 3.39 (2.15-5.35) |
| Schneider et al,19 2016 | US | 2006-2010 | Retrospective cohort | Military veterans at mental health intake visit | 468 | 629 | 7 | 0 | Survey, likely mild TBI | None | OR, 19.1 (1.08-337) |
| Ilie et al,23 2016 | Canada | 2012-2013 | Cross-sectional | Students, grades 9-12 | 658 | 2472 | NR | NR | Survey, TBI | Age, sex, psychiatric comorbidities | OR, 5.21 (2.94-9.23)b |
| Bryant et al,20 2016 | Australia | 2004-2006 | Prospective cohort | Patients admitted to trauma center | 301 | 421 | NR | NR | Physician, mild TBI | Not applicable for suicide attempt | Unable to calculate |
| Topolovec-Vranic et al,24 2017 | Canada | 2009-2011 | Cross-sectional | Homeless individuals | 1370 | 718 | NR | NR | Survey, TBI | None | OR, 2.02 (1.69-2.42) |
| Suicidal ideation | |||||||||||
| Barnes et al,6 2012 | US | 2006-2010 | Case-control | Military personnel at a VHA PTSD Clinic | 44 | 44 | 11 | 5 | Physician, mild TBI | Ethnicity, age | OR, 2.60 (0.82-8.25) |
| Bryan et al,3 2013 | US | 2009 | Retrospective cohort | Military personnel referred to TBI clinic | 143 | 18 | 4d | 0 | Physician, TBI | Neuropsychiatric symptomatology | OR, 1.24 (1.02-1.50) |
| Mackelprang et al,22 2014 | US | 2006-2009 | Cross-sectional | Homeless youth | 1145 | 1549 | 554 | 347 | Survey, mild TBI | Age, sex, race, education level | PR, 1.83 (1.62-2.06) |
| Ilie et al,7 2014 | Canada | 2011 | Cross-sectional | Students, grades 7-12 | 882 | 3803 | 134 | 350 | Survey, mild TBI | Grade of school, sex, survey design | OR, 1.93 (1.42-2.63) |
| Vanderploeg et al,25 2015 | US | 2009-2010 | Cross-sectional | Military personnel | 365 | 2733 | NR | NR | Survey, mild TBI | Sex, race, education, marital status, psychiatric disease, combat factors | OR, 2.03 (1.12-3.69)e |
| Stein et al,21 2015 | US | 2012 | Prospective cohort | Military personnel | 836 | 3753 | NR | NR | Survey, mild TBI | Age, sex, race, prior deployment, combat status, stressors, psychiatric disease, ethnicity, prior TBI | OR (3 mo), 1.39 (0.97-2.01); OR (9 mo), 1.12 (0.86-1.46) |
| Ilie et al,23 2016 | Canada | 2012-2013 | Cross-sectional | Students, grades 9-12 | 658 | 2472 | NR | NR | Survey, TBI | Age, sex, psychiatric comorbidities | OR: 1.71 (1.20-2.44)f |
| Bryant et al,20 2016 | Australia | 2004-2006 | Prospective cohort | General population, trauma center | 301 | 421 | NR | NR | Physician, mild TBI | Age, sex, type and severity of injury, pain and other stressors, psychiatric disease | OR (3 mo), 2.59 (1.41-4.75); OR (12 mo), 1.50 (0.84-2.67) |
Abbreviations: HR, hazard ratio; ICD, International Classification of Diseases, Eighth Revision (ICD-8), Ninth Revision (ICD-9), and Tenth Revision (ICD-10); NA, not available; NR, not reported; OR, odds ratio; PR, prevalence ratio; PTSD, posttraumatic stress disorder; RR, risk ratio; SMR, standardized mortality ratio; TBI, traumatic brain injury; VHA, Veterans Health Administration.
A random sample of 389 053 were used for the analysis.
Pooled male and female estimate using a random-effects model.
Analysis noted to be underpowered.
For people with a single mild TBI.
Pooled deployed risk estimate and nondeployed risk estimate using a random-effects model.
Pooled former and recent TBI using random-effects model.
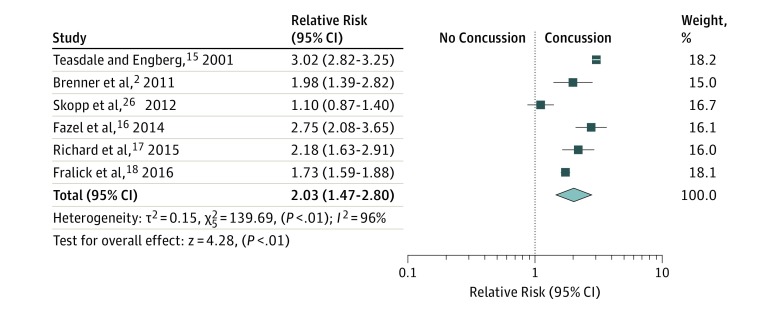
Six studies2,15,16,17,18,26 included suicide as an outcome (Figure 2), and all identified concussion and/or mild TBI using validated ICD-8 or ICD-9 or ICD-10 codes and suicide using death certificate data. For these studies, the reported mean and/or median age of participants ranged from 8 years to 58 years, and the reported mean and/or median percentage of male patients ranged from 52% to 96% (eTable 1 in the Supplement). Eight studies included suicide attempt6,7,8,19,20,22,23,24 as an outcome, most (6 [75%]) of which identified concussion and/or mild TBI using a questionnaire and suicide attempt via a questionnaire or interview. Eight studies included suicidal ideation3,6,7,20,21,22,23,25 as an outcome, most (5 [63%]) of which identified concussion and/or mild TBI and suicidal ideation using a questionnaire or interview.
Figure 2. Meta-analysis of Risk of Suicide After Concussion and/or Mild Traumatic Brain Injury.
Weighed using random effects (inverse variance weighting). The 95% CIs for Skopp et al26 differ slightly from the point estimate in their study (odds ratio, 1.10 [95% CI, 0.88-1.42]), because the study provided the odds ratio to 1 decimal point.
We evaluated each study using the Newcastle-Ottawa Scale quality assessment criteria (eTable 1 in the Supplement). Of 9 possible points, the median score for cohort studies was 6 (range, 2-7), and the median score for case-control studies was 6 (range, 5-7). Of 8 possible points, the median score for cross-sectional studies was 6 (range, 4-8).
Risk of Bias
All 6 studies2,15,16,17,18,26 of suicide used ICD-8, ICD-9, or ICD-10 codes to identify concussions and/or mild TBIs, a method that has a demonstrated specificity of 99%.18,27 These studies all used death certificates to identify suicides, and this method has been validated previously to correctly classify suicide deaths.16,18,28
Studies assessing the risk of suicide attempt6,7,8,19,20,22,23,24 mainly used self-reported data to identify both concussion and/or mild TBI and suicide-associated outcomes. About half of the studies were cross-sectional, which made it challenging to identify associations between the exposure and outcome. We did not meta-analyze results for studies that assessed the risk of suicide attempt6,7,8,19,20,22,23,24 or suicidal ideation3,6,7,20,21,22,23,25 after concussion and/or mild TBI because of concerns about heterogeneity in defining and evaluating both the exposure (ie, concussion and/or mild TBI) and the outcome and the large number of cross-sectional studies.
Risk of Suicide After Concussion and/or Mild TBI
The risk of suicide was 2-fold higher for people diagnosed with at least 1 concussion and/or mild TBI compared with those not diagnosed with a concussion and/or mild TBI (RR = 2.03 [95% CI, 1.47-2.80]; I2 = 96%; P < .001). Despite the high I2, meta-analysis was pursued, because 5 of the 6 included studies were of a similar design (ie, cohort studies), used the same validated method of identifying both concussion and/or mild TBI (ICD-8, ICD-9, or ICD-10) and suicide (death certificate), and were of relatively high quality (median Newcastle-Ottawa Scale score, 6). In addition, the association was slightly stronger when the meta-analysis was restricted to studies that adjusted for factors associated with concussion and/or mild TBI and suicide (RR = 2.10 [95% CI, 1.40-3.13]; I2 = 94%; P < .01).
The absolute risk of suicide for patients diagnosed with concussion and/or mild TBI over time was available, or calculable, for 4 of the 5 cohort studies (eTable 1 in the Supplement). Two studies15,16 provided estimates after a median follow-up time of approximately 3.6 years15 and 4 years,16 respectively, and 1664 of 333 118 participants (0.50%)16 and 750 of 126 114 participants (0.59%)15 of patients who had a concussion and/or mild TBI subsequently died by suicide (eTable 2 in the Supplement). A study with a longer median follow-up time (9.3 years) reported 667 of 235 110 participants (0.28%)18 of participants died by suicide, while another with a 12.3-year median follow-up time reported that 26 of 5314 participants (0.49%)17 died by suicide.
Risk of Suicide Attempt or Suicidal Ideation After Concussion and/or Mild TBI
Most studies reported a heightened risk of suicide attempt after concussion and/or mild TBI (Table). Five studies (63%) provided risk estimates that adjusted for relevant baseline confounders. All 8 studies that assessed risk of suicidal ideation reported a heightened risk following diagnosis of concussion and/or mild TBI (Table), with all 6 studies reporting estimates adjusted for relevant confounders.
Sensitivity Analyses
In separate analyses stratified for military vs nonmilitary personnel, the combined estimate for studies of nonmilitary populations (RR, 2.36 [95% CI, 1.64-3.40]; I2 = 97%, P < .01) was higher than the combined estimate for studies of military populations (RR, 1.46 [95% CI, 0.80-2.58]; I2 = 86%, P < .01).2,26 We also performed a post hoc analysis excluding the results from Skopp et al26 (because it was a case-control study) and the study by Teasdale and Engberg15 (because it reported standardized mortality ratios). Doing so decreased the statistical heterogeneity for the risk of suicide (RR = 2.09 [95% CI, 1.66-2.64]; I2 = 74%; P = .01). When evaluated by the Newcastle-Ottawa Scale, the magnitude of heightened risk of suicide attempt or ideation associated with concussions and/or mild TBIs was weaker in lower-quality studies (score ≤4) than the associations reported studies with scores greater than 4. All of the studies reporting risk of suicide had a Newcastle-Ottawa Scale score greater than 4.
Assessment of Publication Bias
Visual inspection of the funnel plot showed minimal asymmetry (eFigure in the Supplement), and there was no evidence of small studies effect (per the Egger test). There were not enough studies for each outcome type to conduct these tests separately for suicide, suicidal ideation, and suicide attempts.
Discussion
In this systematic review and meta-analysis that included more than 700 000 individuals diagnosed with concussion and/or mild TBI and 6.2 million unaffected individuals, we observed a higher risk of suicide for people diagnosed with concussion and/or mild TBI compared with those without such diagnoses. Despite this heightened risk, nearly all patients diagnosed with concussion and/or mild TBI did not die by suicide.
There are several possible mechanisms that may explain the association between concussion and/or mild TBI and suicide. Recent meta-analyses of neuroimaging studies of patients with mild TBI reported abnormal activity on functional magnetic resonance imaging29 and abnormal structural connectivity30 in brain regions critical for cognitive and emotional processing. Changes in functional neuroimaging have been associated with neuropsychological deficits and clinical depression in athletes with a history of concussion and/or mild TBI.31 In addition, multiple neuropathological models have been proposed for how neurobehavioral impairment may occur in the short term and long term after concussion and/or mild TBI.32 Most notably, chronic traumatic encephalopathy, a progressive neurodegenerative disease characterized by accumulation of phosphorylated tau around blood vessels and at the depths of the sulci, has been associated with prior participation in football and concussion and/or mild TBI.33 That study also reported a pattern of accumulation involving the prefrontal cortex, amygdala, and other brain regions that have been associated with depression, anxiety, impulsivity, and other relevant symptoms.33 However, many cases of chronic traumatic encephalopathy have been reported in athletes without a history of concussion or mild TBI.34 The lack of a prior documented concussion and/or mild TBI might be because of underreporting of these conditions, but this also raises the possibility that subconcussive events could be sufficient to cause chronic traumatic encephalopathy.34,35
Two prior systematic reviews on the association between TBI and suicidality9,10 primarily included patients with severe TBI and were limited by a small number of studies that prevented meta-analysis. Our study focused on concussion and mild TBI and included 3 large studies published since these systematic reviews.16,17,18 Of the studies we identified reporting risk of suicide, there was a high level of statistical heterogeneity.
Despite statistical heterogeneity across the included studies, they were similar in terms of study design (ie, 5 of 6 were cohort studies) and all used the same methods for identifying concussion and/or mild TBI (ICD-8 or ICD-9 or ICD-10) and cause of death (death certificate). Some of the heterogeneity was likely associated with study design and the type of effect estimates reported, because heterogeneity (I2) fell when we excluded the case-control study as well as the study that reported standardized mortality ratios. The heterogeneity may also be associated with differences in injury severity across the included studies. For example, a study by Teasdale and Engberg15 identified patients hospitalized with concussions and/or mild TBIs and reported the highest association with suicide, whereas the study by Fralick et al18 only included patients who were not hospitalized for concussion. Furthermore, 2 of the studies2,26 included military personnel who sustained injuries during combat. Interestingly, the relative risk of suicide after concussion and/or mild TBI appeared to be lower in the studies of military personnel. It is unknown whether this is associated with differences in reporting of concussions and/or mild TBIs or severity of injury, because the studies of military personnel also included fewer participants than the other studies did.
For studies of suicide attempt and ideation, there was heterogeneity in study design, ascertainment of injury, and ascertainment of suicide attempt and ideation, and for these reasons, we did not meta-analyze results of these studies. However, most of these studies reported a heightened risk of suicide attempt or suicidal ideation for people diagnosed with mild TBI compared with those not diagnosed. These findings are consistent with prior systematic reviews for patients with TBI.9
Limitations
There are some limitations of our study. Most included studies only provided relative risks in terms of rate ratios or odds ratios. Therefore, we could not conduct a meta-analysis to quantify the absolute number of excess cases of suicide attributable to concussions and/or mild TBIs. For the studies that did provide absolute risks, the length of follow-up for the different studies varied considerably. A priori, we hypothesized that any heightened suicide risk associated with concussions and/or mild TBIs would increase incrementally with the number of injury incidents, but most studies reported exposure as any history of injury (yes/no). Therefore, we could not quantify the risk of suicide on a per-injury basis. In addition, few studies included the risk of suicide among athletes and children, populations that may be at greatest risk of concussion and adverse sequelae.
Another limitation of this systematic review and meta-analysis was that most of the available studies were retrospective, and most lacked an active comparator (eg, people with a nonneurologic injury). Both can affect confounding control and limit causal inference. Since suicide attempt may affect the reporting of concussion history, there is also a concern that recall bias could overestimate the association. While more prospective studies would be ideal, this would be an inefficient way to assess the risk of suicide after concussion, since suicide after concussion is quite rare. Until large prospective studies with sufficiently large durations of follow-up are available, we have to rely on the currently available data.
Our results suggest that compared with people with no history of concussion and/or mild TBI, there is evidence of a heightened risk of suicide, suicide attempt, and suicidal ideation among individuals diagnosed with these conditions. Whether there are certain characteristics that make some people more susceptible to these risks after concussion and/or mild TBI remains unknown. Because suicides are rare and may occur many years after a concussion, it is challenging to design studies that address the current gaps in knowledge, such as quantifying the typical time between concussion and/or mild TBI and suicide risk and identifying characteristics of patients who experience the greatest risk for suicide. There is currently an ongoing prospective registry in the United States that will include college athletes that sustain a concussion or mild TBI, but results from this registry are at least a decade away.36 In the meantime, future studies are required to develop strategies to prevent concussions and/or mild TBI and to identify patients at highest risk of suicide after incurring such injuries.37
eMethods. Systematic Review Search strategy, Analysis – further details, and PROSPERO Details
eFigure. Funnel plot assessment for risk of publication bias using effect estimates from all included studies.
eTable 1. Results of the critical appraisal using the Newcastle-Ottawa Scale
eTable 2. Additional characteristics of included studies
eReferences.
References
- 1.Harmon KG, Drezner JA, Gammons M, et al. . American Medical Society for Sports Medicine position statement: concussion in sport. Br J Sports Med. 2013;47(1):15-26. doi: 10.1136/bjsports-2012-091941 [DOI] [PubMed] [Google Scholar]
- 2.Brenner LA, Ignacio RV, Blow FC. Suicide and traumatic brain injury among individuals seeking Veterans Health Administration services. J Head Trauma Rehabil. 2011;26(4):257-264. doi: 10.1097/HTR.0b013e31821fdb6e [DOI] [PubMed] [Google Scholar]
- 3.Bryan CJ, Clemans TA. Repetitive traumatic brain injury, psychological symptoms, and suicide risk in a clinical sample of deployed military personnel. JAMA Psychiatry. 2013;70(7):686-691. doi: 10.1001/jamapsychiatry.2013.1093 [DOI] [PubMed] [Google Scholar]
- 4.Fann JR, Hart T, Schomer KG. Treatment for depression after traumatic brain injury: a systematic review. J Neurotrauma. 2009;26(12):2383-2402. doi: 10.1089/neu.2009.1091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Webner D, Iverson GL. Suicide in professional American football players in the past 95 years. Brain Inj. 2016;30(13-14):1718-1721. doi: 10.1080/02699052.2016.1202451 [DOI] [PubMed] [Google Scholar]
- 6.Barnes SM, Walter KH, Chard KM. Does a history of mild traumatic brain injury increase suicide risk in veterans with PTSD? Rehabil Psychol. 2012;57(1):18-26. doi: 10.1037/a0027007 [DOI] [PubMed] [Google Scholar]
- 7.Ilie G, Mann RE, Boak A, et al. . Suicidality, bullying and other conduct and mental health correlates of traumatic brain injury in adolescents. PLoS One. 2014;9(4):e94936. doi: 10.1371/journal.pone.0094936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Oquendo MA, Friedman JH, Grunebaum MF, Burke A, Silver JM, Mann JJ. Suicidal behavior and mild traumatic brain injury in major depression. J Nerv Ment Dis. 2004;192(6):430-434. doi: 10.1097/01.nmd.0000126706.53615.7b [DOI] [PubMed] [Google Scholar]
- 9.Bahraini NH, Simpson GK, Brenner LA, Hoffberg AS, Schneider AL. Suicidal ideation and behaviours after traumatic brain injury: a systematic review. Brain Impair. 2013;14:92-112. doi: 10.1017/BrImp.2013.11 [DOI] [Google Scholar]
- 10.Simpson G, Tate R. Suicidality in people surviving a traumatic brain injury: prevalence, risk factors and implications for clinical management. Brain Inj. 2007;21(13-14):1335-1351. doi: 10.1080/02699050701785542 [DOI] [PubMed] [Google Scholar]
- 11.Moher D, Shamseer L, Clarke M, et al. ; PRISMA-P Group . Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1-9. doi: 10.1186/2046-4053-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wells G, Shea B, O’Connor D The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analysis. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Published 2012. Accessed December 19, 2016.
- 13.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177-188. doi: 10.1016/0197-2456(86)90046-2 [DOI] [PubMed] [Google Scholar]
- 14.Higgins JP, Altman DG, Gøtzsche PC, et al. ; Cochrane Bias Methods Group; Cochrane Statistical Methods Group . The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928-d5928. doi: 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Teasdale TW, Engberg AW. Suicide after traumatic brain injury: a population study. J Neurol Neurosurg Psychiatry. 2001;71(4):436-440. doi: 10.1136/jnnp.71.4.436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fazel S, Wolf A, Pillas D, Lichtenstein P, Långström N. Suicide, fatal injuries, and other causes of premature mortality in patients with traumatic brain injury: a 41-year Swedish population study. JAMA Psychiatry. 2014;71(3):326-333. doi: 10.1001/jamapsychiatry.2013.3935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Richard YF, Swaine BR, Sylvestre MP, Lesage A, Zhang X, Feldman DE. The association between traumatic brain injury and suicide: are kids at risk? Am J Epidemiol. 2015;182(2):177-184. doi: 10.1093/aje/kwv014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fralick M, Thiruchelvam D, Tien HC, Redelmeier DA. Risk of suicide after a concussion. CMAJ. 2016;188(7):497-504. doi: 10.1503/cmaj.150790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schneider AL, Hostetter TA, Homaifar BY, et al. . Responses to traumatic brain injury screening questions and suicide attempts among those seeking Veterans Health Administration mental health services. Front Psychiatry. 2016;7:59. doi: 10.3389/fpsyt.2016.00059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bryant RA, O’Donnell ML, Forbes D, McFarlane AC, Silove D, Creamer M. The course of suicide risk following traumatic injury. J Clin Psychiatry. 2016;77(5):648-653. doi: 10.4088/JCP.14m09661 [DOI] [PubMed] [Google Scholar]
- 21.Stein MB, Kessler RC, Heeringa SG, et al. ; Army STARRS collaborators . Prospective longitudinal evaluation of the effect of deployment-acquired traumatic brain injury on posttraumatic stress and related disorders: results from the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS). Am J Psychiatry. 2015;172(11):1101-1111. doi: 10.1176/appi.ajp.2015.14121572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mackelprang JL, Harpin SB, Grubenhoff JA, Rivara FP. Adverse outcomes among homeless adolescents and young adults who report a history of traumatic brain injury. Am J Public Health. 2014;104(10):1986-1992. doi: 10.2105/AJPH.2014.302087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ilie G, Mann RE, Boak A, et al. . Cross-sectional examination of the association of co-occurring alcohol misuse and traumatic brain injury on mental health and conduct problems in adolescents in Ontario, Canada. BMJ Open. 2016;6(11):e011824. doi: 10.1136/bmjopen-2016-011824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Topolovec-Vranic J, Schuler A, Gozdzik A, et al. . The high burden of traumatic brain injury and comorbidities amongst homeless adults with mental illness. J Psychiatr Res. 2017;87:53-60. doi: 10.1016/j.jpsychires.2016.12.004 [DOI] [PubMed] [Google Scholar]
- 25.Vanderploeg RD, Nazem S, Brenner LA, et al. . Suicidal ideation among Florida National Guard members: combat deployment and non-deployment risk and protective factors. Arch Suicide Res. 2015;19(4):453-471. doi: 10.1080/13811118.2014.957454 [DOI] [PubMed] [Google Scholar]
- 26.Skopp NA, Trofimovich L, Grimes J, Oetjen-Gerdes L, Gahm GA. Relations between suicide and traumatic brain injury, psychiatric diagnoses, and relationship problems, active component, U.S. Armed Forces, 2001-2009. MSMR. 2012;19(2):7-11. [PubMed] [Google Scholar]
- 27.Bazarian JJ, Veazie P, Mookerjee S, Lerner EB. Accuracy of mild traumatic brain injury case ascertainment using ICD-9 codes. Acad Emerg Med. 2006;13(1):31-38. doi: 10.1197/j.aem.2005.07.038 [DOI] [PubMed] [Google Scholar]
- 28.Fralick M, Macdonald EM, Gomes T, et al. ; Canadian Drug Safety and Effectiveness Research Network . Co-trimoxazole and sudden death in patients receiving inhibitors of renin-angiotensin system: population based study. BMJ. 2014;349:g6196. doi: 10.1136/bmj.g6196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Eierud C, Craddock RC, Fletcher S, et al. . Neuroimaging after mild traumatic brain injury: review and meta-analysis. Neuroimage Clin. 2014;4:283-294. doi: 10.1016/j.nicl.2013.12.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Aoki Y, Inokuchi R. A voxel-based meta-analysis of diffusion tensor imaging in mild traumatic brain injury. Neurosci Biobehav Rev. 2016;66:119-126. doi: 10.1016/j.neubiorev.2016.04.021 [DOI] [PubMed] [Google Scholar]
- 31.Hart J Jr, Kraut MA, Womack KB, et al. . Neuroimaging of cognitive dysfunction and depression in aging retired National Football League players: a cross-sectional study. JAMA Neurol. 2013;70(3):326-335. doi: 10.1001/2013.jamaneurol.340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.DeKosky ST, Blennow K, Ikonomovic MD, Gandy S. Acute and chronic traumatic encephalopathies: pathogenesis and biomarkers. Nat Rev Neurol. 2013;9(4):192-200. doi: 10.1038/nrneurol.2013.36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mez J, Daneshvar DH, Kiernan PT, et al. . Clinicopathological evaluation of chronic traumatic encephalopathy in players of American football. JAMA. 2017;318(4):360-370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stein TD, Alvarez VE, McKee AC. Concussion in chronic traumatic encephalopathy. Curr Pain Headache Rep. 2015;19(10):47. doi: 10.1007/s11916-015-0522-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ban VS, Madden CJ, Bailes JE, Hunt Batjer H, Lonser RR. The science and questions surrounding chronic traumatic encephalopathy. Neurosurg Focus. 2016;40(4):E15. doi: 10.3171/2016.2.FOCUS15609 [DOI] [PubMed] [Google Scholar]
- 36.National Collegiate Athletics Association Concussion. http://www.ncaa.org/sport-science-institute/concussion. Published August 2014. Accessed December 19, 2016.
- 37.Burke MJ, Fralick M, Nejatbakhsh N, Tartaglia MC, Tator CH. In search of evidence-based treatment for concussion: characteristics of current clinical trials. Brain Inj. 2015;29(3):300-305. doi: 10.3109/02699052.2014.974673 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods. Systematic Review Search strategy, Analysis – further details, and PROSPERO Details
eFigure. Funnel plot assessment for risk of publication bias using effect estimates from all included studies.
eTable 1. Results of the critical appraisal using the Newcastle-Ottawa Scale
eTable 2. Additional characteristics of included studies
eReferences.