Abstract
Background:
Antihistamines are one of the commonly prescribed groups of drugs for allergic disorders and pruritus. They are broadly grouped into two generations, the second-generation ones being more effective and with less side effects. The family physicians frequently use antihistamines as patients contact them initially for their problem. It will be interesting to know the mode of selection of antihistamines by them.
Materials and Methods:
The study was carried out on a sample of 100 family physicians. Primary data were collected from them after taking informed consent. A pre-validated questionnaire regarding knowledge, awareness, and prescribing schedule of antihistamines was filled up. The data were then analyzed with suitable statistical tests.
Results:
Almost 73% of physicians prescribed second-generation antihistamines, while 27% prescribed the first-generation ones. Only 15% of them were aware about the ARIA and GA2LEN guidelines and their recommendations for prescribing second-generation antihistamines over the older first-generation antihistamines, while 85% had not heard about them previously. A minimum 7% of practitioners revealed that they updosed the same drug four times in the treatment of urticaria, while 93% did not do it.
Conclusion:
Even though a sizeable percentage of family physicians prescribed second-generation antihistamines, most of them were not aware of their dosing guidelines.
KEY WORDS: Antihistamines, guidelines, urticaria
Introduction
Antihistamines are a class of drugs used by physicians in general, and dermatologists in particular. They are the mainstay of treatment for urticaria and other allergic disorders such as angioedema, anaphylaxis, mastocytosis, allergic rhinitis, conjunctivitis, asthma, and pruritus associated with numerous dermatological disorders. The class includes a huge list of drugs which are grouped by their receptor affinity into H1, H2, H3, and H4 (not commercially available) antihistamines. Of relevance to the management of pruritus and allergy are the H1 antihistamines. They are broadly grouped into first- and second-generation antihistamines. They differ mainly in their ability to cause central nervous system (CNS) effects.[1] The first-generation (classic) antihistamines include hydroxyzine, promethazine, chlorpheniramine, and diphenhydramine.[2] The second-generation ones include cetirizine, levocetirizine, loratadine, desloratadine, and fexofenadine.[2]
Nowadays, the second-generation ones are recommended over the first-generation drugs due to their lesser side effect (lesser sedation and cholinergic) profile.[3] As per the latest EAACI/GA2LEN/EDF/WAO guidelines for the management of urticaria, the drugs of the first choice should be of a second generation, nonsedating H1-antihistamines. As per these guidelines, “In patients with urticaria and no special indication, we recommend against the routine use of old-sedating first-generation antihistamines (strong recommendation and high-quality evidence).”[4]
However, a large number of clinicians and family physicians are not aware of the classification of these drugs, their side effect profile, their dosage, use in different age groups, and the guidelines related to their usage (especially in urticaria). This often results in the wrong administration of these drugs and thus leads to unnecessary side effects.
Family physicians are involved in treating a large proportion of patients on a daily basis. Accordingly, antihistamines form an important class of drugs, prescribed by them. Due to this, we made an attempt to assess the knowledge of family physicians towards the usage of antihistamines. This may help to estimate the level of awareness of our family physicians towards the usage of these drugs and accordingly enable us to make efforts to improve the same.
Materials and Methods
This study was a descriptive study carried out by the Department of Dermatology, Dr. D Y Patil Hospital, Navi Mumbai, a tertiary care teaching hospital. It was conducted over a period of 3 months (between March 2017 and May 2017). A total of 100 family physicians (who gave their informed consent) from Navi Mumbai were selected randomly (using a table of random numbers). A relevant pre-validated questionnaire was then filled up which included a total of 10 questions. Every question was first validated by the Chi-square test. The significance of each was below 10%, hence proving validity of these questions. The objective of the study was first explained to them so that they could correctly fill them.
The questions were related to the choice of the antihistamine drugs prescribed (whether first or second generation), knowledge about their common side effects and clinical guidelines, choice and usage of these drugs in various age groups, and finally information about their dosage and availability. Eight out of 10 questions had a dichotomous scale, while the remaining two had multiple-choice answers.
The data obtained were then compiled and analyzed using Statistical Package for the Social Sciences, SPSS version 20 (SPSS Inc., Chicago, IL, USA).
Results
A total of 100 family physicians were enrolled in our screening study. These were selected from a huge number of family physicians of Navi Mumbai, by a process of random sampling (using a table of random numbers). In response to the first question related to their choice while prescribing various antihistamines, it was found that 62% prescribed levocetirizine as their first choice. Hydroxyzine, fexofenadine, and diphenhydramine were prescribed by 21%, 15%, and 2% practitioners, respectively [Figure 1].
Figure 1.
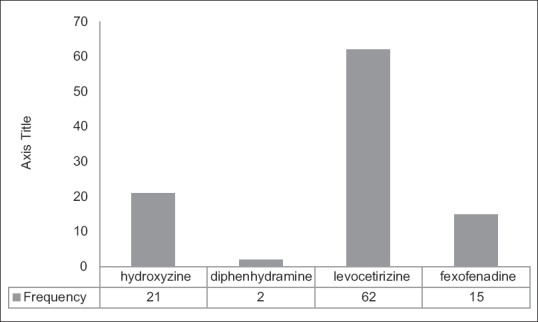
Frequency of common antihistamines prescribed
Out of these 100 physicians, 73% said that they prescribed second-generation antihistamines, while 27% did not prescribe them and still prescribed the first-generation ones only.
In addition, it was found that 71% of physicians were aware that the first-generation antihistamines caused significant impairment of daily activities of patients, while only 29% were not aware of these side effects. Furthermore, 65% of physicians (while prescribing antihistamines) advised their patients to avoid driving and consumption of alcohol, and rest 35% did not give any such instructions to their patients.
About 69% of physicians prescribed different antihistamines to their patients based on their age, occupation, and pregnancy status, while 31% did not take all these factors into consideration.
Almost 91% of physicians reported that their patients complained of problem in staying awake and felt disoriented after taking antihistamines.
However, knowledge about the criteria for prescribing antihistamines was very less as only 15% were aware of the ARIA and GA2LEN guidelines and their recommendations for prescribing second-generation antihistamines over the older first-generation antihistamines, while 85% had not heard about them previously.
When questioned about their reasons for not prescribing second-generation antihistamines routinely, 46% cited high cost as the reason, while another 46% believed that this class of antihistamines was not as effective as the first-generation ones and finally 8% believed that they were not available in most pharmacies and, hence, did not prescribe them.
About 15% practitioners also revealed that their patients asked for a first-generation antihistamine that they were familiar with, rather than the one the physician was prescribing, while 85% was not guided by patient's choice.
On questioning about the dosing of antihistamines, only 7% practitioners revealed that they updosed the same drug four times in the treatment of urticaria, while 93% did not resort to this measure.
Discussion
H1-antihistamines (developed from anticholinergic drugs) act as inverse agonists rather than antagonists of histamine H1 receptors.[5] In addition to their antiallergic action, they have additional tranquilizer, anticonvulsant, decongestant, hypnotic, and antiparkinsonian properties.[6] Based on their pharmacology and other properties, these are grouped into first-generation and second-generation drugs. The two groups differ markedly in their chemical properties and subsequent clinical uses and side effect profiles. The first-generation ones being lipophilic, cross the blood-brain barrier easily, and interfere with neurotransmission by histamine at CNS H1 receptors. Consequently, this group has higher CNS side effects such as drowsiness, sedation, somnolence, fatigue, and headache. In addition, they also impair cognitive function, memory, and psychomotor performance.[7,8,9] The cardiovascular side effects include reflex tachycardia, supraventricular and ventricular arrhythmias, and dose-related prolongation of the QTc interval. Additional side effects include mydriasis, dry eyes, dry mouth, urinary retention, decreased gastrointestinal motility, constipation, peripheral vasodilation, and postural hypotension.[9] Due to these side effects, these drugs should not be routinely prescribed for the management of urticaria and related allergic disorders. The second-generation antihistamines have a much lower side effect profile.
In our study, we found that levocetirizine was the most common antihistamine prescribed by 62% physicians. Among the two groups, the second-generation group was prescribed by 73%, while the first-generation group was prescribed by 27% physicians. This points towards the fact that despite a sizeable proportion of physicians prescribing the second-generation drugs, a significant number still prescribed the first-generation ones, indicating the need for greater awareness in them, which would result in a reduction in the prescription of the first generation antihistamines.
Similarly, 71% of these physicians were aware of the side effects of the first-generation group, while the rest (29%) did not know about them. This again points towards the fact that more awareness needs to be created relating to the properties of the two groups.
Again only 65% of physicians advised their patients to avoid driving and consumption of alcohol after taking the first-generation drugs and only 69% prescribed different antihistamines as per the patient's physical condition. Though significant, these figures need to increase.
However, knowledge about the various criteria for prescribing antihistamines (especially the second-generation ones) was very less as only 15% practitioners were aware of them and only 7% knew about the criterion of updosing the same drug to four times above the licensed dose in urticaria. Hence, greater awareness needs to be created about these guidelines so that the first-generation drugs are prescribed less and the second-generation ones become the mainstay of treatment in urticaria.
Conclusion
Antihistamines are one of the commonly prescribed classes of drugs with a myriad of uses. The second-generation drugs are highly effective with minimum side effects. New criteria have been proposed related to their use in urticaria. A good number of family physicians were aware of these second-generation drugs, but most of them were not aware of the criteria and guidelines for prescribing them. More awareness needs to be dissipated related to the effectiveness and usage of antihistamines to reduce morbidity and thus improve the quality of life of patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Assanasen P, Naclerio RM. Anti-allergic, anti-inflammatory effects of H1 antihistamines in humans. In: Simons FE, editor. Histamine and H1 Antihistamines in Allergic Disease. 2nd ed. New York: Marcel Dekker; 2002. p. 101. [PubMed] [Google Scholar]
- 2.Simons FE. Advances in H1-antihistamines. N Engl J Med. 2004;351:2203–17. doi: 10.1056/NEJMra033121. [DOI] [PubMed] [Google Scholar]
- 3.Urticaria. In: Black AK, Champion RH, editors; Champion RH, Burton JL, Burns DA, editors. Textbook of Dermatology. 6th ed. Oxford, England: Blackwell Science; 1998. pp. 2113–39. [Google Scholar]
- 4.Zuberbier T, Asero R, Bindslev-Jensen C, Walter Canonica G, Church MK, Giménez-Arnau AM, et al. EAACI/GA(2) LEN/EDF/WAO guideline: Management of urticaria. Allergy. 2009;64:1427–43. doi: 10.1111/j.1398-9995.2009.02178.x. [DOI] [PubMed] [Google Scholar]
- 5.Church MK, Church DS. Pharmacology of antihistamines. Indian J Dermatol. 2013;58:219–24. doi: 10.4103/0019-5154.110832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Peggs JF, Shimp LA, Opdycke RA. Antihistamines: The old and the new. Am Fam Physician. 1995;52:593–600. [PubMed] [Google Scholar]
- 7.Hansen J, Klimek L, Hörmann K. Pharmacological management of allergic rhinitis in the elderly: Safety issues with oral antihistamines. Drugs Aging. 2005;22:289–96. doi: 10.2165/00002512-200522040-00002. [DOI] [PubMed] [Google Scholar]
- 8.Holgate ST, Canonica GW, Simons FE, Taglialatela M, Tharp M, Timmerman H, et al. Consensus group on new-generation antihistamines (CONGA): Present status and recommendations. Clin Exp Allergy. 2003;33:1305–24. doi: 10.1046/j.1365-2222.2003.01769.x. [DOI] [PubMed] [Google Scholar]
- 9.Simons FE, Simons KJ. H1 antihistamines: Current status and future directions. World Allergy Organ J. 2008;1:145–55. doi: 10.1186/1939-4551-1-9-145. [DOI] [PMC free article] [PubMed] [Google Scholar]


