Abstract
Background:
Homeless individuals with alcohol use disorders have multiple comorbidities and therefore various service needs. Despite need for services, homeless individuals face numerous barriers to treatment. Little is known about the associations of specific services in relation to homelessness in the context of alcohol problems. The current study analyzed 2-year prospective longitudinal data on a homeless sample, examining relationships between alcohol use disorder, alcohol use, housing status, and service use over time.
Methods:
255 of 400 individuals recruited systematically from shelters and street locations completed 3 annual assessments (69% completion). Data on lifetime and current psychiatric disorders, housing status, and past year service use were obtained and merged with service use data gathered from local agencies. GEE models were created to predict dependent outcome variables of stable housing, alcohol use, and service use in both follow-up years.
Results:
Lifetime alcohol use disorder was positively associated with substance and medical service use. Alcohol problems did not hinder attainment of stable housing, and placement in housing did not necessarily increase risk for alcohol use. Stable housing was negatively associated with psychiatric and substance service use. In the second year, when alcohol use was finally associated with receiving substance services, it appears that these services provided a gateway to psychiatric services. The psychiatric services in turn appeared to provide a gateway to medical services.
Conclusions:
Alcohol use acted differently compared to lifetime alcohol use disorder in relation to service use. Lack of association between alcohol use and housing supports Housing First policy. Obtaining housing may have ameliorative effects on mental health, diminishing perceived need for psychiatric services. Services may also be more accessible during homelessness. Obtaining substance treatment may provide a gateway for those who use alcohol after becoming homeless to connect with psychiatric and medical services, informing policy and practice.
Keywords: Alcohol use, homelessness, Housing First, service utilization
INTRODUCTION
Alcohol problems are highly prevalent in the homeless population. Epidemiological studies using structured diagnostic interviews have reported the lifetime prevalence of alcohol use disorder (AUD) in homeless populations to be about 60% and the current year prevalence to be about 40%,1,2 far higher than general population prevalence rates.3 There is evidence that prevalence of AUDs has been increasing in homeless populations over recent decades.4 North et al.1 found that about two thirds of their homeless sample reported use of alcohol in the previous year, which is the one-year rate of alcohol use in the general population.3
It is important to distinguish among concepts of low-risk alcohol use, risky alcohol use, and AUD as defined in other literature on populations more broadly5,6 because the medical, psychiatric, and social risks differ for these separate types of alcohol use patterns.6-10 Studies of homeless populations have specifically made the distinction between different patterns of alcohol use and related health problems.11,12
It has been well established that alcohol problems are strong contributors to the initiation and maintenance of homelessness. A study investigating the dynamics of homelessness and substance abuse indicated that heavy alcohol use increases the likelihood of subsequent homelessness in the next 6 months by 11%.13 A homeless epidemiologic study by North et al.14 found that the age of onset of AUDs typically preceded the first onset of homelessness and was earlier in homeless compared to non-homeless groups. Additionally, both the presence of AUD and its severity were associated with likelihood, earlier onset, and chronicity of homelessness. The premise of Housing First initiatives is that even people with active AUDs can achieve successful outcomes after receiving housing, but Kertesz et al.15 concluded that more definitive research that overcomes methodological limitations is still needed to determine its success versus risk in this subgroup of the homeless population.
The mechanisms accounting for potentially deleterious associations of alcohol problems with housing outcomes have been mostly unknown. It is possible that alcohol problems present barriers to obtaining housing and to the maintenance of a stable residence. It is also possible that such associations may represent direct effects of alcohol such as problems with the law, inability to sustain behavior conducive to residential stability, or indirect effects through factors comorbid with alcohol problems including medical, psychiatric, and social difficulties. Booth et al.16 have provided an in-depth discussion of the potential mechanisms of the effects of substance abuse on housing outcomes, concluding that prospective longitudinal studies will be needed to disentangle the causal relationships.
AUD is a treatable illness,17-21 even in the homeless population.22 For example, in a study of patients with AUD who received formal treatment and participated in Alcoholics Anonymous, 58% were abstinent at 8 years, more than twice the rate of people who received no treatment.20 A treatment study of individuals with alcohol dependence who were also homeless found that the two-month continuous abstinence rate was 56%.22 Abstinence is the strongest positive outcome, but there exists a variety of other harm reduction strategies that are also considered positive outcomes.23,24 Despite the great need for alcohol treatment in homeless populations, they face many barriers to accessing treatment, including lack of financial resources, poor access to health insurance, non-availability of services, inability to access available services, and stigma.25-27 Additionally, homeless populations have many other problems for which services are greatly needed, including comorbid medical, psychiatric, social, and environmental problems.28 Previous studies of homeless populations have found that alcohol and other drug use disorders are associated with greater service utilization as identified through available public sector service data.29 Further, achieving stable housing may affect service utilization: studies have found that individuals with alcohol problems decreased use of health services after obtaining housing.30-32
Little is known about how alcohol use within versus outside of the context of AUDs relates to service use, or how housing status interacts with these variables. Even less is known about how different types of service use might lead to use of other services in the context of homelessness and alcohol use behaviors. To further investigate these relationships, the current study provides analysis of a longitudinal data set of 255 individuals selected from homeless shelter and street locations and followed for two years. These analyses focus on associations among alcohol consumption; AUDs; housing status; and psychiatric, substance treatment, and medical service use over time.
METHODS
The current study was approved by the Institutional Review Board of Washington University School of Medicine in St. Louis, Missouri. Written informed consents were provided by all participants of the study. A total of 400 participants for this study were recruited systematically from shelters and street locations by study personnel from October 1999 through May 2001 and followed for 2 years. The shelter sample was recruited by random selection from computer-generated lists of shelter guests across all participating shelters proportionate to shelter size. Randomly-generated computerized schedules selected 80% of the sample from 12 homeless shelters. To capture non-sheltered members of the homeless population, the remaining 20% were sampled from 16 systematically traveled circular street routes with computer-randomized starting points (developed prior to this study to maximize street locations traversed by the homeless population). These routes were traveled a maximum of twice, until a homeless participant was identified. Because it is not possible to differentiate homeless from other individuals on the street with certainty,33 every person encountered on the routes was screened for current homelessness until a participant was enrolled in the study.
Inclusion criteria included adults age 18 and above experiencing current homelessness. Homelessness was defined as a 2-week period without a stable address and residing for more than half of that period in a community shelter or in unsheltered environments such as an abandoned building, a car, a bus station, or on the street. Individuals who had spent less than 1 week during their 2 weeks of homelessness staying in other temporary locations such as with friends or relatives were included. Finally, individuals without a stable address for at least 2 weeks and who were residing in inexpensive motels for less than a month were also considered homeless. This relatively conservative definition was chosen to select a sample that was literally homeless and was based on current federal definitions at the time. Exclusion criteria were individuals on street routes within 2 blocks of a shelter, being too intoxicated or otherwise unable to cooperate with a research interview. The study’s overall participation rate was 92%. Participants were incentivized by offering them $25 for completion of the annual interviews, $5 for quarterly interviews, $1 for periodic check-ins with the team, and opportunities to enter monthly and annual lotteries to win $20 and $100 respectively for participation.34
Assessments were conducted with participants at baseline and then annually for 2 years for a total of 3 study assessments. A previous article describes the extensive tracking methodology used to re-locate participants.34 Overall, 69% (N=255) of participants were successfully reassessed in both follow up years with complete longitudinal housing data, and only these participants were included for analyses in this article. Assessments were conducted using the Diagnostic Interview Schedule for DSM-IV35/Homeless Supplement,36 the substance abuse sections of the Composite International Diagnostic Interview-Substance Abuse Module for DSM-III-R,37 the sociodemographic sections of the National Comorbidity Survey interview.38 Lifetime and current psychiatric disorders assessed were major depression, bipolar disorder, schizophrenia, generalized anxiety disorder, panic disorder, antisocial personality disorder, and substance use disorders. At each assessment, participants were asked about their use of mental health and substance abuse services and medical services in the last year, and also their predominant housing status in the past year. At each assessment, the Roche OnTRAK test kit was used to test each participant’s urine for the presence of alcohol and other drugs (cocaine, amphetamines, cannabis, and opiates). There were no statistically significant baseline differences between the participants who followed up with all assessments and those without 3 complete assessments in demographic variables, substance use, chronicity of homelessness, legal problems, or any lifetime or current psychiatric disorders.34
With the permission of participants, their individual service use data were obtained from local medical, mental health, and substance abuse treatment agencies. Service use data were collected through a variety of methods tailored to the capacity of the organization, and included claims data, rosters of participants by date of service use, and individual agencies’ own unique databases of services provided. The service use data were combined with individual report of service use from the structured interviews. The psychiatric services category in this study included psychiatric inpatient, outpatient, day treatment, emergency programs, and pharmacy services. Substance services category included self-help groups, substance abuse individual and group psychotherapy, and substance abuse psychotropic medication management covering any treatment for alcohol or other drug problems together. The medical services category included medical inpatient and outpatient services, medical emergency room visits, medical supply use, and pharmacy services. To address missing data in the study sample, first the missing information was cross-referenced with self-report of service utilization, followed by a multiple-imputation process.
A variable representing lifetime history of serious mental illness was constructed to represent the presence of at least one lifetime diagnosis, including major depression, bipolar disorder, or schizophrenia identified at any of the three study interviews. A variable representing alcohol use in the last year was created from any positive result from either self-report of at least one alcoholic drink or urine substance testing. The drug use disorder variable included as an independent covariate in multivariate models focused on cocaine, because this disorder represented by far the majority of the substance use disorder in this sample and it was highly associated with housing outcomes.1,4
A series of generalized estimating equations (GEE) models were developed to predict dependent outcome variables: stable housing, alcohol use, and service use in the first and second follow-up years. Independent variables entered simultaneously into these models included lifetime AUD, lifetime cocaine use disorder, lifetime serious mental illness, stable housing, current alcohol use, and service use. Independent covariates also entered simultaneously into the model were sex, age, and minority group membership. In the models with the first year dependent variable, only first year independent variables were included, and in the models with the second year dependent variable, both first and second year independent variables were included.
RESULTS
The study sample (N=255) was 73% male, 77% African American, median age 43 years, and 60% high school graduates. A total of 61% (N=156) had a lifetime AUD, 50% (N=127) had a lifetime cocaine use disorder, and 56% (N=142) had a lifetime serious mental illness diagnosed at baseline or either follow up interview.
Of the participants with a lifetime AUD, 86% (134/155) used alcohol during the year prior to study baseline, 67% (104/156) during the first follow up year, and 62% (96/156) in the second follow-up year. Of the participants with a lifetime AUD, 49% (51/104) of those who used alcohol in the first year also received substance treatment in the first year, and 32% (31/96) of those who used alcohol in the second year also received substance treatment in the second year.
Table 1 presents the results of a series of GEE models predicting stable housing, alcohol use, and service use, in the first year (dependent variables, each in a separate model) with simultaneous addition of covariates into the model including lifetime alcohol and cocaine use disorder, lifetime serious mental illness, age, sex, minority group membership, and stable housing, current year alcohol use, and service use. Obtaining stable housing in the first year was not associated with lifetime AUD, lifetime cocaine use disorder, lifetime serious mental illness, alcohol use in the first year, or any type of service use. Men were less likely than women to obtain stable housing in the first year. Alcohol use in the first year was significantly associated with lifetime AUD and male sex. Alcohol use in the first year was negatively associated with psychiatric and medical service use. Psychiatric service use in the first year was significantly associated with serious mental illness. Substance service use in the first year was associated with lifetime alcohol and cocaine use disorder. Substance service use in the first year was also associated with psychiatric service and medical service use. Medical service use in the first year was positively associated with lifetime AUD and negatively associated with lifetime cocaine use disorder.
Table 1.
Multivariate GEE models (one per row) predicting outcomes related to stable housing, alcohol use, and service use in year 1 in a prospective longitudinal 2-year study of a systematically selected homeless sample (N=255) in St. Louis, Missouri
| Year 1 Dependent Variable |
Lifetime alcohol use disorder |
Lifetime cocaine use disorder |
Lifetime serious mental illness |
Stable housing |
Alcohol use |
Psych service use |
Subst. service use |
Medical. service use |
Male sex |
Age | Minority group member ship |
|---|---|---|---|---|---|---|---|---|---|---|---|
| (Significant p values only) | |||||||||||
| Stable housing | .012a | ||||||||||
| Alcohol use | <.001b | .034c | <.001d | ||||||||
| Psychiatric service use | <.001e | .029f | <.001g | ||||||||
| Substance service use | .027h | <.001i | <.001j | <.005k | |||||||
| Medical service use | .042l | .024m | .049n | .005o | |||||||
Relationships in cells with gray shading are negative. All other listed associations are positive.
E=Estimate; SE=Standard Error; CI=Confidence Interval
E=−0.97; SE=0.38; 95% CI=−1.72, −0.22; Z=−2.53.
E=1.77; SE=0.34; 95% CI=1.11, 2.45; Z=5.18.
E=−0.79; SE=0.37; 95% CI=−1.52, −0.06; Z=−2.12.
E=1.66; SE=0.40; 95% CI=0.87, 2.45; Z=4.11.
E=1.46; SE=0.32; 95% CI=0.84, 2.08; Z=4.60.
E=−0.76; SE=0.35; 95% CI=−1.44, −0.08; Z=−2.18.
E=1.05; SE=0.32; 95% CI=0.43, 1.68; Z=3.30.
E=0.80; SE=0.36; 95% CI=0.09, 1.51; Z=2.21.
E=1.17; SE=0.31; 95% CI=0.56, 1.79; Z=3.74.
E=1.07; SE=0.32; 95% CI=0.45, 1.69; Z=3.37.
E=0.97; SE=0.35; 95% CI=0.29, 1.65; Z=2.81.
E=0.74; SE=0.37; 95% CI=0.03, 1.47; Z=2.03.
E=−0.73; SE=0.33; 95% CI=−1.37, −0.10; Z=−2.25.
E=−0.74; SE=0.38; 95% CI=−1.48, −0.01; Z=−1.97.
E=0.96; SE=0.34; 95% CI=0.29, 1.64; Z=2.81.
Table 2 presents the results of a series of GEE models predicting stable housing, alcohol use, and service use, in the second year (dependent variables, each in a separate model) with simultaneous addition of covariates into the model including lifetime alcohol and cocaine use disorder, lifetime serious mental illness, age, sex, minority group membership, and first and second year alcohol use, service use, and stable housing. Stable housing, alcohol use, and all types of service use, in the first year were all significantly associated with the same respective variables in the second year (e.g., year 1 alcohol use was associated with year 2 alcohol use). Stable housing in the second year was negatively associated with current year substance service use, but not associated with lifetime AUD, lifetime cocaine use disorder, lifetime serious mental illness, current or first year alcohol use, or psychiatric or medical service use. Men were less likely than women to be stably housed in the second year. Second year alcohol use was associated with lifetime AUD, current year substance service use, and older age. Second year psychiatric service use was positively associated with lifetime serious mental illness, current year substance service use, and current year medical service use, and negatively associated with stable housing in the first year and minority group membership. Second year substance service use was associated with lifetime cocaine use disorder and current year alcohol use, but not associated with lifetime AUD, lifetime serious mental illness, or medical service use in either year.
Table 2.
Multivariate GEE models (one per row) predicting outcomes related to stable housing, alcohol use, and service use in year 2* in a prospective longitudinal 2-year study of a systematically selected homeless sample (N=255) in St. Louis, Missouri
| Year 2 Dependent Variable |
Lifetime alcohol use disorder |
Lifetime cocaine use disorder |
Lifetime serious mental illness |
Stable housing |
Alcohol use |
Psych service Use |
Substance service use |
Medical service use |
Male sex | Age | Minority group member ship |
|---|---|---|---|---|---|---|---|---|---|---|---|
| (Significant p values only) | |||||||||||
| Stable housing | Y1 <.001a | Y2 .039b | .025c | ||||||||
| Alcohol use | .006d | Y1 <.001e | Y2 .005f | .004g | |||||||
| Psychiatric service use | <.001h | Y1 .013i | Y1 <.001j | Y2 .019k | Y2 <.001l | .020m | |||||
| Substance service use | <.001n | Y2 .002o | Y2 .017p | Y1 <.001q | |||||||
| Medical service use | Y2 <.001r | Y1 <.001s | |||||||||
Relationships in cells with gray shading are negative. All other listed associations are positive. Y1=Year 1, Y2=Year 2.
For independent variables that were measured in both Y1 and Y2 (alcohol use, stable housing, and all services), only Y1 variables were included in models with a Y1 dependent variable, and both Y1 and Y2 variables were included in models with Y2 dependent variable (except for instances in which one of these variables was the same as the dependent variable, in which case the independent variable was not included).
E=Estimate; SE=Standard Error; CI=Confidence Interval
E=1.34; SE=0.33; 95% CI=0.69, 1.99; Z=4.07.
E=−0.76; SE=0.37; 95% CI=−1.49, −0.04; Z=−2.06.
E=−0.94; SE=0.42; 95% CI=−1.77, −0.12; Z=−2.25.
E=1.12; SE=0.40; 95% CI=0.33, 1.90; Z=2.77.
E=2.25; SE=0.36, 95% CI=1.55, 2.95; Z=6.27.
E=1.14; SE=0.41; 95% CI=0.35, 1.94; Z=2.81.
E=0.05; SE=0.018; 95% CI=0.02, 0.09; Z=2.84.
E=1.49; SE=0.42; 95% CI=0.68, 2.31; Z=3.59.
E=−1.06; SE=0.43; 95% CI=−1.90, −0.23; Z=−2.49.
E=2.07; SE=0.40; 95% CI=1.28, 2.86; Z=5.12.
E=1.15; SE=0.49; 95% CI=0.19, 2.12; Z=2.34.p
E=1.92; SE=0.54; 95% CI=0.86, 2.98; Z=3.55.
E=−1.03; SE=0.44; 95% CI=−1.90, −0.16; Z=−2.33.
E=1.65; SE=0.41; 95% CI=0.85, 2.44; Z=4.06.
E=1.16; SE=0.38; 95% CI=0.43, 1.90; Z=3.09.
E=1.13; SE=0.47; 95% CI=0.20, 2.05; Z=2.39.
E=1.60; SE=0.38; 95% CI=0.84, 2.35; Z=4.15.
E=1.74; SE=0.49; 95% CI=0.79, 2.69; Z=3.59.
E=2.02; SE=0.36; 95% CI=1.31, 2.73; Z=5.59.
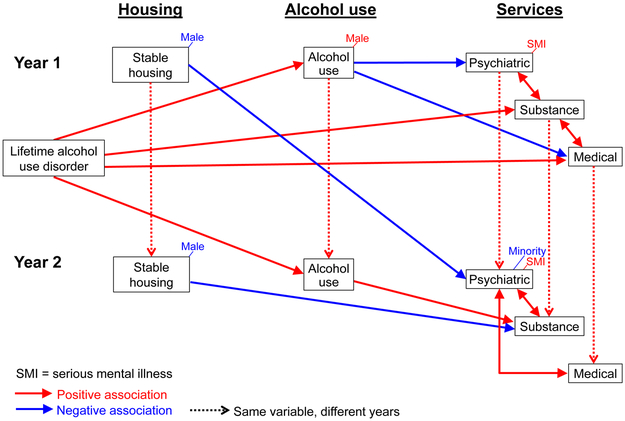
Figure 1 provides a visual model of the significant associations among baseline lifetime AUD, stable housing, alcohol use, and service use across years 1 and 2. Conceptually the model was constructed with service utilization as the final outcome of interest in both years, with stable housing and then alcohol use functioning as intermediate variables associated with subsequent outcomes.
Fig. 1.
Relationships of alcohol, housing, and service use variables
DISCUSSION
The current study provided a prospective longitudinal examination of the temporal associations between alcohol use in a homeless population, housing status, and service use over the course of two years. The findings that neither lifetime AUD nor current alcohol use were related to housing in either year might indicate that past or current alcohol problems do not necessarily impede ability to achieve stable housing, and that placement in housing does not apparently increase risk for alcohol use. Use of alcohol in both years, however, was predicted by a history of alcohol problems. These findings regarding associations of housing and alcohol are in contrast to findings from a previous paper which found cocaine use to be associated with the loss of stable housing.39 The lack of association of housing with alcohol in these analyses are, however, consistent with several Housing First studies that successfully placed people with alcohol problems in housing without subsequent housing instability related to alcohol use.40-44 Additionally, the findings from these analyses are also consistent with Housing First studies that demonstrated that successful placement in housing neither facilitated nor jeopardized alcohol sobriety.42 Further, the lack of association between housing and alcohol is also consistent with Housing First studies that concluded additional services are needed beyond housing to address continuing alcohol problems.15,40
In the first year, lifetime AUD was positively associated with substance and medical service use, but alcohol use was negatively associated with psychiatric and medical service use. In the second year, lifetime AUD was not associated with any service use. Alcohol use, however, was associated with substance service use, but not until the second year, a lagged effect suggesting that achievement of needed treatment was delayed, with apparent substitution of psychiatric services for substance services in the first year. Additionally, alcohol use appeared to act differently than lifetime AUD in relation to service use.
The finding that stable housing in the first year negatively predicted psychiatric services in the second year could suggest that either services were more readily accessible such as through shelters during homelessness, or that achieving housing had such an ameliorative effect on mental health that perceived need for psychiatric services diminished. In general, attaining housing did not result in greater service use of any type. Unlike alcohol use, which was associated with substance service use in the second year, achieving housing was negatively associated with substance service use in the second year. As with psychiatric service use, it is possible that the negative association of housing with substance service use may have reflected better accessibility to substance use services through shelters. These findings are consistent with other studies that have repeatedly found greater service access in homeless circumstances with reduction of service use when housing is attained.32
In the second year, when alcohol use was finally associated with receiving substance services, it appears that these services provided a gateway to psychiatric services. The psychiatric services in turn appeared to provide a gateway to medical services. Thus, the psychiatric and medical services that were never directly accessed were finally achieved through having connected with substance services. The finding of substance services as a gateway to other services including medical services is consistent with another study which also found that substance abuse services provided a point of entry for end-of-life medical and other care services for a homeless population.45 Because the GEE models controlled for psychiatric and substance comorbidity, the associations of medical service use with psychiatric and substance service use are not explained by psychiatric and substance comorbidities. However, because the models did not control for medical comorbidities, the associations between use of medical and other services could relate at least in part to medical comorbidities.
The strengths of this study were the systematic selection of the homeless sample with high participation rates and low attrition without attrition bias. Another strength was the prospective longitudinal annual follow up of the sample over 2 years, identified by Booth et al.16 as essential for disentangling causalities. Psychiatric disorders were assessed using structured diagnostic interviews that provided lifetime and current year diagnosis of AUD as well as current year alcohol use. Agency data and self-report data were combined for optimally comprehensive information on service utilization, using multiple imputation procedures to address missing agency data. Data analysis methods controlled for repeated assessments on the same individuals.
Study limitations include being limited to one city, St. Louis, the data therefore may not necessarily generalize to other geographical locations. Only agency data in the 2 years after baseline were sufficiently complete for these analyses. Urine testing was a poor predictor of alcohol use, and the study relied more on self-report for this information. Finally, more than a decade elapsed since the data were collected, so that the data may not represent current characteristics of the homeless population. Though the data were obtained several years ago, the results revealed new salient information not previously established, and offers a standard for further discussion and comparison with recently acquired data.
Findings from this study are consistent with reported success and stability in Housing First models for individuals with alcohol problems, and with the need for services for other issues such as alcohol, drug, and medical problems in addition to housing. The lack of association found between alcohol use and stable housing in these analyses suggests that the barriers to obtaining stable housing created by cocaine use may not be evident for people with alcohol use or alcohol problems. For people with alcohol problems, it appears their best chances for engaging in substance treatment are while they are homeless, but once they connect with substance services this appears to be an opportunity to help them connect with psychiatric and medical services.
Findings from this study as presented in these analyses and previously published articles have clear implications for policy and practice for homeless populations. For homeless populations with AUD, policy that focuses on Housing First as a first line service is likely to prove effective. However, if AUD is part of multimorbidities such as comorbid with cocaine use disorder, Housing First as a first line service is likely to prove less successful for these populations relative to homeless individuals without these complex comorbidities.28,39,46 Especially for people with multimorbidities, policy for first line service should be substance abuse treatment to serve as a gateway for utilization of psychiatric and medical services as appropriate. Future research delineating the effects of specific diagnoses and clusters of diagnoses on Housing First outcomes might help clarify and increase the effectiveness of current policy advocating for broad dissemination of Housing First.
This study did not specifically examine the cost of the services used in association with housing and alcohol. Future research is needed to understand what these services cost and what associated variables drive cost of service use in subsets of homeless populations. This prospective longitudinal study was merely observational, because it did not experimentally test the effects of housing on other variables. Randomized controlled studies of placement in housing can help clarify the effects of housing on alcohol use and service utilization.
Acknowledgements and Funding:
The authors report no competing interests.
This study was funded by grant R01 DA10713 from the National Institute on Drug Abuse and by grant R25 MH101078 from the National Institute of Mental Health of the National Institute of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Health.
The funding organization had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
REFERENCES
- 1.North CS, Eyrich-Garg KM, Pollio DE, Thirthalli J. A prospective study of substance use and housing stability in a homeless population. Social Psychiatry and Psychiatric Epidemiology. 2010;45(11):1055–1062. [DOI] [PubMed] [Google Scholar]
- 2.Koegel P, Sullivan G, Burnam A, Morton SC, Wenzel S. Utilization of mental health and substance abuse services among homeless adults in Los Angeles. Medical Care. 1999;37(3):306–317. [DOI] [PubMed] [Google Scholar]
- 3.Grant BF, Chou SP, Saha TD, et al. Prevalence of 12-month alcohol use, high-risk drinking, and DSM-IV alcohol use disorder in the United States, 2001-2002 to 2012-2013: results from the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry. 2017;74(9):911–923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.North CS, Eyrich KM, Pollio DE, Spitznagel EL. Are rates of psychiatric disorders in the homeless population changing? American Journal of Public Health. 2004;94(1):103–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Holt S, Tetrault J. Unhealthy alcohol use. Clinics in Liver Disease. 2016;20(3):429–444. [DOI] [PubMed] [Google Scholar]
- 6.Saitz R Unhealthy alcohol use. New England Journal of Medicine. 2005;352(6):596–607. [DOI] [PubMed] [Google Scholar]
- 7.Mukamal KJ, Conigrave KM, Mittleman MA, et al. Roles of drinking pattern and type of alcohol consumed in coronary heart disease in men. New England Journal of Medicine. 2003;348(2):109–118. [DOI] [PubMed] [Google Scholar]
- 8.North CS, Adinoff B, Pollio DE, Kinge S, Downs DL, Pfefferbaum B. Alcohol use disorders and drinking among survivors of the 9/11 attacks on the World Trade Center in New York City. Comprehensive Psychiatry. 2013;54(7):962–969. [DOI] [PubMed] [Google Scholar]
- 9.North CS, Sims O, Hong BA, et al. An empirical study of alcohol consumption by patients considering HCV treatment. The American Journal of Drug and Alcohol Abuse. 2014;40(6):484–489. [DOI] [PubMed] [Google Scholar]
- 10.North CS, Ringwalt CL, Downs D, Derzon J, Galvin D. Postdisaster course of alcohol use disorders in systematically studied survivors of 10 disasters. Archives of General Psychiatry. 2011;68(2):173–180. [DOI] [PubMed] [Google Scholar]
- 11.Stringfellow EJ, Kim TW, Gordon AJ, et al. Substance use among persons with homeless experience in primary care. Substance Abuse. 2016;37(4):534–541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Keane C, Magee CA, Lee JK. Childhood trauma and risky alcohol consumption: A study of Australian adults with low housing stability. Drug and Alcohol Review. 2015;34(1):18–26. [DOI] [PubMed] [Google Scholar]
- 13.McVicar D, Moschion J, van Ours JC. From substance use to homelessness or vice versa? Social Science & Medicine. 2015;136:89–98. [DOI] [PubMed] [Google Scholar]
- 14.North CS, Pollio DE, Smith EM, Spitznagel EL. Correlates of early onset and chronicity of homelessness in a large urban homeless population. The Journal of Nervous and Mental Disease. 1998;186(7):393–400. [DOI] [PubMed] [Google Scholar]
- 15.Kertesz SG, Crouch K, Milby JB, Cusimano RE, Schumacher JE. Housing first for homeless persons with active addiction: are we overreaching? Milbank Quarterly. 2009;87(2):495–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Booth BM, Sullivan G, Koegel P, Burnam A. Vulnerability factors for homelessness associated with substance dependence in a community sample of homeless adults. The American Journal of Drug and Alcohol Abuse. 2002;28(3):429–452. [DOI] [PubMed] [Google Scholar]
- 17.Osterman R, Lewis D, Winhusen T. Efficacy of motivational enhancement therapy to decrease alcohol and illicit-drug use in pregnant substance users reporting baseline alcohol use. Journal of Substance Abuse Treatment. 2017;77:150–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Donoghue K, Elzerbi C, Saunders R, Whittington C, Pilling S, Drummond C. The efficacy of acamprosate and naltrexone in the treatment of alcohol dependence, Europe versus the rest of the world: a meta‐analysis. Addiction. 2015;110(6):920–930. [DOI] [PubMed] [Google Scholar]
- 19.Bouza C, Angeles M, Munoz A, Amate JM. Efficacy and safety of naltrexone and acamprosate in the treatment of alcohol dependence: a systematic review. Addiction (Abingdon, England). 2004;99(7):811–828. [DOI] [PubMed] [Google Scholar]
- 20.Timko C, Moos RH, Finney JW, Lesar MD. Long-term outcomes of alcohol use disorders: Comparing untreated individuals with those in Alcoholics Anonymous and formal treatment. Journal of Studies on Alcohol. 2000;61(4):529–540. [DOI] [PubMed] [Google Scholar]
- 21.Garbutt JC, West SL, Carey TS, Lohr KN, Crews FT. Pharmacological treatment of alcohol dependence: a review of the evidence. JAMA. 1999;281(14):1318–1325. [DOI] [PubMed] [Google Scholar]
- 22.Smith JE, Meyers RJ, Delaney HD. The community reinforcement approach with homeless alcohol-dependent individuals. Journal of Consulting and Clinical Psychology. 1998;66(3):541. [DOI] [PubMed] [Google Scholar]
- 23.Maremmani I, Cibin M, Pani PP, Rossi A, Turchetti G. Harm reduction as “Continuum Care” in alcohol abuse disorder. International Journal of Environmental Research and Public Health. 2015;12(11):14828–14841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Marlatt GA, Witkiewitz K. Harm reduction approaches to alcohol use: Health promotion, prevention, and treatment. Addictive Behaviors. 2002;27(6):867–886. [DOI] [PubMed] [Google Scholar]
- 25.Wenzel SL, Burnam MA, Koegel P, et al. Access to inpatient or residential substance abuse treatment among homeless adults with alcohol or other drug use disorders. Medical Care. 2001;39(11):1158–1169. [DOI] [PubMed] [Google Scholar]
- 26.Kozloff N, Cheung AH, Ross LE, et al. Factors influencing service use among homeless youths with co-occurring disorders. Psychiatric Services. 2013;64(9):925–928. [DOI] [PubMed] [Google Scholar]
- 27.Kushel MB, Vittinghoff E, Haas JS. Factors associated with the health care utilization of homeless persons. JAMA. 2001;285(2):200–206. [DOI] [PubMed] [Google Scholar]
- 28.North CS, Brown ES, Pollio DE. Expanded conceptualization of multimorbidity to encompass substance use disorders and other psychiatric illness. Annals of Clinical Psychiatry. 2016;28(3):182–188. [PubMed] [Google Scholar]
- 29.Bird CE, Jinnett KJ, Burnam MA, et al. Predictors of contact with public service sectors among homeless adults with and without alcohol and other drug disorders. Journal of Studies on Alcohol. 2002;63(6):716–725. [DOI] [PubMed] [Google Scholar]
- 30.Larimer ME, Malone DK, Garner MD, et al. Health care and public service use and costs before and after provision of housing for chronically homeless persons with severe alcohol problems. JAMA. 2009;301(13):1349–1357. [DOI] [PubMed] [Google Scholar]
- 31.Mackelprang JL, Collins SE, Clifasefi SL. Housing First is associated with reduced use of emergency medical services. Prehospital Emergency Care. 2014;18(4):476–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Henwood BF, Dichter H, Tynan R, Simiriglia C, Boermer K, Fussaro A. Service use before and after the provision of scatter-site Housing First for chronically homeless individuals with severe alcohol use disorders. International Journal of Drug Policy. 2015;26(9):883–886. [DOI] [PubMed] [Google Scholar]
- 33.Smith EM, North CS, Spitznagel EL. A systematic study of mental illness, substance abuse, and treatment in 600 homeless men. Annals of Clinical Psychiatry. 1992;4(2):111–120. [Google Scholar]
- 34.North CS, Black M, Pollio DE. Predictors of successful tracking over time in a homeless population. Social Work Research. 2012(36):153–159. [Google Scholar]
- 35.Robins L CL, Bucholz K, et al. Diagnostic Interview Schedule for the DSM-IV (DIS-IV). St Louis, MO: Washington University; 1995. [Google Scholar]
- 36.North CS, Eyrich KM, Pollio DE, Foster DA, Cottler LB, Spitznagel EL. The Homeless Supplement to the Diagnostic Interview Schedule: test‐retest analyses. International Journal of Methods in Psychiatric Research. 2004;13(3):184–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cottler LB, Compton WM. Advantages of the CIDI family of instruments in epidemiological research of substance use disorders. International Journal of Methods in Psychiatric Research. 1993;3(2):109–119. [Google Scholar]
- 38.Kessler RC, McGonagle KA, Zhao S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Archives of General Psychiatry. 1994;51(1):8–19. [DOI] [PubMed] [Google Scholar]
- 39.Ayvaci E, Obiri O, Pollio D, North C. A naturalistic longitudinal study of the order of service provision with respect to cocaine use and outcomes in an urban homeless sample. Epidemiology and Psychiatric Sciences. 2017:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tsai J, Kasprow WJ, Rosenheck RA. Alcohol and drug use disorders among homeless veterans: prevalence and association with supported housing outcomes. Addictive Behaviors. 2014;39(2):455–460. [DOI] [PubMed] [Google Scholar]
- 41.Aubry T, Tsemberis S, Adair CE, et al. One-year outcomes of a randomized controlled trial of housing first with ACT in five Canadian cities. Psychiatric Services. 2015;66(5):463–469. [DOI] [PubMed] [Google Scholar]
- 42.Tsemberis S, Gulcur L, Nakae M. Housing first, consumer choice, and harm reduction for homeless individuals with a dual diagnosis. American Journal of Public Health. 2004;94(4):651–656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Collins SE, Malone DK, Clifasefi SL. Housing retention in single-site Housing First for chronically homeless individuals with severe alcohol problems. American Journal of Public Health. 2013;103(S2):S269–S274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kertesz SG, Weiner SJ. Housing the chronically homeless: high hopes, complex realities. JAMA. 2009;301(17):1822–1824. [DOI] [PubMed] [Google Scholar]
- 45.McNeil R, Guirguis-Younger M, Dilley LB, Aubry TD, Turnbull J, Hwang SW. Harm reduction services as a point-of-entry to and source of end-of-life care and support for homeless and marginally housed persons who use alcohol and/or illicit drugs: a qualitative analysis. BMC Public Health. 2012;12(1):312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Urbanoski K, Veldhuizen S, Krausz M, et al. Effects of comorbid substance use disorders on outcomes in a Housing First intervention for homeless people with mental illness. Addiction. 2018. [DOI] [PubMed] [Google Scholar]