Abstract
Purpose
The objectives of this study were to examine different speech profiles among children with dysarthria secondary to cerebral palsy (CP) and to characterize the effect of different speech profiles on intelligibility.
Method
Twenty 5-year-old children with dysarthria secondary to CP and 20 typically developing children were included in this study. Six acoustic and perceptual speech measures were selected to quantify a range of segmental and suprasegmental speech characteristics and were measured from children's sentence productions. Hierarchical cluster analysis was used to identify naturally occurring subgroups of children who had similar profiles of speech features.
Results
Results revealed 4 naturally occurring speech clusters among children: 1 cluster of children with typical development and 3 clusters of children with dysarthria secondary to CP. Two of the 3 dysarthria clusters had statistically equivalent intelligibility levels but significantly differed in articulation rate and degree of hypernasality.
Conclusion
This study provides initial evidence that different speech profiles exist among 5-year-old children with dysarthria secondary to CP, even among children with similar intelligibility levels, suggesting the potential for developing a pediatric dysarthria classification system that could be used to stratify children with dysarthria into meaningful subgroups for studying speech motor development and efficacy of interventions.
Dysarthria affects functional communication for over 50% of children with cerebral palsy (CP; Nordberg, Miniscalco, Lohmander, & Himmelmann, 2013). The speech presentations of children with dysarthria secondary to CP are diverse, some presenting with only a mild dysarthria and others presenting with anarthria, resulting in no functional verbal communication (Hustad, Gorton, & Lee, 2010). Even speakers with CP who have similar intelligibility levels can have widely varying perceptual and acoustic speech features (Allison & Hustad, 2018; Schölderle, Staiger, Lampe, Strecker, & Ziegler, 2016). Despite this heterogeneity, variations in profiles of abnormal speech features have not been well characterized in children with CP. Identifying subgroups of children with similar speech profiles and developing a system for classifying these profiles are needed to better understand the different speech manifestations of pediatric dysarthria and could provide a meaningful way to group children for studying trajectories of speech development and responses to intervention.
Development and validation of classification tools have been a major focus of CP research across disciplines, and several widely used systems now exist for classifying children with CP according to underlying neuropathology, gross motor function, fine motor function, and communication profiles (Bax, Goldstein, Rosenbaum, & Levinton, 2005; Bax, Tydeman, & Flodmark, 2006; Eliasson et al., 2006; Hidecker et al., 2011; Himmelman, Beckung, Hagberg, & Uvebrant, 2006; Hustad et al., 2010; Pakula, Van Naarden Braun, & Yeargin-Allsopp, 2009; P. Rosenbaum, Paneth, Leviton, Goldstein, & Bax, 2007; P. L. Rosenbaum, Palisano, Bartlett, Galuppi, & Russell, 2008). These systems have led to important advancements in understanding and clinical management of children with CP including enabling comparisons between subgroups, predicting functional outcomes, and understanding different trajectories of development (Hanna, Bartlett, Rivard, & Russell, 2008; P. L. Rosenbaum et al., 2002; Wood & Rosenbaum, 2000). In the communication domain, a speech-language profile group classification system developed in our laboratory (Hustad et al., 2010) has been used to model developmental trajectories in speech and language skills in children with CP (Hustad, Allison, McFadd, & Riehle, 2014; Hustad, Allison, et al., 2016; Lee & Hustad, 2013). However, to our knowledge, no similar efforts have been undertaken to understand different speech motor profiles among children with dysarthria secondary to CP. Determining whether different speech motor subgroups can be identified among children with dysarthria secondary to CP is a first step toward better explaining the heterogeneity in speech presentations in this population and has important theoretical and clinical implications for understanding trajectories of speech motor development and differential responses to speech intervention.
Sources of Variability in Speech Features
A wide variety of speech features have been associated with dysarthria in children with CP. Commonly reported suprasegmental characteristics include hypernasality, deviant voice quality (e.g., breathy, harsh, or strained–strangled voice quality), and slow speaking rate (Duffy, 2013; Hodge, Wellman, Caruso, & Strand, 1999; Workinger & Kent, 1991). Segmental error patterns have also been reported in speakers with CP, including reduction in voicing distinctions (Nordberg, Miniscalco, & Lohmander, 2014; Platt, Andrews, & Howie, 1980), vowel errors (Ansel & Kent, 1992; Workinger & Kent, 1991), and consonant omissions, distortions, and substitutions (Byrne, 1959; Nordberg et al., 2014; Platt et al., 1980; Workinger & Kent, 1991).
Many factors can influence the profile of speech features exhibited by an individual child with CP. Motor control of all physiologic speech subsystems (i.e., respiration, phonation, resonance, and articulation) can be affected to varying degrees, depending on the child's underlying neuropathology. These physiologic impairments result in alterations to the acoustic signal, which are then perceived by listeners as deviant speech features typically associated with dysarthria (Duffy, 2013). In addition, approximately 50% of children with CP have concomitant language or cognitive deficits (Hustad et al., 2010; Sigurdardottir & Vik, 2011), and factors related to children's language, cognitive, and speech sound development can also influence their speech characteristics (Hustad, Schueler, Schultz, & Duhadway, 2012; Nip, 2013; Peeters, Verhoeven, de Moor, & van Balkom, 2009). Although children with dysarthria secondary to CP vary widely in their speech characteristics, the vast majority exhibit reduced speech intelligibility. Because of its importance to functional communication and pervasiveness in adult and pediatric populations with dysarthria, intelligibility is commonly used as an index of severity in the dysarthria literature (Kent, Weismer, Kent, & Rosenbek, 1989; Y. Kim, Kent, & Weismer, 2011; Lee, Hustad, & Weismer, 2014; Weismer & Laures, 2002; Weismer, Martin, & Kent, 1992).
Due to the variation in underlying neurological and physiological impairments among children with CP, there are also likely to be individual differences in the specific speech features that have the greatest impact on intelligibility. Much research effort has been devoted to identifying speech features that contribute most to intelligibility impairment in speakers with dysarthria (e.g., Weismer et al., 1992). In children with CP, multiple acoustic correlates of reduced intelligibility have been identified, including reduced vowel space area (DuHadway & Hustad, 2012; Higgins & Hodge, 2002; Liu, Tsao, & Kuhl, 2005), shallower F2 slope (Lee et al., 2014), and slow articulation rate (DuHadway & Hustad, 2012). Although some research suggests that profiles of speech features in speakers with dysarthria vary as a function of overall severity (Y. Kim et al., 2011; Lee et al., 2014), other studies have suggested that profiles of impaired speech characteristics are not necessarily related to severity of intelligibility impairment (Allison & Hustad, 2018; Schölderle et al., 2016) and that factors contributing to intelligibility may differ depending on children's relative degree of speech subsystem involvement (Allison & Hustad, 2014). For example, children who have relatively intact respiratory support but moderate articulatory imprecision and children who have severe respiratory impairment but only mild articulatory involvement may have similar intelligibility levels but would be expected to exhibit different profiles of acoustic and perceptual speech characteristics and may differ in the factors most affecting their intelligibility.
Because a primary goal of speech therapy for children with dysarthria is to maximize intelligibility, there is an important need for a better understanding of how differences in children's speech motor profiles relate to their intelligibility. Recent research efforts have begun to demonstrate promising gains in speech function for children with CP after an intensive subsystem-based intervention (Pennington, Miller, Robson, & Steen, 2010) and Lee Silverman Voice Treatment (Boliek & Fox, 2014, 2016; Fox & Boliek, 2012; Levy, Ramig, & Camarata, 2012); however, responses were variable across individual children, and authors highlighted the need for understanding characteristics of responders versus nonresponders (Boliek & Fox, 2014; Levy et al., 2012; Pennington et al., 2010, Miller et al., 2013). A recent study on adults with dysarthria demonstrated that participants' responses to speech strategies differed depending on their baseline speech characteristics (Fletcher, McAuliffe, Lansford, Sinex, & Liss, 2017). Identifying different speech motor profiles among children with dysarthria and understanding the relationship of these profiles to intelligibility could provide a framework for evaluating differences in responses to interventions across children with CP.
Classification of Pediatric Dysarthria
There are several possible approaches for classifying dysarthria subtypes in children with CP. The “gold standard” Mayo Clinic system was developed to identify dysarthria subtypes in adults with acquired speech impairment based on profiles of auditory–perceptual speech features (Darley, Aronson, & Brown, 1969); however, the system was not designed to account for developmental influences on speech characteristics, and thus the validity of its application to pediatric dysarthria is highly questionable (Morgan & Liegeois, 2010). Early attempts at identifying subtypes of dysarthria in children with CP focused on comparing auditory–perceptual speech features of children with different medical subtypes of CP (i.e., spastic vs. athetoid CP). These studies found largely overlapping perceptual features between groups (Byrne, 1959; Irwin, 1955; Workinger & Kent, 1991), suggesting that children's medical classification of CP type was not particularly useful for differentiating speech subgroups. Other studies have focused on characterizing impairments in each speech subsystem (Lee et al., 2014; Pennington et al., 2010); however, this approach has not been used to identify subgroups of children with CP who have different speech subsystem profiles.
A few studies have taken a data-driven approach to speech classification in other populations, including adults with dysarthria (Liss et al., 2009) and children with and without speech sound disorders (Vick et al., 2012, 2014). Data-driven approaches use measures of multiple speech dimensions to either classify speakers into predefined categories or identify naturally occurring subgroups of speakers. The benefit of the latter approach is that it does not rely on a priori assumptions about speech profiles and therefore provides an unbiased method for determining similarity in speech characteristics between speakers. Data-driven studies of dysarthria features in adults have shown that acoustic measures can be used to identify meaningful subgroups of speakers with different severity levels and dysarthria subtypes (Y. Kim et al., 2011; Liss et al., 2009) and that even untrained listeners can categorize speakers with dysarthria based on their perceptual similarity (Lansford, Liss, & Norton, 2014). In children, Vick and colleagues found that acoustic and kinematic measures could be used to identify and characterize naturally occurring subgroups of speakers with similar speech features among typically developing (TD) children (Vick et al., 2012) and in children with speech sound disorders (Vick et al., 2014). To our knowledge, no previous studies have taken a similar data-driven approach to classification of pediatric dysarthria. Classification studies in children must carefully account for development, because of the rapid changes in speech development that occur in early childhood. Thus, studies focusing on classification of children within narrow age ranges are necessary to ensure that resulting speech subgroups are not confounded by developmental differences.
The objectives of the present research were to begin examining different speech profiles among 5-year-old children with dysarthria by identifying naturally occurring subgroups of children who have similar speech features and to characterize the effect of different speech profiles on intelligibility. To do this, we chose objective speech measures that reflected a variety of segmental and suprasegmental speech dimensions known to be impaired in children with CP and captured function of multiple speech subsystems. We hypothesized that measures of multiple speech dimensions could be used to identify children with dysarthria who have similar speech motor profiles. Furthermore, given evidence of the variation between individual children with CP in factors affecting intelligibility (Allison & Hustad, 2014) and the heterogeneity in speech motor characteristics among children with CP, we hypothesized that different speech profiles could exist independent of severity of intelligibility impairment. Specific research questions were the following:
What subgroups of children with similar speech features exist among 5-year-olds with dysarthria secondary to CP?
How do subgroups of children with dysarthria differ with regard to profiles of speech characteristics and intelligibility?
Method
Participants
Children With CP
Twenty 5-year-old children with CP were selected for inclusion in this study from a larger cohort of children with CP participating in an ongoing longitudinal project. This study focused on 5-year-old children because, at this age, speech development is not yet complete, but children are generally able to produce multiword sentences without difficulty. Focusing on this narrow age window enabled characterization of children's connected speech within a tightly controlled developmental window, thus minimizing the possibility of developmental effects influencing our findings. Children were selected for this sample who had clear signs of dysarthria. There is no accepted list of standard criteria for diagnosing dysarthria in children, and the diagnosis is typically made by speech-language pathologists (SLPs) based on the presence of any obvious audible signs of dysarthria in one or more speech subsystems (i.e., articulatory imprecision, slow speaking rate, deviant voice quality, hypernasality, or reduced respiratory support) as well as visual evidence of abnormal orofacial and/or respiratory movements during speech associated with abnormal tone or weakness (Duffy, 2013). For this study, two experienced SLPs independently made clinical judgments regarding the presence of dysarthria based on video and audio recordings of an oral motor examination, sentence repetition task, and spontaneous speech sample. There was 100% agreement between the SLPs regarding the presence of dysarthria. Children with CP also met the following additional inclusion criteria: (a) ability to repeat sentences of at least five words in length and (b) pass a hearing screening. Gross motor function, language skills, and dysarthria severity, as indexed by speech intelligibility scores (Kent et al., 1989; Y. Kim et al., 2011), were measured but not explicitly controlled, because we were interested in examining dysarthria profiles within a representative sample of children with dysarthria and CP in a narrow developmental age window. Gross Motor Function Classification System (Palisano, Rosenbaum, Bartlett, & Livingston, 2007) levels, receptive language standard scores on the Test for Auditory Comprehension of Language–Fourth Edition (Carrow-Woolfolk, 2014), and intelligibility scores for each child with CP are listed in Table 1. Overall, children with CP had widely ranging gross motor function levels, and 30% had co-occurring language impairment. Dysarthria severity, as indexed by speech intelligibility measurements from the Test of Children's Speech (TOCS+; Hodge & Daniels, 2007), also varied widely across participants; intelligibility levels ranged from 9% to 86%, with the majority in the moderate to severe range (26%–75% intelligibility).
Table 1.
Demographic, language, and intelligibility characteristics of children with cerebral palsy (CP).
| Child ID | Sex | Age (in months) | TACL-4 SSa | Overall intelligibility (%) | GMFCS b | Anatomic involvement |
|---|---|---|---|---|---|---|
| CP01 | F | 67 | 83 | 85.6 | I | Left hemiplegia |
| CP02 | F | 62 | 106 | 35.7 | IV | Quadriplegia |
| CP03 | F | 66 | 76 | 35.5 | II | Diplegia |
| CP04 | F | 62 | 85 | 57.6 | I | Left hemiplegia |
| CP05 | F | 63 | 119 | 9.5 | II | Right hemiplegia |
| CP06 | F | 63 | 68 | 31.9 | III | Quadriplegia |
| CP07 | F | 61 | 102 | 58.9 | I | Right hemiplegia |
| CP08 | F | 60 | 128 | 55.6 | III | Right hemiplegia |
| CP09 | F | 71 | 76 | 25.6 | V | Quadriplegia |
| CP10 | F | 62 | 74 | 60.7 | IV | Diplegia |
| CP11 | F | 60 | 124 | 64.0 | IV | Diplegia |
| CP12 | F | 62 | 87 | 40.2 | II | Right hemiplegia |
| CP13 | F | 61 | 115 | 86.3 | I | Unknown |
| CP14 | M | 63 | 87 | 71.9 | IV | Quadriplegia |
| CP15 | M | 68 | 98 | 31.7 | IV | Quadriplegia |
| CP16 | M | 62 | 100 | 57.2 | I | Diplegia |
| CP17 | M | 69 | 94 | 59.9 | IV | Quadriplegia |
| CP18 | M | 71 | 72 | 71.6 | III | Right hemiplegia |
| CP19 | M | 65 | 104 | 36.5 | I | Right hemiplegia |
| CP20 | M | 66 | 87 | 38.6 | I | Right hemiplegia |
Note. TACL-4 = Test for Auditory Comprehension of Language–Fourth Edition; SS = standard score; GMFCS = Gross Motor Function Classification System; F = female; M = male.
TACL-4 SS (M = 100, SD = 15).
GMFCS rating (I = no/mild impairment, V = severe impairment).
Children with CP and dysarthria will be subsequently referred to as the group with speech motor impairment (SMI group), consistent with the Speech Language Profile Group communication classification scheme previously developed by our research group to characterize communication profiles of children with CP (Hustad et al., 2010). For this study, children with SMI with and without comorbid language impairment were pooled together. Data from this cohort of children have been reported (Allison & Hustad, 2018), and one of these children has been included in other previous publications (Lee & Hustad, 2013; Lee et al., 2014). The mean age of children in the SMI group was 64.2 months (SD = 3.5 months).
TD Children
Twenty 5-year-old TD children participated as a control group. Children in the TD group were matched for age and sex to participants in the SMI group and met the following inclusion criteria: (a) no reported history of speech, language, or learning problems; (b) pass the Preschool Language Scale–Fourth Edition Screening Test (Zimmerman, Steiner, & Pond, 2005); (c) achieve a standard score within the average range on the Arizona Articulation Proficiency Scale–Third Revision (Fudala, 2000); and (d) pass a hearing screening. Any child who could not repeat sentences of at least five words in length on the speech task was excluded from this study. The mean age of children in the TD group was 63.8 months (SD = 3.09 months). Overall intelligibility of children in the TD group on the TOCS+ ranged from 85% to 96% (M = 91.5%, SD = 3.1%).
Acquisition of Speech Samples
Children in both the SMI group and the TD group completed a standard research protocol for obtaining speech samples. Data collection sessions were conducted in a sound-attenuated room by a certified SLP. All children were asked to repeat an identical set of 42 single words and 60 sentences taken from the TOCS+ for research purposes. Sentences ranged from two to seven words in length and included 10 sentences of each length. Children heard audio-recorded adult models of each word or sentence presented with a related picture and were asked to repeat each stimulus item. Children's productions were recorded using a digital audio recorder (Marantz PMD 570) at a 44.1-kHz sampling rate (16-bit quantization) with a condenser studio microphone (Audio-Technica AT4040) positioned near the child's mouth, using a floor stand. A research assistant monitored the level of the signal on a mixer (Mackie 1202 VLZ) to ensure optimized recording levels and to avoid peak clipping.
Intelligibility
Intelligibility data were obtained by having unfamiliar adult listeners provide orthographic transcriptions of children's recorded speech samples. Audio recordings of the children's word and sentence productions were segmented into individual sound files for each utterance and presented to listeners in a sound-attenuated booth. Two hundred adult listeners (5 listeners per child × 40 children) participated. Fifty-eight men and 142 women between the ages of 18 and 40 years (M = 21 years, SD = 5 years) participated as listeners. Listeners all passed a hearing screening and had no specific training or expertise in listening to impaired speech. Each listener heard the 102 utterances produced by one child and were asked to transcribe what they thought the child said for each utterance, according to a previously published protocol (Hustad et al., 2010). Listeners were blinded to the child's clinical status (i.e., CP or TD), were presented with the child's utterances in a randomized order, and were only able to listen to each utterance one time. Custom software was used to compare listeners' transcriptions to the actual utterances produced by the child. For each utterance, intelligibility was calculated as the percentage of stimulus words correctly identified by the listener. These utterance-level intelligibility scores were averaged across utterances of the same length to obtain an intelligibility score for single words and sentences of each length for each listener (e.g., intelligibility scores of all two-word sentences from the TOCS+ were averaged to obtain a mean two-word intelligibility score). For each child, overall intelligibility was determined by averaging the single word and sentence intelligibility scores for each listener and then calculating the mean overall intelligibility scores across the five listeners, consistent with procedures used in prior publications (Allison, Annear, Policicchio, & Hustad, 2017; Allison & Hustad, 2018; Hustad et al., 2010; Hustad, Oakes, McFadd, & Allison, 2016).
Speech Measures
Six speech measures were obtained from children's productions of 10, five-word sentences from the TOCS+. Five-word sentences were chosen for this analysis because this length is consistent with expected mean length of utterance for 5-year-old children (Rice et al., 2010). Children produced each of the five-word sentences one time. Measures were selected to quantify segmental and suprasegmental speech features known to be associated with dysarthria in children with CP and to sample multiple speech subsystems. Segmental measures were chosen to reflect precision of vowel production (i.e., F2 range), stop consonant production (i.e., proportion of bursts produced), and voicing distinctions (i.e., proportion of closure interval voicing). Suprasegmental measures were selected to reflect voice quality disturbance (i.e., proportion of deviant voice quality), slow rate (i.e., articulation rate), and hypernasality (i.e., nasality rating). Of the six measures, five were acoustic measures made by the first author and a research assistant, both of whom were blinded to the subjects' diagnosis. One measure, nasality rating, was a perceptual rating made by 10 certified SLPs with at least 1 year of experience in assessing or treating children with dysarthria.
Segmental and suprasegmental speech measures are described briefly below, and measurement procedures are detailed in Table 2. Methods for all acoustic measures have also been described in a previous publication (Allison & Hustad, 2018).
Table 2.
Summary of measurement procedures for segmental and suprasegmental speech measures.
| Perceptual dimension | Measure | Procedures | |
|---|---|---|---|
| Segmental | Imprecise articulation: vowel distortion | F2 range of diphthongs | For the six diphthongs produced, F2 trajectories were generated using linear predictive coding in TF32. F2 range (max F2–min F2) was calculated for each diphthong and then averaged across the six diphthongs to obtain an average F2 range for each child. |
| Imprecise articulation: consonant distortions/omissions | Proportion of bursts produced | For 18 plosive consonants, the presence of bursts was determined through visual judgments of screenshots of the spectrogram and waveform for each five-word sentence, without accompanying audio. Locations of target bursts were marked using red lines along the bottom of the spectrogram. Bursts were operationally defined as a distinct line of energy extending across at least 50% of the frequency range present within the target window. For each child, proportion of bursts = number of bursts produced / number of target consonants. | |
| Imprecise articulation: consonant voicing errors | Closure interval voicing | For seven postvocalic voiceless stops, duration of closure interval voicing was measured as the time between the point of closure and the end of voicing (i.e., the point at which glottal pulses terminated). These values were divided by closure interval duration to yield a proportion of persistent closure interval voicing for each target consonant. Proportions were then averaged across the set of target consonants to obtain an average proportion of closure interval voicing for each child. | |
| Suprasegmental | Breathy, harsh, or strained/strangled voice quality | Proportion of deviant voice quality | Each of the 10 sentences produced by each child was perceptually judged for the presence of deviant voice quality. For each sentence identified as containing deviant voice quality, the durations of deviant voice segments were acoustically measured. The proportion of deviant voice quality (summed duration of deviant voice segments/utterance duration [excluding pauses]) was calculated for each sentence and then averaged across the 10 sentences to obtain an average proportion of deviant voice quality for each child. |
| Hypernasality | Nasality rating | Ten SLPs listened to recordings of each child producing the set of five-word sentences and provided a rating for each child's degree of hypernasality on a 7-point Likert scale (1 = normal nasality, 7 = severe hypernasality). | |
| Slow rate | Articulation rate | For each of the 10 sentences produced, articulation rate was quantified as rate of speech (in syllables per second), exclusive of silent intervals longer than 200 ms. Rate was calculated for each sentence as the number of syllables divided by the corrected utterance duration (total utterance duration − summed pause duration). Articulation rate was averaged across the 10 sentences to yield an average articulation rate for each child. | |
Segmental Measures
F2 range of diphthongs was selected as an index of articulatory precision in vowel production. Vowel distortions are a known feature of speech production in children with dysarthria secondary to CP (Workinger & Kent, 1991). Children with dysarthria secondary to CP have been shown to have reduced F2 excursions and shallower F2 slopes in diphthong production, compared with healthy controls (Lee et al., 2014). Measures of F2 excursion have also been shown to correlate with intelligibility in children with CP (Lee et al., 2014), suggesting their utility as an index of articulatory precision. For each child, F2 range was measured for six diphthongs produced across the set of five-word sentences (i.e., “likes,” “toy,” “out,” “tie,” “toys,” “away”), based on time histories of F2 trajectories generated with linear predictive coding in TF32 (Milenkovic, 2002). F2 range was measured for 99.6% of the 240 target diphthongs (40 children × 6 tokens); one diphthong from a child in the SMI group was not measurable because the child truncated the word.
Proportion of observable bursts was selected as an index of consonant precision because children with dysarthria have imprecise articulation that can impact articulatory closure during the production of plosives, thus potentially leading to decreased burst realization. Omission and distortion of consonants, including plosives, are known to be common in children with CP (Byrne, 1959; Nordberg et al., 2014), and research suggests that burst realization may be reduced in adult speakers with dysarthria (Ackermann & Ziegler, 1991; Ansel & Kent, 1992; Liu, Tseng, & Tsao, 2000; Ozsancak, Auzou, Jan, & Hannequin, 2001). For each child, the presence or absence of a visible burst on the spectrogram was judged for 18 initial and medial plosive consonants (i.e., “baby,” “toy,” “hotdogs,” “happy birthday,” “gun,” “doesn't,” “good,” “keep,” “tie,” “garbage,” “bag,” “give,” “put,” “toys”). The proportion of plosive consonants with an observable burst was calculated for each child. Burst presence was judged for 99.3% of the 720 target plosives; two tokens from children in the TD group and three tokens from children in the SMI group were omitted because the children did not produce the target consonant.
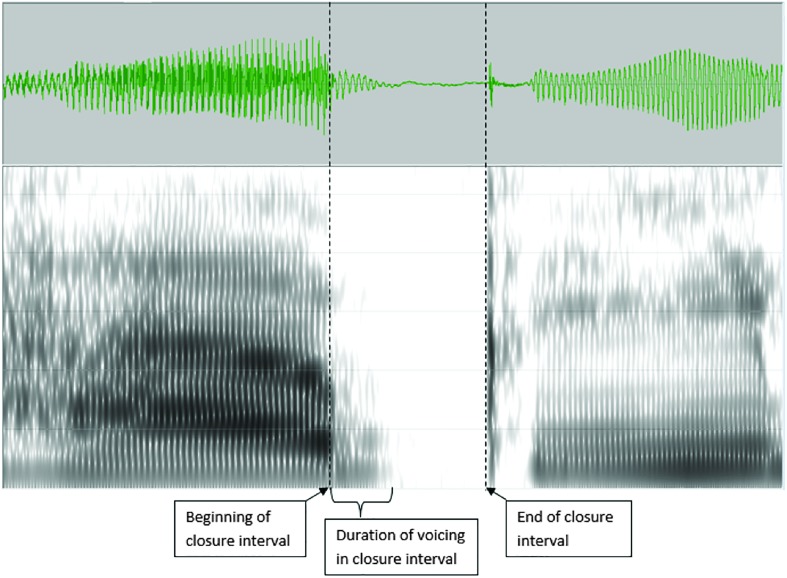
Proportion of closure interval voicing was examined as a measure of children's phonatory control for making voicing distinctions. Voicing errors have been reported as a segmental characteristic of speakers with dysarthria secondary to CP (Ansel & Kent, 1992; Nordberg et al., 2014; Platt et al., 1980). When voiceless stop consonants follow a vowel, voicing from the vowel can briefly persist into the closure interval associated with the consonant. An example of this from a TD child is shown in Figure 1. Offset of this voicing in the closure interval is one cue to the voicing status of the following consonant (Lisker, 1986). Dysarthria may impact the precise timing of voicing offset for the production of voiceless consonants, which could contribute to reduced clarity of voiced/voiceless distinctions. Thus, the duration of persistent voicing in closure intervals may be sensitive to differences in how children with dysarthria regulate their phonation to make voicing distinctions compared with TD children. For each child, the proportion of persistent voicing in closure intervals was measured for seven postvocalic voiceless stop consonants (i.e., “likes,” “eat,” “happy,” “shoots,” “that,” “keep,” “out,” “up”). This measurement was completed for 90% of the 320 target final consonants (40 children × 8 target consonants); six tokens from children in the TD group and 29 tokens from children in the SMI group could not be measured because of final consonant deletion, aphonia, or cluster reduction (e.g., if the child said “shoos” instead of “shoots”).
Figure 1.
Example measurement of closure interval voicing associated with /p/ in the production of the word “happy” in a typically developing child.
Suprasegmental Measures
Proportion of deviant voice quality was examined as a suprasegmental measure of voice quality because vocal quality disturbances are known perceptual features of pediatric dysarthria (van Mourik, Catsman-Berrevoets, Paquier, Yousef-Bak, & van Dongen, 1997; van Mourik, Catsman-Berrevoets, Yousef-Bak, Paquier, & van Dongen, 1998; Workinger & Kent, 1991), and acoustic studies have shown greater vocal instability in children with dysarthria than TD children (Cornwell, Murdoch, Ward, & Morgan, 2003). Periods of deviant voice quality (i.e., phonation breaks, glottal fry, breathiness, aphonia, diplophonia, wet/gurgly voice, and rough or hoarse voice) were identified and measured using a hybrid perceptual–acoustic two-step process: (a) Three researchers independently rated each of the 10 sentences produced by each child for the presence of audible periods of deviant voice quality, and (b) each sentence identified by at least two raters as containing deviant voice quality was then subjected to acoustic analysis. During this step, researchers used visual evidence from the waveform and spectrogram (i.e., deviations from a normal periodicity pattern in vocalic segments) in conjunction with auditory information to identify the beginning and end points of deviant voice segments and measure their durations. The durations of deviant voice segments were used to calculate the proportion of deviant voice quality for each sentence and an average proportion of deviant voice quality for each child. Of 400 total sentences across the 40 participants, 236 (59%) were measured acoustically (142/200 sentences from children in the SMI group [72%] and 94/200 sentences from children in the TD group [47%]).
Articulation rate was selected because slow speaking rate is a key characteristic of dysarthria and common in children with CP (Hustad et al., 2010; Nip, 2013; Workinger & Kent, 1991). Articulation rate is influenced by coordination and timing at all speech subsystem levels. Articulation rate was quantified as rate of speech (in syllables per second [syll/s]), exclusive of silent intervals longer than 200 ms. For each child, articulation rate was obtained for each of the 10 five-word sentences produced and used to calculate an average articulation rate. Because children repeated sentences after a prerecorded model, it is possible that the speaking rate of the model influenced children's articulation rates; however, articulation and speaking rate from the TOCS+ have been previously shown to correlate with intelligibility in children with CP (DuHadway & Hustad, 2012). Articulation rate was calculated for 100% of the sentences.
Nasality ratings by SLPs were used as a measure of resonance because hypernasality is a common perceptual feature of dysarthria in children with CP (Workinger & Kent, 1991). Perceptual ratings of nasality were used because acoustic measures of hypernasality from recorded speech samples have primarily been studied in isolated vowels and single-word productions (Chen, 1995; Kataoka, Warren, Zajac, Mayo, & Lutz, 2001; Lee et al., 2014) and were not appropriate for use with the connected speech samples in this study. Ten SLPs with at least 1 year of experience in treating children with dysarthria rated each child's degree of hypernasality on a 7-point Likert scale by listening to prerecorded speech samples via a web interface. They were instructed to use headphones when completing the tasks and asked to adjust their computer's volume to a comfortable listening level before beginning the experiment. Before beginning the task, SLPs were provided with examples of a speech sample with “normal” nasality (rating = 1) and “severe hypernasality” (rating = 7) as a frame of reference. During the task, SLPs were presented with speech samples from all 40 children in a randomized order. Each speech sample was composed of one child producing the set of 10 five-word utterances. Transcripts of the target sentences were presented along with speech samples to minimize the impact of reduced intelligibility on nasality ratings. After each speech sample was played one time, the SLPs provided a rating between 1 and 7. After every five speech samples, the “normal” reference sample was presented again to help SLPs anchor their ratings, consistent with previous literature (Brancamp, Lewis, & Watterson, 2010; Weismer & Laures, 2002). SLPs were instructed to listen specifically to each child's resonance characteristics and to judge the degree of hypernasality independent of overall severity of speech involvement. SLPs were blinded to the clinical status of participants. Nasality ratings were collected from all 10 SLPs for all 40 children. Ratings from the 10 SLPs were then averaged to obtain a mean nasality rating for each child.
Reliability
Acoustic variables were remeasured for 20% of the children (four TD children and four children with SMI) as a basis for interjudge and intrajudge reliability. For interjudge reliability, a second researcher trained in acoustic analysis independently measured the speech samples. Pearson product–moment correlations showed a strong agreement between the first and second judges for all acoustic measures (r = .93–.99), except for a moderately high (r = .74) correlation between judges for the duration of deviant voice quality intervals. Many factors are known to affect interrater reliability of perceptual voice quality ratings (Kreiman & Gerratt, 2000). In this study, we attempted to increase the objectivity of voice quality measurements through a combined perceptual–acoustic approach. Mean absolute differences in measurements between judges were as follows: F2 range = 109 Hz, voicing duration in closure intervals = 0.004 s, duration of deviant voice quality = 0.048 s, and articulation rate = 0.1 syll/s.
Intrajudge reliability was based on remeasurement of 20% of the speech samples by the first author. Pearson product–moment correlations showed a strong agreement between the first and second ratings for all measures (r = .94–.99). Mean absolute differences between the first and second measurements were as follows: F2 range = 145 Hz, voicing duration in closure intervals = 0.003 s, duration of deviant voice quality = 0.024 s, and articulation rate = 0.05 syll/s. Reliability measurements were within an acceptable range and consistent with prior literature (Auzou et al., 2000; Hustad et al., 2010; Rosen, Goozée, & Murdoch, 2008).
Interjudge and intrajudge reliability was also conducted for nasality ratings completed by the 10 SLPs. A two-way random-effects intraclass correlation coefficient using absolute agreement (Koo & Li, 2016) was conducted in SPSS (v.21) to assess interjudge reliability across ratings of all 10 SLPs. Results of this analysis revealed moderate reliability across the SLPs' nasality ratings (intraclass correlation coefficient = .53). Intrajudge reliability was assessed as agreement within one scale value between the first and second ratings by the same SLP. Each of the 10 SLPs rated four randomly selected samples a second time. Of the 40 samples rerated (4 samples × 10 SLPs), 33 of the second ratings (82.5%) were within one scale value of the first rating, suggesting good intrarater reliability.
Statistical Analysis
Hierarchical cluster analysis was performed using SPSS (v.21) to identify naturally occurring clusters of children with similar speech profiles. All six speech measures (i.e., F2 range of diphthongs, proportion of bursts, proportion of closure interval voicing, proportion of deviant voice quality, articulation rate, and nasality rating) were included as clustering variables. Intelligibility was not included as a clustering variable, as the objective was to identify clusters of children with similar speech profiles, independent of severity. All independent variables were standardized before entering them into the cluster analysis, to ensure that scale differences did not result in unequal weighting of variables (Mooi & Sarstedt, 2011). Each variable was standardized by converting measurements to z scores based on the mean and standard deviation of the TD group, in order to characterize each child (in both the SMI group and the TD group) relative to the normal distribution of the TD children. The hierarchical cluster analysis used squared Euclidean distances as a measure of similarity and Ward's method (Ward, 1963) as a clustering algorithm. Although the goal was to examine clusters of children within the SMI group, all 40 children were included in the cluster analysis to ensure that the cluster solution also accurately separated children with SMI from the TD children. After a clustering solution was obtained, a series of Kruskal–Wallis tests were used to examine whether clusters differed from each other on each of the speech subsystem measures and intelligibility. Follow-up group comparisons were conducted using Mann–Whitney U tests. Because of the small number of children in each cluster, nonparametric tests were used to compare groups.
Results
Cluster Analysis
Hierarchical cluster analysis was used to identify naturally occurring clusters of children with similar speech profiles. Results of the cluster analysis are best visualized with a dendogram (see Figure 2), which illustrates how child speakers were linked together. This method begins by assuming each child is in a cluster alone (as indicated by individual lines for each child at the bottom of Figure 2) and then progressively merges children together based on their similarity on the included variables until all children are grouped together in one cluster (as indicated by the single line at the top of Figure 2). The number of clusters resulting from the analysis is defined by the researcher based on information in the dendogram, rather than by imposing an a priori prediction regarding the number of clusters. As this cluster analysis included all children in both the SMI group and the TD group, two levels of clustering solutions were defined: At the first level, the analysis was expected to separate children with dysarthria from the TD children, and at the second level, it was expected to separate subgroups of children with dysarthria.
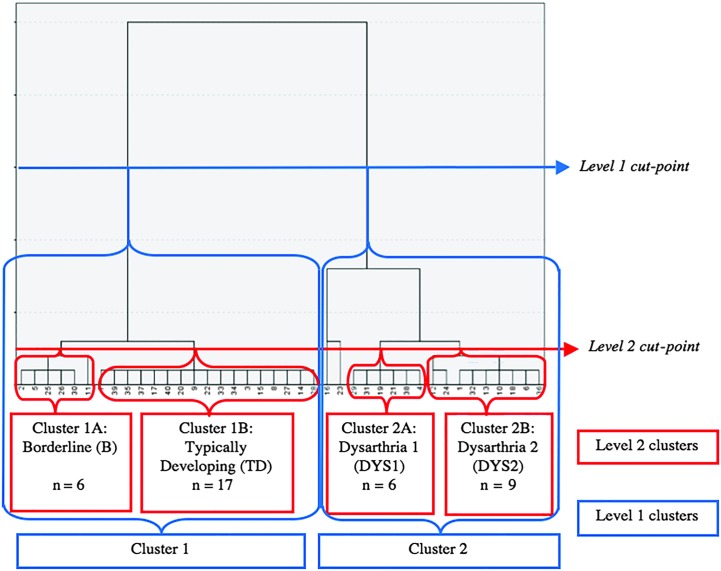
Figure 2.
Dendogram showing the progressive linking of children based on similarity in speech features.
At the first clustering level, indicated by the blue line on the dendogram in Figure 2, two clusters emerged: Cluster 1 contained all 20 TD children and three children with SMI, and Cluster 2 contained the remaining 17 of 20 children in the SMI group. At the second clustering level, indicated by the red line on the dendogram in Figure 2, two subclusters were identified within each of the Level 1 clusters, thus yielding a four-cluster solution. Within Cluster 1, one subcluster (Cluster 1B) contained 17 of the 20 TD children and will be referred to as the TD cluster. The second subcluster (Cluster 1A) was composed of the remaining three TD children and the three children with SMI misclassified at the first level of the cluster analysis and will be referred to as the borderline (B) cluster. Within Cluster 2, two subclusters of children with dysarthria were identified: Cluster 2A contained six children with SMI and will be referred to as Dysarthria Cluster 1 (DYS1), and Cluster 2B contained nine children with SMI and will be referred to as Dysarthria Cluster 2 (DYS2). Two children with SMI (CP05 and CP15) were not grouped with any cluster, nor were they grouped together; thus, they were considered outliers and excluded from subsequent group comparisons. These two children had the most severe dysarthria of the CP group, as indicated by their overall intelligibility levels (i.e., 9% and 31%), extremely slowed articulation rates (i.e., 2.1 and 1.7 syll/s), high proportions of deviant voice quality (24% and 56%), and elevated ratings of hypernasality (6.9 and 4.9 out of 7.0).
Cluster Profiles
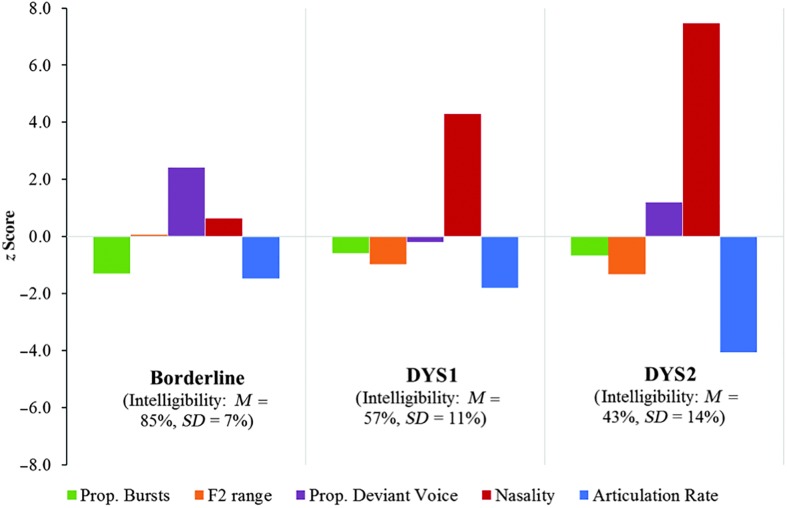
To better visualize the cluster profiles, Figure 3 illustrates how the borderline, DYS1, and DYS2 clusters compared with the TD children on each of the acoustic and perceptual speech measures. z Scores were used so that differences between clusters on all measures could be viewed on the same scale. Descriptive statistics on each of the six speech measures and intelligibility for each cluster are presented in Table 3. Language comprehension scores, Gross Motor Function Classification System levels, and anatomical involvement characteristics of the three dysarthria clusters are summarized in Table 4.
Figure 3.
Profiles of the borderline, Dysarthria 1 (DYS1), and Dysarthria 2 (DYS2) clusters on each of the acoustic and perceptual speech measures. z Scores are based on the mean and standard deviation of the typically developing children. Prop. = proportion of.
Table 3.
Descriptive statistics comparing the four clusters (i.e., typically developing [TD], borderline [B], Dysarthria 1 [DYS1], and Dysarthria 2 [DYS2]) on each speech measure and overall intelligibility.
| Speech measure | TD cluster (n = 17) |
B cluster (n = 6) |
DYS1 cluster (n = 6) |
DYS2 cluster (n = 9) |
|---|---|---|---|---|
| Mdn | Mdn | Mdn | Mdn | |
| Proportion of bursts produced | 0.94 | 0.72 | 0.86 | 0.83 |
| F2 range of diphthongs (Hz) | 1465 | 1521 | 1256 | 2.23 |
| Nasality rating | 1.60 | 1.90 | 3.40 | 4.8 |
| Proportion of deviant voice quality | 0.06 | 0.13 | 0.04 | 0.11 |
| Proportion of closure interval with voicing | 0.41 | 0.33 | 0.49 | 0.29 |
| Articulation rate (syll/s) | 3.24 | 3.01 | 2.92 | 2.29 |
| Overall intelligibility (%) | 91.59 | 86.92 | 58.22 | 38.62 |
Table 4.
Demographic characteristics of children with speech motor impairment in the three dysarthria (DYS) clusters.
| Child characteristic | Cluster |
|||
|---|---|---|---|---|
| Borderline (n = 3) | DYS1 (n = 6) | DYS2 (n = 9) | ||
| Sex (n) | M | 1 | 4 | 1 |
| F | 2 | 2 | 8 | |
| TACL SS | M (SD) | 90 (22) | 95 (8) | 92 (22) |
| GMFCS (n) | I | 2 | 4 | 1 |
| II | 0 | 0 | 2 | |
| III | 1 | 0 | 2 | |
| IV | 0 | 2 | 3 | |
| V | 0 | 0 | 1 | |
| Anatomic involvement (n) | Left hemiplegia | 1 | 1 | 0 |
| Right hemiplegia | 1 | 2 | 3 | |
| Diplegia | 0 | 1 | 3 | |
| Quadriplegia | 0 | 2 | 3 | |
| Unknown | 1 | 0 | 0 | |
| Overall intelligibility | M (SD) | 81.2 (8.3) | 57 (11.4) | 43.1 (13.6) |
Note. For the borderline cluster, only the three children from the group with speech motor impairment in this cluster are described. M = male; F = female; GMFCS = Gross Motor Function Classification System; TACL SS = Test for Auditory Comprehension of Language–Fourth Edition standard score.
A series of Kruskal–Wallis tests were conducted to test for significant differences between the four clusters on each of the acoustic and perceptual speech measures and overall intelligibility. Results showed statistically significant differences between clusters on the following measures: articulation rate (χ2 = 24.89, p < .001), proportion of bursts produced (χ2 = 13.36, p < .01), F2 range of diphthongs (χ2 = 13.33, p < .01), proportion of deviant voice quality (χ2 = 13.99, p < .01), nasality rating (χ2 = 27.65, p < .001), and overall intelligibility (χ2 = 29.04, p < .001). Proportion of closure interval voicing did not significantly differ among any of the clusters (χ2 = 2.90, p > .05).
Follow-up pairwise contrasts were conducted using Mann–Whitney U tests to assess differences between clusters for each of the speech variables with a significant Kruskal–Wallis omnibus test. To control for Type 1 errors, an α level of .05 was partitioned evenly across the six pairwise contrasts (i.e., TD vs. borderline, TD vs. DYS1, TD vs. DYS2, borderline vs. DYS1, borderline vs. DYS2, and DYS1 vs. DYS2) for each family of tests. Thus, a significance criteria of p < .008 was used for each contrast. Effect sizes were calculated for each pairwise contrast using the following formula: r = z/√N (Cohen, 1992).
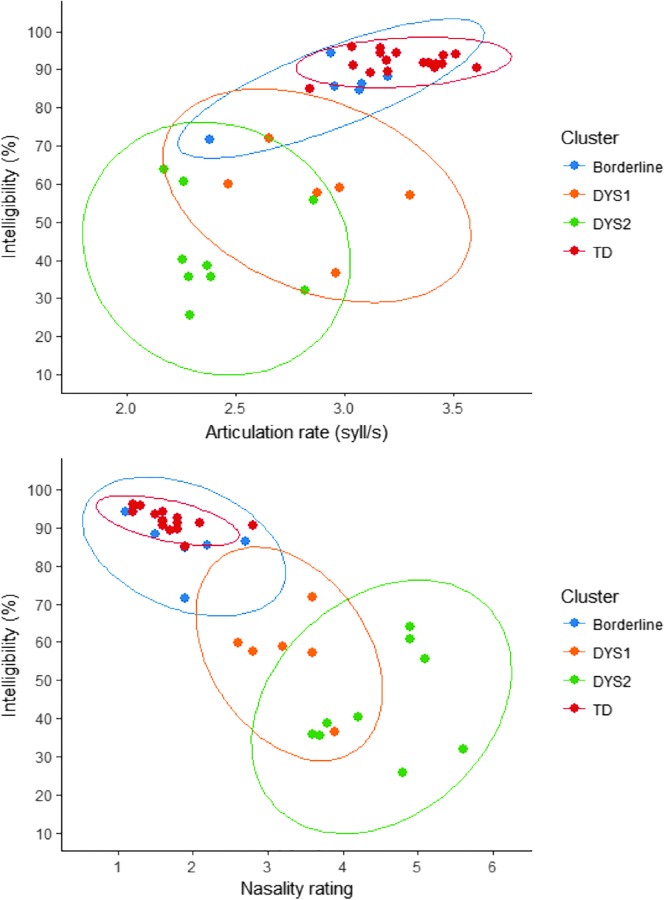
Results and effect sizes of pairwise contrasts are presented in Table 5. The following contrasts were significant: The borderline cluster had a significantly higher proportion of deviant voice quality than the TD cluster but did not significantly differ from the TD cluster on any of the other speech measures, including intelligibility. The DYS1 cluster had a significantly slower articulation rate than the TD cluster as well as significantly higher nasality ratings (indicating more severe hypernasality) and significantly lower intelligibility than the borderline and TD clusters. The DYS2 cluster had a significantly lower proportion of bursts and a smaller F2 range than the TD cluster, as well as a significantly slower articulation rate and higher nasality ratings than the other three clusters, and significantly lower intelligibility than the borderline and TD clusters. Importantly, the DYS1 and DYS2 clusters did not significantly differ in intelligibility, despite their significant differences in articulation rate and nasality rating. Scatter plots in Figure 4 show the distribution of individuals in each cluster in terms of articulation rate (see Figure 4a) and nasality rating (see Figure 4b) relative to intelligibility. Note that children in the DYS1 and DYS2 clusters largely overlap in intelligibility but differ in articulation rate and nasality rating.
Table 5.
Effect sizes (r) for Mann–Whitney U contrasts examining differences between the typically developing (TD), borderline, Dysarthria 1 (DYS1), and Dysarthria 2 (DYS2) clusters on the six speech measures and overall intelligibility.
| Speech measure | Effect sizes (r) for pairwise contrasts |
|||||
|---|---|---|---|---|---|---|
| TD vs. borderline | TD vs. DYS1 | TD vs. DYS2 | Borderline vs. DYS1 | Borderline vs. DYS2 | DYS1 vs. DYS2 | |
| Proportion of bursts produced | .40 | .27 | .51 * | .19 | .20 | .10 |
| F2 range of diphthongs (Hz) | .01 | .34 | .45 * | .40 | .41 | .07 |
| Nasality rating | .16 | .55 * | .65 * | .43 * | .50 * | .43 * |
| Proportion of deviant voice quality | .49 * | .04 | .36 | .46 * | .19 | .28 |
| Proportion of closure interval with voicing | .15 | .04 | .23 | .13 | .07 | .19 |
| Articulation rate (syll/s) | .40 | .43 * | .64 * | .08 | .45 * | .43 * |
| Overall intelligibility (%) | .39 | .56 * | .65 * | .43 * | .50 * | .26 |
Note. A large effect size is .5, a medium effect size is .3, and a small effect size is .1 (Cohen, 1992). Significant contrasts are indicated in bold and with an asterisk.
p ≤ .008.
Figure 4.
Scatter plots showing the relation between intelligibility and articulation rate (top panel) and intelligibility and nasality rating (bottom panel) for children classified in each of the four clusters. DYS1 = Dysarthria 1; DYS2 = Dysarthria 2; TD = typically developing; syll/sec = syllables per second.
Discussion
Results of this study revealed four naturally occurring speech profiles among the sample of 5-year-old children, including three clusters of children with SMI secondary to CP: a borderline cluster including three children who had the mildest dysarthria and two clusters of children with moderate to severe dysarthria, one characterized by a significantly slower articulation rate and more hypernasality (DYS2) than the other (DYS1). Despite their differences in articulation rate and nasality ratings, the DYS2 and DYS1 clusters did not significantly differ in intelligibility. Collectively, these findings suggest that at least three different subgroups of speakers can be identified among 5-year-old children with dysarthria due to CP and that children with similar intelligibility levels can exhibit different speech characteristics. Cluster characteristics and implications of these findings are discussed below.
Borderline Cluster
The borderline cluster contained three children in the SMI group with the mildest speech impairments, grouped with three of the TD children in the cluster analysis. The children with SMI classified into this borderline cluster had some of the highest intelligibility levels in the SMI group (ranging from 72% to 86%), although intelligibility was not included as a clustering variable. The three TD children included in the borderline cluster had the lowest intelligibility of the children in the TD group (ranging from 84% to 94%), and two of these children also had standard scores in the low average range on the Arizona Articulation Proficiency Scale (standard scores = 85 and 87), suggesting that the TD children in this cluster had speech skills in the lower end of the normal range for their age.
Children in the borderline cluster only significantly differed from the TD cluster in the amount of deviant voice quality in their sentence productions. This finding suggests that deviant voice quality may be an indicator of mild dysarthria in children with CP; however, the overlap between children with mild dysarthria and TD children in the borderline cluster suggests that deviant voice quality is not diagnostically specific. In addition, despite having the most deviant voice quality of all the clusters, children in the borderline cluster maintained high intelligibility levels. This suggests that deviant voice quality may not be a key contributor to intelligibility deficits in children with CP. Although voice quality disturbance is a common feature of dysarthria in children with CP (Workinger & Kent, 1991) and is associated with lower listener preference (Fox & Boliek, 2012), impairments in other speech dimensions may have a greater impact on intelligibility. This is consistent with previous studies that have suggested that respiratory, phonatory, and resonatory subsystem functions do not affect intelligibility as much as the articulatory subsystem (De Bodt, Hernandez-Diaz, & Van De Heyning, 2002; Lee et al., 2014).
The emergence of the borderline cluster containing children from both the SMI and TD groups suggests that there is an overlap in the range of normal variability among TD children and children with SMI on acoustic speech measures. A recent study by Hustad and colleagues found that intelligibility differentiated most children with dysarthria from TD children at 5 years old but that there was a “gray area” for children with intelligibility between 75% and 85% for whom classification was less accurate (Hustad, Oakes, & Allison, 2015). Results of this study were consistent with this Hustad et al. (2015), as overall intelligibility levels of children in the borderline cluster were largely in this range. In addition, these results expand upon findings of Hustad and colleagues by demonstrating that children with dysarthria in this borderline range also have acoustic characteristics that can be hard to differentiate from TD children with speech skills at the low end of the normal range. The range of normal variability in children is not well understood for many acoustic measures, although some evidence exists for a spectrum of motor speech skills among TD children (Redford, 2014; Vick et al., 2012). Results of this study underscore the need for studies with large samples of TD children to establish normative data and quantify sensitivity and specificity of different measures or combinations of measures to aid in the diagnosis of mild speech impairment in children.
DYS1 and DYS2 Clusters
The primary finding of this study was that two clusters of children with moderate to severe dysarthria were identified that had similar intelligibility levels but significantly differed in articulation rate and their degree of hypernasality. Children in the DYS2 cluster were rated as significantly more hypernasal and had significantly slower articulation rates than children in the DYS1 and borderline clusters. Children in the DYS1 cluster also had elevated nasality ratings but had articulation rates equivalent to children in the borderline cluster.
Although the DYS1 and DYS2 clusters differed in nasality ratings and articulation rate, their overall profiles across the six speech features appeared similar, except for the degree of impairment in different dimensions and a difference in the proportion of deviant voice quality, which was not statistically significant. This would seem to imply a difference in dysarthria severity between clusters; however, the DYS1 and DYS2 clusters did not significantly differ in intelligibility. There is a long-standing history of using intelligibility as an index of dysarthria severity (Kent et al., 1989; Y. Kim et al., 2011; Weismer & Laures, 2002; Weismer et al., 1992); thus, this finding suggests that overall dysarthria severity was equivalent between these two groups. Descriptively, the median intelligibility of children in the DYS2 cluster was lower than that of children in the DYS1 cluster, but there was a wide range of intelligibility scores among children in both clusters (DYS1 = 36%–71%, DYS2 = 25%–64%) spanning the moderate to severe range of intelligibility impairment. Although preliminary, these results suggest two possible interpretations. First, the DYS1 and DYS2 clusters may represent distinct speech motor subgroups among children with moderate–severe dysarthria secondary to CP (one characterized by a slow articulation rate and pronounced hypernasality and the other characterized by a relatively unimpaired articulation rate and milder hypernasality). Second, it is also possible that the DYS1 and DYS2 clusters reflect subgroups of children that primarily differ in severity of underlying SMI but that these severity differences were not reflected in intelligibility scores.
The first interpretation implies that the differences in articulation rate and nasality between the DYS2 and DYS1 clusters reflect different patterns of neuromuscular constraints that result in distinct speech profiles but have similar functional impacts on intelligibility. Neuromotor constraints have been shown to influence habitual articulation rate even in healthy adults (Tsao & Weismer, 1997) and children (Redford, 2014) with normal speech intelligibility. In this study, this interpretation would suggest that children in the DYS2 cluster have a pattern of underlying neuropathology that disproportionally constrains articulation rate and nasality relative to the neuromotor impairments of children in the DYS1 cluster. The nasality differences between clusters need to be interpreted with caution, however, as slow rate has been shown to influence perception of hypernasality in speakers with dysarthria (McHenry, 1999). Thus, it is possible that the higher nasality ratings of children in the DYS2 cluster may be partially related to their slow articulation rates. As the DYS2 and DYS1 clusters did not significantly differ on any of the other acoustic variables examined in this study, future analyses that capture additional aspects of the speech motor profiles used by these children (e.g., quantifying differences in physiologic measures of speech subsystems or kinematic aspects of speech movement) are needed to fully characterize and validate the existence of these clusters as having distinct speech motor profiles.
The second interpretation suggests that the DYS1 and DYS2 clusters do not have distinct profiles of speech features but rather that they differ in the severity of underlying speech motor involvement, despite their similar intelligibility levels. If true, this interpretation could suggest that articulation rate and nasality ratings did not strongly contribute to intelligibility in these children. Alternately, it may also suggest that factors other than severity of SMI influenced children's intelligibility. One possibility is that interactions between phonological development and SMI contributed to differences in speech characteristics for children in the DYS1 and DYS2 clusters but had similar resulting impacts on intelligibility. Children in both clusters are acquiring speech sounds in the context of an SMI. To our knowledge, no studies have investigated trajectories of speech sound acquisition in children with CP; however, dysarthria has a relatively greater impact on the ability of speakers with CP to produce more motorically complex, later-developing speech sounds compared with simpler speech sounds (H. Kim, Martin, Hasegawa-Johnson, & Perlman, 2010). Children with CP can also have delays in phonological development (Peeters et al., 2009) that may affect their production of speech sounds above and beyond the impact of dysarthria. In the current study, this interaction between speech motor involvement and phonological development may have had differential impacts on the speech characteristics of children in the DYS1 and DYS2 clusters but had similar effects on intelligibility.
This study did not include a measure of segmental accuracy because speakers with dysarthria often have extensive distortions and blurred boundaries between segments that are difficult to characterize even through narrow phonetic transcription. In addition, studies have shown that narrow transcription can be unreliable, even for children without dysarthria (Shriberg & Lof, 1991). Therefore, acoustic measures are generally preferred for characterizing speech features in dysarthria research. However, our findings highlight the need for measures of phonological development in studies of children with congenital dysarthria, as they are crucial to understanding the development of intelligibility in this population. Depending on the relative contributions of SMI and phonological skills to their intelligibility impairments, children with CP may be expected to follow different trajectories in intelligibility development and respond to different intervention strategies.
It is also possible that delays or impairments in language or cognitive skills contributed to the reduced articulation rate of children in the DYS2 cluster. Rate of articulatory movements has been shown to be affected by cognitive and linguistic factors in TD children (Nip & Green, 2013) and children with specific language impairment (Goffman & Smith, 1999). This interpretation is not supported by the present data, which showed virtually no relationship between language comprehension scores and articulation rate. However, it is possible that other aspects of language and cognition (e.g., expressive language abilities, processing speed, working memory) that were not measured in this study may contribute to the differences in articulation rate between the clusters. Future research examining the relationship of expressive language and cognitive measures to articulation rate in children with CP and dysarthria is important for beginning to understand the effect of these skills on children's speech motor performance.
Limitations and Future Directions
Hierarchical cluster analysis is a descriptive method designed to be exploratory in nature. As such, findings of this study are preliminary, and dysarthria clusters need to be replicated and validated in a larger sample of children. Although consistent with the sample size used in many studies involving special populations of children with SMI, having only 20 children in the SMI group limited our statistical power, as the number of children in each cluster was small. In addition, the two outliers in this study both had severe SMI, characterized by very low intelligibility and extreme values on several of the included speech measures. In a larger sample, it is possible that these children may indicate the presence of an additional cluster that was not identified in this study.
The acoustic and perceptual measures selected for this study yielded preliminary information about the characteristics of the three dysarthria clusters; however, they did not provide adequate information to fully characterize distinctions in the speech motor profiles of the groups. Additional research is needed to further examine speech motor differences between clusters and to determine how contributors to intelligibility may differ between the clusters. Future studies employing additional measures of articulatory precision and quantitative measures of other speech subsystems (e.g., objective measurement of hypernasality through nasalance, physiologic measures of respiration) may help to more fully characterize the speech motor patterns of clusters and contributors to intelligibility. In addition, measures of phonological development are needed in conjunction with motor speech measures to capture contributions of both speech motor and phonological skills to intelligibility in children with dysarthria. Additional expressive language and cognitive measures may also provide important information regarding how development in these domains impacts children's speech characteristics.
This study aimed to capture different speech patterns among children with dysarthria at 5 years old; however, this age group represents only one point in time, and it is crucial to consider children's speech characteristics as part of a dynamic, developing system. Speech motor skills develop nonlinearly throughout childhood and adolescence (Smith & Zelaznik, 2004; Vorperian & Kent, 2007), and thus children's speech motor profiles may shift with development. Longitudinal studies of speech development in children with dysarthria are needed to understand how speech patterns emerge and change over time within individuals.
Summary and Clinical Implications
Results of this study suggest that three different speech profiles can be identified among children with dysarthria secondary to CP, including two speech profiles of children with moderate to severe dysarthria that have similar effects on intelligibility. Although preliminary, this finding has important theoretical and clinical implications, because it suggests the potential for developing a dysarthria classification system for children that could be used to stratify children into meaningful subgroups for studying the development of speech motor skills and evaluating responses to intervention techniques. Further characterization and validation of subgroups are needed before a specific classification system can be proposed; however, the present findings provide a first step toward developing a pediatric dysarthria classification system based on differences in children's patterns of speech motor behaviors.
Acknowledgments
This study was funded by Grants R01DC009411 (awarded to Dr. Katherine Hustad) and 1F31DC013925-01 (awarded to Dr. Kristen Allison) from the National Institute on Deafness and Other Communication Disorders. Support was also provided by the Waisman Center core grant, P30HD03352, from the National Institute of Child Health and Human Development. We would like to thank Gary Weismer for his insight and advice on this project and Luke Annear for his assistance with data analysis. We would also like to thank the families and children who participated in this project.
Funding Statement
This study was funded by Grants R01DC009411 (awarded to Dr. Katherine Hustad) and 1F31DC013925-01 (awarded to Dr. Kristen Allison) from the National Institute on Deafness and Other Communication Disorders. Support was also provided by the Waisman Center core grant, P30HD03352, from the National Institute of Child Health and Human Development.
References
- Ackermann H., & Ziegler W. (1991). Articulatory deficits in Parkinsonian dysarthria: An acoustic analysis. Journal of Neurology, Neurosurgery, & Psychiatry, 54(12), 1093–1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allison K. M., Annear L., Policicchio M., & Hustad K. C. (2017). Range and precision of formant movement in pediatric dysarthria. Journal of Speech, Language, and Hearing Research, 60(7), 1864–1876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allison K. M., & Hustad K. C. (2014). Impact of sentence length and phonetic complexity on intelligibility in 5-year-old children with cerebral palsy. International Journal of Speech-Language Pathology, 16(4), 396–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allison K. M., & Hustad K. C. (2018). Acoustic predictors of pediatric dysarthria in cerebral palsy. Journal of Speech, Language, and Hearing Research, 61(3), 462–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ansel B. M., & Kent R. D. (1992). Acoustic–phonetic contrasts and intelligibility in the dysarthria associated with mixed cerebral palsy. Journal of Speech and Hearing Research, 35(2), 296–308. [DOI] [PubMed] [Google Scholar]
- Auzou P., Ozsancak C., Morris R. J., Jan M., Eustache F., & Hannequin D. (2000). Voice onset time in aphasia, apraxia of speech, and dysarthria: A review. Clinical Linguistics & Phonetics, 14(2), 131–150. [Google Scholar]
- Bax M., Goldstein M., Rosenbaum P., & Levinton A. (2005). Proposed definition and classification of cerebral palsy. Developmental Medicine & Child Neurology, 47(8), 571–576. [DOI] [PubMed] [Google Scholar]
- Bax M., Tydeman C., & Flodmark O. (2006). Clinical and MRI correlates of cerebral palsy: The European cerebral palsy study. Journal of the American Medical Association, 296(13), 1602–1608. [DOI] [PubMed] [Google Scholar]
- Boliek C. A., & Fox C. M. (2014). Individual and environmental contributions to treatment outcomes following a neuroplasticity-principled speech treatment (LSVT LOUD) in children with dysarthria secondary to cerebral palsy: A case study review. International Journal of Speech-Language Pathology, 16(4), 372–385. [DOI] [PubMed] [Google Scholar]
- Boliek C. A., & Fox C. (2016). Technology-enhanced maintenance practice following intensive voice treatment in children with cerebral palsy and dysarthria. Archives of Physical Medicine and Rehabilitation, 97(10), e138. [Google Scholar]
- Brancamp T. U., Lewis K. E., & Watterson T. (2010). The relationship between nasalance scores and nasality ratings obtained with equal appearing interval and direct magnitude estimation scaling methods. The Cleft Palate–Craniofacial Journal, 47(6), 631–637. [DOI] [PubMed] [Google Scholar]
- Byrne M. C. (1959). Speech and language development of athetoid and spastic children. Journal of Speech and Hearing Disorders, 24(3), 231–240. [DOI] [PubMed] [Google Scholar]
- Carrow-Woolfolk E. (2014). TACL-4: Test for Auditory Comprehension of Language–Fourth Edition. Austin, TX: Pro-Ed. [Google Scholar]
- Chen M. Y. (1995). Acoustic parameters of nasalized vowels in hearing-impaired and normal-hearing speakers. The Journal of the Acoustical Society of America, 98(5), 2443–2453. [DOI] [PubMed] [Google Scholar]
- Cohen J. (1992). Statistical power analysis. Current Directions in Psychological Science, 1(3), 98–101. [Google Scholar]
- Cornwell P. L., Murdoch B. E., Ward E. C., & Morgan A. (2003). Dysarthria and dysphagia as long-term sequelae in a child treated for posterior fossa tumour. Pediatric Rehabilitation, 6(2), 67–75. [DOI] [PubMed] [Google Scholar]
- Darley F. L., Aronson A. E., & Brown J. R. (1969). Clusters of deviant speech dimensions in the dysarthrias. Journal of Speech and Hearing Research, 12(3), 462–496. [DOI] [PubMed] [Google Scholar]
- De Bodt M. S., Hernandez-Diaz H. M., & Van De Heyning P. H. (2002). Intelligibility as a linear combination of dimensions in dysarthric speech. Journal of Communication Disorders, 35(3), 283–292. [DOI] [PubMed] [Google Scholar]
- Duffy J. R. (2013). Motor speech disorders—E-book: Substrates, differential diagnosis, and management. St. Louis, MO: Elsevier Health Sciences. [Google Scholar]
- DuHadway C. M., & Hustad K. C. (2012). Contributors to intelligibility in preschool-aged children with cerebral palsy. Journal of Medical Speech-Language Pathology, 20(4), 11. [PMC free article] [PubMed] [Google Scholar]
- Eliasson A. C., Krumlinde-Sundholm L., Rosblad B., Beckung E., Arner M., Ohrvall A. M., & Rosenbaum P. (2006). The Manual Ability Classification System (MACS) for children with cerebral palsy: Scale development and evidence of validity and reliability. Developmental Medicine & Child Neurology, 48, 549–554. [DOI] [PubMed] [Google Scholar]
- Fletcher A. R., McAuliffe M. J., Lansford K. L., Sinex D. G., & Liss J. M. (2017). Predicting intelligibility gains in individuals with dysarthria from baseline speech features. Journal of Speech, Language, and Hearing Research, 60(11), 3043–3057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox C. M., & Boliek C. A. (2012). Intensive voice treatment (LSVT LOUD) for children with spastic cerebral palsy and dysarthria. Journal of Speech, Language, and Hearing Research, 55(3), 930–945. [DOI] [PubMed] [Google Scholar]
- Fudala R. B. (2000). Arizona Articulation Proficiency Scale–Third Revision. Torrance, CA: Western Psychological Services. [Google Scholar]
- Goffman L., & Smith A. (1999). Development and phonetic differentiation of speech movement patterns. Journal of Experimental Psychology: Human Perception and Performance, 25(3), 649–660. [DOI] [PubMed] [Google Scholar]
- Hanna S. E., Bartlett D. J., Rivard L. M., & Russell D. J. (2008). Reference curves for the gross motor function measure: Percentiles for clinical description and tracking over time among children with cerebral palsy. Physical Therapy, 88, 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hidecker M. J. C., Paneth N., Rosenbaum P., Kent R. D., Lillie J., Eulenberg J. B., … Taylor K. (2011). Developing and validating the communication function classification system for individuals with cerebral palsy. Developmental Medicine & Child Neurology, 53, 704–710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins C. M., & Hodge M. M. (2002). Vowel area and intelligibility in children with and without dysarthria. Journal of Medical Speech-Language Pathology, 10(4), 271–277. [Google Scholar]
- Himmelman K., Beckung E., Hagberg G., & Uvebrant P. (2006). Gross and fine motor function and accompanying impairments in cerebral palsy. Developmental Medicine & Child Neurology, 48, 417–423. [DOI] [PubMed] [Google Scholar]
- Hodge M., & Daniels J. (2007). TOCS+ intelligibility measures. Edmonton, Canada: University of Alberta. [Google Scholar]
- Hodge M., Wellman L., Caruso A., & Strand E. (1999). Management of children with dysarthria. In Caruso A. & Strand E. (Eds.), Clinical management of motor speech disorders in children (pp. 209–280). New York, NY: Thieme. [Google Scholar]
- Hustad K. C., Allison K., McFadd E., & Riehle K. (2014). Speech and language development in 2-year-old children with cerebral palsy. Developmental Neurorehabilitation, 17(3), 167–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hustad K. C., Allison K. M., Sakash A., McFadd E., Broman A. T., & Rathouz P. J. (2016). Longitudinal development of communication in children with cerebral palsy between 24 and 53 months: Predicting speech outcomes. Developmental Neurorehabilitation, 20, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hustad K. C., Gorton K., & Lee J. (2010). Classification of speech and language profiles in 4-year-old children with cerebral palsy: A prospective preliminary study. Journal of Speech, Language, and Hearing Research, 53(6), 1496–1513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hustad K. C., Oakes A., & Allison K. (2015). Variability and diagnostic accuracy of speech intelligibility scores in children. Journal of Speech, Language, and Hearing Research, 58(6), 1695–1707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hustad K. C., Oakes A., McFadd E., & Allison K. M. (2016). Alignment of classification paradigms for communication abilities in children with cerebral palsy. Developmental Medicine & Child Neurology, 58(6), 597–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hustad K. C., Schueler B., Schultz L., & Duhadway C. (2012). Intelligibility of 4-year-old children with and without cerebral palsy. Journal of Speech, Language, and Hearing Research, 55(4), 1177–1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irwin O. C. (1955). Phonetic equipment of spastic and athetoid children. Journal of Speech and Hearing Disorders, 20(1), 54–57. [DOI] [PubMed] [Google Scholar]
- Kataoka R., Warren D. W., Zajac D. J., Mayo R., & Lutz R. W. (2001). The relationship between spectral characteristics and perceived hypernasality in children. The Journal of the Acoustical Society of America, 109(5), 2181–2189. [DOI] [PubMed] [Google Scholar]
- Kent R. D., Weismer G., Kent J. F., & Rosenbek J. C. (1989). Toward phonetic intelligibility testing in dysarthria. Journal of Speech and Hearing Disorders, 54(4), 482–499. [DOI] [PubMed] [Google Scholar]
- Kim H., Martin K., Hasegawa-Johnson M., & Perlman A. (2010). Frequency of consonant articulation errors in dysarthric speech. Clinical Linguistics & Phonetics, 24(10), 759–770. [DOI] [PubMed] [Google Scholar]
- Kim Y., Kent R. D., & Weismer G. (2011). An acoustic study of the relationships among neurologic disease, dysarthria type, and severity of dysarthria. Journal of Speech, Language, and Hearing Research, 54(2), 417–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koo T. K., & Li M. Y. (2016). A guideline of selecting and reporting intraclass correlation coefficients for reliability research. Journal of Chiropractic Medicine, 15(2), 155–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreiman J., & Gerratt B. R. (2000). Sources of listener disagreement in voice quality assessment. The Journal of the Acoustical Society of America, 108(4), 1867–1876. [DOI] [PubMed] [Google Scholar]
- Lansford K. L., Liss J. M., & Norton R. E. (2014). Free-classification of perceptually similar speakers with dysarthria. Journal of Speech, Language, and Hearing Research, 57(6), 2051–2064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J., & Hustad K. C. (2013). A preliminary investigation of longitudinal changes in speech production over 18 months in young children with cerebral palsy. Folia Phoniatrica et Logopaedica, 65, 32–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J., Hustad K. C., & Weismer G. (2014). Predicting speech intelligibility with a multiple speech subsystems approach in children with cerebral palsy. Journal of Speech, Language, and Hearing Research, 57(5), 1666–1678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy E. S., Ramig L. O., & Camarata S. M. (2012). The effects of two speech interventions on speech function in pediatric dysarthria. Journal of Medical Speech-Language Pathology, 20(4), 82–88. [Google Scholar]
- Lisker L. (1986). “Voicing” in English: A catalogue of acoustic features signaling /b/ versus /p/ in trochees. Language and Speech, 29(1), 3–11. [DOI] [PubMed] [Google Scholar]
- Liss J. M., White L., Mattys S. L., Lansford K., Lotto A. J., Spitzer S. M., & Caviness J. N. (2009). Quantifying speech rhythm abnormalities in the dysarthrias. Journal of Speech, Language, and Hearing Research, 52(5), 1334–1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu H. M., Tsao F. M., & Kuhl P. K. (2005). The effect of reduced vowel working space on speech intelligibility in Mandarin-speaking young adults with cerebral palsy. The Journal of the Acoustical Society of America, 117(6), 3879–3889. [DOI] [PubMed] [Google Scholar]
- Liu H. M., Tseng C.-H., & Tsao F. M. (2000). Perceptual and acoustic analysis of speech intelligibility in Mandarin-speaking young adults with cerebral palsy. Clinical Linguistics & Phonetics, 14(6), 447–464. [Google Scholar]
- McHenry M. A. (1999). Aerodynamic, acoustic, and perceptual measures of nasality following traumatic brain injury. Brain Injury, 13(4), 281–290. [DOI] [PubMed] [Google Scholar]
- Milenkovic P. (2002). TF32: University of Wisconsin-Madison. Retrieved from http://userpages.chorus.net/cspeech/TFpamph.pdf
- Miller N., Pennington L., Robson S., Roelant E., Steen N., & Lombardo E. (2013). Changes in voice quality after speech-language therapy intervention in older children with cerebral palsy. Folia Phoniatrica et Logopaedica, 65(4), 200–207. [DOI] [PubMed] [Google Scholar]
- Mooi E., & Sarstedt M. (2011). Cluster analysis: A concise guide to market research (pp. 237–284). Berlin, Germany: Springer. [Google Scholar]
- Morgan A. T., & Liegeois F. (2010). Re-thinking diagnostic classification of the dysarthrias: A developmental perspective. Folia Phoniatrica et Logopaedica, 62, 120–126. [DOI] [PubMed] [Google Scholar]
- Nip I. S. (2013). Kinematic characteristics of speaking rate in individuals with cerebral palsy: A preliminary study. Journal of Medical Speech-Language Pathology, 20(4), 88–94. [PMC free article] [PubMed] [Google Scholar]
- Nip I. S., & Green J. R. (2013). Increases in cognitive and linguistic processing primarily account for increases in speaking rate with age. Child Development, 84(4), 1324–1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nordberg A., Miniscalco C., & Lohmander A. (2014). Consonant production and overall speech characteristics in school-aged children with cerebral palsy and speech impairment. International Journal of Speech-Language Pathology, 16(4), 386–395. [DOI] [PubMed] [Google Scholar]
- Nordberg A., Miniscalco C., Lohmander A., & Himmelmann K. (2013). Speech problems affect more than one in two children with cerebral palsy: Swedish population-based study. Acta Paediatrica, 102(2), 161–166. [DOI] [PubMed] [Google Scholar]
- Ozsancak C., Auzou P., Jan M., & Hannequin D. (2001). Measurement of voice onset time in dysarthric patients: Methodological considerations. Folia Phoniatrica et Logopaedica, 53(1), 48–57. [DOI] [PubMed] [Google Scholar]
- Pakula A. T., Van Naarden Braun K., & Yeargin-Allsopp M. (2009). Cerebral palsy: Classification and epidemiology. Physical Medicine and Rehabilitation Clinics of North America, 20, 425–452. [DOI] [PubMed] [Google Scholar]
- Palisano R., Rosenbaum P., Bartlett D., & Livingston M. (2007). Gross motor function classification system expanded and revised (GMFCS-E & R). CanChild Center for Childhood Disability Research, McMaster University, Hamilton, Ontario, Canada. [DOI] [PubMed]
- Peeters M., Verhoeven L., de Moor J., & van Balkom H. (2009). Importance of speech production for phonological awareness and word decoding: The case of children with cerebral palsy. Research in Developmental Disabilities, 30(4), 712–726. [DOI] [PubMed] [Google Scholar]
- Pennington L., Miller N., Robson S., & Steen N. (2010). Intensive speech and language therapy for older children with cerebral palsy: A systems approach. Developmental Medicine & Child Neurology, 52(4), 337–344. [DOI] [PubMed] [Google Scholar]
- Platt L. J., Andrews G., & Howie P. M. (1980). Dysarthria of adult cerebral palsy: II. Phonemic analysis of articulation errors. Journal of Speech and Hearing Research, 23(1), 41–55. [DOI] [PubMed] [Google Scholar]
- Redford M. A. (2014). The perceived clarity of children's speech varies as a function of their default articulation rate. The Journal of the Acoustical Society of America, 135(5), 2952–2963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rice M. L., Smolik F., Perpich D., Thompson T., Rytting N., & Blossom M. (2010). Mean length of utterance levels in 6-month intervals for children 3 to 9 years with and without language impairments. Journal of Speech, Language, and Hearing Research, 53(2), 333–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen K. M., Goozée J. V., & Murdoch B. E. (2008). Examining the effects of multiple sclerosis on speech production: Does phonetic structure matter? Journal of Communication Disorders, 41(1), 49–69. [DOI] [PubMed] [Google Scholar]
- Rosenbaum P., Paneth N., Leviton A., Goldstein M., & Bax M. (2007). A report: The definition and classification of cerebral palsy. Developmental Medicine & Child Neurology, 49(s108), 8–14. [PubMed] [Google Scholar]
- Rosenbaum P. L., Palisano R. J., Bartlett D. J., Galuppi B. E., & Russell D. J. (2008). Development of the gross motor function classification system for cerebral palsy. Developmental Medicine & Child Neurology, 50, 249–253. [DOI] [PubMed] [Google Scholar]
- Rosenbaum P. L., Walter S. D., Hanna S. E., Palisano R. J., Russell D. J., Raina P., … Galuppi B. E. (2002). Prognosis for gross motor function in cerebral palsy: Creation of motor development curves. Journal of the American Medical Association, 288, 1357–1363. [DOI] [PubMed] [Google Scholar]
- Schölderle T., Staiger A., Lampe R., Strecker K., & Ziegler W. (2016). Dysarthria in adults with cerebral palsy: Clinical presentation and impacts on communication. Journal of Speech, Language, and Hearing Research, 59(2), 216–229. [DOI] [PubMed] [Google Scholar]
- Shriberg L. D., & Lof G. L. (1991). Reliability studies in broad and narrow phonetic transcription. Clinical Linguistics & Phonetics, 5(3), 225–279. [Google Scholar]
- Sigurdardottir S., & Vik T. (2011). Speech, expressive language, and verbal cognition of preschool children with cerebral palsy in Iceland. Developmental Medicine & Child Neurology, 53(1), 74–80. [DOI] [PubMed] [Google Scholar]
- Smith A., & Zelaznik H. N. (2004). Development of functional synergies for speech motor coordination in childhood and adolescence. Developmental Psychobiology, 45(1), 22–33. [DOI] [PubMed] [Google Scholar]
- Tsao Y. C., & Weismer G. (1997). Interspeaker variation in habitual speaking rate: Evidence for a neuromuscular component. Journal of Speech, Language, and Hearing Research, 40(4), 858–866. [DOI] [PubMed] [Google Scholar]
- van Mourik M., Catsman-Berrevoets C. E., Paquier P. F., Yousef-Bak E., & van Dongen H. R. (1997). Acquired childhood dysarthria: Review of its clinical presentation. Pediatric Neurology, 17(4), 299–307. [DOI] [PubMed] [Google Scholar]
- van Mourik M., Catsman-Berrevoets C. E., Yousef-Bak E., Paquier P. F., & van Dongen H. R. (1998). Dysarthria in children with cerebellar or brainstem tumors. Pediatric Neurology, 18(5), 411–414. [DOI] [PubMed] [Google Scholar]
- Vick J. C., Campbell T. F., Shriberg L. D., Green J. R., Abdi H., Rusiewicz H. L., … Moore C. A. (2012). Distinct developmental profiles in typical speech acquisition. Journal of Neurophysiology, 107, 2885–2900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vick J. C., Campbell T. F., Shriberg L. D., Green J. R., Truemper K., Rusiewiczf H. L., & Moore C. A. (2014). Data-driven subclassification of speech sound disorders in preschool children. Journal of Speech, Language, and Hearing Research, 57(6), 2033–2050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vorperian H. K., & Kent R. D. (2007). Vowel acoustic space development in children: A synthesis of acoustic and anatomic data. Journal of Speech, Language, and Hearing Research, 50(6), 1510–1545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward J. H., Jr. (1963). Hierarchical grouping to optimize an objective function. Journal of the American Statistical Association, 58(301), 236–244. [Google Scholar]
- Weismer G., & Laures J. S. (2002). Direct magnitude estimates of speech intelligibility in dysarthria: Effects of a chosen standard. Journal of Speech, Language, and Hearing Research, 45(3), 421–433. [DOI] [PubMed] [Google Scholar]
- Weismer G., Martin R., & Kent R. D. (1992). Acoustic and perceptual approaches to the study of intelligibility. In Kent R. D. (Ed.), Intelligibility in speech disorders: Theory, measurement and management (pp. 67–118). Amsterdam: John Benjamins Publishing Company. [Google Scholar]
- Wood E., & Rosenbaum P. (2000). The gross motor classification system for cerebral palsy a study of reliability and stability over time. Developmental Medicine & Child Neurology, 42, 292–296. [DOI] [PubMed] [Google Scholar]
- Workinger M. S., & Kent R. D. (1991). Perceptual analysis of the dysarthrias in children with athetoid and spastic cerebral palsy. In Moore C. A., Yorkston K. M., & Beukelman D. R. (Eds.), Dysarthria and apraxia of speech: Perspectives on management (pp. 109–126). Baltimore, MD: Brookes. [Google Scholar]
- Zimmerman I. L., Steiner V. G., & Pond R. E. (2005). Preschool Language Scale–Fourth Edition Screening Test. San Antonio, TX: The Psychological Corporation. [Google Scholar]