Abstract
Hospital-acquired pressure injury is a common preventable condition. Our hospital is a 144-bed governmental hospital in the Kingdom of Saudi Arabia that was found to have a 7.5% prevalence of hospital-acquired pressure injury in 2016. The aim of the improvement project was to reduce the prevalence of pressure injuries in our hospital from 7.5% to below 4% by the end of 2017. Our strategy for improvement was based on the Institute for Healthcare Improvement Model for Improvement. The change strategy was based on implementing an evidence-based risk assessment tool and a bundled evidence-based pressure injury prevention (PIP) intervention termed PIP bundle. After implementing the change package, we observed a reduction in the prevalence of pressure injuries by 84% (RR 0.16;95% CI 0.07 to 0.3; p value <0.0001) over a period of 12 weeks, in addition to an improvement in the compliance of pressure injury risk assessment and PIP interventions. The use of an evidenced-based bundled approach to prevent hospital-acquired pressure injuries has resulted in a significant reduction in the rate of pressure injuries. Improvement results were sustainable. In addition, our outcome measure exhibited minimal variability.
Keywords: pressure ulcer, bed Sore, prevention, hospital
Problem
Hospital-acquired pressure injury is a common yet preventable condition. A clinical audit conducted in our healthcare system in Saudi Arabia has revealed that there is variability in the prevalence of hospital-acquired pressure injury across hospitals within the same healthcare system. One of our healthcare organisations has been found to have a higher than average prevalence of hospital-acquired pressure injuries, averaging 7.5% in 2016. This figure is considered higher than the healthcare system benchmark of 3% and the international benchmark of 4%.
Our hospital is a 144-bed governmental hospital governed by the military healthcare system in the Kingdom of Saudi Arabia, located in the city of Al-Kharj which is located 77 km south of the capital city of Riyadh.
By mid-2017, it was decided by the hospital’s leadership to launch an improvement project aimed at reducing the prevalence of hospital-acquired pressure injuries to below 4% within 6 months.
Background
Pressure injuries are localised injury to the skin and underlying tissue, usually over a bony prominence as a result of pressure or pressure in combination with shear.1
Healthcare-acquired pressure injuries are a common occurrence ranging between 4.7% and 31%.2 Risk factors for developing a hospital-acquired pressure injury include older age, immobility, altered mental condition, urinary or faecal incontinence, hospitalisation for fracture, surgical intervention, reduced appetite, and nasogastric tube or intravenous nutrition.3
Research has shown that pressure injuries may be preventable. Numerous interventions have been studied with varying degree of efficacy. The strategy for preventing pressures injuries relies on two interdependent domains: pressure injury risk identification and pressure injury risk mitigation.
Numerous risk assessment tools are being used to assess patients’ risk for developing a pressure injury. These tools include Norton, Waterlow, Braden and the interRAI Pressure Injury Risk Scale. Current research does not seem to show that any given tool is superior to the others.4 The Braden and Norton risk assessment tools seem to be more accurate than nurses’ clinical judgement in predicting pressure injury risk.5
Interventions should address risk factors that were identified using the risk assessment and tailored to the patient’s individual needs. Interventions include pressure relief, specialised mattresses, dressing over bony prominences, monitoring devices, nutritional support and use of skin moisturisers. Table 1 summaries the evidence supporting each intervention.
Table 1.
Summary of evidence of PIP
| Intervention | Effect size | Comments |
| Pressure relief | RR 0.62 (95% CI 0.10 to 3.97, p value = 0.62)6 | Cochrane review showed limited evidence due to underpowered studies. RCT found no difference between 2, 3 or 4 hours repositioning7 |
| Specialised mattresses | (RR 0.40 95% CI 0.21 to 0.74)8 | Cochrane review showed high-quality evidence for the use of higher-specification foam mattresses or medical sheepskin |
| Dressing over bony prominences | RR 0.21 (95% CI 0.09 to 0.51; p value = 0.0006)9 | Cochrane review showed low-quality evidence with high or unclear risk of bias |
| Nutritional supports | RR 0.86 (95% CI 0.73 to 1.00; p value = 0.05)10 | Cochrane review showed low-quality evidence with high or unclear risk of bias |
| Use of skin moisturisers | RR 0.78 (95% CI 0.47 to 1.31; p value = 0.35)9 | Cochrane review showed low-quality evidence with high or unclear risk of bias |
PIP, pressure injury prevention; RCT, randomised controlled trial.
Measurement
We have selected the prevalence of pressure injuries (hospital-acquired) as our primary outcome measure. This outcome measures the total number of patients that have a hospital-acquired (nosocomial) category/stage 2 or greater pressure injury(s) on the day of the prevalence study. This outcome measure has been selected because it is required to be reported by our hospital’s governing body on a quarterly basis. The measure is based on the Joint Commission’s International Hospital Inpatient Quality Measures Nursing-Sensitive Care (I-NSC-2) indicator. The measurement frequency has been shifted from a quarterly basis during the run-up period to weekly basis to facilitate rapid improvement cycles.
To monitor the process, we decided to measure the compliance of bedside nurses in conducting and documenting the assessment and interventions for the prevention of pressure injuries. For assessment, we measured the proportion of patients who had a documented daily pressure injury risk assessment using the Norton tool. For interventions, we measured the proportion of at-risk patients who received the required interventions with a subgroup analysis on the compliance to each bundle element. Table 2 describes the measures we used in the study.
Table 2.
Project measures
| Indicator | Type | Description | Numerator | Denominator |
| Pressure injury prevalence (hospital-acquired) | Outcome | The proportion of patients that have hospital-acquired (nosocomial) category/stage II or greater pressure injury(s) on the day of the prevalence study | Patients that have at least one category/stage II or greater hospital-acquired pressure injury(s) on the day of the prevalence study | All patients surveyed for the study who are ≥18 years |
| Pressure injury risk assessment | Process | The proportion of patients that have a documented daily risk assessment using the Norton risk assessment tool | Patients that have a documented Norton risk assessment within 24 hours of admission | All patients surveyed for the study who are ≥18 years |
| PIP intervention bundle | Process | The proportion of patients that have a documented delivery of elements of the PIP bundle | Patients that have documented delivery of all three components of the PUP bundle | All patients that were found to be at risk using the Norton risk assessment tool |
PIP, pressure injury prevention.
Data collectors were trained and given standardised data collection tools. Data were collected on a daily basis and analysed on a weekly basis using control and run charts using QI Macros 2018 for excel.
The baseline for the prevalence of pressure injury (hospital-acquired) in our hospital was averaging at 7.5% for the 12 months before starting the project.
Daily pressure risk assessment using the Braden score was 72%. Turning of patients at risk for pressure injury was 63% for the same period.
Design
It was clear that a significant number of patients did not undergo sufficient risk assessment. Additionally, there was no standardised practice for delivering interventions to prevent pressure injuries in our hospital.
A team was formed that consisted of relevant stakeholders including a physician, nurses, the hospital wound care team, a quality improvement advisor and a project manager. The team met on a weekly basis on site and used remote video conferencing with the quality improvement advisor and the project manager.
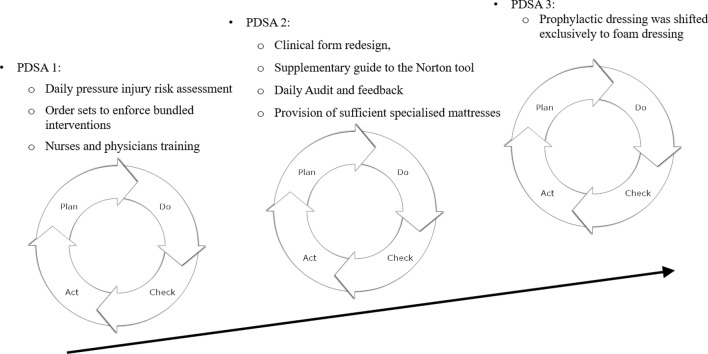
The change package that the team agreed on consisted of the following components (figure 1):
Figure 1.
Project PDSA cycle ramp. PDSA, Plan-Do-Study-Act.
Adoption of an evidence-based PIP guideline.
Daily risk assessment for all inpatients using the Norton tool, as it was easier to use by the bed-side nurses.
Standard order sets for bundled PIP interventions which include repositioning every 3 hours, use of specialised mattresses and prophylactic dressing of bony prominences.
Reinforcement of the role of the multidisciplinary wound care team.
Staff education and training.
Nutritional supports and the use of skin moisturises were omitted from the bundled interventions due to the lack of high-quality evidence.
Also, the interventions mentioned above needed to be integrated into the daily workflow of bed-side nurses to ensure significant compliance and avoid the additional burden on nurses. To achieve this, a lean methodology was used to develop a single page tool that included the risk assessment and PIP interventions.
Strategy
We based our strategy for improvement on the Institute for Healthcare Improvement Model for Improvement. The team decided to proceed to a large-scale test due to the following reasons; high degree of belief of the efficacy of the interventions based on the available evidence, predicted low cost of failure and strong organisational commitment.
The project team ran three ‘Plan -Do -Study-Act’ (PDSA) cycles (figure 1).
First PDSA cycle: our initial intervention aimed to adopt an evidence-based PIP guideline. The guideline was integrated into daily workflow of the bed-side nurses by implementing a daily risk assessment tool for all in-patients using the Norton tool. Standard order sets were implemented for bundled PIP interventions which include repositioning every 3 hours, use of specialised mattresses and prophylactic dressing of bony prominences.
Ten physicians and 235 nurses were educated and trained for 3 weeks on implementing the PIP risk assessment and intervention tool.
Second PDSA cycle: after 2 weeks of implementation, the project team observed a reduction in the prevalence of pressure injuries, but the wound care team noticed that bed-side nurses required further training using the risk assessment and intervention tool. Therefore, the tool was redesigned, a colour-coded legend was added, and a supplementary guide was provided to nurses. The role of the multidisciplinary wound care team was reinforced with daily audits and feedback.
Compliance with the uses of special mattresses was re-enforced. Bed-side nurses raised concern about the shortage of sufficient supply of specialised overlays and mattresses. Therefore, meetings with the hospital leadership resulted in the urgent procurement of sufficient mattresses.
Third PDSA cycle: the team noted that the compliance with the use of prophylactic dressing over a bony prominences was low throughout the first 4 weeks of the project. Further clarification from the wound care team revealed that bed-side nurses observed that frail elderly patients receiving hydrocolloid dressing were suffering from breakdown in skin integrity. Therefore, the prophylactic dressing was shifted exclusively to foam dressing and the tool was modified accordingly.
Results
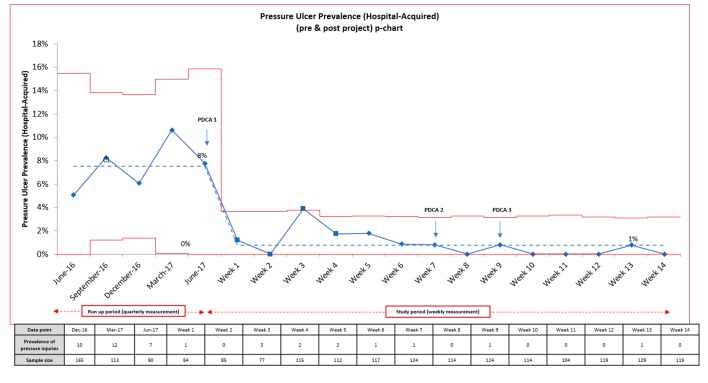
The prevalence of hospital-acquired pressures injuries started to decrease within the first week of implementing the first PDSA cycle and continued to decrease with subsequent PDSA cycles. By the end of week 14, the prevalence of hospital-acquired pressure injuries decreased from an average of 7.5% during the run-up period to an average of 1.2% (figure 2), with a relative risk reduction (RRR) of 84% (RR 0.16; 95% CI 0.07 to 0.3; p value <0.0001).
Figure 2.
P-chart of the prevalence of in-patient pressure injuries pre and post project.
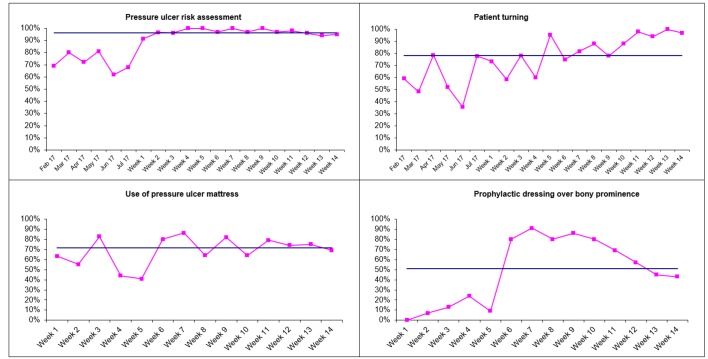
The compliance with patient assessment using the Norton risk assessment tool was high throughout the project averaging at 97%, and showing limited variability compared with 79% when using the Braden risk assessment scale in the preproject period (figure 3).
Figure 3.
Run chart for compliance with (A) pressure injury risk assessment, (B) patient turning, (C) use of pressure injury mattresses and (D) prophylactic dressing over a bony prominence.
The PIP bundle compliance rate was variable for different bundle elements. Patient turning had the highest compliance compared with the rest of the bundle elements (figure 3).
Lessons and limitations
The project aimed to reduce hospital-acquired pressure injury prevalence in admitted patients with a key focus on implementing an evidence-based pressure injury risk assessment and prevention bundle. A redesign of the current process was required to achieve this aim with a priority to develop a practical risk assessment tool that has an integrated intervention tracking tool. The tool was designed to be convenient and applicable to all inpatients with minimal user training.
A key lesson learnt during the project was the importance of iterative PDSA cycles, which helped to ensure that at each stage, the tool was reviewed and optimised.
The Norton scale risk assessment and intervention tool was reported by the bedside nurses to be convenient and easy to use/apply and had a better compliance rate as compared with the Braden scale tool. Daily risk assessment using Norton scale tool helped the bed-side nurses to apply the required evidence-based intervention promptly and minimised the occurrence of hospital-acquired pressure injuries.
In some clinical units, there was initial resistance by nurses in implementing the new pressure injury risk assessment tool. This resistance has been ameliorated by coaching and support by the wound care team, who have coordinated with a bed-side nurse by regularly visiting their clinical units and encouraging them to implement the PIP programme. In some cases, especially paediatric patients, the turning intervention was difficult to implement. In these cases, the bed-side nurses usually turned the baby during feeding and diaper changing.
The liberal use of dressing over a bony prominence in at-risk patients resulted in circumstances in which skin integrity has been compromised. This happened especially in frail elderly patients when using hydrocolloid dressing. This resulted in nurses being hesitant in applying the prophylactic dressing. The breakdown of skin integrity has been eluded when foam dressing was used exclusively as a prophylactic dressing.
The shortage of pressure injury mattresses has been an issue for the hospital, especially at the start of the project which affected the compliance of implementing the full PIP bundle. Hospitals need to review their required supply of high-specification mattresses before moving to full-scale implementation.
Our study has several limitations. We used a quasi-experimental quality improvement project design, which limits the generalisability of the study findings as interventions were not tested in a controlled environment and the outcome might have been affected by other confounders. In addition, this project tested the applicability and effect of implementing bundled evidence-based PIP interventions and adopting it on a hospital scale rather than testing the efficacy of PIP interventions, which have been proven using controlled experimental designs.
Finally, the outcome measure did not evaluate the prevalence of stage 1 pressure injuries.
Conclusion
The project team achieved the aim that they defined at the start of the project, which is to reduce the prevalence of hospital-acquired pressure injuries in our hospital.
Our primary outcome exhibits sustainability, as we have observed >10 data points meeting the designated target. Also, our outcome measure exhibits minimal variability.
Given the favourable results, the next step would be to scale-up the implementation of the PIP bundle to other military health organisations within the Kingdom of Saudi Arabia.
Acknowledgments
Mrs Amal Algosi
Footnotes
Patient consent for publication: Not required.
Contributors: YK-O and AR planned and conducted the study. N-N reviewed and edited the report and article.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Npuap. National pressure ulcer advisory panel support surface standards initiative terms and definitions related to support surfaces. Components 2007:1–10. [Google Scholar]
- 2. Kaltenthaler E, Whitfield MD, Walters SJ, et al. UK, USA and Canada: how do their pressure ulcer prevalence and incidence data compare? J Wound Care 2001;10:530–5. 10.12968/jowc.2001.10.1.26039 [DOI] [PubMed] [Google Scholar]
- 3. Perneger TV, Héliot C, Raë AC, et al. Hospital-acquired pressure ulcers: risk factors and use of preventive devices. Arch Intern Med 1998;158:1940–5. [DOI] [PubMed] [Google Scholar]
- 4. Schoonhoven L, Haalboom JR, Bousema MT, et al. Prospective cohort study of routine use of risk assessment scales for prediction of pressure ulcers. BMJ 2002;325:797 10.1136/bmj.325.7368.797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Pancorbo-Hidalgo PL, Garcia-Fernandez FP, Lopez-Medina IM, et al. Risk assessment scales for pressure ulcer prevention: a systematic review. J Adv Nurs 2006;54:94–110. 10.1111/j.1365-2648.2006.03794.x [DOI] [PubMed] [Google Scholar]
- 6. Gillespie BM, Chaboyer WP, McInnes E, et al. Repositioning for pressure ulcer prevention in adults. Cochrane Database Syst Rev 2014;4:CD009958 10.1002/14651858.CD009958.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Moore Z, Cowman S, Conroy RM. A randomised controlled clinical trial of repositioning, using the 30° tilt, for the prevention of pressure ulcers. J Clin Nurs 2011;20:2633–44. 10.1111/j.1365-2702.2011.03736.x [DOI] [PubMed] [Google Scholar]
- 8. McInnes E, Jammali-Blasi A, Bell-Syer SE, et al. Support surfaces for pressure ulcer prevention. Cochrane Database Syst Rev 2015:CD001735 10.1002/14651858.CD001735.pub5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Moore ZEH, Webster J. Cochrane Wounds Group. Dressings and topical agents for preventing pressure ulcers. Cochrane Database Syst Rev 2013;4 10.1002/14651858.CD009362.pub2 [DOI] [PubMed] [Google Scholar]
- 10. Langer G, Fink A. Nutritional interventions for preventing and treating pressure ulcers. Cochrane Database Syst Rev 2014(6):CD003216 Adolph, M., Eckart, A., Eckart, J. (1995). Fruct. doi 10.1002/14651858.CD003216.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]