Abstract
Background:
Daily cannabis use is increasing in the United States (US). Yet, it is not known whether daily cannabis use is disproportionately common, or whether it has increased differentially over time, by mental health status. This study estimated the prevalence of daily cannabis use among adults in the US with and without past-month serious psychological distress (SPD; measured by the Kessler Psychological Distress Scale (K6)) in 2016 and estimated trends in daily cannabis use by past 30-day SPD status from 2008 to 2016.
Methods:
Data were drawn from adults age 18 and older in the 2008–2016 National Survey on Drug Use and Health (combined total analytic sample n=356,413). Linear time trends of daily cannabis use, stratified by SPD status, were assessed using logistic regression models with continuous year as the predictor.
Results:
In 2016, past-month daily cannabis use was significantly more common among those with past-month SPD (8.07%), compared to those without past-month SPD (2.66%). Daily cannabis use increased significantly from 2008 to 2016 among those both with and without SPD although use among those with SPD was persistently higher than use among those without SPD over the time period studied.
Conclusions:
Daily cannabis use is significantly more common among persons with serious psychological distress and is increasing in this group, as well as among those without. Given this increase and the high prevalence of cannabis use among those with SPD, it may be important to consider potential consequences of this increased use for those with mental health vulnerabilities.
Keywords: Psychological Distress, Cannabis, NSDUH, Epidemiology
1. Introduction
Cannabis is the most widely used illicit drug in the world (WHO, 2017) and frequent use of cannabis is associated with a range of negative health and social consequences (e.g., Fergusson and Boden, 2008; Guttmannova et al., 2017; Suerken et al., 2016; Volkow et al., 2014). Approximately a quarter of cannabis users in the United States (US), over 8 million individuals, use cannabis every day or nearly every day (Compton et al., 2016; Hasin et al., 2015) which reflects significant increases in daily use over the past 10 years (SAMHSA, 2014). Along with the increase in daily cannabis use, there has been a concomitant increase in cannabis-related negative consequences (Azofeifa et al., 2016; Compton et al., 2016; Goodwin et al., 2018; Grucza et al., 2016; Hasin, 2018; Hasin et al., 2015; Mauro et al., 2018). These increases may be associated with the passage of more liberal legal restrictions on cannabis use (Hasin, 2018) as well as a decrease in the perception of risks associated with cannabis use (Azofeifa et al., 2016; Carliner et al., 2017; Compton et al., 2016; Johnston et al., 2016; Pacek et al., 2015). As the number of daily cannabis users increases, it is important to understand what groups are or might be disproportionally impacted by the negative consequences of daily use. For instance, persons who struggle with mental or behavioral health challenges may be more vulnerable to negative consequences of daily cannabis use (see Cousijn et al., 2018; National Academies of Sciences Engineering and Medicine, 2017 for reviews).
Serious psychological distress (SPD) is strongly associated with diagnoses of serious mental illness (Kessler et al., 2003; Kessler et al., 2010; Payton, 2009) and poorer mental health (Payton, 2009). SPD is characterized by feelings of nervousness, hopelessness, sadness, and/or worthlessness (Furukawa et al., 2003; Kessler et al., 2003; Kessler et al., 2010). SPD is reported by approximately 6 million US adults at any one time (Muhuri, 2014) and tends to become more persistent over time (Jokela et al., 2011). SPD is also associated with a large number of negative health indicators including higher prevalences of cigarette smoking, alcohol consumption, obesity, and other chronic health conditions; more emergency room visits; lower social support; greater cancer mortality; and greater overall mortality (Alhussain et al., 2017; Hamer et al., 2009; Lin et al., 2012; McGuire et al., 2009; Muhuri, 2014; Okoro et al., 2009; Pratt et al., 2007; Prochaska et al., 2012; Sung et al., 2011).
People using cannabis often report that they use cannabis in an attempt to decrease anxiety and other SPD-related symptoms and promote a feeling of well-being (Lee et al., 2009; Patrick et al., 2016; Patrick et al., 2011), but little is known about the relationship between SPD and daily cannabis use. A cross-sectional cohort study of Australian adults assessed in 1997 and 2007 found a significant relationship between psychological distress and cannabis dependence at both time points and a stronger relationship (i.e., greater odds ratio) between the two in 2007 than 1997 (Mathews et al., 2011). However, it is also possible that, based on the growing acceptance and popularity of cannabis use in the US, the strength of the relationship between SPD and cannabis use may weaken over time as cannabis use becomes more common among adults in the general population (i.e., as the base rate of cannabis use increases). In this scenario, the strength of the relationship between mental health problems (e.g., SPD) and cannabis use will be diminished. Additional US studies have suggested relations between symptoms and diagnoses of several mental disorders (e.g., anxiety and depression) and cannabis use (Borodovsky and Budney, 2018; Degenhardt et al., 2003; Dierker et al., 2018; Dutra et al., 2018; Kedzior and Laeber, 2014; Shi, 2014; Twomey, 2017). Further, a higher prevalence of serious mental illness (defined as one or more of the following: diagnoses of mood, anxiety, eating, substance use, or adjustment disorders; psychotic symptoms; psychotic symptoms; SPD) has recently been found in states that have legalized medical marijuana (Dutra et al., 2018). At present, however, the relationship between SPD and daily cannabis use and trends in the prevalence of daily cannabis use among people with SPD over time in the US remains unexplored. Little is also known about whether the relationship between SPD and cannabis use differs among demographic subgroups (e.g., by gender, race/ethnicity). Understanding the relationship between cannabis use and SPD could help inform the development of laws that regulate cannabis use in the current changing climate, identify groups who are at higher risk for daily cannabis use, understand whether daily cannabis use is increasing disproportionately among persons with SPD, and perhaps prepare prevention and intervention strategies for groups that may be in greatest need of prevention and/or clinical intervention in the wake of more liberal cannabis use regulations.
The goal of the current study was to investigate the prevalence of daily cannabis use among US adults with and without past-month SPD from 2008 to 2016. The first aim of the study was to examine the prevalence of daily cannabis use in 2016 among those with past-month SPD compared to those without SPD overall and by demographic subgroups. We hypothesized that the prevalence of daily cannabis use would be higher among those with SPD versus no SPD. Examining the relationship between SPD and cannabis use stratified by demographic subgroups was considered exploratory and no a priori hypotheses were specified. The second aim of the study was to examine trends in the prevalence of daily cannabis use among those with and without past-month SPD from 2008 to 2016. We hypothesized that cannabis use would increase more rapidly among those with SPD given that the prevalence is higher in this group and that there seem to be a greater number of reasons for use.
2. MATERIAL AND METHODS
2.1. Study Population
Data for the current study came from the National Survey on Drug Use and Health (NSDUH) public use data files for the years 2008 to 2016. The NSDUH is sponsored by the Substance Abuse and Mental Health Services Administration (SAMHSA) and was designed to provide estimates of drug use. The survey employs a 50-state design with an independent multistage area probability sample for each of the 50 states and the District of Columbia. Though the NSDUH was designed to provide estimates of drug use in US community-based individuals age 12 and older, the present analysis only included persons age 18 and older because respondents under 18 were not administered the measure of SPD. The total sample for 2016 was n=42,625 and the combined total sample from 2008 to 2016 was n=356,413.
Sampling weights for the NSDUH were computed to control for unit-level and individual-level non-response and were adjusted to ensure consistency with population estimates obtained from the US Census Bureau. In order to use the 9 years of combined data, a new weight was created upon aggregating the 9 datasets by dividing the original weight by the number of data sets combined. The analyses were based on de-identified publicly available data exempt from Institutional Review Board review. Additional details regarding the sampling methods and survey techniques for the NSDUH are found elsewhere (Center for Behavioral Health Statistics and Quality, 2016, 2017).
2.2. Measures
2.2.1. Daily Cannabis Use.
Respondents were classified as being daily cannabis users if they indicated using cannabis on at least 25 days out of the past 30 similar to other studies (e.g., (Budney et al., 2003; Pacek et al., 2015; Whitlow et al., 2004)).
2.2.2. Serious psychological distress (SPD).
SPD was assessed using the Kessler Psychological Distress Scale (K6) screening instrument (Furukawa et al., 2003; Kessler et al., 2003; Kessler et al., 2010) which is a 6-item scale that assesses the frequency of feeling nervous; hopeless; restless or fidgety; sad or depressed; that everything is an effort; or feeling down on oneself, no good, or worthless. Items were measured on a 5-point Likert scale (0= “none of the time”, 4 = “all of the time”) and responses were summed across the six items (range = 0–24). Scores of 13 or greater were classified as indicating SPD consistent with other research (Cook et al., 2014; Lawrence and Williams, 2016; Weissman et al., 2015, 2018). Respondents were then classified into one of two non-overlapping groups: 1) Past-month SPD – respondents who met criteria for SPD in the past month, and 2) No SPD – respondents who did not meet criteria for SPD in the past month.
2.2.3. Covariates.
Covariates for the analyses included gender (male, female), age (18–25, 26+), race/ethnicity (Non-Hispanic White, Non-Hispanic Black, Hispanic, Non-Hispanic Other), total annual family income (<$20,000, $20,000-$74,999, $75,000+), and heavy alcohol use (yes/no; i.e., drinking 5 or more drinks on the same occasion on each of 5 or more days in the past 30 days).
2.3. Statistical Analyses
Data were weighted to reflect the complex design of the NSDUH sample and were analyzed with STATA SE version 13.0 software. We used Taylor series estimation methods (STATA “svy” commands) to obtain proper standard error estimates for the cross-tabulations. First, we examined the combined prevalence of daily cannabis use by past-month SPD status in survey year 2016 by demographic characteristics. Next, we examined the prevalence of daily cannabis use among individuals with and without past-month SPD, across time from 2008 to 2016.
Linear time trends of daily cannabis use were assessed using logistic regression models with continuous year as the predictor. Multivariable logistic regression was then used to adjust for demographics (gender, age, race/ethnicity, income) and heavy alcohol use. Within these analyses, odds ratios indicate the slope of the increase/decrease (i.e., rapidity of change) in daily cannabis use between 2008 and 2016. Furthermore, models with year-by-SPD status interaction terms, and F-tests to test the significance of these interactions, were used to assess differential time trends (i.e., differences in the rapidity of change between individuals with SPD versus without).
3. Results
3.1. The Prevalence of SPD Among US Adults 2008 To 2016
The percentage of US adults who reported past-month SPD increased over the study period from 4.78% in 2008 to 5.55% in 2016. This linear trend was significant (aOR=1.02, 95% CI=1.01–1.03; adjusted for gender, age, race/ethnicity, total annual family income, and heavy alcohol use).
3.2. Daily Cannabis Use Among Those with And Without SPD And Associations with Demographic Characteristics
In 2016, the prevalence of daily cannabis use was significantly higher among persons with past-month SPD versus those without past-month SPD (see Table 1). After adjusting for demographic characteristics, persons with past-month SPD were more than twice as likely to report daily cannabis use compared to persons without SPD (aOR=2.38, 95% CI=1.89, 3.01). There were significant associations such that SPD was associated with a significantly greater odds of daily cannabis use than no SPD among all demographic subgroups (OR range: 1.44–3.14; i.e., gender, age, marital status, income, race/ethnicity) except for non-Hispanic Black respondents. When associations between SPD and daily cannabis use were compared among demographic subgroups, there was a significant interaction of SPD and daily cannabis use for Non-Hispanic White respondents compared to Non-Hispanic Black respondents. Specifically, the association between past-month SPD and daily cannabis use was stronger for Non-Hispanic White respondents (aOR=2.68, 95% CI=2.02, 3.55) than Non-Hispanic Black respondents (aOR=1.44, 95% CI=0.87, 2.40). Other demographic subgroups did not significantly differ in the strength of the relationship between SPD and daily cannabis use.
Table 1.
The association between past 30-day daily cannabis use and past-month SPD in 2016 by demographic characteristics (National Survey on Drug Use and Health, adults age 18 and older)
| Unadjusted prevalence of daily cannabis use | ||||
|---|---|---|---|---|
| No SPD | Past-month SPD | Past-month SPD vs. No SPD | ||
| Characteristic | wt% (SE) | wt% (SE) | aOR*(95% CI) | pint |
| Total sample | 2.66 (0.01) | 8.07 (0.76) | 2.38 (1.89, 3.01) | <0.001 |
| Gender | ||||
| Male | 3.76 (0.17) | 11.22 (1.43) | 2.15 (1.59, 2.92) | Ref |
| Female | 1.61 (0.09) | 5.86 (0.64) | 2.71 (2.08, 3.55) | 0.138 |
| Age (years) | ||||
| 18–25 | 6.34 (0.33) | 12.47 (1.21) | 2.15 (1.66, 2.77) | Ref |
| 26+ | 2.09 (0.01) | 6.37 (0.86) | 2.55 (1.85, 3.51) | 0.347 |
| Marital Status | ||||
| Married | 1.28 (0.09) | 4.07 (1.04) | 3.14 (1.82, 5.42) | Ref |
| Widowed/divorced/separated | 1.98 (0.22) | 5.02 (1.28) | 2.90 (1.53, 5.51) | 0.492 |
| Never married | 5.82 (0.27) | 11.94 (1.25) | 2.15 (1.65, 2.81) | 0.120 |
| Total Annual Family Income | ||||
| <$20,000 | 3.73 (0.21) | 7.82 (0.98) | 2.05 (1.52, 2.77) | Ref |
| $20,000-$74,999 | 2.94 (0.15) | 8.92 (1.10) | 2.61 (1.92, 3.56) | 0.193 |
| ≥$75,000 | 1.87 (0.13) | 6.54 (1.30) | 2.46 (1.53, 3.95) | 0.509 |
| Race/Ethnicity | ||||
| Non-Hispanic White | 2.62 (0.11) | 9.35 (1.01) | 2.68 (2.02, 3.55) | Ref |
| Non-Hispanic Black | 3.56 (0.28) | 5.96 (1.34) | 1.44 (0.87, 2.40) | 0.003 |
| Hispanic | 2.34 (0.23) | 5.61 (1.14) | 1.89 (1.15, 3.13) | 0.150 |
| Non-Hispanic Other | 2.25 (0.29) | 6.54 (1.61) | 2.50 (1.43, 4.37) | 0.621 |
Key: aOR, adjusted odds ratio; CI, confidence interval; Ref, reference; SE, standard error; SPD, serious psychological distress; wt %, weighted percentage
Adjusted for all other variables listed in the table
pint = p-value from t-test for product term beta=0; test for multiplicative interaction.
3.3. Trends in daily cannabis use among those with and without SPD from 2008 to 2016
There were significant increases in the prevalence of past-month daily cannabis use among persons with and without past-month SPD (see Figure 1 and Table 2). These increasing trends remained significant after adjusting for demographics and heavy alcohol use. There was no significant interaction of time and SPD status suggesting that the increase in daily cannabis use prevalence over time was similar among those with and without SPD. The prevalence of daily cannabis use among persons with past-month SPD was significantly higher than that among persons without SPD in every year of the study period (p’s<0.001).
Figure 1.
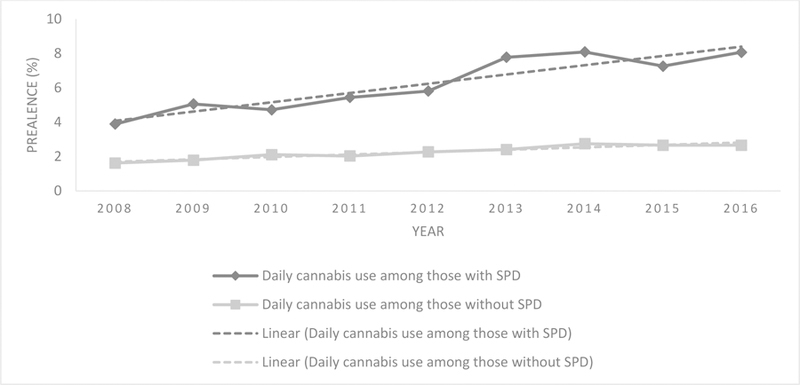
Prevalence of daily cannabis use for those with and without serious psychological distress (SPD) from 2008 to 2016
Table 2.
Prevalence of past 30-day daily cannabis use by SPD status (National Survey on Drug Use and Health, 2008–2016, adults age 18 and older)
| 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | Linear Trend | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| wt % | aOR* (95% CI); | p-value | aOR** (95% CI) | p-value | |||||||||
| Full analytic sample | 1.67 | 1.88 | 2.15 | 2.10 | 2.33 | 2.56 | 2.84 | 2.73 | 2.77 | 1.08 (1.06, 1.09) | <0.001 | 1.09 (1.08, 1.10) | <0.001 |
| No SPD | 1.62 | 1.79 | 2.11 | 2.03 | 2.27 | 2.41 | 2.75 | 2.66 | 2.66 | 1.08 (1.06, 1.09) | <0.001 | 1.09 (1.08, 1.11) | <0.001 |
| Past-month SPD | 3.89 | 5.06 | 4.72 | 5.44 | 5.81 | 7.78 | 8.09 | 7.26 | 8.07 | 1.10 (1.07, 1.12) | <0.001 | 1.11 (1.08, 1.15) | <0.001 |
| Differential time trend: year as continuous x past year SPD status | F(1,110)=1.55 | 0.216 | F(1,110)=1.42 | 0.235 | |||||||||
Key: aOR, adjusted odds ratio; CI, confidence interval; SPD, serious psychological distress; wt %, weighted percentage
Adjusted for gender, age, race/ethnicity, and total annual family income
Adjusted for gender, age, race/ethnicity, total annual family income, and heavy alcohol use (i.e., drinking 5 or more drinks on the same occasion on each of 5 or more days in the past 30 days)
4. Discussion
Since 2008, persons with SPD in the US have been significantly more likely to report using cannabis every day than persons without SPD. In 2008, the prevalence of cannabis use among persons with SPD was nearly two and half that among persons without SPD. In 2016, this proportion increased to over three times that among persons without SPD. Among persons with SPD, daily cannabis use more than doubled from 2008 to 2016 while, in contrast, the increase over that time period for persons without SPD was much less. While there was no significant difference in the trajectory of daily use between 2008 and 2016 among those with and without SPD, cannabis use remained persistently more common among those with SPD than those without SPD in every year from 2008 to 2016. Moreover, all demographic subgroups with SPD had significantly greater odds of daily cannabis use compared to those without SPD. These relationships among subgroups did not differ with the exception of a stronger relationship between SPD and daily cannabis use for non-Hispanic White respondents compared to non-Hispanic Black respondents. Non-Hispanic White respondents with SPD were over twice as likely to report daily cannabis use compared to non-Hispanic White respondents without SPD while non-Hispanic Black respondents with SPD were approximately 1.5 times more likely to use cannabis daily compared to non-Hispanic Black respondents without SPD.
The mechanisms underlying the relationship between SPD and high prevalences of daily cannabis use are not yet clear. One possibility is that individuals with SPD use cannabis for its negative reinforcement effects, e.g., to reduce or remove distress-related symptoms, anxiety, or stress. For example, cannabis is frequently used as a coping strategy for stress (see Hyman and Sinha, 2009 for a review). A study of teenagers and young adults in Australia found that those with higher SPD were less likely than those with lower SPD to report that it would be harmful for someone to use cannabis to relax (Yap et al., 2011). Further, persons who report lower levels of distress tolerance also report greater cannabis-related dependence symptoms and cannabis-related problems and these relationships are mediated by the report of using cannabis to cope with negative affect (Bujarski et al., 2012; Farris et al., 2016).
It is possible that the observed relationship is due to the daily use of cannabis for negative reinforcement effects related to SPD, but the reverse pathway may also be true. While cannabis use might ameliorate immediate symptoms of stress or distress, it might contribute to longer term persistence of symptomology. There is mounting evidence that use of cannabis, especially heavy cannabis use, is associated with the risk of incident psychotic symptoms (Borodovsky and Budney, 2018; Colizzi and Murray, 2018; Gage et al., 2016; Haney and Evins, 2016; Hanna et al., 2017; Marconi et al., 2016; Mustonen et al., 2018) as well as some evidence, though mixed, for a link between cannabis use and bipolar, depressive, anxiety, and posttraumatic stress disorder (Borodovsky and Budney, 2018; Haney and Evins, 2016; Hanna et al., 2017). There may also, of course, be a third variable or other risk factors that lead to concomitant cannabis use and SPD. More research is needed to understand biological and causal mechanisms for the association between SPD and cannabis use. This information is needed to inform intervention, and treatment efforts as well as policy development efforts as cultural norms around cannabis use become more liberal.
The link between cannabis and SPD has implications for treating SPD among people who use cannabis and for treating cannabis use among people with SPD. Abstinence from cannabis is associated with improvements in mental health symptoms such as anxiety and depression (Hser et al., 2017; Jacobus et al., 2017; Moitra et al., 2016) while continued cannabis use is associated with poorer mental health outcomes for depression, bipolar disorder, and schizoaffective disorder (Bahorik et al., 2018; Bahorik et al., 2017; Borodovsky and Budney, 2018; Kim et al., 2015; Kvitland et al., 2015; Zorrilla et al., 2015). On the other hand, in order to improve cannabis treatment outcomes, it may be useful to assess and target SPD jointly with cannabis use especially as SPD has been associated with a lower likelihood of successfully quitting cannabis (Shi, 2014). There are promising pilot data suggesting that interventions can have an impact on SPD or cannabis use by persons with SPD. For example, participants with SPD and either cannabis or alcohol use who received a motivational interviewing intervention reported reduced psychological distress, alcohol use, and cannabis use compared to a control group (Hides et al., 2013). In another study, an internet-based intervention targeting cannabis and alcohol use among adolescents reduced SPD compared to a control group (Newton et al., 2014). More research is needed to understand the potential impact of interventions on cannabis and SPD consequences and outcomes.
Of note, the prevalence of daily cannabis use was significantly higher among persons with SPD compared to persons without SPD in nearly all demographic subgroups suggesting that all groups (e.g., all genders, all ages) should be targeted to address SPD and/or cannabis use among those with SPD. We found one significant difference in the relationship of SPD and daily cannabis use among demographic subgroups: a stronger relationship between SPD and daily cannabis use was observed among non-Hispanic White persons than among non-Hispanic Black persons. In fact, non-Hispanic Black respondents were the only demographic subgroup for which the prevalence of daily cannabis use did not significantly differ among persons with and without SPD. While the prevalence of daily cannabis use among non-Hispanic Black respondents with SPD was similar to Hispanic and non-Hispanic other respondents with SPD, and lower than non-Hispanic White respondents with SPD, the prevalence of daily cannabis use was higher among non-Hispanic Black respondents without SPD compared to non-Hispanic White, Hispanic, and non-Hispanic other respondents without SPD. Non-Hispanic Black persons report higher prevalences of cannabis use and CUDs and lower prevalences of SPD than non-Hispanic White persons (Pacek et al., 2015; Weissman et al., 2015; Wu et al., 2014; Wu et al., 2016). Of note, while non-Hispanic Black persons report a higher prevalence of cannabis use, more non-Hispanic Black persons than non-Hispanic White persons who use cannabis report that cannabis use is risky (Pacek et al., 2015). The current study was the first to examine relationships between daily cannabis use and SPD by race/ethnicity. Future research is needed to expand our knowledge of racial/ethnic differences in the relationship between cannabis use and SPD, including correlates of and mechanisms underlying the relationship. For example, perceived racial discrimination and racism is associated with a range of poorer health outcomes (Paradies et al., 2015; Simons et al., 2018; Williams and Mohammed, 2009) and drug use (Carliner et al., 2016; Clark et al., 2015; Gibbons et al., 2004) for Black individuals. It is possible that experiences or variables related to drug use that are shared by Black individuals with and without SPD (e.g., discrimination) would decrease the relationship between SPD and daily cannabis use for this demographic subgroup. A better understanding racial/ethnic differences in SPD and cannabis use would also provide information needed to determine whether some racial/ethnic subgroups need additional or tailored clinical efforts to reduce the negative consequences of both SPD and daily cannabis use.
A number of limitations must be noted. The analytic sample included US adults ages 18 and older and future research should examine the relationship between cannabis use and SPD for other samples (e.g., adolescents, persons outside of the US). SPD and cannabis use were determined through self-report which may be impacted by a number of variables including underreporting (especially of illegal behaviors such as cannabis use), errors in memory, or biases in reporting. This study used annual cross-sectional data from representative samples of the US adult population. While the multiple years of data allowed us to examine trends in use, we could not follow individual trajectories in SPD or cannabis use. Studies with longitudinal data would be needed to examine changes in individuals over time. This study examined daily cannabis users and it may be useful for future studies, with more detailed information about cannabis use patterns, to examine the relationship of SPD and dimensions of daily cannabis use such as comparing frequency of use per day (e.g., once a day versus multiple times a day). While this study was not able to examine the relationships of SPD and cannabis use at a state level, it would be useful for future research to investigate the relationship of SPD and cannabis use among US states with and without cannabis-related laws and to examine changes in the relationship of SPD and cannabis use over time within states that adopt or make changes to cannabis-related laws.
4.1. Conclusions
Cannabis use is increasing over time and persons with SPD are significantly more likely to use cannabis every day than persons without SPD. Given the rapid legalization of medicinal and recreational use of cannabis in the US and the liberalization of social norms surrounding cannabis use, more research is needed to understand the impact of these changes on vulnerable groups such as those with mental and behavioral health problems.
Highlights.
We examined daily cannabis use by serious psychological distress (SPD).
From 2008 to 2016, daily cannabis use increased for adults with and without SPD.
Persons with SPD reported higher daily cannabis prevalences each study year.
In 2016, daily cannabis use for SPD was about three times higher than no SPD.
Acknowledgments
Role of Funding Source
Funding for this study was provided by the National Institutes of Health (NIH) grants R01-DA20892 to Goodwin and K01-DA043413 to Pacek. The NIH had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest
No conflict declared.
References
- Alhussain K, Meraya AM, Sambamoorthi U, 2017. Serious psychological distress and emergency room use among adults with multimorbidity in the United States. Psychiatry J 2017, 8565186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azofeifa A, Mattson ME, Schauer G, McAfee T, Grant A, Lyerla R, 2016. National estimates of marijuana use and related indicators — National Survey on Drug Use and Health, United States, 2002–2014. MMWR. Surveill. Summ 65, 1–25. [DOI] [PubMed] [Google Scholar]
- Bahorik AL, Campbell CI, Sterling SA, Leibowitz A, Travis A, Weisner CM, Satre DD, 2018. Adverse impact of marijuana use on clinical outcomes among psychiatry patients with depression and alcohol use disorder. Psychiatry Res 259, 316–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bahorik AL, Leibowitz A, Sterling SA, Travis A, Weisner C, Satre DD, 2017. Patterns of marijuana use among psychiatry patients with depression and its impact on recovery. J. Affect. Disord 213, 168–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borodovsky JT, Budney AJ, 2018. Cannabis regulatory science: risk-benefit considerations for mental disorders. Int. Rev. Psychiatry 30, 183–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Budney AJ, Moore BA, Vandrey RG, Hughes JR, 2003. The time course and significance of cannabis withdrawal. J. Abnorm. Psychol 112, 393–402. [DOI] [PubMed] [Google Scholar]
- Bujarski SJ, Norberg MM, Copeland J, 2012. The association between distress tolerance and cannabis use-related problems: the mediating and moderating roles of coping motives and gender. Addict. Behav 37, 1181–1184. [DOI] [PubMed] [Google Scholar]
- Carliner H, Brown QL, Sarvet AL, Hasin DS, 2017. Cannabis use, attitudes, and legal status in the U.S.: A review. Prev. Med 104, 13–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carliner H, Delker E, Fink DS, Keyes KM, Hasin DS, 2016. Racial discrimination, socioeconomic position, and illicit drug use among US Blacks. Soc. Psychiatry Psychiatr. Epidemiol 51, 551–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality, 2016. 2015 National Survey on Drug Use and Health Public Use File Codebook Substance Abuse and Mental Health Services Administration, Rockville, MD: https://samhda.s3-us-gov-west-1.amazonaws.com/s3fs-public/field-uploads-protected/studies/NSDUH-2015/NSDUH-2015-datasets/NSDUH-2015-DS0001/NSDUH-2015-DS0001-info/NSDUH-2015-DS0001-info-codebook.pdf [Google Scholar]
- Center for Behavioral Health Statistics and Quality, 2017. 2016 National Survey on Drug Use and Health Public Use File Codebook Rockville, MD, Substance Abuse and Mental Health Services Administration, Rockville, MD: http://samhda.s3-us-gov-west-1.amazonaws.com/s3fs-public/field-uploads-protected/studies/NSDUH-2016/NSDUH-2016-datasets/NSDUH-2016-DS0001/NSDUH-2016-DS0001-info/NSDUH-2016-DS0001-info-codebook.pdf [Google Scholar]
- Clark TT, Salas-Wright CP, Vaughn MG, Whitfield KE, 2015. Everyday discrimination and mood and substance use disorders: A latent profile analysis with African Americans and Caribbean Blacks. Addict. Behav 40, 119–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colizzi M, Murray R, 2018. Cannabis and psychosis: what do we know and what should we do? Br. J. Psychiatry 212, 195–196. [DOI] [PubMed] [Google Scholar]
- Compton WM, Han B, Jones CM, Blanco C, Hughes A, 2016. Marijuana use and use disorders in adults in the USA, 2002–14: analysis of annual cross-sectional surveys. Lancet Psychiatry 3, 954–964. [DOI] [PubMed] [Google Scholar]
- Cook BL, Wayne GF, Kafali EN, Liu Z, Shu C, Flores M, 2014. Trends in smoking among adults with mental illness and association between mental health treatment and smoking cessation. JAMA 311, 172–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cousijn J, Nunez AE, Filbey FM, 2018. Time to acknowledge the mixed effects of cannabis on health: a summary and critical review of the NASEM 2017 report on the health effects of cannabis and cannabinoids. Addiction 113, 958–966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degenhardt L, Hall W, Lynskey M, 2003. Exploring the association between cannabis use and depression. Addiction 98, 1493–1504. [DOI] [PubMed] [Google Scholar]
- Dierker L, Selya A, Lanza S, Li R, Rose J, 2018. Depression and marijuana use disorder symptoms among current marijuana users. Addict. Behav 76, 161–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutra LM, Parish WJ, Gourdet CK, Wylie SA, Wiley JL, 2018. Medical cannabis legalization and state-level prevalence of serious mental illness in the National Survey on Drug Use and Health (NSDUH) 2008–2015. Int. Rev. Psychiatry 30, 1–13. [DOI] [PubMed] [Google Scholar]
- Farris SG, Metrik J, Bonn-Miller MO, Kahler CW, Zvolensky MJ, 2016. Anxiety sensitivity and distress intolerance as predictors of cannabis dependence symptoms, problems, and craving: the mediating role of coping motives. J. Stud. Alcohol Drugs 77, 889–897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fergusson DM, Boden JM, 2008. Cannabis use and later life outcomes. Addiction 103, 969–976. [DOI] [PubMed] [Google Scholar]
- Furukawa TA, Kessler RC, Slade T, Andrews G, 2003. The performance of the K6 and K10 screening scales for psychological distress in the Australian National Survey of Mental Health and Well-Being. Psychol. Med 33 357–362. [DOI] [PubMed] [Google Scholar]
- Gage SH, Hickman M, Zammit S, 2016. Association between cannabis and psychosis: epidemiologic evidence. Biol. Psychiatry 79, 549–556. [DOI] [PubMed] [Google Scholar]
- Gibbons FX, Gerrard M, Cleveland MJ, Wills TA, Brody G, 2004. Perceived discrimination and substance use in African American parents and their children: A panel study. J. Pers. Soc. Psychol 86, 517–529. [DOI] [PubMed] [Google Scholar]
- Goodwin RD, Pacek LR, Copeland J, Moeller SJ, Dierker L, Weinberger A, Gbedemah M, Zvolensky MJ, Wall MM, Hasin DS, 2018. Trends in daily cannabis use among cigarette smokers: United States, 2002–2014. Am. J. Public Health 108, 137–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grucza RA, Agrawal A, Krauss MJ, Cavazos-Rehg PA, Bierut LJ, 2016. Recent trends in the prevalence of marijuana use and associated disorders in the United States. JAMA. Psychiatry 73, 300–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guttmannova K, Kosterman R, White HR, Bailey JA, Lee JO, Epstein M, Jones TM, Hawkins JD, 2017. The associations bewteen regular marijuana use and adult mental health outcomes. Drug Alcohol Depend 179, 109–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamer M, Chida Y, Molloy GJ, 2009. Psychological distress and cancer mortality. J. Psychosom. Res 66, 255–258. [DOI] [PubMed] [Google Scholar]
- Haney M, Evins AE, 2016. Does cannabis cause, exacerbate or ameliorate psychiatric disorders? An oversimplified debate discussed. Neuropsychopharmacology 41, 393–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanna RC, Perez JM, Ghose S, 2017. Cannabis and development of dual diagnoses: a literature review. Am. J. Drug Alcohol Abuse 43, 442–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, 2018. US epidemiology of cannabis use and associated problems. Neuropsychopharmacology 43, 195–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Saha TD, Kerridge BT, Goldstein RB, Chou SP, Zhang H, Jung J, Pickering RP, Ruan WJ, Smith SM, Huang B, Grant BF, 2015. Prevalence of marijuana use disorders in the United States between 2001–2002 and 2012–2013. JAMA Psychiatry 72, 1235–1242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hides L, Carroll S, Scott R, Cotton S, Baker A, Lubman DI, 2013. Quik fix: a randomized controlled trial of an enhanced brief motivational interviewing intervention for alcohol/cannabis and psychological distress in young people. Psychother. Psychosom 82, 122–124. [DOI] [PubMed] [Google Scholar]
- Hser YI, Mooney LJ, Huang D, Zhu Y, Tomko RL, McClure E, Chou CP, Gray KM, 2017. Reductions in cannabis use are associated with improvements in anxiety, depression, and sleep quality, but not quality of life. J. Subst. Abuse Treat 81, 53–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyman SM, Sinha R, 2009. Stress-related factors in cannabis use and misuse: implications for prevention and treatment. J. Subst. Abuse Treat 36, 400–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobus J, Squeglia LM, Escobar S, McKenna BM, Hernandez MM, Bagot KS, Taylor CT, Huestis MA, 2017. Changes in marijuana use symptoms and emotional functioning over 28-days of monitored abstinence in adolescent marijuana users. Psychopharmacology (Berl) 234, 3431–3442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Miech RA, Bachman JG, Schulenberg JE, 2016. Monitoring the Future national survey results on drug use, 1975–2015: Overview, key findings on adolescent drug use Institute for Social Research, The University of Michigan, Ann Arbor, Michigan: http://www.monitoringthefuture.org/pubs/monographs/mtf-overview2015.pdf [Google Scholar]
- Jokela M, Singh-Manoux A, Shipley MJ, Ferrie JE, Gimeno D, Akbaraly TN, Head J, Elovainio M, Marmot MG, Kivimaki M, 2011. Natural course of recurrent psychological distress in adulthood. J. Affect. Disord 130, 454–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kedzior KK, Laeber LT, 2014. A positive association between anxiety disorders and cannabis use or cannabis use disorders in the general population--a meta-analysis of 31 studies. BMC Psychiatry 14, 136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, Howes MJ, Normand S-LT, Manderscheid RW, Walters EE, Zaslavsky AM, 2003. Screening for serious mental illness in the general population. Arch. Gen. Psychiatry 60, 184–189. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Green JG, Gruber MJ, Sampson NA, Bromet E, Cuitan M, Furukawa TA, Gureje O, Hinkov H, Hu CY, Lara C, Lee S, Mneimneh Z, Myer L, Oakley-Browne M, Posada-Villa J, Sagar R, Viana MC, Zaslavsky AM, 2010. Screening for serious mental illness in the general population with the K6 screening scale: results from the WHO World Mental Health (WMH) survey initiative. Int. J. Methods Psychiatr. Res 19 Suppl 1, 4–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim SW, Dodd S, Berk L, Kulkarni J, de Castella A, Fitzgerald PB, Kim JM, Yoon JS, Berk M, 2015. Impact of cannabis use on long-term remission in bipolar I and schizoaffective disorder. Psychiatry Investig 12, 349–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kvitland LR, Melle I, Aminoff SR, Demmo C, Lagerberg TV, Andreassen OA, Ringen PA, 2015. Continued cannabis use at one year follow up is associated with elevated mood and lower global functioning in bipolar I disorder. BMC Psychiatry 15, 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence D, Williams JM, 2016. Trends in smoking rates by level of psychological distress-time series analysis of US National Health Interview Survey data 1997–2014. Nicotine Tob. Res 18, 1463–1470. [DOI] [PubMed] [Google Scholar]
- Lee CM, Neighbors C, Hendershot CS, Grossbard JR, 2009. Development and preliminary validation of a comprehensive marijuana motives questionnaire. J. Stud. Alcohol Drugs 70, 279–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin MT, Burgess JF Jr., Carey K, 2012. The association between serious psychological distress and emergency department utilization among young adults in the USA. Soc. Psychiatry Psychiatr. Epidemiol 47, 939–947. [DOI] [PubMed] [Google Scholar]
- Marconi A, Di Forti M, Lewis CM, Murray RM, Vassos E, 2016. Meta-analysis of the association between the level of cannabis use and risk of psychosis. Schizophr. Bull 42, 1262–1269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathews RR, Hall WD, Gartner CE, 2011. Depression and psychological distress in tobacco smokers and people with cannabis dependence in the National Survey of Mental Health and Wellbeing. Med. J. Aust 195, S12–S15. [DOI] [PubMed] [Google Scholar]
- Mauro PM, Carliner H, Brown QL, Hasin DS, Shmulewitz D, Rahim-Juwel R, Sarvet AL, Wall MM, Martins SS, 2018. Age differences in daily and nondaily cannabis use in the United States, 2002–2014. J. Stud. Alcohol Drugs 79, 423–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuire LC, Strine TW, Vachirasudlekha S, Anderson LA, Berry JT, Mokdad AH, 2009. Modifiable characteristics of a healthy lifestyle and chronic health conditions in older adults with or without serious psychological distress, 2007 Behavioral Risk Factor Surveillance System. Int. J. Public Health 54 Suppl 1, 84–93. [DOI] [PubMed] [Google Scholar]
- Moitra E, Anderson BJ, Stein MD, 2016. Reductions in cannabis use are associated wtih mood improvement in female emerging adults. Depress. Anxiety 33, 332–338. [DOI] [PubMed] [Google Scholar]
- Muhuri PK, 2014. Serious psychological distress and mortality among adults in the U.S. household population: highlights The CBHSQ Report. Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration, Rockville, MD: Available at https://www.ncbi.nlm.nih.gov/books/NBK385058/ [PubMed] [Google Scholar]
- Mustonen A, Niemela S, Nordstrom T, Murray GK, Maki P, Jaaskelainen E, Miettunen J, 2018. Adolescent cannabis use, baseline prodromal symptoms and the risk of psychosis. Br. J. Psychiatry 212, 227–233. [DOI] [PubMed] [Google Scholar]
- National Academies of Sciences Engineering and Medicine, 2017. The health effects of cannabis and cannabinoids: current state of evidence and recommendations for research The National Academies Press, Washington, DC: Available at https://www.nap.edu/catalog/24625/the-health-effects-of-cannabis-and-cannabinoids-the-current-state [PubMed] [Google Scholar]
- Newton NC, Andrews G, Champion KE, Teesson M, 2014. Universal Internet-based prevention for alcohol and cannabis use reduces truancy, psychological distress and moral disengagement: a cluster randomised controlled trial. Prev. Med 65, 109–115. [DOI] [PubMed] [Google Scholar]
- Okoro CA, Strine TW, Balluz LS, Crews JE, Dhingra S, Berry JT, Mokdad AH, 2009. Serious psychological distress among adults with and without disabilities. Int. J. Public Health 54 Suppl 1, 52–60. [DOI] [PubMed] [Google Scholar]
- Pacek LR, Mauro PM, Martins SS, 2015. Perceived risk of regular cannabis use in the United States from 2002 to 2012: differences by sex, age, and race/ethnicity. Drug Alcohol Depend 149, 232–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paradies Y, Ben J, Denson N, Elias A, Priest N, Pieterse A, Gupta A, Kelaher M, Gee G, 2015. Racism as a determinent of health: A systematic review and meta-analysis. PLoS One 10, e0138511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, Bray BC, Berglund PA, 2016. Reasons for marijuana use among young adults and long-term associations with marijuana use and problems. J. Stud. Alcohol Drugs 77, 881–888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, Schulenberg JE, O’Malley PM, Maggs JL, Kloska DD, Johnston LD, Bachman JG, 2011. Age-related changes in reasons for using alcohol and marijuana from ages 18 to 30 in a national sample. Psychol. Addict. Behav 25, 330–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Payton AR, 2009. Mental health, mental illness, and psychological distress: same continuum or distinct phenomena? J. Health Soc. Behav 50, 213–227. [DOI] [PubMed] [Google Scholar]
- Pratt LA, Dey AN, Cohen AJ, 2007. Characteristics of adults with serious psychological distress as measured by the K6 scale: United States, 2001–04. Adv. Data 382, 1–18. [PubMed] [Google Scholar]
- Prochaska JJ, Sung HY, Max W, Shi Y, Ong M, 2012. Validity study of the K6 scale as a measure of moderate mental distress based on mental health treatment need and utilization. Int. J. Methods Psychiatr. Res 21, 88–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAMHSA, 2014. Results from the 2013 National Survey on Drug Use and Health: summary of national findings, NSDUH Series H-48, HHS Publication No. (SMA) 14–4863 Substance Abuse and Mental Health Services Administration, Rockville, MD. [Google Scholar]
- Shi Y, 2014. At high risk and want to quit: marijuana use among adults with depression or serious psychological distress. Addict. Behav 39, 761–767. [DOI] [PubMed] [Google Scholar]
- Simons RL, Lei M-K, Beach SRH, Barr AB, Simons LG, Gibbons FX, Philibert RA, 2018. Discrimination, segregation, and chronic inflammation: Testing the weathering explanation for the poor health of Black Americans. Dev. Psychol 54, 1993–2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suerken CK, Reboussin BA, Egan KL, Sutfin EL, Wagoner KG, Spangler J, Wolfson M, 2016. Marijuana use trajectories and academic outcomes among college students. Drug Alcohol Depend 162, 137–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sung HY, Prochaska JJ, Ong MK, Shi Y, Max W, 2011. Cigarette smoking and serious psychological distress: a population-based study of California adults. Nicotine Tob. Res 13), 1183–1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twomey CD, 2017. Association of cannabis use with the development of elevated anxiety symptoms in the general population: a meta-analysis. J. Epidemiol. Community Health 71, 811–816. [DOI] [PubMed] [Google Scholar]
- Volkow ND, Baler RD, Compton WM, 2014. Adverse health effects of marijuana use. N. Engl. J. Med 370), 2219–2227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman JF, Pratt LA, Miller EA, Parker JD, 2015. Serious psychological distress among adults: United States, 2009–2013. NCHS. Data Brief 203, 1–8. [PubMed] [Google Scholar]
- Weissman J, Russell D, Jay M, Malaspina D, 2018. Racial, ethnic, and gender disparities in health care access and use among U.S. adults with serious psychological distress. Psychiatr. Serv 69, 517–522. [DOI] [PubMed] [Google Scholar]
- Whitlow CT, Liguori A, Livengood LB, Hart SL, Mussat-Whitlow BJ, Lamborn CM, Laurienti PJ, Porrino LJ, 2004. Long-term heavy marijuana users make costly decisions on a gambling task. Drug Alcohol Depend 76, 107–111. [DOI] [PubMed] [Google Scholar]
- WHO, 2017. Cannabis WHO Press; Accessed from http://www.who.int/substance_abuse/facts/cannabis/en/on10/05/2017, Geneva, Switzerland. [Google Scholar]
- Williams DR, Mohammed SA, 2009. Discrimination and racial disparities in health: evidence and needed research. J Behav Med 32(1), 20–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Brady KT, Mannelli P, Killeen TK, 2014. Cannabis use disorders are comparatively prevalent among nonwhite racial/ethnic groups and adolescents: a national study. J. Psychiatr. Res 50, 26–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Zhu H, Swartz MS, 2016. Trends in cannabis use disorders among racial/ethnic population groups in the United States. Drug Alcohol Depend 165, 181–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yap MBH, Reavley NJ, Jorm AF, 2011. Young people’s beliefs about the harmfulness of alcohol, cannabis, and tobacco for mental disorders: findings from two Australian national youth surveys. Addiction 107, 838–847. [DOI] [PubMed] [Google Scholar]
- Zorrilla I, Aguado J, Haro JM, Barbeito S, Lopez Zurbano S, Ortiz A, Lopez P, Gonzalez-Pinto A, 2015. Cannabis and bipolar disorder: does quitting cannabis use during manic/mixed episode improve clinical/functional outcomes? Acta Psychiatr. Scand 131, 100–110. [DOI] [PubMed] [Google Scholar]


