Abstract
Introduction
State legalization of marijuana for medical purposes could increase illicit marijuana use among young people. Medical marijuana laws may boost the availability of marijuana and reduce perceptions of its harmfulness, leading more young people to try it. Prior studies report little evidence that these laws are impacting marijuana consumption by young Americans, and none have systematically compared developmentally distinct age groups.
Methods
We performed multilevel, serial cross-sectional analyses on 10 annual waves of U.S. National Survey on Drug Use and Health, from 2004–2013, comparing young people in states with and without medical marijuana laws. Disaggregated analyses compared multiple measures of marijuana use across approximately 450,300 individuals in early adolescence (12–14 years), late adolescence (15–17 years) and young adulthood (18–24 years).
Results
Dwelling in a state that had legalized medical marijuana was not associated with marijuana consumption in the past month among early adolescents, late adolescents or young adults. However, young adults living in medical marijuana states were significantly more likely to have initiated first use in the past year.
Conclusions
Medical marijuana laws increase the likelihood that young adults will start using marijuana but do not affect more vulnerable developmental groups in early and late adolescence. Delaying the age of first use into young adulthood can reduce the risk of a drug use disorder later in life. Young adults are in the peak years of engagement with illicit drugs and state medical marijuana laws appear to be leading larger numbers to try the drug.
Keywords: marijuana, medical marijuana laws, development of substance abuse, adolescence, young adulthood
INTRODUCTION
One of the more controversial questions in drug policy today is whether the trend toward legalizing marijuana for medicinal and adult recreational use could increase illicit marijuana use among young people (Hall & Weier, 2015). Since 1996, 28 U.S. states and the District of Columbia have legalized the production and sale of marijuana for medicinal use (Online Resource 1), and eight have legalized marijuana for adult recreational use. Medical marijuana laws could potentially increase the availability of marijuana and reduce perceptions of its harmfulness, leading more young people to try it. State medical marijuana laws include regulations that protect young people from illegally obtaining marijuana (Chapman, Spetz, Lin, Chan, & Schmidt, 2016). But if these restrictions are not carefully enforced, young people could gain increased access to marijuana through the diversion of medical marijuana into illegal markets, which could also lower its price (Babor et al., 2010; Room, Fischer, Hall, Lenton, & Reute, 2010).
Marijuana use by young people is associated with lasting detrimental changes in cognitive functioning of the developing brain, and poor educational and occupational outcomes (Babor et al., 2010; Meier et al., 2012; Room et al., 2010; Volkow, Baler, Compton, & Weiss, 2014; Volkow et al., 2016). Use increases the risk of unintentional injuries and auto fatalities, mood and psychotic disorders, and drug dependence, especially when use is initiated at a young age (Asbridge, Hayden, & Cartwright, 2012; Degenhardt, Hall, & Lynskey, 2003; Feeney & Kampman, 2016; Hartman et al., 2016; Li et al., 2012; Rogeberg & Elvik, 2016; Volkow et al., 2014). Long-term marijuana smokers have a disproportionate burden of upper respiratory illnesses, including chronic bronchitis and some cancers, and an increased risk of cardiovascular disease (Franz & Frishman, 2016; The Office of Environmental Health Hazard Assessment, 2009).
Medical marijuana producers and retailers are promoting new, more potent products such as oils often used as inhalants with Tetrahydrocannabinol (THC) concentrations ranging from 40–70 percent (Substance Abuse and Mental Health Services Administration, 2016). They are also developing new products that appeal to youth, such as packaged edibles and candies, that may increase the hazard of overdose due to their relatively slow rates of absorption and perceived intoxication (Krupnick, 2016; Richter & Levy, 2014; Saloner, McGinty, & Barry, 2014). These products could increase the risk of overdose in young people, who tend to be less experienced users with low tolerance levels.
Studies have reported little evidence that medical marijuana laws increase marijuana use among young people (Anderson, Hansen, & Rees, 2012; Anderson, Hansen, & Rees, 2013; Choo et al., 2014; Gorman & Charles Huber, 2007; Hasin et al., 2015; Lynne-Landsman, Livingston, & Wagenaar, 2013; Wall et al., 2011), although well controlled studies consistently report increased consumption in adults (Cerdá, Wall, Keyes, Galea, & Hasin, 2012; Wen, Hockenberry, & Ciummings, 2014). Using the Youth Risk Behavior Survey, researchers have compared high school students’ consumption before and after medical marijuana laws were enacted, finding no evidence of rising consumption on a national basis (Choo et al., 2014; Lynne-Landsman et al., 2013). A national study of 12–17 year olds found that medical marijuana laws had no causal impact on consumption (Harper, Strumpf, & Kaufman, 2012), as did a carefully controlled national study of 13–18 year olds (Hasin et al., 2015). Wen et al. (Wen, Hockenberry, & Cummings, 2015) reported a five percent increase in the likelihood of trying marijuana among 12–20 year olds who dwell in states with medical marijuana laws, but the study was limited by the need to pool such a broad range of ages.
Prior studies have ignored or been unable to detect age-related variation in the impact of medical marijuana laws by pooling children aged 12–17, or even 12–24, or by studying particular age groups in isolation. Age-related variation is important to capture because young peoples’ access to marijuana and their developmental susceptibility to drug-related harms differs by age (Hadland, Knight, & Harris, 2015). Most studies have focused on high school students (15–17 years) who are likely to have greater access to marijuana and are more susceptible to social pressures than early adolescents (12–14 years) (Joffe & Yancy, 2004; Kandel, 1980). Meanwhile, young adults (18–25 years) different substantially from these younger groups, both in terms of development and access to drugs, being in the peak years of engagement with psychoactive substances during the lifespan (Bachman, Wadsworth, O’Malley, Johnston, & Schulenberg, 2013; Compton, Grant, Colliver, Glantz, & Stinson, 2004).
We performed multi-level, serial cross-sectional analyses on 10 annual waves of the U.S. National Survey on Drug Use and Health (NSDUH), from 2004–2013. Unlike many prior studies, ours included the key years of 2010–13—a period of rapid acceleration in the number of states implementing medical marijuana laws (Online Resource 1), but before state recreational marijuana laws began implementation. In addition, our analyses compared young people across developmentally distinct age groups to account for important age-related heterogeneity in access to marijuana, in the propensity to experiment with psychoactive substances, and in the potential harms of marijuana use.
METHODS
Sample
The primary data source was 10 annual waves of the NSDUH from 2004 to 2013. Following security clearance and a data use agreement with the U.S. Substance Abuse and Mental Health Services Administration, our team obtained access to individual-level NSDUH data that included the state of residence for each respondent. Each wave of the survey represents the U.S. population in all 50 states and the District of Columbia. During the period studied, no major changes in sampling, data collection, or instruments were made, thus preserving comparability across survey years. Full details of the data collection protocols, informed consent, and the questions asked are available in U.S. Substance Abuse and Mental Health Services Administration methodology reports (SAMHDA, 2011). This project received an ethics review and was approved by the University of California at San Francisco’s Committee on Human Research.
The total sample, pooled over 10 years, includes approximately 450,300 individuals. (Reported sample sizes must be rounded in accordance with U.S. Substance Abuse and Mental Health Services Administration confidentiality requirements.) We stratified young people into three discrete age groups: early adolescents (aged 12–14 years, rounded N=111,100), late adolescents (aged 15–17 years, rounded N=114,000), and young adults (aged 18–25 years, rounded N=225,200). Table 1 provides an overview of sample characteristics. All participant data was provided by the U.S. Substance Abuse and Mental Health Services Administration and is not based upon primary collection of clinical study or patient data requiring individual consent.
Table 1.
2013 Characteristics of Young People in Medical Marijuana and Non-Medical Marijuana States
| Age Category | Early Adolescents (12–14) | Late Adolescents (15–17) | Young Adults (18–25) | |||
|---|---|---|---|---|---|---|
| Living in medical marijuana state | MM % (SE) |
Non % (SE) |
MM % (SE) |
Non % (SE) |
MM % (SE) |
Non % (SE) |
| Female | 48.8 (1.1) | 47.8 (.8) | 49.0 (1.2) | 50.1 (.8) | 49.5 (.8) | 49.8 (.5) |
| Ethnicity/Race | Ethnicity/Race*** | Ethnicity/Race*** | Ethnicity/Race*** | |||
| White Non-Hispanic | 47.4 (1.3) | 58.0 (1.1) | 48.6 (1.2) | 59.5 (1.0) | 49.9 (1.1) | 59.7 (.8) |
| African-American/Black | 7.9 (.7) | 16.3 (.8) | 8.2 (.6) | 18.2 (.8) | 8.6 (.5) | 17.8 (.6) |
| Hispanic/Latino | 32.4 (1.3) | 18.3 (.9) | 29.8(1.2) | 16.2 (.8) | 28.8(1.0) | 16.1 (.6) |
| Other/Multi | 12.3 (.8) | 7.5 (.5) | 13.5 (.9) | 6.1 (.5) | 12.7 (.8) | 6.3 (.4) |
| Income | Income | Income** | Income*** | |||
| <$20,000 | 18.8 (1.0) | 18.8 (.7) | 15.9 (.9) | 18.0 (.7) | 29.9(1.2) | 34.0 (.9) |
| $20,000–49,999 | 29.3 (1.1) | 30.1 (.9) | 28.5(1.1) | 30.2 (.9) | 32.7 (.9) | 33.2 (.7) |
| $50,000–74,999 | 15.4 (.8) | 17.2 (.7) | 16.2 (.9) | 17.3 (.6) | 14.3 (.6) | 13.2 (.4) |
| $75,000–99,999 | 12.1 (.7) | 11.7 (.5) | 11.8 (.7) | 11.9 (.5) | 9.0 (.5) | 8.1 (.3) |
| $100,000+ | 24.4 (1.1) | 22.3 (1.0) | 27.6(1.2) | 22.5 (.8) | 14.1 (.7) | 11.5 (.5) |
| Has one or more children | 13.2 (.6) | 17.5 (.5)*** | ||||
| Ever been married | 9.8 (.6) | 12.4 (.4)*** | ||||
| Parents monitor screen time and/or enforce curfew | 76.9 (.9) | 76.3 (.7) | 70.3 (1.0) | 68.4 (.74) | ||
| Was in a group fight | 11.7 (.7) | 12.6 (.5) | 9.7 (.6) | 9.8 (.5) | ||
| Not in school, did not work last week | 16.6 (.7) | 17.0 (.5) | ||||
| Poor or fair health | 3.5 (.42) | 3.0 (.26) | 3.2 (.32) | 4.0 (.32)† | 6.5 (.38) | 5.8 (.26) |
| Lives in an urban area | 90.1 (.75) | 75.5 (1.13)*** | 90.1 (.81) | 77.0 (1.09)*** | 93.4 (.51) | 82.5 (.79)*** |
| Past month marijuana use | 3.0 (.38) 1 | .8 (.20)** | 13.8 (.70) | 10.7 (.45)*** | 22.5 (.70) | 17.0 (44)*** |
| Past year marijuana initiation | 3.3 (3.9) | 2.2 (.23)* | 8.4 (.58) | 7.2 (.41)† | 3.3 (.28) | 3.0 (.20) |
| Unweighted rounded N (%) | 4400 (39%) | 6800 (61%) | 4500 (40%) | 6700 (60%) | 8900 (40%) | 13300 (60%) |
Note: All analyses are weighted, empty cells were not asked of that age group or had insufficient N for analysis.
p<.10,
p<.05,
p<.01,
p<001 comparing MM and Non-MM states within age group
Measures
We examined three dichotomous outcomes at the individual level: self-reports of the accessibility of marijuana, consumption of marijuana within the past month, and initiation or first-time use of marijuana during the past year. The NSDUH framing of the marijuana questions references smoking, edibles, and oils. Individual-level, age-appropriate predictors from the NSDUH dataset were included in the analysis. Across all three age groups, these included sex, race/ethnicity, family income, poor or fair health, and living in an urban area. We included an indicator of poor or fair health status to control for the possibility that participants in medical marijuana states might engage in the legal use of marijuana for health reasons. For early and late adolescents, we also controlled for parental monitoring (i.e., whether parents enforce rules governing screen time and/or impose a curfew) and participation in group fights, variables that could be indicators of the protective factor of parental involvement and the risk factor of delinquent behavior, respectively. For young adults, additional controls included employment, college attendance, parental status, and marital status. These are strong protective factors mitigating against drug use in this age group (Dawson, Grant, Stinson, & Chou, 2006).
We augmented the NSDUH data with annually updated state-level data on medical marijuana laws and other relevant control variables. For state-level controls, we drew on publicly available sources such as Polidata (POLIDATA), including per capita drug courts and whether or not marijuana possession had been decriminalized. We considered a wider range of state-level controls representing demographic, political and religious factors, and aspects of state drug control policies. For the sake of parsimony, we included controls that were most associated with outcome variables. Data collection on state medical marijuana laws included gathering all state statutes and subsequent regulations, and validating information against publicly available data sources and through telephone calls with state officials. Throughout the study, we conducted regular updates to monitor changes in regulations and amendments to state laws (for details on this data collection, see: Chapman et al., 2016).
Analyses incorporated a dichotomous measure reflecting whether a state did or did not have a medical marijuana law enacted during any given year of observation. Thus, a law passed or enacted at any point in a calendar year would count that state as a medical marijuana state for that year’s analysis. We also examined a wide range of characteristics of state laws, such as the amounts of marijuana legally allowed for possession and home cultivation, medical conditions covered, and the number of dispensaries in each state. Through a systematic measurement process, we created and validated a scale capturing the capacity of a given medical marijuana law to control marijuana distribution and diversion into illegal markets (Chapman et al., 2016).
Data Analysis
We concatenated 10 annual waves of the NSDUH and all state-level indicators into a single data file. We conducted all analyses using Stata version 13 (StataCorp, 2015). For descriptive analyses of each survey year, we used weights to adjust for sampling design effects and nonresponse (National Survey on Drug Use and Health, 2011); similar weights were not available for multi-year analyses. Following Williams and others (Froot, 1989; Rogers, 1993; Williams, 2000; Wooldridge, 2002), we accounted for shared variance among participants within states by calculating standard errors clustered at the state level in our regression models. Our analytic approach used logistic regression to predict marijuana consumption and initiation at the individual level separately for early adolescents, late adolescents, and young adults. The regression models incorporated all individual- and state-level controls and annual fixed effects.
A key analytic concern is that people in states that pass medical marijuana laws hold more permissive views about the drug (Schmidt, Jacobs, & Spetz, 2016). These more positive perceptions about marijuana may drive both the passage of the medical marijuana laws and higher rates of consumption (Cerdá et al., 2012). We incorporated that possibility into our uncontrolled comparisons of young people who dwell in states with medical marijuana laws compared to those who do not (see Table 1). By controlling for state-level fixed effects (i.e., including a dummy variable for each state in the models), we were able to examine whether medical marijuana laws have distinct causal impacts on marijuana consumption and initiation (Harper et al., 2012). The coefficients for each state controlled for any state-specific confounding not already captured by other control variables in the models. This technique allowed us to rule out the possibility that unobserved state-level confounders (e.g., more liberal social norms on drug use in medical marijuana states) account for any associations found between state medical marijuana laws and young people’s consumption and initiation of use.
RESULTS
Using the most recent NSDUH survey, 2013, we compared rates of access to marijuana, past-month marijuana use and past-year initiation across early and late adolescent youth and young adults. Table 1 shows pronounced differences in the populations of young people living in states with medical marijuana laws compared with those who were not. These demographic differences—especially ones associated with drug-related attitudes—underscore the importance of applying individual-level controls in the analysis. For example, in 2013, individuals living in medical marijuana states were disproportionately white and Hispanic, and were also less likely to report a high degree of religiosity along with an age-based gradient whereby religiosity dropped off in older age groups. Young adults living in medical marijuana states were comparatively less likely to be married and to have children.
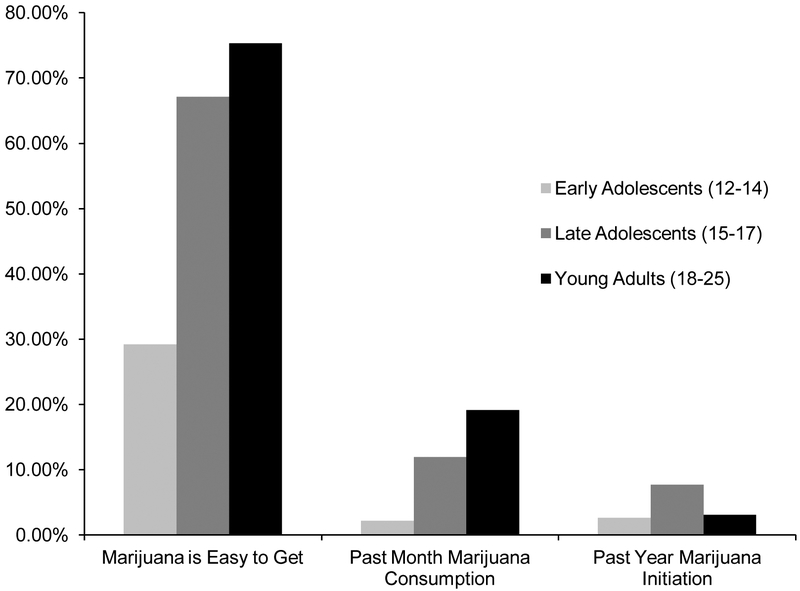
Figure 1 shows a positive age gradient in rates of reporting that marijuana is easily accessible and in past-month marijuana use: The highest prevalence occurred among young adults at 19.1%, then 11.9% of late adolescents and 2.2% of early adolescents (p < .001). In contrast, initiation of marijuana use in the past year was most common among late adolescents (7.7%), with young adults the next most likely to initiate marijuana use (3.1%) and early adolescents the least likely to have tried marijuana for the first time in the past year (2.6%; p< .001).
Figure 1.
This clustered bar chart shows values for the three developmental groups for each of three marijuana outcomes. First, 29.2% of early adolescents (age 12–14) reported that marijuana was easy to get, as compared to 67.1% of late adolescents (age 15–17) and 75.3% of young adults (age 18–25). Only 2.2% of early adolescents reported past month marijuana consumption, compared to 11.9% of late adolescents and 19.1% of young adults. Only 2.6% of early adolescents reported past year initiation of marijuana use, compared to 7.7% of late adolescents and 3.1% of young adults. All differences were statistically significant.
Figure 1 top. 2013 Marijuana Outcomes, By Developmental Group
All differences between age groups statistically significant at p < .001.
Table 2 shows logistic regression models predicting past-month marijuana consumption that include all individual- and state-level controls, and annual and state-level fixed effects. Results provided no evidence of a causal relationship between living in a state where medical marijuana was legal and the past month use of marijuana. Across all age groups, the odds ratio associated with medical marijuana state residence was not statistically significant.
Table 2.
Adjusted Odds Ratios Predicting Past Month Marijuana Consumption
| Age Category | Early Adolescents (12–14) OR, (95%CI) |
Late Adolescents (15–17) OR, (95%CI) |
Young Adults (18–25) OR, (95%CI) |
|---|---|---|---|
| Lives in a medical marijuana state | 1.12 (.89–1.42) | 1.06 (.96–1.16) | 1.02 (.96–1.07) |
| Year of Survey (vs. 2004) | |||
| 2005 | .87 (.75–1.02)† | .95 (.84–1.06) | .99 (.93–1.05) |
| 2006 | .87 (.73–1.03) | .89 (.82-.96)** | .99 (.94–1.05) |
| 2007 | .85 (.70–1.04) | .90 (.83-.98)* | .96 (.90–1.03) |
| 2008 | .85 (.71–1.02)† | .90 (.83-.98)* | .98 (.91–1.05) |
| 2009 | .97 (.82–1.15) | 1.02 (.92–1.14) | 1.06 (1.00–1.14)† |
| 2010 | 1.01 (.85–1.22) | 1.00 (.91–1.10) | 1.12 (1.04–1.20)** |
| 2011 | 1.06 (.90–1.24) | 1.08 (.97–1.20) | 1.11 (1.03–1.20)** |
| 2012 | 1.08 (.90–1.30) | 1.04 (.95–1.14) | 1.11 (1.04–1.18)** |
| 2013 | 1.07 (.93–1.24) | 1.05 (.95–1.17) | 1.10 (1.01–1.19)* |
| Individual-Level Predictors | |||
| Female | .97 (.90–1.04) | .85 (.82–.89)*** | .58 (.56–.59)*** |
| Ethnicity/Race (vs. White Non-Hispanic) | |||
| African-Am erican/Black | .79 (.66–.94)** | .81 (.71–.91)** | .89(.81–.98)* |
| Hispanic/Latino | .89 (.72–1.08) | .78 (.69–.87)*** | .58(.53–.63)*** |
| Other/Multi | 1.13 (.92–1.40) | .91 (.77–1.07) | .73 (.62–.85)*** |
| Income (vs. <$20,000) | |||
| $20,000–49,999 | .81 (.71–.91)*** | .97 (.91–1.04) | .85 (.82–.88)*** |
| $50,000–74,999 | .57(.48–.67)*** | .87 (.80–.94)** | .75 (.71–.79)*** |
| $75,000–99,999 | .55 (.45–.68)*** | .86 (.79–.94)** | .75 (.71–.80)*** |
| $100,000+ | .44 (.37–.53)*** | .86 (.78–.95)** | .84 (.80–.88)*** |
| Has one or more children | .78 (.73–.82)*** | ||
| Ever been married | .43 (.41–.46)*** | ||
| Parents monitor screen time and/or enforce curfew | .62 (.57–.66)*** | .76 (.73–.79)*** | |
| Was in a group fight | 3.95 (3.61–4.33)*** | 2.88 (2.73–3.05)*** | |
| Not in school, did not work last week | 1.28 (1.24–1.33)*** | ||
| Poor or fair health | 1.94 (1.70–2.22)*** | 1.71 (1.61–1.82)*** | 1.57 (1.50–1.65)*** |
| Lives in an urban area | 1.17 (1.00–1.37)† | 1.32 (1.22–1.43)*** | 1.29 (1.22–1.38)*** |
| State-Level Predictors | |||
| Marijuana decriminalized | 1.31 (1.13–1.52)*** | 1.05 (.88–1.26) | 1.01 (.93–1.09) |
| Per capita drug courts | .98 (.91–1.05) | 1.03 (.97–1.09) | 1.04 (1.00–1.08)† |
Note: Standard errors are clustered at the state level.
p<.10
p<.05
p<.01
p<.001. Empty cells were not asked of that age group or had insufficient N for analysis. Fixed effects of state of residence included in analysis, not displayed here.
Table 3 provides similar fully controlled results for logistic regression analyses predicting past-year initiation of marijuana use. Results show that young adults dwelling in states that have legalized medical marijuana are significantly more likely to initiate marijuana use than counterparts in non-medical marijuana states (OR=1.11, p<.05). Such a relationship is not evident for early or late adolescents (for similar models that do not control on state-level fixed effects, see Online Resources 2–4).
Table 3.
Adjusted Odds Ratios Predicting Past Year Marijuana Initiation
| Age Category | Early Adolescents (12–14) OR, (95%CI) |
Late Adolescents (15–17) OR, (95%CI) |
Young Adults (18–25) OR, (95%CI) |
|---|---|---|---|
| Lives in a medical marijuana state | 1.04 (.90–1.21) | .97 (.87–1.08) | 1.11 (1.02–1.22)* |
| Year of Survey (vs. 2004) | |||
| 2005 | .92 (.78–1.08) | .89 (.81–.97)* | .98 (.84–1.14) |
| 2006 | .80 (.69–.93)** | .95 (.87–1.03) | 1.03 (.90–1.18) |
| 2007 | .80 (.67–.96)* | .96 (.87–1.06) | 1.09 (.97–1.21) |
| 2008 | .95 (.82–1.10) | .95 (.87–1.04) | 1.07 (.94–1.22) |
| 2009 | 1.04 (.88–1.23) | 1.04 (.96–1.13) | 1.33 (1.19–1.49)*** |
| 2010 | 1.10 (.94–1.29) | 1.03 (.94–1.12) | 1.21 (1.06–1.38)** |
| 2011 | 1.06 (.90–1.25) | 1.03 (.94–1.13) | 1.29 (1.15–1.45)*** |
| 2012 | 1.02 (.86–1.21) | 1.00 (.91–1.10) | 1.18 (1.04–1.34)* |
| 2013 | .96 (.81–1.14) | 1.01 (.93–1.09) | 1.19 (1.05–1.34)** |
| Individual-Level Predictors | |||
| Female | 1.10 (1.04–1.16)** | 1.14 (1.10–1.19)*** | 1.28 (1.20–1.36)*** |
| Ethnicity/Race (vs. White Non-Hispanic) | |||
| African-Am erican/Black | .78 (.68–.90)** | .92(.83–1.02)† | 1.10(1.02–1.18)* |
| Hispanic/Latino | .89 (.78–1.02)† | .86(.80–.93)*** | .92 (.86–.97)** |
| Other/Multi | 1.05 (.88–1.25) | .87 (77–.99)* | .97 (.88–1.06) |
| Income (vs. <$20,000) | |||
| $20,000–49,999 | .93 (.84–1.03) | 1.02 (.96–1.09) | .66(.61–.70)*** |
| $50,000–74,999 | .74(.65–.85)*** | 1.06 (.98–1.15) | .76 (.69–.84)*** |
| $75,000–99,999 | .70 (.59–.84)*** | 1.12(1.03–1.22)** | .83 (74–.94)** |
| $100,000+ | .55 (.47–.64)*** | 1.21(1.11–1.32)*** | .95 (.88–1.03) |
| Has one or more children | .29 (.26–.32)*** | ||
| Ever been married | .36(.31–.42)*** | ||
| Parents monitor screen time and/or enforce curfew | .71 (.65–.77)*** | 1.01 (.97–1.05) | |
| Was in a group fight | 2.81 (2.56–3.10)*** | 1.53(1.44–1.61)*** | |
| Not in school, did not work last week | .57(.52–.62)*** | ||
| Poor or fair health | 1.32(1.11–1.56)** | 1.13(1.01–1.27)* | .97 (.85–1.11) |
| Lives in an urban area | 1.34(1.17–1.54)*** | 1.26(1.18–1.35)*** | 1.08 (.99–1.18)† |
| State-Level Predictors | |||
| Marijuana decriminalized | 1.16 (.80–1.70) | 1.04 (.92–1.18) | 1.09 (.96–1.23) |
| Per capita drug courts | 1.05 (.97–1.15) | 1.01 (.98–1.06) | .98 (.94–1.02) |
Note: Standard errors are clustered at the state level.
p<.10
p<.05
p<.01
p<.001. Empty cells were not asked of that age group or had insufficient N for analysis. Fixed effects of state of residence included in analysis, not display
We performed additional analyses to rule out several alternate explanations of these findings. Incorporating the amount of time since the passage of the medical marijuana law into our models produced similar results regardless of duration of the law. To rule out the possibility that young adults are more likely to initiate marijuana use due to mental health conditions, which in some states are legally allowed indications for a medical marijuana prescription, we estimated an alternate version of the models that included additional mental health-related variables, specifically, past-year use of mental health treatment and past-year unmet need for mental health treatment. After introduction of these additional controls, the effect of living in medical marijuana state remained statistically significant for young adults (Online Resource 5).
We also considered the possibility that states with less restrictive medical marijuana laws (e.g., allowing home cultivation, possession of larger amounts, a high density of dispensaries) could have more significant impacts on young people. We repeated all analyses with these variables and a summary scale reflecting the strength of controls on medical marijuana distribution, but these analyses failed to produce statistically significant results for any age group (Online Resources 6–11).
DISCUSSION
Prior studies focusing on whether medical marijuana laws impact young people’s consumption of marijuana have produced mixed results. In the absence of robust evidence that medical marijuana laws are not adversely impacting young people, the number of states passing these laws has accelerated. The analyses presented here found that medical marijuana laws are not causally associated with recent marijuana consumption in young people. However, we did find that medical marijuana laws impact the initiation of marijuana use, but that this is confined to young adults and does not include the more vulnerable populations of early and late adolescents.
Prior research has largely focused on how medical marijuana laws impact rates of marijuana consumption, placing less emphasis on the initiation of marijuana use. But the potential for these laws to impact the age-at-first use of marijuana has considerable public health significance. Initiating marijuana use in early adolescence is an important prognosticator for subsequent drug dependence (Flory, Lynam, Milich, Leukefeld, & Clayton, 2004; Lynskey, Heath, Bucholz, & et al., 2003; Merline, O’Malley, Schulenberg, Bachman, & Johnston, 2004; Stuart & Green, 2008). Younger age at initiation is one of the strongest predictors of drug dependence and related problems later in life (Lynskey et al., 2003; Robins, 1984).
Although we found a positive age gradient in the rates of consuming marijuana during the past month, patterns were different for initiating marijuana use. Our analysis showed that the initiation of marijuana use most commonly occurs during late adolescence. This finding is consistent with developmental theories suggesting that high-school age youth are uniquely prone to act on social messages and to experimentation with drugs (Johnston, O’Malley, & Bachman, 2016; Kandel, 1980).
Fully controlled regression analyses showed that medical marijuana laws significantly increase the likelihood of trying marijuana for the first time among young adults, but not younger age groups. Young adults are in the peak years of engagement with illicit drugs during the life course (Bachman et al., 2013; Compton et al., 2004). Compared to early and late adolescents, young adults have heightened availability and opportunities to use illicit drugs. This age group is past the peak age for initiating marijuana use and is therefore at a reduced risk for developing persistent marijuana-use disorders. However, our findings suggest that some of the young adults in this study might never have tried marijuana had they not been in a state that legalized medical marijuana.
Future research should disentangle the mechanisms that account for why young adults in states with medical marijuana laws are more prone to initiating use. This finding is consistent with the notion that medical marijuana products may be diverted into illegal markets, thus increasing marijuana’s availability and driving down its price (Nussbaum, Thurstone, McGarry, Walker, & Sabel, 2015). Increased accessibility of illicit drugs is an important factor predicting the likelihood that individuals will initiate use (Babor et al., 2010). Where larger numbers are using marijuana, whether for medical or non-medical reasons, individuals interested in trying the drug can more easily access information on how to obtain it (Jacobi & Sovinsky, 2016). Another possibility is that, in states with relatively lax enforcement of existing medical marijuana regulations, young adults are more willing to try marijuana because they perceive that the risk of arrest is low or generally perceive the drug as less risky. Given the importance of this issue for drug policy, research on the mechanisms through which medical marijuana laws promote the initiation of marijuana use by young adults should be prioritized.
This study was subject to several limitations. We were unable to rule out the possibility that, over longer windows of time, state medical marijuana laws will exert impacts on marijuana consumption and initiation by younger people dwelling in these states. We tested models using variables representing the length of time that each state’s medical marijuana law had been in place but found no statistically significant effects. We also could not examine whether legalization of marijuana for medical purposes has different effects as compared with recreational legalization; the NSDUH data did not extend into the years after recreational policies were established. The NSDUH data collection takes place at various points through the calendar year, and the date of any given participant interview may or may not have matched up with enactment of new medical marijuana legislation in their state; however local variation in availability of marijuana (dispensaries, local zoning, etc.) would make even a stricter date-based classification subject to the same potential mismatch on the individual level. Underreporting of drug consumption and initiation is also likely because of social acceptability concerns and survey respondents’ fears of disclosure (Babor, Brown, & Boca, 1990; Midanik, 1982). The NSDUH used computer-assisted interviewing to increase the validity of self-reports consistently throughout the 10-year observation period. As young peoples’ views about marijuana grow more permissive over time (Schmidt et al., 2016), survey respondents could become more willing to report that they have tried marijuana thus introducing bias into this analysis. Our multivariate models controlled for time trends to address this problem. Finally, our analyses could not capture sub-state variation in the implementation of medical marijuana laws (e.g., localities within medical marijuana states that have opted out of its legalization).
Implications
Scientists studying the impacts of drug laws should consider the potential for differential impacts across developmentally distinct age groups. Limited sample sizes often require researchers to pool age groups despite strong evidence that the availability of, and engagement with, illicit drugs profoundly differs for early and late adolescents, and young adults. This study, showing significantly different impacts across age groups, underscores the hazards of this approach.
This study suggests that medical marijuana laws are impacting young people by increasing the likelihood that young adults will initiate use, but that these laws are not affecting more vulnerable age groups of early and late adolescents. Given marijuana’s detrimental impacts on the developing brain well into young adulthood (Volkow, 2014), public health interventions should continue to target awareness of marijuana’s risks as it becomes more readily accessible. Policymakers should redouble efforts to enforce measures that limit the diversion of medical marijuana into illegal markets accessed by young adults and ensure that existing regulations are enforced to deter non-medical use.
Supplementary Material
SIGNIFICANCE.
State medical marijuana laws do not appear to affect marijuana use by early or late adolescents. These laws do increase the likelihood that young adults will try marijuana for the first time. Studies should compare developmentally distinct age groups given the heterogeneity of effects.
Acknowledgements
We would like to thank our colleagues who assisted in the data collection and technical execution of this manuscript, including Timothy Bates MA, Susan Chapman PhD, Casey Palmer MS, and Juliana Fung of the University of California at San Francisco. We would also like to acknowledge staff at the Substance Abuse and Mental Health Administration and the University of Michigan for their assistance in data acquisition and management. This study was supported by a grant from the U.S. National Institute on Drug Abuse (R01 DA034091) but played no role in the design and conduct of the study; data collection, management, analysis, and interpretation of the data; or in the preparation of this manuscript.
Footnotes
Conflicts of Interest
All authors declare that they have no conflicts of interest.
REFERENCES
- Anderson DM, Hansen B, & Rees DI (2012). Medical Marijuana Laws and Teen Marijuana Use. [Google Scholar]
- Anderson DM, Hansen B, & Rees DI (2013). Medical Marijuana Laws, Traffic Fatalities, and Alcohol Consumption. Journal of Law and Economics, 56(2), 333–369. doi: 10.1086/668812 [DOI] [Google Scholar]
- Asbridge M, Hayden JA, & Cartwright JL (2012). Acute Cannabis Consumption And Motor Vehicle Collision Risk: Systematic Review Of Observational Studies And Meta-Analysis. BMJ, 344, e536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babor T, Brown J, & Boca FD (1990). Validity of Self-Reports in Applied Research on Addictive Behaviors: Fact or Fiction? Behavioral Assessment, 12, 5–31. [Google Scholar]
- Babor TF, P. CJ, Edwards G, Fischer, Foxcroft DR, Humphreys K, … Reuter P (2010). Drug Policy and the Public Good. New York NY: Oxford University Press. [Google Scholar]
- Bachman JG, Wadsworth KN, O’Malley PM, Johnston LD, & Schulenberg JE (2013). Smoking, drinking, and drug use in young adulthood: The impacts of new freedoms and new responsibilities: Psychology Press. [Google Scholar]
- Cerdá M, Wall M, Keyes KM, Galea S, & Hasin D (2012). Medical Marijuana Laws In 50 States: Investigating The Relationship Between State Legalization Of Medical Marijuana And Marijuana Use, Abuse And Dependence. Drug And Alcohol Dependence, 120(1), 22–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman SA, Spetz J, Lin J, Chan K, & Schmidt LA (2016). Capturing Heterogeneity In Medical Marijuana Policies: A Taxonomy Of Regulatory Regimes Across The United States. Substance Use & Misuse, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choo EK, Benz M, Zaller N, Warren O, Rising KL, & McConnell KJ (2014). The Impact of State Medical Marijuana Legislation on Adolescent Marijuana Use. J Adolesc Health, 55(2), 160–166. [DOI] [PubMed] [Google Scholar]
- Compton WM, Grant BF, Colliver JD, Glantz MD, & Stinson FS (2004). Prevalence Of Marijuana Use Disorders In The United States: 1991–1992 And 2001–2002. JAMA, 291(17), 2114–2121. doi: 10.1001/jama.291.17.2114 [DOI] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, & Chou PS (2006). Maturing out of alcohol dependence: the impact of transitional life events. J Stud Alcohol, 67(2), 195–203. [DOI] [PubMed] [Google Scholar]
- Degenhardt L, Hall W, & Lynskey M (2003). Testing Hypotheses About The Relationship Between Cannabis Use And Psychosis. Drug And Alcohol Dependence, 71(1), 37–48. [DOI] [PubMed] [Google Scholar]
- Feeney KE, & Kampman KM (2016). Adverse effects of marijuana use. The Linacre Quarterly, 83(2), 174–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flory K, Lynam D, Milich R, Leukefeld C, & Clayton R (2004). Early adolescent through young adult alcohol and marijuana use trajectories: Early predictors, young adult outcomes, and predictive utility. Development and psychopathology, 16(01), 193–213. [DOI] [PubMed] [Google Scholar]
- Franz CA, & Frishman WH (2016). Marijuana Use and Cardiovascular Disease. Cardiology in Review, 24(4), 158–162. [DOI] [PubMed] [Google Scholar]
- Froot KA (1989). Consistent Covariance Matrix Estimation With Cross-Sectional Dependence And Heteroskedasticity In Financial Data. Journal of Financial and Quantitative Analysis, 24(03), 333–355. [Google Scholar]
- Gorman DM, & Charles Huber J Jr. (2007). Do medical cannabis laws encourage cannabis use? Int J Drug Policy, 18(3), 160–167. doi: S0955–3959(06)00211–8 [pii] 10.1016/j.drugpo.2006.10.001 [DOI] [PubMed] [Google Scholar]
- Hadland SE, Knight JR, & Harris SK (2015). Medical Marijuana: Review of the Science and Implications for Developmental-Behavioral Pediatric Practice. Journal of Developmental & Behavioral Pediatrics, 36(2), 115–123. doi: 10.1097/dbp.0000000000000129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall W, & Weier M (2015). Assessing The Public Health Impacts Of Legalising Recreational Cannabis Use In The Usa. Clinical Pharmacology & Therapeutics, 97(6), 607–615. doi: 10.1002/cpt.110 [DOI] [PubMed] [Google Scholar]
- Harper S, Strumpf EC, & Kaufman JS (2012). Do Medical Marijuana Laws Increase Marijuana Use? Replication Study And Extension. Ann Epidemiol, 22(3), 207–212. doi: 10.1016/j.annepidem.2011.12.002 [DOI] [PubMed] [Google Scholar]
- Hartman RL, Brown TL, Milavetz G, Spurgin A, Pierce RS, Gorelick DA, … Huestis MA (2016). Cannabis Effects On Driving Longitudinal Control With And Without Alcohol. Journal of Applied Toxicology. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Wall M, Keyes KM, Cerda M, Schulenberg J, O’Malley PM, … Feng T (2015). Medical Marijuana Laws And Adolescent Marijuana Use In The USA From 1991 To 2014: Results From Annual, Repeated Cross-Sectional Surveys. The Lancet Psychiatry, 2(7), 601–608. doi: 10.1016/S2215-0366(15)00217-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobi L, & Sovinsky M (2016). Marijuana on Main Street? Estimating Demand in Markets with Limited Access. American Economic Review, 106(8), 2009–2045. [Google Scholar]
- Joffe A, & Yancy WS (2004). Legalization Of Marijuana: Potential Impact On Youth. Pediatrics, 113(6), e632–638. [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, & Bachman JG (2016). Monitoring The Future National Survey Results On Drug Use,1975–2015: Overview, Key Findings On Adolescent Drug Use. Ann Arbor. [Google Scholar]
- Kandel DB (1980). Drug And Drinking Behavior Among Youth. Annual Review Of Sociology, 235–285. [Google Scholar]
- Krupnick M (2016, May 1, 2016). High Times and Agency Unite to Sell Marijuana to Mainstream, The New York Times. Retrieved from http://www.nytimes.com/2016/05/02/business/media/high-times-and-agency-unite-to-sell-marijuana-to-mainstream.html?r=3
- Li MC, Brady JE, DiMaggio CJ, Lusardi AR, Tzong KY, & Li G (2012). Marijuana Use And Motor Vehicle Crashes. Epidemiol Rev, 34(1), 65–72. doi: 10.1093/epirev/mxr017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynne-Landsman SD, Livingston MD, & Wagenaar AC (2013). Effects of State Medical Marijuana Laws on Adolescent Marijuana Use. American Journal of Public Health, e1–e7. doi: 10.2105/AJPH.2012.301117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynskey MT, Heath AC, Bucholz KK, & et al. (2003). Escalation Of Drug Use In Early-Onset Cannabis Users Vs Co-Twin Controls. JAMA, 289(4), 427–433. doi: 10.1001/jama.289.4.427 [DOI] [PubMed] [Google Scholar]
- Meier MH, Caspi A, Ambler A, Harrington H, Houts R, Keefe RSE, … Moffitt TE (2012). Persistent Cannabis Users Show Neuropsychological Decline From Childhood To Midlife. Proceedings of the National Academy of Sciences, 109(40). doi: 10.1073/pnas.1206820109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merline AC, O’Malley PM, Schulenberg JE, Bachman JG, & Johnston LD (2004). Substance use among adults 35 years of age: prevalence, adulthood predictors, and impact of adolescent substance use. American Journal of Public Health, 94(1), 96–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Midanik L (1982). The Validity of Self-Reported Alcohol Consumption and Alcohol Problems: A Literature Review. British Journal of Addiction, 77, 357–382. [DOI] [PubMed] [Google Scholar]
- National Survey on Drug Use and Health. (2011). Person-Level Sampling Weight Calibration. Rockville, Maryland. [Google Scholar]
- Nussbaum AM, Thurstone C, McGarry L, Walker B, & Sabel AL (2015). Use And Diversion Of Medical Marijuana Among Adults Admitted To Inpatient Psychiatry. Am J Drug Alcohol Abuse, 41, 166–172. doi: 10.3109/00952990.2014.949727 [DOI] [PubMed] [Google Scholar]
- POLIDATA.). Demographic & Political Guides: Political Data Analysis. http://www.polidata.org
- Richter KP, & Levy S (2014). Big Marijuana--Lessons From Big Tobacco. New England Journal of Medicine, 371(5), 399–401. doi: 10.1056/NEJMp1406074 [DOI] [PubMed] [Google Scholar]
- Robins LN (1984). The natural history of adolescent drug use. American Journal of Public Health, 74(7), 656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogeberg O, & Elvik R (2016). The Effects Of Cannabis Intoxication On Motor Vehicle Collision Revisited And Revised. Addiction, doi: 10.1111/add.13347. [DOI] [PubMed] [Google Scholar]
- Rogers W (1993). Quantile Regression Standard Errors. Stata Technical Bulletin, 2(9). [Google Scholar]
- Room R, Fischer B, Hall W, Lenton S, & Reute P (2010). Cannabis Policy: Moving Beyond Stalemate. New York, NY: Oxford University Press. [Google Scholar]
- Saloner B, McGinty EE, & Barry CL (2015). Policy Strategies to Reduce Youth Recreational Marijuana Use. Pediatrics, 135(6), 955–957. [DOI] [PubMed] [Google Scholar]
- SAMHDA. (2011). National Survey on Drug Use and Health, 2011. Ann Arbor, Michigan. [Google Scholar]
- Schmidt LA, Jacobs LM, & Spetz J (2016). Young People’s More Permissive Views About Marijuana: Local Impact of State Laws or National Trend? American Journal of Public Health(0), e1–e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp. (2015). Stata Statisitical Software: Release 14. College Station, TX: StataCorp LP. [Google Scholar]
- Stuart EA, & Green KM (2008). Using full matching to estimate causal effects in nonexperimental studies: Examining the relationship between adolescent marijuana use and adult outcomes. Developmental Psychology, 44(2), 395–406. doi: 10.1037/0012-1649.44.2.395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2016). Youth Perception of Marijuana Harm Decreases as “710” Becomes More Potent. http://newsletter.samhsa.gov/2016/05/25/710-oil-risks/.
- The Office of Environmental Health Hazard Assessment. (2009). Health and Safety Code section 25249.8(b) and Title 27, Cal Code of Regs., section 25302 et seq.A. Availability of Hazard Identification Materials for Marijuana Smoke, from http://oehha.ca.gov/proposition-65/crnr/availability-hazard-identification-materials-marijuana-smoke
- Volkow ND, Baler RD, Compton WM, & Weiss SRB (2014). Adverse Health Effects of Marijuana Use. New England Journal of Medicine, 370(23), 2219–2227. doi: doi :10.1056/NEJMra1402309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow ND, Swanson JM, Evins AE, DeLisi LE, Meier MH, Gonzalez R, … Baler R (2016). Effects of cannabis use on human behavior, including cognition, motivation, and psychosis: a review. JAMA Psychiatry, 73(3), 292–297. [DOI] [PubMed] [Google Scholar]
- Wall MM, Poh E, Cerda M, Keyes KM, Galea S, & Hasin DS (2011). Adolescent Marijuana Use From 2002 To 2008: Higher In States With Medical Marijuana Laws, Cause Still Unclear. Annals Of Epidemiology, 21(9), 714–716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen H, Hockenberry JM, & Ciummings JR (2014). The Effect of Medical Marijuana Laws on Marijuana, Alcohol, and Hard Drug Use. National Bureau of Economic Research Working Paper Series, No. 20085. [Google Scholar]
- Wen H, Hockenberry JM, & Cummings JR (2015). The Effect of Medical Marijuana Laws on Adolescent and Adult Use of Marijuana, Alcohol, and Other Substances. Journal of Health Economics, 42, 64–80. [DOI] [PubMed] [Google Scholar]
- Williams RL (2000). A Note On Robust Variance Estimation For Cluster-Correlated Data. Biometrics, 56(2), 645–646. [DOI] [PubMed] [Google Scholar]
- Wooldridge JM (2002). Econometric Analysis Of Cross Section And Panel Datamit Press. Cambridge, MA. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.