Abstract
Introduction
Unintended pregnancy during the postpartum period is common. The aim of this study was to describe contraceptive use among postpartum women and assess whether family planning counseling offered by health care providers during well-baby clinic visits increased use of modern contraceptive methods at six months following delivery.
Methods
Data comes from a cohort of women enrolled in a breastfeeding promotion trial in Kinshasa, Democratic Republic of Congo who reported being sexually active at 24-weeks post-partum. Modern contraceptive methods included intrauterine devices, injectables, implants, and contraception pills. Logistic regression models were used to estimate odd ratios (OR) and 95% confidence intervals (CI) for the impact of nurse counseling on use of modern birth control methods.
Results
Of 522 participants who reported being sexually active, 251 (48.0%) reported doing at least one thing to avoid pregnancy and were included in this analysis. Of these 251, 14.3% were using a modern contraceptive method, despite availability at the clinic. Discussion with a nurse about family planning was associated with increased odds of using modern birth control relative to other methods (OR = 4.0, 95%CI: 1.9, 8.6).
Discussion
Discussion of family planning with a nurse increased the odds of using a modern contraceptive among postpartum women. Integration of family planning counseling into postpartum services offers a potential avenue to increase modern contraceptive use among women with access.
Keywords: Postpartum, contraceptive use, family planning counselling, well-baby clinics, DR Congo
Introduction
Unintended pregnancies are pregnancies that are mistimed, unplanned or unwanted at the time of conception. Approximately 40 percent of all pregnancies worldwide are unintended (Sedgh, Singh, & Hussain, 2014). The postpartum period is an elevated at-risk period for unintended pregnancy since, most women wish to delay or prevent future pregnancies for up to a year following delivery (Ross & Winfrey, 2001). A recent study using the Global Network for Women’s and Children’s Health Research’s and involving over 36,000 postpartum women from 100 rural geographic clusters in 5 countries (India, Pakistan, Zambia, Kenya, and Guatemala), showed that at six weeks postpartum, less than 5% of these women wished to have another pregnancy within the year (Pasha et al., 2015). Yet half of those who wished to delay or prevent a future pregnancy had an unmet need for family planning services.
Short birth intervals are known to be associated with increased risk of poor perinatal outcomes including low birth weight, preterm birth, and newborn/infant mortality (Boerma & Bicego, 1992; Conde-Agudelo, Rosas-Bermudez, & Kafury-Goeta, 2006; Kuate Defo, 1997; Perin & Walker, 2015). Prior work estimated that preventing unmet need for contraception could prevent 29% of all maternal deaths annually (Saifuddin Ahmed, Li, Liu, & Tsui). At the household level, a previous randomized controlled trial showed that improved access to family planning services is associated with improved women’s earnings, assets, and children’s schooling and body mass indexes (Canning & Schultz, 2012).
Africa is the world’s region with the lowest prevalence of contraception use (Alkema, Kantorova, Menozzi, & Biddlecom, 2013). Despite recent progress in the region regarding maternal and child mortality, the burden remains substantial. The Democratic Republic of Congo (DRC) is the largest and most populous country in Central Africa and accounts for a significant portion of under-five mortality in West and Central Africa (You et al., 2015) and has substantially short birth intervals (Chirwa, Mantempa, Kinziunga, Kandala, & Kandala, 2014; Kandala et al., 2014). An estimated 30% of mothers in DRC have less than 24 months between births (Chirwa et al., 2014). Analysis of the DRC’s 2007 Demographic Health Surveys data showed that shorter birth intervals play a significant role in the observed high maternal and child death in the country (Kandala et al., 2014). Although the promotion of modern contraceptives has been traditionally integrated into prenatal care programs, even in Kinshasa, the capital city where utilization of well-baby services is high, there are no efforts to integrate family planning counseling into well-baby visits. Contraceptive counselling by a health provider during those visits has been recently shown to increase usage of contraceptives among postpartum women (Jarvis, Wickstrom, Vance, & Gausman, 2018).
The aim of this study was to assess whether family planning counseling offered by health care provider during well-baby clinic visits increased use of modern birth control methods at six months following delivery in a cohort of sexually active breastfeeding women in Kinshasa, DRC.
Methods
Study design and population
This study is a cross-sectional, secondary analysis of data from a cohort of women enrolled in a breastfeeding promotion trial in Kinshasa, DRC (trial registration: NCT01428232). Between May 24 and August 25, 2012, all women who gave birth to a healthy singleton in one of the six health facilities selected for the original study, were enrolled if they intended to attend well-baby clinic visits in the respective facilities, and consented to be part of the study. Details on selection of facilities and the main result from the study have been reported elsewhere (Yotebieng, Chalachala, Labbok, & Behets, 2013; Yotebieng et al., 2015; Zivich, Lapika, Behets, & Yotebieng, 2018).
Measures and variables definition
At enrollment interviews, in addition to demographic and obstetrical history, participants were also asked whether the pregnancy that led to the delivery was intended or not and for those who reported unintended pregnancy, whether they wanted to have a baby later or did not want any more children. At 24 weeks, participants were asked if they had any sexual intercourse since delivery. Those who responded yes to this question were considered to be sexually active. Since women might have been using abstinence as birth control, only women who reported to be sexually active at the 24 weeks after delivery interview were included in the analysis. Sexually active women asked if they were using any method to delay or avoid getting pregnant, and if yes, to specify which method they were using. Participants who reported doing something to delay or avoid getting pregnant were asked if a nurse in the health facility discussed contraceptive methods with them (nurse counseling). Nurse counseling was assessed via the following question, “did a nurse in this health structure discuss with you what contraceptive is appropriate for a breastfeeding mother like you?” As a result of the built-in skip pattern, our analysis of the impact of family planning counseling is limited to women who reported using some method to prevent pregnancy.
Three outcomes were considered for this analysis: modern contraceptive use (yes or no), condom use (yes or no), or other contraceptive methods (yes or no). Participants who reported one of the following were classified as user of modern contraceptives: intrauterine device (IUD), injectables, implants, contraception pills, sterilization (male or female), diaphragm, or foam jelly. Use of condoms (either male or female) was analyzed as a separate variable. All other reported methods were grouped into a single category.
All covariates were measured at enrollment and include age (continuous), education level (less than primary education, primary education or higher), marital/relationship status (married/live-in boyfriend, never married/separated/divorced), previous children (none / at least one), not wanting additional children (yes / no), and socio-economic status (SES). SES was a wealth index score divided into quintiles. Principal component analysis (PCA) was used to reduce the dimensions of the multiple structural SES indicators and calculate summarization scores. To calculate SES scores, the average number of household members per room (indication of crowding), number of sleeping beds in household, household water source (communal or private pipe), cooking fuel type (electric stove or wood/charcoal), and ownership of durable assets (radio, refrigerator, mobile phone, television) were included in the PCA model. The first PCA component explained 20.2% of the variability between the above indicators of SES and was divided into quintiles.
Statistical analysis
Logistic regression models were used to estimate odd ratios (OR) and 95% confidence intervals (CI) for the relation between each of the nurse counseling on family planning and birth control method categories independently. Generalized estimation equations were utilized to account for potential clustering at the clinic level. Confounders were identified a priori and included; age, education, marital status, previous children, wanting additional children, and SES. Nonlinearity was assessed for age through quadratic and cubic terms.
All analyses were conducted in SAS 9.4 (Cary, NC, USA). This study was approved by the Ohio State University Institutional Review Board and the Kinshasa School of Public Health Ethical Committee, and all women gave consent prior to inclusion in the study.
Results
Population characteristics
Among the 855 participants included in the original trial with available data at 24 weeks postpartum, 522 (61.1%) reported being sexually active. Less than half of sexually active women (n=251, 48.0%) reported doing something to avoid or delay pregnancy. Of women reporting action to avoid pregnancy, most had their first child as part of the study, were younger, and had not had their menstrual cycle return (TABLE 1).
TABLE 1:
Maternal characteristics of sexually active 24-week post-partum women in Kinshasa, Democratic Republic of Congo (n = 522)
| Reported action to prevent pregnancy (n = 251) | Did not report any action to prevent pregnancy (n = 271) | |
|---|---|---|
| Age (median, IQR) | 27 (23, 32) | 28 (24, 32) |
| Less than 20 years old | 21 (8.4%) | 15 (5.5%) |
| 20–29 | 134 (53.4%) | 149 (55.0%) |
| 30+ | 96 (38.2%) | 107 (39.5%) |
| Education | ||
| Less than primary | 170 (67.7%) | 179 (66.1%) |
| Primary or Higher | 81 (32.3%) | 92 (33.9%) |
| SES* | ||
| Fifth | 48 (19.3%) | 62 (23.2%) |
| Fourth | 55 (22.1%) | 57 (21.3%) |
| Third | 47 (18.9%) | 50 (18.7%) |
| Second | 51 (20.5%) | 42 (15.7%) |
| First | 48 (19.3%) | 56 (21.0%) |
| Missing | 2 | 4 |
| Marital Status | ||
| Married / live-in boyfriend | 233 (93.2%) | 260 (95.9%) |
| Never married / separated / | 17 (6.8%) | 11 (4.1%) |
| divorced | ||
| Missing | 1 | 0 |
| Previous births | ||
| First birth | 53 (21.1%) | 43 (15.9%) |
| Second or subsequent birth | 198 (78.9%) | 228 (84.1%) |
| Wants additional children | ||
| Yes | 224 (89.2%) | 235 (87.0%) |
| No | 27 (10.8%) | 35 (13.0%) |
| Missing | 0 | 1 |
| Menstrual cycle returned | ||
| Yes | 101 (40.9%) | 182 (67.2%) |
| No | 146 (59.1%) | 89 (32.8%) |
| Missing | 4 | 0 |
IQR: interquartile range, SES: socio-economic status. Data comes from women enrolled in a breastfeeding promotional trial in the DRC between May 24 and August 25, 2012. To be eligible, women had to have a singleton birth at study enrollment and consented to be part of the trial. Twenty-three women did not have a response to this question.
SES is wealth index score divided into quintiles. To determine the SES measure, the average number of household members per room (indication of crowding), number of sleeping beds in household, household water source (communal or private pipe), cooking fuel type (electric stove or wood/charcoal), and ownership of durable assets (radio, refrigerator, mobile phone, television) were included in principal component analysis. The first component explained 20.2% of the variability in the data.
Pregnancy avoidance practices
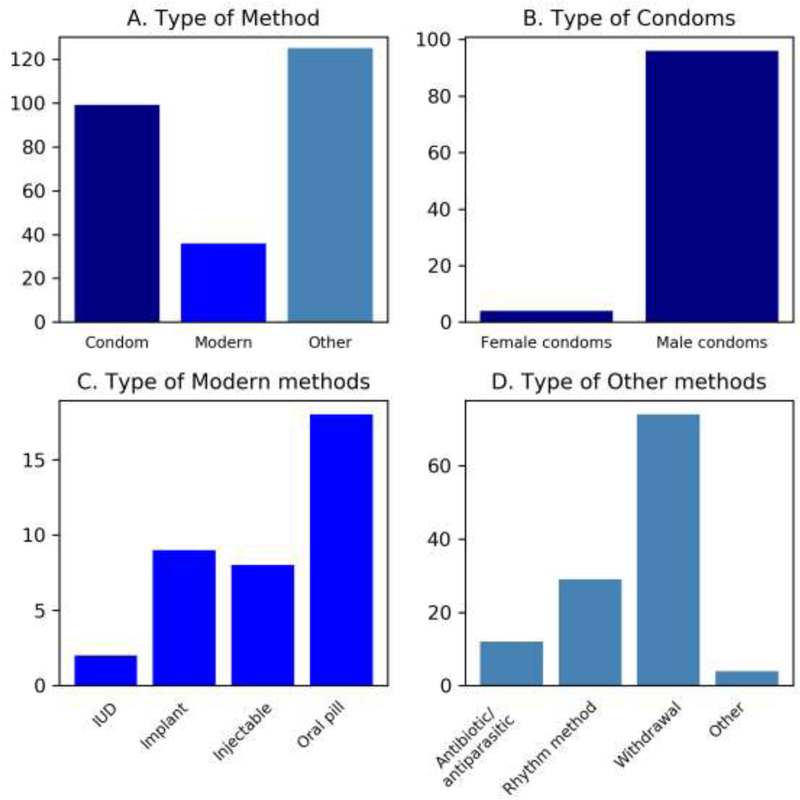
Of the 251 women included in the analysis, 99 (39.4%) reported using condoms, 36 (14.3%) reported using modern birth control methods, and 125 (49.8%) reported using other birth control methods (FIGURE 1). Eight women reported using both modern birth control and other birth control methods. One woman reported using modern birth control and condoms. Male condoms were reported more often than female condoms (97.0% vs. 4.0%). Reported modern contraceptives included intra-uterine devices (IUD) (5.6%), implants (25.0%), injectables (22.2%), and oral contraceptive pills (50.0%). Other birth control methods included antibiotics/antiparasitics (9.6%), rhythm method (23.2%), withdrawal (59.2%), and other methods (3.2%).
Figure 1:
Types of contraception used among 251 sexually active women who reported action to prevent pregnancy from six clinics in Kinshasa, Democratic Republic of Congo. *Cohort of women enrolled in a breastfeeding promotional trial in the DRC between May 24 and August 25, 2012. To be included women had to have a singleton birth at study enrollment and consented to be part of the trial. a Distribution of type of contraceptive method reported by the 251 women. b Distribution of female and male condoms among 99 who reported using condoms. c Distribution of type of methods among 36 women who reported using a modern contraceptive method. d Distribution of types of method used among 125 who reported using a method other than modern contraceptive or condoms.
Modern contraceptive methods were used more by older, higher educated, and multiparous women (TABLE 2). Women who reported modern contraceptive methods also wanted additional children compared to women using condoms or other methods. No modern contraceptive users were never married, separated, or divorced. About 10% of women who reported other, ineffectual, contraceptive methods reported not wanting additional children.
Table 2:
Contraceptive methods among sexually-active who reported trying to avoid or delay pregnancy at 24-weeks post-partum in Kinshasa, Democratic Republic of Congo (n = 251)
| Modern* (n = 36) | Condom* (n = 99) | Other* (n = 125) | |
|---|---|---|---|
| Nurse counseling† | |||
| Yes | 13 (38.2%) | 13 (14.1%) | 11 (10.0%) |
| No | 21 (61.8%) | 79 (85.9%) | 99 (90%) |
| Missing | 2 | 7 | 15 |
| Age (median, IQR) | 28 (24, 34) | 26 (22, 32) | 27 (24, 32) |
| Less than 20 years old | 3 (8.3%) | 9 (9.1%) | 9 (7.2%) |
| 20–29 | 18 (13.4%) | 52 (52.5%) | 71 (56.8%) |
| 30+ | 15 (41.7%) | 38 (38.4%) | 45 (36.0%) |
| Education | |||
| Primary or less | 22 (61.1%) | 66 (66.7%) | 85 (68.0%) |
| Secondary or higher | 14 (38.9%) | 33 (33.3%) | 40 (32.0%) |
| SES‡ | |||
| Fifth | 7 (20.6%) | 19 (19.2%) | 27 (21.6%) |
| Fourth | 8 (23.5%) | 20 (20.2%) | 28 (22.4%) |
| Third | 8 (23.5%) | 20 (20.2%) | 21 (16.8%) |
| Second | 7 (20.6%) | 20 (20.2%) | 25 (20.0%) |
| First | 4 (11.8%) | 20 (20.2%) | 24 (19.2%) |
| Missing | 2 | 0 | 0 |
| Marital Status | |||
| Married / live-in boyfriend | 36 (100%) | 90 (90.9%) | 114 (91.9%) |
| Never married / | |||
| separated / divorced | 0 (0%) | 9 (9.1%) | 10 (8.1%) |
| Missing | 0 | 0 | 1 |
| Previous births | |||
| First birth | 6 (16.7%) | 26 (26.3%) | 24 (19.2%) |
| Second or subsequent | |||
| birth | 30 (83.3%) | 73 (73.7%) | 101 (80.8%) |
| Wants additional children | |||
| No | 2 (5.6%) | 12 (12.1%) | 13 (10.4%) |
| Yes | 34 (94.4%) | 87 (87.9%) | 112 (89.6%) |
| Menstrual cycle returned | |||
| Yes | 25 (69.4%) | 52 (54.2%) | 75 (60.5%) |
| No | 11 (30.6%) | 44 (45.8%) | 49 (39.5%) |
| Missing | 0 | 3 | 1 |
IQR: interquartile range, SES: socio-economic status. Nurse counseling Birth control methods add up to more than 251, since eight women reported using both condoms and other methods and one woman reported using modern birth control with other methods.
Modern birth control methods included; intra-uterine device, implants, injectable, and oral contraceptive pills. Condoms included both male and female condoms. Other birth control methods included rhythm method, withdrawal, antibiotics/antiparasitics, and other. Other birth control methods are considered ineffectual
Nurse counseling on family planning was collected via the following question, “Did a nurse in this health structure discuss with you what contraceptive is appropriate for a breastfeeding mother like you?”. This question was only asked for women who reported action to prevent pregnancy
SES is wealth index score divided into quintiles. To determine the SES measure, the average number of household members per room (indication of crowding), number of sleeping beds in household, household water source (communal or private pipe), cooking fuel type (electric stove or wood/charcoal), and ownership of durable assets (radio, refrigerator, mobile phone, television) were included in principal component analysis. The first component explained 20.2% of the variability in the data.
Nurse counseling on family planning and choice of contraceptive methods
Discussion with a nurse about family planning was associated with increased odds of using modern birth control, decreased odds of reporting the use of other birth control methods, and a negligible decrease in odds of reported condom use (TABLE 3). Due to the sparsity of data, adjustment was only feasible for age, education, and SES. Nurse counseling regarding family planning remained associated with increased odds of modern birth control (OR = 4.0, 95% CI: 1.9, 8.6), and a decreased odds of other birth control methods (OR = 0.5, 95% CI: 0.2, 1.2). No relation between nurse counseling and condom use was observed in the adjusted model (OR = 1.0, 95% CI: 0.4, 2.6).
TABLE 3:
Relation between nurse counseling on family planning and type of contraceptive used among sexually active women who reported trying to avoid or delay pregnancy at 24-weeks post-partum in Kinshasa, Democratic Republic of Congo
| OR |
95% CI |
|
|---|---|---|
| Modern birth control methods | ||
| Bivariate* | 4.9 | 2.1, 11.1 |
| Multivariate model† | 4.0 | 1.9, 8.6 |
| Condom | ||
| Bivariate* | 0.8 | 0.3, 2.6 |
| Multivariate model† | 1.0 | 0.4, 2.6 |
| Other birth control methods | ||
| Bivariate* | 0.5 | 0.2, 1.0 |
| Multivariate model† | 0.5 | 0.2, 1.2 |
OR: odds ratio, 95% CI: 95% confidence interval.
Modern birth control methods included; intra-uterine device, implant, injectable, or oral contraceptives. Condoms included both male and female condoms. Other birth control methods included; rhythm method, withdrawal, antibiotics/antiparasitics, and other methods.
Bivariate model was modeled using generalized estimation equation to account for unknown correlation with clinic attended
Multivariate model was modeled using generalized estimation equation to account for unknown correlation with clinic attended. Confounders adjusted for were age, education, and socio-economic status
Discussion
In our analysis of sexually active women accessing well-baby services in Kinshasa, about half reported doing at least one thing to delay or avoid pregnancy. Of those who reported doing at least one thing, a majority reported using ineffective contraceptive methods. Miscommunication is a possible explanation for the observation that women reported using antibiotics or antiparasitics, since this has not been previously reported to our knowledge. To understand these observations, it is important to remember that these women were attending monthly well-baby visits in health facilities with modern contraceptives available on-site. Previous work in Kinshasa has indicated that providing free contraception in the postpartum period increases its uptake (Jarvis et al., 2018). However, low utilization despite access has also been previously been described in Kinshasa. In a survey of health facilities in Kinshasa conducted during 2012 and 2013, researchers found that lack of physical access was not the defining reason for low contraceptive use (Kayembe et al., 2015). In a follow-up study using focus groups, fear of side effects (especially sterility) and lack of information or misinformation were among key barriers to modern contraceptive use (M. Muanda, Gahungu Ndongo, Taub, & Bertrand, 2016). Fear of side effects and lack of information on contraceptive as barrier to adoption of modern contraceptives has also been reported in eastern Congo (Mathe, Kasonia, & Maliro, 2011). In this context, our finding that discussion with a nurse about family planning increased the odds of using effective modern contraceptive method support the importance of misinformation as a barrier. Our results align with recent work demonstrating that educating clinic staff and integrating referral tools can further increase modern contraceptive use over free access alone (Jarvis et al., 2018).
Antenatal counseling has not been observed to have a substantial effect on uptake of modern contraceptives in African settings (Ayiasi, Muhumuza, Bukenya, & Orach, 2015; Keogh et al., 2015). In a community-based intervention in Bangladesh, training of community health workers to provide integrated family planning counseling and services during home visits along with maternal and child health services increase contraceptive use by 15% at 12 months postpartum (S. Ahmed et al., 2015). Another study found that implementation of a package of instructions to healthcare staff to initiate conversations about family planning with all eligible women and to actively propose family planning during curative and under-fives consultations in rural health centers in Niger was followed by marked increases in family planning uptake (Bossyns, Miye, & vLerberghe, 2002). A systematic review found that integration of family planning into other healthcare services is likely to be beneficial, but concluded that further studies are needed (Kuhlmann, Gavin, & Galavotti, 2010). In light of others’ and our results, well-baby clinic visits provide an effective opportunity to provide postpartum women with information regarding modern contraceptives at a time they are most in need.
While we interpreted our findings as causal, there are substantive limitations to our interpretation. The major limitation of our study is how the information on nurse counseling was collected. Discussion with a nurse was self-reported by participants at 24-weeks (susceptible to recall bias) and counseling may have occurred after modern contraception was started. No information was collected regarding who initiated the conversation or the content of the conversation. While evidence indicates that family planning counseling increases the use of modern contraceptive during the postpartum period (Barber, 2007), women may have initiated the discussion with a nurse because they previously decided to use modern contraception. Another major limitation is that due to the original survey design, the analytic sample was restricted to sexually active women who reported doing something to avoid or delay pregnancy. Although this restriction is a good proxy for women with potential unmet need for contraceptives, providing contraceptives to women who might be abstaining or not doing anything to avoid pregnancy with information on modern contraceptives may alter their behavior as well. Additionally, women who were lost to follow-up before 24-weeks may have responded differently to nurse counseling about family planning or their contraceptive choices. Lastly, residual confounding in our estimates in likely. Due to the sparsity of data, our adjustment was reduced to only age, education, and SES. One important confounder we were unable to account for was male partners’ role regarding contraception choice. Previous research has shown influence of male partners in contraception decisions (Morse, Rowen, Steinauer, Byamugisha, & Kakaire, 2014; M. F. Muanda, Ndongo, Messina, & Bertrand, 2017; Orji, Ojofeitimi, & Olanrewaju, 2007; Sano et al., 2018). The limitations of our study could be addressed in future work by using a well-defined family planning intervention, prospectively following women after the discussion with a nurse, and studying a less restricted study population. Ideally, studies would follow women over a two-year period to determine the long-term impact of improved family planning counseling.
Conclusion
At six months postpartum, most sexually active women were not using any contraceptive in our study. Of women who reported using some form of contraception, few were using modern contraception, despite availability at their clinic. Reporting having discussed family planning with a nurse during well-baby clinic visits substantially increased odds of using modern birth control. In light of previous work and our results, integration of family planning counseling in well-baby clinic visits has promise regarding the uptake of modern contraceptives among postpartum women in low resource settings, like DRC.
Significance.
Recent evidence from low resource settings show that up to half of those who wished to delay or prevent a future pregnancy in postpartum had unmet need for family planning services. We found that less than half of sexually active women were using any form of contraceptive. Of those reporting contraceptive use, few used modern contraception. Postpartum women who reported having a discussion with a nurse regarding family planning at the well-baby visit were more likely to be using effective modern birth control. Together with other results, our study suggests integrated family planning counseling in postpartum follow-up is a simple strategy that can increase modern contraceptive use.
Acknowledgements
We are grateful for the participation and time of the study mothers and infants; the time and efforts of the personnel of the participating clinics (Esengo, Kikenda, Kitega, Libikisi, Lukunga, and Luyindu); the technical support of Drs. Aimee Lulebo, Dinah Kayembe, Landry Kiketa, Jean Lambert S. Chalachala, Mrs. Kathryn Salisbury, and Deidre Thompson; the data collection and data entry contributions of Clever Akili, Dyna Anambatu, Valerie B. Chalachala, Marie Dauly, Dydy Kayembe, Mamie Lulebo, Fanny Matadi, Myriam Mbonze, Espérance Mindia, Sarah Mushiya, Gisèle Mvumbi, Dodo Mwela, Jolly Ntirume, Ros Samba; and the administrative support of the UNC, KSPH, and Alive & Thrive administrative teams.
Funding
The original trial was supported by a grant from the Bill & Melinda Gates Foundation to FHI 360, through the Alive & Thrive Small Grants Program managed by UC Davis via a sub-award to the University of North Carolina at Chapel Hill. MY is partially supported by the NIAID U01AI096299–01 and the NICHD R01HD087993. The sponsors of the study had no role in study design, data collection, data analysis, data interpretation, writing of the report, or the decision to submit the paper for publication.
PNZ is supported by National Institute of Child Health and Human Development T32-HD091058
References
- Ahmed S, Ahmed S, McKaig C, Begum N, Mungia J, Norton M, & Baqui AH (2015). The Effect of Integrating Family Planning with a Maternal and Newborn Health Program on Postpartum Contraceptive Use and Optimal Birth Spacing in Rural Bangladesh. Stud Fam Plann, 46(3), 297–312. doi: 10.1111/j.1728-4465.2015.00031.x [DOI] [PubMed] [Google Scholar]
- Ahmed S, Li Q, Liu L, & Tsui AO Maternal deaths averted by contraceptive use: an analysis of 172 countries. The Lancet, 380(9837), 111–125. doi: 10.1016/S0140-6736(12)60478-4 [DOI] [PubMed] [Google Scholar]
- Alkema L, Kantorova V, Menozzi C, & Biddlecom A (2013). National, regional, and global rates and trends in contraceptive prevalence and unmet need for family planning between 1990 and 2015: a systematic and comprehensive analysis. Lancet, 381(9878), 1642–1652. doi: 10.1016/s0140-6736(12)62204-1 [DOI] [PubMed] [Google Scholar]
- Ayiasi RM, Muhumuza C, Bukenya J, & Orach CG (2015). The effect of prenatal counselling on postpartum family planning use among early postpartum women in Masindi and Kiryandongo districts, Uganda. Pan Afr Med J, 21, 138. doi: 10.11604/pamj.2015.21.138.7026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barber SL (2007). Family planning advice and postpartum contraceptive use among low-income women in Mexico. Int Fam Plan Perspect, 33(1), 6–12. doi: 10.1363/ifpp.33.006.07 [DOI] [PubMed] [Google Scholar]
- Boerma JT, & Bicego GT (1992). Preceding birth intervals and child survival: searching for pathways of influence. Stud Fam Plann, 23(4), 243–256. [PubMed] [Google Scholar]
- Bossyns P, Miye H, & vLerberghe W (2002). Supply-level measures to increase uptake of family planning services in Niger: the effectiveness of improving responsiveness. Trop Med Int Health, 7(4), 383–390. [DOI] [PubMed] [Google Scholar]
- Canning D, & Schultz TP (2012). The economic consequences of reproductive health and family planning. Lancet, 380(9837), 165–171. doi: 10.1016/s0140-6736(12)60827-7 [DOI] [PubMed] [Google Scholar]
- Chirwa TF, Mantempa JN, Kinziunga FL, Kandala JD, & Kandala NB (2014). An exploratory spatial analysis of geographical inequalities of birth intervals among young women in the Democratic Republic of Congo (DRC): a cross-sectional study. BMC Pregnancy Childbirth, 14, 271. doi: 10.1186/1471-2393-14-271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conde-Agudelo A, Rosas-Bermudez A, & Kafury-Goeta AC (2006). Birth spacing and risk of adverse perinatal outcomes: a meta-analysis. Jama, 295(15), 1809–1823. doi: 10.1001/jama.295.15.1809 [DOI] [PubMed] [Google Scholar]
- Jarvis L, Wickstrom J, Vance G, & Gausman J (2018). Quality and Cost Interventions During the Extended Perinatal Period to Increase Family Planning Use in Kinshasa, DRC: Results From an Initial Study. Glob Health Sci Pract, 6(3), 456–472. doi: 10.9745/ghsp-d-18-00075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kandala NB, Mandungu TP, Mbela K, Nzita KP, Kalambayi BB, Kayembe KP, & Emina JB (2014). Child mortality in the Democratic Republic of Congo: cross-sectional evidence of the effect of geographic location and prolonged conflict from a national household survey. BMC Public Health, 14, 266. doi: 10.1186/1471-2458-14-266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kayembe P, Babazadeh S, Dikamba N, Akilimali P, Hernandez J, Binanga A, & Bertrand JT (2015). Family Planning Supply Environment in Kinshasa, DRC: Survey Findings and Their Value in Advancing Family Planning Programming. Glob Health Sci Pract, 3(4), 630–645. doi: 10.9745/ghsp-d-15-00298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keogh SC, Urassa M, Kumogola Y, Kalongoji S, Kimaro D, & Zaba B (2015). Postpartum Contraception in Northern Tanzania: Patterns of Use, Relationship to Antenatal Intentions, and Impact of Antenatal Counseling. Stud Fam Plann, 46(4), 405–422. doi: 10.1111/j.1728-4465.2015.00040.x [DOI] [PubMed] [Google Scholar]
- Kuate Defo B (1997). Effects of infant feeding practices and birth spacing on infant and child survival: a reassessment from retrospective and prospective data. J Biosoc Sci, 29(3), 303–326. [DOI] [PubMed] [Google Scholar]
- Kuhlmann AS, Gavin L, & Galavotti C (2010). The integration of family planning with other health services: a literature review. Int Perspect Sex Reprod Health, 36(4), 189–196. doi: 10.1363/3618910 [DOI] [PubMed] [Google Scholar]
- Mathe JK, Kasonia KK, & Maliro AK (2011). Barriers to adoption of family planning among women in Eastern Democratic Republic of Congo. Afr J Reprod Health, 15(1), 69–77. [PubMed] [Google Scholar]
- Morse JE, Rowen TS, Steinauer J, Byamugisha J, & Kakaire O (2014). A qualitative assessment of Ugandan women’s perceptions and knowledge of contraception. Int J Gynaecol Obstet, 124(1), 30–33. doi: 10.1016/j.ijgo.2013.07.014 [DOI] [PubMed] [Google Scholar]
- Muanda M, Gahungu Ndongo P., Taub LD, & Bertrand JT (2016). Barriers to Modern Contraceptive Use in Kinshasa, DRC. PLoS ONE, 11(12), e0167560. doi: 10.1371/journal.pone.0167560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muanda MF, Ndongo GP, Messina LJ, & Bertrand JT (2017). Barriers to modern contraceptive use in rural areas in DRC. Cult Health Sex, 19(9), 1011–1023. doi: 10.1080/13691058.2017.1286690 [DOI] [PubMed] [Google Scholar]
- Orji EO, Ojofeitimi EO, & Olanrewaju BA (2007). The role of men in family planning decision- making in rural and urban Nigeria. Eur J Contracept Reprod Health Care, 12(1), 70–75. doi: 10.1080/13625180600983108 [DOI] [PubMed] [Google Scholar]
- Pasha O, Goudar SS, Patel A, Garces A, Esamai F, Chomba E, … Goldenberg RL (2015). Postpartum contraceptive use and unmet need for family planning in five low-income countries. Reprod Health, 12 Suppl 2, S11. doi: 10.1186/1742-4755-12-s2-s11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perin J, & Walker N (2015). Potential confounding in the association between short birth intervals and increased neonatal, infant, and child mortality. Glob Health Action, 8, 29724. doi: 10.3402/gha.v8.29724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross JA, & Winfrey WL (2001). Contraceptive Use, Intention to Use and Unmet Need during the Extended Postpartum Period. International Family Planning Perspectives, 27(1), 20–27. doi: 10.2307/2673801 [DOI] [Google Scholar]
- Sano Y, Antabe R, Atuoye KN, Braimah JA, Galaa SZ, & Luginaah I (2018). Married women’s autonomy and post-delivery modern contraceptive use in the Democratic Republic of Congo. BMC Womens Health, 18(1), 49. doi: 10.1186/s12905-018-0540-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sedgh G, Singh S, & Hussain R (2014). Intended and Unintended Pregnancies Worldwide in 2012 and Recent Trends. Studies in family planning, 45(3), 301–314. doi: 10.1111/j.1728-4465.2014.00393.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yotebieng M, Chalachala JL, Labbok M, & Behets F (2013). Infant feeding practices and determinants of poor breastfeeding behavior in Kinshasa, Democratic Republic of Congo: a descriptive study. Int Breastfeed J, 8(1), 11. doi: 10.1186/1746-4358-8-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yotebieng M, Labbok M, Soeters HM, Chalachala JL, Lapika B, Vitta BS, & Behets F (2015). Ten Steps to Successful Breastfeeding programme to promote early initiation and exclusive breastfeeding in DR Congo: a cluster-randomised controlled trial. Lancet Glob Health, 3(9), e546–555. doi: 10.1016/s2214-109x(15)00012-1 [DOI] [PubMed] [Google Scholar]
- You D, Hug L, Ejdemyr S, Idele P, Hogan D, Mathers C, … Alkema L (2015). Global, regional, and national levels and trends in under-5 mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Inter-agency Group for Child Mortality Estimation. Lancet, 386(10010), 2275–2286. doi: 10.1016/s0140-6736(15)00120-8 [DOI] [PubMed] [Google Scholar]
- Zivich P, Lapika B, Behets F, & Yotebieng M (2018). Implementation of Steps 1–9 to Successful Breastfeeding Reduces the Frequency of Mild and Severe Episodes of Diarrhea and Respiratory Tract Infection Among 0–6 Month Infants in Democratic Republic of Congo. Matern Child Health J, 22(5), 762–771. doi: 10.1007/s10995-018-2446-9 [DOI] [PMC free article] [PubMed] [Google Scholar]