Abstract
Purpose:
There is considerable variation in epidemiology and clinical course of psychotic disorders across social and geographical contexts. To date, very little data is available from low- and middle-income countries (LMICs). In Sub-Saharan Africa, most people with psychoses remain undetected and untreated, partly due to lack of formal health care services. This study in rural South Africa aimed to investigate if it is possible to identify individuals with recent onset psychosis in collaboration with traditional health practitioners (THPs).
Methods:
We developed a strategy to engage with THPs. Fifty THPs agreed to collaborate and were asked to refer help-seeking clients with recent onset psychosis to the study. At referral, the THPs rated probability of psychosis (“maybe disturbed” or “disturbed”). A two-step diagnostic procedure was conducted, including the self-report Community Assessment of Psychic Experiences (CAPE) as screening instrument, and a semi-structured interview using the Schedules for Clinical Assessment in Neuropsychiatry (SCAN). Accuracy of THP referrals, and test characteristics of the THP rating and the CAPE were calculated.
Results:
149 help-seeking clients were referred by THPs, of which 44 (29.5%) received a SCAN DSM-IV diagnosis of psychotic disorder. The positive predictive value of a THP “disturbed” rating was 53.8%. Test characteristics of the CAPE were poor.
Conclusion:
THPs were open to identifying and referring individuals with possible psychosis. They recognized “being disturbed” as a condition for which collaboration with formal psychiatric services might be beneficial. By contrast, the CAPE performed poorly as a screening instrument. Collaboration with THPs is a promising approach to improve detection of individuals with recent onset psychosis in rural South Africa.
Keywords: Psychosis, South Africa, Traditional Health Practitioners, Case finding, Screening
Introduction
In recent years, the global understanding of the epidemiology and clinical course of psychosis has changed substantially. We now know that there are variations in the incidence of psychotic disorders between and within countries, but to date most evidence has originated from high-income countries (HICs), with very little data available from low- and middle-income countries (LMICs). There are no reliable incidence data on psychotic disorders in Sub-Saharan Africa (SSA). While the 1992 World Health Organization (WHO) Collaborative Study on the Determinants of Outcome of Severe Mental Disorders (DOSMeD) 10-country study included data from Nigeria 1, and researchers in Butajira, Ethiopia in the early 2000s 2 found some incident cases in their community prevalence study of severe mental disorders, methodological limitations meant that incidence rates could not be calculated. Recently, Morgan and colleagues reported incidence rates from a pilot study in Ibadan, Nigeria 3. They detected 48 individuals with psychotic disorders and estimated incidence rates of 31.2/100 000 person years for all psychotic disorders and 27.5/100 000 person years for schizophrenia. And a retrospective hospital-based study in KwaZulu-Natal, South Africa, reported a treated incidence rate for psychotic disorders of 33.7/100 000 person years 4. Obtaining valuable evidence from under-represented regions such as SSA holds the promise of advancing our knowledge and understanding of psychosis and will provide a strong basis for redressing inequities in service provision for people with psychotic disorders living in LMICs. A major barrier to realizing this goal is the very substantial ‘mental health gap’ that characterizes most LMICs, where the lack of (good quality) formal mental health resources results in poor access to care for people with mental illnesses. Kebede and colleagues in Ethiopia reported that over 90% of those identified with psychotic disorders in rural Butajira had never received formal treatment 2, while the South African Stress and Health Study (SASH), which was part of the Global Mental Health Surveys, found that only 28% of individuals with severe mental illness had received treatment 5. This gap calls for novel strategies for identifying people with psychosis in resource-limited settings, that do not rely upon contact with mental health services. One such strategy is to incorporate traditional health practitioners (THPs) in efforts to improve detection of psychosis. Research in a number of Sub-Saharan regions suggests that consultation of a THP as first care provider is very common in pathways to accessing mental health care of people with first onset psychosis 6–8. Within Africa, there are several examples of successful collaboration between biomedical services and THPs in relation to tuberculosis and HIV counseling, screening, referral and co-management 9,10. These collaborations were motivated by the same need confronting mental health to find solutions to the problem of lack of access to formal health care. In relation to psychotic disorders, collaboration with THPs may be more difficult, given the apparent gulf separating biomedical from traditional/spiritual explanations and understandings of psychological and behavioural phenomena 11. However, in relation to a Ugandan study by Abbo 12, Patel notes the perhaps surprising observation that “not only were descriptions based on the biomedical classifications of psychoses recognised by the traditional healers, but … the indigenous taxonomy mapped on to the biomedical categories.” 13. This is encouraging, as are the findings of Sorsdahl and colleagues in South Africa that THPs are generally very positive about collaboration with biomedical services in optimizing the care of people with mental health problems 14.
The current study was designed as a preparatory study for the investigation of the incidence, early course and treatment pathways of psychotic disorders - so called FEP-INCET study - in a rural South African community. We aimed to describe local pathways to care, identify key gatekeepers for case identification of psychotic disorders, and investigate if it is possible to identify patients with recent onset psychosis in collaboration with THPs. In this paper we report on:
Our strategy to build a successful collaboration with THPs with a view to the development of a method for screening and referral of individuals in the community with possible incident psychosis.
The positive predictive value of referrals by THPs for a DSM-IV diagnosis of psychotic disorder as made by trained psychiatrists using a semi-structured psychiatric diagnostic interview (Schedules for Clinical Assessment in Neuropsychiatry (SCAN) 15).
The test characteristics of a self-report questionnaire (the Community ssessment of Psychic Experiences (CAPE) 16) as screening instrument for improving detection of psychotic disorder in patients referred by THPs for suspected psychosis.
Methods
The study site
South Africa, as with most countries in Sub-Saharan Africa, has a significant treatment gap in terms of mental health care resources available to identify and treat a large burden of mental disorders 17. In KwaZulu-Natal Province, it has been estimated that only 25% of the beds required to provide adequate in-patient psychiatric care are available 17. Community mental health services are even less adequate, especially in rural and remote regions of this geographically large province. Vulindlela is one such rural region, 150 kms inland of the city of Durban. Vulindlela, with a population of approximately 250,000, has a strong traditional council with five traditional wards, each headed by a tribal chief. The tribal chiefs play a key role in community life in parallel with formal government authorities. The region is characterized by widespread poverty and unemployment (unemployment rate 45%) and many households lack basic amenities such as running water and electricity 18. The HIV prevalence in KZN is among the highest in the country with 60% in 25–40 years old women and 40% in men of the same age group 19. The only formal health services available in Vulindlela are 8 primary health care (PHC) clinics across the five wards, and four general practitioners, all in one ward. The nearest hospitals (two district hospitals, a tertiary level general hospital, and the Town Hill psychiatric hospital) are 40kms away in the nearest town, Pietermaritzburg, and are effectively inaccessible for many residents, the majority of whom live below the poverty line, struggling to afford food, let alone the costs of public transport. One can reasonably assume therefore, that a major proportion of health care delivered to this community comes from the traditional health practitioners practicing in the region.
A strategy to build collaboration with traditional health practitioners
We developed a strategy to engage with THPs with the objective of involving them in screening and detection of psychosis amongst their help-seeking clients. This strategy is best summarized in terms of the following steps: 1. Engagement with community leadership to establish a partnership; 2. Establishment of a Community Research Advisory Board (CRAB); 3. Engagement with THPs to develop mutual understanding of traditional and biomedical concepts of psychosis; 4. Developing a method for screening and referral by THPs of individuals in the community with possible incident psychosis.
1. Engagement with community leadership to establish a partnership
In the FEP-INCET study, we first identified and recruited as project coordinator a key individual (EM) who is both a psychiatric nurse and has worked closely with traditional leadership and THP groups in the region for many years. The project coordinator held initial meetings with tribal counselors, followed by an audience with the senior traditional ‘Inkosi’ or chief of the Vulindlela region, where he presented the study his Traditional Council and to the other amakhosi. The study was received favorably as having social value for the community. It is important to note that, in part, our favorable reception was due to the fact that we collaborated from the outset with a group of HIV researchers who previously had not only investigated HIV infection in Vulindlela, but had also provided HIV prevention and care within this community 20. An ‘Induna’ or traditional counselor was assigned to work with EM to arrange a community meeting where the research team could present the study to local traditional and government authorities, THPs from the region and other key stakeholders in the community. With the chief’s blessing and consent, a partnership was established between the Traditional Council and the FEP-INCET study through a formal signed memorandum of understanding (MOU). The MOU governed the conduct and accountability of the research team and its activities, clarified expectations of both parties and, critical to the success of the study, provided the authority of the traditional leadership and chief for participation of THPs within the region. Upon signing of the MOU, the Traditional Council provided the research team with a list of all approximately 200 bona fide THPs in the region and their contact details.
2. Establishment of a Community Research Advisory Board (CRAB)
The MOU made provision for the establishment at the outset of a Community Research Advisory Board (CRAB). This was a necessary step in building the collaboration and safeguarding its fairness and accountability to the community. The CRAB provided an oversight role to ensure the research proceeded ethically and in a socially and culturally appropriate manner that would not violate the values and beliefs of participants and the wider community. This was key to overcoming historic antipathy between biomedical practitioners and researchers and THPs. In addition to providing ethical oversight, the CRAB provided community input and feedback to the research team, raised any concerns from the community, linked researchers to key community resources, helped disseminate research-related information, and took on an advocacy role for mental health awareness in Vulindlela.
3. Engagement with THPs to develop mutual understanding of traditional and biomedical concepts of psychosis
THPs from the tribal authorities of Vulindlela, listed by the Traditional Council, were contacted and invited to attend a meeting focused on information sharing and mutual education about concepts of mental health, disease and healing. Thereafter, we used snowballing to identify and invite additional THPs to subsequent meetings. Efforts were made to ensure that all THPs in the region had the opportunity to participate if they so wished. Meetings were structured to explore respective notions and understandings of a variety of psychological and behavioral phenomena, with an emphasis on psychotic symptoms using case vignettes. In addition a focus group discussion (with 8 THPs) as well as 10 individual semi-structured interviews with THPs were held to elicit knowledge, attitudes and practices associated with mental illness (again emphasizing psychosis) and its traditional treatment in that community 21. While it is beyond the scope of this paper to describe the actual worldview of THPs and their understanding of psychotic phenomena, it is relevant here to report that a degree of common ground was discovered during this process. Where THPs recognize a number of different causes for abnormal mental functioning and behavior, including displeasure of ancestors, failure to perform ritual duties, calling to become a healer (ukuthwasa), and bewitchment, they also ascribe some presentations to biological, psychological or social etiologies (e.g. epilepsy, cannabis, and ‘stress’). They also recognize a category of severe mental and behavioral disturbance they define as mental illness and in most cases regard as the treatment domain of biomedical health systems. According to THPs, violence, picking up garbage, talking randomly, walking for long periods of time and undressing in public are characteristic signs of this category of mental health problems 11. The discovery of this ‘common ground’ allowed the research team to move on to the next key phase of this collaboration, namely collaboration with THPs to develop a method for screening and referral of individuals in the community becoming ill with possible psychosis.
4. Developing a method for screening and referral of individuals in the community with possible incident psychosis
Including THPs in screening and referral of individuals with possible incident psychosis in the community, required the recruitment of specific healers who would be verified by tribal authorities as authentic, would consent to participate in the study, and would commit to participating in training. Of the approximately 200 THPs verified as legitimate by the Traditional Council, 50 were finally recruited to the study, signing informed consent. Of these, 8 stated they specialised in clients with mental health conditions. We recorded contact details, working hours, and category of healer (i.e. isangoma (diviner), inyanga (herbalist) or umthandazi (faith healer)), as well as areas of specialization for all 50 THPs.
THPs were requested to refer to the research team any of their adult clients (aged 21 – 48 years) who had made first contact with the THP for a mental health problem and whom they suspected of “being disturbed”, with an onset of symptoms not more than six months ago. The “disturbed” terminology was decided upon during the preparatory educational/training meetings as a translation of an isiZulu term that refers to a syndrome recognized by THPs most closely describing the clinical construct of psychotic disorder. At referral, potential client participants were contacted by the research team and written (and if not possible due to illiteracy, oral) informed consent was obtained. The study was approved by the University of KwaZulu-Natal Biomedical Research Ethics Committee and Columbia University Institutional Review Board and has therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Assessments of individuals referred to the study by THPs
THPs were instructed to refer not only cases they had no doubts about being disturbed, but also cases with possible psychosis, i.e., if they were unsure. At referral, THPs were asked to rate how likely they thought a diagnosis of psychotic disorder would be made, with response options “maybe disturbed” and “disturbed”. Thus, a rating of “maybe disturbed” did not reflect a definite view of the THP that psychosis was present, but rather the view that it might possibly be present without being sure. THPs did not refer people to the study who they felt confident were not disturbed.
Sociodemographic information was noted by research assistants including marital status, level of education (highest grade), occupational status, religious affiliation, race and primary language. Participants completed the Community Assessment of Psychic Experiences (CAPE) 16, a 42-item instrument for screening on subclinical psychotic symptoms in the general population. Whereas this is a self-report instrument, it had to be administered by trained research assistants, as the level of illiteracy is high in this area. The CAPE was translated into isiZulu and back translated according to WHO guidelines. The CAPE assesses frequency and distress of positive, negative and depressive (subclinical) symptoms, with 20, 14 and 8 items respectively. Response options range from “never” to “nearly always” (frequency) and “not” to “very” (distress). A symptom was rated as present if the frequency was “often” or “nearly always”. Distress was defined as a symptom associated with distress levels “quite” or “very”.
Next, a semi-structured diagnostic interview was conducted by one of the three Zulu psychiatrists in the research team (MS, NS and SS), all three being trained in biomedical psychiatry, fluent in English and isiZulu, and familiar with the Zulu culture. The Schedules for Clinical Assessment in Neuropsychiatry (SCAN 15) sections on mood disorders and psychotic disorders were used. The psychiatrists received a formal SCAN training by two experienced clinical psychiatrists (WV and HWH) to conduct this clinical diagnostic interview. A diagnostic classification according to the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV 22) was made for every participant during a consensus meeting of four psychiatrists (including author JKB), who were blind to THP rating and CAPE results.
Statistical analysis
Positive predictive value of the THP referrals was calculated as the proportion of referrals who received a SCAN diagnosis of psychotic disorder. In order to explore the understanding by THPs of the western concept of psychosis further, the predictive values of the separate THP probability ratings (“maybe disturbed” or “disturbed”) were calculated.
Analysis of Variance (ANOVA) was used to compare CAPE symptom scores between diagnostic groups (no diagnosis, psychotic disorder and non-psychotic psychiatric disorder). For each possible cut-off total symptoms score of the CAPE, sensitivity, specificity and predictive values were calculated of a SCAN diagnosis of psychotic disorder. Area Under the Curve (AUC) plots were made for total symptom scores as well as the three dimensions of the CAPE.
Results
During a 6-month period, 149 individuals were referred to the research team by THPs with possible recent onset psychosis. Of the 50 THPs who agreed to participate in the study and who attended the training, 15 referred at least one client participant. Sociodemographic characteristics of the sample are shown in Table 1. All participants had Black African race and had IsiZulu as their primary language.
Table 1.
Sociodemographic characteristics of the study sample.
| N* / Mean | % / SD | |
|---|---|---|
| Sex | ||
| Male | 79 | 53.0 |
| Female | 70 | 47.0 |
| Age, mean | 29.7 | 7.4 |
| Marital status | ||
| Single | 139 | 93.3 |
| Married** | 4 | 2.7 |
| Widowed | 1 | 0.7 |
| Level of education, mean grade (1–12) | 10.1 | 2.4 |
| Employment | ||
| Unemployed | 129 | 86.6 |
| Employed | 12 | 8.1 |
| Self-employed | 1 | 0.7 |
| Student | 2 | 1.3 |
| Religious affiliation | ||
| None | 38 | 25.5 |
| Christian | 106 | 71.1 |
Data is missing from five participants, except for sex.
Note that while only 2.7% were officially married, it is likely that a larger proportion were unofficially married but in traditionally recognized marriages. The latter are not included in official statistics but are very common within this particular context.
SCAN diagnoses
Sixty-six participants (44.3 %) had a diagnosis of any mood or psychotic disorder included in the SCAN, 83 (55.7 %) did not meet criteria for a disorder. Forty-four individuals (29.5%) were diagnosed with a psychotic disorder, nearly two-thirds of which were psychotic disorder not otherwise specified (NOS) (Table 2). Individuals with a psychotic disorder NOS diagnosis had at least one or some psychotic symptoms but did not meet DSM-IV criteria for a specific psychotic disorder. In many cases, individuals had persistent auditory hallucinations.
Table 2.
DSM-IV classifications.
| N | % | |
|---|---|---|
| Schizophrenia | 4 | 2.7 |
| Psychotic disorder NOS | 28 | 18.8 |
| Substance-induced psychotic disorder | 2 | 1.3 |
| Psychotic disorder due to a medical condition | 3 | 2.0 |
| Bipolar disorder with psychotic features | 0 | 0.0 |
| Depressive disorder with psychotic features | 7 | 4.7 |
| Depressive disorder | 14 | 9.4 |
| Dysthymic disorder | 1 | 0.7 |
| Depressive disorder NOS | 1 | 0.7 |
| Adjustment disorder | 4 | 2.7 |
| Substance abuse | 2 | 1.3 |
| No diagnosis | 83 | 55.7 |
Predicting diagnosis of psychotic disorder by THPs
As 44 from the 149 referrals received a SCAN diagnosis of a psychotic disorder, the positive predictive value of THP referrals was 29.5%. Ninety-three participants (62.4 %) were rated by the THPs as “maybe disturbed” and 56 (37.6 %) as “disturbed”. The positive predictive value of a “disturbed” rating was 53.8%. Of the “maybe disturbed” patients, 16 had a psychotic disorder, resulting in a positive predictive value of 17.2%.
CAPE scores and test characteristics
The number of positive, negative and depressive symptoms with and without distress and total number of symptoms are shown in Table 3. Depressive symptoms, but not positive, negative and total symptoms showed statistically significant differences across diagnostic groups (no diagnosis, psychotic disorder and non-psychotic psychiatric disorder), with the highest number of depressive symptoms in the people with non-psychotic disorders.
Table 3.
CAPE number of symptoms, by SCAN diagnosis.
| No diagnosis (N=83) |
Psychotic disorder (N=44) |
Non-psychotic psychiatric disorder (N=22) |
||||||
|---|---|---|---|---|---|---|---|---|
| Symptom score* | Mean | SD | Mean | SD | Mean | SD | F (df=2) | p-value |
| Positive symptoms | ||||||||
| All | 5.2 | 3.8 | 5.7 | 4.5 | 6.2 | 3.4 | 0.580 | 0.561 |
| With distress | 3.5 | 3.6 | 4.2 | 4.3 | 4.4 | 3.0 | 0.783 | 0.459 |
| Negative symptoms | ||||||||
| All | 3.1 | 2.9 | 4.4 | 3.5 | 3.9 | 3.4 | 2.661 | 0.073 |
| With distress | 2.4 | 3.0 | 3.5 | 3.5 | 2.9 | 3.3 | 1.500 | 0.227 |
| Depressive symptoms | ||||||||
| All | 2.0 | 2.1 | 2.8 | 2.4 | 3.2 | 2.1 | 3.616 | 0.029 |
| With distress | 1.8 | 2.1 | 2.9 | 2.5 | 3.0 | 2.1 | 4.683 | 0.011 |
| Total symptoms | ||||||||
| All | 10.0 | 7.5 | 12.9 | 10.0 | 13.3 | 7.6 | 2.316 | 0.103 |
| With distress | 7.8 | 7.8 | 10.6 | 9.4 | 10.2 | 7.3 | 1.956 | 0.145 |
Dichotomous symptom scores, symptom rated as present if frequency was “often” or “nearly always”. Symptom with distress if present with distress “quite” or “very”.
For all possible cut-off scores of the total CAPE score, sensitivity, specificity and predictive values were calculated for predicting diagnosis of psychotic disorder (Table 4). Even with a cut-off of 0, a sensitivity of 100% was not achieved. The best cut-off, that is, with the highest average of sensitivity and specificity, was 21, but the average score for this cut-off (0.6) was still poor.
Table 4.
Classification accuracy of CAPE total score a, psychotic disorder vs other/no diagnosis.
| CAPE cut- off, total score a |
Sensitivity | Specificity | PPV | NPV |
|---|---|---|---|---|
| 0 | 0.95 | 0.04 | 0.29 | 0.67 |
| 1 | 0.91 | 0.08 | 0.29 | 0.67 |
| 2 | 0.84 | 0.13 | 0.29 | 0.67 |
| 3 | 0.80 | 0.17 | 0.29 | 0.67 |
| 4 | 0.80 | 0.18 | 0.29 | 0.68 |
| 5 | 0.75 | 0.27 | 0.30 | 0.72 |
| 6 | 0.75 | 0.33 | 0.32 | 0.76 |
| 7 | 0.73 | 0.38 | 0.33 | 0.77 |
| 8 | 0.61 | 0.42 | 0.31 | 0.72 |
| 9 | 0.59 | 0.46 | 0.31 | 0.73 |
| 10 | 0.59 | 0.50 | 0.33 | 0.75 |
| 11 | 0.59 | 0.56 | 0.36 | 0.77 |
| 12 | 0.52 | 0.61 | 0.36 | 0.75 |
| 13 | 0.50 | 0.64 | 0.37 | 0.75 |
| 14 | 0.50 | 0.67 | 0.39 | 0.76 |
| 15 | 0.43 | 0.70 | 0.37 | 0.74 |
| 16 | 0.41 | 0.75 | 0.41 | 0.75 |
| 17 | 0.36 | 0.76 | 0.39 | 0.74 |
| 18 | 0.36 | 0.80 | 0.43 | 0.75 |
| 19 | 0.34 | 0.83 | 0.45 | 0.75 |
| 21 | 0.34 | 0.84 | 0.47 | 0.75 |
| 22 | 0.32 | 0.86 | 0.48 | 0.75 |
| 23 | 0.30 | 0.87 | 0.48 | 0.75 |
| 24 | 0.27 | 0.88 | 0.48 | 0.74 |
| 25 | 0.23 | 0.89 | 0.45 | 0.73 |
| 26 | 0.23 | 0.90 | 0.48 | 0.73 |
| 27 | 0.23 | 0.90 | 0.50 | 0.74 |
| 29 | 0.18 | 0.90 | 0.44 | 0.73 |
| 31 | 0.18 | 0.92 | 0.50 | 0.73 |
| 33 | 0.16 | 0.92 | 0.47 | 0.72 |
| 34 | 0.16 | 0.93 | 0.50 | 0.73 |
| 37 | 0.14 | 0.93 | 0.46 | 0.72 |
Total score of dichotomized frequency items of CAPE positive, negative and depressive symptoms. Item is rated as present if frequency is often or nearly always.
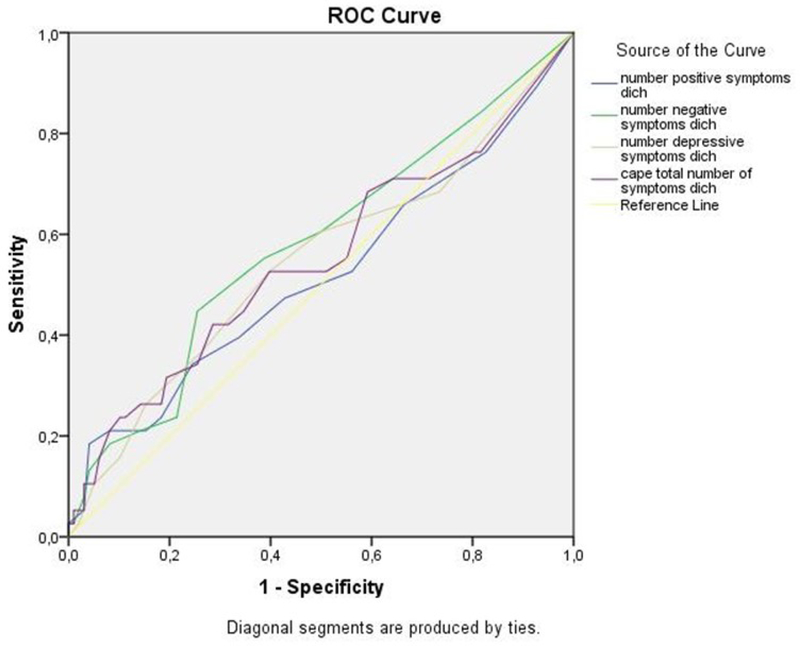
ROC curves were plotted for CAPE dimension scores to predict diagnosis of psychotic disorder (Figure 1). The AUC scores were 0.52 (95% CI, 0.40–0.64, p=0.73) for positive symptoms, 0.58 for negative symptoms (95% CI, 0.47–0.69, p=0.15), 0.55 for depressive symptoms (95% CI, 0.43–0.66, p=0.40) and 0.55 (95%CI, 0.43–0.67, p=0.37) for total symptoms. This can be interpreted to mean that CAPE predicted diagnosis of psychotic disorder hardly better than chance.
Figure 1.
Receiver Operating Curve, CAPE total symptoms as screening test for SCAN diagnosis of psychotic disorder versus other or no diagnosis.
Discussion
This pilot study in rural South Africa found that it is possible to identify patients with recent onset psychosis in collaboration with traditional health practitioners (THPs). We succeeded in establishing collaboration with regional THPs. Key to the successful collaboration between psychiatry, THPs and the local community, was the building of trust by recognizing and acknowledging local authorities, mutual respect for health constructs, taking time to find common ground, and adaptation of the procedures to sociocultural norms. THPs were willing to engage in the study and referred 149 patients in total. They were able to recognize recent onset psychosis, as 53.8% of patients they rated as “disturbed” received a diagnosis of psychotic disorder, opposed to only 17.2% of the patients they referred as “maybe disturbed”. The self-report CAPE did not perform well as a screening instrument for detecting psychotic disorder in this sample of patients referred by THPs with possible psychosis.
The high positive predictive value of THP referrals shows that it is certainly possible to develop some common understanding about western psychiatric concepts of psychosis with practitioners in a non-western context like THPs in KwaZulu Natal. THPs recognized “being disturbed” as a condition for which collaboration with psychiatric mental health care might be beneficial. As researchers of other recent projects also have noted 3,23, the prerequisite for such collaboration is building of trust, which takes long-term engagement and mutual respect. When these conditions are met, it seems feasible to build partnerships with THPs who are the primary health care providers in many areas where formal health care is virtually absent. Collaboration with THPs may open up opportunities to reduce the enormous treatment gap that exists for people with psychotic disorders in LMIC 24. Various models exist for collaboration between THPs and conventional mental health care. In a task shifting model, THPs could deliver components of conventional psychiatric treatment, e.g., administration and monitoring of antipsychotic medication, or social-psychiatric support. In a collaborative care model, THPs’ unique skills and advantages are acknowledged, THPs and mental health care function independently but in full cooperation. An integrative model implies a blended approach in which THP and conventional psychiatric care are combined in one service. Several examples of collaborative care between THPs and conventional health care in South Africa as well as elsewhere suggest that patients appreciate a collaborative approach and THPs are open to such collaboration 12,14. The results of this pilot study suggest that a similar collaboration is possible for patients with psychotic disorders.
We still do not know much about the epidemiology, clinical presentation, treatment and outcome of psychotic disorders in LMIC. It is important to study psychotic disorders in these countries, in the first place to advance mental health care infrastructures and to increase detection and access to care for patients who remain largely untreated. The few studies that investigated rates of psychotic disorders in LMIC were of different methodological quality and generally did not identify patients outside mental health care settings 3. It is therefore likely that most patients with psychotic disorder were still missed in these studies. A recent feasibility incidence study in India, Nigeria and Trinidad aimed to include not only mental health care providers but also healers and key informants 3,25. These researchers succeeded in establishing collaboration with THPs in some, but not all sites, partly due to lack of trust and because some THPs feared that the research team would take over their clients’ care. In our study, after establishing contact through the regional Traditional Council and careful searching for common ground, 50 THPs consented to participate, 30% of whom referred patients to the study.
Use of a screening instrument did not improve the positive predictive value of having a diagnosis of psychotic disorder in this population. The CAPE was designed for measuring psychotic experiences in the general population and has been successfully used as a screening tool for emerging psychosis in help-seeking populations 26,27. As it has not been validated as a screening instrument for psychotic disorders, CAPE may be too non-specific for this purpose. The CAPE items on positive psychotic experiences, however, are not very different from those in brief screening instruments such as the Psychosis Screening Questionnaire 28. We rated an experience only as present if it was associated with at least moderate distress, increasing the likelihood of being clinically meaningful. In our study, patients diagnosed with a psychotic disorder did not have higher scores on positive symptoms than patients with a non-psychotic psychiatric disorder, which suggests that the use of other screening instruments with similar items on positive psychotic symptoms would not have improved the test characteristics. Endorsement of positive items of the CAPE may reflect distress or affective dysregulation rather than psychosis risk. It may also be argued that the items of the CAPE should have been adapted to the local culture, but a study of a similar screening instrument that was culturally adapted, reported a poor sensitivity and a low positive predictive value of psychosis risk in Kenyan young adults 29. We intended to use the CAPE for screening purposes in a subsequent incidence study of psychotic disorders in Vulindlela, in order to enrich the sample and reduce the number of individuals needing in-depth diagnostic interviews. The results of this pilot study indicate that this would not be a useful strategy.
Finally, the study of psychotic disorders in LMIC is critical as this will increase our general global understanding of the nature of psychosis 25. Exposure to known environmental risk and protecting factors is quite different in LMIC compared with HIC, as a result of which novel factors may be discovered and psychopathological mechanisms unraveled. The sociocultural context influences clinical presentation, comorbidity, idioms of distress, pathways to care, explanatory models, treatment options, chances of recovery and long-term course of illness. This pilot study was a first step towards establishing a basis for further study of these issues in KwaZulu Natal; and as such, is an important step towards expanding our global understanding of psychotic disorder.
Strengths and limitations
An important strength of this study is the careful, step-by-step, culturally sensitive procedure of establishing partnerships between THPs and the research team. By involving local and professional authorities, the support for this project gradually increased, allowing organization of focus groups, establishing a community research advisory board and involving THPs in the project. Still, this pilot study is only a first step towards improving identification of people with psychotic disorders in this area. Fifty of the 200 THPs in the area consented to participate, and less than half of them referred patients to the study. We were not able to evaluate the study with the THPs, which makes any interpretation of these figures speculative. They may indicate mistrust to some extent. For this pilot study, however, we did not intend to include all THPs and not all 200 were necessarily made aware of the study (despite our efforts to invite all). Also, THPs who did not refer patients may not have seen patients meeting inclusion criteria during the study period. In our preparatory meetings with THPs, we learnt that many THPs have areas of specialist practice for which they become known and clients often take account of this in deciding whom to consult.
We focused on THPs as key health care providers, but it is certain that there are other informal care providers who play key roles. The regional Traditional Health council provided a list of all “bona fide” THPs, indicating that there are other, less trustworthy practitioners as well, collaboration with whom was deemed undesirable. Better identification of people with psychotic disorder in this rural part of South Africa also is likely to require collaboration with other local key informants with a good knowledge of their community, such as religious leaders, faith healers and police (see Labys et al 21 for a report on this aspect). Previous experiences in our and other regions show that these sources are open for collaboration with formal health care 30.
The diagnostic procedure was of high quality. Semi-structured SCAN interviews were conducted by trained local psychiatrists who were fluent in isiZulu and English. Diagnosis was made in consensus meetings of four psychiatrists, based on the SCAN reports. Risk of cultural misunderstanding and misdiagnosis was reduced. Notably, nearly two-thirds of individuals with psychosis were diagnosed with psychotic disorder NOS and this merits brief consideration. All such individuals manifested psychotic symptoms, but insufficient to meet diagnostic criteria for a specific psychotic disorder. Twenty of the 28 cases with psychotic disorder NOS had persistent auditory hallucinations without delusions. By extending case-finding outside mental health care, we may have detected patients in an early stage of psychosis. There is some evidence that hallucinatory experiences precede development of delusions, which may emerge as a consequence of the abnormal perceptual experiences 31,32. In non-Western contexts, clinical characteristics and course of psychotic disorders may differ from patterns in Western countries. Hallucinatory experiences may less often be perceived as abnormal, thus preventing subsequent development of delusions. Also, other types of psychosis, such as acute non-affective remitting psychosis, may be more common in non-Western countries 33. Finally, there may have been selection bias in referrals by THPs. Hallucinations may be more easy to detect and associated with psychosis than delusional ideas, negative symptoms and disorganization, resulting in selective referral of cases with hallucinations.
Conclusion
Traditional health practitioners were open to identifying and referring individuals with possible psychosis. They recognized “being disturbed” as a condition for which collaboration with psychiatric mental health care might be beneficial. Collaboration between mental health care and THPs is a promising method to identify patients with recent onset psychosis in rural South Africa. This approach may lead to improvement of regional mental health care infrastructures, and provides opportunities to gain more insight into the epidemiology, aetiology and treatment of psychotic disorders.
Acknowledgments
Funding:
Research in this publication was supported by the National Institute of Mental Health under award R21MH93298 (recipient ES). AT was supported by SA MRC Flagship grant (MRC-RFA-UFSP-01-2013/UKZN HIVEPI) and NIH Research Training Grant (R25TW009337), funded by the Fogarty International Center and the National Institute of Mental Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding bodies.
Footnotes
Conflict of interest:
None.
References
- 1.Jablensky A, Sartorius N, Ernberg G, et al. Schizophrenia - Manifestations, Incidence and Course in Different Cultures - a World-Health-Organization 10-Country Study. Psychol Med 1992:1–97. doi:Article. [DOI] [PubMed]
- 2.Kebede D, Alem A, Shibre T, Negash A, Deyassa N, Beyero T. The sociodemographic correlates of schizophrenia in Butajira, rural Ethiopia. Schizophr Res. 2004;69(2–3):133–141. doi: 10.1016/S0920-9964(03)00089-6. [DOI] [PubMed] [Google Scholar]
- 3.Morgan C, John S, Esan O, et al. The incidence of psychoses in diverse settings, INTREPID (2): A feasibility study in India, Nigeria, and Trinidad. Psychol Med 2016;46:1923–1933. doi: 10.1017/S0033291716000441. [DOI] [PubMed] [Google Scholar]
- 4.Burns JK, Esterhuizen T. Poverty, inequality and the treated incidence of first-episode psychosis: an ecological study from South Africa. Soc Psychiatry Psychiatr Epidemiol 2008;43(4):331–335. doi: 10.1007/s00127-008-0308-2. [DOI] [PubMed] [Google Scholar]
- 5.Williams DR, Herman A, Stein DJ, et al. Twelve-month mental disorders in South Africa: prevalence, service use and demographic correlates in the population-based South African Stress and Health Study. Psychol Med 2008;38:(02). doi: 10.1017/S0033291707001420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bekele YY, Flisher AJ, Alem A, Baheretebeb Y. Pathways to psychiatric care in Ethiopia. Psychol Med 2009;39(03):475. doi: 10.1017/S0033291708003929. [DOI] [PubMed] [Google Scholar]
- 7.Adeosun II, Adegbohun AA, Adewumi TA, Jeje OO. The Pathways to the First Contact with Mental Health Services among Patients with Schizophrenia in Lagos, Nigeria. Schizophr Res Treatment 2013;2013:769161. doi: 10.1155/2013/769161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Odinka PC, Oche M, Ndukuba AC, et al. The Socio-demographic Characteristics and Patterns of Help-Seeking among Patients with Schizophrenia in South-east Nigeria. J Health Care Poor Underserved 2014;25(1):180–191. doi: 10.1353/hpu.2014.0055. [DOI] [PubMed] [Google Scholar]
- 9.Peltzer K, Mngqundaniso N, Petros G. A controlled study of an HIV/AIDS/STI/TB intervention with traditional healers in KwaZulu-Natal, South Africa. AIDS Behav 2006;10(6):683–690. doi: 10.1007/s10461-006-9110-x. [DOI] [PubMed] [Google Scholar]
- 10.Audet CM, Salato J, Blevins M, Amsalem D, Vermund SH, Gaspar F. Educational Intervention Increased Referrals to Allopathic Care by Traditional Healers in Three High HIV-Prevalence Rural Districts in Mozambique. PLoS One 2013;8:(8). doi: 10.1371/journal.pone.0070326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sorsdahl K, Stein DJ, Flisher AJ. Traditional healer attitudes and beliefs regarding referral of the mentally ill to Western doctors in South Africa. Transcult Psychiatry 2010;47(4):591–609. doi: 10.1177/1363461510383330. [DOI] [PubMed] [Google Scholar]
- 12.Abbo C Profiles and outcome of traditional healing practices for severe mental illnesses in two districts of Eastern Uganda. Glob Health Action 2011;4. doi: 10.3402/gha.v4i0.7117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Patel V Traditional healers for mental health care in Africa. Glob Health Action 2011;4. doi: 10.3402/gha.v4i0.7956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sorsdahl K, Stein DJ, Grimsrud A, et al. Traditional healers in the treatment of common mental disorders in South Africa. J Nerv Ment Dis 2009;197(6):434–441. doi: 10.1097/NMD.0b013e3181a61dbc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wing JK, Babor T, Brugha T, et al. SCAN: Schedules fonr Clinical Assessment in Neuropsychiatry. Arch Gen Psychiatry 1990;47(6):589–593. doi:10.1001. [DOI] [PubMed] [Google Scholar]
- 16.Konings M, Bak M, Hanssen M, van Os J, Krabbendam L. Validity and reliability of the CAPE: a self-report instrument for the measurement of psychotic experiences in the general population. Acta Psychiatr Scand 2006;114(1):55–61. doi: 10.1111/j.1600-0447.2005.00741.x. [DOI] [PubMed] [Google Scholar]
- 17.Burns JK. The burden of untreated mental disorders in KwaZulu-natal province - mapping the treatment gap. South African J Psychiatry 2014;20(1):6–10. doi: 10.7196/SAJP.499. [DOI] [Google Scholar]
- 18.MacQueen KM, Karim QA. Practice Brief: Adolescents and HIV Clinical Trials: Ethics, Culture, and Context. J Assoc Nurses AIDS Care 2007;18(2):78–82. doi: 10.1016/j.jana.2007.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.de Oliveira T, Kharsany ABM, Gräf T, et al. Transmission networks and risk of HIV infection in KwaZulu-Natal, South Africa: a community-wide phylogenetic study. Lancet HIV 2017;4(1):e41–e50. doi: 10.1016/S2352-3018(16)30186-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abdool KQ, Abdool Karim SS, Frohlich J a, et al. Effectiveness and safety of tenofovir gel, an antiretroviral microbicide, for the prevention of HIV infection in women.[Erratum appears in Science. 2011 Jul 29;333(6042):524]. Science (80- ) 2010;329(2010):1168–1174. doi: 10.1126/science.1193748.Effectiveness. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Labys CA, Susser E, Burns JK. Psychosis and help-seeking behavior in rural KwaZulu Natal: unearthing local insights. Int J Ment Health Syst 2016;10(1):57. doi: 10.1186/s13033-016-0089-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders Washington DC: American Psychiatric Association; 2000. doi: 10.1016/B978-1-4377-2242-0.00016-X. [DOI] [Google Scholar]
- 23.Musyimi CW, Mutiso VN, Nandoya ES, Ndetei DM. Forming a joint dialogue among faith healers, traditional healers and formal health workers in mental health in a Kenyan setting: towards common grounds. J Ethnobiol Ethnomed 2016;12(1):4. doi: 10.1186/s13002-015-0075-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gureje O, Nortje G, Makanjuola V, Oladeji BD, Seedat S, Jenkins R. The role of global traditional and complementary systems of medicine in the treatment of mental health disorders. The Lancet Psychiatry 2015;2:168–177. doi: 10.1016/S2215-0366(15)00013-9. [DOI] [PubMed] [Google Scholar]
- 25.Morgan C, Hibben M, Esan O, et al. Searching for psychosis: INTREPID (1): systems for detecting untreated and first-episode cases of psychosis in diverse settings. Soc Psychiatry Psychiatr Epidemiol 2015;50:879–893. doi: 10.1007/s00127-015-1013-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mossaheb N, Becker J, Schaefer MR, et al. The Community Assessment of Psychic Experience (CAPE) questionnaire as a screening-instrument in the detection of individuals at ultra-high risk for psychosis. Schizophr Res 2012;141(2–3):210–214. doi: 10.1016/j.schres.2012.08.008. [DOI] [PubMed] [Google Scholar]
- 27.Kline E, Schiffman J. Psychosis risk screening: A systematic review. Schizophr Res 2014;158(1–3):11–18. doi: 10.1016/j.schres.2014.06.036. [DOI] [PubMed] [Google Scholar]
- 28.Bebbington P, Nayani T. The Psychosis Screening Questionnaire. Int J Methods Psychiatr Res 1995. doi: 10.1037/t30040-000. [DOI] [Google Scholar]
- 29.Owoso A, Ndetei DM, Mbwayo AW, Mutiso VN, Khasakhala LI, Mamah D. Validation of a modified version of the PRIME screen for psychosis-risk symptoms in a non-clinical Kenyan youth sample. Compr Psychiatry 2014;55(2):380–387.doi: 10.1016/j.comppsych.2013.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Burns JK, Tomita A. Traditional and religious healers in the pathway to care for people with mental disorders in Africa: a systematic review and meta-analysis. Soc Psychiatry Psychiatr Epidemiol 2015;50:867–877. doi: 10.1007/s00127-014-0989-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Krabbendam L, Myin-Germeys I, Hanssen M, et al. Hallucinatory experiences and onset of psychotic disorder: Evidence that the risk is mediated by delusion formation. Acta Psychiatr Scand 2004;110:264–272. doi: 10.1111/j.1600-0447.2004.00343.x. [DOI] [PubMed] [Google Scholar]
- 32.Smeets F, Lataster T, Dominguez MDG, et al. Evidence that onset of psychosis in the population reflects early hallucinatory experiences that through environmental risks and affective dysregulation become complicated by delusions. Schizophr Bull 2012;38:531–542. doi: 10.1093/schbul/sbq117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Susser E, Wanderling J. Epidemiology of Nonaffective Acute Remitting Psychosis vs Schizophrenia: Sex and Sociocultural Setting. Arch Gen Psychiatry 1994;51:294–301. doi: 10.1001/archpsyc.1994.03950040038005. [DOI] [PubMed] [Google Scholar]