Abstract
Objective.
To develop an educational mobile application (app) for expectant parents diagnosed with risk factors for premature birth.
Methods.
Parent and medical advisory panels delineated the vision for the app. The app helps prepare for preterm birth. For pilot testing, obstetricians offered the app between 18–22 weeks gestational age to English speaking parents with risk factors for preterm birth. After 4 weeks of use, each participant completed a questionnaire. The software tracked topics accessed and duration of use.
Results.
For pilot testing, 31 participants were recruited and 28 completed the questionnaire. After app utilization, participants reported heightened awareness of preterm birth (93%), more discussion of pregnancy or prematurity issues with partner (86%), increased questions at clinic visits (43%), and increased anxiety (21%). Participants reported receiving more prematurity information from the app than from their healthcare providers. The 15 participants for whom tracking data was available accessed the app for an average of 8 hours.
Conclusion.
Parents with increased risk for preterm birth may benefit from this mobile app educational program.
Keywords: high-risk pregnancy, Medical complications of pregnancy, premature infant, Prenatal Care
1. Introduction
One in every ten infants in the U.S. is born prematurely at <37 weeks gestational age (GA) [1]. Preterm infants are more likely than full-term infants to die or develop long term health challenges [2–7]. According to one estimate, half of all U.S. premature births have associated risk factors [8]. Despite prenatal identification, parents with risk factors first receive prematurity education when the mother is hospitalized for preterm birth [9,10]. This “last minute” education is not ideal since parental learning during hospitalization is compromised by labor, anxiety, and medications [11–15]. Lack of prenatal prematurity education leaves parents unprepared to make informed healthcare choices before and during the preterm birth hospitalization [16–19].
There are several reasons for the current lack of prematurity education during prenatal visits. First, obstetric healthcare providers are hesitant to provide premature infant health outcome information to parents, especially regarding neurodevelopmental outcomes [20, 21]. Secondly, obstetric healthcare providers are reluctant to risk frightening pregnant women with discussions of potential neonatal death and disability, since most pregnancies will not result in a preterm birth [22]. Finally, there is concern that the parents will not be receptive to anticipatory education unless the threat of preterm birth is a “clear and present danger” [23].
Several public health websites list preterm birth associated risk factors [1, 24]. Preterm births may be classified as spontaneous or medically indicated. Risk factors for spontaneous preterm birth include a prior spontaneous preterm birth and short cervical length [25]. Risk factors for medically indicated preterm birth include intrauterine growth restriction, chronic hypertension and history of preeclampsia [26]. Most parents do not currently receive comprehensive prematurity education at the time of identification of preterm birth associated risk factors [9].
Text4baby is the first national mobile health service in the United States that aims to provide information to pregnant women to help improve health outcomes. More than 320,000 participants enrolled in the program between 2010 and 2012 [27]. The “Text4baby” service models how smartphone technology can successfully address the challenges of prenatal education, health literacy and reaching parents from underserved communities regarding routine pregnancy care [28]. Similar interventions in maternal and newborn healthcare have also been reported from abroad [29]. A smartphone-based prematurity education program that provides anticipatory guidance to parents with preterm birth associated risk factors may enhance the quality of parental healthcare decisions and improve prematurity care.
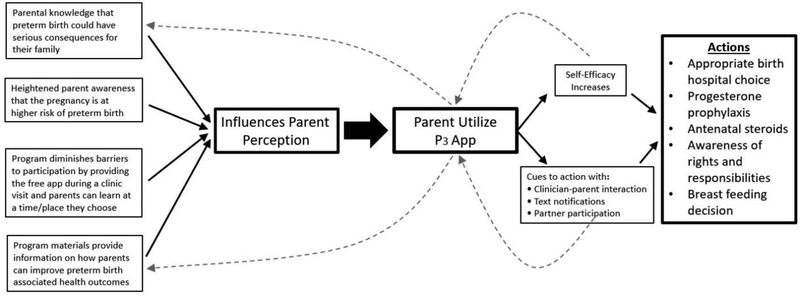
The Health Belief Model suggests that a prematurity education program can be successful if: 1) parents believe they are at risk of preterm birth, 2) parents recognize that the preterm birth could seriously affect their lives, 3) the educational program informs parents how they can improve outcomes, 4) participation in the program is easy, 5) program provides cues to parental action, and 6) program enhances parental self-efficacy [30]. Our hypothesis is that a Health Belief Model based smartphone parent education program that is recommended by obstetric healthcare providers at the time of diagnosis of a preterm birth risk factor, will engage and prepare parents without adding undue anxiety [31].
2. Methods
Two objectives were set for the study: 1) Develop an educational multimedia mobile application (app) for parents at risk for preterm birth and 2) Pilot the mobile app and test feasibility of the concept in a group of expectant parents diagnosed to be at increased risk of preterm birth. We first assembled a study team with expertise in mobile health, health literacy, neonatology, and maternal-fetal medicine, as well as a parent advocate. Weekly to biweekly meetings delineated the vision of the app. To ensure that the educational content was relevant and appropriate, both a medical advisory panel (obstetric, neonatology and maternal-fetal medicine providers) and a parent advisory panel (four mothers and one father of preterm infants) were formed and consulted throughout app development. Based on parental input, the app was named “Preemie Prep for Parents (P3) mobile app.” The Institutional Review Board (IRB) approved the study.
Development of the P3 app:
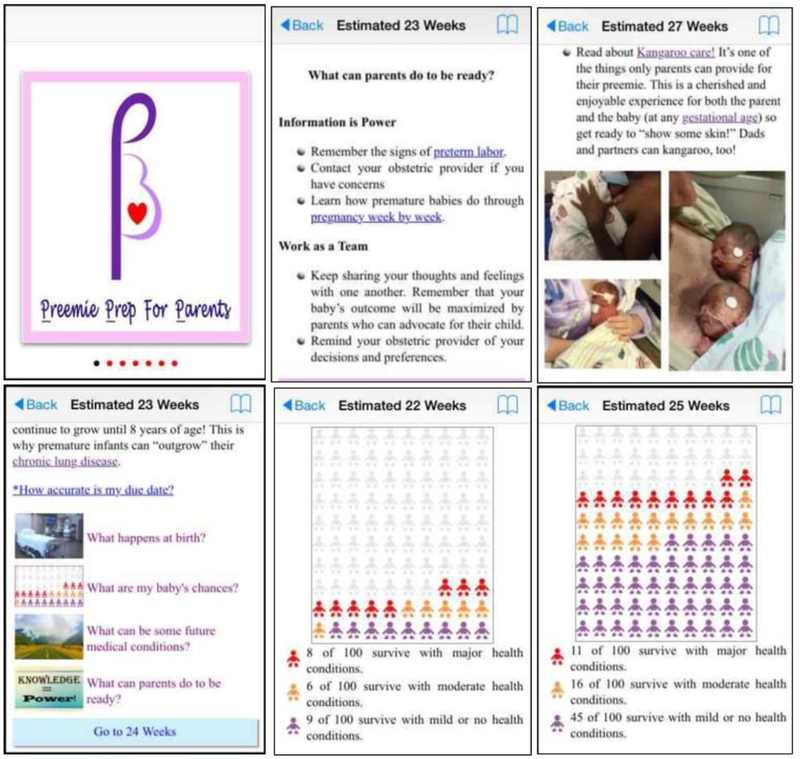
Educational content is determined using published literature and input from the two advisory panels [17, 32]. The information domains include: 1) medical knowledge, 2) preparedness for preterm birth, 3) parent emotional health, 4) advocacy for themselves and their unborn child, and 5) partnership with their significant other and/or physician. Educational content is organized in a week-by-week format for 18 to 33 weeks GA and includes fetal growth and development, introduction to the levels and capabilities of neonatal intensive care units (NICUs), and signs and treatment of preterm labor. A library containing pictures of premature infants at various GA and information on organ-based neonatal conditions is included. The app utilizes published national premature infant health outcome data with the option for centers to add their specific data [33]. The GA specific chances of survival and morbidity are presented with interactive icon array pictographs. Representative screen shots from the P3 app are shown in Figure 1.
Fig. 1.
Screen shots of the Preemie Prep for Parents (P3) mobile app. Top left: Logo designed by parents and providers for the mobile app Top center: An example of anticipatory guidance provided to parents Top right: An example of information that encourages parental involvement Bottom left: Page for parents who are at 23 weeks gestation. Bottom center: A pictograph showing neonatal outcome at 22 week gestation Bottom right: A pictograph showing neonatal outcome at 25 week gestation
Patient education best practices and health literacy principles are utilized throughout the app to maximize comprehension and learning [34]. Based on the Health Belief Model the app motivates the user by providing cues to action via text notifications including achieved pregnancy milestones, encouraging statements and informational pearls (Table1) [30]. Information is presented through interactive pictographs, pictures, visual-aids, and both instructional and real-life videos. The app is designed to be motivational and personalized to the user. For example, the parent enters his/her name, gender of the fetus, due date and has the option to upload personal pictures, including ultrasound images.
Table 1.
Sample text notifications sent via the P3 mobile app to parents with identified preterm birth associated risk factors
| [Participant’s first name], did you know? A “full-term” pregnancy lasts 280 days or 40 weeks from the first day of the last menstrual period. Click Next to learn more. |
| [Participant’s first name], did you know? Babies are most healthy when they are born between 39 weeks and 0 days to 40 weeks and 6 days. Click Next to learn more. |
| [Participant’s first name], did you know? Important medical decisions for you and your baby are based on the due date. An ultrasound in the first 13 weeks (first trimester) is the most accurate estimate but can still be off by 5–7 days. Click Next to learn more. |
| [Participant’s first name], it is important that you know that current medical technology can only help certain premature babies. Click Next to learn more. |
| [Participant’s first name], did you know? The length of the pregnancy is not the only factor that determines how a baby will do after birth. Click Next to learn more. |
| [Participant’s first name], did you know? Premature babies, seem to be developed on the outside but they may not be fully functioning on the inside. Click Next to learn more. |
| [Participant’s first name], it is important that you know the signs and symptoms of preterm labor. Call your doctor right away if you notice any of these. Click Next to learn more. |
| [Participant’s first name], did you know? Preterm babies born before 28 weeks of pregnancy have more complications. Click Next to learn more. |
| [Participant’s first name], did you know? All premature babies born before 34 weeks of pregnancy require specialized care in the neonatal intensive care unit (NICU). Click Next to learn more. |
| [Participant’s first name], did you know? Premature babies have the best outcomes when both the medical team and parents work together. Want to know what you can do to help? Click Next to learn more. |
| [Participant’s first name], did you know? Premature babies need special medical care immediately after birth. Click Next to learn more. |
The P3 app pilot and feasibility testing:
We set a recruitment goal of 30 participants for the pilot study. The two recruitment sites included an academic health center and an obstetric private practice clinic. Enrollment criteria included: English literate, ≥18 years of age, increased risk for preterm birth as determined by the patient’s obstetric provider, 18–22 weeks GA at enrollment, absence of known fetal anomalies, possession of a personal smartphone, and no plan to change mobile service provider, upgrade phone or travel outside the country during the study period (4 weeks). The enrollment GA window was selected to allow enough time for parents to review the app prior to possible birth at a GA when neonatal resuscitation is an option. Potential participants were identified by the obstetric provider who also informed the patient (and partner) of the availability of the P3 app. A study team member met with interested patients (and partner) during a routine visit to obtain informed consent. Depending on participant preference, the app was either downloaded by the study team onto the participant’s smartphone or a link and unique password were provided to the participant to download the app later. Once downloaded, remote tracking of the app’s use began. Study limitations required that each participant’s use of the app be limited to 4 weeks after enrollment or up to the time of delivery, whichever occurred first. The P3 app is iOS and Android compatible and was available on the Apple App Store and Google Play Store for the study. Downloading of the app was password restricted to only allow access by study participants. The P3 app also tracks an individual participant’s use. Tracked data includes time spent using the app, topics visited, and time spent on each topic.
A 15-item entry survey was given to collect participant demographics, prior use of mobile apps, and obstetric history. At study completion, a 45-item exit survey was given to collect feedback regarding the app’s educational content, features, and usability. Both surveys were tested for readability and comprehension by the medical and parent advisory panels. The items required a yes or a no response and open-ended comments and suggestions were collected. Data from the surveys were entered in a spreadsheet and cross checked for accuracy. At the end of the study, monetary compensation was provided to each participant in appreciation of their time.
3. Results
The development of the P3 mobile app began in April 2015. The parent and medical advisory panels met separately for a total of 8 meetings to refine app content and presentation. For the pilot trial, 57 potential participants were screened, 32 were study eligible, 31 consented and 28 (10 fathers and 18 mothers) completed the exit survey. Participant demographics are presented in Table 2. The most common risk factors for preterm birth included prior spontaneous preterm birth and multifetal gestation. The median GA at enrollment was 20 (range, 18–22) weeks. Twenty participants were part of a mother/father pair. The majority (56%) of the mothers already had a pregnancy app on their phone at enrollment while none of the fathers had a pregnancy app. Participants (71%) reported using mobile apps regularly and the majority (64%) were Android users.
Table 2.
Demographics, n=28 (18 mothers and 10 fathers)
| Variable | |
|---|---|
| Age, mean(SD) years | 32 ± 5 |
| Reproductive history | |
| Gestational age week at enrollment, median (range) | 20 (18–22) |
| Number of prior pregnancies, median (range) | 3 (1–6) |
| Number of prior live births, median (range) | 1 (0–5) |
| Risk factor for preterm birth, n=14a | |
| Multiple gestation | 5 |
| Previous preterm delivery | 5 |
| Shortened cervix | 2 |
| Lupus | 1 |
| Anti-Kell | 1 |
| Race (%) | |
| Caucasian | 71 |
| African-American | 21 |
| Hispanic | 4 |
| Asian | 4 |
| Education (%) | |
| High school | 24 |
| College | 44 |
| Postgraduate | 32 |
| Smartphone | |
| Android phone (%) | 64 |
| Number of apps on phone, median (range) | 15 (0–60) |
| Has a pregnancy app on their phone (%) | |
| Fathers, n=10 | 0 |
| Mothers, n=18 | 56 |
| Frequency of app use in general (%) | |
| Sometimes | 29 |
| All the time | 71 |
Data missing for 4 of the 18 pregnancies
Since most mothers delivered after the 4-week study period, GA at birth is known for 15 of the 18 mothers, with 6 (40%) experiencing preterm birth between 22 and 36 weeks. All participants who completed the study (n=28) reported that the app provided important, new information and they believed access to the app would be beneficial for families. The exit survey items and participant responses are presented in Table 3. The vast majority of participants (94%) reported that the app improved and enhanced their medical knowledge and preparedness. They reported receiving more information from the app in areas of preterm labor, premature infants and parental role and responsibilities, than from their healthcare provider. One parent commented, “Prior to being part of this study, my husband and I toured NICUs, talked to neonatologists and researched online for info. Had we had access to this app earlier in our pregnancy this would have given us reliable, trustworthy information and eased our minds sooner, just because we knew what to expect sooner. I think this will be SO beneficial for families in similar situations in the future.” Another parent who delivered at 26 weeks GA stated, “I was hoping I can continue to use the app as it has been very helpful both before I delivered and now with the NICU experience.” Another comment was, “The week by week information on how my baby was developing at each gestational age was my favorite!” One study mother who presented for delivery at 22 weeks GA utilized the app pictograph (Figure 1) on her smartphone during the shared decision-making process to advocate for resuscitation and respond to medical team’s concern for poor developmental outcome.
Table 3.
Exit-survey items and participant responses
| Yes (%) | ||
|---|---|---|
| Medical knowledge | ||
| 1. | Did the app provide new information to you? | 100 |
| 2. | Was some of the information given in the app important for you to know? | 100 |
| 3. | Because of the app, do you feel better prepared if you were to have a premature infant? | 100 |
| 4. | Did the app answer at least some of your questions about premature infants? | 100 |
| 5. | In your opinion, will this app benefit families? | 100 |
| 6. | Did the app help you learn about what happens in the delivery room? | 79 |
| 7. | Did the app inform you about the NICU? | 96 |
| 8. | Did the app inform you about difficulties that a premature baby may face at birth? | 89 |
| Emotional health | ||
| 1. | Did the app make you feel more aware of your risk for having a premature delivery? | 93 |
| 2. | Did the app increase your anxiety unnecessarily? | 14 |
| 3. | As time passed and you were familiar with the information provided, did the app increase your anxiety about having a premature infant later? | 21 |
| Partnership and Advocacy | ||
| 1. | Because of the app, did you ask more questions at your doctor visits? | 43 |
| 2. | Because of the app, did you and your partner discuss pregnancy or prematurity issues? | 86 |
| 3. | Did you share information given in the app with other family/friends (excluding a partner already enrolled in the study)? | 57 |
| Content and desire for information | ||
| 1. | Did the app give too much information about premature infants? | 18 |
| 2. | The information in the library was not enough. | 46 |
| 3. | Did you learn something new from the videos showing an actual resuscitation of a newly born premature infant in the delivery room? | 54 |
| 4. | The information about medical equipment NICU was not helpful. | 25 |
| 5. | I liked the week by week information on how my baby was developing at each gestational age. | 100 |
| 6. | Information on major and moderate health conditions faced by premature infants should be removed from the app. | 89 |
In the areas of partnership and advocacy, 86% of participants reported discussions regarding prematurity issues with their partner as a result of app utilization. Fifty-seven percent shared the app information with friends and other family members. When asked “Which source gave you more information about the role of parents of premature infants during hospitalization?”, 79% reported the app provided them more information than their healthcare provider. Only 43% of the participants reported asking more questions during their obstetric visits. One participant suggested adding a “section for questions to ask your doctor, a pre-written list AND ability to add own questions with reminders for time of appointment.” One father commented, “I would have liked if the app addressed me (instead of my wife) and addressed more of a father’s role and what I can specifically do. Overall loved the app though!.”
When examining effects on parental emotional health, most (93%) parents reported heightened awareness of their risk of preterm birth. With app use, a minority of the parents (21%) reported anxiety about having a premature infant. One participant suggested “more information on the long-term effects.” Another suggested adding “success stories of premature babies that are of different ages so that it may provide some hope for parents.”
Participant ratings of the features of the P3 mobile app are presented in Table 4. The majority (89%) of the parents responded positively to the use of text notifications. The main area of improvement was in app functionality. One parent said, “At first it took me a while to click “More Details” on the notifications to read more details. It just didn’t stand out to me.” Other comments included, “The look of the app (needs improvement) and more functionality,” and “I think the app should have more videos.” Twenty-three participants gave information regarding where they used the app, with 61% identifying only home utilization and the remainder identifying home and work utilization.
Table 4.
Participant rating of Preemie Prep for Parents (P3) mobile app features, n=28
| Percent | ||||||
|---|---|---|---|---|---|---|
| Poor | Low | Average | Good | Excellent | ||
| 1. | Rate your overall experience with this app. | 0 | 4 | 10 | 43 | 43 |
| 2 | Rate how easy it was to use the app. | 0 | 0 | 7 | 50 | 43 |
| 3 | Rate how well you were able to understand the information. | 0 | 0 | 4 | 32 | 64 |
| 4 | Rate the audio explanations of the app. | 7 | 4 | 19 | 33 | 37 |
| 5 | Rate the video/visual aids of the app. | 0 | 6 | 0 | 47 | 47 |
| 6 | Rate the “look” of the app. | 0 | 21 | 29 | 25 | 25 |
| 7 | Rate how reliably the app functioned. | 4 | 0 | 18 | 25 | 53 |
| 8 | Rate your learning experience with the app. | 0 | 4 | 4 | 52 | 40 |
| 9 | Rate how trustworthy you felt the information was. | 0 | 0 | 11 | 18 | 71 |
| 1 | How do you rate the options to personalize the app to you and your baby? | 0 | 14 | 21 | 39 | 26 |
| 0 | ||||||
| 1 | Rate how well the app kept your attention. | 4 | 7 | 29 | 18 | 42 |
| 1 | ||||||
| 1 | Rate how well the app encouraged you to learn more about prematurity. | 0 | 7 | 21 | 29 | 43 |
| 2 | ||||||
| 1 | Rate how well you liked the color scheme of the app. | 0 | 7 | 36 | 32 | 25 |
| 3 | ||||||
| 1 | Rate how well you liked the “Feedback questions” that popped up throughout the app. | 0 | 14 | 14 | 41 | 31 |
| 4 | ||||||
Due to unforeseen app tracking limitations, partial app utilization data are available for 15 of the 28 participants. Over the 4-week study period, the app was accessed for an average of 8 hours by the 15 participants, with user-specific range of 6 minutes to 14 hours. The most accessed module included week-by-week information regarding GA-specific problems and outcomes of premature infants. The second most accessed module included maternal care information regarding route of delivery, delivery room care for preterm births, interventions to stop premature labor, and fetal monitoring. The third most accessed module included general pregnancy information regarding duration of a normal pregnancy, due date accuracy, full-term vs. preterm pregnancy, signs of preterm labor, and risk factors for preterm birth.
4. Discussion and Conclusion
4.1. Discussion
The 2014 National Institute of Child Health and Human Development (NICHD) workshop on management and counseling at periviable gestation identified several issues that still remain unresolved, including timing of parental prematurity counseling. The expert panel acknowledged that birth hospitalization is not an ideal time for parents to receive new medical information as the “healthcare team and the family must quickly make complex, ethically challenging decisions - often in an emotionally charged setting” [32]. A mother featured in a publication regarding extreme premature birth reported “most of the information that I received was at 3 AM when I was in premature labor- you only hear bits and pieces” [35]. While other families have stated that readily accessible, pertinent, and understandable information is requisite for family centered neonatal care [36, 37]. We developed the P3 mobile app to provide parents a foundation of knowledge before the preterm birth hospitalization. Pilot users reported feeling better prepared for a preterm birth and receiving more prematurity information from the app as compared to their obstetric healthcare provider. Most users reported heightened awareness of risk of preterm birth and a small proportion of participants reported increase in anxiety, but overall, the app made participants feel better informed. These preliminary findings suggest that a smartphone parent education program may benefit pregnancies at risk of preterm birth.
Improved knowledge before preterm birth hospitalization can help parents influence healthcare decisions that impact prematurity health outcomes [38]. For example, appropriate choice of birth hospital will optimize care in the first postnatal hour, also known as the “Golden Hour.” Studies show that evidence based care in the first postnatal hour reduces hypothermia, hypoglycemia, intraventricular hemorrhage, chronic lung disease and retinopathy of prematurity in preterm infants [39]. Other examples of decisions that improve preterm health outcomes include breast feeding and progesterone prophylaxis [40–43]. If pregnancy ultimately does result in preterm birth hospitalization, parents can also benefit from better understanding of periviability GA health outcomes, options and complexities of neonatal delivery room care, and awareness of expected parental role in medical decision making [32].
We believe that having the obstetric healthcare provider recommend the app to the parents is important for program success as studies show that mere knowledge of having a preterm birth risk factor is not associated with higher parental perceived risk of preterm birth [44, 45]. This patient-clinician interaction then serves as the trigger for parental action. Cues to action are also provided via 3–5/week text messages and from the partner’s use of the P3 app. The educational content, design and convenient availability of the P3 app decreases barriers and encourages self-efficacy. Figure 2 shows the characteristics of the smartphone prenatal prematurity education program with reference to the Health Belief Model.
Fig. 2.
P3 mobile app anticipatory prematurity education program theoretical model
A strength of the P3 app is that it allows families to learn and deliberate management and treatment options at their own pace. This is important as decisions made without adequate opportunity to discuss and contemplate the choices can result in suboptimal “gut reaction” decisions. Family deliberation is especially important for preterm birth decision making as research reveals that for high risk decisions the preference is to share the burden of decision making with the other parent [46]. Most P3 app users reported that because of the app they discussed pregnancy and prematurity issues with their partner and shared information with other family members.
The P3 app provides evidence-based information independent of the healthcare professional who counsels the parents at the time of hospitalization. Some parents who have experienced shared medical decision making reported feeling that healthcare providers present information in a manner that encourages parents to agree with the healthcare provider recommendations [46, 47]. The experience of the 22-week GA mother, referenced in the results, highlights how the P3 app can empower parents to effectively advocate their treatment preference to the medical team. We envision that the smartphone based education will supplement and not replace the information parents receive during preterm birth hospitalization. However, we hypothesize that parents already familiar with the P3 app information will better comprehend the more specific medical facts provided by clinicians during the hospitalization and be able to make better informed medical care decisions.
According to Pew Research, 91% of U.S. adults of child-bearing age own a smartphone, and 63% with lower income (<30K) use their smartphone to get health information [48, 49]. This should allow for wide dissemination of the P3 app materials, especially because preterm birth is more common among those with the lower socioeconomic status (African-American decent, unmarried and not living with the partner, and teenage motherhood) [50, 51]. Printed educational aids have also been tested by us and other investigators [31, 52-55]. Despite benefit in limited trials, printed aids have failed to have a wide impact due to maintenance and dissemination difficulties. In a study, 81% of parents with preterm birth reported using their smartphones for information, significantly more than brochures (33%) or books (56%) [50]. Multimedia information is also more effective than printed information [56, 57]. One of our participants commented in the exit survey “It’s important to always keep (the information) up to date.” Unlike printed educational-aids, the P3 app can be updated centrally and distributed universally. These qualities make the P3 app program easily scalable and suitable for wider implementation.
Mobile smartphone technology can remotely track use of educational materials. Tracking of self-directed learning will identify information valued by families as they prepare for preterm birth. Currently, there is controversy regarding whether neonatal mortality and morbidity data is valued by parents, as some studies suggest that parents base their decisions on religious and/or cultural values [58, 59]. Unfortunately, usage data was lost for some of our pilot participants due to problems in device-server syncing of data; however, this technical limitation has been addressed and we will be able to gather more P3 app usage information in a future trial. This will inform future educational materials development and clinician training.
4.2. Conclusion
Our findings suggest that smartphone-based prenatal prematurity education is feasible. Larger trials testing the effect of the P3 app on parental knowledge and healthcare decision-making are required before establishing a wider program for parents with preterm birth risk factors.
4.3. Practice Implications
Smartphone-based prematurity education will allow for wide dissemination of information and empower parents to influence prehospitalization healthcare decisions known to impact prematurity health outcomes. If the pregnancy results in preterm birth hospitalization, parents would have built a foundation of knowledge and thus have the chance to better comprehend medical facts provided during the hospitalization, be aware of their rights and obligations, and be able to advocate for care aligned with their values.
Highlights:
Half of all premature births in the United States have preterm birth associated risk factors
Prematurity education is currently offered to parents upon hospitalization for preterm birth
Lack of prematurity education before the birth hospitalization leaves parents unprepared
Smartphone-based prenatal prematurity education benefited parents at-risk for preterm birth
In the majority of participants, the smartphone-based prenatal prematurity education did not increase parental anxiety
Practice implications.
If the pregnancy results in preterm birth hospitalization, parents would have built a foundation of knowledge to make informed medical care choices.
Acknowledgments
Grant support: This project was supported by the National Center for Advancing Translational Sciences, National Institutes of Health (NIH) [grant number UL1TR001436]. Its content is solely the responsibility of the authors and do not necessarily represent the official views of NIH.
Financial disclosure: None
Footnotes
Conflict of Interest: The authors have no conflict of interest relevant to this article to disclose
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- [1].Center for Disease Control and Prevention Website. Accessed 20180608 http://www.cdc.gov/reproductivehealth/maternalinfanthealth/pretermbirth.htm
- [2].Leuthner SR. Borderline viability: Controversies in caring for the extremely premature infant. Clin Perinatol. 2014;41:799–814. [DOI] [PubMed] [Google Scholar]
- [3].Soria-Pastor S, Padilla N, Zubiaurre-Elorza L, et al. Decreased regional brain volume and cognitive impairment in preterm children at low risk. Pediatrics. 2009;124:e1161–70. [DOI] [PubMed] [Google Scholar]
- [4].The Consortium on Safe Labor,. Respiratory morbidity in late preterm births. J Amer Med Assoc. 2010;304:419–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Kramer MS. Late preterm birth: Appreciable risks, rising incidence. J Pediatr. 2009;154:159–60. [DOI] [PubMed] [Google Scholar]
- [6].Lindstrom K, Lindblad F, Hjern A. Psychiatric morbidity in adolescents and young adults born preterm: A Swedish national cohort study. Pediatrics. 2009;123:e47–53. [DOI] [PubMed] [Google Scholar]
- [7].Younge N, Goldstein RF, Bann CM, et al. Survival and neurodevelopmental outcomes among periviable infants. N Engl J Med. 2017;376:617–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Wen SW, Smith G, Yang Q, Walker M. Epidemiology of preterm birth and neonatal outcome. Seminars in Fetal and Neonatal Medicine. 2004;9:429–35. [DOI] [PubMed] [Google Scholar]
- [9].Mehrotra A, Lagatta J, Simpson P, Kim UO, Nugent M, Basir MA. Variations among US hospitals in counseling practices regarding prematurely born infants. J Perinatol. 2013;33:509–13. [DOI] [PubMed] [Google Scholar]
- [10].Harrison H The principles for family-centered neonatal care. Pediatrics. 1993;92:643–50. [PubMed] [Google Scholar]
- [11].Swan HD, Borshoff DC. Informed consent--recall of risk information following epidural analgesia in labour. Anaesth Intensive Care. 1994;22:139–41. [DOI] [PubMed] [Google Scholar]
- [12].Paulus MP, Yu AJ. Emotion and decision-making: Affect-driven belief systems in anxiety and depression. Trends Cogn Sci (Regul Ed ). 2012;16:476–83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Rilling JK, Sanfey AG. The neuroscience of social decision-making. Annu Rev Psychol. 2011;62:23–48. [DOI] [PubMed] [Google Scholar]
- [14].Ghia N, Spong CY, Starbuck VN, Scialli AR, Ghidini A. Magnesium sulfate therapy affects attention and working memory in patients undergoing preterm labor. Obstet Gynecol. 2000;183:940–4. [DOI] [PubMed] [Google Scholar]
- [15].Massett HA, Greenup M, Ryan CE, Staples DA, Green NS, Maibach EW. Public perceptions about prematurity: A national survey. Am J Prev Med. 2003;24:120–7. [DOI] [PubMed] [Google Scholar]
- [16].Govande VP, Brasel KJ, Das UG, Koop JI, Lagatta J, Basir MA. Prenatal counseling beyond the threshold of viability. J Perinatol. 2013;33:358–62. [DOI] [PubMed] [Google Scholar]
- [17].Cummings J, COMMITTEE ON FETUS AND NEWBORN . Antenatal counseling regarding resuscitation and intensive care before 25 weeks of gestation. Pediatrics. 2015;136:588–95. [DOI] [PubMed] [Google Scholar]
- [18].Kim UO, Basir MA. Informing and educating parents about the risks and outcomes of prematurity. Clin Perinatol. 2014;41:979–91. [DOI] [PubMed] [Google Scholar]
- [19].American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine, Ecker JL, Kaimal A, et al. #3: Periviable birth. Am J Obstet Gynecol. 2015;213:604–14. [DOI] [PubMed] [Google Scholar]
- [20].Powell MR, Kim UO, Weisgerber MC, Simpson PM, Nugent M, Basir MA. Readiness of obstetric professionals to inform parents regarding potential outcome of premature infants. J Obstet Gynaecol. 2012;32:326–31 [DOI] [PubMed] [Google Scholar]
- [21].Haywood JL, Goldenberg RL, Bronstein J, Nelson KG, Carlo WA. Comparison of perceived and actual rates of survival and freedom from handicap in premature infants. Am J Obstet Gynecol. 1994;171:432–9. [DOI] [PubMed] [Google Scholar]
- [22].Catlin Anita DNS, Fnp Faan. Thinking outside the box: Prenatal care and the call for a prenatal advance directive. J Perinat Neonatal Nurs. 2005;19:169–76. [DOI] [PubMed] [Google Scholar]
- [23].Catlin AJ, Stevenson DK. Physicians’ neonatal resuscitation of extremely low-birth-weight preterm infants. Image - the Journal of Nursing Scholarship. 1999;31:269–75. [DOI] [PubMed] [Google Scholar]
- [24].National Institutes of Child Health and Human Development Website. Accessed 20180608 https://www.nichd.nih.gov/health/topics/preterm/conditioninfo/Pages/who_risk.aspx
- [25].Son M, Miller ES. Predicting preterm birth: Cervical length and fetal fibronectin. Semin Perinatol. 2017;41:445–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Purisch SE, Gyamfi-Bannerman C. Epidemiology of preterm birth. Semin Perinatol. 2017;41:387–91. [DOI] [PubMed] [Google Scholar]
- [27].Whittaker R, Matoff-Stepp S, Meehan J, et al. Text4baby: Development and implementation of a national text messaging health information service. Am J Public Health. 2012;102:2207–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Tamrat T, Kachnowski S. Special delivery: An analysis of mHealth in maternal and newborn health programs and their outcomes around the world. Maternal & Child Health Journal. 2012;16:1092–101. [DOI] [PubMed] [Google Scholar]
- [29].Rosenstock I, Historical origins of the Health belief Model. Health Educ Monogr. 1974:2 [DOI] [PubMed] [Google Scholar]
- [30].Muthusamy AD, Leuthner S, Gaebler-Uhing C, Hoffmann RG, Li S, Basir MA. Supplemental written information improves prenatal counseling: A randomized trial. Pediatrics. 2012;129:1269–74. [DOI] [PubMed] [Google Scholar]
- [31].Raju TN, Mercer BM, Burchfield DJ, Joseph GF Jr. Periviable birth: Executive summary of a joint workshop by the Eunice Kennedy Shriver national institute of child health and human development, society for Maternal-fetal medicine, American academy of pediatrics, and American college of obstetricians and gynecologists. Obstet Gynecol. [DOI] [PubMed] [Google Scholar]
- [32].Stoll BJ, Hansen NI, Bell EF, et al. Neonatal outcomes of extremely preterm infants from the NICHD neonatal research network. Pediatrics. 2010;126(3):443–56. 2014;123:1083–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Hodgins S, Tielsch J, Rankin K, Robinson A, Kearns A, Caglia J. A new look at care in pregnancy: Simple, effective interventions for neglected populations. PLoS ONE. 2016;11:e0160562 Accessed 20160819. 10.1371/journal.pone.0160562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Sharma D Golden hour of neonatal life: Need of the hour. Matern Health Neonatol Perinatol. 2017. 19;3:16. doi: 10.1186/s40748-017-0057-x. eCollection 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Lucas A, Cole TJ. Breast milk and neonatal necrotizing enterocolitis. The Lancet. 1990;336:1519–23. [DOI] [PubMed] [Google Scholar]
- [36].Murray SR, Stock SJ, Norman JE. Long-term childhood outcomes after interventions for prevention and management of preterm birth. Semin Perinatol. 2017;41:519–27. [DOI] [PubMed] [Google Scholar]
- [37].Chien EK. Prevention of periviable birth: Bed rest, tocolysis, progesterone, and cerclage. Semin Perinatol. 2013;37:404–9. [DOI] [PubMed] [Google Scholar]
- [38].Ge WJ, Mirea L, Yang J, Bassil KL, Lee SK, Shah PS. Prediction of neonatal outcomes in extremely preterm neonates. Pediatrics. 2013;132:e876–85. [DOI] [PubMed] [Google Scholar]
- [39].Weisman CS, Hillemeier MM, Chase GA, et al. Preconceptional health: Risks of adverse pregnancy outcomes by reproductive life stage in the central Pennsylvania women’s health study (CePAWHS). Womens Health Issues. 2006;16:216–24. [DOI] [PubMed] [Google Scholar]
- [40].Chuang CH, Green MJ, Chase GA, Dyer A, Ural SH, Weisman CS. Perceived risk of preterm and low-birthweight birth in the central Pennsylvania women’s health study. Obstet Gynecol. 2008;199:64.e1–64.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41]. [Accessed 20180608]; http://www.pewinternet.org/fact-sheet/mobile/
- [42]. [Accessed 20180608]; http://www.pewinternet.org/2015/04/01/chapter-two-usage-and-attitudes-toward-smartphones/
- [43].Orr TBS, CampbellYeo MNNPBC, Benoit BN, Hewitt, Brenda MN,C.N.C.C.P., B.C.L.C., Stinson J, C.P.N.P., McGrath POC, F.R.S.C. Smartphone and internet preferences of parents: Information needs and desired involvement in infant care and pain management in the NICU. Advances in Neonatal Care. 2017;17:131–8. [DOI] [PubMed] [Google Scholar]
- [44].Ly K MHealth: Better health through your smartphone. Community Practitioner. 211;84:16–7. [PubMed] [Google Scholar]
- [45].Koh TH, Casey A, Harrison H. Use of an outcome by gestation table for extremely premature babies: A cross-sectional survey of the views of parents, neonatal nurses and perinatologists. J Perinatol. 2000;20:504–8. [DOI] [PubMed] [Google Scholar]
- [46].Blanco F, Suresh G, Howard D, Soll RF. Ensuring accurate knowledge of prematurity outcomes for prenatal counseling. Pediatrics; Pediatrics. 2005;115:e478–87. [DOI] [PubMed] [Google Scholar]
- [47].Kakkilaya V, Groome LJ, Platt D, et al. Use of a visual aid to improve counseling at the threshold of viability. Pediatrics. 2011;128:e1511–9. [DOI] [PubMed] [Google Scholar]
- [48].Guillen U, Suh S, Munson D, et al. Development and pretesting of a decision-aid to use when counseling parents facing imminent extreme premature delivery. J Pediatr. 2012;160:382–7. [DOI] [PubMed] [Google Scholar]
- [49].Wilson EAH, Makoul G, Bojarski EA, et al. Comparative analysis of print and multimedia health materials: A review of the literature. Patient Education & Counseling. 2012;89:7–14. [DOI] [PubMed] [Google Scholar]
- [50].Pusic MV, Ching K, Yin HS, Kessler D. Seven practical principles for improving patient education: Evidence-based ideas from cognition science. Paediatrics & Child Health. 2014;19:119–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Janvier A, Lorenz JM, Lantos JD. Antenatal counselling for parents facing an extremely preterm birth: Limitations of the medical evidence. Acta Paediatrica. 2012;101(:800–4. [DOI] [PubMed] [Google Scholar]
- [52].Boss RD, Hutton N, Sulpar LJ, West AM, Donohue PK. Values parents apply to decision-making regarding delivery room resuscitation for high-risk newborns. Pediatrics. 2008;122:5839. [DOI] [PubMed] [Google Scholar]