Abstract
Background
The Limberg flap reconstruction and the Karydakis flap reconstruction are the 2 most used off-midline closure techniques in pilonidal sinus surgery. The current evidence is inconclusive as to which is the optimal technique. The aim of this systematic review and meta-analysis was to compare differences in outcomes between these 2 flap-based techniques.
Methods
We identified studies by a systematic literature search of the Embase, MEDLINE (PubMed), Cochrane Library and Google Scholar databases and studies selected as per the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist. Only randomized controlled trials (RCTs) that compared the Limberg flap (standard or modified) and the Karydakis flap were included in this review.
Results
Operative time was shorter by 7 minutes in the Karydakis group than in the Limberg group (mean difference 7.00 min, 95% confidence interval [CI] 0.53 to 13.48). The seroma formation rate was significantly higher in the Karydakis cohort (odds ratio [OR] 0.36, 95% CI 0.24 to 0.56); however, after excluding studies with a high risk of bias, the sensitivity analysis showed no significant differences in seroma formation rate between the 2 techniques (OR 0.76, 95% CI 0.31 to 1.85). Other outcomes of interest showed no significant differences between the Limberg and Karydakis techniques.
Conclusion
There were no significant differences between the Limberg and Karydakis techniques. Future RCTs with strict adherence to CONSORT guidelines will further elucidate the efficacy of these surgical procedures.
Abstract
Contexte
Les reconstructions à l’aide de lambeaux de Limberg et de Karydakis sont 2 des techniques de fermeture décalées de la ligne médiane les plus utilisées pour la chirurgie du sinus pilonidal. Les preuves actuelles ne permettent pas de conclure à la supériorité de l’une par rapport à l’autre. Le but de la présente revue systématique/ méta-analyse était de comparer les différences de résultats entre ces 2 techniques de lambeaux.
Méthodes
Nous avons recensé des études au moyen d’une interrogation systématique des bases de données Embase, MEDLINE (PubMed), bibliothèque Cochrane et Google Scholar et les études sélectionnées à l’aide de la liste de vérification PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses). Seuls les essais randomisés et contrôlés (ERC) qui comparaient les lambeaux de Limberg (standard ou modifié) et de Karydakis ont été inclus dans cette revue.
Résultats
Les interventions ont duré 7 minutes de moins dans le groupe Karydakis que dans le groupe Limberg (différence moyenne 7,00 min, intervalle de confiance [IC] de 95 % 0,53 à 13,48). Le taux de formation de séromes a été significativement plus élevé dans la cohorte Karydakis (rapport ces cotes [RC] 0,36, IC de 95 % 0,24 à 0,56); par contre, après avoir exclu les études comportant un important risque de biais, l’analyse de sensibilité n’a montré aucune différence significative quant au taux de formation de séromes entre les 2 techniques (RC 0,76, IC de 95 % 0,31 à 1,85). Les autres paramètres d’intérêt n’ont montré aucune différence significative entre les techniques de Limberg et de Karydakis.
Conclusion
On n’a noté aucune différence significative entre les techniques de Limberg et de Karydakis. De prochains ERC strictement conformes aux lignes directrices CONSORT permettront de préciser davantage l’efficacité de ces interventions chirurgicales.
The reported incidence rate of pilonidal disease is 25 per 100 000 people.1 Initially, the pathogenesis was considered to be congenital.2 Today, however, the theory that it is acquired is more widely accepted. Work by Georgios Karydakis,3,4 who highlighted 3 main factors contributing to pilonidal disease (loose hair, an external force that facilitates insertion of hair into the skin and an underlying vulnerability of natal cleft skin), had a pivotal role in this paradigm shift. The first 2 factors are related to personal hygiene and lifestyle, and their modulation can influence the initiation, development and recurrence of pilonidal disease. Armstrong and Barcia5 reported that improved hygiene, an active lifestyle and hair control in the natal cleft area decreased the need for surgical procedures and resulted in faster return to work. However, the third factor can be modified only surgically. The rhomboid, well-vascularized transposition Limberg flap was first proposed by the Russian maxillofacial surgeon Alexander Limberg (1894–1974), author of the fundamental work in plastic surgery “Mathematical principles of local plastic procedures on the surface of the human body.”6,7
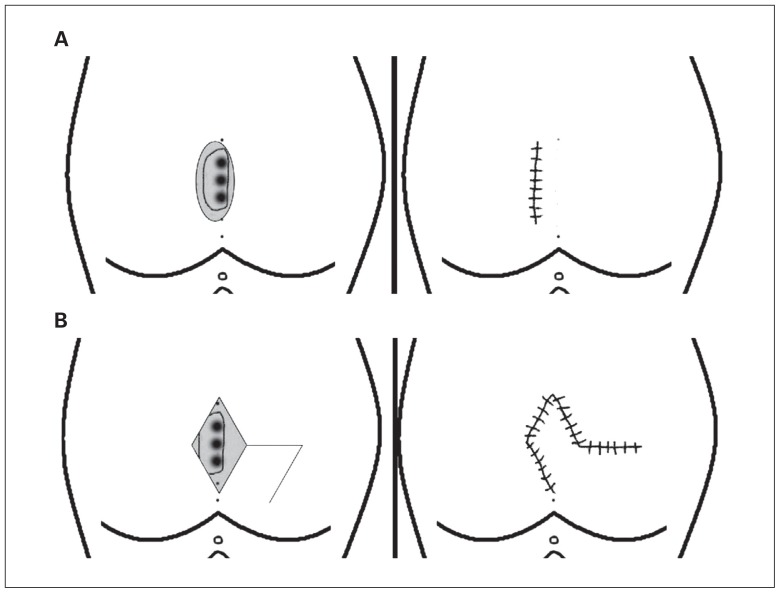
Patients with chronic pilonidal sinus disease are usually candidates for flap procedures. A chronic disease can be defined as any condition with constant or recurrent symptoms observed over several months, without any indication of spontaneous healing.8,9 Flap-based Limberg and Karydakis techniques both aim to achieve off-midline closure of the surgical defect to flatten the natal cleft. In both techniques, methylene blue is injected in the pilonidal sinuses to guide the excision. The Karydakis technique consists of an asymmetric elliptical excision of the affected area (Fig. 1). The upper and lower poles of the ellipse are placed about 2 cm to the side of the midline. Subsequently, after full-thickness mobilization of the contralateral surgical margin and fixation of the base of the flap to the sacral fascia, the skin edges are sutured off the midline. In the modified Karydakis technique, fixation to the sacral fascia is not required. The Limberg technique consists of a rhomboid-shaped excision of the affected area down to the sacral fascia (Fig. 1). The cephalic and caudal apex of the rhombus are placed about 2 cm to the side of the midline. A fasciocutaneous rhomboid flap is then created and transposed so the defect can be covered without any tension. In contrast, the classic Limberg flap consists of a symmetric rhomboid excision with its apices placed on the midline.3,6–8 Karydakis reported a wound complication rate of 8% and a recurrence rate of 2% for 7471 procedures.3,4 The reported recurrence rate with the Limberg technique is 5%.8
Fig. 1.
(A) Karydakis technique. (B) Limberg technique with rhomboid transposition flap.
The existing evidence is inconclusive as to which technique is the optimal treatment for pilonidal sinus disease. To help clarify this issue, we performed a systematic review to compare the Limberg and Karydakis flap techniques through meta-analysis of randomized controlled trials (RCTs). The primary outcomes investigated were wound infection, wound dehiscence and time to return to work. Hematoma formation, length of hospital stay, recurrence and patient satisfaction rate were secondary outcomes.
Methods
This systematic review and meta-analysis was carried out in accordance with the guidelines set out in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist.
Literature search
We performed a systematic literature search of articles published in the last 20 years using the Embase, MEDLINE (PubMed), Cochrane Library and Google Scholar databases and free text and MeSH search terms (standard or modified Limberg flap; standard or modified Karydakis flap; pilonidal sinus surgery and disease; randomized or nonrandomized controlled trial). We also performed a grey literature search on the ClinicalTrials.gov Web site. We manually checked references of the retrieved articles for further analysis. Disagreements between the authors were resolved by consensus.
Study selection and inclusion and exclusion criteria
Only RCTs that compared standard or modified Limberg flap and standard or modified Karydakis flap in pilonidal sinus surgery were included in the study. All nonrandomized studies, reviews and narrative articles were excluded.
Data extraction and outcomes
Two reviewers (P.G. and E.B.) independently extracted the following summary data for the included studies: name of authors, patient age, operative time, wound infections, wound dehiscence, hematoma, seroma, recurrences, length of hospital stay, time to return to work and patient satisfaction.
Risk of bias assessment of included studies
The 2 authors independently assessed the risk of selection bias, attrition bias, detection bias, performance bias and reporting bias for each included study. We categorized the risk of bias according to the Cochrane Handbook for Systematic Reviews of Interventions10 as high, low or unclear.
Definitions
We defined operative time as time from scalpel to the skin until the last skin stitch. Wound infections and seromas were reported based on clinical findings. Culture results and wound dehiscence (partial or complete) were defined by the individual study authors. We defined length of hospital stay as the number of days from the operation day until the day of discharge. Patient satisfaction was reported as described by each of the included studies’ authors.
Statistical analysis
We conducted statistical analysis using Review Manager 5.3 software (Cochrane Collaboration). Heterogeneity was assessed through the I2 test, and cut-off values of 25%, 50% and 75% were considered low, moderate and high, respectively.11 For I2 values above 25%, both fixed- and random-effects models were used and the results compared between them. In cases in which the I2 value was 25% or less, we used fixed-effects models throughout.
We analyzed dichotomous variables based on odds ratios (ORs) with 95% confidence intervals (CIs). For the analyzed outcomes, the reference categories were selected so that OR < 1 favoured the Limberg technique. We combined continuous variable based on both the mean difference and standardized mean difference. For studies that did not report the means and variances for the 2 groups, we estimated these values from the median, range and sample size where possible, using the technique described by Hozo and colleagues.12 In all analyses, the significance level was set at p < 0.05.
Sensitivity analysis
We conducted analyses of primary and secondary outcomes using both random-effects and fixed-effect models in order to assess the impact of heterogeneity on the results. In addition, we performed subgroup analysis of the studies in which the modified flap technique was used. We did not estimate publication bias because fewer than 10 studies were included in the review.13
Results
Characteristics of included studies
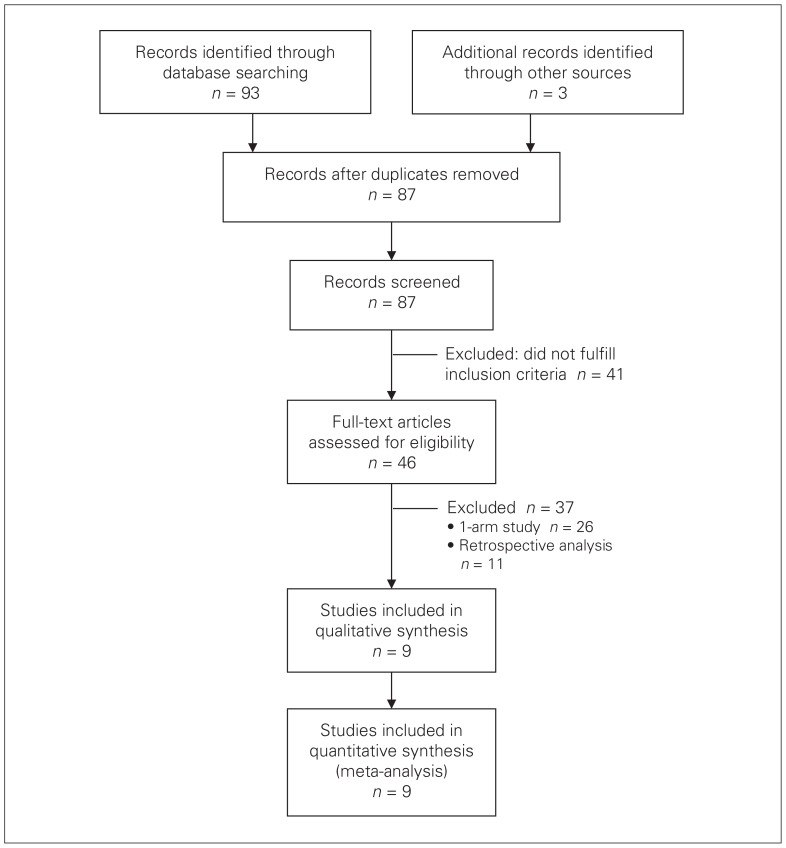
The search strategy yielded 93 papers. A further 3 papers were obtained via manual reference searching, for a total of 96 studies. After removal of duplicates, 87 studies remained. Their abstracts were screened and 41 studies were removed as they did not fulfill the inclusion criteria. The full articles of the remaining 46 studies were read. Twenty-six 1-arm studies and 11 retrospective analyses were excluded, leaving 9 studies14–22 that met the criteria for inclusion in this systematic review and meta-analysis (Fig. 2).
Fig. 2.
Flow diagram of literature search strategy.
A total of 1421 patients were involved in the selected studies, of whom 773 (54.4%) underwent Limberg and 648 (45.6%) underwent Karydakis flap reconstruction. Demographic characteristics were similar between the 2 groups (Table 1). All studies included patients with chronic pilonidal disease. Five studies compared the modified Limberg flap to the Karydakis flap;15,17–19,21 those results were similar to those for the total sample (Table 2). Bali and colleagues19 enrolled only patients with recurrent disease. The most commonly used excluding criteria of the RCTs were recurrent disease, American Society of Anesthesiologists physical status class 3 or greater, diabetes, drug or alcohol addiction, renal failure and immunosuppression. Patients with laterally extended sinuses unsuitable to be included in the fusiform excision of the Karydakis procedure were transferred to the Limberg procedure.15
Table 1.
Study characteristics*
| Study/year/ country | No. of patients | Age, yr, mean ± SD | Operative time, min, mean ±_SD | No. (%) with wound infection | No. (%) with wound dehiscence | No. (%) with hematoma formation | No. (%) with seroma formation | Type of drain | Length of hospital stay, d, mean ±_SD | Time to return to work, d, mean ± SD | Patient satisfaction rate, mean score ± SD or no. (%) | No. (%) with recurrence |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ahmed et al.,22 2017, Pakistan | 75 | 32.2 ± 9.8 | NR | NR | NR | NR | NR | Redivac | 3.97 ± 0.71 | 15.53 ± 1.22 | NR | NR |
| 75 | 33.6 ± 9.7 | 2.93 ± 0.66 | 13.13 ± 1.15 | |||||||||
| p = 0.2 | p < 0.001 | p < 0.001 | ||||||||||
|
| ||||||||||||
| Khan et al.,21 2016, Pakistan† | 90 | 42.7 ± 14 | NR | 11 (12) | NR | NR | 6 (7) | NR | NR | NR | NR | NR |
| 90 | 43.4 ± 16 | 30 (33) | 20 (22) | |||||||||
| p = 0.2 | p = 0.001 | p = 0.003 | ||||||||||
|
| ||||||||||||
| Bali et al.,20 2015, Turkey | 37 | 25 ± 5 | 54 ± 5 | 4 (11) | 1 (3) | 8 (22) | 3 (8) | B-Vak | 1.44 ± 0.5 | 8 ± 1.5 | 2.88 ± 0.16 | 0 (0) |
| 34 | 24 ± 5 | 48 ± 5 | 8 (24) | 2 (6) | 3 (9) | 4 (12) | 3 ± 0.75 | 17 ± 1.5 | 1.43 ± 0.4 | 0 (0) | ||
| p = 0.2 | p = 0.001 | p = 0.001 | p = 0.6 | p = 0.004 | p = 0.8 | p = 0.001 | p < 0.001 | p < 0.001 | ||||
|
| ||||||||||||
| Tokac et al.,19 2015, Turkey† | 46 | 29.28 ± 85 | 44.5 ± 6.6 | 3 (7) | NR | NR | NR | Placed, type NR | 1.06 ± 0.3 | 20.61 ± 7.89 | NR | 3 (7) |
| 46 | 28.35 ± 85 | 42.9 ± 6.2 | 3 (7) | 1.03 ± 0.17 | 23.29 ± 6.42 | 2 (4) | ||||||
| p > 0.05 | p > 0.05 | p > 0.05 | p > 0.05 | p < 0.05 | p > 0.05 | |||||||
|
| ||||||||||||
| Arslan et al.,18 2014, Turkey‡ | 96 | 26.5 ± 5.9 | 51.1 ± 6.8 | 2 (2) | 2 (2) | 4 (4) | 5 (5) | Jackson-Pratt | 1.3 ± 0.5 | 20.8 ± 6.5 | 71 (74) | 6 (6) |
| 91 | 24.7 ± 5.1 | 50.9 ± 7.3 | 6 (7) | 14 (15) | 3 (3) | 18 (20) | 1.3 ± 0.4 | 19.1 ± 3.4 | 64 (70) | 10 (11) | ||
| p = 0.08 | p = 0.08 | p < 0.05 | p < 0.001 | p = 0.9 | p < 0.05 | p = 0.5 | p = 0.7 | p = 0.8 | p = 0.003 | |||
|
| ||||||||||||
| Arslan et al.,18 2014, Turkey† | 108 | 24.7 ± 5.1 | 52.9 ± 7.3 | 5 (5) | 4 (4) | 3 (3) | 8 (7) | Jackson-Pratt | 1.3 ± 0.4 | 19.8 ± 4.6 | 84 (78) | 2 (2) |
| 91 | 24.7 ± 5.1 | 50.9 ± 7.3 | 6 (7) | 14 (15) | 3 (3) | 18 (20) | 1.3 ± 0.4 | 19.1 ± 3.4 | 64 (70) | 10 (11) | ||
| p = 1.0 | p = 0.08 | p = 0.3 | p < 0.002 | p = 1.0 | p = 0.002 | p = 1.0 | p = 1.0 | p = 0.7 | p = 0.002 | |||
|
| ||||||||||||
| Bessa,17 2013, Egypt† | 60 | 23 ± 2.25 | 52 ± 3.5 | 3 (5) | 11 (18) | NR | 0 (0) | 18 French | NR | NR | 43 (72) | 2 (3) |
| 60 | 23 ± 6.25 | 33 ± 3 | 2 (3) | 6 (10) | 3 (5) | 58 (97) | 1 (2) | |||||
| p = 0.4 | p = 0.001 | p = 1.0 | p = 0.003 | p = 0.2 | p = 0.6 | |||||||
|
| ||||||||||||
| Ates et al.,16 2011, Turkey | 134 | NR | 50.14 ± 6.964 | 8 (6) | 14 (10) | 3 (2) | 3 (2) | Placed, type NR | 3.80 ± 1.19 | 8.55 ± 1.18 | 3.16 ± 1.40 | 9 (7) |
| 134 | 2.32 ± 8.64 | 4 (3) | 8 (6) | 1 (1) | 1 (1) | 3.40 ± 0.94 | 8.45 ± 1.16 | 7.08 ± 1.7 | 4 (3) | |||
| p = 0.001 | p = 0.9 | p = 0.9 | p = 0.03 | p = 0.5 | p = 0.001 | |||||||
|
| ||||||||||||
| Can et al.,15 2010, Turkey† | 77 | 22 ± 5.25 | 52.8 ± 16 4 | 3 (4) | 1 (1) | 1 (1) | 3 (4) | On surgeon’s preference | 4.8 ± 2.6 | 21.5 ± 8.5 | 70 (91) | 4 (5) |
| 68 | 22 ± 2.75 | 0.4 ± 2.5 | 3 (4) | 1 (1) | 1 (1) | 3 (4) | 5.5 ± 2 | 18.8 ± 7.7 | 60 (88) | 3 (4) | ||
| p = 0.6 | p = 0.01 | p = 1.0 | p = 1.0 | p = 1.0 | p = 1.0 | p = 0.1 | p = 0.09 | p = 1.0 | p = 1.0 | |||
|
| ||||||||||||
| Ersoy et al.,14 2009, Turkey | 50 | 27.8 ± 6.5 | NR | 4 (8) | NR | NR | NR | Placed, type NR | NR | 14 ± 10.25 | NR | NR |
| 50 | 25.8 ± 6.4 | 13 (26) | 15 ± 10 | |||||||||
| p = 0.02 | p = 0.3 | |||||||||||
|
| ||||||||||||
| Pooled difference (n = 1421) | 773 648 |
MD 0.47 (95% CI 0.18 to 1.11) | MD 7.00 (95% CI 0.53 to 13.48) | OR 0.6 (95% CI 0.41 to 1.4) | OR 0.60 (95% CI 0.20 to 1.81) | OR 1.6 (95% CI 0.76 to 3.51 | OR 0.36 (95% CI 0.24 to 0.56) | — | MD −0.07 (95% CI 0.45 to 0.30) | MD 0.33 (95% CI 0.99 to 1.66) | OR 0.83 (95% CI 0.34 to 2.01) | OR 0.88 (95% CI 0.38 to 2.04) |
CI = confidence interval; MD = mean difference; NR = not reported; OR = odds ratio; SD = standard deviation.
Throughout table, first value is for Limberg flap, second value is for Karydakis flap.
Modified Limberg flap.
Standard Limberg flap.
Table 2.
Outcomes of interest
| Outcome | No. of studies/ patients | Estimated effect (95% CI) | I2, % |
|---|---|---|---|
| Total sample | |||
| Age13–21 | 9/1244 | MD 0.47 (−0.18 to 1.11) | 0 |
| Operative time14–19 | 7/1082 | MD 7.00 (0.53 to 13.48) | 99 |
| Wound infection13–21 | 8/1182 | OR 0.65 (0.41 to 1.04) | 18 |
| Wound dehiscence14–19 | 6/990 | OR 0.60 (0.20 to 1.81) | 72 |
| Hematoma14–19 | 5/870 | OR 1.63 (0.76 to 3.51) | 0 |
| Seroma14–20 | 7/1170 | Peto OR 0.36 (0.24 to 0.56) | 19 |
| High-quality seroma studies14–16,19 | 4/604 | Peto OR 0.76 (0.31 to 1.85) | 25 |
| Recurrence14–19 | 6/1011 | OR 0.88 (0.38 to 2.04) | 94 |
| Length of hospital stay14–19 | 7/1112 | MD −0.07 (−0.45 to 0.30) | 97 |
| Time to return to work14–19 | 8/1212 | MD 0.33 (−0.99 to 1.66) | 94 |
| Patient satisfaction rate14,19 | 6/990 | OR 0.83 (0.34 to 2.01) | 75 |
| Subgroup analysis, modified Limberg flap | |||
| Wound infection14,17,18,20 | 4/556 | OR 0.91 (0.42 to 1.94) | 0 |
| Wound dehiscence14,17,18 | 3/464 | OR 0.70 (0.13 to 3.84) | 75 |
| Seroma14,17,18,20 | 4/644 | OR 0.33 (0.99 to 0.57) | 0 |
| Recurrence14,17,18,20 | 4/556 | OR 0.77 (0.22 to 2.63) | 48 |
| Length of hospital stay14,17,18 | 3/436 | MD −0.00 (−0.12 to 0.12) | 45 |
| Time to return to work14,17,18 | 3/436 | MD 0.37 (−2.04 to 2.77) | 72 |
CI = confidence interval; MD = mean difference; OR = odds ratio.
Study quality
Generally, RCT quality was poor (Table 3). There was a widespread high risk of inadequate blinding and incomplete outcome data. Allocation was adequately concealed in 516–19 of the 9 studies. Only 1 study17 adequately addressed the sequence generation and blinding of outcome assessors, and none of the studies performed an intention-to-treat analysis for the missing data.
Table 3.
Risk of bias
| Study | Type of bias; risk | |||
|---|---|---|---|---|
| Sequence generation | Allocation concealment | Incomplete outcome data | Blinding | |
| Ahmed et al.22 | Unclear | High | High | High |
| Khan et al.21 | Unclear | High | High | High |
| Bali et al.20 | High | High | High | High |
| Tokac et al.19 | Unclear | Low | High | High |
| Arslan et al.18 | Unclear | Low | High | High |
| Bessa17 | Low | Low | Unclear | Low |
| Ates et al.16 | Unclear | Low | High | High |
| Can et al.15 | Unclear | Low | High | High |
| Ersoy et al.14 | High | High | High | High |
| Pooled data | Low 1 | Low 5 | Low 0 | Low 1 |
Outcomes of interest
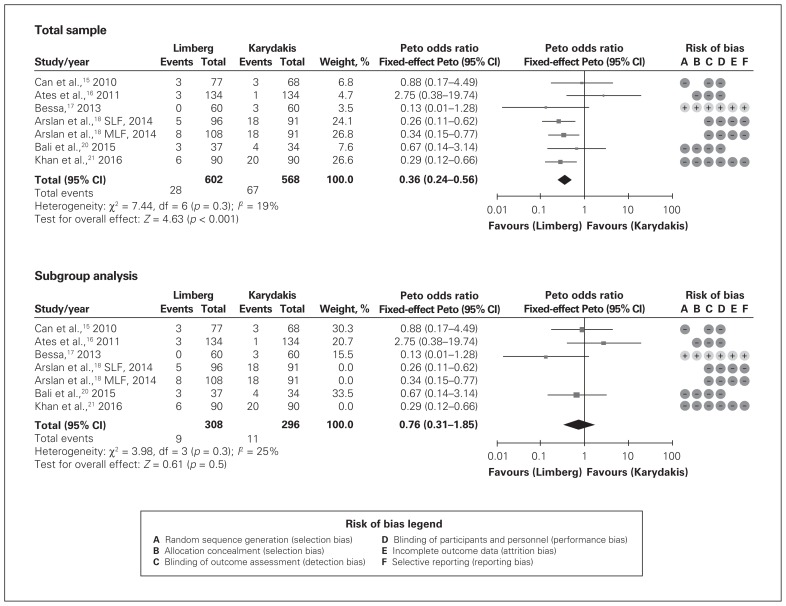
Operative time was 7 minutes shorter in the Karydakis group than in the Limberg group (mean difference 7.00 min, 95% CI 0.53 to 13.48), although heterogeneity was extremely high (I2 = 99%). The seroma formation rate was significantly higher in the Karydakis group than in the Limberg group (OR 0.36, 95% CI 0.24 to 0.56, I2 = 19%) (Fig. 3). However, subgroup analysis including only studies with a low risk of bias showed no statistically significant difference in seroma formation rate between the 2 techniques (OR 0.76, 95% CI 0.31 to 1.85, I2 = 25%) (Fig. 3). For all other outcomes (wound infection/dehiscence, hematoma, recurrence, length of hospital stay and patient satisfaction), no significant differences were found between the 2 procedures (Table 2).
Fig. 3.
Rate of seroma formation. Top: total sample; bottom: subgroup analysis of higher-quality studies. CI = confidence interval; SLF = standard Limberg flap; MLF = modified Limberg flap.
Sensitivity analysis
Subgroup analysis of the studies including the modified Limberg flap did not show any differences compared to the total sample of studies. The differences found in seroma formation rates disappeared when studies with high risk of bias were excluded (Fig. 3, Table 2). No discrepancies were found between the results produced with fixed-effects and random-effects models.
Discussion
This systematic review and meta-analysis showed no remarkable differences between the Limberg and Karydakis procedures in rates of wound infection/dehiscence, hematoma, recurrence and patient satisfaction, or length of hospital stay. There were only 2 differences between the 2 techniques: operative time and seroma formation rate. In the analysis, a modest difference in operative time was noted: the procedure time was 7 minutes shorter for the Karydakis group than for the Limberg group. In a clinical setting, however, this is unlikely to be of any importance. Previous authors have attributed this difference in operative time to 2 factors: first, the classic Karydakis flap does not require extensive mobilization, and second, it does not require fixation at the sacral fascia,15,17 thereby reducing the amount of operative time required. One potential confounding factor with this finding may be the type of anesthesia used in each study. However, it was not possible to retrieve this information adequately for every study, which made it impossible to determine whether anesthetic type did indeed influence operative time.
Seroma formation rates were slightly lower in the Limberg group than in the Karydakis group. However, a subgroup analysis including only higher-quality studies did not show differences in seroma formation rates between the 2 procedures. Arslan and colleagues18 reported the highest difference in seroma formation rate between the Limberg and Karydakis procedures (5% and 20%, respectively). However, their study contained incomplete data regarding dislodgement of drains, which made it difficult to control for confounders. In the same study, there is contradictory information regarding the length of hospital stay and the duration of drainage and follow-up. Overall, the patients had a mean length of hospital stay of 1.3 (standard deviation 0.4) days and a duration of drainage of 3.1 (standard deviation 1.3) days. The authors reported that some patients were discharged with their drain in situ. However, this proportion of patients was not reflected in the study’s mean difference and standard deviation of the duration of drainage. Milone and colleagues’23 meta-analysis of the role of drainage after excision and primary closure revealed that the routine use of drains does not have a statistically significant advantage regarding rates of seroma formation, infection or recurrence.
All other outcomes (wound infection, wound dehiscence, hematoma, recurrence, length of hospital stay and patient satisfaction) in the current study were similar between the Limberg and Karydakis groups.
Enriquez-Navascues and colleagues24 compared different surgical techniques for chronic pilonidal disease using traditional meta-analysis. By default, traditional meta-analyses can be used only to compare 2 treatment approaches. When 3 or more treatments are to be compared, network meta-analysis using either Bayesian or frequentist statistics must be used.25
Limitations
The main limitation of this review is that, although the included studies were RCTs, most were of relatively low quality and had an unclear or high risk of bias: of the 9 studies, only 1 was graded as having a low risk of bias.17 Also, the studies’ populations were likely heterogeneous, as shown by the high I2 value in the analysis of outcome of interests. The protocols, inclusion criteria, surgical technique and follow-up periods also differed, which make the findings not only statistically but also clinically heterogeneous. In this context, the results of this meta-analysis must be interpreted with caution.
Conclusion
Even taking the study limitations into account, the Limberg and Karydakis flap operations in adequately selected patients with pilonidal disease do not show any significant differences between them. Future RCTs should have strict selection criteria, predefined surgical outcome measures, blind outcome assessors, common methods of outcome assessment and follow-up periods of 2–3 years, and must show strict adherence to standards recommended in the CONSORT guidelines.26 These features will help further elucidate the efficacy of these 2 surgical procedures.
Footnotes
Competing interests: None declared.
Contributors: P. Gavriilidis designed the study and wrote the article. Both authors acquired and analyzed the data, reviewed the article and approved the final version for publication.
References
- 1.Lee PJ, Raniga S, Biyani DK, et al. Sacrococcygeal pilonidal disease. Colorectal Dis. 2008;10:639–50. doi: 10.1111/j.1463-1318.2008.01509.x. discussion 651–2. [DOI] [PubMed] [Google Scholar]
- 2.Hodges RM. Pilonidal sinus. Boston Med Surg J. 1880;103:485–6. [Google Scholar]
- 3.Karydakis GE. New approach to the problem of pilonidal disease. Lancet. 1973;2:1414–5. doi: 10.1016/s0140-6736(73)92803-1. [DOI] [PubMed] [Google Scholar]
- 4.Karydakis GE. Easy and successful treatment of pilonidal sinus after explanation of its causative process. Aust N Z J Surg. 1992;62:385–9. doi: 10.1111/j.1445-2197.1992.tb07208.x. [DOI] [PubMed] [Google Scholar]
- 5.Armstrong JH, Barcia PJ. Pilonidal sinus disease. The conservative approach. Arch Surg. 1994;129:914–7. doi: 10.1001/archsurg.1994.01420330028006. [DOI] [PubMed] [Google Scholar]
- 6.Triana RJ. Alexander A. Limberg MD. Arch Facial Plast Surg. 1999;1:226. [Google Scholar]
- 7.de Parades V, Bouchard D, Janier M, et al. Pilonidal sinus disease. J Visc Surg. 2013;150:237–47. doi: 10.1016/j.jviscsurg.2013.05.006. [DOI] [PubMed] [Google Scholar]
- 8.Petersen S, Koch R, Stelzner S, et al. Primary closure techniques in chronic pilonidal sinus: a survey of the results of different surgical approaches. Dis Colon Rectum. 2002;45:1458–67. doi: 10.1007/s10350-004-6451-2. [DOI] [PubMed] [Google Scholar]
- 9.Søndenaa K, Andersen E, Nesrik I, et al. Patient characteristics and symptoms in chronic pilonidal sinus disease. Int J Colorectal Dis. 1995;10:39–42. doi: 10.1007/BF00337585. [DOI] [PubMed] [Google Scholar]
- 10.Higgins JPT, Greens S, editors. Cochrane handbook for systematic reviews of interventions. Version 5.1. London (UK): The Cochrane Collaboration; 2011. [update March 2011] [Google Scholar]
- 11.Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hozo SP, Diulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13. doi: 10.1186/1471-2288-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Harbord RM, Harris RJ, Sterne JA. Updated tests for small-study effects in meta-analyses. Stata J. 2009;9:197–210. [Google Scholar]
- 14.Ersoy E, Devay AO, Aktimur R, et al. Comparison of the short-term results after Limberg and Karydakis procedures for pilonidal disease: randomized prospective analysis of 100 patients. Colorectal Dis. 2009;11:705–10. doi: 10.1111/j.1463-1318.2008.01646.x. [DOI] [PubMed] [Google Scholar]
- 15.Can MF, Sevinc MM, Hancerliogullari O, et al. Multicentre prospective randomized trial comparing modified Limberg flap transposition and Karydakis flap reconstruction in patients with sacrococcygeal pilonidal disease. Am J Surg. 2010;200:318–27. doi: 10.1016/j.amjsurg.2009.08.042. [DOI] [PubMed] [Google Scholar]
- 16.Ates M, Dirican A, Savac M, et al. Short and long-term results of the Karydakis flap versus the Limberg flap for treating pilonidal sinus disease: a prospective randomized study. Am J Surg. 2011;202:568–73. doi: 10.1016/j.amjsurg.2010.10.021. [DOI] [PubMed] [Google Scholar]
- 17.Bessa SS. Comparison of short-term results between the modified Karydakis flap and the modified Limberg flap in the management of pilonidal sinus disease: a randomised controlled trial. Dis Colon Rectum. 2013;56:491–8. doi: 10.1097/DCR.0b013e31828006f7. [DOI] [PubMed] [Google Scholar]
- 18.Arslan K, Said Kokcam S, Koksal H, et al. Which flap method should be preferred for the treatment of pilonidal sinus? A prospective randomized study. Tech Coloproctol. 2014;18:29–37. doi: 10.1007/s10151-013-0982-2. [DOI] [PubMed] [Google Scholar]
- 19.Tokac M, Dumlu EG, Aydin MS, et al. Comparison of modified Limberg flap and Karydakis flap operations in pilonidal sinus surgery: prospective randomized study. Int Surg. 2015;100:870–7. doi: 10.9738/INTSURG-D-14-00213.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bali I, Aziret M, Sözen S, et al. Effectiveness of Limberg and Karydakis flap in recurrent pilonidal sinus disease. Clinics (Sao Paulo) 2015;70:350–5. doi: 10.6061/clinics/2015(05)08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Khan KJ, Ghaffar A, Choudhry S, et al. Comparison of early outcome between modified Limberg and Karydakis flap procedures in patients with sacrococcygeal pilonidal sinus. Pak J Med Health Sci. 2016;10:631–4. [Google Scholar]
- 22.Ahmed Z, Shahid M, Malik MS, et al. Comparison of Karydakis technique with Limberg flap procedure for sacrococcygeal pilonidal sinus disease in terms of hospital stay and work loss. Pak Armed Forces Med J. 2017;67:141–4. [Google Scholar]
- 23.Milone M, Di Minno MND, Musella M, et al. The role of drainage after excision and primary closure of pilonidal sinus; a meta-analysis. Tech Coloproctol. 2013;17:625–30. doi: 10.1007/s10151-013-1024-9. [DOI] [PubMed] [Google Scholar]
- 24.Enriquez-Navascues JM, Emparanza Jl, Alkorta M, et al. Meta-analysis of randomized controlled trials comparing different techniques with primary closures for chronic pilonidal sinus. Tech Coloproctol. 2014;18:863–72. doi: 10.1007/s10151-014-1149-5. [DOI] [PubMed] [Google Scholar]
- 25.Palmer TM, Sterne AC, editors. Meta-analysis in Stata: an updated collection from the Stata Journal. 2nd ed. College Station (TX): Stata Press; 2016. [Google Scholar]
- 26.CONSORT 2010. Ottawa: The Consort Group; [accessed 2018 Nov 14]. Available: www.consort-statement.org/consort-2010. [Google Scholar]