Abstract
Background
Road traffic injury (RTI) is one of the main reasons for trauma-related admission in Ethiopian hospitals. Nationally representative data is needed to develop and implement the public health emergency management strategy. Therefore, this study was aimed to estimate the national pooled prevalence of RTI among trauma patients in Ethiopia.
Methods
PubMed, Excerpta Medica Database (EMBASE), psycEXTRA, and Google Scholar databases were searched. Heterogeneity of studies was assessed using the I2 statistics. Publication bias was checked by using funnel plot and Egger’s regression test. The DerSimonian and Laird's random-effects model was used to estimate the pooled prevalence. Subgroup analysis was conducted by age and region. The trend of RTI estimated as well.
Results
The pooled prevalence of RTI among trauma patients in Ethiopia was 31.5% (95% CI: 25.4%, 37.7%). Regional subgroup analysis showed that the pooled prevalence of RTI was 58.3% in the region of southern, nation, nationalities, and peoples (SNNPR) and 33.3% in Addis Ababa. Subgroup analysis based on patients age showed that the pooled prevalence of RTI was 51.7% in adults, 14.2% in children, and 32.6% in all age group. The time-trend analysis has shown an increasing burden of RTI in Ethiopian hospitals.
Conclusion
The burden of RTI among trauma patients was high. Therefore, strengthening road safety management throughout the country is needed to reduce RTI.
Keywords: Hospitals, Road traffic injury, Trauma patients, Ethiopia
African relevance
-
•
Road traffic injury is a major cause of global disability
-
•
Likewise the burden of road traffic injury was found to be high in Ethiopia
-
•
Strengthening road safety throughout the country is needed to reduce disability
Background
Road traffic injury (RTI) is one of the major causes of patient admission, which increases global disability-adjusted life years (DALYs) population [1] and health care expenditure ($518 billion USD per year) [2], [3]. According to 2013 World Health Organization (WHO) report, nearly 20–50 million people were injured due to RTI [4], which attributes to an occurrence of 1.25 million road traffic deaths per year. The burden of DALYs is also apparent and listed under the top ten leading causes of disease [5], [6].
In 2009, 1.8 million people injured in Europe, 2.8 million in Eastern Mediterranean, 4.1 million in Western Pacific, 4.7 million in Africa, and 8.6 million in Southeast Asia [7]. Based on 2000–2020 WHO projection, road traffic-related deaths expected to increase by 80% in low- and middle-income countries [8]. The estimated prevalence of RTI among trauma patients in sub-Sahara Africa was 32% [9]. RTI is a hidden epidemic causes of morbidity and mortality in developing countries [10] where by more than 90% of death are related with road traffic accidents [11]. Consequently, RTI will have a significant outcome on the social, economic, political, and health development of different countries [12], [13], [14].
To prevent RTI, road safety startegies such as control of driving speed and alcohol consumption, using seatbelt and helmet, designing safer roads and vehicles, and new traffic laws have been globally implemented [15]. However, the burden of RTI is not decreasing in various settings including hospitals.
In Ethiopia, the prevalence of RTI among trauma patients in hospital settings ranges from 1.3% [16] to 62.5% [17]. To date, several studies have been conducted in Ethiopia to determine the prevalence of RTI among trauma patients in hospital settings [18], [19], [20], [21], [22], [23], [24]. Nevertheless, substantial variability of results hinder generalization of studies. Thus, the national prevalence of RTI among trauma patients remains unknown. This meta-analysis was aimed to estimate the national burden of RTI among trauma patients in Ethiopian hospitals.
Methods
The result of this review was reported based on the Preferred Reporting Items for the Systematic Reviews and Meta-Analyses guideline (PRISMA) [25].
Searching strategy
PubMed, psycEXTRA, Excerpta Medica Database (EMBASE), and Google Scholar were searched using the following search terms: “injury”, “trauma”, “unintentional injury”, “intentional injury”, “road traffic injury”, “road traffic collision”, “trauma patient”, “injured patient”, “emergency”, “hospital”, “Ethiopia”. The search strategies were developed using ”AND” and/or “OR” Boolean operators. Additional file 1 illustrated PubMed search string.
The inclusion criteria were: 1) hospital-based studies, 2) observational studies reported the prevalence of RTI among trauma patients, 3) studies conducted in Ethiopia, and 4) studies published in English.
Articles excluded were: 1) studies based on police reports, 2) studies didn’t report the prevalence of RTI in hospitals, and 3) studies published before 2000. We excluded studies published before 2000 to generate globally fitted data. Global estimation about the burden of RTI was considered the year from 2000 to 2020.
Two reviewers independently evaluated the titles and abstracts of all retrieved studies. These articles passed the title and abstract screening process were further eligible for full-text review. The full-text of the eligible articles were reviewed by two authors. The disagreement was handled based on the settled inclusion and exclusion criteria. Whenever the disagreement would continue, the third reviewer was involved for final decision.
The Joanna Briggs Institute (JBI) quality assessment criteria [26] was used to assess the quality of included studies. The criteria were: 1) appropriate sampling frame and technique, 2) sample size adequacy, 3) description of study participants and setting, 4) data analysis with sufficient coverage of sample, 5) using of valid measurement, 6) application of valid measurement for all participants, 7) using of appropriate statistical analysis, and 8) response rate. Two reviewers assessed the quality of included studies. The procedure was repeated whenever disagreement happened. Studies scored ≥50% of the quality assessment criteria were considered low risk of bias.
Two independent reviewers extracted the following data: first author and year, study region, study design, target population, sample size, and prevalence. Reviewers cross-checked for variations in the extracted data. The discrepancies were handled by discussion and re-evaluating the full-text.
The aim of this review was to answer the question “what is the percentage of RTI among trauma patients in Ethiopian hospitals?” The included studies reported the prevalence of RTI among trauma patients in Ethipian hospitals.
Endnote X-7 reference manager software was used to manage the selection process. STATA version 14 (Stata Corp, College Station, TX, USA) was used for the meta-analysis. Potential publication bias was checked by funnel plot and Egger’s regression test [27]. Heterogeneity of studies was assessed using the I2 statistics. The DerSimonian and Laird's random-effects model [28] was used to estimate the pooled prevalence of RTI among trauma patients. Subgroup analysis by region and age was conducted. The leave-one-out sensitivity analysis was done to assess the effect of individual study on the pooled estimate. In addition, the time-trend analysis was employed to investigate change in the burden of RTI over time.
Result
A total of 706 articles were retrieved through searching electronic databases: 654 articles from PubMed, 11 from Excerpta Medica Database (EMBASE), 19 from psycEXTRA, and 22 from Google Scholar. Following a stringent screening process, 17 cross-sectional studies with 61,716 trauma patients were included in the final meta-analysis (Fig. 1).
Fig. 1.
PRISMA flow chart depicting study selection process.
As presented in Table 1, six studies were published between 2003 and 2010 [16], [20], [21], [22], [24], [29] and 11 studies were between 2011 and 2017 [17], [18], [19], [23], [30], [31], [32], [33], [34], [35], [36]. Regarding geographical distribution of studies, seven studies were conducted in Addis Ababa [18], [19], [20], [21], [22], [23], [24], four in Amhara [29], [30], [31], [36], three in Oromia [16], [32], [35], two in SNNPR [17], [34], and one in Tigray region [33]. None of the included studies were excluded due to poor quality.
Table 1.
General characteristics of the included studies.
| Author/Year | Region | Sample size | Patient with RTI | Source population | Age of the participant | Quality of studies |
|---|---|---|---|---|---|---|
| Bashah DT et al./2015 | Amhara | 230 | 78 | all types of trauma | All ages | Low risk |
| Tiruneh BT et al./2014 | Addis Ababa | 356 | 131 | all types of trauma | All ages | Low risk |
| Ayele TA et al./2017 | Amhara | 616 | 245 | all types of trauma | All ages | Low risk |
| Woldemichael K & Berhanu N/2011 | Oromia | 1102 | 334 | all types of trauma | All ages | Low risk |
| Abebe GM et al./2006 | Oromia | 452 | 6 | all types of trauma | Children | Low risk |
| Amdeslasie F et al./2016 | Tigray | 600 | 85 | all types of trauma | All ages | Low risk |
| Hailemichael F et al./2015 | SNNPs | 384 | 240 | all types of trauma | All ages | Low risk |
| Wuhib Z & Tigist B/2014 | Addis Ababa | 380 | 84 | all types of trauma | Children | Low risk |
| Osman M et al./2003 | Amhara | 1982 | 292 | all types of trauma | All ages | Low risk |
| Taye M & Munie T/2003 | Addis Ababa | 3822 | 1568 | all types of trauma | All ages | Low risk |
| Wolde A et al./2008 | Addis Ababa | 40,752 | 4523 | all types of trauma | All ages | Low risk |
| Thomas F & Nebyou S/2014 | SNNPs | 345 | 186 | all types of trauma | Adults | Low risk |
| Kebede T et al./2008 | Addis Ababa | 9000 | 2178 | all types of trauma | All ages | Low risk |
| Mengistu Z & Azaj A/2012 | Addis Ababa | 328 | 161 | all types of trauma | All ages | Low risk |
| Tiruneh BT et al./2017 | Amhara | 893 | 173 | all types of trauma | Children | Low risk |
| Admassie D et al./2010 | Addis Ababa | 422 | 202 | musculoskeletal trauma | Adults | Low risk |
| Aenderl I et al./2014 | Oromia | 52 | 26 | Head trauma | All ages | Low risk |
Meta-analysis
Fig. 2 shows the distribution of included studies. The symmetrical funnel plot (Fig. 2) and non-signicant Egger’s regression test (P = 0.243) revealed the absence of publication bias.
Fig. 2.

Funnel plot to assess publication bias. The vertical line indicates the effect size whereas the diagonal line indicates precision of individual studies with 95% confidence interval.
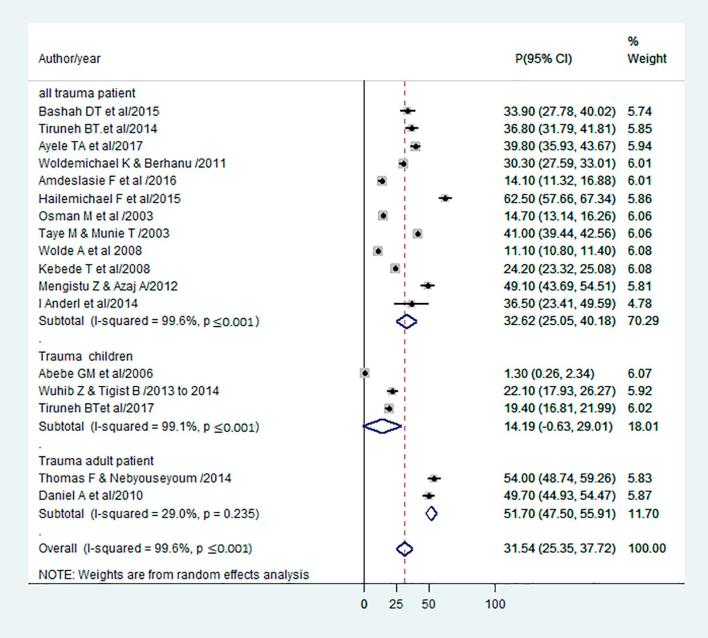
The pooled prevalence of RTI among trauma patients in Ethiopia was 31.5% (95%CI: 25.4%, 37.7%; I2 = 99.6%, p < 0.001) (Fig. 3).
Fig. 3.
Forest plot of the prevalence of RTI with its 95% confidence interval. The midpoint of each line illustrates the prevalence rate reported in each study. The diamond shows the pooled prevalence.
Based on regional subgroup analysis, the pooled prevalence of RTI among trauma patients was high in SNNPR (58.3%) followed by Addis Ababa (33.3%) (Fig. 4). Moreover, subgroup analysis based on patients age, the pooled prevalence of RTI was 51.7% in adults, 14.2% in children, and 32.6% in all age group (Fig. 5).
Fig. 4.
Forest plot of the prevalence of RTI with its 95% confidence interval based on region where the studies conducted. The midpoint of each line illustrates the prevalence; the horizontal line indicates the confidence interval; and the diamond shows the pooled prevalence.
Fig. 5.
Forest plot of the prevalence of RTI with its 95% confidence interval based on the age of the patients. The midpoint of each line illustrates the prevalence; the horizontal line indicates the confidence interval; and the diamond shows the pooled prevalence.
The time-trend analysis showed that RTI among trauma patients in Ethiopian hospitals has risen from 2003 to 2017 (Fig. 6).
Fig. 6.

Trend of prevalence of RTI among traumatic patients from 2003 to 2017.
The leave-one-out analysis showed that the minimum (29.6%) and maximum (33.5%) prevalence was observed when Hailemichael F et al./2015 [17] and Abebe GM et al./2006 [16] excluded from the overall analysis respectively (Table 2).
Table 2.
The sensitivity analysis to estimate of the prevalence of road traffic injury among trauma patients in Ethiopian Hospitals.
| Study Omitted | Prevalence (95%CI) |
|---|---|
| Bashah DT et al./2015 | 31.4 (25.0, 37.7) |
| Tiruneh BT et al./2014 | 31.2 (24.9, 37.5) |
| Ayele TA et al./2017 | 31.0 (24.7, 37.3) |
| Woldemichael K & Berhanu N/2011 | 31.6 (25.2, 38.0) |
| Abebe GM et al./2006 | 33.5 (26.8, 40.2) |
| Amdeslasie F et al./2016 | 32.7 (26.2, 39.1) |
| Hailemichael F et al./2015 | 29.6 (23.5, 35.7) |
| Wuhib Z & Tigist B/2014 | 32.1 (25.7, 38.5) |
| Osman M et al./2003 | 32.6 (25.9, 39.4) |
| Taye M & Munie T/2003 | 30.8 (25.2, 36.5) |
| Wolde A et al./2008 | 32.9 (25, 40.9) |
| Thomas F & Nebyou S./2014 | 30.1 (23.9, 36.4) |
| Kebede T et al./2008 | 32.1 (25.0, 39.1) |
| Mengistu Z & Azaj A/2012 | 30.4 (24.2, 36.7) |
| Tiruneh BTet al./2017 | 32.3 (25.8, 38.8) |
| Anderl I et al./2014 | 31.3 (24.9, 37.6) |
| Admassie D et al./2010 | 30.4 (24.2, 36.6) |
| Combined | 31.5 (25.4, 37.7) |
Discussion
This study revealed that the pooled prevalence of RTI among trauma patients in Ethiopian hospitals was 31.5%. This finding was comparable with a prevalence report in sub-Saharan Africa (32%) [9] and low- and middle-income countries (13% to 31%) [14]. Although low-income countries have nearly half of the world's vehicles, the majority of vehicles accident had been occurred in these countries [37] and the burden of RTI in the hospitals become still higher than the developed world.
Based on the regional subgroup analysis, the pooled prevalence of RTI was high in SNNPR followed by Addis Ababa, whereas low prevalence was observed in Tigray region. This discrepancy might be attributed to high traffic flow in Addis Ababa, in which by the year 2013 more than 16,422 public transportation buses were recorded [38]. In SNNPR, poor road transportation could be a contributing factor to the high burden of RTI. The lowest prevalence in Tigray region might be due to only a single study found and somehow a good road construction has been implemented in this region. In addition, the Tigray ethnic group political dominance since 1991 may leads to good road construction and a lower burden of RTI as a result. Furthermore, the low burden of RTI might be related with population size, low motorization, and strict rules and regulations on driving license accreditation [39].
Our study showed that the burden of RTI in adults higher than children. This could be related to the frequency of travelling and use of vehicles transportation in adult population. Furthermore, adults use vehicles as a source of breadwinning or income.
In agreement with the global RTI rate estimate [40], this meta-analysis revealed the increment of RTI among trauma patients from 2003 to 2017. This might be due to driving at midnight, over speeding, failing to give priority to other vehicles and pedestrians, and vehicle technical problems [41]. Besides, indaquate mechanical knowledge and skill, increasing traffic flow, inappropriate road infrastructure, not using a seatbelt, carelessness of the driver, driver age, massive road and railway construction might be attributed for the increment of RTI.
General Assembly resolution 64/2551 of March 2010 proclaimed that increasing national, regional, and global intervention is an important strategy to reduce the burden of RTI [42]. Therefore, our finding would have relevant policy implication for strengthening road safety management, safer roads and mobility, promoting to use safer vehicles, and establishing immediate post-crash response throughout the country. Standardized emergency management center and well-trained professionals in hospital are required. Further research is required to identify influencing factors of RTI in Ethiopia.
This is the first meta-analysis study of its kind and provides crucial evidence on the burden of RTI in Ethiopian hospitals. The result may not represent the national figure because of the small number of studies included in the analysis.
Conclusions
In conclusion, this study revealed that the prevalence of RTI among trauma patients was high in Ethiopian hospitals and has been increasing over time. Besides, the prevalence of RTI differed by region. Therefore, the implementation of globally recommended interventions is needed.
Author contributions
Authors contributed as follows to the conception or design of the work; the acquisition, analysis, or interpretation of data for the work; and drafting the work or revising it critically for important intellectual content: AE contributed 80%; TDH, AA, AD and YB each contributed 5%. All authors approved the version to be published and agreed to be accountable for all aspects of the work.
Conflict of interest
The authors declare no conflicts of interest.
Footnotes
Peer review under responsibility of African Federation for Emergency Medicine.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.afjem.2019.01.013.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Murray C.J., Vos T., Lozano R., Naghavi M., Flaxman A.D., Michaud C. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. lancet. 2012;380(9859):2197–2223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 2.Finkelstein E., Corso P.S., Miller T.R. Oxford University Press, USA; 2006. The incidence and economic burden of injuries in the United States. [Google Scholar]
- 3.Commission for Global Road Safety. Safe roads for all: a post-2015 agend for health and development: Foundation for the Automobile & Society (FIA). London, UK; 2013.
- 4.World Health Organization. Global status report on road safety. Geneva, Switzerland; 2013.
- 5.Toroyan T. Global status report on road safety: Time for action. WHO. 2009 doi: 10.1136/ip.2009.023697. [DOI] [PubMed] [Google Scholar]
- 6.Peden M, Scurfield R, Sleet D, Mohan D, Hyder AA, Jarawan E, et al. World report on road traffic injury prevention. World Health Organization Geneva; 2004.
- 7.Paniker J., Graham S.M., Harrison J.W. Global trauma: the great divide. SICOT-J. 2015;1 doi: 10.1051/sicotj/2015019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization. World report on road traffic injury prevention. Geneva, Switzerland; 2004.
- 9.Vissoci J.R.N., Shogilev D.J., Krebs E., Andrade Ld., Vieira I.F., Toomey N. Road traffic injury in Sub-Saharan African countries: a systematic review and summary of observational studies. Traffic Injury Prevention. 2017;18(7):767–1763. doi: 10.1080/15389588.2017.1314470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hazen A., Ehiri J.E. Road traffic injuries: hidden epidemic in less developed countries. J Natl Med Assoc. 2006;98(1):73. [PMC free article] [PubMed] [Google Scholar]
- 11.Bhalla K., Shotten M., Cohen A., Brauer M., Shahraz S., Burnett R. Transport for health: the global burden of disease from motorized road transport. TRID. 2014;1(1):39. [Google Scholar]
- 12.World Health Organization. Global status report on road safety: time for action. Geneva, Switzerland: 2009.
- 13.Alemu M.H. Patterns of pre hospital fatal injuries in Mekelle, Ethiopia. Ethiopian Med J. 2008;46(2):179–183. [PubMed] [Google Scholar]
- 14.Odero W., Garner P., Zwi A. Road traffic injuries in developing countries: a comprehensive review of epidemiological studies. Trop Med Int Health. 1997;2(5):445–460. [PubMed] [Google Scholar]
- 15.Brubacher J.R.C.H., Brasher P., Erdelyi S., Desapriya E., Asbridge M. Reduction in fatalities, ambulance calls, and hospital admissions for road trauma after implementation of new traffic laws. Am J Public Health. 2014;104(10):e89–e97. doi: 10.2105/AJPH.2014.302068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Abebe G.-M., Minas W.-S., Gutema J. Patterns of accidents among children visiting Jimma University Hospital, South West of Ethiopia. Ethiop Med J. 2006;44(4):339–345. [PubMed] [Google Scholar]
- 17.Hailemichael F., Suleiman M., Pauolos W. Magnitude and outcomes of road traffic accidents at Hospitals in Wolaita Zone, SNNPR, Ethiopia. BMC Res Notes. 2015;8(1):135. doi: 10.1186/s13104-015-1094-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tiruneh B.T., Dachew B.A. Bifftu BB. Incidence of road traffic injury and associated factors among patients visiting the emergency department of Tikur Anbessa specialized teaching hospital, Addis Ababa, Ethiopia. Emergency Med Int. 2014;2014 doi: 10.1155/2014/439818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wuhib Z., Tigist B. Addis Ababa University Ethiopia; 2014. A cross-sectional study to assess the patterns of childhood injuries at TikurAnbessa Hospital. [Google Scholar]
- 20.Taye M., Munie T. Trauma registry in Tikur Anbessa Hospital, Addis Ababa, Ethiopia. Ethiopian Med J. 2003;41(3):221–226. [PubMed] [Google Scholar]
- 21.Wolde A., Abdella K., Ahmed E., Tsegaye F., Babaniyi O., Kobusingye O. Pattern of injuries in Addis Ababa, Ethiopia: a one-year descriptive study. East Central Afr J Surgery. 2008;13(2):14–22. [Google Scholar]
- 22.Kebede T., Mekonene T., Bartolemes K., Taye M., Munie T., Meleses M. Injury surveillance in six hospitals of Addis Ababa, Ethiopia. Ethiopian Med J. 2008;46(4):383–390. [PubMed] [Google Scholar]
- 23.Mengistu Z., Azaj A. Trauma severities scores and their prediction of outcome among trauma patients in two hospitals of Addis Ababa, Ethiopia. Ethiopian Med J. 2012;50(3):231–237. [PubMed] [Google Scholar]
- 24.Admassie D., Yirga T., Wamisho B.L. Brief communication: Adult limb fractures in Tikur Anbessa Hospital caused by road traffic injuries: Half year plain radiographic pattern. Ethiopian J Health Dev. 2010;24(1) [Google Scholar]
- 25.PRISMA. PRISMA transparent reporting of systematic reviews and meta‐analyses. 2011. Available from http://www.prisma-statement.org/documents/PRISMA-P.
- 26.Joanna Briggs Institute. Critical Appraisal Tools Australia: The University of Adelaide; 2018. Available from: http://joannabriggs.org/research/critical-appraisal-tools.html.
- 27.Egger M., Smith G.D., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Borenstein M., Hedges L.V., Higgins J., Rothstein H.R. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synthesis Methods. 2010;1(2):97–111. doi: 10.1002/jrsm.12. [DOI] [PubMed] [Google Scholar]
- 29.Osman M., Kebede Y., Anberbir S. Magnitude and pattern of injuries in north Gondar administrative zone, northwest Ethiopia. Ethiop Med J. 2003;41(3):213–220. [PubMed] [Google Scholar]
- 30.Bashah D.T., Dachew B.A., Tiruneh B.T. Prevalence of injury and associated factors among patients visiting the Emergency Departments of Amhara Regional State Referral Hospitals, Ethiopia: a cross-sectional study. Bmc Emergency Med. 2015;15(1):20. doi: 10.1186/s12873-015-0044-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ayele T.A., Zeleke B.M., Tessema G.A., Melak M.F. Magnitude and patterns of injuries among patients in Gondar University Hospital, northwest Ethiopia: an institutional-based study. Open Access Surgery. 2017;10:25–31. [Google Scholar]
- 32.Woldemichael K., Berhanu N. Magnitude and pattern of injury in jimma university specialized hospital, South West Ethiopia. Ethiopian J Health Sci. 2011;21(3) [PMC free article] [PubMed] [Google Scholar]
- 33.Amdeslasie F., Kidanu M., Lerebo W., Ali D. Patterns of trauma in patient seen at the emergency clinics of public hospitals in Mekelle, northern Ethiopia. Ethiop Med J. 2016;54(2) [PubMed] [Google Scholar]
- 34.Thomas Fako N. Pattern of injuries and associated factors in patients visiting the emergency department of Hawassa university referral hospital; 2014.
- 35.Aenderl I., Gashaw T., Siebeck M., Mutschler W. Head injury-a neglected public health problem: a four-month prospective study at Jimma University specialized hospital, Ethiopia. Ethiopian J Health Sci. 2014;24(1):27–34. doi: 10.4314/ejhs.v24i1.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tiruneh B.T. State. University of Gondar; Ethiopia: 2017. Factors associated with unintentional injury among the paediatric age population in the hospitals of amhara national regional. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.World Health Organization. Global status Report on Road Safety. Geneva, Switzerland; 2015.
- 38.Number of Passenger Cars in Addis Ababa [press release]. 2013. Available from http://www.nationmaster.com/country-info/profiles/Ethiopia/Transport.
- 39.International Organization for Migration. Country Fact Sheet Ethiopia. 2014. Available from https://www.iom.int/countries/ethiopia.
- 40.Adeloye D., Thompson J.Y., Akanbi M.A., Azuh D., Samuel V., Omoregbe N. The burden of road traffic crashes, injuries and deaths in Africa: a systematic review and meta-analysis. Bull World Health Organ. 2016;94(7):510. doi: 10.2471/BLT.15.163121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Asefa F., Assefa D., Tesfaye G. Magnitude of, trends in, and associated factors of road traffic collision in central Ethiopia. BMC Public Health. 2014;14(1):1072. doi: 10.1186/1471-2458-14-1072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.World Health Organization. Global Plan for the Decade of Action for Road Safety 2011-2020. Geneva, Switzerland: 2011.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.