Abstract
Introduction
Injury and violence are neglected global health concerns, despite being largely predictable and therefor preventable. We conducted a small study to indirectly describe and compare the perception of availability of resources to manage major trauma in high-income, and low- and middle-income countries using evidence-based guidance (as per the 2016 National Institute of Clinical Excellence guidelines), as self-reported by delegates attending the 2016 International Conference on Emergency Medicine held in South Africa.
Methods
A survey was distributed to delegates at the International Conference on Emergency Medicine 2016. The survey instrument captured responses from participants working in both pre- and in-hospital settings. Responses were grouped according to income group (either high-income, or low- and middle-income) based on the respondent’s nationality (using the World Bank definition for income group). A Fisher’s Exact test was conducted to compare responses between different income groups.
Results
The survey was distributed to 980 delegates, and 392 (40%) responded. A total of 206 (53%) respondents were from high-income countries and 186 (47%) were from low- to middle-income countries. Respondents described significantly less access to resources and services for low- and middle-income countries to adequately care for major trauma patients both pre- and in-hospital when compared to high-income countries. Shortages ranged from consumables to analgesia, imaging to specialist services, and pre-hospital to in-hospital care.
Conclusion
Major trauma care requires a chain of successful, evidence-based events for outcomes to benefit. This small study suggests that many of the links of this chain are either missing or broken within low- and middle-income countries. These settings simply do not benefit from the currently available evidence-base in major trauma care. It is important that this evidence-base also be evaluated within low- and middle-income countries. The capacity of low- and middle-income country emergency care systems also needs better describing.
Keywords: Self-report, Specialization, Global health, Income, Emergency medicine, Developed countries
African relevance
-
•
Resource restriction is a major concern for major trauma care in low- and middle-income countries.
-
•
Current accepted reference standards provide little room for clinicians working in these countries.
-
•
More research is required to describe the problem of resource restrictions in LMICs.
Introduction
Injury and violence are neglected global health concerns, despite being largely predictable and therefor preventable [1]. According to the World Health Organisation (WHO), road traffic injuries account for 1.3 million deaths annually and are likely to rise from the ninth leading (2004), to the third leading cause of disability worldwide by 2030 [1]. Even more poignant, road traffic injuries and other forms of trauma are significant health issues within low- to middle-income countries (LMICs), where the burden of death and disability are notably higher than elsewhere [2], [3], [4]. This disproportionately higher burden in LMICs, coupled with multiple barriers to provide evidence-based trauma care (lack of systems, staff, consumables, infrastructure, etc.) simply translate to poor outcomes for the injured patients in these regions [5], [6], [7]. There are little data on the resource availability to implement the evidence-based injury guidance commonly adhered to in high-income countries (HICs) in countries within lower income categories. It is unlikely that policies and evidence-based guidelines developed in HIC settings can meaningfully apply in LMIC settings as a result, thus depriving these communities (which makes up a substantial proportion of the global population) from this rapidly developing evidence base [8], [9].
We conducted a small study to indirectly describe and compare the perception of availability of resources to manage major trauma in HICs and LMICs using evidence-based guidance, as self-reported by delegates attending the 2016 International Conference on Emergency Medicine held in Cape Town, South Africa, using the 2016 National Institute of Clinical Excellence (NICE) guidelines for the management of patients with major trauma.
Methods
A survey was distributed to delegates at the International Conference on Emergency Medicine 2016, Cape Town to achieve the study aim. The survey instrument was based on the 2016 National Institute of Clinical Excellence (NICE) guidelines for the management of patients with major trauma as the best summary of current evidence-based major trauma care [10]. We initially considered using the World Health Organization’s Guidelines for Essential Trauma Care [11]. However, this was published in 2004 and as such cannot be considered evidence-based [11]. We did not consider other guidelines. The survey captured both resource availability in the pre-hospital and in-hospital settings and was piloted prior to use in the study (available as appendix in the data supplement). Descriptive statistics were used to describe the study variables for both the pre-hospital and in-hospital parts of the survey. Participants were required to indicate availability of a resource in their practice setting using the following responses: always, sometimes, never, don’t know. Responses were then grouped according to income group (HIC or LMIC) based on the participant’s stated practice country (using the World Bank definition for income group). A Fisher’s Exact test was conducted to compare participant responses. Key findings are presented in table format using the key recommendations from the 2016 NICE guidelines as a guide. Only always-responses (where resources are consistently available) are reported in the table included in the paper. The full dataset is tabulated in the appendix (data supplement) The study received ethical approval from the University of Cape Town Human Research Ethics Committee (110/2016).
Results
The survey was distributed to 980 delegates, and 392 (40%) responded. A total of 206 (53%) respondents were from HICs and 186 (47%) were from LMICs. Male respondents accounted for 223 (57%) of respondents and the mean age of the sample was 42 years (SD = 10.7 years). A higher proportion of specialist physicians were from HICs (160, 78%) versus LIMCs (90, 48%) (p ≤ 0001). The majority of respondents, from both groups, worked in the public sector: 165 (80%) from HICs and 115 (62%) from LMICs (p < 0.0001). Notably, a larger proportion of LMIC respondents worked in privately-funded institutions: 48 (26%) versus HICs 12 (6%) (p < 0.0001). More than half of the respondents (220, 56%) worked in a tertiary institution, of which 133 (60%) were from HICs and 87 (40%) from LMICs. A higher proportion of LMIC respondents, compared to HIC respondents, reported the lack of a prehospital service in their region – 79% versus 21% respectively. There were 105 (27%) respondents who practised in a prehospital setting.
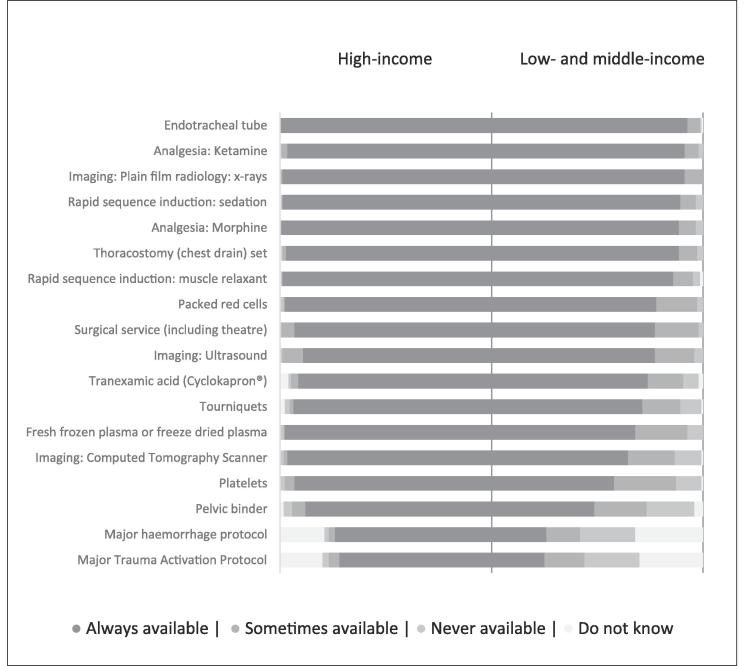
Table 1 provides the self-reported pre- and in-hospital resource and service availability between respondents from high-income countries and low- and middle-income countries. Fig. 1, Fig. 2 provide a visualisation of self-reported pre- and in-hospital resource and service availability, ranked for reported availability of respondents from low- and middle-income countries, compared with those of high-income countries. Detailed findings are available as Tables 1-3 in the appendix (data supplement).
Table 1.
Pre- and in-hospital resources and services that are always available for the management of major trauma; as self-reported by participants from high-income, and low- and middle-income countries.
| High-income country responses |
Pre- and in-hospital resource or service variables | Low- and middle-income country responses |
||
|---|---|---|---|---|
| n | % | Immediate destination after injury | n | % |
| 37 | 93% | Pre-hospital triage Protocol*** | 40 | 62% |
| 36 | 90% | Pre-arrival Major Trauma Notification Protocol*** | 19 | 29% |
| 126 | 72% | In-hospital Major Trauma Activation Protocol*** | 38 | 25% |
| n | % | Airway management in pre-hospital and in-hospital settings | n | % |
| 33 | 83% | Pre-hospital rapid sequence induction: sedation*** | 25 | 38% |
| 24 | 60% | Pre-hospital rapid sequence induction: muscle relaxant** | 21 | 32% |
| 34 | 85% | Pre-hospital endotracheal tube** | 38 | 58% |
| 35 | 88% | Pre-hospital supraglottic airways (e.g. laryngeal mask)*** | 30 | 46% |
| 173 | 99% | In-hospital rapid sequence induction: sedation*** | 134 | 89% |
| 173 | 99% | In-hospital rapid sequence induction: muscle relaxant*** | 129 | 86% |
| 175 | 100% | In-hospital endotracheal tube*** | 139 | 93% |
| n | % | Management of chest trauma in pre-hospital and in-hospital settings | n | % |
| 28 | 70% | Pre-hospital chest injury management guideline*** | 17 | 26% |
| 40 | 100% | Pre-hospital IV cannula** | 52 | 80% |
| 19 | 48% | Pre-hospital thoracostomy (chest drain) set*** | 12 | 18% |
| 170 | 97% | In-hospital thoracostomy (chest drain) set** | 133 | 89% |
| 156 | 89% | In-hospital imaging: Ultrasound* | 116 | 77% |
| 173 | 99% | In-hospital imaging: Plain film radiology: x-rays** | 137 | 91% |
| 169 | 97% | In-hospital imaging: Computed Tomography Scanner (CT-scan)*** | 97 | 65% |
| n | % | Management of haemorrhage in pre-hospital and in-hospital settings | n | % |
| 31 | 78% | Pre-hospital tourniquets | 35 | 54% |
| 31 | 78% | Pre-hospital pelvic binder*** | 18 | 28% |
| 12 | 30% | Pre-hospital Tranexamic acid (Cyclokapron®)* | 8 | 12% |
| 38 | 95% | Pre-hospital IV fluids: Isotonic crystalloids (e.g. Saline) | 53 | 82% |
| 164 | 94% | In-hospital tourniquets*** | 107 | 71% |
| 154 | 88% | In-hospital pelvic binder*** | 73 | 49% |
| 160 | 91% | In-hospital Tranexamic acid (Cyclokapron®)*** | 111 | 74% |
| 129 | 74% | In-hospital major haemorrhage protocol*** | 39 | 26% |
| 171 | 98% | In-hospital packed red cells*** | 117 | 78% |
| 171 | 98% | In-hospital fresh frozen plasma (or freeze dried plasma)*** | 102 | 68% |
| 163 | 93% | In-hospital platelets*** | 87 | 58% |
| 163 | 93% | In-hospital surgical service (including theatre)*** | 116 | 77% |
| (see ultrasound, x-ray and CT scan availability above) | ||||
| n | % | Pain management in pre-hospital and in-hospital settings | n | % |
| 17 | 43% | Pre-hospital analgesia: Morphine*** | 8 | 12% |
| 33 | 83% | Pre-hospital analgesia: Ketamine*** | 29 | 45% |
| 174 | 99% | In-hospital analgesia: Morphine | 133 | 89% |
| 169 | 97% | In-hospital analgesia: Ketamine*** | 137 | 91% |
*, p < 0.05; **, p < 0.01; p < 0.001.
Fig. 1.
Visualisation of self-reported pre-hospital resource and service availability, ranked for reported availability of delegates from low- and middle-income countries, compared with those of high-income countries.
Fig. 2.
Visualisation of self-reported in-hospital resource and service availability, ranked for reported availability of delegates from low- and middle-income countries, compared with those of high-income countries.
Discussion
A significant perceived discrepancy were described between the self-reported resources and services available respectively to HICs and LMICs to adequately care for major trauma patients using current, evidence-based guidance in this small study. Shortages ranged over a wide range of items, from consumables to analgesia, imaging to specialist services, both pre-hospital and in-hospital. Although the finding of lower resource availability in LMICs was not altogether surprising, the sheer extend of the reported findings were. This is problematic as this study suggests that LMICs – which make up around 82% of the world’s population – apparently do not have access to evidence-based trauma practice. [12] We believe that many healthcare workers in LMICs would be able to relate to these results.
Fig. 1 reveals some variables that should be relatively easy to address such as simply addressing the lack of treatment protocols (even if this is based on the WHO Guidelines for Essential Trauma Care). Major trauma activation criteria and major haemorrhage protocols where implemented can guide best available care in most income settings. Often this means considering the reasonable outcomes that can be achieved given the resources available, and then optimising what is available. It was disappointing to see that these were uncommonly available (even in HICs). Tranexamic acid is fairly inexpensive and linen sheets can be used to proxy as a pelvic binder. Arguably access to blood products and a round-the-clock surgical service are more challenging.
Another interesting observation was that despite a larger proportion of LMIC respondents working in private institutions, resources were still reported as insufficient. This difference can likely be described as non-adherence to evidence-based practice (which may be connected to the lower proportion of specialists in the LMIC cohort). The growth of emergency medicine as a specialty in LMICs would likely present an opportunity for LMICs to better balance available resources with the best available evidence.
There are a number of limitations to this study, and these were largely the reason we decided to publish the findings as a short report. These include the small sample size and low response rate. A larger study would provide more validity to the findings. We expected a better response rate, and it is not exactly clear why this wasn’t better. That said, the findings confirm anecdotal evidence. The large gap between LMIC and HIC responses, and the consistency of the answers are fairly convincing despite the study sample and response rate. We do not believe a larger study would yield substantially different findings. Self-reporting of resources is unlikely to be as robust as actual measurement. Sadly, these data are not well-reported in the literature. These findings should serve as a call to action for fledgling emergency care programmes in LMICs to record and publish access to resources.
Conclusions
Major trauma care requires a chain of successful, evidence-based events for outcomes to benefit. This small study suggests that many of the links of this chain are either missing or broken within LMICs. These settings simply do not benefit from the currently available evidence-base in major trauma care. It is important that this evidence-base be evaluated within LMIC settings in order to determine the value it would contribute to outcome. This would help prioritising of resources. Systems research is required, specifically research that describes the capacity of LMIC emergency care systems. Such work will go a long way to shape future major trauma guidelines. Finally, location-specific research is required that can address specific injury-patterns that are endemic to certain regions. This would help find alternate solutions that are less dependent on the HIC evidence-base, but with similar (or better) outcomes.
Dissemination of results
Results from this study was shared with the Division of Emergency Medicine at both the University of Stellenbosch and the University of Cape Town – Results were subsequently shared with local hospitals. The results were also presented at informal academic meetings at local hospitals.
Author contribution
Authors contributed as follow to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; drafting the work or revising it critically for important intellectual content; and final approval of the version to be published: AA 35%, CH 25% and SB 40%. All authors agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Grant support
The study was funded by the authors. No external funding was received.
Conflict of interest
Drs Clint Hendrikse and Stevan Bruijns are editors of African Journal of Emergency Medicine. Neither were involved in the editorial workflow for this manuscript. The African Journal of Emergency Medicine applies a double blinded process for all manuscript peer reviews. The authors declared no further conflict of interest.
Footnotes
Peer review under responsibility of African Federation for Emergency Medicine.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.afjem.2019.01.004.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.The World Health Organization. The global burden of disease 2004. [cited 2015 Dec 27]. Available from: http://www.who.int/healthinfo/global_burden_disease/GBD_report_2004update_full.pdf.
- 2.Peden M, McGee K, Krug E. Injury: a leading cause of the global burden of disease. [cited 2015 Dec 27]. Available from: http://www.who.int/violence_injury_prevention/publications/other_injury/injury/en/.
- 3.Krug E.G., Sharma G.K., Lozano R. The global burden of injuries. Am J Public Health. 2000;90(4):523–526. doi: 10.2105/ajph.90.4.523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mock C., Quansah R., Krishnan R. Strengthening the prevention and care of injuries worldwide. Lancet. 2004;363(9427):2172–2179. doi: 10.1016/S0140-6736(04)16510-0. [DOI] [PubMed] [Google Scholar]
- 5.Gosselin R. Injuries: the neglected burden in developing countries. Bull World Health Organ. 2009;87(4):246. doi: 10.2471/BLT.08.052290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mock C.N., Jurkovich G.J., Nii-Amon-Kotei D., Arreola-Risa C., Maier R.V. Trauma mortality patterns in three nations at different economic levels: implications for global trauma system development. J Trauma. 1998;44(5):804–812. doi: 10.1097/00005373-199805000-00011. [DOI] [PubMed] [Google Scholar]
- 7.Reynolds T.A., Stewart B., Drewett I. The impact of trauma care systems in low- and middle-income countries. Annu Rev Public Health. 2017;38:507–532. doi: 10.1146/annurev-publhealth-032315-021412. [DOI] [PubMed] [Google Scholar]
- 8.Wisborg T., Montshiwa T.R., Mock C. Trauma research in low- and middle-income countries is urgently needed to strengthen the chain of survival. Scand J Trauma Resusc Emerg Med. 2011;19:62. doi: 10.1186/1757-7241-19-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Henry J.A., Reingold A.L. Prehospital trauma systems reduce mortality in developing countries. J Trauma Acute Care Surg. 2012;73(1):261–268. doi: 10.1097/TA.0b013e31824bde1e. [DOI] [PubMed] [Google Scholar]
- 10.National Institute of Clinical Excellence. Major trauma: assessment and initial management: NICE guideline NG39 [Internet]. 2016 [cited 2018 October 09]. Available from: https://www.nice.org.uk/guidance/ng39.
- 11.World Health Organization. Guidelines for Essential Trauma Care [Internet]. 2004 [cited 2017 December 11]. Available from: http://apps.who.int/iris/bitstream/10665/42565/1/9241546409_eng.pdf.
- 12.World Health Organization. Global Health Observatory data repository [Internet]. [cited 2017 December 11]. Available from: http://apps.who.int/gho/data/view.main.POP2030.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.