Abstract
Introduction
Trauma accounts for a significant proportion of the global burden of disease, with highest mortality rates seen in Africa. This epidemic is predicted to increase with urbanisation and an aim of the Sustainable Development Goals is to reduce deaths and trauma caused by road accidents. Data available on urban trauma in Sierra Leone is limited.
Methods
We conducted a retrospective observational study of trauma and injury related presentations to the emergency centre (EC) of Connaught Hospital, the principal adult tertiary referral centre in Freetown, Sierra Leone between January and March 2016. Patient demographics are described with mechanism of injury. Additional data on length of stay and surgical procedures were recorded for admissions to the trauma ward.
Results
During the 3-month period, a total of 340 patients with injury presented to the EC, accounting for 11.6% of total attendances and 68% of adult surgical admissions. The majority were male (66%) and mean age was 26 years (IQR 15–40). The proportion of trauma presentations were higher in the evening and at weekends and 41% of patients were triaged as emergency or very urgent cases. Road traffic accidents were the most frequent cause of injury (55%) followed by falls (17%) and assaults (14%). Burns were more common in children. Head and lower limbs were the most commonly injured body parts and a minority of patients underwent surgical procedures. Median length of stay for adult patients was 4.5 days (IQR 2–11) and 7 days (IQR 4–14) for children.
Discussion
Injury accounts for a high burden of disease at Connaught Hospital and consumes a significant proportion of EC and hospital resources. Efforts should be directed towards strengthening the pre-hospital and emergency trauma systems with accurate, formal data collection as well as targeting injury prevention initiatives and improving road safety to reduce morbidity and mortality.
Keywords: Trauma, Injury, Africa, Sierra Leone, Emergency department, Registry
African relevance
-
•
Trauma accounts for significant morbidity and mortality in the majority of African countries.
-
•
The burden of trauma is poorly described in many African countries.
-
•
The aetiology and numbers of trauma cases presenting as emergencies in Freetown have not been previously analysed.
Introduction
It is estimated that injury is responsible for 10% of the global burden of disease [1], resulting in around 5 million deaths annually [2], 90% of which occur in low and middle income countries [3]. Road traffic injuries are the leading cause of death in people aged 15–29 years [4], [5] with the World Health Organization (WHO) Africa Region having the highest fatality rate worldwide [6]. In addition to mortality, injury is associated with a high burden of morbidity and economic cost accounting for 6% of global years lived with disability [7].
Sierra Leone is a country situated on the West coast of Africa with a population of just over 7 million people. It is amongst the world’s poorest countries, ranked 179 out of 188 countries in the Human Development Index with a life expectancy of 53 years [8] with injury representing 7% of the burden of disease [9] and responsible for an estimated 325,000 deaths [10]. It is currently recovering from the worst Ebola epidemic on record during which 221 health care workers lost their lives [11] and medical and surgical services were severely disrupted across the country, including at the only adult tertiary referral centre [12]. Even prior to the epidemic, trauma and emergency capacity were limited [13], [14], with a yearly non-fatal injury prevalence of 12.4% and fatal injury prevalence of 5.6% [10].
The emphasis is now on health sector recovery and capacity building, with Emergency Care included as an Essential Health Service [15] and the establishment of a National Medical Emergency Service [11] and strengthening of the referral system as part of the country’s National Recovery Plan. The World Health Assembly resolution 60.22 highlights the need for strengthening emergency care systems to reduce the burden of disease from acute injury and illness [16] and one of the aims of the Sustainable Development Goals is to halve the number of global deaths and injuries from road traffic accidents [17] by 2020.
With this in mind, Connaught Hospital, the only adult government referral hospital in Sierra Leone has re-opened its refurbished emergency centre, used as an Ebola isolation unit during the epidemic, and is in the process of strengthening its trauma service. Data on the burden of trauma in Freetown, the capital of Sierra Leone is limited. There is currently no formal trauma registry and no established pre-hospital emergency service. The aim of this study was to assess the volume of trauma presenting to the national referral hospital in order to focus resources, direct training and lobby for improved preventive measures.
Methods
Connaught Hospital is the national government referral hospital based in the capital, Freetown. With 300 beds, it is the only adult tertiary care centre in the country and serves a local population of 2 million people. It provides both adult and paediatric surgical services, acute medicine including treatment for HIV and TB and has recently opened a refurbished emergency centre (EC) and trauma admissions unit. King’s Sierra Leone Partnership is a capacity-building organisation which has been working in partnership with Connaught in-country to improve health and health services, including emergency care, in Sierra Leone since 2013.
We conducted a retrospective observational study of the trauma-related EC attendances and subsequent admissions to the acute trauma ward between January and March 2016, just under 2 months after the country was initially declared free of Ebola. A standardised data collection tool was developed to include information on patient demographics, triage classification, injury details including mechanism and body region affected and, for those admitted, we examined surgical interventions and length of stay.
Multiple sources of data were utilised to ensure adequate reliability. Emergency centre attendance data was collected from registers in the triage office and EC clinicians’ consultation rooms. For patients admitted to hospital, additional data was sourced from admission ledgers, ward registers and nurses’ handover documents from all surgical wards in the hospital including the paediatric ward. Finally, data was collected from patient case notes for those admitted to the wards and emergency centre record cards for those discharged from EC. We included all adults and children whose presenting complaint involved trauma, injury or burns and excluded patients attending for follow up consultation.
Data was collected manually, cross checked to avoid duplication and collated anonymously on Excel spreadsheet for analysis. Categorical data were expressed as percentages, while continuous data were expressed in terms of means and medians with interquartile ranges (IQR) as appropriate. Categorical variables were compared using the chi-squared test with statistical significance assumed when p < 0.05. Permission for the study was granted by the Sierra Leone Ethics and Scientific Review Committee.
Results
Over the 3-month study period, a total of 2928 patients were triaged at the EC of which 340 (11.6%) were trauma related attendances (Fig. 1). 66% of these injured patients were male and the mean age was 26 years with age 15–29 years being the most common group to present and children under the age of 15 accounting for 15% of presentations (Table 1). Age was not documented in 18.8% of cases and 22.6% of patients were documented only as adult when patients were not able to give an accurate date of birth.
Fig. 1.
Trauma attendance flow chart.
Table 1.
Basic demographics of patients with injury presenting to the emergency centre.
| Category | n [340] (%) |
|---|---|
| Sex | |
| Male | 224 (65.8) |
| Female | 115 (33.8) |
| Unknown | 1 (0.3) |
| Age (years) | |
| Child | 3 (0.9) |
| 0–14 | 48 (14.1) |
| 15–29 | 70 (20.6) |
| 30–45 | 47 (13.8) |
| >45 | 31 (9.1) |
| Adult | 77 (22.6) |
| Unknown | 64 (18.8) |
| Triage Category | |
| Green | 74 (21.8) |
| Yellow | 120 (35.3) |
| Orange | 93 (27.4) |
| Red | 46 (13.5) |
| Unknown | 7 (2.1) |
| Day of Presentation | |
| Monday | 52 (15.3) |
| Tuesday | 53 (15.6) |
| Wednesday | 65 (19.1) |
| Thursday | 52 (15.3) |
| Friday | 48 (14.1) |
| Saturday | 32 (9.4) |
| Sunday | 38 (11.1) |
| Time of Presentation | |
| Early Shift (0800–1400) | 125 (36.7) |
| Late Shift (1400–2200) | 135 (39.7) |
| Night Shift (2200–0800) | 77 (22.6) |
| Unknown | 3 (0.9) |
Patients were triaged on arrival using the South African Triage Scale (SATS) [18]. Fourteen percent of patients were categorised as triage category red (emergency) and 27% were category orange (very urgent). The evening shift [1400–2000] was the busiest time for trauma presentations with 40% of total injury related attendances. In addition, red and orange cases accounted for 52% of all presentations on the evening shift and 44% during the night shift compared to only 27% of patients that present during the early shift [0800–1400] (p < 0.001). While trauma attendances were lower in absolute numbers at weekends compared to weekdays, the proportion of injury related presentations attending the EC was higher at weekends (17.9% of all presentations) compared to 10.6% of weekday attendances (p < 0.001).
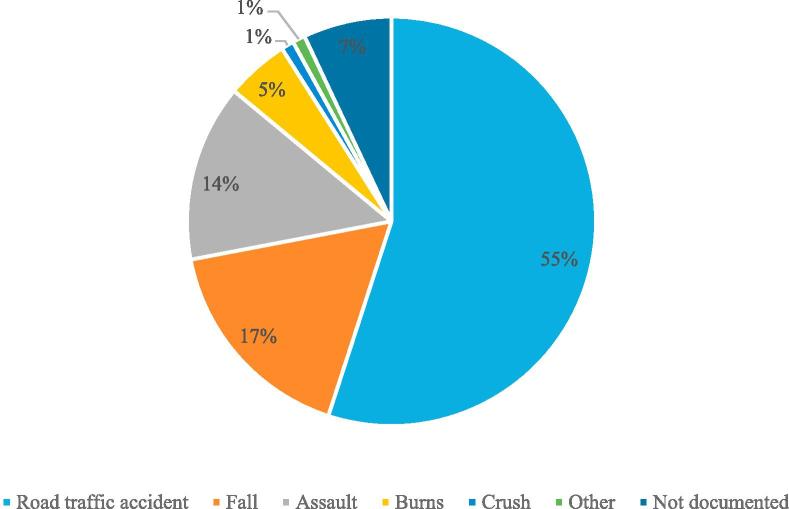
The most common mechanism of injury was road traffic accident which was responsible for 55% of injuries (Fig. 2), followed by falls (17%) and then assaults (14%). Of the assaults, 43% were due to penetrating trauma (17 stabbings and 3 gunshot wounds), 19% were blunt trauma and the remainder did not have a mechanism documented. Looking specifically at children (age less than 16), road traffic accident remained most common (41%) followed by falls (25%) but burns was the third most common cause for presentation with 16% of attendances.
Fig. 2.
Mechanism of injury.
After triage, patients were assessed by a clinician. The majority of patients were seen by doctors (53%) while Community Health Officers (CHO) saw 44% of patients and there was no record in 3% of cases. Of those cases that were seen by a doctor, 71% were assessed by a house officer and the remainder were seen by a medical officer. 19% of category red (emergency) and orange (very urgent) were seen by a medical officer, the rest were seen by house officer or CHO.
Of the 340 injured patients that presented to Connaught during the study period, 154 (45%) were admitted, representing 68% of all adult surgical admissions and 27% of total paediatric admissions. Seventy percent of admissions were patients that had presented directly to the hospital, the remainder were referred from other hospitals around the country. In-patient records were available for 72% (n = 96) of adult patients and all paediatric patients. For adult in-patients, where data was available for mechanism of injury and body area injured (Table 2), we identified that head injury was the most common primary presenting injury (41%) followed by injury to the lower limbs (22%).
Table 2.
Primary body region injured in adult trauma admissions.
| Body Area Injured | No. of Patients = N [96] (%) |
|---|---|
| Head | 39 (40.6) |
| Lower Limb | 21 (21.9) |
| Upper Limb | 8 (8.3) |
| Pelvis/Hips | 8 (8.3) |
| Neck/Spine | 7 (7.3) |
| Trunk | 7 (7.3) |
| Eye | 2 (2.1) |
| Multiple Injuries | 2 (2.1) |
| Other | 2 (2.1) |
There were 5 surgical procedures undertaken in the adult patients; 1 exploratory laparotomy for stab wound, 1 open fracture reduction and fixation and 3 wound debridements including 1 limb amputation. Six paediatric patients underwent surgery including reduction of supracondylar fracture, drainage of haematoma and 4 maxillofacial procedures.
The median length of stay for adult patients was 4.5 days (IQR 2–11). The longest stay was a patient with a neck of femur fracture that was admitted for 55 days. It was interesting to note that a total of 49 patients (51%) either self-discharged or were taken by family against medical advice. The median length of stay for children was 7 days (IQR 4–14) with an in-patient mortality rate of 23%. Data on adult mortality was not available.
Discussion
Our study demonstrates that trauma accounts for a significant burden of disease in Sierra Leone, accounting for 11.6% of all emergency centre attendances at the main government referral hospital. Almost half of these injured patients are subsequently admitted to hospital and make up two-thirds of all adult surgical admissions and 30% of paediatric surgical admissions. We found that trauma patients are predominantly male and young with the majority aged less than 45 years old. These findings are in keeping with a recent population-based survey [10] and similar to attendance demographics from other African low and middle income referral centres in Malawi [19], Mozambique [20], Zambia [21] and Botswana [22]. The study from Botswana found that trauma represented between 6 and 10% of emergency admissions across 5 centres. A recent South African study [23] analysed data from the District Health Information System on trauma attendances to emergency centres in KwaZulu-Natal. This found that 27% of emergency centre visits were trauma related with injured patients accounting for 2.4% of admissions. This is in a region with a predicted annual trauma incidence of 12.0 per 1000 population and a higher rate of inter-personal violence [24]. The high admission rate in our study could be explained by a number of factors. As well as Connaught receiving referrals from other district hospitals, patients may often access hospital care late when pathology is complex and advanced or attendance may only be prompted by more significant injury. The fact that 41% of patients that attended the EC were triaged as emergency or very urgent categories adds strength to this argument.
We found that trauma accounts for a higher proportion of overall EC attendances in the evening and overnight and these presentations are of higher acuity than those that present during the morning shift. There is little data reported in the literature describing triage severity scores in trauma patients or the time of day that they present in low-income settings so our study is fairly unique in this respect. These findings could be due to patients arriving later in the day from surrounding districts or referral hospitals as well as violence and accidents occurring more frequently at night when drivers and riders are fatigued and alcohol or other illicit substances may be contributing factors. This has implications for service provision and design as staffing numbers and seniority are generally higher during the dayshift. Even during this period, many severely injured patients are being initially assessed and managed by junior medical staff.
We found that road traffic accidents were the most common cause of injury overall, followed by falls and then assaults. It is not surprising that injuries due to traffic accidents were so common, low-income countries across Africa are currently experiencing a dramatic increase in traffic related trauma and Sierra Leone is no different [24]. The reasons for this are multi-factorial including an increasing number of vehicles on the roads [25] driven by poorly trained drivers and riders, inadequate transport infrastructure to accommodate this growth and poor enforcement of safety legislation [5]. Many roads in Freetown do not have pavements and pedestrians are forced to walk among the traffic and petty trading occurs along the streets of big cities like Freetown. In addition, during the Ebola epidemic, the use of motorbike taxis increased within the city with passengers reluctant to wear helmets for fear of infection.
A cross-sectional survey conducted in 2012 [10] found that falls were the most common cause of non-fatal injuries (40%), followed by wounds from blunt trauma and then burns. Road traffic injuries were the 4th most common cause of injury but the leading cause of death. This differs from our study but this could be explained by traffic related injuries being more severe and requiring attendance at hospital. Many injuries due to falls or wounds will be managed at home or in community health care facilities. In addition, the Western Area in which Connaught is based is more urbanised than the rest of the country and therefore more likely to see a higher degree of traffic related injuries than more rural populations. A similar finding was noted in Ghana [26].
Burns were the fourth most common reason for presentation and third most common cause of injury in children but no burns surgery was carried out due to lack of surgical facilities. A retrospective study looking at admissions to Bo government hospital, in Sierra Leone’s second biggest city after Freetown also found that burns were a common cause for admission in the under 5 age-group [27] and burns prevalence is estimated at 4%, most frequently reported in the 0–4 age group [28]. Burns are a frequent cause of morbidity and mortality amongst young patients in low-income countries in association with poverty and crowded living conditions, mostly occurring at home due to hot liquids and open flames [29].
The head and lower limbs were the most commonly injured body parts in patients admitted to the surgical and trauma wards. A similar finding was identified in a recent Kenyan study [30] as well as the cross sectional survey in Sierra Leone [10] and this links in to the fact that pedestrians and motorbike riders are more commonly admitted. These patients are more vulnerable and less protected than people in vehicles and helmets may not be worn as previously stated.
This is the first study to detail the burden of trauma and injury that presents to the national adult surgical referral hospital in Sierra Leone and, as such, can be used to guide training, resources and quality improvement initiatives to improve the care of these patients that form a majority of surgical admissions from the emergency centre. There is currently no funding available for a formal trauma registry in Sierra Leone and the pre-hospital service is in the early stages of development. The large majority of patients arrive at hospital on foot or by public transport. The hospital emergency and trauma service are working to improve the management of trauma patients through staff training and the introduction of a trauma pathway but it is important to document the extent of disease in order to gain financial backing and influence policy and preventative measures at a national level. Surgical capacity at the hospital was severely diminished during the Ebola outbreak [12] which may explain the small number of surgical procedures carried out in this study. The hospital employed 8 surgeons prior to the epidemic, 3 of whom died and during the peak of the epidemic, surgery rates fell to 3% of pre-Ebola levels [12]. At the time of data collection, surgical activity was still limited and there is currently only 1 paediatric surgeon based in the city with no burn surgery equipment available. The situation is improving, with WHO and Ministry focus on human resource development, establishment of a university teaching hospital complex and accreditation for basic surgical training.
We acknowledge that our study does not capture the full extent of trauma in Freetown. Many trauma patients in the city are managed by a non-government organisation-run surgical centre based outside the city. Patients with less severe injury will be managed in smaller facilities or in the community without seeking care or by traditional healer. Significant barriers to accessing care exist including inadequate numbers of trained staff, lack of money to pay for treatment or transport to health facilities as well as lack of trust in the facilities [31]. All of these factors may also explain why many patients self-discharge.
The other significant limitation is the retrospective nature of the study. An attempt was made to minimise the amount of missing data by using multiple sources and registers and we are confident that the majority of patients presenting to the EC were identified, although a minority may have not been triaged but seen directly in the resuscitation area or may have died on arrival. Although data on basic physiology is recorded on the SATS form at triage, this was not collected as part of this study as triage category was used a surrogate marker for severity of presentation. This data could potentially be useful for predicting need for admission and risk of mortality and will be incorporated into future audit tools. We were unable to collect mortality data for adult patients and it was not possible to obtain admission records for 28% of adult patients. Other low-income trauma studies have identified similar limitations due to inadequate medical records and documentation [20], [32]. Mortality was not routinely recorded in the trauma ward ledger, however, this process is now undergoing review by the hospital quality improvement committee and morbidity and mortality meetings have been established.
Subsequent to collection and presentation of this data to the hospital surgeons and management, there have been several initiatives to improve data collection and a focus on developing the trauma service. A trauma form has been developed in partnership with the surgical staff that is added to the patient clinical record and completed by nursing and medical staff. This is adapted from the African Federation for Emergency Medicine trauma form and includes data on presentation, mechanism of injury and basic physiology measurements that are routinely recorded by triage staff. The hospital records system has recently been revolutionised with introduction of basic information technology and a trauma audit tool based on Epi-Info software is in the process of being developed to facilitate registry development. Use of the trauma form is currently being audited and two successful Primary Trauma Care courses, including a train-the-trainer course, have been run.
Traumatic injuries account for a significant burden of illness in Sierra Leone, especially in the government referral hospital based in Freetown, the capital city. Current systems are inadequate to effectively manage this volume of injury and quality improvement initiatives in line with World Health Organisation guidelines [33] are being instigated to address this deficiency including training of clinical staff, improved surgical resources and improved data collection. Funding for a formal trauma registry is urgently required. Accurate data collection will strengthen the need for a robust pre-hospital care system as well as focus public health initiatives to reduce and prevent injury through legislation and government policy. The recent refurbishment of the emergency centre and trauma unit at Connaught aims to facilitate this process and improve outcomes for this young cohort of patients.
Acknowledgments
Acknowledgements
The authors would like to thank all the staff in the Accident and Emergency Department and Trauma Units at Connaught Hospital whose hard work and dedication made this study possible, as well as Drs Ling Harrison, Fiona Napier and Miss Lisa Cleveley of the King’s Sierra Leone Partnership.
Conflicts of interest
The authors declare no conflicts of interest.
Dissemination of results
The results of this research were presented at the hospital surgical consultants’ meeting as well as at informal presentations to the staff of both the trauma and emergency centres as part of the audit and teaching programme.
Authors’ contributions
Authors contributed as follows to the conception or design of the work; the acquisition, analysis, or interpretation of data for the work; and drafting the work or revising it critically for important intellectual content: IB and RL contributed 30% each; HPV, SPK, AMJ, and COSS contributed 10% each. All authors approved the version to be published and agreed to be accountable for all aspects of the work.
Footnotes
Peer review under responsibility of African Federation for Emergency Medicine.
Supplementary data associated with this article can be found, in the online version, at https://doi.org/10.1016/j.afjem.2018.07.008.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Murray C.J., Vos T., Lozano R., Naghavi M., Flaxman A.D., Michaud C. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2197–2223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 2.Haagsma J.A., Graetz N., Bolliger I., Naghavi M., Higashi H., Mullany E.C. The global burden of injury: incidence, mortality, disability-adjusted life years and time trends from the Global Burden of Disease study 2013. Inj Prev. 2016;22(1):3–18. doi: 10.1136/injuryprev-2015-041616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gosselin R.A., Spiegel D.A., Coughlinc R., Zirkle L.G. Injuries: the neglected burden in developing countries. Bull World Health Organ. 2009;87:246. doi: 10.2471/BLT.08.052290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World health statistics 2017: monitoring health for the SDGs, Sustainable Development Goals. Geneva: World Health Organization; 2017.
- 5.Global status report on road safety 2015. Geneva: World Health Organization; 2015.
- 6.Adeloye D., Thompson J.Y., Akanbi M.A., Azuh D., Samuel V., Omoregbec N. The burden of road traffic crashes, injuries and deaths in Africa: a systematic review and meta-analysis. Bull World Health Organ. 2016;94:510–521. doi: 10.2471/BLT.15.163121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vos T., Flaxman A.D., Naghavi M., Lozano R., Michaud C., Ezzati M. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2163–2196. doi: 10.1016/S0140-6736(12)61729-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.United Nations Development Program. Human development report 2016: Human development for everyone. http://hdr.undp.org/sites/default/files/2016_human_development_report.pdf [accessed 12 June 2017].
- 9.Sierra Leone: WHO statistical profile. World Health Organisation; 2015. http://www.afro.who.int/en/sierra-leone/country-health-profile.html [accessed 12 June 2017].
- 10.Stewart K., Groen R.S., Kamara T.B., Farahzard M., Samai M., Yambasu S.E. Traumatic injuries in developing countries: report from a nationwide cross-sectional survey of Sierra Leone. JAMA Surg. 2013;148(5):463–469. doi: 10.1001/jamasurg.2013.1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Health sector annual performance report 2015. Government of Sierra Leone Ministry of Health and Sanitation. http://www.afro.who.int/en/sierra-leone/country-health-profile.html [accessed 12 June 2017].
- 12.Bundu I., Patel A., Mansaray A., Kamara T.B., Hunt L.M. Surgery in the time of Ebola: how events impacted on a single surgical institution in Sierra Leone. J R Army Med Corps. 2016;162(3):212–216. doi: 10.1136/jramc-2015-000582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wong E.G., Gupta S., Deckelbaum D.L., Razek T., Kamara T.B., Nwomeh B.C. The international assessment of capacity for trauma (INTACT): an index for trauma capacity in low-income countries. J Surg Res. 2014;190:522–527. doi: 10.1016/j.jss.2014.01.060. [DOI] [PubMed] [Google Scholar]
- 14.Coyle R.M., Harrison H.L. Emergency care capacity in Freetown, Sierra Leone: a service evaluation. BMC Emerg Med. 2015;15(1):2. doi: 10.1186/s12873-015-0027-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ministry of Health and Sanitation [Sierra Leone] MoHS; Freetown: 2015. Sierra Leone basic package of essential health services 2015–2020. [Google Scholar]
- 16.Anderson P.D., Suter R.E., Mulligan T., Bodiwala G., Razzak J.A., Mock C. World Health Assembly Resolution 60.22 and its importance as a health care policy tool for improving emergency care access and availability globally. Ann Emerg Med. 2012 Jul;60(1):35–44. doi: 10.1016/j.annemergmed.2011.10.018. [DOI] [PubMed] [Google Scholar]
- 17.World Health Organisation. From MDGs to SDGs. A new era for global public health 2016–2030. http://www.who.int/mediacentre/events/meetings/2015/un-sustainable-development-summit/en/ [accessed 12 June 2017].
- 18.Twomey M., Wallis L., Thompson M.L., Myers J.E. The South African triage scale (adult version) provides valid ratings when used by doctors and enrolled nursing assistants. Afr J Emerg Med. 2012;2(1):3–12. doi: 10.1016/j.ienj.2011.08.002. [DOI] [PubMed] [Google Scholar]
- 19.Samuel J.C., Akinkuotu A., Villaveces A., Charles A.G., Lee C.N., Hoffman I.F. Epidemiology of injuries at a tertiary care center in Malawi. World J Surg. 2009;33(9):1836–1841. doi: 10.1007/s00268-009-0113-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Taibo C.L.A., Moon T.D., Joaquim O.A., Machado C.R., Merchant A., McQueen K. Analysis of trauma admission data at an urban hospital in Maputo, Mozambique. Int J Emerg Med. 2016;9:6. doi: 10.1186/s12245-016-0105-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Seidenberg P., Cerwensky K., Brown R.O., Hammond E., Mofu Y., Lungu J. Epidemiology of injuries, outcomes, and hospital resource utilisationat a tertiary teaching hospital in Lusaka, Zambia. Afr J Emerg Med. 2014;4:115–122. [Google Scholar]
- 22.Mwandri M.B., Hardcastle T.C. Burden, characteristics and process of care among the pediatric and adult trauma patients in Botswana’s Main Hospitals. World J Surg. 2018;42:1629–1638. doi: 10.1007/s00268-018-4528-7. [DOI] [PubMed] [Google Scholar]
- 23.Lutge E., Moodley N., Tefera A., Sartorius B., Hardcastle T., Clarke D. A hospital based surveillance system to assess the burden of trauma in KwaZulu-Natal Province South Africa. Injury. 2016;47(1):135–140. doi: 10.1016/j.injury.2015.08.020. [DOI] [PubMed] [Google Scholar]
- 24.Hardcastle T., Samuels C., Muckart D. An Assessment of the hospital disease burden and the facilities for the in-hospital care of trauma in KwaZulu-Natal, South Africa. World J Surg. 2013;37:1550–1561. doi: 10.1007/s00268-012-1889-1. [DOI] [PubMed] [Google Scholar]
- 25.Adeloye D., Thompson J.Y., Akanbi M.A., Azuh D., Samuel V., Omoregbec N. The burden of road traffic crashes, injuries and deaths in Africa: a systematic review and meta-analysis. Bull World Health Organ. 2016;94:510–521A. doi: 10.2471/BLT.15.163121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mock C.N., Forjuoh S.N., Rivara F.P. Epidemiology of transport-related injuries in Ghana. Accid Anal Prev. 1999;31(4):359–370. doi: 10.1016/s0001-4575(98)00064-5. [DOI] [PubMed] [Google Scholar]
- 27.Grimes C., Billingsley M., Dare A., Day N., George P.M., Kamara T.B. The demographics of patients affected by surgical disease in district hospitals in two sub-Saharan African countries: a retrospective descriptive analysis. Springer Plus. 2015;4:750. doi: 10.1186/s40064-015-1496-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wong E.G., Groen R.S., Kamara T.B., Stewart K., Cassidy L.D., Samai M. Burns in Sierra Leone: a population-based assessment. Burns. 2014;40:1748–1753. doi: 10.1016/j.burns.2014.03.007. [DOI] [PubMed] [Google Scholar]
- 29.Rybarczyka M.M., Schaferb J.M., Elmc C.M., Sarvepallid S., Vaswanie P.A. A systematic review of burn injuries in low- and middle-income countries: epidemiology in the WHO-defined African Region. Afr J Emerg Med. 2017;7(1):30–37. doi: 10.1016/j.afjem.2017.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Matheka D.M., Kitonyi M.N., Alkizim F.O. Three-month pattern of road traffic injuries at a Kenyan level 4 hospital. Pan Afr Med J. 2015;20:78. doi: 10.11604/pamj.2015.20.78.5206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Elliott I.S., Groen R.S., Kamara T.B., Ertl A., Cassidy L.D., Kushner A. The burden of musculoskeletal disease in Sierra Leone. Clin Orthop Relat Res. 2015;473(1):380–389. doi: 10.1007/s11999-014-4017-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chokotho L., Mulwafu W., Jacobsen K.H., Pandit H., Lavy C. The burden of trauma in four rural district hospitals in Malawi: a retrospective review of medical records. Inj Int. J. Care Inj. 2014;45:2065–2070. doi: 10.1016/j.injury.2014.10.001. [DOI] [PubMed] [Google Scholar]
- 33.Mock C., Lormand J.D., Goosen J., Joshipura M., Peden M. World Health Organization; Geneva: 2004. Guidelines for essential trauma care.http://whqlibdoc.who.int/publications/2004/9241546409.pdf [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.