Abstract
Introduction
Retail pharmacies in NJ are permitted to dispense naloxone without a prescription. However, not all pharmacies have participated in this effort, and it is not clear what factors may impact its availability. We sought to determine the naloxone availability of select NJ cities and what sociodemographic factors are associated with its availability. We compared naloxone availability in retail pharmacies to median household income, population, and the prevalence of opioid-related hospital visits (ORHV).
Methods
All retail pharmacies in ten New Jersey cities were surveyed by phone in February–July 2017. The standardized survey instrument asked scripted questions to each pharmacist concerning the stocking of naloxone for dispensing. Median household income data and population data for each city were obtained from census.gov. Opioid-related hospital visits were obtained through the NJ SHAD database and the prevalence of ORHV was calculated. Naloxone availability was compared to median household income, population, and ORHV using Spearman’s rho and Pearson’s correlation.
Results
Naloxone availability in the 90 retail pharmacies we surveyed was 31% and ranged from 15.38 to 66.67% by city. An increase in median household income indicated more pharmacy naloxone availability. An increase in population indicated less pharmacy naloxone availability. While no significant relationship existed between ORHV and pharmacy naloxone availability, we did identify individual cities with severe opioid-related public health concerns with limited naloxone access.
Conclusions
Naloxone deserts exist in select high-risk New Jersey cities, and pharmacy naloxone availability may be positively related to median household income and negatively related to population.
Electronic supplementary material
The online version of this article (10.1007/s13181-019-00700-7) contains supplementary material, which is available to authorized users.
Keywords: Analgesics, Opioid, Naloxone, Pharmaceutical services
Background
Drug overdose deaths have nearly tripled from 1999 to 2015, with the majority of deaths involving opioids [1]. Fentanyl has compounded this problem, and in 2016 it ranked first among overdose deaths that mentioned a specific drug [2]. Naloxone, a mu opioid receptor antagonist, has been used in hospitals since the 1960s to reverse opioid overdoses and shortly thereafter by prehospital care providers. Over the past decade, naloxone has been distributed to family members, friends, and other individuals in proximity to someone likely to experience an opioid overdose. The World Health Organization and US Surgeon General recommend its use [3, 4] and various other US federal agencies have recommended increasing access for prescription opioid users. Protections for the prescribers of naloxone, and those who administer it as bystanders, vary by state [5]. In New Jersey, the New Jersey Overdose Prevention Act of 2013 [6] provides immunity from liability for the prescriber, the pharmacy, and the individual administering naloxone to a patient with a presumed opioid overdose. Additionally, it allows for pharmacies to dispense naloxone on a standing order without requiring a prescription. Unfortunately, not all pharmacies in New Jersey are participating in this effort. We sought to determine the naloxone availability of select NJ cities and what sociodemographic factors are associated with its availability. We compared naloxone availability in retail pharmacies to median household income, population, and the prevalence of opioid-related hospital visits (ORHV).
Methods
Ten New Jersey cities were chosen for inclusion with an attempt to balance size and severity of the opioid problem. We chose cities based on their population and prevalence of ORHV based on four quadrants of interest (Table 1). Any pharmacy whose listed address matched the city of interest was included.
Table 1.
City inclusion demographics
| Low population low ORHV | High population low ORHV |
| Low population high ORHV | High population high ORHV |
Naloxone availability was determined by a scripted phone survey of all retail pharmacies in the selected cities. The standardized survey instrument was conducted in English and did not require interpretation. It was written at the 4th grade reading level. The survey began by confirming the name and address of the pharmacy. All surveys were conducted with self-identified pharmacists. If a pharmacist was unavailable at the time of survey, subsequent calls were placed until a pharmacist was available. The investigator began by asking “Do you have naloxone or Narcan™ in stock?”. Confirmation of the correct drug was obtained during every survey due to “naloxone’s” similar name to “suboxone.” This was achieved by asking if the drug was “the opioid antidote” or “used to reverse opioid overdoses.” The standardized survey instrument requested that each pharmacist search the computer for naloxone availability when possible. Naloxone availability was recorded as a “yes” or a “no,” depending on the availability at the time of the conversation. Necessity of prescription for purchase was also obtained at time of interview. On occasion, off-script discussion was necessary for clarification or to respond to an unexpected question. Initially, information regarding willingness to order naloxone, cost, and recent change to prescription policy was collected but was removed from the survey after frequent unavailability of this information. A single investigator conducted all the surveys from February to July 2017. Ninety pharmacies in total were surveyed.
Median household income and population data were obtained through the website census.gov [7]. Population values are based on the July 1, 2017 estimates and median household income values are from 2012 to 2016 in 2016 dollars. Opioid-related hospital visit data were obtained from the New Jersey State Health Assessment Data (NJ SHAD) database [8]. The prevalence of ORHV in a given city population was calculated by dividing the number of opioid discharges by population of that city, and multiplying by 100,000. ORHV = (City Opioid Discharges/City Population) × 100,000. OHRV data included discharges from both the emergency department and the hospital, and an opioid-related ICD9 code during the encounter from the years 2008–2015.
The availability of hospital and community-based naloxone distribution programs was gathered by reaching out to the New Jersey Department of Health and the New Jersey Hospital Association.
Shapiro-Wilk’s test for normality was performed for pharmacy availability, median household income, population, and ORHV data. Spearman’s rho and Pearson’s correlations were then calculated. All statistical analysis was made using IBM SPSS statistics version 25.
Results
Naloxone availability in the 90 retail pharmacies we surveyed was 31%. Naloxone availability ranged from 15.38 to 66.67% by city (Table 2).
Table 2.
Raw data
| City | Readington | Atlantic City | Vineland City | Millville | Flemington | Old Bridge | Camden | Wildwood | Little Silver | Newark |
|---|---|---|---|---|---|---|---|---|---|---|
| Pharmacy Availability | 66.67% | 16.67% | 15.38% | 28.57% | 60.00% | 28.57% | 25.00% | 50.00% | 66.67% | 21.43% |
| Median household income | 125,703.00 | 26,566.00 | 48,986.00 | 48,892.00 | 54,261.00 | 84,594.00 | 26,214.00 | 28,271.00 | 137,652.00 | 33,025.00 |
| Population | 15,963 | 38,429 | 60,392 | 27,918 | 4621 | 67,032 | 74,532 | 5070 | 5908 | 285,154 |
| ORHV | 1241 | 16,582 | 4142 | 5845 | 8666 | 883 | 10,489 | 11,992 | 441 | 16,844 |
| Number of pharmacies | 3 | 6 | 13 | 7 | 10 | 14 | 16 | 4 | 3 | 14 |
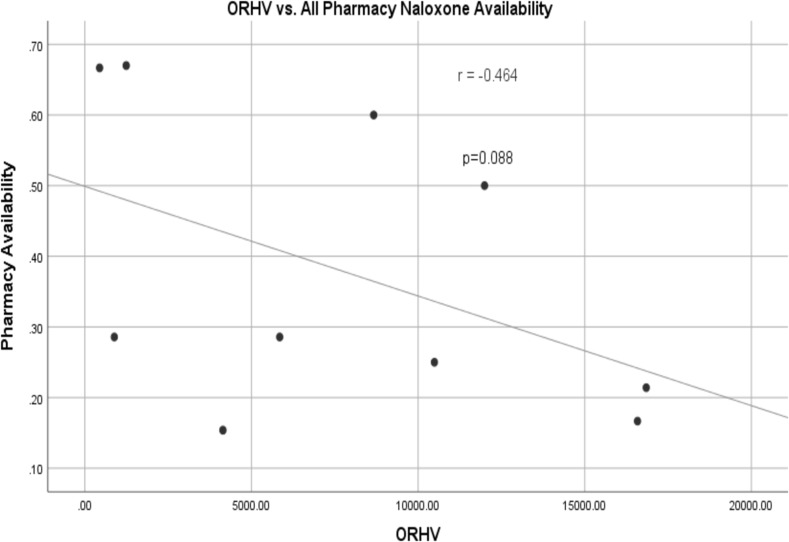
Shapiro-Wilk’s test for normality are as follows: pharmacy availability 0.057, median household income 0.021, population 0.000, ORHV 0.289. Spearman’s rho comparing median household income and pharmacy availability = 0.632, p = 0.050. Spearman’s rho comparing population and pharmacy availability = − 0.693, p = 0.026. Pearson’s correlation comparing ORHV and pharmacy availability = − 0.464, p = 0.088 (Fig. 1).
Fig. 1.
Opioid-related hospital visits vs. all pharmacy naloxone availability
No New Jersey emergency departments at the time of study dispensed take-home naloxone. No centralized database existed for New Jersey community-based take-home naloxone programs.
Discussion
The results suggest an unsurprising and concerning pattern: patients living in the most populous poorer areas are also living in areas with less access to naloxone. Two cities stand out illustrating this dichotomy. Little Silver, a small and wealthy city (population 5908, median household income $137,652) with a low ORHV, has high pharmacy naloxone availability. Newark, a large and poor city (population 285,154, median household income $33,025) with a high ORHV, has low pharmacy naloxone availability. A similar dichotomy exists when you compare Readington and Camden. The cities we surveyed show a relationship between naloxone pharmacy availability and median household income, where an increase in median household income indicates more pharmacy naloxone availability. Additionally, we observed a relationship between naloxone pharmacy availability and population, where an increase in population indicates less pharmacy naloxone availability. While we did not find a statistically significant relationship between naloxone pharmacy availability and ORHV, we did find individual cities with severe opioid-related public health concerns that had limited naloxone access (Newark, Camden, Atlantic City). We also were unable to find reliable sources of information for non-pharmacy naloxone distribution programs in NJ. We believe our data reflects a need for targeted improvement in naloxone availability.
One potential explanation for this observation is that poorer cities do not create demand for pharmacies to stock naloxone. Without insurance, Narcan™ nasal spray can range from $70 to $300. Additionally, the Evzio™ autoinjector costs as much as $4500 for a package of two. Naloxone is covered by Medicaid in NJ, which would help reduce this price barrier, but unfortunately many patients lack health insurance. 9.7% of New Jersey’s population is uninsured and 21.3% of Newark’s population is uninsured [9]. Another factor impacting the availability of naloxone is that CVS and Walgreens both committed to stocking naloxone in their stores in New Jersey [10, 11]. We found that 75% of the CVS/Walgreens surveyed had naloxone available. Only 14% of the non-CVS/Walgreens pharmacies we surveyed had naloxone available. Less CVS/Walgreens may exist in poorer areas, creating less availability. The sample sizes are too low to run a sensitivity analysis to determine if the proportion of CVS and Walgreens in a city impacted the analysis. However, it is important to note that the aim of this study was not to create a model to predict pharmacy naloxone availability. This does not change our observation that high-risk areas do not have access to a potentially life-saving medication.
There are a number of limitations to this study. First, only retail pharmacy naloxone availability is included in the analysis. If cities have alternative methods of dispensing naloxone, such as community-based distribution, or from a hospital or emergency department, this would not be represented in our data. We were surprised how difficult it was to access information on New Jersey emergency departments and community-based distribution programs. Without this knowledge, we can only speculate about the true access to naloxone in these areas, and it seems unlikely that pharmacies would have sufficient knowledge of the local distribution programs to impact their stocking. What does appear clear, though, is that naloxone availability is low in some low-income, highly populated, high-risk areas in New Jersey. These areas lack robust hospital distribution programs, community distribution programs, and naloxone pharmacy availability. Compounding this problem is the low proportion of patients prescribed naloxone that actually pick it up at the pharmacy [12]. University Hospital in Newark recently began the first emergency department-based naloxone distribution program in New Jersey, and future study will evaluate its effectiveness.
Other limitations include the low sample size of both the number of cities we surveyed (10), pharmacies in each city (3–16), and the different number of pharmacies surveyed in each city (although we surveyed 100% in each). Confidence intervals would be inappropriate to use, because we are reporting 100% of the data that exists from each the cities we surveyed. Also, this data is also only as reliable as the pharmacist who was interviewed. Additionally, our surrogate measures of severity of the opioid problem and socioeconomic status may not be completely representative. For example, wealthy areas may be averse to coding for opioid-related diagnoses. Median household income of a city may not fully capture the variability in poverty. Furthermore, since the study was performed over 5 months, it is unknown if the percentage of pharmacies stocking naloxone changed. These limits make it impossible to run any rigorous statistical analysis or extrapolate any broad conclusions. What we have attempted to show is naloxone deserts exist in areas with a need for naloxone in select New Jersey cities. Future study could analyze if the vendor impacts ability of the pharmacy to obtain naloxone. Furthermore, larger studies, like that recently conducted in Pennsylvania [13], are great avenues for making broader correlations and conclusions about naloxone availability.
The opioid crisis requires unique solutions along with consistent implementation of known best practices. The scientific community acknowledges that naloxone can be a life-saving drug in the hands of bystanders [3, 4]. However, barriers still exist to widespread availability [14]. In 2017, New Jersey passed additional legislation that specifically encouraged pharmacies to stock and dispense naloxone [15], although the impact of this statute is not yet known. Further study should seek to develop and evaluate strategies that enhance the consistency of naloxone stocking and distribution, like that recently conducted in California [16].
Conclusion
Naloxone deserts exist in select high-risk New Jersey cities, and pharmacy naloxone availability may be positively related to median household income and negatively related to population.
Electronic Supplementary Material
(DOCX 13 kb)
Sources of Funding
None.
Compliance with Ethical Standards
Conflicts of Interest
None.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Rudd RA, Seth P, David F, Scholl L. Increases in drug and opioid-involved overdose deaths - United States, 2010-2015. MMWR Morb Mortal Wkly Rep. 2016;65:1445–1452. doi: 10.15585/mmwr.mm655051e1. [DOI] [PubMed] [Google Scholar]
- 2.Hedegaard H, Bastian BA, Trinidad JP, Spencer M, Warner M. Drugs most frequently involved in drug overdose deaths: United States, 2011-2016. National vital statistics reports: from the Centers for Disease Control and Prevention, National Center for Health Statistics. Natl Vital Stat Syst. 2018;67(9):1–13. [PubMed] [Google Scholar]
- 3.WHO Guidelines Approved by the Guidelines Review Committee. Community management of opioid overdose. 2014.
- 4.General S. Surgeon general’s advisory on naloxone and opioid overdose. https://www.surgeongeneral.gov/priorities/opioid-overdose-prevention/naloxone-advisory.html. Accessed Jan 28 2019.
- 5.Davis C, Carr D. State legal innovations to encourage naloxone dispensing. J Am Pharm Assoc : JAPhA. 2017;57:S180–S184. doi: 10.1016/j.japh.2016.11.007. [DOI] [PubMed] [Google Scholar]
- 6.Overdose Prevention Act Sect NJSA. 2013;2C:35–30. [Google Scholar]
- 7.United State Census Bureau. 2019. https://www.census.gov. Accessed Jan 28 2019.
- 8.New Jersey State Health Assessment Data. 2019. https://www-doh.state.nj.us/doh-shad/home/Welcome.html. Accessed Jan 28 2019.
- 9.United States Census Bureau, American Community Survey (ACS). 2019. https://www.census.gov/programs-surveys/acs/. Accessed Jan 28 2019.
- 10.Wichert B. CVS to offer anti-overdose drug without prescription at N.J. locations. 2015. https://www.nj.com/news/index.ssf/2015/10/cvs_to_offer_anti-overdose_drug_without_prescripti.html. Accessed Jan 28 2019.
- 11.Walgreens makes life saving naloxone available without prescription in New Jersey pharmacies. 2016. https://news.walgreens.com/press-releases/general-news/walgreens-makes-life-saving-naloxone-available-without-prescription-in-new-jersey-pharmacies.htm. Accessed Jan 28 2019.
- 12.Verdier M, Routsolias JC, Aks SE. Naloxone prescriptions from the emergency department: an initiative in evolution. Am J Emerg Med. 2019;37:164–165. doi: 10.1016/j.ajem.2018.05.044. [DOI] [PubMed] [Google Scholar]
- 13.Graves RL, Andreyeva E, Perrone J, Shofer FS, Merchant RM, Meisel ZF. Naloxone availability and pharmacy staff knowledge of standing order for naloxone in Pennsylvania pharmacies. J Addict Med. 2018:1. 10.1097/adm.0000000000000492. [DOI] [PMC free article] [PubMed]
- 14.Wheeler E, Jones TS, Gilbert MK, Davidson PJ. Opioid overdose prevention programs providing naloxone to laypersons - United States, 2014 MMWR Morb Mortal Wkly Rep 2015;64(23):631–635. [PMC free article] [PubMed]
- 15.An act concerning overdose prevention and the dispensation of opioid antidotes and supplementing P.L.2003, c.280 (C.45:14–40 et seq.) [and amending P.L.2013, c.46], (2017).
- 16.Puzantian T, Gasper JJ. Provision of naloxone without a prescription by California pharmacists 2 years after legislation implementation. JAMA. 2018;320:1933–1934. doi: 10.1001/jama.2018.12291. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 13 kb)