Abstract
The tumor microenvironment represents a complex network, in which tumor cells not only communicate with each other but also with stromal and immune cells. Current research has demonstrated the vital role of the tumor microenvironment in supporting tumor phenotype via a sophisticated system of intercellular communication through direct cell-to-cell contact or by classical paracrine signaling loops of cytokines or growth factors. Recently, extracellular vesicles have emerged as an important mechanism of cellular interchange of bioactive molecules. Extracellular vesicles isolated from tumor and stromal cells have been implicated in various steps of tumor progression, such as proliferation, angiogenesis, metastasis, and drug resistance. Inhibition of extracellular vesicles secretion, and thus of the transfer of oncogenic molecules, holds promise for preventing tumor growth and drug resistance. This review focuses on the role of extracellular vesicles in modulating the tumor microenvironment by addressing different aspects of the bidirectional interactions among tumor and tumor-associated cells. The contribution of extracellular vesicles to drug resistance will also be discussed as well as therapeutic strategies targeting extracellular vesicles production for the treatment of cancer.
Keywords: Tumor microenvironment, Stroma, Metastasis, Extracellular vesicles, Drug resistance
Background
The last decades have revealed that the malignant properties and progression of tumors are not controlled by cancer cells exclusively [1]. The area surrounding the tumor contains various non-malignant cell types, including fibroblasts, lymphocytes, inflammatory cells, endothelial cells, adipose tissue, and mesenchymal stem cells [1]. In the early stages of tumorigenesis, the microenvironment displays anti-tumor immunity and controls tumor growth [2]. As the tumor continues to develop, the role of the microenvironment shifts over to be tumor promotive [2]. Cells found in the tumor microenvironment (TME) have been recognized as key regulators of tumor promotion by providing mitogenic growth factors, growth inhibitory signals or trophic factors [2]. The complex heterotypic interactions between tumor cells and non-cancerous cells within the TME occur through direct contact between cells or paracrine signal exchange of cytokines and growth factors [2]. The most well-recognized cell-to-cell interaction within the TME is between tumor cells and macrophages or fibroblasts [2]. Macrophages play an integral role in host innate immune response against infections [3]. Tumor cells release factors, such as vascular endothelial growth factor (VEGF), colony stimulating factor 1 (CSF1), and platelet-derived growth factor (PDGF), that aid in the recruitment of macrophages to tumors [3]. Once the macrophages are recruited to the tumor, they can promote tumor progression by enhancing tumor cell proliferation, as well as by remodeling the tumor stroma to facilitate invasion and angiogenesis [3]. Fibroblasts are responsible for the production of extracellular matrix (ECM), such as collagen and fibronectin, and facilitate remodeling in wound healing [4]. Cancer-associated fibroblasts (CAFs) support tumor growth, invasion, metastasis and induce inflammation [4]. Stromal cell-derived factor 1 (SDF1) is a CAF-secreted factor that can activate C-X-C chemokine receptor type 4 (CXCR4) and ultimately stimulates cancer cell proliferation [2, 4]. CAF-derived transforming growth factor-beta (TGF-β) promotes the metastatic potential of tumor cells by driving an epithelial-to-mesenchymal transition (EMT) [2, 4].
Recently, it has become apparent that secreted extracellular vesicles (EVs) are proficient intercellular communication mediators [2]. EVs are a heterogeneous population of cell-derived membrane vesicles that are secreted by various cell types. They exhibit a wide size range and differ by their biogenesis. EVs include exosomes, which are small membrane vesicles, ranging from 30 to 150 nm in diameter, and shed microvesicles (MVs), which are large membrane vesicles of 150 to 1000 nm diameter budding off the plasma membrane [5]. Smaller shed MVs have also been reported, which are ~ 100 nm in diameter [6]. Oncosomes are even larger EVs that are also shed off from the plasma membrane and are 1 to 10 μm in diameter [7]. EVs contain a diverse array of bioactive cargoes, including proteins, lipids, and nucleic acid [5, 7, 8]. The lipid bilayer of EVs encapsulates their contents, shielding them from enzymatic degradation [2]. EVs regulate multiple cellular processes including cell proliferation, survival, and transformation through autocrine and paracrine interactions [5, 8].
Multiple mechanisms are involved in the biogenesis of EVs: exosomes originate as intraluminal vesicles (ILVs) via inward budding of the limiting membrane of maturing endosomes, giving rise to multivesicular endosomes (MVEs) [5]. MVEs are prone to fuse with lysosomes for degradation of their contents, however, they can also dock and fuse with the plasma membrane to release ILVs into the extracellular space [5]. One of the best-characterized mechanism of exosome biogenesis involves the recruitment of the endosomal sorting complex required for transport (ESCRT) machinery to ubiquitinated proteins in the early endosome. There are four ESCRT complexes (ESCRT-0, −I, −II, and -III), which associate with ESCRT-associated accessory proteins, such as the ATPase VPS4, its cofactor VTA-1, TSG101, and Alix. ESCRT-0 complex recognizes and sequesters ubiquitinated proteins on the outside of the endosomal membrane. ESCRT-I and –II complexes are responsible for starting and driving intraluminal membrane budding. ESCRT-III complex performs vesicle scission to form MVEs [9]. Trajkovic et al. have also described an ESCRT-independent exosome biogenesis pathway, which is mediated by the sphingolipid ceramide [10]. Ceramide is produced from the hydrolysis of sphingomyelin by neutral sphingomyelinase 2 (nSMase2) [10]. The cone-shaped structure of ceramide stimulates the negative membrane curvature to facilitate the membrane invagination of ILVs [10]. The authors reported that nSMase2 is needed for the release of proteolipid protein (PLP) from Oli-neu cells [10]. In addition, the ceramide-mediated exosome biogenesis pathway appears to be important for microRNA (miRNA) export via exosomes [11]. Tetraspanin CD63 has also been shown to be involved in the sorting of melanocyte protein PMEL into exosomes in an ESCRT-independent mechanism [12]. Some of the key regulators of MVE docking and fusion with the plasma membrane include several Rab family members (Rab11, Rab35, Rab27) as well as synaptotagmin-7 [13–17]. It was previously reported that cortactin and Rab27a coordinate to stabilize branched actin networks to allow MVE docking near the plasma membrane and exosome secretion at invadopodia [18].
MVs are formed by the outward budding, fission of the plasma membrane, and release into the extracellular space [5, 7]. The biogenesis of MVs is distinct from that of MVEs-derived exosomes [5, 7]. During MVs generation, there are molecular rearrangements at the sites of MVs budding resulting in an alteration of the lipid and protein compositions of the plasma membrane [5, 7]. One of the mechanisms of the MVs formation involves phospholipid reorganization by aminophospholipid translocases (floppases and flippases) [5, 7]. The translocation of phosphatidylserine (PS) from the inner leaflet to the outer leaflet by floppase induces the budding and release of MVs [5, 7]. Another contributor to MVs budding is the small GTPase protein, ADP-ribosylation factor 6 (ARF6). ARF6 stimulates phospholipase D (PLD), which subsequently leads to the association of extracellular signal-regulated kinase (ERK) with the plasma membrane [19]. ERK is responsible for the phosphorylation of myosin light-chain kinase (MLCK) [19]. Activated MLCK promotes the phosphorylation and the activation of the myosin light chain. The end result of this signaling cascade is the contraction of actomyosin at the “necks” of MVs, which facilitates MVs release [19]. Another mechanism of MVs formation is mediated by Arrestin 1 domain-containing protein 1 (ARRDC1). Nabhan et al. reported that ESCRT-I subunit TSG101 is recruited to the plasma membrane through its interaction with ARRDC1, which is dependent on a conserved PSAP motif in ARRDC1 [6]. The budding of ARRDC1-mediated microvesicles (ARMMs) needs both TSG101 and the ESCRT-associated ATPase VSP4 [6]. The association of ARRDC1 with ubiquitin ligase WWP2 subsequently leads to the ubiquitination of ARRDC1 and drives the budding of ARMMs [6]. One characteristic of ARMMs is that they differ from other MVs in their size. ARMMs are ~ 100 nm in diameter, which is similar to the size of exosomes [6]. Wang et al. recently reported that a functional NOTCH2 receptor is released via ARMMs. Once the NOTCH2-containing ARMMs are transferred to recipient cells, the expression of NOTCH2 target genes (HES1 and HES5) was induced [20].
It is now clear that EVs serve as vehicles for bidirectional communication between cells. The receptors and ligands found on the outside of EVs provide a vectorial cargo transfer to cells expressing the cognate ligand/receptors, conferring specificity to this interaction [8, 12]. There are multiple processes by which EVs and their cargoes can be transferred to recipient cells. EVs may anchor at the plasma membrane of a target cell [21, 22]. Bound EVs may fuse directly with the plasma membrane of the recipient cell [21, 22]. Additionally, bound EVs can be taken up by phagocytosis, macropinocytosis, lipid raft-mediated endocytosis, clathrin-mediated endocytosis, or caveolin-mediated endocytosis [21, 22]. When endocytosed, EVs can be targeted to lysosomes for degradation [21, 22]. An alternative fate is that EVs could fuse with the delimiting membrane of an endocytic compartment, which subsequently allows for the release of EV content into the cytosol of the recipient cells [21, 22]. EVs carry bioactive molecular cargoes, including various proteins, lipids and nucleic acids (DNA, mRNA fragments, miRNA, small nucleolar RNA, Y RNA, mitochondrial RNA, and other non-coding RNAs) that can affect the functions and phenotypes of recipient cells by altering gene expression via de-novo translation and/or post-translational modifications of target mRNAs [5, 8] or by activating various signaling pathways [8, 22].
Given the lack of standardized nomenclature and isolation protocols for extracellular vesicles, we will commonly refer to exosomes, microvesicles, oncosomes, or microparticles as extracellular vesicles.
Extracellular vesicles as modulators of the tumor microenvironment
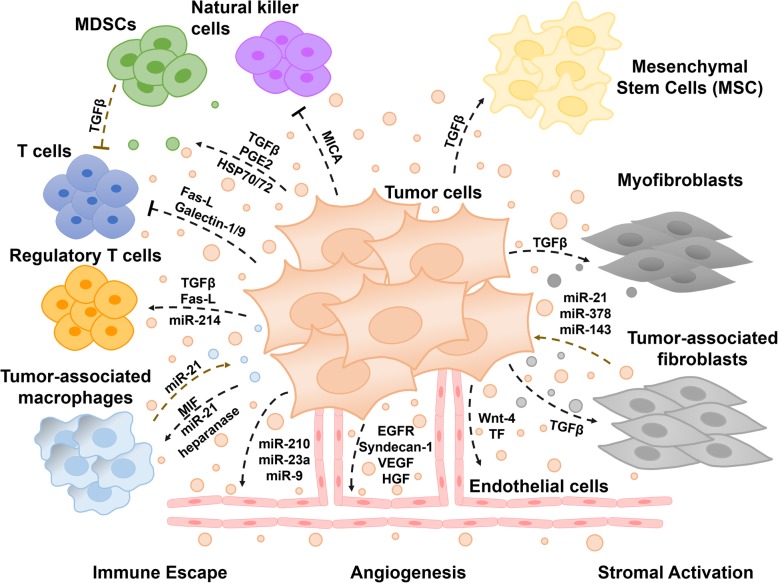
A critical biological feature that contributes significantly to cancer progression, invasion and metastasis is the ‘tumor microenvironment’ [23]. The tumor microenvironment (TME) is an interactive cellular environment surrounding the tumor whose main function is to establish cellular communication pathways supporting tumorigenesis [24]. The cellular component of the TME mainly comprises immune and inflammatory cells, stromal fibroblasts, and endothelial cells forming the blood vessels that secrete a series of extracellular/angiogenesis signaling molecules, which in turn lead to a functional modulation of TME [23]. The TME then converts into a pathological entity that continually evolves to aid cancer progression and invasion [24]. The extracellular vesicles (EVs) secreted by tumors, commonly known as tumor-derived EVs, have been well documented to modulate the tumor microenvironment (Fig. 1) [25]. EVs are highly specialized entities of communication carrying several surface markers and signaling molecules, oncogenic proteins and nucleic acids that can be transferred horizontally to the stromal target cells and condition the tumor microenvironment for an improved tumor growth, invasion, and metastasis [26–28]. The role of EVs in cancer progression and metastasis is described in detail below.
Fig. 1.
Role of the extracellular vesicles-mediated intercommunication in tumor development and progression. Tumor and stromal cells release extracellular vesicles as a mean of communication contributing to the complexity and heterogeneity of the tumor microenvironment. Extracellular vesicles-mediated transport of bioactive materials can induce a tumor microenvironment favorable for tumor growth and resistance to anti-cancer drugs
Extracellular vesicles and stromal activation
Stromal cells, together with extracellular matrix components are critical components of the tumor microenvironment, playing crucial roles in tumor initiation, progression, and metastasis [29]. One of the main stromal changes within the TME is the appearance of cancer-associated fibroblasts (CAFs) [29]. CAFs constitute a major portion of the reactive tumor stroma and play a crucial role in tumor progression. Tumor-derived EVs are essential mediators of the intercommunication between tumor and stromal cells, contributing to stromal support of tumor growth. Tumor-associated EVs have been reported to play a significant role in the differentiation of fibroblasts into CAFs, inducing a tumor-promoting stroma [30]. In addition to fibroblasts activation, tumor-derived EVs can also induce the differentiation of mesenchymal stem cells, and other bone marrow-derived cells to become tumor-supportive cells by delivering growth factors, such as transforming growth factor-beta (TGF-β) and various miRNAs [1, 31]. For instance, breast cancer and glioma cells are capable of conferring cancer transformed characteristics to normal fibroblasts and epithelial cells through the transfer of cancer cell-derived EVs carrying the cross-linking enzyme tissue transglutaminase (tTG)-crosslinked fibronectin [32]. More recently, it was reported that ovarian cancer cells secrete EVs capable of modulating fibroblasts behavior towards a CAF-like state. The secretome of the CAFs is, in turn, able to promote the proliferation, motility, and invasion of the tumor and endothelial cells [33]. Furthermore, in a prostate cancer cell model, the release of TGF-β1-associated EVs triggers fibroblast differentiation into a myofibroblast phenotype supporting angiogenesis in vitro and accelerating tumor growth in vivo [34]. Likewise, EVs derived from osteosarcoma cells carry a high level of surface-associated TGF-β1, which induces mesenchymal stem cells to secrete interleukin-6 and is associated with increased metastatic dissemination [35]. Breast cancer cells-derived EVs have also been reported to promote the acquisition of myofibroblast-like features in mesenchymal stem cells derived from adipose tissue [36]. Moreover, colorectal cancer-derived EVs were able to induce a tumor-like behavior in mesenchymal stromal cells, suggesting that the inflammatory microenvironment initiated by cancer cells-derived EVs promotes tumor growth and invasiveness [37]. Another mechanism described in tumor-stromal remodeling via EVs is the transfer of non-coding oncogenic miRNAs. Indeed, transfer of the pro-metastatic miRNA, miR-9, in breast cancer-derived EVs enhanced the switch of human breast fibroblasts to CAFs, resulting in enhanced cell motility [38]. Consequently, CAF-derived EVs may, in turn, support tumor growth, survival, invasion, and metastasis. For instance, CAF-derived EVs have been reported to increase the expression of Snail in recipient pancreatic ductal adenocarcinoma cells and thus to promote proliferation and drug resistance [39]. It has also been shown that fibroblasts secrete EVs that promote breast cancer cells protrusive activity, motility, and metastasis by activating autocrine Wnt-planar cell polarity (PCP) signaling [40]. Moreover, breast cancer cells exposed to CAF-derived EVs carrying miRs − 21, −378e, and − 143 display significantly increased stemness and EMT phenotypes [41].
Extracellular vesicles and angiogenesis
Angiogenesis is the process of new blood vessels formation from pre-existing vessels occurring in physiological conditions such as growth or in response to tissue injury. In healthy tissues, angiogenesis is tightly regulated by a precise balance between stimulatory and inhibitory angiogenic signals controlling the proliferation and migration of endothelial cells. An imbalance in this regulatory network may cause several diseases, such as cancer. In the past decade, EVs secreted by different cells within the tumor microenvironment have been shown to be important mediators of pathological angiogenesis through the release of angiogenic factors that can be transferred to endothelial cells, thus leading to the generation of a pro-angiogenic niche that supports tumor growth [42]. Indeed, EVs produced by human lung or colorectal cancer cells transfer oncogenic EGFR to cultured endothelial cells, in which they elicit EGFR-dependent responses, including activation of MAPK and AKT pathways, as well as an autocrine production and signaling of VEGF [43]. It was also reported that upregulation of heparanase in myeloma and breast cancer cells is associated with increased release of Syndecan-1, Vascular Endothelial Growth Factor (VEGF), and Hepatocyte Growth Factor (HGF) in EVs, leading to increased endothelial invasion through the ECM [44]. Furthermore, hypoxic glioblastoma cells have been shown to induce the secretion of high amounts of tissue factor (TF)-associated EVs that trigger a paracrine activation of endothelial cells through a PAR-2-mediated heparin-binding EGF signaling [45]. Interestingly, a study conducted by Kucharzewska and colleagues has shown that endothelial cells were programmed by glioblastoma cell-derived hypoxic EVs to secrete several potent growth factors and cytokines and to stimulate pericyte PI3K/AKT signaling activation and migration. Using an in vivo glioblastoma mouse xenograft model, the authors found that hypoxic EVs significantly enhanced tumor vascularization, pericyte vessel coverage, and glioblastoma cell proliferation [46]. Also, hypoxic colorectal cancer cells have been shown to secrete Wnt4-enriched EVs that promote beta-catenin (β-catenin) nuclear translocation and proliferation of endothelial cells [47]. Tumor EVs have also been reported to modulate angiogenesis in tumors via the release of non-coding RNAs. For example, miR-9 contained in EVs promotes tumor angiogenesis and endothelial cells migration through the reduction of suppressor of cytokine signaling 5 (SOCS5) levels and the activation of the JAK/STAT pathway [48], while EVs carrying miR-23a are capable of inducing angiogenesis in different angiogenic model systems by targeting SIRT1 in recipient endothelial cells [49]. Likewise, neutral sphingomyelinase 2 (nSMase2) (an enzyme that generates ceramide) promotes angiogenesis in endothelial cells through the transfer of pro-angiogenic EVs enriched for miR-210 [50].
Extracellular vesicles and immune escape
The tumor microenvironment is infiltrated by a variety of immune cells, such as lymphocytes (T cells, B cells, natural killer cells, and T regulatory cells), dendritic cells, monocytes, macrophages, myeloid-derived suppressor cells (MDSC), and granulocytes (neutrophils, basophils, eosinophils, and mast cells). The main role of these cells is to assure immune surveillance. However, tumor cells have been recognized to be capable of modulating signaling pathways within these immune cells and converting them into an immunosuppressive entity, thus leading to enhanced cancer cell survival and proliferation [51]. Despite the fact that EVs contain tumor antigens capable of priming an anti-tumor immune response, accumulating evidence demonstrates that tumor cells utilize EVs in order to suppress the anti-tumor response through the secretion of bioactive immunosuppressive molecules. Actually, EVs have been shown to be critical mediators of the immune-cancer cell communication. One example of how tumor-derived EVs aid in evading immune surveillance is by inducing apoptosis in immune cells. Indeed, several tumor-derived EVs have been shown to be enriched for Fas ligand (Fas-L) which induces cell apoptosis when binding to its receptor. Wieckowski et al. described that Fas-L-positive tumor-derived EVs induce immune suppression by promoting the expansion of T regulatory cells and the apoptosis of anti-tumor CD8(+) effector T cells, thus contributing to immune escape [52]. Similarly, this immune suppression mechanism through the release of Fas-L-containing EVs capable of inducing T-cell apoptosis was also reported in several cancer models, such as head and neck squamous cell carcinoma, melanoma, prostate, and colorectal cancer [53–56]. The presence of other mediators of T- cell apoptosis in tumor-derived EVs has been reported for galectin-1 and -9, both causing T-cell apoptosis and immune suppression [57, 58]. Similarly, EVs released from mesothelioma, acute myeloid leukemia, or colorectal cancer have been shown to contain the transforming growth factor (TGF-β) on their surface and to deliver it to T-cells, inhibiting their proliferation in response to interleukin-2 and changing their phenotype to regulatory T cells [59–61]. Moreover, tumor-released EVs have been shown to impair monocyte differentiation into dendritic cells and to promote the generation of a TGF-β secreting myeloid immunosuppressive cell subset (MDSC), which inhibit T lymphocyte proliferation [62]. The enrichment of prostaglandin E2 (PGE2) and TGF-β in tumor-derived EVs induces the accumulation of MDSCs with immune suppressive properties [63]. Similarly, it has been shown that tumor-derived EV-associated Hsp72 or Hsp70 mediate the suppressive activity of the MDSCs via STAT3 activation [64, 65]. The presence of HSP72 and HSP105 in EVs has also been reported in melanoma, lung, and breast cancer cell lines, as well as in the serum of breast cancer patients. These EVs have been shown to activate dendritic cells and induce secretion of interleukin-6, which promotes tumor invasion by increasing MMP-9 metalloproteinase expression [66]. Tumor cells can also release EVs containing MHC class 1 related chain ligand A (MICA) that is capable of binding to the NK cells receptor, NKG2D, leading to its downregulation and resulting in a marked reduction in NK cytotoxicity independent of NKG2D ligand expression by the target cell [67]. Tumor-released miRNAs have also been involved in immune suppression. For instance, miR-214 secreted into EVs from Lewis Lung carcinoma cells was sufficiently delivered into recipient T cells and in vivo studies indicated that miR-214 mediates regulatory T cell expansion resulting in enhanced immune suppression and tumor growth in mice [68].
Extracellular vesicles and metastasis
Metastasis is a multistep process leading to the dissemination of primary tumor cells to distant organs. Tumor-derived EVs have almost been involved in all steps of tumor invasion and metastasis [15, 69–71]. Studies have reported that tumor-associated EVs play a significant role in invasion and metastasis through invadopodia formation [18, 72]. Invadopodia are dynamic actin-rich membrane protrusions that tumor cells produce to degrade and invade through the extracellular matrix [72]. It was recently proposed that invadopodia are docking sites for EVs facilitating the degradation of the extracellular matrix through a localized secretion of metalloproteinase MT-1-MMP, thus promoting cell invasion [15, 73]. Similarly, the migration of tumor cells through tissues and chemotactic gradients is also initiated by the formation and release of fibronectin-bound EVs at the leading edge of migrating cells. These fibronectin-bound EVs are proposed to promote adhesion assembly and stabilization allowing a directional and persistent tumor cell migration [74, 75]. Tumor-derived EVs are also known to influence the integrity of vascular barriers, which is frequently associated with metastatic dissemination. Proteomics analysis of tumor-associated EVs has shown that EVs release a number of proteins such as SERPINA1, SERPINF2, and MMP9, the up-regulation of which play a significant role in ECM remodeling, vascular leakiness, and invasiveness [76]. Likewise, melanoma-derived EVs have been shown to induce pulmonary vascular leakiness [77], while EVs produced by glioblastoma cells containing high levels of VEGF-A induce endothelial cell permeability and angiogenesis in vitro [78]. In addition, EVs derived from lung cancer or breast cancer cells were reported to carry miR-23a and miR-105 respectively, which both target tight junction protein ZO-1, thereby increasing vascular permeability and cancer transendothelial migration [79, 80]. An interesting feature of tumor-derived EVs is their ability to establish a pre-metastatic niche, a phenomenon where the primary tumor can promote its own metastasis by recruiting stromal cells to distant organs or by modulating gene expression of distant cells in order to establish a growth supportive environment. EVs derived from colorectal cancer cells enriched for miR-21 can be specifically targeted to liver tissue and induce liver macrophage polarization towards an interleukin-6 (IL-6)-secreting pro-inflammatory phenotype, therefore promoting an inflammatory pre-metastatic niche supportive of liver metastasis [81]. Moreover, melanoma EVs were shown to home to lymph nodes and consequently enhance the migration of melanoma cells to sentinel lymph nodes. In addition, melanoma EVs were able to upregulate the expression of genes within the distal lymph node microenvironment related to tumor cell recruitment to sentinel nodes, extracellular matrix modifiers promoting trapping of melanoma cells, and vascular growth factors promoting melanoma growth, creating a pre-metastatic niche supportive of metastasis [82]. Melanoma-derived EVs were further reported to educate bone marrow-derived cells towards a pro-vasculogenic and pro-metastatic phenotype through the receptor tyrosine kinase MET [77]. More recently, the uptake of pancreatic ductal adenocarcinoma-derived EVs by Kupffer cells (liver macrophages) was reported to cause TGF-β secretion and upregulation of fibronectin production by hepatic stellate cells, leading to an enhanced recruitment of bone marrow-derived macrophages through macrophage migration inhibitory factor (MIF), whose association with EVs correlated with liver metastasis occurrence and disease progression [83]. Interestingly, using different tumor models, Hoshino and colleagues reported that the metastatic organotropism and establishment of a pre-metastatic niche is mediated by EVs via the secretion of different sets of integrins (for e.g. integrin- α6β4, α6β1, or αvβ5) that favor the preferential fusion of tumor cells with resident cells at their predicted destination. The authors showed that tumor-derived EVs taken-up by organ-specific cells prepared the pre-metastatic niche and that distinct integrin patterns predicted the organotropism of tumor cells, integrins α6β4, and α6β1 being associated with lung metastasis, while integrin αvβ5 was found to be associated with liver metastasis [84]. Reprogrammed glucose metabolism is a hallmark of cancer cells. Remarkably, cancer cells are also proficient in reprograming the glucose metabolism of stromal cells through the release of EVs carrying high levels of the miR-122 that target the glycolytic enzyme pyruvate kinase. This mechanism is proposed to facilitate metastasis by increasing nutrient availability in the pre-metastatic niche [70].
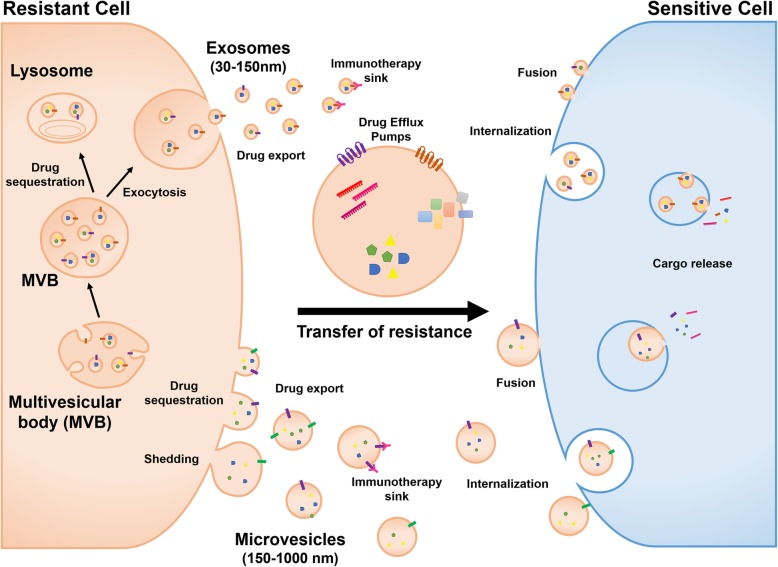
Extracellular vesicles as modulators of anti-cancer drug resistance
Drug resistance poses a serious challenge for the treatment of cancer and occurs when cancer cells become tolerant to anti-cancer drugs. Although many types of cancers are initially susceptible to anti-cancer drugs, tumor cells can develop resistance over time through different mechanisms that impair drug efficacy. The most common mechanisms of drug resistance include genetic or epigenetic upregulation of prosurvival signaling and inhibition of apoptotic pathways, drug inactivation or alteration of drug target molecules, overexpression of multidrug resistance proteins (MDR) and increased transport of efflux pumps, or drug export. Recently, the emergence of EVs as novel drug resistance modulators has added to the complexity of resistance mechanisms. EVs mediate intercellular communication by transferring proteins and nucleic acids to remote target cells. The development of drug resistance via EVs is articulated around mechanisms involving such cargo. EVs can mediate drug resistance by directly exporting or sequestering cytotoxic drugs, reducing their effective concentration at target sites. Recent evidence has shown that EVs play an important role not only in mediating drug resistance, but also in conferring resistance to drug-sensitive cancer cells. Indeed, EVs are capable of horizontal transfer of specific bioactive cargoes that may alter cell cycle control and apoptotic programs in recipient cells (Fig. 2). EVs can also mediate intercommunication between cancer cells and stromal cells within the tumor microenvironment, leading to the acquisition of drug resistance and tumor progression. Mastering our understanding of these resistance mechanisms will help in improving cancer treatments and subsequently patients’ outcome. Detailed mechanisms by which resistance may occur are outlined in this section.
Fig. 2.
Mechanisms of extracellular vesicles-mediated transfer of anti-cancer drug resistance. Extracellular vesicles can mediate drug resistance by directly exporting or sequestering cytotoxic drugs reducing their effective concentration at target sites. Extracellular vesicles can also compete with bona fide target cells for the binding of immunotherapeutic agents targeting cellular antigens. Extracellular vesicles also mediate transfer of drug resistance to drug-sensitive cancer cells through the horizontal transfer of specific bioactive cargoes including drug efflux pumps, prosurvival factors, inhibitors of apoptosis, and non-coding RNAs
Extracellular vesicles as a sink for immunotherapies
Cancer cells use extracellular vesicles to compromise targeted therapies. EVs carry on their surface, a plethora of cellular antigens displayed in an orientation identical to that found on the surface of cells from which they emanate. The presence, on EVs surface, of cellular antigens targeted by immunotherapy acts as a sink for monoclonal antibodies-based drugs, thereby diminishing their bioavailability to their intended target. In the case of B-cell lymphoma, the presence of CD20 on the surface of EVs protects targeted lymphoma cells from rituximab (an anti-CD20 monoclonal antibody) attack [85]. In vitro as well as in vivo studies in breast cancer point to the role of HER2-positive extracellular vesicles in modulating resistance to anti-HER2 monoclonal antibody Trastuzumab. Extracellular vesicles secreted either by HER2-positive tumor cells in vitro or found in the serum of breast cancer patients bind to Trastuzumab, and inhibit its activity in vitro [86]. More recently, EVs have been involved in another type of drug resistance mediated by cellular receptor expression. The immunotherapy breakthrough crowned by the 2018 Medicine Nobel prize consists in the use of inhibitors of immune-checkpoints to unleash the power of an immune system otherwise tamed by immune checkpoint ligand expressed on the surface of tumor cells. The disruption of the interaction of the checkpoint ligand (e.g. PD-L1) with the inhibitory checkpoint receptor (PD-1) on T cells, restores T cell function and anti-tumor immunity. However, not all patients respond to such immune checkpoint inhibitor therapy, and the presence of checkpoint ligand (PD-L1) on EVs early after therapy, classifies patients as responders or resistant to anti-PD-1 therapy in melanoma [87]. By capturing the immunotherapeutic antibody on their surface, EVs drive this antibody away from the tumor, leaving it free to engage PD-1 on oncoming tumor-specific T cells. The same mechanism has been described in the case of glioblastoma in vitro, in which tumor-derived EVs were shown to express PD-L1 and inhibit T cell proliferation as well as antigen-specific T cell responses [88].
Extracellular vesicles-mediated drug export and sequestration
Irrespective of the administration route of anti-cancer drugs, systemic, oral or subcutaneous, the main goal of the treatment is to target drugs to the tumor site, where cellular drug uptake or membrane permeability are determinant in the drug efficacy and treatment success. However, it is recognized that abnormal tumor architecture (e.g.: poor vascularization, abnormal extracellular matrix) complicates drug uptake and is associated with therapy failure and drug resistance [89]. Even in case of efficient uptake of drugs by targeted cells, cancer cells are known to export drugs in the extracellular space using specialized transporters of the multi-drug resistance (MDR)-ATP binding-cassette (ABC transporters) system [90]. These pumps reduce the intracellular accumulation of many anti-cancer drugs to sub-therapeutic levels, thus decreasing or abolishing drug efficacy. In addition, EVs can be utilized by cancer cells as drug vehicles to facilitate drug resistance through drug sequestration and expulsion. Shedden and colleagues were the first to report a positive correlation between the expression of genes associated with vesicle shedding and drug resistance in a large panel of different cancer cell lines [91]. Furthermore, using a breast cancer cell line, they showed by fluorescence microscopy and flow cytometry that the fluorescent chemotherapeutic agent doxorubicin was physically encapsulated into vesicles and expelled out into the extracellular media [91]. More recently, melanoma cells were shown to resist to cisplatin treatment through an extracellular acidification-mediated increase of EVs secretion and the direct export of cisplatin into these vesicles [92]. Similarly, cisplatin was found to be disposed out of resistant ovarian carcinoma cells in extracellular vesicles [93]. Interestingly, EVs from resistant cells not only contained Multidrug Resistance-associated Protein 2 (MRP-2) but also the copper-transporting P-type ATPases, ATP7A and ATP7B [93]. B-cell lymphoma cells also efficiently extruded doxorubicin and pixantrone in EVs in vitro [94]. Interestingly, ATP-transporter A3 (ABCA3) expression is crucial for EVs biogenesis and contributes to the observed drug resistance. Indeed, genetic or chemical depletion of ABCA3 enhanced intracellular retention of both drugs [94].
Cancer cells can also sequester drugs within intracellular vesicles preventing them from reaching the targeted subcellular compartment and rendering them nonfunctional. In a breast cancer cell model resistant to mitoxantrone, cells displayed increased EV-like structures at the plasma membrane containing the ATP-binding cassette ABCG2 in which mitoxantrone was significantly sequestered [95]. Subcellular drug sequestration was also shown to be mediated by ABCA3 in leukemia cells resistant to a panel of cytostatic drugs [96]. Indeed, ABCA3 localized to the limiting membranes of lysosomes and multivesicular bodies and caused cytostatic drugs to be efficiently sequestered [96].
Extracellular vesicles-mediated transfer of drug efflux pumps
In addition to drug export or sequestration, cancer cells can transmit resistance through horizontal transfer of EVs carrying drug efflux pumps. Drug efflux transporters of the multi-drug resistance (MDR)-ATP binding-cassette (ABC transporters) system have long been acknowledged as major contributors to multidrug resistance in tumor cells [90]. EVs carrying P-glycoprotein (P-gp, MDR-1 or ABCB1), one of the most well-studied drug efflux pump, have been implicated in the transfer of multidrug resistance to sensitive cells in several human cancer models, such as prostate and ovarian cancers, acute T lymphoblastic leukemia, and osteosarcoma [97–100]. Indeed, EVs from sera of patients undergoing a course of docetaxel treatment compared to matched EVs from the same patients prior to commencing docetaxel treatment, when applied to both prostate cancer drug sensitive and resistant cells, showed a correlation between cellular response to docetaxel and patients’ response to treatment with docetaxel [97]. Similarly, extracellular vesicles-mediated intercellular transfer of functional MRP1 drug efflux transporter (ABCC1) was reported in leukemia cells [101]. Other drug efflux exporters such as ABCG2 or ABCA3 have been shown to transfer horizontally through EVs and modulate drug resistance in recipient cells [85, 102]. Although tumor cells represent an abundant source of EVs, it is important to question whether the consequences of this transfer of cargo is sustainable in vivo. The presence of selective P-gp/MDR-1 mRNA in EVs released from doxorubicin-resistant osteosarcoma cells suggests that resistant tumor cells use several means to spread drug resistance to sensitive cells, either by transferring MDR proteins directly to sensitive cells or by transferring the mRNA that encodes them, contributing to the diversity of drug resistance mechanisms [100]. On the other hand, depletion of drug efflux pumps through EVs exocytosis has been shown to increase the sensitivity of tumor cells to anti-cancer drugs in vitro. In an in vivo setting, one can legitimately wonder whether this in vitro beneficial response could not result in a net drug resistance within the tumor microenvironment. Indeed, these EVs loaded with MDR transporters could be transferred to other cells within the heterogeneous tumor itself or the stromal cells within the tumor microenvironment, therefore possibly influencing their response to treatment.
Extracellular vesicles-mediated export of prosurvival cargo
EVs transfer of cargo can contribute to the heterogeneity of tumor response to anti-cancer drugs. This cargo includes prosurvival factors, which enhance cell viability and decrease apoptosis sensitivity, thus leading to resistance to anti-cancer drugs. For instance, components associated with the PI3K/AKT pathway, one of the major oncogenic signaling axis involved in cancer cell proliferation and survival, have been reported in EVs. In hepatocellular carcinoma (HCC) invasive cells lines, resistance to Sorafenib in vitro as well as in vivo was induced by delivery of hepatocyte growth factor (HGF) through EVs and subsequent activation of the HGF/c-MET/PI3K/AKT signaling pathway [103]. In addition, platelet-derived growth factor receptor-beta (PDGFR-β), which is enriched in EVs released by melanoma cells resistant to BRAF inhibitor, PLX4720, can be transferred to recipient melanoma cells, resulting in a dose-dependent activation of PI3K/AKT signaling and escape from BRAF inhibition [104]. More recently, triple negative breast cancer cell lines resistant to Docetaxel and Doxorubicin were shown to release EVs that induced resistance to these chemotherapy drugs in recipient non-tumorigenic breast cells [105]. Indeed, these EVs caused changes in gene expression associated with cell proliferation and apoptosis including the PI3K/AKT pathway, suggesting that they may contain ligands or receptors connected to the PI3K signaling axis [105]. Likewise, EVs can also carry prosurvival molecules that modulate the immune system functions likely inducing immune tolerance and escape. Transforming growth factor-β (TGF-β) cytokines have been shown to play a critical role in establishing immunological suppression [106]. Indeed, TGF-β1 was found in tumor-derived EVs and reported to inhibit the proliferation of healthy donor peripheral blood lymphocytes in response to IL-2 and to induce regulatory T cells [59]. Additionally, in vivo and in vitro studies on HER2-overexpressing breast cancer have reported the presence of increased amounts of the immunosuppressive cytokine TGF-β1 in EVs released from cells resistant to HER2-targeting drugs [107]. Although the patients’ cohort was too small to be conclusive, these findings suggest that the level of EVs-associated TGF-β1 in the plasma of the patients correlates with resistance to Lapatinib and Trastuzumab [107]. Resistance to apoptosis is a vital escape mechanism by which tumor cells acquire drug resistance and thus contribute to cancer progression. EVs-mediated delivery of prosurvival factors is proposed to provide tumor cells with an additional mechanism to suppress cell death induced by anti-cancer drugs. Survivin is a prosurvival protein member of the inhibitors of apoptosis (IAP) family shown to be present in EVs derived from different tumor types [108–110]. Survivin has been implicated in the suppression of cell death and the regulation of mitosis, and therapeutic strategies targeting survivin in cancer are intensively investigated [111]. Indeed, Khan and colleagues identified EVs as mediators of stress-induced survivin secretion from HeLa cells treated with a sublethal dose of proton irradiation [109]. More recently, Kreger and colleagues have reported that treating highly aggressive MDA-MB-231 breast cancer cells with Paclitaxel (PTX) induces the secretion of EVs enriched with survivin that significantly promote the survival of serum-starved and PTX-treated fibroblasts and SKBR3 breast cancer cells [112].
Moreover, the enrichment of microRNAs (miR) in EVs have been shown to promote anti-cancer drugs resistance in different cancers (Table 1). For example, the investigation of drug resistance in breast cancer cells or pancreatic ductal adenocarcinoma cells revealed that EVs-mediated transfer of miR-155 to sensitive cells resulted in chemoresistance spreading. Interestingly, increased accumulation of miRNA in EVs exposed to chemotherapeutic agents can also serve as a disposal mechanism aimed at decreasing the intracellular levels of miRNA with drug sensitivity promoting roles [113, 114].
Table 1.
Extracellular vesicles miRNA cargo and chemoresistance in different cancers
| Cancer | Anti-cancer drugs | Cell lines | miRNA cargo | Mechanism | Reference |
|---|---|---|---|---|---|
| Lung | Cisplatin | A549/A549-DDP | ↓ miR-100-5p | horizontal transfer | [133] |
| Lung | Gemcitabine | A549/A549-GR | ↑ miR-222-3p | horizontal transfer | [134] |
| Lung | Cisplatin | A549/H1299 | ↑ miR-96 | horizontal transfer | [135] |
| Lung | Cisplatin | A549/A549-DDP | ↓ miR-146a-5p | horizontal transfer | [136] |
| Breast | Docetaxel | MCF-7 | ↑ miR-100, miR-222, miR-30a, miR-17 | horizontal transfer | [137] |
| Breast | Tamoxifen | MCF-7 | ↑ miR-221/222 | horizontal transfer | [138] |
| Breast | Cisplatin 17-AAG PU-H71 |
Hs578Ts | ↓ miR-134 | horizontal transfer | [139] |
| Breast | Doxorubicin Paclitaxel |
MCF-7/MDA-MB-231 | ↑ miR-155 | horizontal transfer | [140] |
| Breast | Docetaxel Epirubicin Gemcitabine |
MDA-MB-231/HMLE | ↑ miR-1246 | horizontal transfer | [141] |
| Breast | Adriamycin | MCF-7/MCF-7-Adr | ↑ miR-222 | horizontal transfer | [142] |
| Oral cavity | Cisplatin | HSC-3/HSC-3R SCC-9/SCC-9R |
↑ miR-21 | horizontal transfer | [143] |
| Melanoma | Vemurafenib (PLX4032) |
MML-1/MML-1R A375 PDX |
↑ miR-211–5p | Autocrine | [144] |
| Glioblastoma | Temozolomide | SHG-44/U87MG | ↑ miR-221 | horizontal transfer | [145] |
| Prostate | Docetaxel | 22Rv1/22Rv1RD DU145/DU145RD PC3/PC3RD |
↓ miR-34a | horizontal transfer | [146] |
| Colon | Fluorouracil (5-FU) |
DLD-1/DLD-1-5-FU | ↑ miR-145, miR-34a | expulsion | [113] |
| Pancreas | Gemcitabine | Panc1/Panc1-GR | ↑ miR-155 | horizontal transfer | [147] |
| Leukemia | Imatinib | K562/K562-G01 | ↑ miR-365 | horizontal transfer | [148] |
| Leukemia | Daunorubicin | HL60/HL60AR | ↑ miR-196, miR20a | expulsion | [114] |
Tumor microenvironment-mediated intercellular communication and drug resistance
Tumor growth and drug resistance are not only determined by cancer cells but are also supported by non-tumor cells within the tumor microenvironment. The importance of the role of EVs in the intercellular communication within the tumor microenvironment is increasingly acknowledged. The bidirectional EV-mediated transfer of cargo to and from non-tumor cells effectively influences recipient cell’s phenotype as well as their response to anti-tumor treatments, thus promoting the development of an environment hospitable towards cancer growth, invasion, and metastasis. For instance, by secreting chemoresistance-inducing EVs containing Snail and miR-146, pancreatic cancer-associated fibroblasts (CAFs), that are intrinsically resistant to the chemotherapeutic agent gemcitabine, have been shown to mediate the transfer of resistance to pancreatic cancer epithelial cells when exposed to this drug, thereby increasing their proliferation and survival [39]. Similarly, Binenbaum and colleagues have recently reported that transfer of miR-365 in macrophage-derived EVs induces resistance of pancreatic adenocarcinoma cells to gemcitabine in vitro and in vivo [115]. Moreover, CAF-derived EVs further promoted tumor growth of colorectal cancer stem cells (CSCs) upon treatment with 5-fluorouracil or oxaliplatin, even though these cells were intrinsically chemoresistant. Interestingly, the authors have also shown that inhibition of EVs secretion by CAF increased chemosensitivity of colorectal CSCs [116]. Likewise, the vesicular transfer of miR-21 from cancer-associated adipocytes and fibroblasts to ovarian cancer cells has been reported to decrease apoptosis and promote chemoresistance to paclitaxel by downregulating the expression of apoptotic peptidase activating factor (APAF1) mRNA [117]. Similarly, tumor-associated macrophages (M2 polarized macrophages)-derived secretion of miR-21 has been shown to confer cisplatin resistance in gastric cancer cells. Functional studies revealed that vesicular miR-21 can be directly transferred from macrophages to gastric cancer cells, where it suppresses cell apoptosis and enhances activation of PI3K/AKT signaling pathway through down-regulation of PTEN [118]. Furthermore, Boelens and colleagues have previously reported that vesicular RNA from stromal cells, which are largely noncoding transcripts and transposable elements, can be transferred to breast cancer cells, leading to the expansion of therapy and radiation resistant breast cancer cells through a mechanism involving NOTCH3 induction [119]. Accumulating pieces of evidence show that mesenchymal stem cells (MSCs) are chemo-attracted by tumors where their plastic properties are reported to support tumor growth. Indeed, human MSC-derived EVs were found to induce resistance of gastric cancer cells to 5-Fluorouracil both in vivo and ex vivo through the inhibition of 5-fluorouracil-induced apoptosis and enhanced expression of multidrug resistance-associated proteins. The authors have reported that mesenchymal stem cells-EVs could induce drug resistance in gastric cancer cells by activating CaM-Ks/Raf/MEK/ERK signaling pathway [120].
Cancer and stromal cells within the tumor microenvironment have often restricted access to nutrients and oxygen and thus are subjected to hypoxia [121]. In this setting, hypoxia-induced EVs have been shown to contribute to the chemoresistance of ovarian cancer cells in a mechanism involving STAT3. Indeed, hypoxia-induced EVs are capable of increasing the survival of tumor cells in response to cisplatin treatment in vitro. In addition, cisplatin efflux through EVs was shown to be significantly augmented in ovarian cancer cell lines cultured under hypoxic conditions [122].
The crosstalk between tumor cells and stromal cells is bidirectional as cancer cells can also influence the behavior of stromal cells through EVs secretion. For instance, Bandari and colleagues found that anti-myeloma chemotherapy (Bortezomib, Carfilzomib, or Melphalan) dramatically stimulates surface heparanase-rich EVs secretion capable of degrading the ECM and that exposure of these EVs to macrophages enhanced the secretion of TNF-α (an important myeloma growth factor) and stimulated their migration [123]. On the other hand, anti-cancer drugs (Paclitaxel, etoposide, irinotecan hydrochloride, or carboplatin) have been reported to cause chemoresistant hepatocellular carcinoma cells to release EVs that elicit superior anti-tumor NK cell responses compared to chemosensitive cells, in a mechanism mediated by EV secretion of heat shock proteins. Interestingly, this study provides a clue for finding an effective vaccine for hepatocellular carcinoma immunotherapy [124].
Strategies to mitigate EVs-mediated drug resistance
When considering strategies to mitigate the role of EVs in transferring drug resistance, two major avenues come to mind. The first one is to modulate the production of EVs, by blocking their secretion. Because of the universality of EVs secretion and of the lack of drugs that can specifically target secretion of EVs by cancer cells, this strategy is likely to interfere with unwanted EVs secretion, including the secretion of EVs involved with the acquisition and transfer of resistance to anti-cancer drugs, as well as with the secretion EVs involved in normal physiological processes. The second possibility for mitigating drug resistance mediated by tumor-derived EVs is to specifically remove these EVs once they have been produced, without interfering with EVs secretion. This approach has the advantage of maintaining the secretion of “beneficial” EVs, affecting only those EVs secreted by cancer cells. This second approach relies on the availability of markers specific for tumor-derived EVs. Such markers are available for certain cancers. Both strategies have been pursued in vitro and in vivo.
Federici et al. described the effect of proton pump inhibitor on both cisplatin uptake and EVs release in vitro an in vivo in a mouse xenograft model of melanoma, in which they show that treatment with a proton pump inhibitor decreases the overall EVs release and increases tumor cell sensitivity to cisplatin [92]. Roseblade et al. have evaluated the efficacy of several inhibitors of EVs release in response to calcium mobilization, including the use of a calpain inhibitor [125], which was also shown to block EVs release by prostate cancer cell lines in vitro and increased their sensitivity to chemotherapy in vivo [126]. Similarly, Muralidharan-Chari et al. showed that the inhibition of EVs release by preventing the activation of the extracellular signal-regulated kinase (ERK) using a MEK inhibitor, resulted in an increased sensitivity of pancreatic cancer cell lines to gemcitabine in vitro and in a tumor graft model in vivo [127]. While the selectivity of agents specifically blocking EVs release in cancer maybe lacking for most, some inhibitors target isoforms of enzymes preferentially associated with cancer cells. This is the case for inhibitors of peptidylarginine deiminase PAD2 and PAD4 which are overexpressed in prostate, ovarian and other types of cancer cells, and whose inhibition by chloramidine reduces the release of EVs and increases cancer cell sensitivity to drugs [128]. In a more systematic in vitro approach, interference with different steps of EVs biogenesis in prostate and breast cancer cell lines, Kosgodage et al. confirmed that among a series of 11 inhibitors targeting various steps of EVs biogenesis, PAD inhibitors, as well as inhibitors of PKC (Bisindolylmaleimide-I), were the most powerful inhibitors in prostate and breast cancer cell lines [129]. Recently, the same group demonstrated the powerful role of cannabinol (CBD) as an inhibitor of EVs release by prostate, hepatocellular carcinoma, and breast cancer cell lines, increasing cell sensitivity to anti-cancer drugs [130].
While these pharmacologic interventions have proven successful in vitro and in some cases in animal models in vivo, their lack of selectivity for cancer cells, for the most part, calls for some reservations on their systematic therapeutic use. This is not the case for the specific removal of circulating EVs from plasma. A method similar to hemodialysis, extracorporeal hemofiltration using cartridges made of hollow fibers with a size cutoff of 200 nm coupled with an affinity matrix allows the specific removal of ultrafiltrated EVs. This method, called Adaptive Dialysis-like Affinity Platform Technology (ADAPT™), has been originally developed by Aethlon Medical Inc. for removing Hepatitis C virus (HCV) particles from the blood of infected patients. The safety and efficacy of the method have been clinically validated in HCV infected end-stage renal disease patients using a lectin as an affinity matrix for the selective removal of HCV particles [131]. The extension of this method to the specific removal of EVs with a size inferior to that of the hollow fiber cutoff has been discussed by Marleau et al. [132]. In a previous section, we discussed the involvement of EVs in the escape to immunotherapies, by acting as a sink for immuno-targeting drugs specific for cancer-associated antigens such as CD20 in the case of B cell lymphoma [85], HER2 in the case of breast cancer [86] and more generally, PD-L1 [87, 88]. The specific removal of EVs expressing these antigens by an appropriate affinity hemofiltration device, such as those described in the ADAPT™ method will likely mitigate the immunotherapy sink effect mediated by EVs bearing the targeted antigens.
Conclusions and future perspectives
Drug resistance is a huge hurdle in the treatment of cancer. Among the mechanisms governing the establishment of resistance to anti-cancer therapies, EVs have recently emerged as important modulators of drug resistance through a variety of mechanisms described in this review. EVs dynamically contribute, even though transiently, to the heterogeneity of the tumor through their diverse cargo content. Unraveling the precise biological composition of EVs will be critical to determining their role in cancer and will likely aid in developing therapies targeting these roles. However, the field still struggles to assess EVs heterogeneity due to the lack of standardized isolation techniques that go beyond subcellular origin, size, and floatation density. Further dissection of EVs heterogeneity will be essential to improving our understanding of the critical roles of EVs in cancer.
Exploiting EVs molecular cargo as well as the potential development of EVs as drug vehicles for effective therapeutic strategies both hold promises in cancer diagnostics and therapeutics. Omics on EVs derived from liquid biopsies (such as blood, saliva or urine) will likely aid in the early diagnosis of cancer through biomarkers discovery or in the assessment of response to therapies while avoiding invasive biopsy procedures. Related to therapeutics, EVs have been proposed as a new type of drug delivery system. Bioengineered EVs loaded with chemotherapeutic drugs or expressing ligands which target particular malignant cells have the potential for future cancer treatment. The inherent protection of the cargo and personalized cellular targeting simultaneously enhance the solubility, stability, and specificity of the therapeutic agent.
Given the prominence of EVs in almost all aspects of tumor development and progression, it seems evident to explore translational approaches that would prevent these undesirable effects. Nevertheless, EVs-mediated cell-to-cell communication is a conserved mechanism in normal cell physiology and their inhibition is likely to be toxic unless specific strategies distinguishing pathogenic EVs from beneficial ones are developed. In order to develop such strategies, it is essential to establish standardized techniques allowing consistent isolation of EVs subpopulations. This knowledge is necessary to identify cancer-derived EVs that should be targeted by any therapeutic approach. The use of EVs as cell-free therapies has also been employed in cancer vaccine and immunotherapy fields. Encouraging studies suggest the use of immune cells-derived EVs as a new potential strategy for cancer vaccine research. Only if taken together, technology and biology will pave the way for the future use of EVs in many clinical applications.
Acknowledgments
SM, MH, and JCG are supported by Sidra Medicine institutional funding. AAB is supported by Sidra Medicine internal grant (SIRF_20046). LJ is supported by NIH F32 grant (CA217064). AR is supported by NCCCR, HMC institutional funding. SU is supported by Medical Research Center, HMC institutional grant (Grant #16354/16).
Funding
The authors declare no funding support was received for this study.
Availability of data and materials
Not applicable, please refer to the original reference.
Abbreviations
- ABC
ATP binding-cassette
- ADAPT™
Adaptive Dialysis-like Affinity Platform Technology
- AKT
AKT serine/threonine kinase
- Alix
Apoptosis-linked gene 2-interacting protein X
- APAF1
Apoptotic peptidase activating factor
- ARF6
ADP-ribosylation factor 6
- ARMM
ARRDC1-mediated microvesicles
- ARRDC1
Arrestin 1 domain-containing protein 1
- ATP7A
ATPase Copper Transporting alpha
- ATP7B
ATPase Copper Transporting beta
- CAF
Cancer-associated fibroblast
- CaM-K
Calcium/calmodulin-dependent protein kinase
- CBD
Cannabinol
- c-MET
MET proto-oncogene, receptor tyrosine kinase
- CSF1
Colony stimulating factor 1
- CXCR4
C-X-C chemokine receptor type 4
- ECM
Extracellular matrix
- EGF
Epidermal growth factor
- EGFR
Epidermal growth factor receptor
- EMT
Epithelial-to-mesenchymal transition
- ERK
Extracellular signal-regulated kinase
- ESCRT
Endosomal sorting complex required for transport
- Fas-L
Fas ligand
- HCC
Hepatocellular carcinoma
- HCV
Hepatitis C virus
- HER2
Human epidermal growth factor receptor 2
- HES1
Hes family BHLH transcription factor 1
- HES5
Hes family BHLH transcription factor 5
- HGF
Hepatocyte growth factor
- HSP105
Heat shock protein 105
- Hsp70
Heat shock protein 70
- Hsp72
Heat shock protein 72
- IAP
Inhibitors of apoptosis
- IL-2
Inteleukin-2
- IL6
Interleukin-6
- ILV
Intraluminal vesicle
- JAK
Janus kinase
- MAPK
Mitogen-activated protein kinase
- MDR
Multidrug resistance proteins
- MDSC
Myeloid-derived suppressor cells
- MEK
MAPK/ERK Kinase
- MICA
MHC class 1 related chain ligand A
- MIF
Migration inhibitory factor
- MLCK
Myosin light-chain kinase
- MMP9
Matrix metalloproteinase 9
- MRP1
Multidrug resistance-associated protein 1
- MSCs
Mesenchymal stem cells
- MT-1-MMP
Membrane-type-1 matrix metalloproteinase
- MVE
Multivesicular endosome
- NK
Natural killer
- NKG2D
NKG2-D-activating natural killer receptor
- NOTCH2
Neurogenic locus notch homolog protein 2
- NOTCH3
Neurogenic locus notch homolog protein 3
- nSMase2
Neutral sphingomyelinase 2
- PAD2
Peptidylarginine deiminase 2
- PAD4
Peptidylarginine deiminase 4
- PAR-2
Protease-activated receptor 2
- PCP
Planar cell polarity
- PD-1
Programmed cell death receptor 1
- PDGF
Platelet-derived growth factor
- PDGFRβ
Platelet-derived growth factor receptor-beta
- PD-L1
Programmed death ligand 1
- PGE2
Prostaglandin E2
- P-gp
P-glycoprotein
- PI3K
Phosphatidylinositol-3-kinase
- PLD
Phospholipase D
- PLP
Proteolipid protein
- PMEL
Premelanosome protein
- PS
Phosphatidylserine
- PSAP motif
Proline-serine-alanine-proline motif
- PTEN
Phosphatase and tensin homolog
- Raf
Raf-1 proto-oncogene, serine/threonine kinase
- SDF1
Stromal cell-derived factor 1
- SERPINA1
Serpin family A member 1
- SERPINF2
Serpin family F member 2
- SOCS5
Suppressor of cytokine signaling 5
- STAT
Signal transducer and activator of transcription
- TF
Tissue factor
- TGF-β
Transforming growth factor-beta
- TME
Tumor microenvironment
- TNF-α
Tumor necrosis factor alpha
- TSG101
Tumor susceptibility gene 101
- tTG
Tissue transglutaminase
- VEGF
Vascular endothelial growth factor
- VPS4
Vacuolar protein sorting 4
- VTA-1
Vesicle trafficking 1
- Wnt4
Wingless-type MMTV integration site family, member 4
- WWP2
WW Domain containing E3 ubiquitin protein ligase 2
- ZO-1
Zonula occludens protein 1
Authors’ contributions
SM, AAB, and LJ performed the scientific literature search, designed the review structure, elaborated the figures and tables, and wrote the manuscript. AR helped with the writing of the manuscript. MH and SU assisted with the design of the manuscript. JCG helped with the manuscript writing and corrected the final version of the document. All authors have read and approved the final version of the manuscript.
Ethics approval and consent to participate
Not applicable, neither ethics approval was required for this review nor involvement of patients.
Consent for publication
All authors consent to publication.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Selma Maacha, Email: smaacha@sidra.org.
Ajaz A. Bhat, Email: abhat@sidra.org
Lizandra Jimenez, Email: lizandra.jimenez@vanderbilt.edu.
Afsheen Raza, Email: ARaza@hamad.qa.
Mohammad Haris, Email: mharis@sidra.org.
Shahab Uddin, Email: Skhan34@hamad.qa.
Jean-Charles Grivel, Phone: +974 40 037 407, Email: jgrivel@sidra.org.
References
- 1.Naito Y, Yoshioka Y, Yamamoto Y, Ochiya T. How cancer cells dictate their microenvironment: present roles of extracellular vesicles. Cell Mol Life Sci. 2017;74(4):697–713. doi: 10.1007/s00018-016-2346-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sullivan R, Maresh G, Zhang X, Salomon C, Hooper J, Margolin D, et al. The Emerging Roles of Extracellular Vesicles As Communication Vehicles within the Tumor Microenvironment and Beyond. Front Endocrinol (Lausanne) 2017;8:194. doi: 10.3389/fendo.2017.00194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liu Y, Cao X. The origin and function of tumor-associated macrophages. Cell Mol Immunol. 2015;12(1):1–4. doi: 10.1038/cmi.2014.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xing F, Saidou J, Watabe K. Cancer associated fibroblasts (CAFs) in tumor microenvironment. Front Biosci (Landmark Ed) 2010;15:166–179. doi: 10.2741/3613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van Niel G, D'Angelo G, Raposo G. Shedding light on the cell biology of extracellular vesicles. Nat Rev Mol Cell Biol. 2018;19(4):213–228. doi: 10.1038/nrm.2017.125. [DOI] [PubMed] [Google Scholar]
- 6.Nabhan JF, Hu RX, Oh RS, Cohen SN, Lu Q. Formation and release of arrestin domain-containing protein 1-mediated microvesicles (ARMMs) at plasma membrane by recruitment of TSG101 protein. P Natl Acad Sci USA. 2012;109(11):4146–4151. doi: 10.1073/pnas.1200448109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Minciacchi VR, Freeman MR, Di Vizio D. Extracellular vesicles in cancer: exosomes, microvesicles and the emerging role of large oncosomes. Semin Cell Dev Biol. 2015;40:41–51. doi: 10.1016/j.semcdb.2015.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maas SLN, Breakefield XO, Weaver AM. Extracellular Vesicles: Unique Intercellular Delivery Vehicles. Trends Cell Biol. 2017;27(3):172–188. doi: 10.1016/j.tcb.2016.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Abels ER, Breakefield XO. Introduction to extracellular vesicles: biogenesis, RNA cargo selection, content, release, and uptake. Cell Mol Neurobiol. 2016;36(3):301–312. doi: 10.1007/s10571-016-0366-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Trajkovic K, Hsu C, Chiantia S, Rajendran L, Wenzel D, Wieland F, et al. Ceramide triggers budding of exosome vesicles into multivesicular endosomes. Science. 2008;319(5867):1244–1247. doi: 10.1126/science.1153124. [DOI] [PubMed] [Google Scholar]
- 11.Kosaka N, Iguchi H, Yoshioka Y, Takeshita F, Matsuki Y, Ochiya T. Secretory mechanisms and intercellular transfer of microRNAs in living cells. J Biol Chem. 2010;285(23):17442–17452. doi: 10.1074/jbc.M110.107821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.van Niel G, Charrin S, Simoes S, Romao M, Rochin L, Saftig P, et al. The tetraspanin CD63 regulates ESCRT-independent and -dependent endosomal sorting during melanogenesis. Dev Cell. 2011;21(4):708–721. doi: 10.1016/j.devcel.2011.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Savina A, Fader CM, Damiani MT, Colombo MI. Rab11 promotes docking and fusion of multivesicular bodies in a calcium-dependent manner. Traffic. 2005;6(2):131–143. doi: 10.1111/j.1600-0854.2004.00257.x. [DOI] [PubMed] [Google Scholar]
- 14.Hsu C, Morohashi Y, Yoshimura S, Manrique-Hoyos N, Jung S, Lauterbach MA, et al. Regulation of exosome secretion by Rab35 and its GTPase-activating proteins TBC1D10A-C. J Cell Biol. 2010;189(2):223–232. doi: 10.1083/jcb.200911018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hoshino D, Kirkbride KC, Costello K, Clark ES, Sinha S, Grega-Larson N, et al. Exosome secretion is enhanced by invadopodia and drives invasive behavior. Cell Rep. 2013;5(5):1159–1168. doi: 10.1016/j.celrep.2013.10.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ostrowski M, Carmo NB, Krumeich S, Fanget I, Raposo G, Savina A, et al. Rab27a and Rab27b control different steps of the exosome secretion pathway. Nat Cell Biol. 2010;12(1):19–30. doi: 10.1038/ncb2000. [DOI] [PubMed] [Google Scholar]
- 17.Bobrie A, Krumeich S, Reyal F, Recchi C, Moita LF, Seabra MC, et al. Rab27a supports exosome-dependent and -independent mechanisms that modify the tumor microenvironment and can promote tumor progression. Cancer Res. 2012;72(19):4920–4930. doi: 10.1158/0008-5472.CAN-12-0925. [DOI] [PubMed] [Google Scholar]
- 18.Sinha S, Hoshino D, Hong NH, Kirkbride KC, Grega-Larson NE, Seiki M, et al. Cortactin promotes exosome secretion by controlling branched actin dynamics. J Cell Biol. 2016;214(2):197–213. doi: 10.1083/jcb.201601025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Muralidharan-Chari V, Clancy J, Plou C, Romao M, Chavrier P, Raposo G, et al. ARF6-regulated shedding of tumor cell-derived plasma membrane microvesicles. Curr Biol. 2009;19(22):1875–1885. doi: 10.1016/j.cub.2009.09.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang Q, Lu Q. Plasma membrane-derived extracellular microvesicles mediate non-canonical intercellular NOTCH signaling. Nat Commun. 2017;8(1):709. doi: 10.1038/s41467-017-00767-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Raposo G, Stoorvogel W. Extracellular vesicles: exosomes, microvesicles, and friends. J Cell Biol. 2013;200(4):373–383. doi: 10.1083/jcb.201211138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mulcahy LA, Pink RC, Carter DR. Routes and mechanisms of extracellular vesicle uptake. J Extracell Vesicles. 2014;3. [DOI] [PMC free article] [PubMed]
- 23.Zhang L, Zhao Y, Dai Y, Cheng JN, Gong Z, Feng Y, et al. Immune landscape of colorectal Cancer tumor microenvironment from different primary tumor location. Front Immunol. 2018;9:1578. doi: 10.3389/fimmu.2018.01578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Quail DF, Joyce JA. Microenvironmental regulation of tumor progression and metastasis. Nat Med. 2013;19(11):1423–1437. doi: 10.1038/nm.3394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bebelman MP, Smit MJ, Pegtel DM, Baglio SR. Biogenesis and function of extracellular vesicles in cancer. Pharmacol Ther. 2018;188:1–11. doi: 10.1016/j.pharmthera.2018.02.013. [DOI] [PubMed] [Google Scholar]
- 26.Tovar-Camargo OA, Toden S, Goel A. Exosomal microRNA biomarkers: emerging Frontiers in colorectal and other human cancers. Expert Rev Mol Diagn. 2016;16(5):553–567. doi: 10.1586/14737159.2016.1156535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Higginbotham JN, Demory Beckler M, Gephart JD, Franklin JL, Bogatcheva G, Kremers GJ, et al. Amphiregulin exosomes increase cancer cell invasion. Curr Biol. 2011;21(9):779–786. doi: 10.1016/j.cub.2011.03.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rak J, Guha A. Extracellular vesicles--vehicles that spread cancer genes. Bioessays. 2012;34(6):489–497. doi: 10.1002/bies.201100169. [DOI] [PubMed] [Google Scholar]
- 29.Shiga K, Hara M, Nagasaki T, Sato T, Takahashi H, Takeyama H. Cancer-Associated Fibroblasts: Their Characteristics and Their Roles in Tumor Growth. Cancers (Basel) 2015;7:2443–2458. doi: 10.3390/cancers7040902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Guo W, Gao Y, Li N, Shao F, Wang C, Wang P, et al. Exosomes: new players in cancer (review) Oncol Rep. 2017;38(2):665–675. doi: 10.3892/or.2017.5714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fu H, Yang H, Zhang X, Xu W. The emerging roles of exosomes in tumor-stroma interaction. J Cancer Res Clin Oncol. 2016;142(9):1897–1907. doi: 10.1007/s00432-016-2145-0. [DOI] [PubMed] [Google Scholar]
- 32.Antonyak MA, Li B, Boroughs LK, Johnson JL, Druso JE, Bryant KL, et al. Cancer cell-derived microvesicles induce transformation by transferring tissue transglutaminase and fibronectin to recipient cells. Proc Natl Acad Sci U S A. 2011;108(12):4852–4857. doi: 10.1073/pnas.1017667108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Giusti I, Di Francesco M, D'Ascenzo S, Palmerini MG, Macchiarelli G, Carta G, et al. Ovarian cancer-derived extracellular vesicles affect normal human fibroblast behavior. Cancer Biol Ther. 2018;19(8):722–734. doi: 10.1080/15384047.2018.1451286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Webber JP, Spary LK, Sanders AJ, Chowdhury R, Jiang WG, Steadman R, et al. Differentiation of tumour-promoting stromal myofibroblasts by cancer exosomes. Oncogene. 2015;34(3):290–302. doi: 10.1038/onc.2013.560. [DOI] [PubMed] [Google Scholar]
- 35.Baglio SR, Lagerweij T, Perez-Lanzon M, Ho XD, Leveille N, Melo SA, et al. Blocking tumor-educated MSC paracrine activity halts osteosarcoma progression. Clin Cancer Res. 2017;23(14):3721–3733. doi: 10.1158/1078-0432.CCR-16-2726. [DOI] [PubMed] [Google Scholar]
- 36.Cho JA, Park H, Lim EH, Lee KW. Exosomes from breast cancer cells can convert adipose tissue-derived mesenchymal stem cells into myofibroblast-like cells. Int J Oncol. 2012;40(1):130–138. doi: 10.3892/ijo.2011.1193. [DOI] [PubMed] [Google Scholar]
- 37.Lugini L, Valtieri M, Federici C, Cecchetti S, Meschini S, Condello M, et al. Exosomes from human colorectal cancer induce a tumor-like behavior in colonic mesenchymal stromal cells. Oncotarget. 2016;7(31):50086–50098. doi: 10.18632/oncotarget.10574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Baroni S, Romero-Cordoba S, Plantamura I, Dugo M, D'Ippolito E, Cataldo A, et al. Exosome-mediated delivery of miR-9 induces cancer-associated fibroblast-like properties in human breast fibroblasts. Cell Death Dis. 2016;7(7):e2312. doi: 10.1038/cddis.2016.224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Richards KE, Zeleniak AE, Fishel ML, Wu J, Littlepage LE, Hill R. Cancer-Associated Fibroblast Exosomes Regulate Survival And Proliferation Of Pancreatic Cancer Cells. Oncogene. 2017;36(13):1770–1778. doi: 10.1038/onc.2016.353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Luga V, Zhang L, Viloria-Petit AM, Ogunjimi AA, Inanlou MR, Chiu E, et al. Exosomes mediate stromal mobilization of autocrine Wnt-PCP signaling in breast cancer cell migration. Cell. 2012;151(7):1542–1556. doi: 10.1016/j.cell.2012.11.024. [DOI] [PubMed] [Google Scholar]
- 41.Donnarumma E, Fiore D, Nappa M, Roscigno G, Adamo A, Iaboni M, et al. Cancer-associated fibroblasts release exosomal microRNAs that dictate an aggressive phenotype in breast cancer. Oncotarget. 2017;8(12):19592–19608. doi: 10.18632/oncotarget.14752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Todorova D, Simoncini S, Lacroix R, Sabatier F, Dignat-George F. Extracellular vesicles in angiogenesis. Circ Res. 2017;120(10):1658–1673. doi: 10.1161/CIRCRESAHA.117.309681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Al-Nedawi K, Meehan B, Kerbel RS, Allison AC, Rak J. Endothelial expression of autocrine VEGF upon the uptake of tumor-derived microvesicles containing oncogenic EGFR. Proc Natl Acad Sci U S A. 2009;106(10):3794–3799. doi: 10.1073/pnas.0804543106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Thompson CA, Purushothaman A, Ramani VC, Vlodavsky I, Sanderson RD. Heparanase regulates secretion, composition, and function of tumor cell-derived exosomes. J Biol Chem. 2013;288(14):10093–10099. doi: 10.1074/jbc.C112.444562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Svensson KJ, Kucharzewska P, Christianson HC, Skold S, Lofstedt T, Johansson MC, et al. Hypoxia triggers a proangiogenic pathway involving cancer cell microvesicles and PAR-2-mediated heparin-binding EGF signaling in endothelial cells. Proc Natl Acad Sci U S A. 2011;108(32):13147–13152. doi: 10.1073/pnas.1104261108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kucharzewska P, Christianson HC, Welch JE, Svensson KJ, Fredlund E, Ringner M, et al. Exosomes reflect the hypoxic status of glioma cells and mediate hypoxia-dependent activation of vascular cells during tumor development. Proc Natl Acad Sci U S A. 2013;110(18):7312–7317. doi: 10.1073/pnas.1220998110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Huang Z, Feng Y. Exosomes derived from hypoxic colorectal Cancer cells promote angiogenesis through Wnt4-induced beta-catenin signaling in endothelial cells. Oncol Res. 2017;25(5):651–661. doi: 10.3727/096504016X14752792816791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zhuang G, Wu X, Jiang Z, Kasman I, Yao J, Guan Y, et al. Tumour-secreted miR-9 promotes endothelial cell migration and angiogenesis by activating the JAK-STAT pathway. EMBO J. 2012;31(17):3513–3523. doi: 10.1038/emboj.2012.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sruthi TV, Edatt L, Raji GR, Kunhiraman H, Shankar SS, Shankar V, et al. Horizontal transfer of miR-23a from hypoxic tumor cell colonies can induce angiogenesis. J Cell Physiol. 2018;233(4):3498–3514. doi: 10.1002/jcp.26202. [DOI] [PubMed] [Google Scholar]
- 50.Kosaka N, Iguchi H, Hagiwara K, Yoshioka Y, Takeshita F, Ochiya T. Neutral sphingomyelinase 2 (nSMase2)-dependent exosomal transfer of angiogenic microRNAs regulate cancer cell metastasis. J Biol Chem. 2013;288(15):10849–10859. doi: 10.1074/jbc.M112.446831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tauriello DVF, Batlle E. Targeting the microenvironment in advanced colorectal Cancer. Trends Cancer. 2016;2(9):495–504. doi: 10.1016/j.trecan.2016.08.001. [DOI] [PubMed] [Google Scholar]
- 52.Wieckowski EU, Visus C, Szajnik M, Szczepanski MJ, Storkus WJ, Whiteside TL. Tumor-derived microvesicles promote regulatory T cell expansion and induce apoptosis in tumor-reactive activated CD8+ T lymphocytes. J Immunol. 2009;183(6):3720–3730. doi: 10.4049/jimmunol.0900970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Andreola G, Rivoltini L, Castelli C, Huber V, Perego P, Deho P, et al. Induction of lymphocyte apoptosis by tumor cell secretion of FasL-bearing microvesicles. J Exp Med. 2002;195(10):1303–1316. doi: 10.1084/jem.20011624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Abusamra AJ, Zhong Z, Zheng X, Li M, Ichim TE, Chin JL, et al. Tumor exosomes expressing Fas ligand mediate CD8+ T-cell apoptosis. Blood Cells Mol Dis. 2005;35(2):169–173. doi: 10.1016/j.bcmd.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 55.Kim JW, Wieckowski E, Taylor DD, Reichert TE, Watkins S, Whiteside TL. Fas ligand-positive membranous vesicles isolated from sera of patients with oral cancer induce apoptosis of activated T lymphocytes. Clin Cancer Res. 2005;11(3):1010–1020. [PubMed] [Google Scholar]
- 56.Huber V, Fais S, Iero M, Lugini L, Canese P, Squarcina P, et al. Human colorectal cancer cells induce T-cell death through release of proapoptotic microvesicles: role in immune escape. Gastroenterology. 2005;128(7):1796–1804. doi: 10.1053/j.gastro.2005.03.045. [DOI] [PubMed] [Google Scholar]
- 57.Klibi J, Niki T, Riedel A, Pioche-Durieu C, Souquere S, Rubinstein E, et al. Blood diffusion and Th1-suppressive effects of galectin-9-containing exosomes released by Epstein-Barr virus-infected nasopharyngeal carcinoma cells. Blood. 2009;113(9):1957–1966. doi: 10.1182/blood-2008-02-142596. [DOI] [PubMed] [Google Scholar]
- 58.Maybruck BT, Pfannenstiel LW, Diaz-Montero M, Gastman BR. Tumor-derived exosomes induce CD8(+) T cell suppressors. J Immunother Cancer. 2017;5(1):65. doi: 10.1186/s40425-017-0269-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Clayton A, Mitchell JP, Court J, Mason MD, Tabi Z. Human tumor-derived exosomes selectively impair lymphocyte responses to interleukin-2. Cancer Res. 2007;67(15):7458–7466. doi: 10.1158/0008-5472.CAN-06-3456. [DOI] [PubMed] [Google Scholar]
- 60.Yamada N, Kuranaga Y, Kumazaki M, Shinohara H, Taniguchi K, Akao Y. Colorectal cancer cell-derived extracellular vesicles induce phenotypic alteration of T cells into tumor-growth supporting cells with transforming growth factor-beta1-mediated suppression. Oncotarget. 2016;7(19):27033–27043. doi: 10.18632/oncotarget.7041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Szczepanski MJ, Szajnik M, Welsh A, Whiteside TL, Boyiadzis M. Blast-derived microvesicles in sera from patients with acute myeloid leukemia suppress natural killer cell function via membrane-associated transforming growth factor-beta1. Haematologica. 2011;96(9):1302–1309. doi: 10.3324/haematol.2010.039743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Valenti R, Huber V, Filipazzi P, Pilla L, Sovena G, Villa A, et al. Human tumor-released microvesicles promote the differentiation of myeloid cells with transforming growth factor-beta-mediated suppressive activity on T lymphocytes. Cancer Res. 2006;66(18):9290–9298. doi: 10.1158/0008-5472.CAN-06-1819. [DOI] [PubMed] [Google Scholar]
- 63.Xiang X, Poliakov A, Liu C, Liu Y, Deng ZB, Wang J, et al. Induction of myeloid-derived suppressor cells by tumor exosomes. Int J Cancer. 2009;124(11):2621–2633. doi: 10.1002/ijc.24249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Chalmin F, Ladoire S, Mignot G, Vincent J, Bruchard M, Remy-Martin JP, et al. Membrane-associated Hsp72 from tumor-derived exosomes mediates STAT3-dependent immunosuppressive function of mouse and human myeloid-derived suppressor cells. J Clin Invest. 2010;120:457–471. doi: 10.1172/JCI40483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Diao J, Yang X, Song X, Chen S, He Y, Wang Q, et al. Exosomal Hsp70 mediates immunosuppressive activity of the myeloid-derived suppressor cells via phosphorylation of Stat3. Med Oncol. 2015;32(2):453. doi: 10.1007/s12032-014-0453-2. [DOI] [PubMed] [Google Scholar]
- 66.Shen Y, Guo D, Weng L, Wang S, Ma Z, Yang Y, et al. Tumor-derived exosomes educate dendritic cells to promote tumor metastasis via HSP72/HSP105-TLR2/TLR4 pathway. Oncoimmunology. 2017;6(12):e1362527. doi: 10.1080/2162402X.2017.1362527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ashiru O, Boutet P, Fernandez-Messina L, Aguera-Gonzalez S, Skepper JN, Vales-Gomez M, et al. Natural killer cell cytotoxicity is suppressed by exposure to the human NKG2D ligand MICA*008 that is shed by tumor cells in exosomes. Cancer Res. 2010;70(2):481–489. doi: 10.1158/0008-5472.CAN-09-1688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Yin Y, Cai X, Chen X, Liang H, Zhang Y, Li J, et al. Tumor-secreted miR-214 induces regulatory T cells: a major link between immune evasion and tumor growth. Cell Res. 2014;24:1164–1180. doi: 10.1038/cr.2014.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Mu W, Rana S, Zoller M. Host matrix modulation by tumor exosomes promotes motility and invasiveness. Neoplasia. 2013;15(8):875–887. doi: 10.1593/neo.13786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Fong MY, Zhou W, Liu L, Alontaga AY, Chandra M, Ashby J, et al. Breast-cancer-secreted miR-122 reprograms glucose metabolism in premetastatic niche to promote metastasis. Nat Cell Biol. 2015;17(2):183–194. doi: 10.1038/ncb3094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hood JL, Pan H, Lanza GM, Wickline SA. Consortium for translational research in advanced I, nanomedicine. Paracrine induction of endothelium by tumor exosomes. Lab Investig. 2009;89(11):1317–1328. doi: 10.1038/labinvest.2009.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sedgwick AE, Clancy JW, Olivia Balmert M, D'Souza-Schorey C. Extracellular microvesicles and invadopodia mediate non-overlapping modes of tumor cell invasion. Sci Rep. 2015;5:14748. doi: 10.1038/srep14748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Jacob A, Linklater E, Bayless BA, Lyons T, Prekeris R. The role and regulation of Rab40b-Tks5 complex during invadopodia formation and cancer cell invasion. J Cell Sci. 2016;129(23):4341–4353. doi: 10.1242/jcs.193904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Sung BH, Ketova T, Hoshino D, Zijlstra A, Weaver AM. Directional cell movement through tissues is controlled by exosome secretion. Nat Commun. 2015;6:7164. doi: 10.1038/ncomms8164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sung BH, Weaver AM. Exosome secretion promotes chemotaxis of cancer cells. Cell Adhes Migr. 2017;11(2):187–195. doi: 10.1080/19336918.2016.1273307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Hon KW, Abu N, Ab Mutalib NS, Jamal R. Exosomes as potential biomarkers and targeted therapy in colorectal Cancer: a mini-review. Front Pharmacol. 2017;8:583. doi: 10.3389/fphar.2017.00583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Peinado H, Aleckovic M, Lavotshkin S, Matei I, Costa-Silva B, Moreno-Bueno G, et al. Melanoma exosomes educate bone marrow progenitor cells toward a pro-metastatic phenotype through MET. Nat Med. 2012;18(6):883–891. doi: 10.1038/nm.2753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Treps L, Perret R, Edmond S, Ricard D, Gavard J. Glioblastoma stem-like cells secrete the pro-angiogenic VEGF-A factor in extracellular vesicles. J Extracell Vesicles. 2017;6(1):1359479. doi: 10.1080/20013078.2017.1359479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Hsu YL, Hung JY, Chang WA, Lin YS, Pan YC, Tsai PH, et al. Hypoxic lung cancer-secreted exosomal miR-23a increased angiogenesis and vascular permeability by targeting prolyl hydroxylase and tight junction protein ZO-1. Oncogene. 2017;36(34):4929–4942. doi: 10.1038/onc.2017.105. [DOI] [PubMed] [Google Scholar]
- 80.Zhou W, Fong MY, Min Y, Somlo G, Liu L, Palomares MR, et al. Cancer-secreted miR-105 destroys vascular endothelial barriers to promote metastasis. Cancer Cell. 2014;25(4):501–515. doi: 10.1016/j.ccr.2014.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Shao Y, Chen T, Zheng X, Yang S, Xu K, Chen X, et al. Colorectal Cancer-derived Small Extracellular Vesicles Establish an Inflammatory Pre-metastatic Niche in Liver Metastasis. Carcinogenesis. 2018;39(11):1368-79. [DOI] [PubMed]
- 82.Hood JL, San RS, Wickline SA. Exosomes released by melanoma cells prepare sentinel lymph nodes for tumor metastasis. Cancer Res. 2011;71(11):3792–3801. doi: 10.1158/0008-5472.CAN-10-4455. [DOI] [PubMed] [Google Scholar]
- 83.Costa-Silva B, Aiello NM, Ocean AJ, Singh S, Zhang H, Thakur BK, et al. Pancreatic cancer exosomes initiate pre-metastatic niche formation in the liver. Nat Cell Biol. 2015;17(6):816–826. doi: 10.1038/ncb3169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Hoshino A, Costa-Silva B, Shen TL, Rodrigues G, Hashimoto A, Mark MT, et al. Tumour exosome integrins determine organotropic metastasis. Nature. 2015;527(7578):329–335. doi: 10.1038/nature15756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Aung T, Chapuy B, Vogel D, Wenzel D, Oppermann M, Lahmann M, et al. Exosomal evasion of humoral immunotherapy in aggressive B-cell lymphoma modulated by ATP-binding cassette transporter A3. Proc Natl Acad Sci U S A. 2011;108(37):15336–15341. doi: 10.1073/pnas.1102855108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ciravolo V, Huber V, Ghedini GC, Venturelli E, Bianchi F, Campiglio M, et al. Potential role of HER2-overexpressing exosomes in countering trastuzumab-based therapy. J Cell Physiol. 2012;227(2):658–667. doi: 10.1002/jcp.22773. [DOI] [PubMed] [Google Scholar]
- 87.Chen G, Huang AC, Zhang W, Zhang G, Wu M, Xu W, et al. Exosomal PD-L1 contributes to immunosuppression and is associated with anti-PD-1 response. Nature. 2018;560(7718):382–386. doi: 10.1038/s41586-018-0392-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Lubin JA, Zhang RR, Kuo JS. Extracellular vesicles containing PD-L1 contribute to immune evasion in glioblastoma. Neurosurgery. 2018;83(3):E98–e100. doi: 10.1093/neuros/nyy295. [DOI] [PubMed] [Google Scholar]
- 89.Yu M, Tannock IF. Targeting tumor architecture to favor drug penetration: a new weapon to combat chemoresistance in pancreatic cancer? Cancer Cell. 2012;21(3):327–329. doi: 10.1016/j.ccr.2012.03.002. [DOI] [PubMed] [Google Scholar]
- 90.Robey RW, Pluchino KM, Hall MD, Fojo AT, Bates SE, Gottesman MM. Revisiting the role of ABC transporters in multidrug-resistant cancer. Nat Rev Cancer. 2018;18(7):452–464. doi: 10.1038/s41568-018-0005-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Shedden K, Xie XT, Chandaroy P, Chang YT, Rosania GR. Expulsion of small molecules in vesicles shed by cancer cells: association with gene expression and chemosensitivity profiles. Cancer Res. 2003;63(15):4331–4337. [PubMed] [Google Scholar]
- 92.Federici C, Petrucci F, Caimi S, Cesolini A, Logozzi M, Borghi M, et al. Exosome release and low pH belong to a framework of resistance of human melanoma cells to cisplatin. PLoS One. 2014;9(2):e88193. doi: 10.1371/journal.pone.0088193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Safaei R, Larson BJ, Cheng TC, Gibson MA, Otani S, Naerdemann W, et al. Abnormal lysosomal trafficking and enhanced exosomal export of cisplatin in drug-resistant human ovarian carcinoma cells. Mol Cancer Ther. 2005;4(10):1595–1604. doi: 10.1158/1535-7163.MCT-05-0102. [DOI] [PubMed] [Google Scholar]
- 94.Koch R, Aung T, Vogel D, Chapuy B, Wenzel D, Becker S, et al. Nuclear trapping through inhibition of Exosomal export by indomethacin increases cytostatic efficacy of doxorubicin and Pixantrone. Clin Cancer Res. 2016;22(2):395–404. doi: 10.1158/1078-0432.CCR-15-0577. [DOI] [PubMed] [Google Scholar]
- 95.Ifergan I, Scheffer GL, Assaraf YG. Novel extracellular vesicles mediate an ABCG2-dependent anticancer drug sequestration and resistance. Cancer Res. 2005;65(23):10952–10958. doi: 10.1158/0008-5472.CAN-05-2021. [DOI] [PubMed] [Google Scholar]
- 96.Chapuy B, Koch R, Radunski U, Corsham S, Cheong N, Inagaki N, et al. Intracellular ABC transporter A3 confers multidrug resistance in leukemia cells by lysosomal drug sequestration. Leukemia. 2008;22(8):1576–1586. doi: 10.1038/leu.2008.103. [DOI] [PubMed] [Google Scholar]
- 97.Corcoran C, Rani S, O'Brien K, O'Neill A, Prencipe M, Sheikh R, et al. Docetaxel-resistance in prostate cancer: evaluating associated phenotypic changes and potential for resistance transfer via exosomes. PLoS One. 2012;7(12):e50999. doi: 10.1371/journal.pone.0050999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Zhang FF, Zhu YF, Zhao QN, Yang DT, Dong YP, Jiang L, et al. Microvesicles mediate transfer of P-glycoprotein to paclitaxel-sensitive A2780 human ovarian cancer cells, conferring paclitaxel-resistance. Eur J Pharmacol. 2014;738:83–90. doi: 10.1016/j.ejphar.2014.05.026. [DOI] [PubMed] [Google Scholar]
- 99.Bebawy M, Combes V, Lee E, Jaiswal R, Gong J, Bonhoure A, et al. Membrane microparticles mediate transfer of P-glycoprotein to drug sensitive cancer cells. Leukemia. 2009;23(9):1643–1649. doi: 10.1038/leu.2009.76. [DOI] [PubMed] [Google Scholar]
- 100.Torreggiani E, Roncuzzi L, Perut F, Zini N, Baldini N. Multimodal transfer of MDR by exosomes in human osteosarcoma. Int J Oncol. 2016;49(1):189–196. doi: 10.3892/ijo.2016.3509. [DOI] [PubMed] [Google Scholar]
- 101.Lu JF, Luk F, Gong J, Jaiswal R, Grau GE, Bebawy M. Microparticles mediate MRP1 intercellular transfer and the re-templating of intrinsic resistance pathways. Pharmacol Res. 2013;76:77–83. doi: 10.1016/j.phrs.2013.07.009. [DOI] [PubMed] [Google Scholar]
- 102.Bhattacharya S, Pal K, Sharma AK, Dutta SK, Lau JS, Yan IK, et al. GAIP Interacting Protein C-Terminus Regulates Autophagy and Exosome Biogenesis of Pancreatic Cancer through Metabolic Pathways. PLoS One. 2014;9(12):e114409 [DOI] [PMC free article] [PubMed]
- 103.Qu Z, Wu J, Luo D, Jiang C, Ding Y. Exosomes derived from HCC cells induce sorafenib resistance in hepatocellular carcinoma both in vivo and in vitro. J Exp Clin Cancer Res. 2016;35(1):159. doi: 10.1186/s13046-016-0430-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Vella LJ, Behren A, Coleman B, Greening DW, Hill AF, Cebon J. Intercellular resistance to BRAF inhibition can be mediated by extracellular vesicle-associated PDGFRbeta. Neoplasia. 2017;19(11):932–940. doi: 10.1016/j.neo.2017.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Ozawa PMM, Alkhilaiwi F, Cavalli IJ, Malheiros D, de Souza Fonseca Ribeiro EM, Cavalli LR. Extracellular vesicles from triple-negative breast cancer cells promote proliferation and drug resistance in non-tumorigenic breast cells. Breast Cancer Res Treat. 2018;172(3):713–723. doi: 10.1007/s10549-018-4925-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Yoshimura A, Muto G. TGF-beta function in immune suppression. Curr Top Microbiol Immunol. 2011;350:127–147. doi: 10.1007/82_2010_87. [DOI] [PubMed] [Google Scholar]
- 107.Martinez VG, O'Neill S, Salimu J, Breslin S, Clayton A, Crown J, et al. Resistance to HER2-targeted anti-cancer drugs is associated with immune evasion in cancer cells and their derived extracellular vesicles. Oncoimmunology. 2017;6(12):e1362530. [DOI] [PMC free article] [PubMed]
- 108.Khan S, Aspe JR, Asumen MG, Almaguel F, Odumosu O, Acevedo-Martinez S, et al. Extracellular, cell-permeable survivin inhibits apoptosis while promoting proliferative and metastatic potential. Br J Cancer. 2009;100(7):1073–1086. doi: 10.1038/sj.bjc.6604978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Khan S, Jutzy JMS, Aspe JR, McGregor DW, Neidigh JW, Wall NR. Survivin is released from cancer cells via exosomes. Apoptosis. 2011;16(1):1–12. doi: 10.1007/s10495-010-0534-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Khan S, Jutzy JM, Valenzuela MM, Turay D, Aspe JR, Ashok A, et al. Plasma-derived exosomal survivin, a plausible biomarker for early detection of prostate cancer. PLoS One. 2012;7(10):e46737. doi: 10.1371/journal.pone.0046737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Martinez-Garcia D, Manero-Ruperez N, Quesada R, Korrodi-Gregorio L, Soto-Cerrato V. Therapeutic strategies involving survivin inhibition in cancer. Med Res Rev. 2018. 10.1002/med.21547. [DOI] [PubMed]
- 112.Kreger BT, Johansen ER, Cerione RA, Antonyak MA. The Enrichment of Survivin in Exosomes from Breast Cancer Cells Treated with Paclitaxel Promotes Cell Survival and Chemoresistance. Cancers (Basel). 2016;8(12). [DOI] [PMC free article] [PubMed]
- 113.Akao Y, Khoo F, Kumazaki M, Shinohara H, Miki K, Yamada N. Extracellular disposal of tumor-suppressor miRs-145 and -34a via microvesicles and 5-FU resistance of human colon cancer cells. Int J Mol Sci. 2014;15(1):1392–1401. doi: 10.3390/ijms15011392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Bouvy C, Wannez A, Laloy J, Chatelain C, Dogne JM. Transfer of multidrug resistance among acute myeloid leukemia cells via extracellular vesicles and their microRNA cargo. Leuk Res. 2017;62:70–76. doi: 10.1016/j.leukres.2017.09.014. [DOI] [PubMed] [Google Scholar]
- 115.Binenbaum Y, Fridman E, Yaari Z, Milman N, Schroeder A, Ben David G, et al. Transfer of miRNA in macrophage-derived exosomes induces drug resistance in pancreatic adenocarcinoma. Cancer Res. 2018;78(18):5287–5299. doi: 10.1158/0008-5472.CAN-18-0124. [DOI] [PubMed] [Google Scholar]
- 116.Hu Y, Yan C, Mu L, Huang K, Li X, Tao D, et al. Fibroblast-Derived Exosomes Contribute to Chemoresistance through Priming Cancer Stem Cells in Colorectal Cancer. PLoS One. 2015;10(5):e0125625. [DOI] [PMC free article] [PubMed]
- 117.Au Yeung CL, Co NN, Tsuruga T, Yeung TL, Kwan SY, Leung CS, et al. Exosomal transfer of stroma-derived miR21 confers paclitaxel resistance in ovarian cancer cells through targeting APAF1. Nat Commun. 2016;7:11150. doi: 10.1038/ncomms11150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Zheng P, Chen L, Yuan X, Luo Q, Liu Y, Xie G, et al. Exosomal transfer of tumor-associated macrophage-derived miR-21 confers cisplatin resistance in gastric cancer cells. J Exp Clin Cancer Res. 2017;36(1):53. doi: 10.1186/s13046-017-0528-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Boelens MC, Wu TJ, Nabet BY, Xu B, Qiu Y, Yoon T, et al. Exosome transfer from stromal to breast cancer cells regulates therapy resistance pathways. Cell. 2014;159(3):499–513. doi: 10.1016/j.cell.2014.09.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Ji R, Zhang B, Zhang X, Xue J, Yuan X, Yan Y, et al. Exosomes derived from human mesenchymal stem cells confer drug resistance in gastric cancer. Cell Cycle. 2015;14(15):2473–2483. doi: 10.1080/15384101.2015.1005530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Petrova V, Annicchiarico-Petruzzelli M, Melino G, Amelio I. The hypoxic tumour microenvironment. Oncogenesis. 2018;7(1):10. [DOI] [PMC free article] [PubMed]
- 122.Dorayappan KDP, Wanner R, Wallbillich JJ, Saini U, Zingarelli R, Suarez AA, et al. Hypoxia-induced exosomes contribute to a more aggressive and chemoresistant ovarian cancer phenotype: a novel mechanism linking STAT3/Rab proteins. Oncogene. 2018;37(28):3806–3821. doi: 10.1038/s41388-018-0189-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Bandari SK, Purushothaman A, Ramani VC, Brinkley GJ, Chandrashekar DS, Varambally S, et al. Chemotherapy induces secretion of exosomes loaded with heparanase that degrades extracellular matrix and impacts tumor and host cell behavior. Matrix Biol. 2018;65:104–118. doi: 10.1016/j.matbio.2017.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Lv LH, Wan YL, Lin Y, Zhang W, Yang M, Li GL, et al. Anticancer drugs cause release of exosomes with heat shock proteins from human hepatocellular carcinoma cells that elicit effective natural killer cell antitumor responses in vitro. J Biol Chem. 2012;287(19):15874–15885. doi: 10.1074/jbc.M112.340588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Roseblade A, Luk F, Ung A, Bebawy M. Targeting microparticle biogenesis: a novel approach to the circumvention of cancer multidrug resistance. Curr Cancer Drug Targets. 2015;15(3):205–214. doi: 10.2174/1568009615666150225121508. [DOI] [PubMed] [Google Scholar]
- 126.Jorfi S, Ansa-Addo EA, Kholia S, Stratton D, Valley S, Lange S, et al. Inhibition of microvesiculation sensitizes prostate cancer cells to chemotherapy and reduces docetaxel dose required to limit tumor growth in vivo. Sci Rep. 2015;5:13006. doi: 10.1038/srep13006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Muralidharan-Chari V, Kohan HG, Asimakopoulos AG, Sudha T, Sell S, Kannan K, et al. Microvesicle removal of anticancer drugs contributes to drug resistance in human pancreatic cancer cells. Oncotarget. 2016;7(31):50365–50379. doi: 10.18632/oncotarget.10395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Kholia S, Jorfi S, Thompson PR, Causey CP, Nicholas AP, Inal JM, et al. A novel role for peptidylarginine deiminases in microvesicle release reveals therapeutic potential of PAD inhibition in sensitizing prostate cancer cells to chemotherapy. J Extracell Vesicles. 2015;4:26192. doi: 10.3402/jev.v4.26192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Kosgodage US, Trindade RP, Thompson PR, Inal JM, Lange S. Chloramidine/Bisindolylmaleimide-I-Mediated Inhibition of Exosome and Microvesicle Release and Enhanced Efficacy of Cancer Chemotherapy. Int J Mol Sci. 2017;18(5). [DOI] [PMC free article] [PubMed]
- 130.Kosgodage US, Mould R, Henley AB, Nunn AV, Guy GW, Thomas EL, et al. Cannabidiol (CBD) is a novel inhibitor for exosome and microvesicle (EMV) release in Cancer. Front Pharmacol. 2018;9:889. doi: 10.3389/fphar.2018.00889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Tullis RH, Duffin RP, Handley HH, Sodhi P, Menon J, Joyce JA, et al. Reduction of hepatitis C virus using lectin affinity plasmapheresis in dialysis patients. Blood Purif. 2009;27(1):64–69. doi: 10.1159/000167011. [DOI] [PubMed] [Google Scholar]
- 132.Marleau AM, Chen CS, Joyce JA, Tullis RH. Exosome removal as a therapeutic adjuvant in cancer. J Transl Med. 2012;10:134. doi: 10.1186/1479-5876-10-134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Qin X, Yu S, Zhou L, Shi M, Hu Y, Xu X, et al. Cisplatin-resistant lung cancer cell-derived exosomes increase cisplatin resistance of recipient cells in exosomal miR-100-5p-dependent manner. Int J Nanomedicine. 2017;12:3721–3733. doi: 10.2147/IJN.S131516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Wei F, Ma C, Zhou T, Dong X, Luo Q, Geng L, et al. Exosomes derived from gemcitabine-resistant cells transfer malignant phenotypic traits via delivery of miRNA-222-3p. Mol Cancer. 2017;16(1):132. doi: 10.1186/s12943-017-0694-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Wu H, Zhou J, Mei S, Wu D, Mu Z, Chen B, et al. Circulating exosomal microRNA-96 promotes cell proliferation, migration and drug resistance by targeting LMO7. J Cell Mol Med. 2017;21:1228–1236. doi: 10.1111/jcmm.13056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Yuwen DL, Sheng BB, Liu J, Wenyu W, Shu YQ. MiR-146a-5p level in serum exosomes predicts therapeutic effect of cisplatin in non-small cell lung cancer. Eur Rev Med Pharmacol Sci. 2017;21(11):2650–2658. [PubMed] [Google Scholar]
- 137.Chen WX, Cai YQ, Lv MM, Chen L, Zhong SL, Ma TF, et al. Exosomes from docetaxel-resistant breast cancer cells alter chemosensitivity by delivering microRNAs. Tumour Biol. 2014;35(10):9649–9659. doi: 10.1007/s13277-014-2242-0. [DOI] [PubMed] [Google Scholar]
- 138.Wei Y, Lai X, Yu S, Chen S, Ma Y, Zhang Y, et al. Exosomal miR-221/222 enhances tamoxifen resistance in recipient ER-positive breast cancer cells. Breast Cancer Res Treat. 2014;147(2):423–431. doi: 10.1007/s10549-014-3037-0. [DOI] [PubMed] [Google Scholar]
- 139.O'Brien K, Lowry MC, Corcoran C, Martinez VG, Daly M, Rani S, et al. miR-134 in extracellular vesicles reduces triple-negative breast cancer aggression and increases drug sensitivity. Oncotarget. 2015;6(32):32774–32789. doi: 10.18632/oncotarget.5192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Santos JC, Lima NDS, Sarian LO, Matheu A, Ribeiro ML, Derchain SFM. Exosome-mediated breast cancer chemoresistance via miR-155 transfer. Sci Rep. 2018;8(1):829. doi: 10.1038/s41598-018-19339-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Li XJ, Ren ZJ, Tang JH, Yu Q. Exosomal MicroRNA MiR-1246 promotes cell proliferation, invasion and drug resistance by targeting CCNG2 in breast Cancer. Cell Physiol Biochem. 2017;44(5):1741–1748. doi: 10.1159/000485780. [DOI] [PubMed] [Google Scholar]
- 142.Yu DD, Wu Y, Zhang XH, Lv MM, Chen WX, Chen X, et al. Exosomes from adriamycin-resistant breast cancer cells transmit drug resistance partly by delivering miR-222. Tumour Biol. 2016;37(3):3227–3235. doi: 10.1007/s13277-015-4161-0. [DOI] [PubMed] [Google Scholar]
- 143.Liu T, Chen G, Sun D, Lei M, Li Y, Zhou C, et al. Exosomes containing miR-21 transfer the characteristic of cisplatin resistance by targeting PTEN and PDCD4 in oral squamous cell carcinoma. Acta Biochim Biophys Sin Shanghai. 2017;49(9):808–816. doi: 10.1093/abbs/gmx078. [DOI] [PubMed] [Google Scholar]
- 144.Lunavat TR, Cheng L, Einarsdottir BO, Olofsson Bagge R, Veppil Muralidharan S, Sharples RA, et al. BRAF(V600) inhibition alters the microRNA cargo in the vesicular secretome of malignant melanoma cells. Proc Natl Acad Sci U S A. 2017;114(29):E5930–E59e9. doi: 10.1073/pnas.1705206114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Yang JK, Yang JP, Tong J, Jing SY, Fan B, Wang F, et al. Exosomal miR-221 targets DNM3 to induce tumor progression and temozolomide resistance in glioma. J Neuro-Oncol. 2017;131(2):255–265. doi: 10.1007/s11060-016-2308-5. [DOI] [PubMed] [Google Scholar]
- 146.Corcoran C, Rani S, O'Driscoll L. miR-34a is an intracellular and exosomal predictive biomarker for response to docetaxel with clinical relevance to prostate cancer progression. Prostate. 2014;74(13):1320–1334. doi: 10.1002/pros.22848. [DOI] [PubMed] [Google Scholar]
- 147.Mikamori M, Yamada D, Eguchi H, Hasegawa S, Kishimoto T, Tomimaru Y, et al. MicroRNA-155 controls exosome synthesis and promotes gemcitabine resistance in pancreatic ductal adenocarcinoma. Sci Rep. 2017;7:42339. doi: 10.1038/srep42339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Min QH, Wang XZ, Zhang J, Chen QG, Li SQ, Liu XQ, et al. Exosomes derived from imatinib-resistant chronic myeloid leukemia cells mediate a horizontal transfer of drug-resistant trait by delivering miR-365. Exp Cell Res. 2018;362(2):386–393. doi: 10.1016/j.yexcr.2017.12.001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable, please refer to the original reference.