Abstract
Prone ventilation is used to manage patients with refractory hypoxia in the critical care unit. Complex chest trauma and chest drains have been a considered relative contraindication to prone ventilation. To the best of our knowledge, it is hitherto unreported in patients having traumatic floating sternum and acute respiratory distress. We present a brief case report of a patient with floating sternum (complete disruption of sternum) managed successfully by prone position ventilation.
Keywords: mechanical ventilation, trauma, adult intensive care
Background
Prone ventilation is controversial in sternotomy and in patients after cardiac surgeries. Information about prone positioning of the patients with complex chest traumas is sparse. Through this write up we wish to demonstrate that a patient with complete disruption of sternum, chest drains and haemodynamic instability can be managed in the prone ventilation safely.
Case presentation
A 45-year-old man was admitted with respiratory distress to the emergency room after a high impact road traffic accident. Glassgow Coma Scale (GCS) on arrival was 15, without evidence of head injury. There was paradoxical breathing with anterior flail and emphysema over chest wall. Invasive mechanical ventilation was initiated and chest drains inserted on both sides for haemothorax evidenced on point of care ultrasound. CT thorax demonstrated pulmonary contusion with major disruption of sternocostal joints (figure 1). Thoracic epidural analgesia along with systemic analgesics was initiated for pain control. The patient was on epidural bupivacaine and fentanyl infusion for analgesia which was monitored with Visual Analogue Scale (VAS) score <4. The patient was sedated with Inj. midazolam infusion with Richmond Agitation and Sedation Scale (RASS) score monitoring. Patient had normal urine output (≥1 mL/kg/hour) throughout the first 3 days and there was no episode of hypotension.
Figure 1.
Reconstructed chest CT.
By the third day of ICU stay, the patient developed severe hypoxia, hypotension and became irritable. He was sedated and paralysed. The acidosis, refractory hypoxia and acute respiratory distress did not improve in spite of optimal lung protective ventilation (figure 2, tables 1 and 2). The cumulative fluid balance was 1.6 L (excluding insensible loss). The point of care ultrasound of chest was used to assess cardiac function, lung B lines, fluid responsiveness and vena caval distensibility, suggested a non-compromised heart without evidence of fluid overload. Hypotension was managed with intravenous fluids and infusion of noradrenalin initiated at the rate 0.05–1 mcg/kg/hour and titrated to affect.
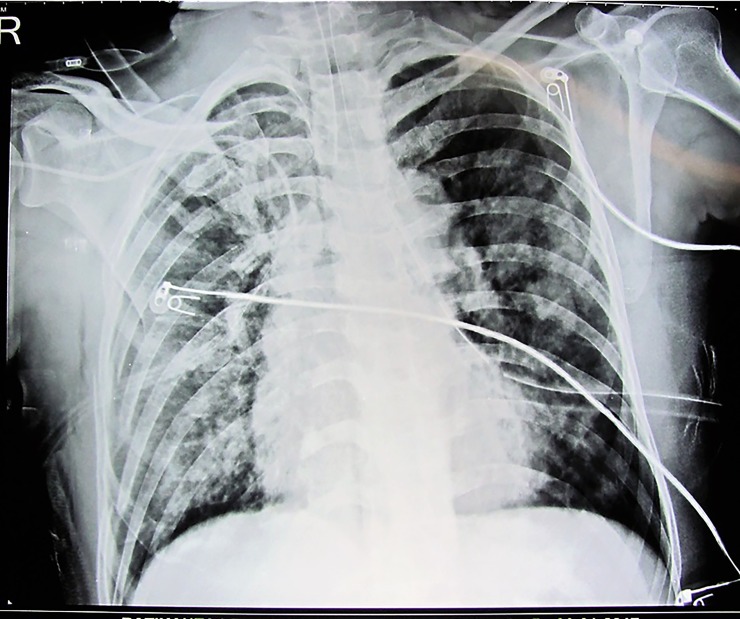
Figure 2.
CXR with features of acute respiratory distress syndrome (ARDS).
Table 1.
Ventilator modes at different time
| Time | Mode | TV set | TV delivered | PEEP | Plateau | PIP | FiO2 | RR/min | P/F | SpO2 |
| T (−2) | VCV | 300 | 240–280 | 12–14 | 34–37 | 45–50 | 100 | 24 | 54 | 72% |
| T (−1) | VCV | 320 | 300–320 | 14–20 | 32–34 | 45 | 100 | 24 | 55 | 71%–75% |
| T0 | VCV | 350 | 300–350 | 20 | 32–34 | 43 | 100 | 24 | 71%–75% | |
| T4hr | VCV | 360 | 350–400 | 18 | 30–34 | 40 | 60 | 22 | 131 | 92% |
| T8hr | VCV | 360 | 360–400 | 16 | 28–30 | 35 | 60 | 22 | 99% | |
| T16 hr | VCV | 400 | 400 | 16 | 25–30 | 35 | 55 | 20 | 257 | 99% |
(T (−2) before sedation and paralysis, T (−1) after 4 hours of sedation and paralysis. T0- immediately after proning, T4h, T8hr, T16hr- corresponding hour after proning). FiO2, fraction of inspired oxygen; PEEP, positive end expiratory pressure; PIP, peak inspiratory pressure; P/F, PaO2/Fio2; RR, respiratory rate; SpO2-peripheral oxygen saturation; TV, tidal volume; VCV, volume control ventilation.
Table 2.
Corresponding arterial blood gas (ABG) at different time interval
| Time | pH | PaCo2 | PaO2 | HCO3 | Lactate | MAP | FIO2 | P/F |
| T (−2) | 6.83 | 146.7 | 54.4 | 9.6 | 1.9 | 55–65 | 100 | 54 |
| T (−1) | 7.03 | 110 | 55 | 10.1 | 1.8 | 65 | 100 | 55 |
| T4hr | 7.08 | 80.1 | 78.8 | 20 | 2.4 | 65–70 | 60 | 131 |
| T16hr | 7.27 | 47.7 | 141.6 | 22.4 | 1.9 | 70 | 55 | 257 |
(T (−2) before sedation and paralysis, T (−1) after 4 hours of sedation and paralysis. T0- immediately after proning, T4hr, T16hr- corresponding hour after proning).
Prone ventilation was initiated as the last resort (extracorporeal membrane oxygenation [ECMO] facility is not available at our centre).
There are no guidelines for proning patients with chest trauma. The methodology followed was as done in the PROSEVA trial,1 which is a standard protocol on our unit. (https://www.youtube.com/watch?v=E_6jT9R7WJs.) Infusion of the noradrenalin was continued targeting the mean arterial pressure of 65 mm Hg and above. The patient showed gradual improvement in oxygenation and haemodynamic with prone ventilation for 16 hours (tables 1 and 2). The noradrenalin infusion was tapered off by 10 hours. There were no position-related complications.
Investigations
Chest CT scan, chest X-ray, ABG.
Differential diagnosis
Ventilator-associated pneumonia. However, lab parameters and culture reports did not support this diagnosis.
Outcome and follow-up
The patient maintained haemodynamic and oxygen saturation (SpO2) after the single episode of proning with high PEEP and FiO2. Over the next 2 days though the P/F ratio stays in between 220 and 300. He maintained good saturation in supine position with PEEP 6–10 and FiO2 between 40% and 60%. Over the next week he underwent tracheostomy for difficult weaning due to an unstable sternum. He was discharged at 6 weeks, completely recovered.
Discussion
Improvement in oxygenation in the prone position is thought to result from a reduction in intrapulmonary ventilation perfusion mismatch, ventilator induced lung injury and better drainage of secretions.2 Complex chest trauma has been considered a relative contraindication to prone positioning. A few cases of flail chest have shown benefit from prone positioning.3 4 It is hitherto unreported in patients with a floating sternum where the haemodynamic effects of the sternum on the heart may be an added concern. In our case, we found improvement in haemodynamic and oxygenation possibly attributed to the additional sternal splinting.
Patient’s perspective.
Thank God for saving my life, I do not remember much of what my family and doctors tell me. But I am happy to be alive!
Learning points.
Chest trauma with a floating sternum is not a contraindication for prone ventilation in the event of refractory hypoxaemia.
It may improve haemodynamic parameters, possibly due to sternal splinting.
Acknowledgments
All the Staff of Department of Anaesthesiology and SICU, AIIMS, Bhubaneswar, Odisha.
Footnotes
Contributors: Planning: AKS, ST. Conduct: AKS, ST, SKS. Reporting: AKS. Conception and design: AKS, ST, SKS. Acquisition of data: SKS. Analysis and interpretation of data: AKS, ST. Manuscript: AKS. Review of Manuscript-ST.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Obtained.
References
- 1.Guérin C, Reignier J, Richard JC, et al. . Prone positioning in severe acute respiratory distress syndrome. N Engl J Med 2013;368:2159–68. 10.1056/NEJMoa1214103 [DOI] [PubMed] [Google Scholar]
- 2.Gattinoni L, Taccone P, Carlesso E, et al. . Prone position in acute respiratory distress syndrome. Rationale, indications, and limits. Am J Respir Crit Care Med 2013;188:1286–93. 10.1164/rccm.201308-1532CI [DOI] [PubMed] [Google Scholar]
- 3.Ashton-Cleary DT, Duffy MR. Prone ventilation for refractory hypoxaemia in a patient with severe chest wall disruption and traumatic brain injury. Br J Anaesth 2011;107:1009–10. 10.1093/bja/aer374 [DOI] [PubMed] [Google Scholar]
- 4.Kenn S, Weber-Carstens S, Weizsaecker K, et al. . Prone positioning for ARDS following blunt chest trauma in late pregnancy. Int J Obstet Anesth 2009;18:268–71. 10.1016/j.ijoa.2009.02.003 [DOI] [PubMed] [Google Scholar]