Abstract
Background
Self-stigma, also known as internalised stigma, is a global public health threat because it keeps people from accessing HIV and other health services. By hampering HIV testing, treatment and prevention, self-stigma can compromise the sustainability of health interventions and have serious epidemiological consequences. This review synthesised existing evidence of interventions aiming to reduce self-stigma experienced by people living with HIV and key populations affected by HIV in low-income and middle-income countries.
Methods
Studies were identified through bibliographic databases, grey literature sites, study registries, back referencing and contacts with researchers, and synthesised following Cochrane guidelines.
Results
Of 5880 potentially relevant titles, 20 studies were included in the review. Represented in these studies were 9536 people (65% women) from Ethiopia, India, Kenya, Lesotho, Malawi, Nepal, South Africa, Swaziland, Tanzania, Thailand, Uganda and Vietnam. Seventeen of the studies recruited people living with HIV (of which five focused specifically on pregnant women). The remaining three studies focused on young men who have sex with men, female sex workers and men who inject drugs. Studies were clustered into four categories based on the socioecological level of risk or resilience that they targeted: (1) individual level only, (2) individual and relational levels, (3) individual and structural levels and (4) structural level only. Thirteen studies targeting structural risks (with or without individual components) consistently produced significant reductions in self-stigma. The remaining seven studies that did not include a component to address structural risks produced mixed effects.
Conclusion
Structural interventions such as scale-up of antiretroviral treatment, prevention of medication stockouts, social empowerment and economic strengthening may help substantially reduce self-stigma among individuals. More research is urgently needed to understand how to reduce self-stigma among young people and key populations, as well as how to tackle intersectional self-stigma.
Keywords: self-stigma, HIV, key populations, stigma, low- and middle-income countries
Key questions.
What is already known?
Self-stigma among people living with and affected by HIV is a global public health threat because it hampers use of healthcare services, as well as uptake of and adherence to life-saving antiretroviral treatment (ART).
Little is known about what works to reduce self-stigma, particularly in low-income and middle-income countries where specialised psychological and psychiatric support services are scarce.
What are the new findings?
Interventions that resulted in consistent self-stigma reductions were ART provision, social empowerment, economic strengthening and cognitive-behavioural therapy.
Interventions with null effects on self-stigma were health awareness raising, stigma coping and behaviour change (although they were effective for other outcomes which were not the focus of this review).
What do the new findings imply?
Interventions targeting a combination of structural-level and individual-level risks and resilience hold promise for tackling self-stigma.
Introduction
A strong evidence base suggests that stigma—and the resultant fear of being judged or treated poorly—keeps people from accessing HIV and other health services.1–7 As such, stigma is a global public health threat that can have consequences on the epidemiology of HIV and other health conditions. The most commonly used definition of stigma is the one articulated by Goffman in his seminal work ‘Stigma: Notes on the Management of Spoiled Identity’.8 He defined stigma as a process through which individuals are ‘disqualified from full social acceptance’ due to an undesirable ‘mark’ or ‘label’. This label can be a physical, health or behavioural attribute that is deemed ‘deeply discrediting’. Half a century after Goffman’s seminal work was first published, interest in stigma has grown exponentially.9 The study of stigma has extended beyond sociology (where it originated) to public health and, most notably, HIV epidemiology.2 9–18
The vast majority of stigma intervention research focuses on averting discrimination (also known as enacted stigma).12 14 But people may also internalise stigma,19 leading to what Goffman called ‘spoiled identities’ or self-stigma. Self-stigma occurs when people who belong to a socially discredited group (eg, people living with HIV, people who use illicit drugs) internalise feelings of shame and worthlessness due to their socially devalued identity, or ‘spoiled identity’.16 20 Although self-stigma is experienced by individuals, it is also influenced by structural and relational forces that dominate their lives, such as discrimination, social exclusion and poverty.16 21 22 In line with this, Livingston and Boyd16 define self-stigma as ‘asubjective process, embedded within a socio-cultural context, which may be characterized by negative feelings (about self), maladaptive behaviour, identity transformation, or stereotype endorsement resulting from an individual’s experiences, perceptions, or anticipation of negative social reactions on the basis of their [socially devalued identity or] illness’. Self-stigma is particularly dangerous because it impacts anticipated and perceived stigma, and influences affective, cognitive and mental health outcomes, as well as healthcare behaviours, which ultimately affect physical health outcomes.19 21 23 In short, self-stigma contributes to AIDS-related morbidity and mortality by hampering adherence to life-saving antiretroviral treatment (ART),2 7 constraining people’s quality of life and spurring suicidal ideation.24 25
Unlike HIV-related discrimination, self-stigma remains strikingly understudied with no evidence of well-established, large-scale programmes to address it.12 13 26 In particular, there are two major gaps in our understanding of how to address self-stigma among people living with or affected by HIV. First, there is no synthesis of evidence on what works to address self-stigma in resource-limited settings. A recent systematic review and meta-analysis examined antistigma interventions in healthcare settings but only found eight studies reporting on self-stigma as a stand-alone outcome. Of these eight studies, three studies reported significant reductions in self-stigma, another three reported reductions in self-stigma that were not statistically significant, and two provided insufficient data for inferences about stigma reduction.14 While this previous review focused on interventions in healthcare settings, specialised mental health resources are scarce in low-income and middle-income countries (LMICs),27 and interventions are often delivered by community-based organisations or peers outside of the healthcare system.28 In such settings, it is essential to advance our understanding on what works to address self-stigma through scalable, community-based responses.
Second, no systematic review has explored what works to address other sources of self-stigma experienced by people living with or affected by HIV. For example, gay, bisexual and other men who have sex with men, sex workers, transgender people, people who inject drugs and incarcerated people are identified as ‘key populations’ who are particularly vulnerable to HIV.29 But a number of sociostructural risks including stigma and discrimination, poverty, punitive laws and policies, and violence also make these populations vulnerable to self-stigma related to their marginalised identities.30–35 Key populations may experience additional self-stigma due to viral hepatitis, which is highly prevalent in these groups.36 Similarly, people living with HIV in LMICs are also highly vulnerable to tuberculosis (TB) coinfection, and it is important to understand what works to address the resultant self-stigma.37 38 It is essential to review this body of evidence to inform culturally sensitive, scalable and sustainable service delivery models that reach the most marginalised populations disproportionately affected by HIV-related and other types of self-stigma.
In this review, we aim to address these gaps by identifying, synthesising and critically appraising existing evidence of interventions aiming to reduce self-stigma experienced by people living with HIV and key populations affected by HIV in LMICs. It is hoped that this review will inform much-needed programmes to address self-stigma among communities that are disproportionately marginalised.
Methods
Review scope
The scope of this review is restricted to intervention studies measuring any type of self-stigma as an outcome among people living with HIV or key populations affected by HIV (table 1).
Table 1.
Scope of the review
| Outcome | Internalised or self-stigma, shame, negative self-image, negative self-perception related to HIV status, other diseases that disproportionately affect people living with HIV (tuberculosis, hepatitis) or stigmatised behaviours of key populations affected by HIV (sex work, male-to-male sexual intercourse, drug use, transgender expression). |
| Population | People living with HIV, sex workers, men who have sex with men, people who use drugs, transgender people of all ages. |
| Geographical location | Low-income and middle-income countries. |
| Study design |
|
Search strategy
Studies were identified through electronic searches of bibliographic databases and grey literature sites, examining citations of retrieved studies, and contacting researchers working in the area. The larger databases were searched through OvidSP (PsycARTICLES, Embase, Global Health, Ovid MEDLINE and PsycINFO), using a sensitive search string summarised in the study protocol.39 Smaller databases (Cumulative Index to Nursing and Allied Health Literature and WHO Afro Library) incorporated a simpler, more inclusive search string also summarised in the protocol.39 The exact search strings used for each database are included in online supplementary file 1 for reproducibility. Key authors were contacted for unpublished and ongoing studies, as well as additional information from published papers. References listed from other reviews on HIV/AIDS stigma12 17 40–42 and other relevant studies were also screened.
bmjgh-2018-001285supp001.pdf (626.3KB, pdf)
Inclusion and exclusion criteria
To be eligible for inclusion in the review, the study had to meet all of the prespecified inclusion criteria and none of the exclusion criteria set out in table 2. In an attempt to assess intervention effectiveness and inform potential scale-up of promising interventions, only study designs that allowed for causal inferences were included.43 Therefore, this systematic review included randomised controlled trials, controlled clinical trials, prospective controlled cohort studies, retrospective controlled cohort studies if baseline exposure data were collected at time of baseline of study, controlled before and after studies including econometric studies, and interrupted time series studies.
Table 2.
Inclusion and exclusion criteria
| Inclusion criteria | Exclusion criteria |
Study population:
|
|
| Study design: The following designs IF they report on self-stigma as an outcome:
|
|
Outcome measure
|
|
Study selection process
Following Cochrane Collaboration guidelines,44 search results were merged and de-duplicated. The initial screening involved examination of titles and abstracts by two review authors (JP, JIS) to remove irrelevant reports. Ten per cent of retrieved records were double-screened and yielded high inter-rater reliability (>0.95). Screening of the remaining records was split between both review authors. Full-text documents were retrieved for potentially relevant reports and examined in detail for compliance with eligibility criteria (see above). Where appropriate, authors (corresponding authors and coauthors if contact information could be retrieved) were contacted with up to three follow-up emails over the course of 5 months to clarify study eligibility and request additional information or data.
Data extraction and quality appraisal
The data extraction form was adapted from the template and guidelines provided by Cochrane Collaboration. Each included study was independently reviewed by two or more authors (JP, JIS and MP). Quality of included studies was assessed using an adapted version of the Cambridge Quality Checklist,45 which rates evidence based on sampling procedures, participation rates, sample size and statistical power, measurement reliability, population involvement, and credibility of causal inferences drawn (ie, whether data are prospective, change in outcomes is analysed and a counterfactual/control is used). Following guidelines for reporting patient and public involvement in research,46 we adapted the checklist by additionally extracting information on the involvement of the population of interest in the research design and implementation. For randomised controlled trials, quality appraisal was further augmented with the Cochrane Risk of Bias Assessment Tool47 to account for potential flaws in the experimental design. A percentage score for each study was computed based on the study’s total score across both appraisal tools. A detailed description of the quality assessment tool and individual study ratings is provided in online supplementary file 2.
bmjgh-2018-001285supp002.pdf (423KB, pdf)
Data synthesis
A meta-analysis was not conducted due to heterogeneity in self-stigma measures, intervention type and study design. However, whenever possible, standardised effect sizes were calculated, allowing for comparisons in magnitude of effects across included studies. Standardised mean differences (Cohen’s d) were calculated wherever sufficient data were available. For cluster-randomised controlled trials that did not account for clustering, corrections were made by multiplying SEs with the variance inflation factor as suggested by Littell and colleagues.48
Lastly, a narrative synthesis was conducted following Bronfrenbrenner’s ecological framework of human development,49 which has previously been used for examining internalised stigma among same-sex couples in the USA.50 For the narrative synthesis, interventions were clustered based on the highest socioecological level of risk or resilience that the intervention targeted: microsystem or individual level, mesosystem or relational level, and macrosystem or structural level.49 Consistency, direction and strength of effects were reported for each of these clusters.
Results
Study characteristics
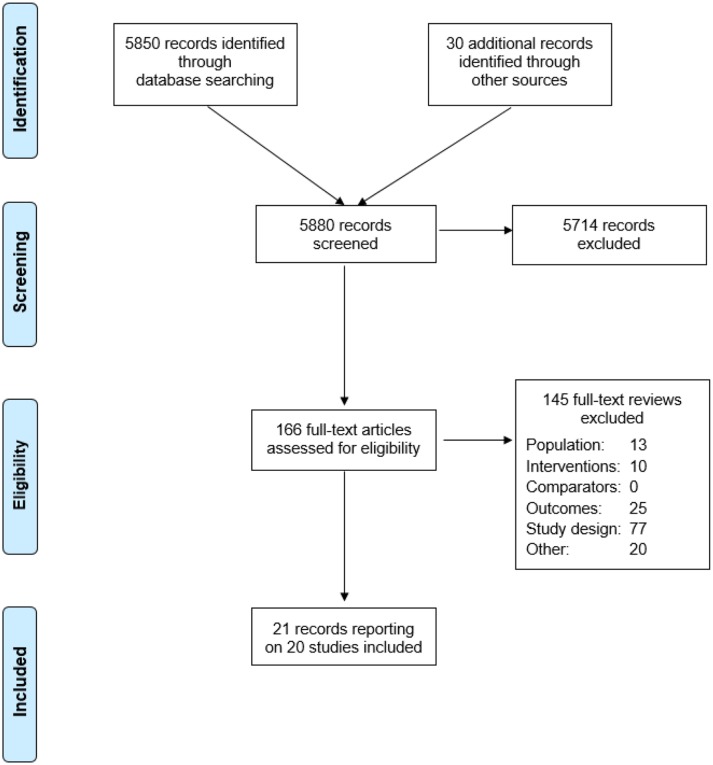
Of 5877 potentially relevant titles, 20 unique studies were included in the review. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram, including reasons for study exclusion, is provided in figure 1. Represented in the included studies are 9426 people in Uganda, Lesotho, Malawi, Ethiopia, South Africa, Swaziland, Tanzania, Kenya, Thailand, China, Vietnam, India and Nepal. Seventeen of the studies recruited people living with HIV (of which five focused specifically on pregnant women). The remaining three studies focused on young men who have sex with men,51 female sex workers31 and men who inject drugs.52
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram.
Intervention characteristics
Interventions were broadly grouped based on the socioecological levels of risk they aimed to target: individual, relational + individual, structural + individual, and structural level (figure 2). The following paragraphs describe the specific intervention components in more detail. Table 3 summarises which intervention components were included within individual studies and provides information on intervention dosage, with more detailed information on quality appraisal provided in online supplementary file 2.
Figure 2.
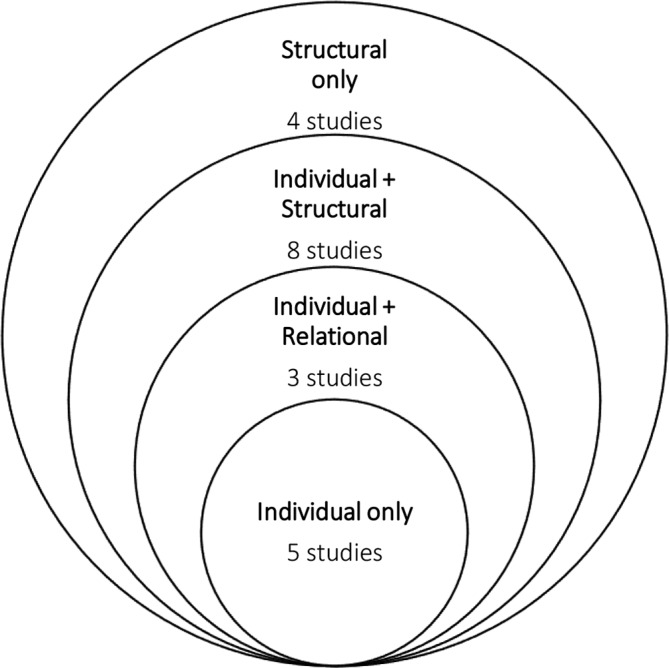
Socioecological levels of risk and resilience targeted within self-stigma interventions.
Table 3.
Characteristics of included studies and intervention effects
| Study reference | Country/Setting | Population | Intervention components and description | Programme dose | Study design | Sample size | Self-stigma measure used | Additional outcomes reported | Time to follow-up | Impact on self-stigma and effect size |
| Interventions targeting only individual-level risks and resilience | ||||||||||
| Low et al 53 | Western Kenya | People living with HIV (mean age: 45) | Behavioural (door-to-door HIV testing aimed to increase testing uptake in the presence of stigma). | 18 months. | Cluster randomised controlled trial | 3295 (not clear how many are T and C, equal split assumed) |
17 stigma items drawn from various sources,84 85 subscales: community stigma, personal stigma, community stigma actions, personal stigma actions, self-stigma. Focus on latter. | Community leader stigma towards PLH (reduced), community member stigma towards PLH (reduced). | 18 months |
No significant change in self-stigma, 0.05 (−0.02, 0.12). |
| Mundell57 | South Africa | HIV-positive pregnant women (mean age: 27) | Health education. Stigma coping. | 10 weeks. | Prospective cohort study with treated and non-treated (non-experimental) | T: 72 C: 84 |
Personal stigma scale based on ref 86 composed of 12 items focused on own experience of stigma and internalised blame. | Positive coping (improved), self-esteem (improved), levels of positive support and HIV-related support (improved), disclosure (improved), depression (no significant change), HIV knowledge (no significant change). | 3 months | Study reports no significant change in self-stigma, but did not provide sufficient information for calculating effect size. |
| Rongkavilit et al 51 | Thailand, Bangkok | Young men who have sex with men, living with HIV (mean age: 23) | Behavioural (motivational interviewing focused on changing sexual risks and alcohol use). | 4 sessions. | Randomised controlled trial | T: 37 C: 37 |
12 internalised stigma items drawn from Berger’s 40-item HIV Stigma Scale.73 | Sexual risk behaviour (reduced), adherence (no significant change), alcohol and drug use (no significant change), general mental health (no significant change). | 1 and 6 months |
No significant change in self-stigma, −0.43 (−0.90, 0.03). |
| Tshabalala and Visser54 | South Africa | Women living with HIV (age range 22–40) | Cognitive-behavioural therapy: Psychological support.
Behavioural. |
8 weekly sessions. | Randomised controlled trial | T: 10 C: 10 |
Serithi Internalised Stigma Scale,87 16 items denoting two factors of tendency towards self-blame and interpersonal distance. | Coping (improved), self-esteem (improved), depression (reduced), enacted stigma (no significant change). | 2 months |
Reduction in self-stigma, −1.22 (−2.17, −0.26). |
| Van Tam et al 55 | Vietnam, Quang Ninh (4 outpatient clinics) | Adults living with HIV (age range: 18–60) | Behavioural (peers aimed to increase participants’ ART adherence through check-ins following a checklist). | Biweekly visits for first 2 months, after this weekly. | Cluster randomised controlled trial | T: 119 C: 109 |
Internal AIDS-Related Stigma Scale.71 | Quality of life (improved). | 12 months |
No significant change in self-stigma, −0.03 (−0.29, 0.23). |
| Interventions targeting relational-level and individual-level risks and resilience | ||||||||||
| Go et al 52 | Vietnam, Thai Nguyen Province | Men who inject drugs (mean age: 35) |
Stigma awareness and coping.
Health education. Community stigma reduction (through video screenings and home visits to raise awareness and debunking misconceptions). |
Men living with HIV who inject drugs received:
Community members received:
|
Four-arm factorial randomised controlled trial | Community T: 139 Individual T: 95 Both T: 132 C: 89 |
New scale developed for the purposes of this study, capturing both HIV-related as well as injecting drug use-related internalised stigma. | HIV seroconversions (no significant change), sexual and injection risks (initial reductions at 6 months’ follow-up observed but not sustained at 24 months). | Every 6 months, 24-month endpoint |
No significant change in self-stigma, −0.07 (−0.39, 0.25). |
| Peltzer et al 60 | South Africa, Mpuma-langa | HIV-positive pregnant women (median age: 28) | ’Protect your Family’ programme: Health education for both women and their male partners (delivered separately for women and their male partners, and focused on health-seeking behaviours, adherence, intimate partner violence, communication). Psychological support (individual counselling for women). Cognitive-behavioural intervention for both women and their male partners (to improve communication, health-seeking behaviours, anger management and reduce intimate partner violence). |
Standard PMTCT care and three prenatal weekly 2-hour group sessions and one 1-hour individual counselling session (at 32 weeks’ gestation) and two 1-hour monthly individual or couples counselling sessions (6 and 12 weeks postnatally). | Cluster randomised controlled trial | T: 342 C: 357 |
12 items drawn from Berger’s 40-item HIV Scale73 (contains four stigma subscales: personalised stigma, disclosure concerns, negative self-image and public attitude stigma). |
HIV serostatus (no change) and ART adherence for mothers and infants (no change), HIV and PMTCT knowledge (no change). Additional outcomes listed in study protocol: intimate partner violence and communication and male HIV testing and engagement in PMTCT. |
12 months |
Reduction in self-stigma, −0.48 (−0.63, −0.33). |
| Prinsloo et al 61 | Urban South Africa | People living with HIV (mean age: NA) |
Stigma coping. Community stigma reduction intervention (through raising awareness, acting psychodramas and pamphlet distribution). |
5 months in total:
|
Mixed-methods prospective cohort study | 62 | HASI-P internalised stigma subscale.24 | Reported by people living with HIV: verbal abuse, healthcare neglect, social isolation, fear of contagion (no significant changes in any of the above outcomes). Reported by community members: behaviour towards PLH, symbolic and instrumental stigma (no significant changes in any of the above outcomes). |
5 months | Study reports no significant change in self-stigma, but did not provide sufficient information for calculating effect size. |
| Interventions targeting structural-level and individual-level risks and resilience | ||||||||||
| Bhatta and Liabsuetrakul62 | Nepal | People living with HIV (mean age: 36) | Empowerment (focusing on autonomy and community activism, self-care, stress management and rights). | 6 weekly, 90 min sessions | Randomised controlled trial | T: 66 C: 66 |
Stigma was measured using a 23-item scale drawn from Genberg et al (2008),88 including three subscales, namely shame/blame, perceived discrimination and equity. | Empowerment (improved), social support (improved), quality of life (improved). | 3, 6 months |
Reduction in self-stigma, −1.37 (−1.74, −0.98). |
| Chidrawi et al
63 and 2014 (reporting on same sample) |
South Africa, North-West Province | People living with HIV (mean age: 37) | Empowerment (to implement a stigma reduction intervention in their communities). |
|
Prospective cohort study | 18 | HASI-P internalised stigma subscale.24 | HIV signs and symptoms (reduced), quality of Life (no significant change). | Every 4 months, 12 months endpoint |
Reduction in self-stigma. Effect size calculated for longest follow-up (after 12 months): −0.51 (−1.17, −0.15). |
| Ghosal et al 83 | India, Kolkata | Female sex workers (mean age: 32) | ‘Dream building’: Empowerment (dream-building workshops whereby participants set their own goals, are supported to reshape their self-image in positive direction and are provided skills to assert their rights). Economic strengthening (training session focused on saving that were also provided to control group). |
8 weekly group sessions. | Cluster randomised controlled trial | T: 264 C: 203 |
Newly developed measures, shame related to sex work, captured by one item: ’Are you ashamed of your occupation?’
Self-worth, coded as 0 if the person referred to herself as a ’Bad woman’, ’Fallen woman’, ’Woman with no future’, ’Criminal’. |
Happiness (improved), self-efficacy (improved), future-oriented behaviour captured by savings and healthcare choices (improved), decision-making power (no significant change), comfort in public interaction, aspirations (no significant change). | Immediate post-test |
Reduction in self-stigma. Shame: −1.05 (−1.24, −0.85). Self-worth: 2.55 (2.31, 2.80). |
| Lifson et al 59 | Rural Ethiopia | People living with HIV (mean age: 34) | Community health support workers provided: Health education (including facilitated communication with the clinic about the client’s health and treatment regimens). Psychological support (counselling and social support). Economic strengthening (through referrals to community organisations for support with nutrition, clothing, housing or income-generating activities). |
1–4 times per month over 12 months. | Prospective cohort study | 142 | HASI-P internalised stigma subscale.24 | HIV knowledge (improved), physical and mental quality of life (improved), perceived social support (improved). | 12 months | Study reports a statistically significant reduction in self-stigma scores (from 1.6 to 0.05, p<0.001), but did not provide sufficient information for calculating the effect size. |
| Maluccio et al 65 | Uganda (Gulu and Soroti) | ART-naïve adults living with HIV (mean age: 39) |
ART initiation (in healthcare facility). Economic strengthening (food assistance). Treatment support (monthly meeting with a support officer who provided treatment and disclosure counselling). |
12 months. | Quasi- experimental difference-in-difference matching | T: 448 C: 456 |
HASI-P internalised stigma subscale.24 | External, enacted, received stigma (no significant change). | 12 months |
Reduction in self-stigma, −0.14 (−0.25, −0.02). |
| Nyamathi et al 58 | Rural India | Women living with HIV (mean age: 31) |
Health education (living with HIV, ART, parenting and maintaining a healthy home environment). Stigma coping. Economic strengthening (monthly supply of grains, bus token and life skills training). |
6 sessions—45 min, then weekly visits for 15–60 min. | Cluster randomised controlled trial | T: 34 C: 34 |
10-item scale which was one of four stigma scales based on previous research89 90 and adapted to India (eg, ’How much do you feel that you deserve to have HIV?’). | Disclosure avoidance/avoidance coping (improved). | 6 months |
Reduction in self-stigma, −4.60 (−5.51, −3.69). |
| Turan et al 67 | Rural Kenya (Nyanza) | Newly diagnosed pregnant women living with HIV (mean age: 24) |
ART initiation (in healthcare facility). Health education (HIV care and treatment programme, which provided access to health education, adherence counselling services, patient support group). |
6 weeks. | Prospective cohort study | 135 | HASI-P internalised stigma subscale.24 | Postpartum depression (reduced). | 6 weeks | Study reports a reduction in self-stigma, but did not provide sufficient information for calculating effect size. |
| Uys et al 64 | Lesotho, Malawi, South Africa, Swaziland and Tanzania | Adults living with HIV (mean age: 38) | Empowerment (people living with HIV, together with healthcare workers, designed and implemented interventions). | Workshop: 21 hours, peer-organised meetings varied between 5 and 8 hours, total dose thus varied between 8 and 20 hours. | Cohort study | 41 | HASI-P internalised stigma subscale.24 | Self-esteem (improved), self-efficacy (no significant change). | 1 month |
Reduction in self-stigma, −0.50 (−0.93, −0.06). |
| Interventions operating only at the structural-level | ||||||||||
| Makoae et al 70 | Lesotho, Malawi, South Africa, Swaziland and Tanzania | People living with HIV (mean age: 36) | Clinical ART provision. | 12 months. | Prospective cohort study with treated and non-treated (non-experimental) | T: 488 C: 443 |
HASI-P internalised stigma subscale.24 | None. | 6, 12 months |
Reduction in self-stigma, −0.18 (−0.05, −0.31). |
| Peltzer and Ramlagan69 | South Africa, KwaZulu-Natal | ART-naive adults living with HIV (mean age: 36) | ART initiation (in healthcare facility). | Not applicable. | Prospective cohort study | 735 | 6-item Internalised AIDS-Related Stigma Scale capturing self-defacing beliefs.71 | HIV-related health status (improved), quality of Life (improved), depression (significant increase, adverse effect). |
6 and 12 months |
Reduction in self-stigma, −0.59 (−0.69, −0.48). |
| Tsai et al 68 | Rural Uganda | ART-naïve adults living with HIV (median age: 34) |
ART initiation (in healthcare facility). | 2 counselling sessions preinitiation, then 2–5 times annually, more counselling sessions on request. | Prospective cohort study | 262 | Internal AIDS-Related Stigma Scale.71 | HIV symptom burden (improved), physical and psychological well-being (improved), depression symptom severity (reduced). | Varies, but medium 3.4 years |
Reduction in self-stigma, −0.25 (−0.42, −0.08). |
| Wagner et al 66 | Uganda, Kampala and Kakira | Adults living with HIV (mean age: 36) | ART initiation (in healthcare facility). | 12 months; ART patients attend clinic on a monthly basis at first and then bimonthly; non-ART patients attend clinic between 2 and 6 months depending on their CD4 count. | Prospective cohort study with treated and non-treated (non-experimental) | T: 300 C: 302 |
Internal AIDS-Related Stigma Scale drawn from Kalichman et al.71 | Depression (reduced), hopelessness (reduced). | 6 and 12 months |
Reduction in self-stigma, −0.47 (−0.64, −0.31). |
ART, antiretroviral treatment; C, control arm; HASI-P, HIV/AIDS Stigma Instrument for People Living with HIV; NA, not applicable; PLH, people living with HIV; PMTCT, prevention of mother-to-child transmission; T, treatment arm.
Individual-level intervention components included health education, behaviour change, stigma coping and psychological support. Health education 51 53–55 included information about living with HIV and treatment regimens. Behaviour change for people living with HIV or key populations 51 53 55 was incorporated in three studies that evaluated interventions aiming to alter behaviours that make individuals more vulnerable to acquiring or transmitting HIV.56 These included interventions focusing on reducing sexual risk behaviours and alcohol use, or those aiming to improve ART adherence and HIV testing uptake. Stigma coping for people living with HIV and key populations 52 57 58 involved psychoeducational sessions with the purpose of defining stigmatisation and discussing ways of coping with it, combined with health education. One of the studies combined stigma coping with economic strengthening.58 Finally, psychological support 54 59 60 in the form of counselling and group and individual cognitive-behavioural therapy was examined in three studies.
Relational-level components were community-wide stigma awareness and reduction campaigns and cognitive-behavioural therapy for partners of women living with HIV. Community-wide stigma awareness and reduction interventions52 61 aimed to debunk myths around HIV and raising awareness in the general community. One study included cognitive-behavioural therapy for partners of women living with HIV,61 which aimed to reduce intimate partner violence, improve communication skills and anger management, and enhance health-seeking behaviours.
At the structural level components included social or economic empowerment approaches and ART roll-out. These additionally included individual-level components in eight studies and did not in four. In social empowerment interventions, people living with HIV or key populations were offered skills and opportunities to mobilise, assert their rights, and/or develop and implement their own antistigma interventions.31 62–64 Economic strengthening 31 58 59 65 interventions offered schemes for savings, housing and nutrition support, and income-generating activities. ART roll-out interventions included ART initiation for treatment-naïve people living with HIV66–69 or continued ART provision70 for people who were already on treatment.
Outcomes
All of the self-stigma measures used are listed in table 3. Self-stigma was most commonly measured through previously validated scales for HIV-related stigma, including the HIV/AIDS Stigma Instrument for People Living with HIV scale24 in seven studies,59 61 63–65 67 70 followed by the Internalized AIDS-Related Scale71 used in four studies55 66 69 72 and the Berger Scale73 used in two studies.51 60 Two studies measured self-stigma related to belonging to a key population, specifically self-stigma related to drug use52 and sex work.31 No studies explored self-stigma related to hepatitis, TB or other health conditions.
Aside from self-stigma outcomes, studies measured HIV-related outcomes (HIV symptoms, HIV seroconversions, ART adherence, CD4 counts, HIV knowledge, sexual and injection risks for acquiring HIV), psychological outcomes (general mental health, depression, happiness, self-esteem, self-efficacy, positive coping, avoidant coping, hopelessness, aspirations, quality of life, alcohol and drug use), relational outcomes (comfort in public interaction, enacted stigma or discrimination, HIV status disclosure, social support) and empowerment (decision-making power and future-oriented behaviour).
Intervention effectiveness
This section focuses on self-stigma outcomes. Other outcomes recorded in the primary studies were not the scope of this review but are summarised in table 3.
Less than three-quarters (14/20) of the studies reported significant reductions in self-stigma. Effect sizes were extracted or calculated wherever possible; however, five papers did not provide sufficient information and neither could these be obtained through contacting authors. Most of the interventions included multiple components. They are broadly categorised based on the socioecological levels of risk or resilience that they aimed to target: (1) interventions that only targeted individual-level risk and resilience (but not relational or structural factors); (2) interventions targeting relational and individual factors (but not structural factors); (3) interventions targeting structural and individual factors (but not relational factors); and (4) interventions targeting exclusively structural factors.
Individual-level interventions
There were five interventions operating solely at the individual level. Behavioural interventions that did not include any other components (three studies) consistently produced no significant changes in self-stigma.51 53 55 One intervention (n=20) focused solely on psychological support (cognitive-behavioural therapy), and it resulted in a significant reduction in self-stigma (d=−1.22, 95% CI −2.17 to 0.26).54 The remaining studies focused on education related to stigma (including coping) and health, and it did not result in a significant self-stigma reduction.57
Interventions operating at the relational and individual levels
There were three studies examining interventions operating at both the relational and individual levels. Two interventions combined stigma reduction in the broader community through awareness raising with individual-level psychoeducational components for men who inject drugs52 and people living with HIV.61 Neither of these interventions resulted in significant self-stigma reduction.
The remaining intervention used cognitive-behavioural therapy and health education for both women living with HIV and their male partners (separately), combined with psychological support for the women.60 This intervention resulted in a significant reduction in self-stigma (d=−0.48, 95% CI −0.63 to 0.33).
Interventions operating at the structural and individual levels
There were eight studies examining interventions operating at both the structural and individual levels. They consistently produced significant reductions in self-stigma, irrespective of what components they included. Empowerment interventions consistently resulted in reductions in self-stigma, with standardised effect sizes of d=0.50 in two studies and d>1 in the other two.31 62–64 All interventions that had an economic strengthening component (such as food assistance, income generation, saving promotion) also resulted in significant reductions in self-stigma, with effect sizes ranging from d=−4.60 to d=−0.02.31 58 65 One economic strengthening study reported a statistically significant reduction in self-stigma scores (from 1.6 to 0.05, p<0.001) without sufficient statistical data to calculate the standardised effect size.59 One study evaluated the effects of combined ART provision with health education and reported significant reductions in self-stigma (although there was insufficient information to calculate the effect size).67
Structural-level interventions
Four studies examined interventions at the structural level only. Specifically, all of these studies included ART provision—both initiation and continuation. They consistently resulted in reductions in self-stigma over time, with effect sizes ranging from d=−0.59 to d=−0.18.41 66 69 70
Study quality
Across studies, time to follow-up ranged from 1 month to 3 years, with ART-based interventions typically assessed within longer timeframes. For studies with particularly short timelines, it is difficult to establish whether reductions in self-stigma are sustainable over the longer term. In addition, only 4 of 20 studies52 58 60 indicated that sample sizes were determined based on power calculations. Lastly, half of the included studies (10/20) reported whether and how the population of interest was engaged in the research beyond mere participation.
There was substantial heterogeneity in the quality of included studies, with quality scores ranging from 30% to 78%. Half of the included studies (10/20) were randomised controlled trials. As a standard, the impact of ART provision on self-stigma was assessed within prospective cohort studies, as withholding life-saving treatment from people living with HIV would be ethically unacceptable. Overall study quality was rated as medium to high for studies evaluating pure behavioural interventions,51 53 55 ART provision,41 66 67 69 70 relational interventions52 61 and economic strengthening.31 58 59 65 In contrast, quality of evidence was limited by small sample sizes for stigma-related education, stand-alone psychological therapy and social empowerment interventions; hence, further studies are needed for more conclusive and robust inferences.
Discussion
This is the first systematic review of interventions aiming to reduce self-stigma among people living with HIV or affected by HIV. We identified a wide range of interventions that aimed to address individual, relational and structural risk and resilience factors. Despite the nascent state of the literature, several consistent findings offer direction for policy and programming.
What worked?
We found considerable evidence in support of structural interventions or interventions aiming to mitigate structural risks, within methodologically strong studies. These approaches included economic strengthening, social empowerment and ART roll-out. ART initiation consistently resulted in reductions in self-stigma, which is in line with systematic review-level evidence indicating that improvements in HIV-related health outcomes can drive reductions in self-stigma.13 Therefore, a cyclical relationship between self-stigma and ART use is likely, whereby ART uptake reduces self-stigma but persistent self-stigma compromises ART adherence.2
Structural interventions that focused on empowerment and/or economic strengthening components consistently appeared to be effective in reducing self-stigma. They additionally included individual-level components such as health and/or stigma education,58 59 67 ART support or counselling,59 65 making it difficult to identify the ‘active’ component of the intervention in the absence of multiarm factorial designs. Yet it may be worth noting that interventions combining structural-level and individual-level components had stronger effects on stigma reductions than structural-only interventions (the latter were all ART-provision interventions). This is in line with recent epidemiological and theoretical work which suggests that self-stigma is shaped by factors operating both at the individual (mental health) and structural (poverty) levels.21 41 74 75 The broader literature on mental health also points to the role of structural-level risks in psychological distress. For example, a recent meta-analysis found that income inequality at the national level was associated with higher risk of depression, with a pooled risk ratio of 1.19 (95% CI 1.07 to 1.31). The authors ‘propose an ecological framework with mechanisms operating at the national level (the neo‐material hypothesis), neighbourhood level (the social capital and the social comparison hypotheses) and individual level (psychological stress and social defeat hypotheses) to explain this association’.76 Similar pathways are plausible in the production of self-stigma among people living with or affected by HIV, and more research on multilevel interventions is needed.
High variability in the content of these interventions limits inferences for programme implementation. For example, economic strengthening interventions ranged from food assistance to financial literacy, while empowerment interventions included autonomy, community activism, and people living with HIV designing and implementing stigma reduction interventions. More research is essential to unpack which empowerment and economic strengthening interventions are suitable under what circumstances and for whom. For example, multiarm trials and mediation analyses could help identify active intervention components and mechanisms of effect. Despite these nuances, we found a reasonable amount of consistent and robust evidence suggesting that interventions that effectively buffer against structural risks and enhance individual-level resilience are likely to have a substantial impact on reducing self-stigma.
Cognitive-behavioural therapy appeared to be the only effective intervention at the individual level and at the relational and individual levels combined. At the solely individual level, one study offered cognitive-behavioural therapy to a small sample of people living with HIV.54 At the relational and individual levels, one study combined cognitive-behavioural therapy with health education for a large sample of both women living with HIV and their male partners (separately), in addition to psychological support for the women.60 Providing cognitive behavioural therapy (CBT) to both women living with HIV and their partners, with a focus on anger management for the partners, may have produced self-stigma both directly by improving the women’s mental health, and indirectly by reducing emotional and physical violence victimisation.21
Both of the CBT studies scored highly on quality assessment, with the individual-level one having a small sample size (n=20). Given the scarcity of research on the effectiveness of CBT to reduce self-stigma, more research on this is needed to inform decisions about scale-up. For example, more research is needed to evaluate effectiveness of CBT when delivered by trained lay professionals and online counselling services, which might address shortages in clinical psychologists in many resource-limited settings.
What did not work, or had insufficient evidence in support of it?
It is also important to highlight what did not appear to be effective. However, it should also be noted that for studies that did not report on sample size calculations, there is a high risk of type II error, making it difficult to establish whether they were truly ineffective or simply underpowered to detect changes in self-stigma.
All interventions focusing solely on individual-level risk and resilience factors, except for CBT, appeared to be ineffective. Specifically, all three behavioural interventions that aimed to change individuals’ healthcare behaviours (HIV risks, HIV testing and ART adherence) and did not include any other components consistently produced no significant changes in self-stigma.51 55 Two of these studies were well powered, rendering type II error highly unlikely. Evidence suggests that self-stigma acts as a barrier to HIV testing, status disclosure and ART adherence.2 72 77 In light of this, behavioural interventions that result in short-term HIV risk reduction may not be sustainable if they fail to address self-stigma.
Likewise, studies focusing solely on education related to stigma and/or health did not result in significant self-stigma reductions.52 57 61 This applies to both interventions aiming to raise awareness among individuals who have internalised stigma57 61 and among the broader community,52 suggesting that neither individual-level nor community-level knowledge around HIV and stigma is sufficient to combat self-stigma. These findings are in line with systematic review-level evidence of interventions to reduce self-stigma among people living with mental health difficulties, which suggest that psychoeducational interventions are largely ineffective for reducing self-stigma.78 79
Knowledge gaps and recommendations for research
This systematic review found that more than a quarter of examined interventions were ineffective in reducing self-stigma. This points to the complexity in achieving impact on self-stigma reductions and highlights the need for rigorous evaluations when implementing.
Notable gaps in the evidence base were identified and more research is urgently needed to address them. First, the vast majority of research focused on general populations of people living with HIV or pregnant women living with HIV. Of the three studies focusing on key populations, only one effectively reduced self-stigma. Only one study focusing on young people was identified, despite evidence of high levels of self-stigma in this group.21 The study aimed to reduce self-stigma among young men who have sex with men in Thailand but did not result in significant reductions in self-stigma.51 The intervention focused on behaviour change through motivational interviewing—it resulted in significant reductions in sexual risk behaviour, and no changes in adherence, alcohol and drug use, and general mental health.
None of the studies reported on intersectional stigmas, which occurs when different types of stigma are compounded due to belonging to more than one marginalised social group.32 Evidence suggests that intersectional self-stigma is common among people living with HIV and affected by HIV,30 32 80 but it remains unknown how to address this issue and support people with intersecting vulnerabilities. Intervention research on this is clearly needed. None of the studies examined self-stigma related to TB, viral hepatitis or other infectious diseases that are common among people living with or affected by HIV. South Africa’s current National Strategic Plan for HIV, TB and sexually transmitted infections recognises both HIV-related and TB-related self-stigma as major public health concerns. As such, it aims to halve both HIV-related and TB-related self-stigma by 2022.81 Evidence is urgently needed to inform ambitious goals such as this one.
Only half of the studies reported on community engagement in the intervention design or research process (online supplementary file 2), despite increasing calls for this by the British Medical Journal Patient and Public Partnership initiative and others.46 82 Failure to report on community engagement in the research process does not necessarily mean that the researchers did not engage with the community. But without reporting on this, it is impossible to infer whether and to what extent this happened. While examining this in detail was not within the scope of the review, findings suggest a need for more accountability on this within academic publishing. For example, standard reporting guidelines on community engagement would allow for more transparency and clarity on whether and how this occurs in practice.82
Limitations
A few limitations of this systematic review should be noted. First, it is possible that more studies with null effects on self-stigma exist but remain unpublished due to the file drawer problem. However, by specifically screening grey literature data and contacting key authors in this research field, we were able to identify two (yet) unpublished studies.57 83 Second, due to the heterogeneity of interventions and outcomes, we were not able to conduct a meta-analysis. However, whenever possible, standardised effect sizes were calculated and presented in a summary table to allow readers to compare effects between studies. Lastly, while no language restrictions were enforced, all searches were conducted in English and we did not identify any documents in other languages.
Conclusions
This systematic review provides an unprecedented overview of evidence on interventions aiming to reduce self-stigma among people living with and affected by HIV in LMICs. Findings suggest that interventions aiming to buffer against structural stressors hold promise for reducing self-stigma. In particular, interventions focusing on social empowerment, economic strengthening and ART scale-up may substantially reduce self-stigma among individuals living with or affected by HIV. We found little evidence in support of individual-level interventions such as those focusing on health behaviour change, individuals coping with stigma or awareness raising. The only individual-level intervention that appeared to be effective (within a limited number of studies) was cognitive-behavioural therapy. More research is urgently needed to understand what works among key populations affected by HIV and young people, as well as what approaches might help reduce intersectional self-stigma.
Footnotes
Handling editor: Seye Abimbola
Twitter: New #systematicreview by @PantelichMarija et al. identifies what works to address self #stigma among people living with and affected by #HIV in resource-limited settings.
Contributors: MP conceptualised the study with input from SM. JIS double-screened and double-coded the studies. JIS contributed to interpretation of findings. MP had the final responsibility of writing the paper, with feedback from all authors.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1. UNAIDS Reducing HIV stigma and discrimination: a critical part of national AIDS programmes. Geneva, 2007. [Google Scholar]
- 2. Katz IT, Ryu AE, Onuegbu AG, et al. Impact of HIV-related stigma on treatment adherence: systematic review and meta-synthesis. J Int AIDS Soc 2013;16 10.7448/IAS.16.3.18640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Earnshaw VA, Smith LR, Shuper PA, et al. HIV stigma and unprotected sex among PLWH in KwaZulu-Natal, South Africa: a longitudinal exploration of mediating mechanisms. AIDS Care 2014;26:1506–13. 10.1080/09540121.2014.938015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Treves-Kagan S, El Ayadi AM, Pettifor A, et al. Gender, HIV testing and stigma: the association of HIV testing behaviors and community-level and individual-level stigma in rural South Africa differ for men and women. AIDS Behav 2017;21:2579–88. 10.1007/s10461-016-1671-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Moshabela M, Zuma T, Orne-Gliemann J, et al. "It is better to die": experiences of traditional health practitioners within the HIV treatment as prevention trial communities in rural South Africa (ANRS 12249 TasP trial). AIDS Care 2016;28 Suppl 3:24–32. 10.1080/09540121.2016.1181296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ng CK, Tsai AC. Proximate context of HIV-related stigma and women's use of skilled childbirth services in Uganda. AIDS Behav 2017;21:307–16. 10.1007/s10461-016-1401-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sweeney SM, Vanable PA. The association of HIV-related stigma to HIV medication adherence: a systematic review and synthesis of the literature. AIDS Behav 2016;20:29–50. 10.1007/s10461-015-1164-1 [DOI] [PubMed] [Google Scholar]
- 8. Goffman E. Stigma: notes on the management of spoiled identity. New Jersey US: Prentice-Hall, 1963. [Google Scholar]
- 9. AER B, Pryor JB, Reeder GD, et al. Stigma: advances in theory and research. Basic Appl Soc Psych 2013;35. [Google Scholar]
- 10. Scambler G, stigma H-related. Health-related stigma. Sociol Health Illn 2009;31:441–55. 10.1111/j.1467-9566.2009.01161.x [DOI] [PubMed] [Google Scholar]
- 11. Parker R, Aggleton P. HIV and AIDS-related stigma and discrimination: a conceptual framework and implications for action. Soc Sci Med 2003;57:13–24. 10.1016/S0277-9536(02)00304-0 [DOI] [PubMed] [Google Scholar]
- 12. Stangl AL, Lloyd JK, Brady LM, et al. A systematic review of interventions to reduce HIV-related stigma and discrimination from 2002 to 2013: how far have we come? J Int AIDS Soc 2013;16 10.7448/IAS.16.3.18734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Pantelic M, Shenderovich Y, Cluver L, et al. Predictors of internalised HIV-related stigma: a systematic review of studies in sub-Saharan Africa. Health Psychol Rev 2015;9:469–90. 10.1080/17437199.2014.996243 [DOI] [PubMed] [Google Scholar]
- 14. Siegfried N, Beanland R, 2017. Systematic Review on the Evidence-base for Eliminating Stigma and Discrimination in Health Care Settings [Internet]. Available: http://files.icap.columbia.edu/files/uploads/2017.12.04_Final_Report_Stigma_and_Discrimination_Review.pdf
- 15. Mahajan AP, Sayles JN, Patel VA, et al. Stigma in the HIV/AIDS epidemic: a review of the literature and recommendations for the way forward. AIDS 2010;22(Suppl 2):S67–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Livingston JD, Boyd JE. Correlates and consequences of internalized stigma for people living with mental illness: a systematic review and meta-analysis. Soc Sci Med 2010;71:2150–61. 10.1016/j.socscimed.2010.09.030 [DOI] [PubMed] [Google Scholar]
- 17. Sengupta S, Banks B, Jonas D, et al. HIV interventions to reduce HIV/AIDS stigma: a systematic review. AIDS Behav 2011;15:1075–87. 10.1007/s10461-010-9847-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. McAteer CI, Truong N-AT, Aluoch J, et al. A systematic review of measures of HIV/AIDS stigma in pediatric HIV-infected and affected populations, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Earnshaw VA, Smith LR, Chaudoir SR, et al. HIV stigma mechanisms and well-being among PLWH: a test of the HIV stigma framework. AIDS Behav 2013;17:1785–95. 10.1007/s10461-013-0437-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Goffman E. Stigma: the management of spoiled identity. Harmmondsworth Penguin, 1968. [Google Scholar]
- 21. Pantelic M, Boyes M, Cluver L, et al. HIV, violence, blame and shame: pathways of risk to internalized HIV stigma among South African adolescents living with HIV. J Int AIDS Soc 2017;20:21771–9. 10.7448/IAS.20.1.21771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Abadía-Barrero CE, Castro A. Experiences of stigma and access to HAART in children and adolescents living with HIV/AIDS in Brazil. Soc Sci Med 2006;62:1219–28. 10.1016/j.socscimed.2005.07.006 [DOI] [PubMed] [Google Scholar]
- 23. Turan B, Budhwani H, Fazeli PL, et al. How does stigma affect people living with HIV? The mediating roles of internalized and anticipated HIV stigma in the effects of perceived community stigma on health and psychosocial outcomes. AIDS Behav 2017;21:283–91. 10.1007/s10461-016-1451-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Holzemer WL, Uys LR, Chirwa ML, et al. Validation of the HIV/AIDS Stigma Instrument - PLWA (HASI-P). AIDS Care 2007;19:1002–12. 10.1080/09540120701245999 [DOI] [PubMed] [Google Scholar]
- 25. Pantelic M, Boyes M, Cluver L, et al. 'They say HIV is a punishment from God or from ancestors': cross-cultural adaptation and psychometric assessment of an HIV stigma scale for South African adolescents living with HIV (ALHIV-SS). Child Indic Res 2018;11 10.1007/s12187-016-9428-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ma PHX, Chan ZCY, Loke AY. Self-Stigma reduction interventions for people living with HIV/AIDS and their families: a systematic review. AIDS Behav 2018. [Epub ahead of print: 08 Oct 2018]. 10.1007/s10461-018-2304-1 [DOI] [PubMed] [Google Scholar]
- 27. Saxena S, Thornicroft G, Knapp M, et al. Resources for mental health: scarcity, inequity, and inefficiency. The Lancet 2007;370:878–89. 10.1016/S0140-6736(07)61239-2 [DOI] [PubMed] [Google Scholar]
- 28. Singla DR, Kohrt BA, Murray LK, et al. Psychological treatments for the world: lessons from low- and middle-income countries. Annu Rev Clin Psychol 2017;13:149–81. 10.1146/annurev-clinpsy-032816-045217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Macdonald V, Verster A, Baggaley R. A call for differentiated approaches to delivering HIV services to key populations. J Int AIDS Soc 2017;20 10.7448/IAS.20.5.21658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hargreaves JR, Busza J, Mushati P, et al. Overlapping HIV and sex-work stigma among female sex workers recruited to 14 respondent-driven sampling surveys across Zimbabwe, 2013. AIDS Care 2017;29:675–85. 10.1080/09540121.2016.1268673 [DOI] [PubMed] [Google Scholar]
- 31. Ghosal S, Jana S, Mani A, et al. Discrimination and Self-Image: evidence from Kolkata Brothels, 2017. [Google Scholar]
- 32. Logie CH, James LLana, Tharao W, et al. HIV, gender, race, sexual orientation, and sex work: a qualitative study of intersectional stigma experienced by HIV-positive women in Ontario, Canada. PLoS Med 2011;8 10.1371/journal.pmed.1001124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. DeBeck K, Cheng T, Montaner JS, et al. HIV and the criminalisation of drug use among people who inject drugs: a systematic review. Lancet HIV 2017;4:e357–74. 10.1016/S2352-3018(17)30073-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Oldenburg CE, Perez-Brumer AG, Reisner SL, et al. Human rights protections and HIV prevalence among MSM who sell sex: Cross-country comparisons from a systematic review and meta-analysis. Glob Public Health 2018;13:414–25. 10.1080/17441692.2016.1149598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Shannon K, Strathdee SA, Goldenberg SM, et al. Global epidemiology of HIV among female sex workers: influence of structural determinants. The Lancet 2015;385:55–71. 10.1016/S0140-6736(14)60931-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Martin NK, Vickerman P, Dore GJ, et al. The hepatitis C virus epidemics in key populations (including people who inject drugs, prisoners and MSM). Curr Opin HIV AIDS 2015;10:374–80. 10.1097/COH.0000000000000179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Bond V, Nyblade L. The importance of addressing the unfolding TB-HIV stigma in high HIV prevalence settings. J Community Appl Soc Psychol 2006;16:452–61. 10.1002/casp.893 [DOI] [Google Scholar]
- 38. Deribew A, Hailemichael Y, Tesfaye M, et al. The synergy between TB and HIV co-infection on perceived stigma in Ethiopia. BMC Res Notes 2010;3 10.1186/1756-0500-3-249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Pantelic M, Steinert J, Park J, et al. , 2017. Systematic review protocol: a systematic review of interventions aiming to reduce self-stigma among people living with HIV and key populations affected by HIV in low and middle income countries [Internet]. Available: https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=83972 [Accessed 9 Oct 2018].
- 40. Logie C, Gadalla TM. Meta-analysis of health and demographic correlates of stigma towards people living with HIV. AIDS Care 2009;21:742–53. 10.1080/09540120802511877 [DOI] [PubMed] [Google Scholar]
- 41. Tsai AC, Bangsberg DR, Weiser SD. Harnessing poverty alleviation to reduce the stigma of HIV in sub-Saharan Africa. PLoS Med 2013;10:e1001557 10.1371/journal.pmed.1001557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Brown L, Macintyre K, Trujillo L. Interventions to reduce HIV/AIDS stigma: what have we learned? [Internet]. Vol. 15, AIDS education and prevention: official publication of the International Society for AIDS Education. New Orleans 2003. [DOI] [PubMed] [Google Scholar]
- 43. Fraser MW, Richman JM, Galinsky MJ, et al. Intervention research: developing social programs. New York: Oxford University Press, 2009. [Google Scholar]
- 44. Deeks JJ, Higgins J, Altman DG. Analysing Data and Undertaking Meta‐Analyses : Higgins JPT, Green S, Cochrane handbook for systematic reviews of interventions: cochrane book series [Internet. The Cochrane Collaboration, 2008: 243–96. [Google Scholar]
- 45. Murray J, Farrington DP, Eisner MP. Drawing conclusions about causes from systematic reviews of risk factors: the Cambridge quality checklists. J Exp Criminol 2009;5:1–23. 10.1007/s11292-008-9066-0 [DOI] [Google Scholar]
- 46. BMJ , 2017. Reporting patient and public involvement in research [Internet]. Available: https://drive.google.com/file/d/14vnXwTJ2CDn2KQsuNpuEnSwad69gc7dR/view
- 47. Higgins JPT, Green S, 2011. Cochrane handbook for systematic reviews of interventions | cochrane training [Internet]. The cochrane collaboration. Available: https://training.cochrane.org/handbook [Accessed 22 Oct 2018].
- 48. Littell JH, Corcoran J, Pillai V. Systematic reviews and meta-analysis. Oxford University Press, 2008. [Google Scholar]
- 49. Bronfenbrenner U. The ecology of human development: experiments by nature and design. Cambridge MA: Harvard University Press, 1979. [Google Scholar]
- 50. Goldberg AE, Smith JZ, Stigma SJZ. Stigma, social context, and mental health: lesbian and gay couples across the transition to adoptive parenthood. J Couns Psychol 2011;58:139–50. 10.1037/a0021684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Rongkavilit C, Wang B, Naar-King S, et al. Motivational interviewing targeting risky sex in HIV-positive young Thai men who have sex with men. Arch Sex Behav 2015;44:329–40. 10.1007/s10508-014-0274-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Go VF, Frangakis C, Minh NL, et al. Efficacy of a multi-level intervention to reduce injecting and sexual risk behaviors among HIV-infected people who inject drugs in Vietnam: a Four-Arm randomized controlled trial. PLoS One 2015;10:1–19. 10.1371/journal.pone.0125909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Low C, Pop-Eleches C, Rono W, et al. The effects of home-based HIV counseling and testing on HIV/AIDS stigma among individuals and community leaders in Western Kenya: evidence from a cluster-randomized trial. AIDS Care 2013;25(Suppl 1):S97–S107. 10.1080/09540121.2012.748879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Tshabalala J, Visser M. Developing a cognitive behavioural therapy model to assist women to deal with HIV and stigma. South African Journal of Psychology 2011;41:17–28. 10.1177/008124631104100103 [DOI] [Google Scholar]
- 55. Tam V, Larsson M, Pharris A, et al. Peer support and improved quality of life among persons living with HIV on antiretroviral treatment : A randomised controlled trial from. Health Qual Life Outcomes [Internet] 2012;10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Bonell C, Imrie J. Behavioural interventions to prevent HIV infection: rapid evolution, increasing rigour, moderate success. Br Med Bull 2001;58:155–70. 10.1093/bmb/58.1.155 [DOI] [PubMed] [Google Scholar]
- 57. Mundell JP. The impact of structured support groups for pregnant South African women recently diagnosed HIV positive. University of Pretoria, 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Nyamathi A, Ekstrand M, Salem BE, et al. Impact of Asha intervention on stigma among rural Indian women with AIDS. West J Nurs Res 2013;35:867–83. 10.1177/0193945913482050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Lifson AR, Workneh S, Hailemichael A, et al. Implementation of a peer HIV community support worker program in rural Ethiopia to promote retention in care. J Int Assoc Provid AIDS Care 2017;16:75–80. 10.1177/2325957415614648 [DOI] [PubMed] [Google Scholar]
- 60. Peltzer K, Weiss SM, Soni M, et al. A cluster randomized controlled trial of lay health worker support for prevention of mother to child transmission of HIV (PMTCT) in South Africa. AIDS Res Ther 2017;14:1–12. 10.1186/s12981-017-0187-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Prinsloo CD, Greeff M, Kruger A, et al. HIV stigma experiences and stigmatisation before and after a HIV stigma-reduction community "hub" intervention. Afr J AIDS Res 2017;16:203–13. 10.2989/16085906.2017.1349683 [DOI] [PubMed] [Google Scholar]
- 62. Bhatta DN, Liabsuetrakul T. Efficacy of a social self-value empowerment intervention to improve quality of life of HIV infected people receiving antiretroviral treatment in Nepal: a randomized controlled trial. AIDS Behav 2017;21:1620–31. 10.1007/s10461-016-1546-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Chidrawi HC, Greeff M, Temane QM, et al. HIV stigma experiences and stigmatisation before and after an intervention. Health SA Gesondheid 2016;21:196–205. 10.4102/hsag.v21i0.953 [DOI] [Google Scholar]
- 64. Uys L, Chirwa M, Kohi T, et al. Evaluation of a health setting-based stigma intervention in five African countries. AIDS Patient Care STDS 2009;23:1059–66. 10.1089/apc.2009.0085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Maluccio JA, Wu F, Rokon RB, et al. Assessing the impact of food assistance on stigma among people living with HIV in Uganda using the HIV/AIDS stigma Instrument-PLWA (HASI-P). AIDS Behav 2017;21:766–82. 10.1007/s10461-016-1476-9 [DOI] [PubMed] [Google Scholar]
- 66. Wagner GJ, Ghosh-Dastidar B, Garnett J, et al. Impact of HIV antiretroviral therapy on depression and mental health among clients with HIV in Uganda. Psychosom Med 2012;74:883–90. 10.1097/PSY.0b013e31826629db [DOI] [PubMed] [Google Scholar]
- 67. Turan B, Stringer KL, Onono M, et al. Linkage to HIV care, postpartum depression, and HIV-related stigma in newly diagnosed pregnant women living with HIV in Kenya: a longitudinal observational study. BMC Pregnancy Childbirth 2014;14:1–10. 10.1186/s12884-014-0400-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Tsai AC, Bangsberg DR, Bwana M, et al. How does antiretroviral treatment attenuate the stigma of HIV? Evidence from a cohort study in rural Uganda. AIDS Behav 2013;17:2725–31. 10.1007/s10461-013-0503-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Peltzer K, Ramlagan S. Perceived stigma among patients receiving antiretroviral therapy: a prospective study in KwaZulu-Natal, South Africa. AIDS Care 2011;23:60–8. 10.1080/09540121.2010.498864 [DOI] [PubMed] [Google Scholar]
- 70. Makoae LN, Portillo CJ, Uys LR, et al. The impact of taking or not taking ARVs on HIV stigma as reported by persons living with HIV infection in five African countries. AIDS Care 2009;21:1357–62. 10.1080/09540120902862576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Kalichman SC, Simbayi LC, Cloete A, et al. Measuring AIDS stigmas in people living with HIV/AIDS: the internalized AIDS-related stigma scale. AIDS Care 2009;21:87–93. 10.1080/09540120802032627 [DOI] [PubMed] [Google Scholar]
- 72. Tsai AC, Bangsberg DR, Kegeles SM, et al. Internalized stigma, social distance, and disclosure of HIV seropositivity in rural Uganda. Ann Behav Med 2013;46:285–94. 10.1007/s12160-013-9514-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: psychometric assessment of the HIV stigma scale. Res Nurs Health 2001;24:518–29. 10.1002/nur.10011 [DOI] [PubMed] [Google Scholar]
- 74. Tsai AC. Socioeconomic gradients in internalized stigma among 4,314 persons with HIV in sub-Saharan Africa. AIDS Behav 2015;19:270–82. 10.1007/s10461-014-0993-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Pantelic M, Sprague L, Stangl A. It’s not “all in your head”: critical knowledge gaps on internalized HIV stigma and a call for integrating social and structural conceptualizations, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Patel V, Burns JK, Dhingra M, et al. Income inequality and depression: a systematic review and meta-analysis of the association and a scoping review of mechanisms. World Psychiatry 2018;17:76–89. 10.1002/wps.20492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Hu Y, Lu H, Raymond HF, et al. Measures of condom and safer sex social norms and stigma towards HIV/AIDS among Beijing MSM. AIDS Behav 2014;18:1068–74. 10.1007/s10461-013-0609-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Griffiths KM, Carron-Arthur B, Parsons A, et al. Effectiveness of programs for reducing the stigma associated with mental disorders. A meta-analysis of randomized controlled trials. World Psychiatry 2014;13:161–75. 10.1002/wps.20129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Wood L, Byrne R, Varese F, et al. Psychosocial interventions for internalised stigma in people with a schizophrenia-spectrum diagnosis: a systematic narrative synthesis and meta-analysis. Schizophr Res 2016;176:291–303. 10.1016/j.schres.2016.05.001 [DOI] [PubMed] [Google Scholar]
- 80. Earnshaw VA, Smith LR, Cunningham CO, et al. Intersectionality of internalized HIV stigma and internalized substance use stigma: implications for depressive symptoms. J Health Psychol 2015;20:1083–9. 10.1177/1359105313507964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. SANAC , 2017. South Africa’s national strategic plan for HIV, TB and STIs 2017-2022 [Internet]. Available: http://sanac.org.za/wp-content/uploads/2017/05/NSP_FullDocument_FINAL.pdf
- 82. Pantelic M, Stegling C, Shackleton S, et al. Power to participants: a call for person-centred HIV prevention services and research. J Int AIDS Soc 2018;21:e25167 10.1002/jia2.25167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Ghosal S, Jana S, Mani A, et al. Sex workers, Self-Image and stigma: evidence from Kolkata Brothels, 2016. [Google Scholar]
- 84. Thirumurthy H, Zivin JG, Goldstein M. The economic impact of AIDS Treatment: labor supply in Western Kenya. J Hum Resour 2008;43:511–52. [PMC free article] [PubMed] [Google Scholar]
- 85. d’Adda G, Goldstein M, Zivin JG, et al. ARV treatment and time allocation to household tasks: evidence from Kenya. African Dev Rev 2009;21:180–208. 10.1111/j.1467-8268.2009.00207.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Westbrook L, Bauman L. Perceived stigma of HIV/AIDS scale. Bronx New York: Albert Einstein College of Medicine, 1996. [Google Scholar]
- 87. Visser MJ, Kershaw T, Makin JD, et al. Development of parallel scales to measure HIV-related stigma. AIDS Behav 2008;12:759–71. 10.1007/s10461-008-9363-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Genberg BL, Kawichai S, Chingono A, et al. Assessing HIV/AIDS stigma and discrimination in developing countries. AIDS Behav 2008;12:772–80. 10.1007/s10461-007-9340-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Ekstrand ML, Bharat S, Ramakrishna J, et al. Blame, symbolic stigma and HIV misconceptions are associated with support for coercive measures in urban India. AIDS Behav 2012;16:700–10. 10.1007/s10461-011-9888-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Steward WT, Chandy S, Singh G, et al. Depression is not an inevitable outcome of disclosure avoidance: HIV stigma and mental health in a cohort of HIV-infected individuals from southern India. Psychol Health Med 2011;16:74–85. 10.1080/13548506.2010.521568 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2018-001285supp001.pdf (626.3KB, pdf)
bmjgh-2018-001285supp002.pdf (423KB, pdf)