Abstract
Background
Injury of the inferior alveolar nerve (IAN) sustained during surgical removal of an impacted lower third molar may cause paresthesia of the lower lip, chin, lower gingivae and anterior teeth. Lingual nerve (LN) injuries may result in ipsilateral paresthesia of the anterior two thirds of the tongue, mucosa of floor of mouth and lingual gingivae. A close anatomic relationship between the roots of the third molar and mandibular canal places the IAN at risk of damage.
Purpose
The primary aim of this retrospective audit was to ascertain the incidence of IAN and LN damage after mandibular third molar surgery in National Dental Centre Singapore. A secondary aim was to identify the contributory factors for the risk of IAN and LN nerve injury on the basis of the data collected.
Methods
This retrospective audit included 1276 mandibular third molar surgical removals performed in the local anesthesia operating theatre (LAOT) at the National Dental Centre Singapore (NDCS) from April to December 2013. Data included patient details, clinical characteristics, and 1 week postoperative presence/absence of sensory alteration as reported by the patient.
Results
Summary of results- Out of 1276 third molar sites audited, 8 (0.62%) sites had altered sensation of the IAN and 1 (0.078%) had altered sensation of the LN at 1 week postoperative review.
Conclusion
The incidence of IAN injury (0.62%) and lingual Nerve injury (0.08%) after one week from surgery in our audit was low compared to similar studies. This retrospective audit did not show any correlation of nerve injury to age, gender, race, site, angulation of tooth, grade of operator, removal of bone or tooth division. There was no single radiological sign associated with paresthesia, although the most common radiological signs were interruption of the canal line and darkening of the roots.
Keywords: Third molar, Inferior alveolar nerve, Lingual nerve, Altered sensation
Background
Inferior alveolar nerve (IAN) and lingual nerve (LN) injuries in mandibular third molar (3M) surgeries are uncommon but are troublesome complications when they do occur, and result in partial or total paresthesia of the ipsilateral lower lip and chin, and the anterior two-thirds of the tongue, respectively. The incidence of IAN sensory disturbance about 1 week after mandibular 3M surgery in prospective cohort studies in the English literature ranges from 0.6 to 6.0% [1–9], and the incidence of LN sensory disturbance at 1 week after mandibular 3M surgery in prospective cohort studies ranges from 0.7 to 11.5% [2–7, 9–13]. The majority of nerve injuries results in transient paresthesia, but 0.9% of IAN injuries [7] and 0.2% LN injuries [2] continue to persist at 6 months postoperatively.
Injury of the IAN results in sensory alteration in the ipsilateral chin, lip (vermilion, skin and mucosa), and labial–buccal alveolar mucosa of the mandibular anterior teeth. Injury of the LN is manifested by sensory alteration in the ipsilateral anterior two-thirds of the tongue including the dorsum, lateral and ventral surfaces, floor of the mouth and lingual alveolar mucosa of the mandibular arch.
Sensory disturbance has been described as numbness, sensation of swelling, tightness, pulling, sometimes as tingling, pins and needles or electric sensation. Rarely altered sensation may be described as pain or burning sensation and may qualify in some cases as neuropathic pain. Sensory loss in the IAN is associated with functional disability such as lip-drooling, lip-biting and speech difficulties, while that in LN manifests as loss of taste, tongue-biting, speech difficulties and difficulty controlling food when eating.
Aim
The primary aim of this retrospective audit was to determine the incidence of IAN and LN injury after surgical removal of mandibular third molars. A secondary aim was to identify the contributing factors for nerve injury.
Materials and Methods
A retrospective audit was conducted of mandibular third molar surgeries performed in the local anesthesia operating theater (LAOT) at the National Dental Centre Singapore (NDCS) over 9 months from April to December 2013. Consecutive patients who had undergone removal of mandibular 3Ms under local anesthesia in the LAOT were included in this study to a total of 1276 mandibular third molars. Only patients who presented for the 1 week postoperative review were included. All patients were first reviewed after 1 week, and those with numbness were reviewed further after 1, 3 and 6 months whenever possible.
Inclusion criteria included patients of at least 14 years of age, any race or gender, who underwent surgical removal of mandibular 3Ms under local anesthesia. Exclusion criteria included preexisting sensory alteration for any reason, previous mandibular surgery (e.g., cyst enucleation, orthognathic surgery) or fracture likely to have affected the IAN.
A list of patients who had undergone mandibular 3Ms surgery in the NDCS LAOT during the time stipulated was compiled from the LAOT register. Clinical records of these patients were reviewed and entered into a data collection form, which was compiled in an MS Excel® database. Data collected included patient details (gender, age, race), FDI (Federation Dentaire Internationale) tooth number, type and degree of impaction (complete bony, partial bony or soft tissue), imaging performed (dental panoramic radiograph [DPT], intraoral periapical radiograph or cone beam computed tomography [CBCT]), radiological relationship of the third molar roots to the mandibular canal, details of surgery (surgery date, surgeon’s grade, removal whole or with tooth division) and 1 week postoperative presence/absence of sensory alteration as reported by the patient. Standard digital DPTs which were taken preoperatively were analyzed for relationship between the mandibular canal and the roots of the 3M. The radiographic features studied were darkening of root (DR), loss of white lines (LC) (interruption of either superior or inferior lines of the inferior alveolar canal), narrowing of canal (NC), narrowing of root (NR), diversion of root (DVR) and diversion of canal (DVC).
Continuous variables were summarized as mean and standard deviation, and categorical variables were summarized as a number and percentage. The Wilcoxon rank sum test was used for continuous variables, and the Fisher’s exact test was used for categorical variables in comparison with two groups. All statistical analyses were performed using SAS version 9.4 (SAS@9.4 Inc, Cary, NC, USA) (Figs. 1, 2).
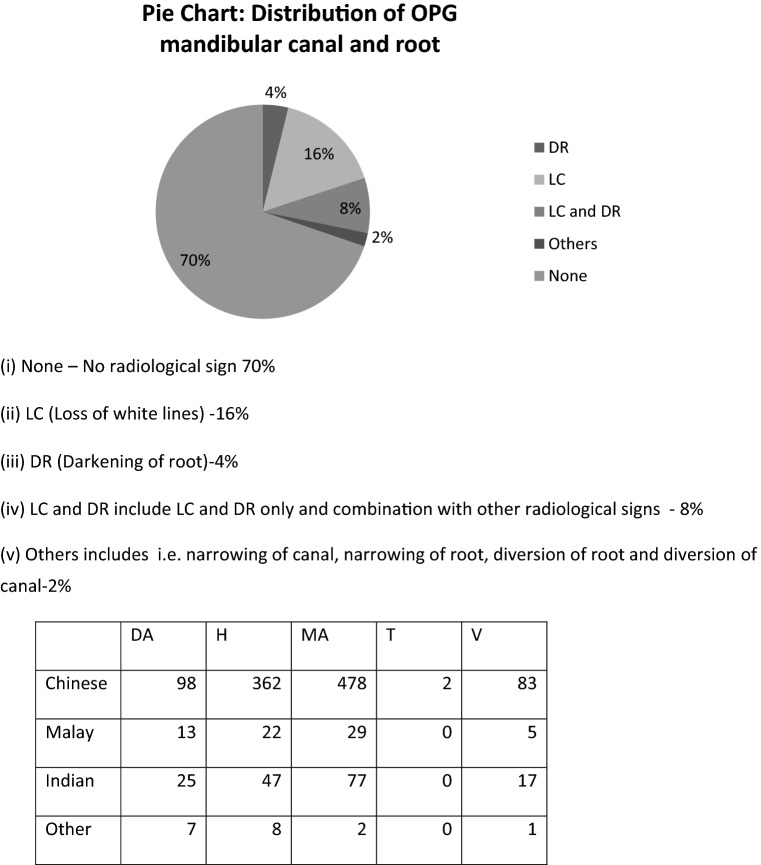
Fig. 1.
Distribution of OPG mandibular canal and root
Fig. 2.
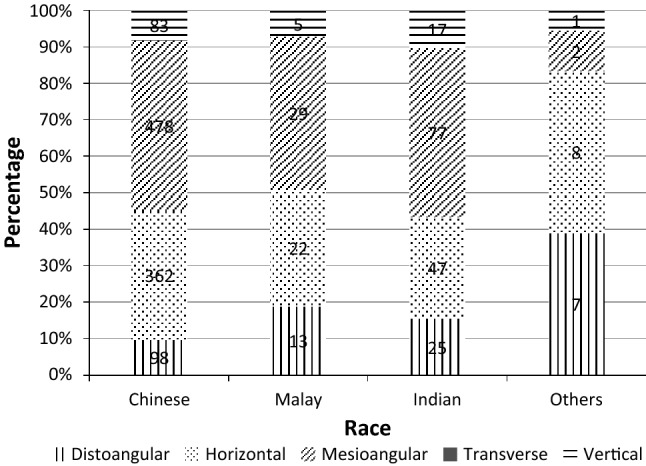
Type of impaction by race (number in middle of the bar is count for each category)
Results
A total of 1276 sites of mandibular 3M surgeries performed from April to December 2013 were audited. Table 1 shows the patient demographics. The mean age was 30.5 years with a range of 15–80 years. The majority were female (818, 64.1%). The ethnic proportions roughly reflected the population ethnicity in Singapore; Chinese formed the largest ethnic group by proportion. There were slightly more left-sided mandibular 3Ms [#38] than right-sided mandibular 3Ms [#48]. The great majority of 3Ms were excised with a combination of bone removal and tooth sectioning/division. Table 2 shows the tooth characteristics. Dental panoramic radiographs were the main imaging used. The majority of 3Ms by depth of impaction were partially covered by bone followed by teeth completely covered by bone. By type of impaction, the most common were mesioangular impactions followed in decreasing order by horizontal impactions, distoangular impactions, vertical impactions and transverse impactions. Radiographic signs of proximity of the mandibular canal were absent in the majority of cases. When present, the most common radiographic signs of proximity to the mandibular canal were loss of white line alone, loss of white line with root darkening together and darkening of the root alone.
Table 1.
Patient characteristics
| Variablea | Total (N = 1276) | No IAN numbness (N = 1268) | IAN numbness (N = 8) | p value* |
|---|---|---|---|---|
| Age, mean (SD) | 30.5 (10.2) | 30.5 (10.2) | 30.0 (10.6) | 0.890 |
| Age, median (min–max) | 28.0 (15.0–80.0) | 28.0 (15.0–80.0) | 26.5 (21.0–55.0) | 0.924 |
| Gender, n (%) | 1.000 | |||
| Female | 818 (64.1%) | 813 (64.1%) | 5 (62.5%) | |
| Male | 458 (35.9%) | 455 (35.9%) | 3 (37.5%) | |
| Race, n (%) | 0.001 | |||
| Chinese | 1023 (80.2%) | 1020 (80.4%) | 3 (37.5%) | |
| Malays | 166 (13.0%) | 163 (12.9%) | 3 (37.5%) | |
| Indians | 69 (5.4%) | 69 (5.4%) | 0 (0.0%) | |
| Others | 18 (1.4%) | 16 (1.3%) | 2 (25.0%) | |
| Site, n (%) | 0.292 | |||
| Left | 668 (52.4%) | 662 (52.2%) | 6 (75.0%) | |
| Right | 607 (47.7%) | 606 (47.8%) | 2 (25.0%) | |
| Surgery, n (%) | 1.000 | |||
| BR with TD | 1184 (92.8%) | 1176 (92.7%) | 8 (100%) | |
| BR without TD | 83 (6.5%) | 83 (6.6%) | 0 (0.0%) | |
| No BR or TD | 9 (0.7%) | 9 (0.7%) | 0 (0%) | |
IAN inferior alveolar nerve, BR bone removal, TD tooth division
*p value was calculated using Wilcoxon rank sum test for continuous variables and Fisher’s exact test for categorical variables
aContinuous variables (i.e., age) were summarized in mean (standard deviation) and categorical variables were summarized in count (percentage)
Table 2.
Clinical characteristics
| Variablea | Total (N = 1276) | No IAN numbness (N = 1268) | IAN numbness (N = 8) | p value* |
|---|---|---|---|---|
| Radiography, n (%) | ||||
| OPG, Yes | 1272 (99.7%) | 1264 (99.7%) | 8 (100%) | 1.000 |
| CBCT, Yes | 3 (0.2%) | 3 (0.2%) | 0 (0.0%) | 1.000 |
| PA, Yes | 5 (0.4%) | 5 (0.4%) | 0 (0.0%) | 1.000 |
| Depth of impaction, n (%) | 0.035 | |||
| Partial bony | 989 (77.5%) | 986 (77.8%) | 3 (37.5%) | |
| Complete bony | 278 (21.8%) | 273 (21.5%) | 5 (62.5%) | |
| Soft tissue | 9 (0.7%) | 9 (0.7%) | 0 (0.0%) | |
| Type of impaction, n (%) | 0.632 | |||
| Mesioangular | 576 (45.1%) | 573 (45.2%) | 3 (37.5%) | |
| Horizontal | 439 (34.4%) | 435 (34.3%) | 4 (50.0%) | |
| Distoangular | 143 (11.2%) | 143 (11.3%) | 0 (0.0%) | |
| Vertical | 106 (8.3%) | 105 (8.3%) | 1 (11.1%) | |
| NA | 10 (0.8%) | 10 (0.8%) | 0 (0.0%) | |
| Transverse | 2 (0.2%) | 2 (0.2%) | 0 (0.0%) | |
| OPG canal and root | 0.001 | |||
| None | 890 (69.8%) | 889 (70.1%) | 1 (12.5%) | |
| Loss of white line (LC) | 205 (16.1%) | 202 (15.9%) | 3 (37.5%) | |
| LC and DR | 106 (8.3%) | 105 (8.3%) | 1 (12.5%) | |
| Darkening of root (DR) | 49 (3.8%) | 47 (3.7%) | 2 (25.0%) | |
| Others | 26 (2.0%) | 25 (2.0%) | 1 (12.5%) | |
| Surgeon’s grade | 1.000 | |||
| Consultant | 908 (71.2%) | 902 (71.1%) | 6 (75.0%) | |
| Registrar | 273 (21.4%) | 271 (21.4%) | 2 (25.0%) | |
| Trainee | 95 (7.5%) | 95 (7.5%) | 0 (0.0%) | |
| Radiological signal | 0.001 | |||
| No | 890 (69.8%) | 889 (70.1%) | 1 (12.5%) | |
| Yes | 386 (30.3%) | 379 (29.9%) | 7 (87.5%) | |
IAN inferior alveolar nerve
*p value was calculated using Fisher’s exact test for categorical variable
aCategorical variable was summarized in count (percentage)
Of 1276 3M sites audited, 8 (0.62%) sites had altered sensation of the IAN and 1 (0.08%) had altered sensation of the LN at 1 week postoperatively. Of the 8 patients with IAN sensory disturbance, 1 had complete recovery after 6 weeks and 4 had complete recovery in 3 months. Three were lost to follow up between 6 weeks and 3 months. These 3 patients were contacted by telephone: 2 had complete recovery in 3 months and 1 had persistent sensory disturbance in left side of lower lip even after 1 year. The incidence of permanent numbness of the IAN was 1 out of 1276 (0.08%). Of the 8 IAN cases with sensory disturbance, 6 were operated by Consultant grade and 2 were operated by Registrar grade surgeons.
Of the 8 sites with IAN sensory disturbance, 5 (62.5%) were complete bony impacted and 3 (37.5%) were partially bony impacted. Of the 8 sites of IAN sensory disturbance, 3 had both loss of white line (LC) and root darkening (DR), 2 had only DR, 1 had only LC, 1 had diversion of canal, and 1 had no radiographic feature. IAN sensory disturbance correlated strongly with the presence of at least 1 radiological sign or a combination of signs (87.5%) in our audit.
Comparison between the no IAN numbness group and IAN numbness group showed no significant differences in the grade of the operator, type of angulation impaction, need for tooth division during excision, gender or race.
LN paresthesia was present only in 1 site, and the type of impaction was distoangular, and the tooth was removed with bone removal and tooth sectioning. The only patient with LN sensory disturbance was also lost to follow up after 2 weeks. However, the patient was contacted over the phone and it was confirmed that the patient had complete recovery after 3 months. Permanent disturbances were absent for LN numbness in our study
Discussion
The incidence of IAN damage after lower 3M removal ranges from 0.5% [14] to approximately 8% [3]. A review of prospective, large sample (at least 300 operations) observational studies not including the lingual split technique, that focused on IAN injury in 3M surgery, resulted in an incident range of 1.3% to 3.6% at 1 week after surgery [2, 5, 6, 8, 9].
In this study, removal of impacted mandibular 3Ms by buccal bone removal without raising a lingual flap resulted in very low incidence of lingual nerve sensory alteration 0.08% (1/1276 teeth) and IAN sensory alteration in 0.62% (8/1276 teeth) at 1 week after surgery. The patient with LN paresthesia had complete spontaneous recovery within 3 months.
The incidence of temporary sensory disturbance was lower than most other studies.
Gulicher et al. [7] reported incidences of 3.6% IAN paresthesia and 2.1% LN paresthesia following removal of impacted mandibular third molars. Wofford and Miller [2] reported an incidence of 3.3% IAN paresthesia in their prospective study, also concluded that the incidence of paresthesia of IAN and LN is more likely to occur with complete bony impacted mandibular molars, mesioangular impaction, impacted molars with the crown at the cervical junction of the adjacent second molars, when burs are used to remove bone and when roots are in close proximity to the mandibular canal. Bataineh et al. [9] reported incidences of 3.9% IAN paresthesia and 2.6% LN paresthesia. Their statistical analysis showed that paresthesia was unrelated to age, gender, site, angulation of tooth impaction, grade of operator, removal of bone or tooth division, which is consistent with the findings of our audit.
In 2013, Smith presented a clinical study on 1000 patients, removing 1589 impacted 3Ms [15]. Of the 1589 3Ms extracted, 466 (29%) demonstrated a distant relationship of their apices to the mandibular canal, 869 (55%) were close to the canal, and only 254 (16%) were deemed to be intimate to the canal by radiography. After surgery, 39 patients (3.9%) reported neurosensory disturbance in the IAN in 40 sites (2.5%). Seven patients (0.7%) sustained permanent sensory loss. The incidence of IAN neurosensory deficit was highest with horizontal impaction (4.7%) and lowest when the teeth were vertically impacted (0.9%). [Ashok—should use % based on impacted tooth site not on patient. Are numbers for impaction by patient or by site?]
Rafel et al. [16] reported the incidence of injury to IAN after 3M removal to be 0.35–8.4%, with risk factors that may increase the injury to the nerve including patient age over 24 years, horizontal impaction in close radiographic proximity to the mandibular canal and extraction by trainee surgeons.
Clinical observation of the neurovascular bundle exposed in the socket during surgery indicates an increased risk of postoperative IAN sensory disturbance. Tay and Go found that an intact IAN bundle observed during 3M surgery indicated an intimate relationship with the 3M and had a 20% risk of postoperative paresthesia, and with a 70% chance of recovery within 1 year [17].
Kim et al. [18] showed that the significant factors for neurosensory deficits according to the panoramic radiograph were the 5 radiographic superimposition signs: darkening of roots, deflection of roots, narrowing of roots, dark and bifid apex of roots and narrowing of the canal were significantly associated with neurosensory deficits of the IAN after impacted mandibular third molar extraction. The number of subjects in this study was significantly large (12,842 patients), increasing the reliability of their results.
In our audit, there was no single important radiological sign in patients who had postoperative paresthesia in contrast to diversion of mandibular canal near the third molar roots by Valmaseda et al. [8]. The interruption of white line of the mandibular canal and darkening of the roots were the most common radiological signs noted in our audit. Valmaseda’s study also suggested patients’ age, presence of radiological relationship between 3Ms and the mandibular canal, deflection of mandibular canal and need for distal bone as predictors for IAN damage [8], which is in contrast to the findings in our audit where statistical analysis revealed that paresthesia was unrelated to age, site, angulation of tooth, presence of any particular radiological sign.
Dental panoramic radiography was the radiological investigation of choice before 3M surgery. The radiographic signs indicative of IAN injury are identifiable on this radiograph, but like other conventional radiographs, it is unable to give information in 3 dimensions [19]. The advent of 3-dimensional imaging using cone beam computed tomography (CBCT) allows greater clarity of the relationship of the mandibular canal with the impacted or buried mandibular third molar. The use of CBCT has been shown to be helpful in experienced hands in avoiding encroaching on the IAN intraoperatively [20]. The use of CBCT should be considered for patients who have positive signs of proximity of the 3M root to the mandibular canal.
IAN paresthesia is usually temporary, and the majority of cases recover within 6 months [21]. The risk of permanent injury, in which sensory alteration lasts longer than 1 year, is less than 1% [7]. In most cases, complete recovery of IAN sensory disturbance occurs 6–8 weeks after the trauma, although it may take up to 24 months.
Limitations of study include the inability to study certain parameters given the retrospective nature of this audit, loss of data due to dropouts from follow-up and the exclusion of patients who had not returned for 1 week postoperative follow-up.
Conclusion
The incidence of IAN injury (0.62%) and lingual Nerve injury (0.08%) after 1 week from surgery in our audit was low compared to similar studies.
Removal of impacted mandibular third molars by buccal bone removal without raising a lingual flap resulted in very low incidence of lingual nerve damage. No permanent LN sensitivity disturbances were found.
Seven patients with IAN paresthesia had temporary sensory disturbance which resolved complete and spontaneously between 6 weeks to 6 months. Only one patient (0.08%) had permanent numbness (numbness for over a year).
This retrospective audit did not show any correlation of nerve injury to age, gender, race, site, angulation of tooth, grade of operator, removal of bone or tooth division.
There was no single radiological sign associated with paresthesia, although the most common radiological signs were interruption of the canal line and darkening of the roots.
References
- 1.Osborn TP, Frederickson G, Small IA, Torgerson TS. A prospective study of complications related to mandibular third molar surgery. J Oral Maxillofac Surg. 1985;43:767–769. doi: 10.1016/0278-2391(85)90331-3. [DOI] [PubMed] [Google Scholar]
- 2.Wofford DT, Miller RI. Prospective study of dysesthesia following odontectomy of impacted mandibular third molars. J Oral Maxillofac Surg. 1987;45:15–19. doi: 10.1016/0278-2391(87)90080-2. [DOI] [PubMed] [Google Scholar]
- 3.Rood JP. Permanent damage to inferior alveolar and lingual nerves during the removal of impacted mandibular third molars. Comparison of two methods of bone removal. Br Dent J. 1992;172:108–110. doi: 10.1038/sj.bdj.4807777. [DOI] [PubMed] [Google Scholar]
- 4.Carmichael FA, McGowan DA. Incidence of nerve damage following third molar removal: a West of Scotland Oral Surgery Research Group Study. Br J Oral Maxillofac Surg. 1992;30:78–82. doi: 10.1016/0266-4356(92)90074-S. [DOI] [PubMed] [Google Scholar]
- 5.Schultze-Mosgau S, Reich RH. Assessment of inferior alveolar and lingual nerve disturbances after dentoalveolar surgery, and of recovery of sensitivity. Int J Oral Maxillofac Surg. 1993;22:214–217. doi: 10.1016/S0901-5027(05)80638-1. [DOI] [PubMed] [Google Scholar]
- 6.Brann CR, Brickley MR, Shepherd JP. Factors influencing nerve damage during lower third molar surgery. Br Dent J. 1999;186:514–516. doi: 10.1038/sj.bdj.4800155. [DOI] [PubMed] [Google Scholar]
- 7.Gulicher D, Gerlach KL. Sensory impairment of the lingual and inferior alveolar nerves following removal of impacted mandibular third molars. Int J Oral Maxillofac Surg. 2001;30:306–312. doi: 10.1054/ijom.2001.0057. [DOI] [PubMed] [Google Scholar]
- 8.Valmaseda-Castellon E, Berini-Aytes L, Gay-Escoda C. Inferior alveolar nerve damage after lower third molar surgical extraction: a prospective study of 1117 surgical extractions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92:377–383. doi: 10.1067/moe.2001.118284. [DOI] [PubMed] [Google Scholar]
- 9.Bataineh AB. Sensory nerve impairment following mandibular third molar surgery. J Oral Maxillofac Surg. 2001;59:1012–1017. doi: 10.1053/joms.2001.25827. [DOI] [PubMed] [Google Scholar]
- 10.Mason DA. Lingual nerve damage following lower third molar surgery. Int J Oral Maxillofac Surg. 1988;17:290–294. doi: 10.1016/S0901-5027(88)80005-5. [DOI] [PubMed] [Google Scholar]
- 11.Blackburn CW, Bramley PA. Lingual nerve damage associated with the removal of lower third molars. Br Dent J. 1989;167:103–107. doi: 10.1038/sj.bdj.4806922. [DOI] [PubMed] [Google Scholar]
- 12.Robinson PP, Smith KG. Lingual nerve damage during lower third molar removal: a comparison of two surgical methods. Br Dent J. 1996;180:456–461. doi: 10.1038/sj.bdj.4809126. [DOI] [PubMed] [Google Scholar]
- 13.Valmaseda-Castellon E, Berini-Aytes L, Gay-Escoda C. Lingual nerve damage after third lower molar surgical extraction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:567–573. doi: 10.1067/moe.2000.110034. [DOI] [PubMed] [Google Scholar]
- 14.Sisk AL, Hammer WB, Shelton DW, Joy ED., Jr Complications following removal of impacted lower third molars: the role of the experience of the surgeon. J Oral Maxillofac Surg. 1986;44:855–859. doi: 10.1016/0278-2391(86)90221-1. [DOI] [PubMed] [Google Scholar]
- 15.Smith WP. The relative risk of neurosensory deficit following removal of mandibular third molar teeth: the influence of radiography and surgical technique. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;115(1):18–24. doi: 10.1016/j.oooo.2012.03.017. [DOI] [PubMed] [Google Scholar]
- 16.Rafel S, Gintaras J (2014) Inferior alveolar nerve injury after mandibular third molar extraction: a literature review. J Oral Maxillofac Res 5(4):e1. 10.5037/jomr.2014.5401. URL: http://www.ejomr.org/JOMR/archives/2014/4/e1/v5n4e1ht.pdf [DOI] [PMC free article] [PubMed]
- 17.Tay AB, Go WS. Effect of exposed inferior alveolar neurovascular bundle during surgical removal of impacted lower third molars. J Oral Maxillofac Surg. 2004;62(5):592–600. doi: 10.1016/j.joms.2003.08.033. [DOI] [PubMed] [Google Scholar]
- 18.Kim JW, Cha IH, Kim SJ, Kim MR. Which risk factors are associated with neurosensory deficits of inferior alveolar nerve after mandibular third molar extraction? J Oral Maxillofac Surg. 2012;70(11):2508–2514. doi: 10.1016/j.joms.2012.06.004. [DOI] [PubMed] [Google Scholar]
- 19.Jhamb A, Dolas RS, Pandilwar PK, Mohanty S. Comparative efficacy of spiral computed tomography and orthopantomography in preoperative detection of relation of inferior alveolar neurovascular bundle to the impacted mandibular third molar. J Oral Maxillofac Surg. 2009;67(1):58–66. doi: 10.1016/j.joms.2008.06.014. [DOI] [PubMed] [Google Scholar]
- 20.Umar G, Obisesan O, Bryant C, Rood JP. Elimination of permanent injuries to the inferior alveolar nerve following surgical intervention of the “high risk” third molar. Br J Oral Maxillofac Surg. 2013;51:353–357. doi: 10.1016/j.bjoms.2012.08.006. [DOI] [PubMed] [Google Scholar]
- 21.Valmaseda-Castellón E, Berini-Aytés L, Gay-Escoda C. Inferior alveolar nerve damage after lower third molar surgical extraction: a prospective study of 1117 surgical extractions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92(4):377–383. doi: 10.1067/moe.2001.118284. [DOI] [PubMed] [Google Scholar]