Abstract
Background and Objectives
To compare the efficacy of three-dimensional (3D) miniplates with standard miniplates in the osteosynthesis of anterior mandibular fractures on the basis of bite force recordings and other clinical parameters.
Methods
A prospective randomized double-blinded clinical trial was carried out for the treatment of anterior mandibular fractures. In total, 20 patients were randomly divided into two groups of 2-mm 3D and standard titanium miniplates. The assessment of patients was done at weekly intervals for 6 weeks using bite force recordings and other clinical parameters.
Results
A statistically significant difference was found in the duration of surgery which was less in group A as compared to group B (p = 0.03). No significant difference was found in other clinical parameters.
Interpretation and Conclusion
The clinical outcome of both the 3D and standard miniplate systems in the present study was similar; however, the following advantages with the use of 3D miniplates can be highlighted:
Relatively lesser operating time.
Three-dimensional stability of the fracture site and simultaneous stabilization at superior and inferior borders in the fixation of mandibular fractures.
Keywords: 3D plate system, Mandibular fracture, Miniplate osteosynthesis, Bites force
Introduction
Open reduction with internal fixation (ORIF) methods are aimed to make patient return to normal function as soon as possible and to avoid the need for long-term IMF and to attain anatomic reduction, achieve good occlusion with excellent aesthetic results [1–4]. Champy’s miniplates and lag screws are less technique sensitive and produced consistently good results with regard to occlusion and are economical and also helped to avoid the need for long-term IMF [5]. Miniplates are comparatively better than lag screws for their ease of applications and have become more popular among maxillofacial surgeons [6, 7].
The 3D miniplate system is one of the newest internal semirigid fixations for maxillomandibular surgery in recent years. The disadvantage of semirigid fixation is that single miniplate does not provide sufficient stability for the fractures that are grossly displaced. The shortcomings of rigid and semirigid fixation led to the development of 3D miniplates [8], with interconnecting cross-struts. Unlike compression and reconstruction plates, their stability is not derived from the thickness of the plate. In combination with the monocortical screws fixed to the outer cortex, the rectangular plate forms cuboids, which possesses 3D stability. Although experimental studies on biomechanics have confirmed sufficient stability of the 3D plating system, only a few studies have previously reported clinical experiences with these plates in the treatment of mandibular fractures. The 3D plating systems are based on the principle of obtaining support through geometrically stable configuration. The quadrangle geometry of plate assures a good stability in three dimensions of fractured mandibular sites, since it offers good resistance against torque forces [9–13]. To our knowledge, no studies have been carried out for evaluating 3D plate with bite force as parameter. Considering this current concept of 3D miniplates, a study was carried out to evaluate the efficacy of 2-mm 3D titanium miniplates over 2-mm conventional miniplates in the management of anterior mandibular fractures with bite force as a parameter.
Materials and Methods
A prospective randomized double-blinded (patient and evaluator) clinical trial was done on 20 patients with anterior mandibular fractures in the department of OMFS in three hospitals of Hassan from November 2012 to October 2014, with predefined inclusion and exclusion criteria. After obtaining the ethical and research committee clearance, informed consents were obtained and patients were randomly assigned by lottery method to receive 2.0-mm titanium 3D miniplates (group A) and 2.0-mm titanium standard miniplates (group B) with each group containing 10 patients.
Inclusion criteria were as follows
Age of the patient 15–60 years with anterior mandibular fractures (from right to left mental foramen),
Dentition complete enough to apply Erich’s arch bars.
Exclusion criteria were as follows:
ASA 2 and above patients
Associated other facial bone fractures
The study design included a thorough case history taking in a case sheet which was custom made for the study. Demographic data collected consisted of gender, age, cause of fracture, duration between injury and surgery and the site of fracture.
Surgical Technique
All patients were given prophylactic antibiotic intravenously 30 min prior to the procedure followed by two times daily for 4 days. Surgical procedures were carried out under local/general anesthesia via nasotracheal intubation as required. Following the strict aseptic precautions, an appropriate intra-/extraoral approach (translabial, crevicular, extraoral in case of existing laceration) was selected, fracture site was exposed after the subperiosteal dissection, fractured segments were reduced, and after achieving satisfactory occlusion, MMF was done. Fixation was done using either a single 2.0-mm 3D plate/screw system (group A) (Fig. 1) or 2.0-mm standard miniplates/screw system applied along Champy’s lines of osteosynthesis’ (group B). MMF was released intraoperatively, and the passive occlusion was checked. A watertight wound closure was achieved. Duration of procedure from incision to wound closure was noted. Elastoplast pressure dressing was applied extraorally for 24 h postoperatively. Patients were advised to remain on soft diet for 2 weeks.
Fig. 1.
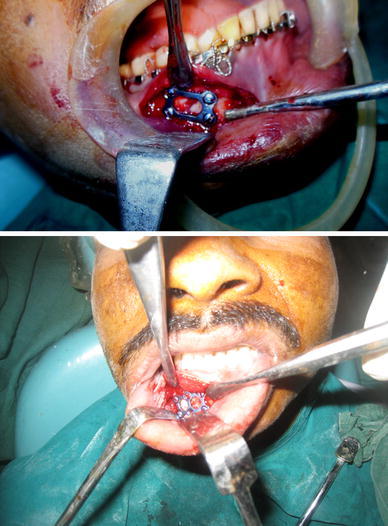
Fixation of mandibular fracture done using 3D titanium miniplate
Follow-Up
Patients were followed up for a period of 6 weeks at weekly intervals. During each follow-up, maximum bite forces at the incisor, canine and molar region were recorded by the blinded same examiner with the help of a bite force device consisting of a force transducer designed to measure the maximum force (in kg) exerted provided with a digital indicator (Fig. 2). All measurements were taken with the patient seated with the head upright, looking forward and in an unsupported natural head position. The instrument could be conveniently positioned between a single pair of antagonizing cusps in the region of incisors, right and left canines and first molars. The patients were advised to bite as forcefully as possible five times. The highest value was recorded and entered in the data sheet. Other clinical parameters evaluated at the aforesaid intervals consisted of the duration of the surgery, occlusal discrepancies, infection at the fracture site (based on CDC criteria for surgical site infection) [14].
Fig. 2.

Fixation of mandibular fracture done using titanium miniplate along Champy’s lines of osteosynthesis
Results were evaluated using appropriate statistical test, and p < 0.05 was considered statistically significant (Figs. 3, 4).
Fig. 3.
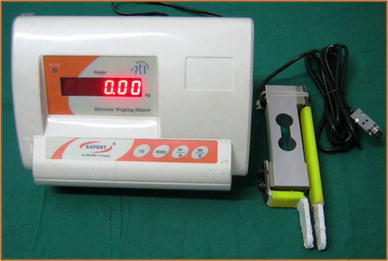
Bite force device with digital indicator
Fig. 4.

Bite force measurement with the patient seated with the head upright, looking forward and in an unsupported natural head position
Results
Among 20 patients enrolled in the study, 18 were males and two were females with 10 patients in each group. Demographic data, etiology, incidence and surgical access to fracture site are summarized in Table 1.
Table 1.
Demographic data, etiology, incidence and surgical access to fracture site
| Variables of the study | Group 1 (n = 12) | Group 2 (n = 12) |
|---|---|---|
| Demographic data | ||
| Gender | ||
| Male | 8 | 10 |
| Female | 2 | 0 |
| Average age (in years) | 37.60 ± 11.73 | 34.10 ± 10.86 |
| Etiology | ||
| RTA | 04 | 10 |
| Self-fall | 03 | 00 |
| Others | 03 | 00 |
| Incidence of fracture site | ||
| Symphysis | 01 | 01 |
| Parasymphysis | 09 | 09 |
| Surgical access | ||
| Translabial | 09 | 07 |
| Crevicular | 01 | 01 |
| Existing laceration | 00 | 02 |
The mean duration of surgery in group A was 52.50 ± 12.74 min with a range of 30–80 min and that in group B was 67.4 ± 14.9 min with a range of 45–90 min. There was a statistically significant difference between the two groups with p = 0.76 (Table 2).
Table 2.
Different parameters of the study
| Parameter | Group A (n = 10) | Group B (n = 10) | Significance |
|---|---|---|---|
| Duration of surgery (mean min) | 52.5 min | 67 min | S (p = 0.03) |
| Mouth opening | 3.5 cm | 3.2 cm | NS |
| Infection | 0 | 0 | NS |
| Segmental mobility | 0 | 0 | NS |
| Improper occlusion | 2 | 2 | NS |
| Oral hygiene | 12.4 | 14.6 | NS |
S statistically significant, NS statistically nonsignificant
Postoperatively two patients in each group reported with mild occlusal derangement which was managed with MMF of 14 days, after which all of them had functional occlusion. No instances of surgical site infection were encountered during the study in both groups (Table 2).
In both groups, incisor, canine and molar bite forces at the right and left side increased at progressive follow-up visits as compared with the preoperative recording, but no statistically significant difference was found (Table 3 and Figs. 5, 6).
Table 3.
Comparison of bite force at incisor region at different intervals of time
| Miniplates | Mean | SD | Unpaired t test | p value and significance | |
|---|---|---|---|---|---|
| Preoperative | Standard | 2.85 | 0.56 | 1.323 | 0.202 (NS) |
| 3D plates | 3.22 | 0.68 | |||
| 1 week | Standard | 3.24 | 0.54 | 1.707 | 0.105 (NS) |
| 3D plates | 3.66 | 0.56 | |||
| 2 week | Standard | 3.44 | 0.50 | 1.872 | 0.077 (NS) |
| 3D plates | 3.86 | 0.50 | |||
| 3 week | Standard | 3.67 | 0.42 | 1.829 | 0.084 (NS) |
| 3D plates | 4.05 | 0.50 | |||
| 4 week | Standard | 3.89 | 0.43 | 1.020 | 0.321 (NS) |
| 3D plates | 4.09 | 0.45 | |||
| 5 week | Standard | 4.03 | 0.36 | 0.472 | 0.643 (NS) |
| 3D plates | 4.11 | 0.39 | |||
| 6 week | Standard | 4.08 | 0.31 | 0.339 | 0.738 (NS) |
| 3D plates | 4.13 | 0.35 |
p < 0.05
NS nonsignificant
Fig. 5.
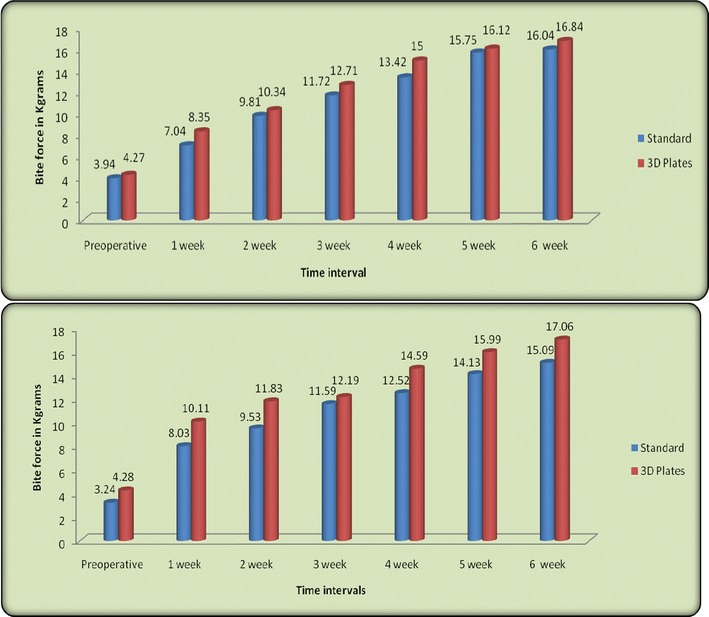
Comparison of bite force at right and left canine at different intervals of time
Fig. 6.
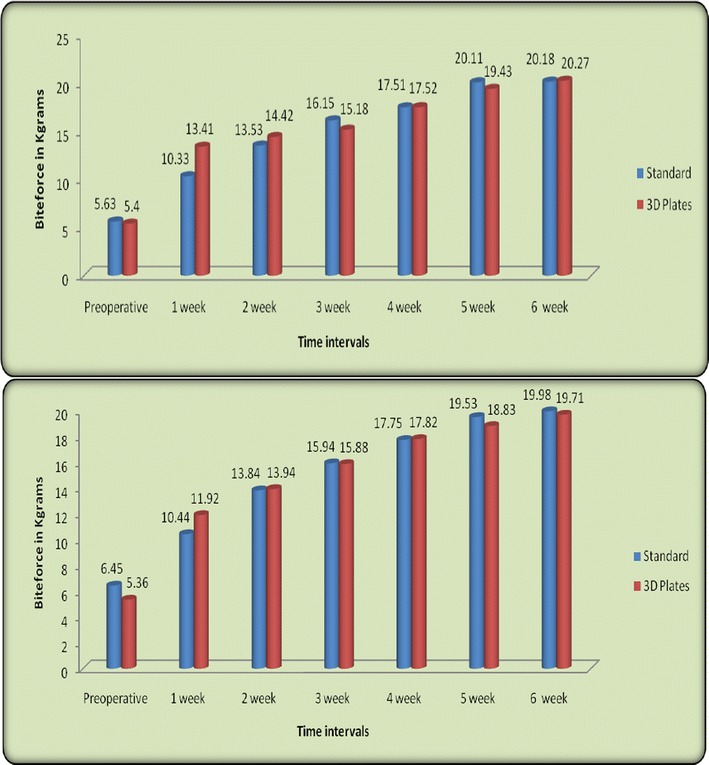
Comparison of bite force at right and left molar at different intervals of time
Discussion
Mostafa Farmand introduced new 3D plating system. This unique plate consists of square or rectangular units 2 × 2, 3 × 2, 4 × 2 holes and provides an increased torsional stability [15]. The 3D miniplate itself is a misnomer as the plates themselves are not three dimensional but hold the fracture segments rigidly by resisting the three-dimensional forces, namely shearing, bending and torsional forces acting on the fracture site in function [9–11, 17].
The use of 3D miniplates in mandibular fracture fixation has not yet become established. As per the recent survey by Gear et al. [17], among 104 AO/ASIF surgeons only 6% use these types of plates.
The bite force is related to number of factors, including tactile impulses, pain and pressure perception in the periodontal ligament, the number of teeth present and patient age, because reduction in bite force can occur with age owing to the age-dependent deterioration of the dentition. It has long been known that a neuromuscular protective mechanism occurs throughout the body. For instance, one of the first protective mechanisms that comes into play when a fracture occurs is “muscle splinting,” in which selective components of the neuromuscular system are activated or deactivated to remove the force from the damaged bone. In 1994, Tate et al. [18] stated that sufficient internal fixation hardware should be applied to resist the maximal force of mastication. Thus, they hypothesized that the stability of fractured segments would be ensured even under the full function of the masticatory system. The forces that must be countered in a mandibular fracture have been derived from maximal voluntary bite force measurement, which, in a healthy adult, could be about 15.3 kPa in the incisor and 48.3 and 49.3 kPa in the left and right molar regions, respectively. The amount of force generated by the patients with untreated as well as treated fractures is much less. Furthermore, one must remember that the data reported concerned the maximal voluntary bite force (i.e., the maximum bite force an individual can voluntarily generate) [19]. The amount of force used during functional activities would probably be much less. Hence, the fixation requirements, determined from the maximal voluntary bite force of noninjured subjects, might be inflated [18], and this fixation requirement is perhaps a semirigid form of fixation such as monocortical fixation [19]. In 2002, Gerlach and Schwarz in their study on bite force of treated mandibular fractures concluded that the maximal bite force in patients with mandibular fractures treated with miniplate osteosynthesis had reached only 31% at 1 week postoperatively compared with a healthy control group. These values had increased to 58% at 6 weeks postoperatively [20]. Similarly, in the present study, a positive correlation was found between the preoperative and postoperative weeks and the bite force for the anterior and posterior regions of the fracture sites in both groups. There was a progressive increase in the bite force readings from the preoperative period to 6 weeks postoperatively in both the groups. At other regions, the bite force in both the groups increased at the same rate with no statistically significant difference.
In our clinical experience, the 3D plate allows for almost no movements at the superior and inferior borders with manual torsional and bending forces. The screws were placed in a box configuration on both sides of the fracture rather than on a single line as in cases of miniplates, broad platform was created that may increase the resistance to torsional force along the axis of the plate. Therefore, to provide greater resistance against gap opening at the inferior border with biting forces, the locking system further increases the stability of the plate screw system [21, 22].
In conclusion, the results from this study suggest that 2.0-mm 3D miniplates provide three-dimensional stability and carry low morbidity and infection rates, supporting the studies carried out by other studies [16–22]. The mean duration of surgery directly reflects the ease/difficulty in the placement of particular plate, and operating time was less in case of 3D plating because of simultaneous stabilization at both superior and inferior borders supporting the study carried out by Jain et al. [23].
Advantages of Three-Dimensional Miniplates [8, 9, 21–24]
The quadrangle geometry of plate assures a three-dimensional stability of fracture site as it offers good resistance against torque forces.
Simplicity, malleability, low profile and ease of application.
Less postoperative surgical morbidity with early restoration of functions.
Less operating time.
The possible limitations of these plates are:
Excessive implant material due to the extravertical bars incorporated for countering the torque forces limits its use.
Difficult to use in communited fractures.
Cost of these plates which is slightly more than the conventional plates.
Difficult to adapt at the mental foramen region.
Limitations of the present study include the shorter follow-up period and a smaller sample size. To show significant improvements of 3D plate/screw system over conventional system, further studies with a larger sample size with longer follow-up are required.
Summary and Conclusion
The clinical outcome of both the 3D and standard miniplate systems in the present study was similar; however, the following advantages with the use of three-dimensional miniplates can be highlighted:
Relatively lesser operating time due to simultaneous stabilization at superior and inferior borders.
Three-dimensional stability of the fracture site.
Easy and simple to use.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Mukerji R, McGurk M. Mandibular fractures: historical perspective. Br J Oral Maxillofac Surg. 2006;44:222–228. doi: 10.1016/j.bjoms.2005.06.023. [DOI] [PubMed] [Google Scholar]
- 2.Fonseca RJ. Oral and maxillofacial trauma. 3. Philadelphia: W B Saunders Company; 2005. pp. 291–293. [Google Scholar]
- 3.Zix J, Lieger O, Iizuka T. Use of straight and curved 3-dimensional titanium miniplates for fracture fixation at the mandibular angle. J Oral Maxillofac Surg. 2007;65:1758–1763. doi: 10.1016/j.joms.2007.03.013. [DOI] [PubMed] [Google Scholar]
- 4.Alkan A, Celebi N, Ozden B, Bas B, Inal S. Biomechanical comparison of different plating techniques in repair of mandibular angle fractures. Oral Surg Oral Med Oral Path Oral Radiol Endod. 2007;104:752–756. doi: 10.1016/j.tripleo.2007.03.014. [DOI] [PubMed] [Google Scholar]
- 5.Bui P, Demian N, Beetar P. Infection rate in mandibular angle fractures treated with a 2.0-mm 8-hole curved strut plate. J Oral Maxillofac Surg. 2009;67:804–808. doi: 10.1016/j.joms.2008.08.034. [DOI] [PubMed] [Google Scholar]
- 6.Gassner R, Tuli T, Hachl O, Rudisch A, Ulmer H. Craniomaxillofacial trauma a 10 year review of 9543 cases with 21067 injuries. J Craniomaxillofac Surg. 2003;31:51–61. doi: 10.1016/S1010-5182(02)00168-3. [DOI] [PubMed] [Google Scholar]
- 7.Brasileiro BF, Passeri LA. Epidemiological analysis of maxillofacial fractures in Brazil: a 5-year prospective study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:28–34. doi: 10.1016/j.tripleo.2005.07.023. [DOI] [PubMed] [Google Scholar]
- 8.Tams J, Loon JP, Otten E, Rozema FR, Bos RRM. A three-dimensional study of bending and torsion moments for different fracture sites in the mandible: an in vitro study. Int J Oral Maxillofac Surg. 1997;26:383–388. doi: 10.1016/S0901-5027(97)80803-X. [DOI] [PubMed] [Google Scholar]
- 9.Guimond C, Johnson JV, Marchena JM. Fixation of mandibular angle fractures with a 2.0 mm 3-dimensional curved angle strut plate. J Oral Maxillofac Surg. 2005;63:209–214. doi: 10.1016/j.joms.2004.03.018. [DOI] [PubMed] [Google Scholar]
- 10.Farmand M. The 3D plating system in maxillofacial surgery. J Oral Maxillofac Surg. 1993;51(3):166–167. [Google Scholar]
- 11.Wittenberg JM, Mukherjee DP, Smith BR, Kruse RN. Biomechanical evaluation of new fixation devices for mandibular angle fractures. Int J Oral Maxillofac Surg. 1997;26:68–73. doi: 10.1016/S0901-5027(97)80852-1. [DOI] [PubMed] [Google Scholar]
- 12.Fridrich KL, Pena-Velasco G, Olson RAJ. Changing trends with mandibular fractures. J Oral Maxillofac Surg. 1992;50:586–589. doi: 10.1016/0278-2391(92)90438-6. [DOI] [PubMed] [Google Scholar]
- 13.Khalifa ME, El-Hawary HE, Hussein MM. Titanium three dimensional miniplate versus conventional titanium miniplate in fixation of anterior mandibular fractures. Life Sci J. 2012;9(2):1006. [Google Scholar]
- 14.Centres for Disease Control and Prevention (CDC). Definition for surgical site infection, Atlanta, GA (2002)
- 15.Jimson S, Sankar A, Prasad R. Comparative study of stainless steel miniplates, three dimensional plate and titanium three dimensional plate for fixation of mandibular fractures. Int J Maxillofac Surg. 2009;03:380. [Google Scholar]
- 16.Vijay E, Balakrishnan R. Three dimensional miniplate fixation in mandibular fractures. Indian J Multidiscip Dent. 2011;1(2):1. [Google Scholar]
- 17.Gear JLA, Apasova E, Schmitz JP, Schubert W. Treatment modalities for mandibular angle fractures. J Oral Maxillofac Surg. 2005;63:655–663. doi: 10.1016/j.joms.2004.02.016. [DOI] [PubMed] [Google Scholar]
- 18.Tate GS, Ellis E, III, Thockmorton GS. Bite force in patients treated for mandible angle fractures: implications for rigid fixation. J Oral Maxillofac Surg. 1994;52:734–736. doi: 10.1016/0278-2391(94)90489-8. [DOI] [PubMed] [Google Scholar]
- 19.Agarwal M, Mohammad S, Singh RK, Singh V. Prospective randomized clinical trial comparing bite force in 2-mm locking plates versus 2-mm standard plates in treatment of mandibular fractures. J Oral Maxillofac Surg. 2011;69:1995–2000. doi: 10.1016/j.joms.2010.10.014. [DOI] [PubMed] [Google Scholar]
- 20.Gerlach KL, Schwarz A. Bite forces in patients after treatment of mandibular angle fractures with miniplate osteosynthesis according to champy. Int J Oral Maxillofac Surg. 2002;31:345–348. doi: 10.1054/ijom.2002.0290. [DOI] [PubMed] [Google Scholar]
- 21.Jain MK, Sankar K, Ramesh C, Bhatta R. Management of mandibular interforaminal fractures using 3 dimensional locking and standard titanium miniplates—a comparative preliminary report of 10 cases. J Craniomaxillofac Surg. 2012;40(8):e475–e478. doi: 10.1016/j.jcms.2012.03.007. [DOI] [PubMed] [Google Scholar]
- 22.Goyal M, Marya K, Chawla S, Pandey R. Mandibular osteosynthesis: a comparative evaluation of two different fixation using 2.0 mm titanium miniplates and 3-D locking plates. J Maxillofac Oral Surg. 2011;10(1):32–37. doi: 10.1007/s12663-010-0087-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jain MK, Manjunath KS, Bhagwan BK, Shah DK. Comparison of 3-dimensional and standard miniplate fixation in the management of mandibular fractures. J. Oral Maxillofacial Surg. 2010;68:1568–1572. doi: 10.1016/j.joms.2009.07.083. [DOI] [PubMed] [Google Scholar]
- 24.Renton TF, Wiesenfeld D. Mandibular fracture osteosynthesis: a comparison of three techniques. Br J Oral Maxillofac Surg. 1996;34:166–173. doi: 10.1016/S0266-4356(96)90372-1. [DOI] [PubMed] [Google Scholar]


