Abstract
Objective
Various surgical techniques to release temporomandibular joint (TMJ) ankylosis have been described in the literature. The purpose of this paper is to report our Institution’s experience regarding the post-surgical outcome of different surgical techniques for the release of ankylosis of the TMJ.
Materials and Methods
The records from our hospital of 386 patients (521 joints) treated for TMJ ankylosis were reviewed. Data analysis included the etiology of TMJ ankylosis, gender distribution, age group, distribution of ankylosis based on location, type, interincisal opening and complications in the perioperative period.
Results
Out of 521 joints, 65.02% were unilateral and 73.89% had bony ankylosis. The mean maximal incisal opening preoperative was 5.4 mm (SD 3.63 mm) and at 1-year follow-up was 36.9 mm (SD 3.3 mm). There was no permanent facial nerve paralysis. However, transient facial nerve paresis was 14.78%. There was an overall recurrence rate of 8.82%.
Conclusion
We conclude that after TMJ ankylosis release with interpositional arthroplasty, reconstruction of the RCU with L ramus osteotomy is the most favorable. This procedure not only causes least complications, but also maintains height of ramus, facilitating surgeries for secondary asymmetry correction.
Keywords: TMJ ankylosis, Interpositional arthroplasty, Ramus condyle unit reconstruction
Introduction
Temporomandibular joint (TMJ) ankylosis is a pathologic condition which interferes with mastication and normal life activities, including limited chewing ability, difficulty in swallowing and speech and compromised oral and nutritional status.
Depending on the type and extent of involvement, the age of incidence and the duration of ankylosis, patients may present with differing symptoms. When this occurs during development, it results in an alteration of the normal potential growth leading to mandibular micrognathia, facial asymmetry, obstructive sleep apnea and reduction in the normal functional spurs necessary for the development of the whole maxillofacial complex. Early diagnosis, proper therapeutic intervention and appropriate rehabilitation are essential in the treatment of TMJ ankylosis [1].
The treatment of bony ankylosis is surgical, but the methods vary; so, surgeons have to decide which method to adopt to achieve the best results subjectively and objectively [2]. Multiple surgical modalities have been proposed to manage TMJ ankylosis including gap arthroplasty, interpositional arthroplasty and total joint reconstruction (TJR). For interposition, alloplastic materials such as Proplast, Teflon and silastic have been used, but with high failure rates. Autogenous tissues, such as costochondral graft (CCG), sternoclavicular graft, coronoid process, resected condyle autograft, auricular cartilage, temporalis myofascial flap, dermal and buccal fat pad, have also been used.
The purpose of this article is to report our experience of managing 386 patients having 521 ankylosed joints and to assess the post-surgical outcome of different surgical techniques (gap arthroplasty(GAP) alone, GAP + temporalis, GAP + temporalis + costochondral graft, GAP + temporalis + coronoid process, GAP +temporalis + vertical ramal osteotomy (VRO) and GAP + temporalis + “L” osteotomy for the release of ankylosis of TMJ).
Materials and Methods
This retrospective study included 386 patients having 521 TMJ ankylosis treated at the Department of Oral and Maxillofacial Surgery, Government Dental College and Hospital, Ahmedabad, from January 2000 to December 2016. Data analysis included the etiology of TMJ ankylosis, gender distribution, age group of patients, location, type, maximal interincisal opening, various treatment modalities and complications in the perioperative period.
The preoperative assessment included a detailed patient history, physical and radiological examinations and mouth opening (in millimeter—mm) measurements at various time intervals: preoperatively, intraoperatively and postoperatively (immediately, 1, 6 and 12 months).
All patients were operated on under general anesthesia using a standard preauricular approach with temporal extension when temporalis myofascial flap was used. The incision was made through the skin, subcutaneous connective tissue to the depth of superficial layer of temporalis fascia. Oblique incision through the superficial layer of the temporalis fascia was given. A periosteal elevator inserted beneath the superficial layer of the temporalis muscle was used to strip periosteum off the lateral portion of the zygomatic arch, and dissection was continued below the arch just superficial to the capsule of the temporomandibular joint. A vertical incision was made through the intervening tissues just in front of the external auditory meatus to the depth of the periosteal elevator. Any bleeding superficial vessels were cauterized before deeper dissection was proceeded with, and the ankylotic mass was then exposed.
Patients were categorized, according to the surgical technique employed, into two main groups: Group I gap arthroplasty; Group II: gap arthroplasty followed by placement of various autogenous interpositional materials.
Most of the patients in our Institute had undergone only gap arthroplasty (Group I) in the initial days, as that was the protocol followed then in our Department. Gap arthroplasty later than that was done only in those who had declined any type of bone grafting or interpositional materials. Group II patients underwent interpositional arthroplasty using autogenous materials like temporalis myofascial flap alone, temporalis and costochondral graft, temporalis and coronoid process, temporalis and vertical ramal osteotomy (VRO) and temporalis and “L” osteotomy.
In Group I patients, a 1.5-cm gap was created after resection of the ankylotic mass and left without any interpositional material. Ipsilateral coronoidectomy was performed through the same preauricular incision. This was the procedure followed for all cases before the year 2005.
In Group II cases, the temporalis myofascial flap was used for interposition between the bony segments. A 3.5-cm-long myofascial flap was turned outward and downward over the zygomatic arch and placed into the glenoid fossa and sutured [1–3].
Costochondral graft was used in all cases below 12 years of age till the year 2011. In unilateral cases the graft was taken from the 5th rib through a submammary incision, while in bilateral cases, both the 5th and the 7th ribs were employed. The length of the cartilaginous component of the CCG was 2–3 mm, and its end was made dome-shaped to resemble the condylar head. This graft was secured to the outer posterior surface of the ascending ramus of the mandible with screws [1, 2].
From the year 2011 onward, after realizing CCG’s unpredictable growth, we started using resected coronoid process for reconstruction of ramus condyle unit (RCU) in the age group of 5–8 years. The resected coronoid process was reshaped and fixed to the ramal stump using a 4-hole plate or a bicortical screw [4].
In the same time period, we performed L and vertical ramus osteotomy (VRO) in all patients above 8 years of age, as in patients less than 8 years the amount of bone posterior to the lingula was not sufficient for osteotomies of posterior border of ramus [5]. When “L” osteotomy was planned, a vertical osteotomy was performed on the posterior border of the mandibular ramus till about 1.0 cm above the angle of the mandible. This segment was moved up, and the resected ipsilateral coronoid process was implanted in the gap between the sliding segment and the angle of the mandible. VRO was done where an obvious antegonial notch was present. In VRO a vertical osteotomy was performed on the entire posterior border of the mandibular ramus and then moved up into the glenoid fossa. Subsequently, fixation of the bone graft was done with miniplates and the sharp edges at the lower border of mandible were smoothened. The osteotomized segment was pedicled lingually on the medial pterygoid muscle. In both L osteotomy and VRO the upper end of the cut ramus was then recontoured to simulate the neocondyle. The final position of the neocondyle in the glenoid fossa was determined by placing the teeth in occlusion.
Results
A total of 386 patients (521 TM Joints) were included in this study from January 2000 to December 2016. In our study, 57.25% female and 42.75% male patients were present. The age group of 5–10 years—20.47%, above 20 years—19.69%; and with the most frequent age group of 11–20 years was 59.84%. Unilateral TMJ was diagnosed in 251 (65.02%) patients, 154 (61.35%) of which were on the right side and 97 (38.65%) on the left side, while bilateral ankylosis was diagnosed in 135 (34.98%) patients. Out of 386 patients, 354 patients (91.71%) had a history of trauma followed by 28 patients (7.25%) infection and 4 patients (1.04%) history not confirmed. Three different types of ankylosis were identified: bony ankylosis in 385 (73.89%) joints; fibrous ankylosis in 56 (10.75%); and fibro-osseous ankylosis in 80 (15.36%) joints.
Other data analyses included various treatment modalities employed in patients (Fig. 1), IIO (Table 1) and complications in the perioperative period (Fig. 2).
Fig. 1.
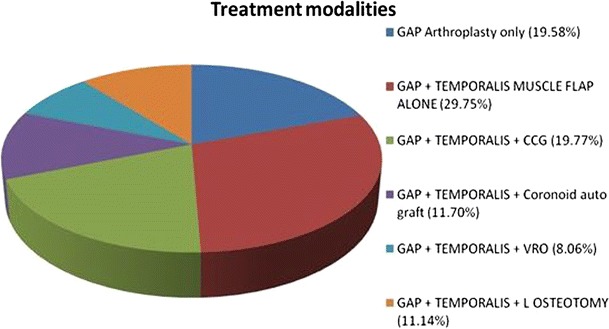
Treatment modalities employed in patients
Table 1.
Mouth opening (in mm)
| Preoperative | Intraoperative | Postoperative | ||||
|---|---|---|---|---|---|---|
| Immediate | 1 month | 6 months | 12 months | |||
| Mean | 5.4 | 38.3 | 27.4 | 38.2 | 37.9 | 36.9 |
| SD | 3.63 | 3.52 | 3.22 | 3.10 | 3.3 | 3.3 |
| Range | 0-10 | 26-40 | 20-35 | 36-39.6 | 36-38.8 | 36-38.4 |
mm millimeter; SD standard deviation
Fig. 2.
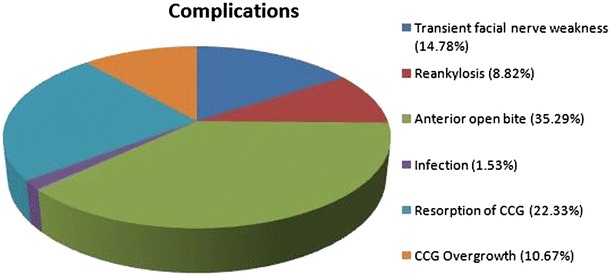
Complications
Discussion
Ankylosis of the TMJ is one of the most common disorders affecting the craniofacial complex. Because the development of TMJ ankylosis is slow and concealed, sometimes the patient and doctors overlook it until the mouth opening is completely restricted [1]. TMJ ankylosis occurs primarily in the first and second decades of life (35–92%) and is commonly associated with trauma (13–100%), local or systemic infection (0–53%), and systemic diseases such as ankylosing spondylitis, rheumatoid arthritis and psoriasis (28%); it also occurs after TMJ surgery [6, 7]. Trauma (91.71%) as the most common cause of the condition documented in our study is almost similar to 86% in India [8]; 83.33% in China [9]. In accordance with the results from Elgazzar [10], the current study showed that patients aged 11–20 years were the most affected age group (50.78%).
Autogenous sources present donor site morbidity; however, joints reconstructed with alloplastic materials have experienced infection and inflammatory problems as the immune system reacts to a foreign body [11, 12]. Several authors have used autogenous interpositional materials, such as temporalis muscle, dermis–fat graft, auricular cartilage and buccal pad fat [13–16]. Some authors have suggested using the remaining TMJ disk [17], after its repositioning. Several autologous bone grafts are used to reconstruct the RCU, including costochondral and sternoclavicular bone grafts [18]. Resected elongated coronoid process [4] and excised ankylotic mass [19] have also been tried.
In the current study, RCU reconstruction unit with costochondral graft, coronoid process, TM flap, L or VROs reduced the sequelae of gap arthroplasty: open bite; lack of functional restoration of the joint; shortened ramus; deviated jaw; and increased possibility of recurrent ankylosis [8, 15]. Indications of each modality have been mentioned in Materials and Methods section. Merits and demerits of each modality are shown in Table 2.
Table 2.
Merits and demerits of various treatment modalities
| Treatment modalities | Merits | Demerits |
|---|---|---|
| Gap arthroplasty | Re-ankylosis chances are less in comparison with condylectomy | Increased recurrence rates compared to interpositional arthroplasty Shortening of the ramus Occlusal discrepancy In bilateral cases chances of postoperative OSA (obstructive sleep apnea) |
| Temporalis myofascial flap | Same surgical site Flap is well vascularized by temporal vessels The muscle provides proper bulk so that stresses in the joint can be absorbed |
Chances of necrosis if not properly pedicled Chances of injury to temporal branch of facial nerve Temporal hollowing Cannot be reused |
| Costochondral graft | Both bone and cartilaginous components have intrinsic growth potential Gross anatomical similarity to the mandibular condyle |
Additional surgical site and donor site morbidity Unpredictable growth in terms of both resorption and hypertrophy |
| Autogenous coronoid | It provides enough length and strength for RCU reconstruction Second surgical site and donor site morbidity avoided |
Risk of resorption as it is a non-vascularized graft |
| VRO | Grafts of posterior border of ramus are pedicled on the medial pterygoid muscle, thus reducing chances of resorption Hence, less decrease in height of ramus, less deviation and less occlusal discrepancy |
Cannot be used in less than 8 years of age due to inadequate width and height of ramus Lack of inherent growth Extra submandibular incision |
| L osteotomy | Similar to VRO. The only difference between L and VRO is the fact that complete height of ramus is maintained in L osteotomy, whereas some height of ramus decrease occurs in VRO at the time of shaving off the step at the inferior border of mandible | Similar to VRO |
RCU ramus condyle unit, VRO vertical ramus osteotomy
The significance of RCU reconstruction with interpositional material using hard tissues is important because:
It maintains the height of ramus.
Thereby, it facilitates further surgeries for secondary deformity correction.
It prevents occlusal discrepancies: anterior open bite in bilateral cases and occlusal deviation in unilateral cases.
Finally, it possibly resolves the problem of secondary mandibular asymmetry due to rerestoration of growth spurts (application of MOSS’s functional matrix therapy).
The results of the current and some previous studies [1, 20] highlight the importance of immediate postoperative physiotherapy as a key element in the success of TMJ ankylosis management. Besides the reduction in the rate of re-ankylosis, vigorous immediate postoperative jaw exercises helped most of our patients to regain or exceed the measurements recorded during intraoperative mouth opening. Mouth opening was significantly improved from 5.4 mm preoperatively to 38.3 mm intraoperatively, 27.4 mm immediate postoperatively, 38.2 mm 1 month postoperatively, 37.9 mm 6 months postoperatively and 36.9 mm 12 months postoperatively(Table 1).
Temporary and mild facial nerve paresis lasting for 3–5 weeks postoperatively is observed in 14.78% (77 joints) similar to 11% [10]; this was mainly due to excessive flap traction during surgery; and there was no reported permanent facial nerve damage (Fig. 3). Postoperative facial nerve weakness was managed by IV steroids and physiotherapy.
Fig. 3.
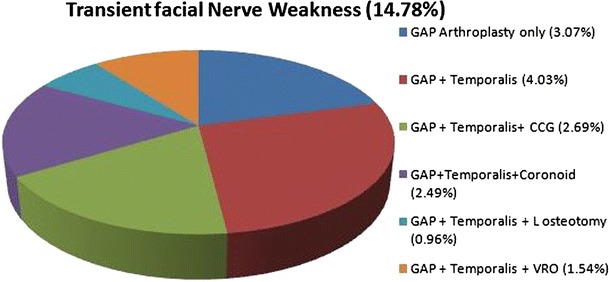
Transient facial nerve weakness
Recurrence of ankylosis was documented in 8.82% (46 joints) of this series compared with 5% [21] and 86% [22] in other reports (Fig. 4). The cases of re-ankylosis in this series were mainly due to the use of gap arthroplasty without interpositional materials and non-compliance with physiotherapy. Re-ankylosis was managed by the elimination of the etiology, retreatment and intensive physiotherapy with close follow-up.
Fig. 4.
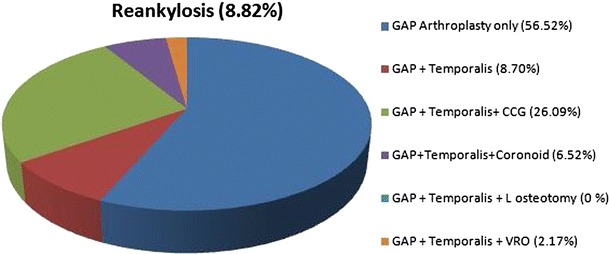
Recurrence of ankylosis
Anterior open bite was present in 35.29% observed in our study was most commonly associated with bilateral condylectomy with Group I while not a single patient was found in Group II. Zhi et al. [9] found in their study that 23.8% operated patients have anterior open bite. The interposition of materials usually reduces the anterior open bite. Dental occlusion in younger patients has improved naturally, as their dentition has developed.
Resorption and cartilage overgrowth of CCG were present in 23 joints (22.33%) and 11 joints (10.67%), respectively, in our study which is similar to the study done by Medra et al. [23] and Praveen kumar [24]. Perrott et al. [25] reported that when only 2–4 mm of cartilage transplanted with the rib, no overgrowth of the grafts occurred.
Conclusion
Thus, trauma to TMJ is the primary source of ankylosis; however, early release of TMJ ankylosis and RCU reconstruction followed by aggressive physiotherapy and follow-up play an important role in the prevention of recurrence. We conclude that of all techniques used to release TMJ ankylosis with interpositional arthroplasty and reconstruction of the RCU with L ramus osteotomy is the most favorable. This procedure not only causes least complications, but also maintains height of the ramus, facilitating surgeries for secondary asymmetry correction.
Acknowledgements
We sincerely thank our former Head of Dept. of GDCH, Ahmedabad, Dr Babu S Parmar for his contribution toward patient’s surgical work in the Department in his tenure.
Conflict of interest
The authors declare that they have no conflict of interest.
Human Rights and Informed Consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and the Declaration of Helsinki of 1975 that was revised in 2000. Written informed consent was obtained from the patient before their inclusion in the study with the approval from ethical committee. The procedure was explained to them regarding the nature and benefit of the study.
Contributor Information
Sonal Anchlia, Email: sonal.anchlia@gmail.com.
Jigar Dhuvad, Email: drjigardhuvad1981@gmail.com.
Jay Chetan Shah, Email: drjayshah2002@yahoo.com.
References
- 1.Kaban LB, Perrott DH. A protocol for management of temporomandibular joint ankylosis. J Oral Maxillofac Surg. 1990;48:1145–1151. doi: 10.1016/0278-2391(90)90529-B. [DOI] [PubMed] [Google Scholar]
- 2.Kaban LB, Bouchard C, Troulis MJ. A protocol for management of TMJ ankylosis in children. J Oral Maxillofac Surg. 2009;67:1966–1978. doi: 10.1016/j.joms.2009.03.071. [DOI] [PubMed] [Google Scholar]
- 3.Kearns G. Subjective and objective assessment of the temporalis myofascial flap in previously operated temporomandibular joints. J Oral Maxillofac Surg. 1999;57:1065–1067. doi: 10.1016/S0278-2391(99)90326-9. [DOI] [PubMed] [Google Scholar]
- 4.Hussein MM. Condylar reconstruction in extensive ankylosis of TMJ in adults using resected coronoid segment as autograft. Egypt Dent J. 2002;48:903–908. [Google Scholar]
- 5.Liu Y, Khada A, Li J, Hu J, Zhu S, Hsu Y, Wang Q, Wang D. Sliding reconstruction of the condyle using posterior border of mandibular ramus in patients with TMJ ankylosis. Int J Oral Maxillofac Surg. 2011;40:1238–1245. doi: 10.1016/j.ijom.2011.04.016. [DOI] [PubMed] [Google Scholar]
- 6.He D, Ellis E, 3rd, Zhang Y. Etiology of temporomandibular joint ankylosis secondary to condylar fractures: the role of concomitant mandibular fractures. J Oral Maxillofac Surg. 2008;66:77–84. doi: 10.1016/j.joms.2007.08.013. [DOI] [PubMed] [Google Scholar]
- 7.El-Sheikh MM, Medra AM. Management of unilateral temporomandibular joint ankylosis associated with facial asymmetry. J Craniomaxillofac Surg. 1997;25:109–115. doi: 10.1016/S1010-5182(97)80001-7. [DOI] [PubMed] [Google Scholar]
- 8.Roychoudhury A, Parkash H, Trikha A. Functional restoration by gap arthroplasty in temporomandibular joint ankylosis. A report of 50 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;87:166–169. doi: 10.1016/S1079-2104(99)70267-2. [DOI] [PubMed] [Google Scholar]
- 9.Zhi K, Ren W, Zhou H, Gao LL, Zhao CH, et al. Management of temporomandibular joint ankylosis: 11 years’ clinical experience. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:687–692. doi: 10.1016/j.tripleo.2009.06.041. [DOI] [PubMed] [Google Scholar]
- 10.Elgazzar RF, Abdelhady AI, Sada KA, Elshaal MA, Hussain MM, Abdelal SE, et al. Treatment modalities of TMJ ankylosis: experience in Delta Nile, Egypt. Int J Oral Maxillofac Surg. 2010;39(4):333–342. doi: 10.1016/j.ijom.2010.01.005. [DOI] [PubMed] [Google Scholar]
- 11.Raveh J, Vuillemin TH, Ladrach K, Sutter F. Temporomandibular joint ankylosis: surgical treatment and long term results. J Oral Maxillofac Surg. 1989;47:900–906. doi: 10.1016/0278-2391(89)90371-6. [DOI] [PubMed] [Google Scholar]
- 12.Lee JJ, Worthington P. Reconstruction of the temporomandibular joint using calvarial bone after a failed Teflon-Proplast implant. J Oral Maxillofac Surg. 1999;57:457–461. doi: 10.1016/S0278-2391(99)90290-2. [DOI] [PubMed] [Google Scholar]
- 13.Abdelhady AI. Role of buccal fat pad interposition after temporomandibular joint ankylosis surgery. Egypt Dent J. 2004;50:1057–1069. [Google Scholar]
- 14.Dimitroulis G. The interpositional dermis–fat graft in the management of temporomandibular joint ankylosis. Int J Oral Maxillofac Surg. 2004;33:755–760. doi: 10.1016/j.ijom.2004.01.012. [DOI] [PubMed] [Google Scholar]
- 15.Qudah M, Qudeimat MA, Al-Maaita J. Treatment of TMJ ankylosis in Jordanian children—a comparison of two surgical techniques. J Craniomaxillofac Surg. 2005;33:30–36. doi: 10.1016/j.jcms.2004.07.005. [DOI] [PubMed] [Google Scholar]
- 16.Su-Gwan K. Treatment of temporomandibular joint ankylosis with temporalis muscle and fascia flap. Int J Oral Maxillofac Surg. 2001;30:189–193. doi: 10.1054/ijom.2001.0047. [DOI] [PubMed] [Google Scholar]
- 17.Nitzan DW, Bar-Ziv J, Shteyer A. Surgical management of temporomandibular joint ankylosis type III by retaining the displaced condyle and disc. J Oral Maxillofac Surg. 1998;56:1133–1138. doi: 10.1016/S0278-2391(98)90753-4. [DOI] [PubMed] [Google Scholar]
- 18.Ellis E, Carlson DS. Histologic comparison of the costochondral, sternoclavicular and temporomandibular joints during growth in Macaca Muttata. J Oral Maxillofac Surg. 1986;44:312–321. doi: 10.1016/0278-2391(86)90082-0. [DOI] [PubMed] [Google Scholar]
- 19.Gunaseelan R. Condylar reconstruction in extensive ankylosis of temporomandibular joint in adults using resected segment as autograft: a new technique. Int J Oral Maxillofac Surg. 1997;26(6):405–407. doi: 10.1016/S0901-5027(97)80002-1. [DOI] [PubMed] [Google Scholar]
- 20.Matsuura H, Miyamoto H, Ishimaru J, Kurita K, Goss AN. Effect of partial immobilization on reconstruction of ankylosis of the temporomandibular joint with an autogenous costochondral graft: an experimental study in sheep. Br J Oral Maxillofac Surg. 2001;39:196–203. doi: 10.1054/bjom.2001.0623. [DOI] [PubMed] [Google Scholar]
- 21.Sawhney CP. Bony ankylosis of the temporomandibular joint: follow-up of 70 patients treated with arthroplasty and acrylic spacer interposition. Plast Reconstr Surg. 1986;77:29–38. doi: 10.1097/00006534-198601000-00006. [DOI] [PubMed] [Google Scholar]
- 22.Saeed NR, Kent JN. A retrospective study of the costochondral graft in TMJ reconstruction. Int J Oral Maxillofac Surg. 2003;32:606–609. doi: 10.1054/ijom.2003.0418. [DOI] [PubMed] [Google Scholar]
- 23.Medra AM. Follow up of mandibular costochondral grafts after release of ankylosis of the temporomandibular joints. Br J Oral Maxillofac Surg. 2005;43:118–122. doi: 10.1016/j.bjoms.2004.05.004. [DOI] [PubMed] [Google Scholar]
- 24.Kumar P, Rattan V, Rai S. Do costochondral grafts have any growth potential in temporomandibular joint surgery? A systematic review. J Oral Biol Craniofac Res. 2015;5(3):198–202. doi: 10.1016/j.jobcr.2015.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Perrott DH, Umeda H, Kaban LB. Costochondral graft construction/reconstruction of the ramus/condyle unit: long-term follow-up. Int J Oral Maxillofac Surg. 1994;23:321. doi: 10.1016/S0901-5027(05)80046-3. [DOI] [PubMed] [Google Scholar]


