Abstract
Objective
To correlate the clinical course and biochemical analysis in odontogenic space infections.
Methods
A randomized prospective study was undertaken in 50 patients presenting with infections of odontogenic origin. The data were subjected to statistical analysis to co-relate the values of CRP, WBC count and ESR with the clinical course of odontogenic infections. The statistical analysis was carried out using SPSS Version 17.0 clinical parameters included pain, swelling, mouth opening, dyspnea, dysphagia, hoarseness, body temperature, active discharge, length of hospital stay and number of fascial spaces involved.
Results
There was a significant correlation between all the clinical parameters and biochemical markers preoperatively as well as on various postoperative days.
Conclusion
According to the percentage rate of fall, CRP was considered as the best indicator of clinical course/recovery of the patient, followed by WBC count and ESR, respectively.
Keywords: Odontogenic infections, Biomarkers, WBC, ESR, CRP
Introduction
The oral cavity is considered to be sterile at the time of birth. However, as one grows, the oral cavity gets harbored with a diverse, indigenous flora which includes bacteria, viruses, fungi and protozoa. Generally in orofacial region, most bacterial infections involve either a disturbance of the normal flora or a displacement of normal microorganisms to the sites where they are usually not seen.
The last decade has seen a notable change in behavior of odontogenic infections. The severity of these infections is far greater than what it was in the past, thereby demanding swift recognition of the disease followed by prompt and more aggressive treatment. Thus, in these situations, we often decide the line of treatment based on clinical laboratory monitoring. Erythrocyte sedimentation rate (ESR) and white blood cell (WBC) counts are the most commonly performed conventional laboratory tests used to detect the presence of acute inflammation and to monitor the development of postoperative infections [1].
Advocates of inflammatory markers narrate numerous advantages for their usage. According to them, quantitative determination of serum markers can be used for determining therapeutic efficacy of different treatment regimes of infections and the duration of antibiotic usage [2].
The present study was undertaken to correlate the values of CRP, WBC count and ESR with the clinical course of odontogenic infections.
Materials and Methods
The present randomized prospective study was undertaken in 50 patients presenting with infections of odontogenic origin in the Department of Oral and Maxillofacial Surgery. Institutional ethical committee approval was obtained before undertaking the study, along with an informed consent from all the patients. Patients with infections of odontogenic origin requiring surgical intervention were included in the study. Medically compromised patients, pregnant females, chronic alcoholics, patients on steroid therapy and on contraceptives were excluded from the study. All the patients were treated and observed by the same surgeon.
Diagnosis of the space involved was made on the basis of history and clinical examination. All the patients underwent hematological investigations and radiological examination (OPG). For bacteriological examination, pus sample was collected by aspiration from abscess site with a disposable 18-gauge needle and syringe. The sample was processed for gram staining, bacterial culture and antimicrobial sensitivity.
Preoperative assessment included the following parameters: dental etiology, teeth involved, number of spaces involved (evident clinically or on computerized tomography if required), body temperature, mouth opening (measurement of maximum inter-incisal opening with vernier calliper), and pain (using visual analogue scale running from 1 to 10). Active pus discharge, dysphagia, hoarseness, dyspnoea and swelling were assessed as score 0 if absent and score 1 if present.
Based on the diagnosis, management of the patients with odontogenic infection was carried out. Definitive management consisted of incision and drainage of abscess and the extraction of the offending tooth as indicated. Empirical antimicrobial therapy and appropriate analgesic drugs were started for the control of infection and relief of pain. After culture and sensitivity report was available, definitive antimicrobial therapy was instituted. Treatment regimen was considered effective if both clinical parameters and laboratory values of the biochemical markers showed improvement.
Supportive therapy in the form of high protein diet, multivitamin and parenteral fluid therapy was instituted as indicated in the individual cases. Duration of hospital stay was noted down.
Postoperative assessment of patients was carried out on 4th day, 7th day, 14th day or till the time clinical signs and symptoms subsided. The data were subjected to statistical analysis to co-relate the values of CRP, WBC count and ESR with the clinical course of odontogenic infections.
Statistical Analysis
The statistical analysis was carried out using SPSS Version 17.0. Regression test was applied to determine the correlation of biochemical values and clinical parameters (mouth opening, pain, number of fascial spaces and length of hospital stay). The Pearson correlation coefficient (‘r’ value) was accordingly used to find the correlation between the variables. Paired ‘t’ test was used to compare the paired ‘t’ values (preoperatively and on day 14) of swelling, dyspnoea, dysphagia, hoarseness, core temperature and active discharge.
Results
Out of 50 patients in the study, there were 30 (60%) male patients and 20 (40%) female patients. A maximum number of patients (30%) were in the age-group of 21–30 years. Thirty-three patients (66%) had the involvement of a single tooth with mandibular third molar being the most frequently involved offending tooth (26.67%). In 62% patients, single space was involved, whereas in 38% patients, multiple spaces were involved. Submandibular space was involved in maximum number of patients (60%).
Gram-positive cocci were isolated in 94% samples. It was observed that maximum number of patients (76%) had isolates of aerobic bacteria and most of the microorganisms (96.67%) isolated in pus culture were found to be sensitive to co-amoxiclav and amikacin.
The preoperative clinical characteristics in patients with odontogenic infections are depicted in Fig. 1. The mean values of all the three biochemical parameters preoperatively and on various postoperative days are depicted in Fig. 2.
Fig. 1.
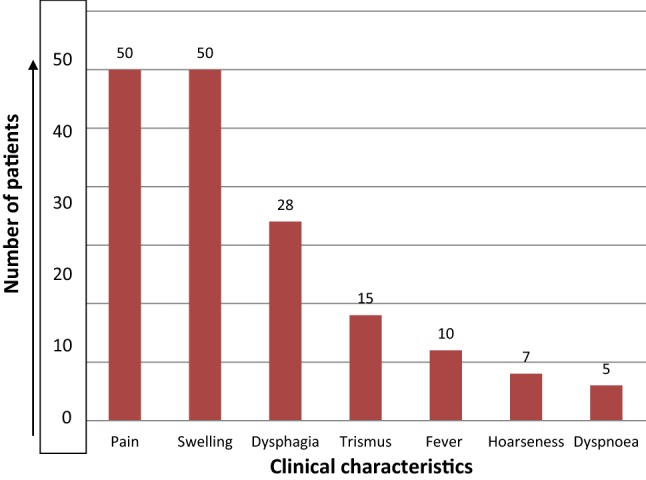
Preoperative clinical analysis in patients with odontogenic infections
Fig. 2.
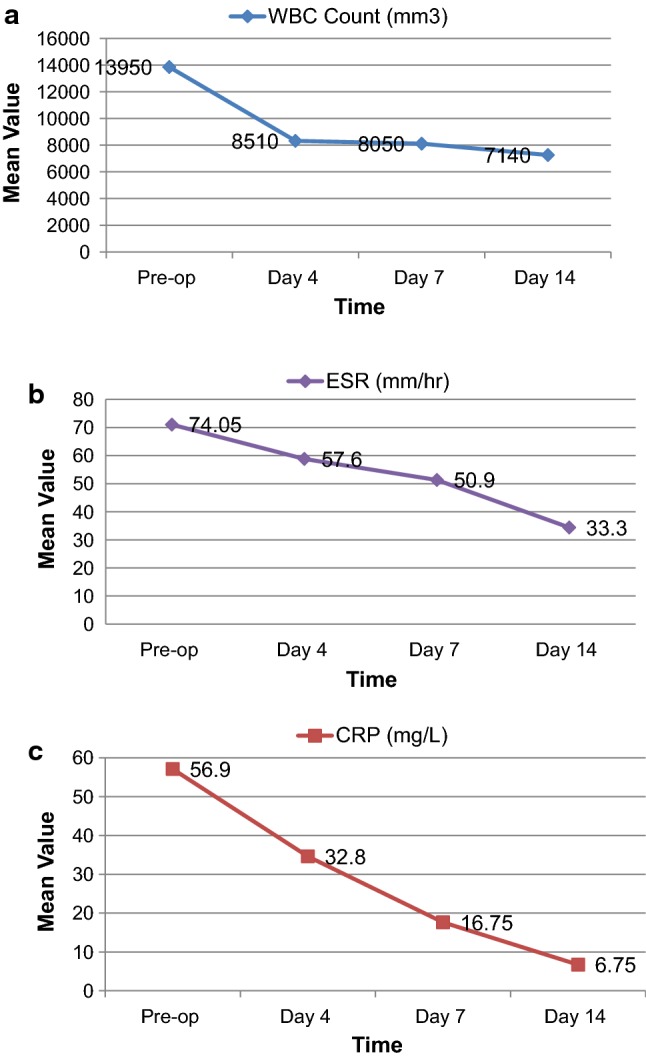
Mean value of biomarkers in patients with odontogenic space infection a WBC, b ESR, c CRP
Pain and swelling were present in 100% of the patients preoperatively (Fig. 1).
There was positive and significant Pearson correlation coefficient (r) between VAS score of pain and the three biochemical parameters (WBC, ESR and CRP) as shown in Table 1.
Table 1.
Statistical correlation of pain with biochemical parameters
| Pain (VAS score) | ||||
|---|---|---|---|---|
| At preop | At day 4 | At day 7 | At day 14 | |
| WBC count |
r = 0.375 p = 0.035* |
r = 0.029 p = 0.974 |
r = − 0.049 p = 0.853 |
r = − 0.056 p = 0.792 |
| CRP |
r = 0.389 p = 0.035* |
r = 0.179 p = 0.336 |
r = − 0.044 p = 0.803 |
r = − 0.174 p = 0.359 |
| ESR |
r = 0.462 p = 0.012* |
r = − 0.169 p = 0.391 |
r = 0.182 p = 0.384 |
r = 0.044 p = 0.192 |
r Pearson correlation coefficient
*p < 0.05 is considered to be statistically significant
The regression equation implies that preoperatively, 15.1% variation in pain was explained by WBC count. Secondly, with every one unit increase in ESR, there was an increase of 0.019 units in pain and 20.3% variation in pain was explained by ESR. Thirdly, with every one unit increase in CRP, there was an increase of 0.017 units in pain and 14.9% variation in pain was explained by CRP.
As shown in Table 2, the Pearson correlation coefficient (r) between mouth opening and WBC count was − 0.290 (p = 0.117), which shows their nonsignificant relationship. Further, with every one unit increase in the Pearson coefficient between mouth opening and WBC count, there was a decrease of 0.06 units in mouth opening. The Pearson correlation coefficient (r) between mouth opening and ESR (r = − 0.568, p = 0.001) as well as CRP (r = − 0.483, p = 0.007) shows their negative but statistically significant correlation (Table 2). The regression equation implies that preoperatively, with every one unit decrease in ESR, there was an increase of 0.018 units in mouth opening .32.4% of variation in mouth opening was explained by ESR. With every one unit decrease in CRP, there was an increase of 0.016 units in mouth opening and 23.4% change in mouth opening was explained by CRP.
Table 2.
Statistical correlation of mouth opening with biochemical parameters
| Mouth opening | ||||
|---|---|---|---|---|
| Preop | At day 4 | At day 7 | At day 14 | |
| WBC count |
r = − 0.290 p = 0.117 |
r = − 0.440 p = 0.015* |
r = − 0.259 p = 0.172 |
r = − 0.062 p = 0.751 |
| CRP |
r = − 0.483 p = 0.007* |
r = − 0.013 p = 0.949 |
r = − 0.339 p = 0.069 |
r = − 0.268 p = 0.152 |
| ESR |
r = − 0.568 p = 0.001* |
r = − 0.191 p = 0.314 |
r = − 0.539 p = 0.002* |
r = − 0.580 p = 0.001* |
r Pearson correlation coefficient
*p < 0.05 is considered to be statistically significant
Day 4
The Pearson correlation coefficient between pain and all the three biochemical parameters showed a nonsignificant correlation (Table 1). At day 4, Pearson correlation coefficient (r) between mouth opening and WBC count was − 0.440 (p = 0.015), which shows their negative but significant correlation. 19.4% change in mouth opening was explained by WBC count. However, the correlation of mouth opening with CRP and also with ESR was nonsignificant (Table 2).
Day 7
At day 7, there was negative but significant correlation between mouth opening and ESR (r = − 0.539, p = 0.002). With every one unit decrease in ESR, there was an increase of 0.015 units in mouth opening. 28.9% of variation in mouth opening was explained by ESR (Table 2). However, there was a nonsignificant correlation between Pearson correlation coefficient of CRP and WBC with mouth opening. Further, similar to the pattern on day 4, the relation between pain and all the three biochemical parameters showed a nonsignificant correlation (Table 1).
Day 14
There was a nonsignificant correlation between Pearson correlation coefficient of CRP and WBC count with mouth opening on day 14. However, there was a negative but significant correlation between mouth opening and ESR. With every one unit decrease in ESR, there was an increase of 0.017 units in mouth opening. 33.8% of variation in mouth opening was explained by ESR. Further, also the correlation between pain and all the three biochemical parameters was nonsignificant which is similar to that on day 4 and 7.
Comparison of the ‘p’ value for all the three biochemical parameters (WBC count, CRP and ESR) between preoperative day and day 14 in relation to swelling, dysphagia, dyspnoea, hoarseness, body temperature and active pus discharge was statistically significant (p < 0.05), which shows that the severity of signs and symptoms had a significant correlation with the values of all three biochemical markers.
Number of Fascial Spaces Involved
The regression equation implied that for every one unit increase in WBC count, CRP and ESR, there was an increase of 0.05 units, 0.01 units and 0.008 units, respectively, in the number of fascial spaces involved. 33.4% of the variation in number of fascial spaces involved was explained by WBC count, 20.2% by CRP and 16.7% by ESR. All the three biochemical markers were found to be significant predictors of the number of fascial spaces involved (Fig. 3a–c).
Fig. 3.
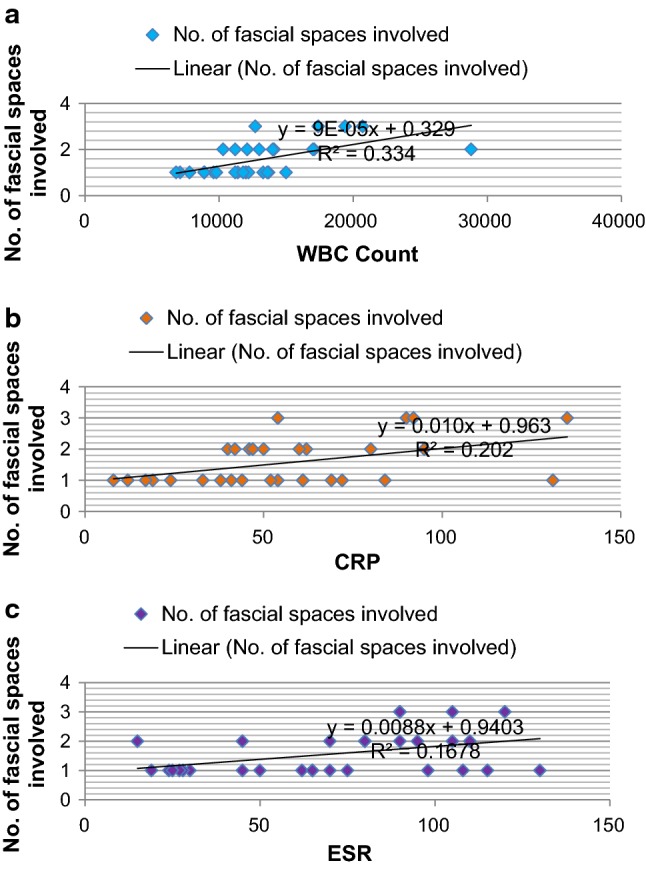
Correlation of clinical parameters with number of fascial spaces involved
Length of Hospital Stay
The regression equation implied that with every one unit increase in WBC count, CRP and ESR, there was an increase of 0.034 units, 0.028 units and 0.025 units, respectively, in the length of hospital stay. 34.9% of variation in hospital stay was explained by WBC count, 28.7% by CRP and 26.2% by ESR. Hence, all the three biochemical markers were considered to be good predictors of the length of hospital stay (Fig. 4a–c).
Fig. 4.
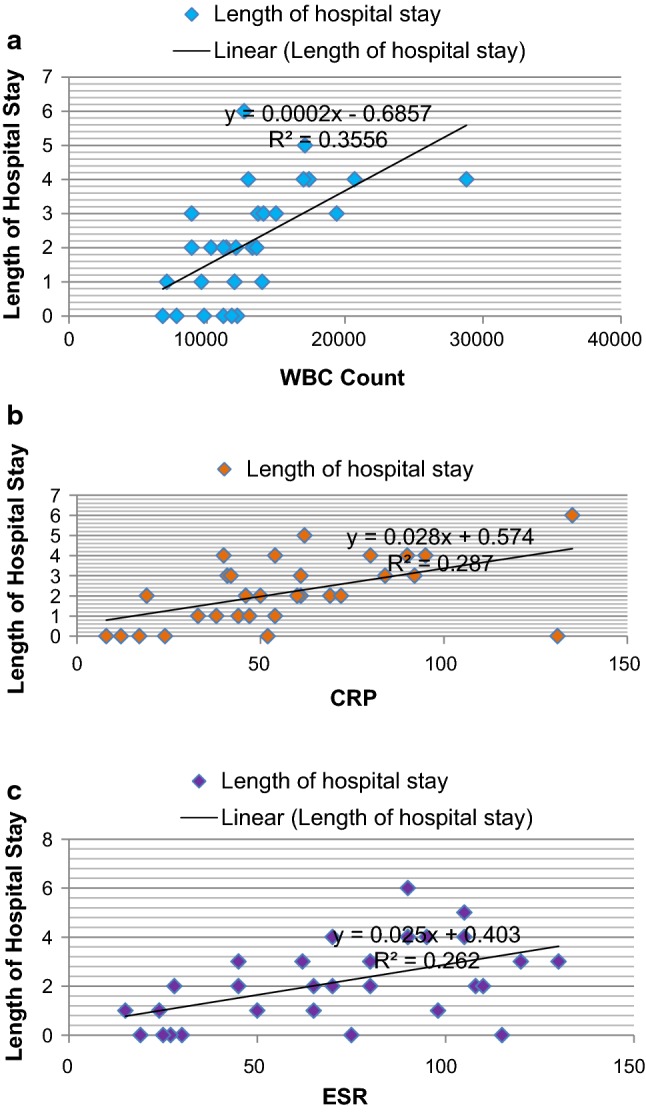
Correlation of clinical parameters with length of hospital stay
Rate of Fall of Biomarkers
On an average, according to the percentage rate of fall, CRP was considered as the best indicator of clinical course/recovery of the patient, followed by WBC count and ESR, respectively (Fig. 5).
Fig. 5.
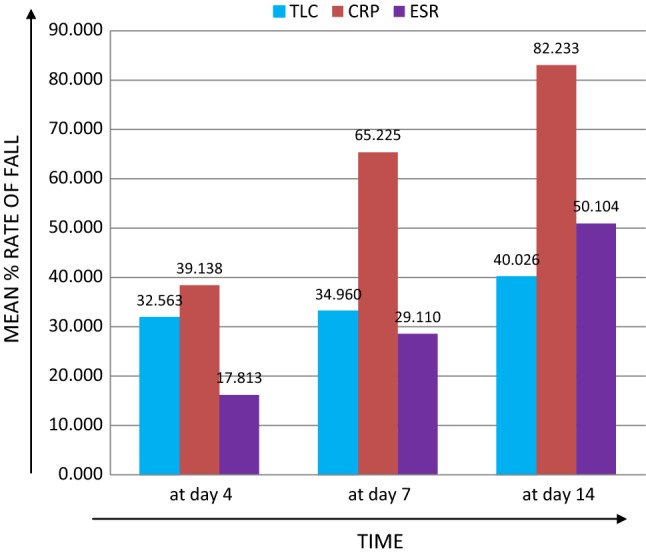
Mean %age rate of fall in WBC, ESR and CRP at different time periods
Discussion
Severe odontogenic infections are often unpredictable in terms of their course; hence, careful clinical analysis in conjunction with specific laboratory tests is required to reach a final diagnosis [3]. Although conventional measures to estimate infections such as WBC count [4] and ESR values are valuable in determining state of patient at the time of testing, predictability of these is worth limited thereby arising interest in more specific inflammatory markers [1].
Out of the various acute phase proteins, C-reactive protein is considered to be the most dynamic among the pentraxin protein family. The main biologic function of CRP is determined by its ability to recognize pathogens and damaged cells of the host and to mediate their elimination by recruiting the complement system and phagocytic cells [5]. Normal value of CRP ranges from 1 to 10 mg/L. Serum CRP is nearly absent in healthy individuals but increases to 1000-fold or more when tissue damage occurs during infection, tissue injuries and inflammation [6].
In the present study, the preoperative values of WBC count, CRP and ESR had a significant correlation with the severity of infection (p < 0.01) as far as pain and mouth opening were concerned. The results of the present study are supported by the study of Sharma et al. [7, 8], in which regression equation implied that CRP was a significant predictor of pain and mouth opening on the day of presentation. We found that on day 4, there was a significant correlation (r = 0.440; p = 0.015) between mouth opening and WBC count.
On day 7, a significant correlation between mouth opening and ESR showed that ESR is a late indicator of clinical state of the patient. Though the patients were markedly improved by day 7, the time taken for normalization of WBC count was 4 days on an average and for CRP between 7 and 14 days, but ESR had not fallen back to normal level even on day 14 thereby indicating persistent inflammatory state which further means that body needs nutritional support till this time [9].
Further, a highly significant correlation (p < 0.001) was present between clinical parameters determining the severity of infection (swelling, dysphagia, dyspnoea, body temperature, hoarseness of voice and active pus discharge) and three biochemical parameters preoperatively and on day 14. The results of the present study are supported by studies of Sharma et al. [7, 8] and Singh et al. [10] in which regression equation implied a direct linear relation between CRP and swelling, with CRP being a significant predictor of swelling. These results are also in accordance with those of Pepsy and Hirschfield [11], Hirschfield et al. [12] and Pinilla et al. [13] who found excellent correlation of circulating CRP concentrations with severity, extent and progression of disease process in their respective studies.
In the present study, the mean length of hospital stay was 2.16 days. A statistically significant relationship (p < 0.001) was observed between the length of hospital stay and all the three biochemical parameters. Also in accordance were the results of Seppanen et al. [14], Lemberg et al. [15] who found that patients without preceding treatment had the highest CRP levels and WBC counts, length of stay of such patients was also longer and they more often needed intensive care than the other patients. The results of the present study are supported by Sharma et al. [7], Ylijoki et al. [1], Sharma et al. [8] and Stathopoulos et al. [16].
In the present study, among the three biochemical markers, postoperatively there was rapid rate of fall in the CRP followed by WBC and ESR when compared to preoperative values. This showed that serum CRP reflected immediate effect of treatment. Studies by Ylijoki et al. [1] and Cunningham et al. [17] also support that CRP exhibited a rapid rise and fall of its serum levels with the inflammatory process which made it much more sensitive indicator of inflammation than ESR and WBC count.
Similarly, Shetty and Shah [6] reported that ESR, like CRP, increased significantly preoperatively in patients having odontogenic space infection and it remained significantly high in 1st week postoperatively. Also the decrease in ESR was significantly slower than the serum CRP. They found no significant change in the level of ESR before and after the treatment, thus leading to the conclusion that though both CRP and ESR were useful in diagnosis and monitoring of the disease and helped in prognosis, assessment of level of serum CRP was much more sensitive than ESR in relation to the fascial space infections of odontogenic origin. Similarly, Chana et al. [18] conducted a study on pediatric patients undergoing routine/emergency surgery by measuring CRP, ESR and general blood picture. They found that CRP levels were higher in patients having postoperative inflammation and more significant than other parameters like TLC and ESR.
CRP, WBC count and body temperature correlated with the clinical improvement, and their decrease toward the reference range signifies the resolution of infection. The results of the present study are further supported by Bali et al. [19] and Bagul et al. [20] who in their respective studies concluded that CRP and WBC count acted as good guide for determining the severity of infection in patients with fascial space infections of odontogenic origin.
In conclusion, the combination of CRP, ESR and WBC count reliably predicts the clinical course of odontogenic infection [9]. The quantitative determination of these serum markers can be used for determining not only the therapeutic efficacy of different treatment regimens of infection, but also the duration of antibiotic usage becomes more appropriate with them. Among the three biomarkers, there was earliest rise in the value of CRP at the time of presentation followed by rapid percentage rate of fall postoperatively. Therefore, CRP was considered as the best indicator of the regression of infection, followed by WBC count and ESR. However, the value of CRP must always be interpreted in the clinical context and should not be used alone as an indicator to rule out a specific diagnosis.
Acknowledgements
The authors would like to thank late Dr. Sumeet Sandhu for her guidance and support in conducting the present study.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval for Research Involving Human Participants
All procedures performed in the study involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all the individual participants included in the study.
Contributor Information
Amreen Kaur, Email: dramreen007@gmail.com.
Amneet Sandhu, Email: sandhuamneet@yahoo.com.
Tejinder Kaur, Email: tkgumber@gmail.com.
Ramandeep Singh Bhullar, Email: drbhullar07@gmail.com.
Amit Dhawan, Email: surg.amit@gmail.com.
Jasmine Kaur, Email: jasmine.rahul@gmail.com.
References
- 1.Ylijoki S, Hanelle JS, Suvronen R, Meurman JH, Lindquist C. Differences between patients with or without the need for intensive care due to severe odontogenic infections. J Oral Maxillofac Surg. 2001;59:867–872. doi: 10.1053/joms.2001.25017. [DOI] [PubMed] [Google Scholar]
- 2.Ren TF, Malmstrom HS. Rapid quantitative determination of C-reactive protein at chair side in dental emergency patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol. 2007;104:49–55. doi: 10.1016/j.tripleo.2007.01.007. [DOI] [PubMed] [Google Scholar]
- 3.Ayazi P, Mahyar A, Daneshi M, Hashemi HJ, Pirouzi M, Esmailzadehha N. Diagnostic accuracy of the quantitative C-reactive protein, erythrocyte sedimentation rate and white blood cell count in urinary tract infections among infants and children. Malays J Med Sci. 2013;20:40–46. [PMC free article] [PubMed] [Google Scholar]
- 4.Srivanitchapoom C, Sittitrai P, Pattarasakulchai T. Tananuvat R. Deep neck infection in Northern Thailand. Eur Arch Otorhinolaryngol. 2012;269(1):241–246. doi: 10.1007/s00405-011-1576-0. [DOI] [PubMed] [Google Scholar]
- 5.Volanakis JE. Human C-reactive protein: expression, structure, and function. Mol Immunol. 2001;38:189–197. doi: 10.1016/S0161-5890(01)00042-6. [DOI] [PubMed] [Google Scholar]
- 6.Shetty JN, Shah PD. A comparative biochemical evaluation of serum C-reactive protein and erythrocyte sedimentation rate in healthy individuals and patients having odontogenic infections. Int J Sci Res. 2013;2:460–461. [Google Scholar]
- 7.Sharma A, Gokkulakrishnan S, Shahi AK, Kumar V. Efficacy of serum CRP levels as monitoring tools for patients with fascial space infections of odontogenic origin: a clinicobiochemical study. Natl J Maxillofac Surg. 2012;3:148–151. doi: 10.4103/0975-5950.111369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sharma A, Giraddi G, Shahi AK. Efficacy of serum prealbumin and CRP levels as monitoring tools for patients with fascial space infections of odontogenic origin: a clinicobiochemical study. J Maxillofac Oral Surg. 2014;13(1):1–9. doi: 10.1007/s12663-012-0376-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Choi MK, Kim SB, Kim KD, Ament JD. Sequential changes of plasma CRP, ESR and WBC count in spine surgery: a comparison between lumbar open discotomy and posterior lumbar interbody fusion. J Korean Neurosurg Soc. 2014;56:218–223. doi: 10.3340/jkns.2014.56.3.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Singh WT, Singh WR, Devi WM, Devi NA. C-reactive protein as a monitoring tool for fascial space infections of odontogenic origin: a prospective study. IJCD. 2012;3(3):18–22. [Google Scholar]
- 11.Pepsy MB, Hirschfield GM. C-Reactive Protein: a critical update. J Clin Invest. 2003;111(12):1805–1812. doi: 10.1172/JCI200318921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hirschfield GM, Gallimore JR, Kahan MC, Hutchinson WL, Sabin CA, Benson GM, Dhillon AP, Tennent GA, Pepsy MB. C-reactive protein and cardiovascular disease: new insights from an old molecule. QJM. 2004;97(3):163–166. doi: 10.1093/qjmed/hch025. [DOI] [PubMed] [Google Scholar]
- 13.Pinilla JC, Hayes P, Laverty W, Arnold C, Laxdal V. C-reactive protein to prealbumin ratio correlates with the severity of multiple organ dysfunction. Surgery. 1998;124(4):799–805. doi: 10.1067/msy.1998.91365. [DOI] [PubMed] [Google Scholar]
- 14.Seppanen L, Lauhio A, Lindquist C, Suuronen R, Rautema R. Analysis of systemic and local odontogenic infection complications requiring hospital care. J Infect. 2008;57(2):116–122. doi: 10.1016/j.jinf.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 15.Lemberg KK, Seppanen L, Lauhio A, Lindquist C, Rautema R. Is dental treatment of an infected tooth a risk factor for locally invasive spread of infection? J Oral Maxillofac Surg. 2011;69(4):986–993. doi: 10.1016/j.joms.2010.05.015. [DOI] [PubMed] [Google Scholar]
- 16.Stathopoulos P, Igoumenakis D, Shuttleworth J, Smith W, Ameerally P. Predictive factors of hospital stay in patients with odontogenic maxillofacial infections: the role of C-reactive protein. Br J Oral Maxillofac Surg. 2017;55(4):367–370. doi: 10.1016/j.bjoms.2016.11.004. [DOI] [PubMed] [Google Scholar]
- 17.Cunningham RC, Knight AK. Inflammation and autoimmune complications of common variable immune deficiency. Autoimmun Rev. 2006;5(2):156–159. doi: 10.1016/j.autrev.2005.10.002. [DOI] [PubMed] [Google Scholar]
- 18.Chana RS, Khalid M, Redhu N, Nazir B, Khalid S, Jha A. Diagnostic value of ultrasonography in evaluation and management of acute abdominal condition in paediatric age group. Afr J Paediatric Surg. 2012;9(3):198–201. doi: 10.4103/0189-6725.104719. [DOI] [PubMed] [Google Scholar]
- 19.Bali R, Sharma P, Gaba S. Use of metronidazole as part of an empirical antibiotic regimen after incision and drainage of infections of the odontogenic spaces. Br J Oral Maxillofac Surg. 2015;53:18–22. doi: 10.1016/j.bjoms.2014.09.002. [DOI] [PubMed] [Google Scholar]
- 20.Bagul R, Chandan S, Sane VD, Patil S, Yadav D. Comparative evaluation of C-reactive protein and WBC count in fascial space infections of odontogenic origin. J Maxillofac Oral Surg. 2016 doi: 10.1007/s12663-016-0953-z. [DOI] [PMC free article] [PubMed] [Google Scholar]


