Abstract
Computational simulation models have potential to inform childhood obesity prevention efforts. To guide their future use in obesity prevention policies and programs, we assessed Baltimore City policymakers’ perceptions of computational simulation models. Our research team conducted 15 in-depth interviews with stakeholders (policymakers in government and non-profit sectors), then transcribed and coded them for analysis. We learned that informants had limited understanding of computational simulation modeling. Although they did not understand how the model was developed, they perceived the tool to be useful when applying for grants, adding to the evidence base for decision-making, piloting programs and policies, and visualizing data. Their concerns included quality and relevance of data used to support the model. Key recommendations for model design included a visual display with explanations to facilitate understanding and a formal method for gathering feedback during model development.
Keywords: Childhood obesity, Agent based model, Qualitative research, Policymakers
Introduction
In the United States, childhood obesity has reached epidemic levels [1]. It is a complex, multifaceted problem with multiple causal factors and a range of actors including families, schools, retailers, media, government, industry, and more [1, 2]. Computational simulation models are valuable in both studying and informing methods to combat this epidemic [2–7]. They can be explanatory, helping to better understand the mechanisms, relationships, and drivers of obesity and the relative impact of each causal factor [2, 3]. They can also be used to simulate ‘virtual experiments’ which highlight the trade-offs of proposed obesity policies and interventions [2, 3]. Virtual demonstration saves considerable time, effort, and resources that may otherwise be expended in trial and error [8–10]. Our team has developed one such computational simulation model, and this model has been validated to simulate the impact of multiple policies to reduce obesity [11–13].
Although computational simulation models are increasingly incorporated into public health research [8, 14–18], with underlying implications for policy and program development, there are only a few reported examples of policymakers using models in their decision-making [11, 19–22]. This reflects a larger issue in public health: the lack of policymakers incorporating research evidence into policy [23–25]. Policymakers want data to support health policy [26], but it is often difficult for them to translate evidence into policy [26, 27].
Early use of computational simulation models in health policy primarily focused on infectious disease control rather than prevention of chronic non-communicable conditions such as obesity [9, 10]. Within the field of childhood obesity, there are a few reported cases of policymakers using computational simulation models to directly inform decision-making [21, 22]. In 2015, our team collaborated with a member of the Baltimore City Council to support an urban farm tax credit that provided 90% tax credit to owners of vacant lots if they converted them into urban farms [22]. Our computational simulation model showed that this legislation would lead to increased fresh produce availability and consumption in low-income neighborhoods in Baltimore [22]. These results were presented to City Council in the form of a narrated video, which contributed to passage of the legislation [22]. Based on this work, we outlined five guiding principles for developing community-level models for obesity prevention. Here, we focus on the fifth: “make the model understandable and accessible to key decision-makers” [3].
Research aims
A key gap in current childhood obesity prevention is the infrequent use of computational simulation models to drive, support, or refute specific policies or programs [28]. Limited research has been done to assess the acceptability, perceived utility, or doubts about computational simulation modeling amongst policymakers in government and non-profit sectors working in childhood obesity prevention.
The primary aim of this study is to assess the perceptions of childhood obesity policy stakeholders in Baltimore, Maryland regarding the use of computational simulation modeling, such that researchers can incorporate these points of view into model development. Through our formative research, we address the following questions:
How well do Baltimore City policymakers understand computational simulation modeling?
How do they envision its utility in their work?
What are their doubts and concerns about using computational simulation modeling?
How can the model itself be designed to be most useful to policymakers?
Methods
We conducted 15 semi-structured in-depth interviews from April 2015–April 2016 with childhood obesity policy stakeholders in Baltimore, Maryland.
Sampling
We used purposive sampling to identify and recruit participants for our interviews. We used both maximum variation and snowball sampling. We approached 25 people and 15 agreed to participate. Participants included policymakers and other stakeholders involved in childhood obesity prevention policies and programs in Baltimore (Table 1). One of the informants had prior experience using computational simulation models.
Table 1.
Study participants
| Sector | Organization | Number of participants |
|---|---|---|
| Elected official | Maryland State Delegate | 1 |
| Baltimore City Council member | 3 | |
| Baltimore City government employee | City Council aides | 3 |
| Health Department | 3 | |
| Public Schools District | 1 | |
| Department of Planning | 1 | |
| Other | Family League after-school meals | 1 |
| Food-related non-profit | 2 | |
| Total | – | 15 |
Data collection
Eight members of the research team conducted in-depth interviews. Although each researcher had a background in public health and obesity research, none had experience with computational simulation modeling. Each member was trained in qualitative research methods with a special focus on in-depth interview skills, plus an overview of computational simulation modeling in public health.
Two interviewers attended each interview: one person asked questions and the other took notes to supplement an audio recording. Thirteen out of fifteen interviews had one interviewee, and two had a second interviewee present. Each interview, either at Johns Hopkins School of Public Health or at the interviewee’s workplace (e.g., Baltimore City Hall) lasted about 1 hour.
The interviews were semi-structured, with open-ended questions in a suggested order, allowing interviewers to deviate from specific questions to elicit new themes and information.
The first set of questions focused on the informant’s influence on Baltimore’s food and physical activity environment. The second set asked more specific questions about the informant’s perceptions of computational simulation modeling, based on a 2-minute mock-up visualization of the model (https://www.youtube.com/watch?v=MKCGu-GJ14M&feature=youtu.be).
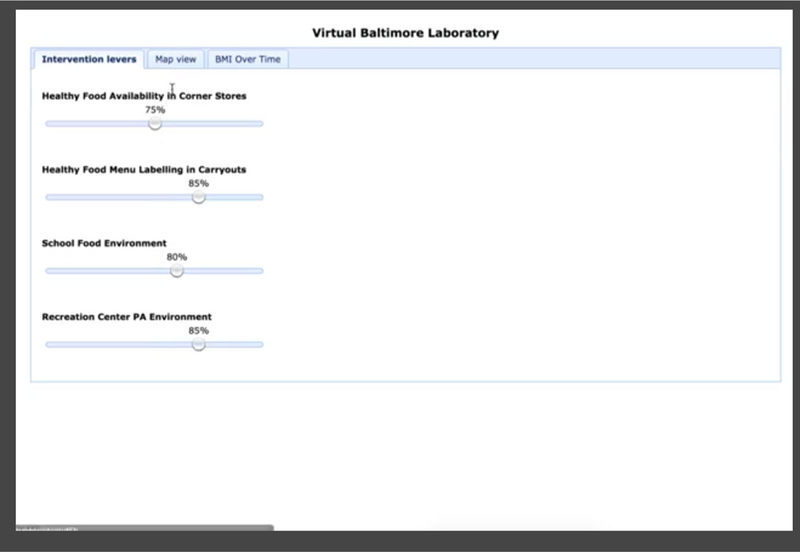
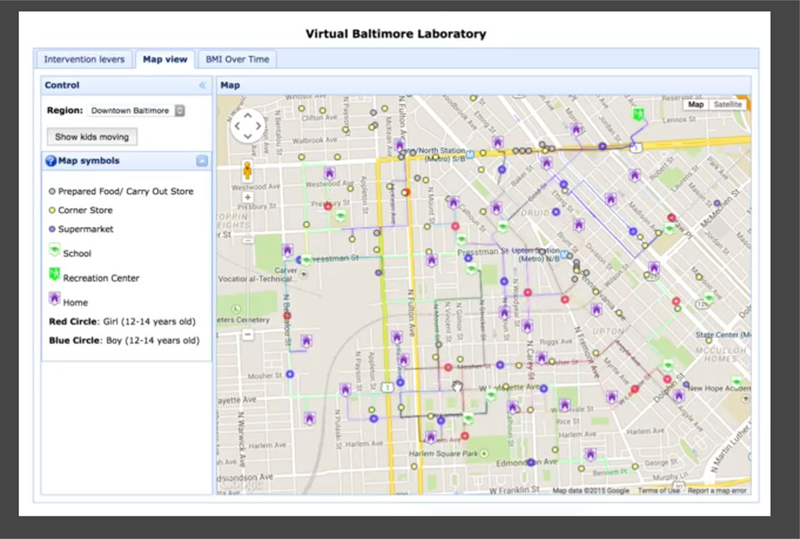
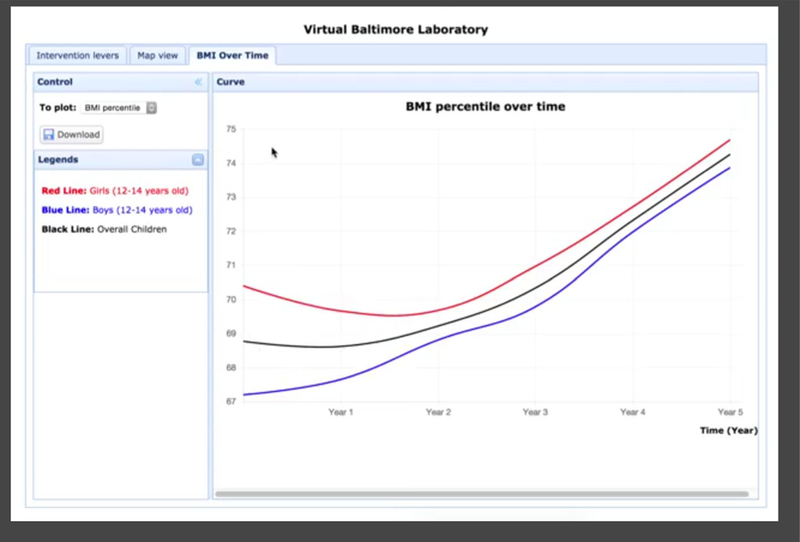
The video began with a screen showing sample inputs that a user could adjust (i.e., healthy food availability in corner stores) (Fig. 1). It then showed ‘agents’ (autonomous individuals; in this case, the agents are children) moving in a map, interacting with their environment (Fig. 2). The video ended with a screen showing sample outputs of the model in a graphic format [i.e., BMI (body mass index) percentile over time] (Fig. 3).
Fig. 1.
Screenshot from video demonstration of model: Adjusting inputs
Fig. 2.
Screenshot from video demonstration of model: Kids moving on map
Fig. 3.
Screenshot from video demonstration of model: Outputs
Interview guide questions included:
Please tell me about yourself and the work that you do.
What are your initial reactions to seeing the sample model?
If a particular food policy were to be changed based on the model, what unintended consequences do you foresee occurring?
Data analysis
Members of the research team transcribed interview recordings verbatim. One interview was unable to be transcribed due to poor quality of sound on the digital recorder and inadequate notes, so we did not analyze it. We used both deductive and inductive coding in the analysis. First, we developed an initial deductive codebook based on the questions in the interview guide. Next, two researchers developed an inductive codebook based on the emergent themes and concepts they found [29]. Finally, two researchers coded all of the interviews. They analyzed the coded data to identify emerging themes using qualitative data analysis software: Atlas. ti 7. (For a description of this tool, see http://atlasti.com/).
Johns Hopkins School of Public Health School Institutional Review Board deemed the project non-human subjects research. All research participants gave oral informed consent prior to any data collection. Interviews were recorded only with the informants’ permission.
Results
How policymakers understand computational simulation modeling
Most participants had a rudimentary understanding of computational simulation modeling after watching the video demonstration and hearing the interviewer explain the concept. Only two informants claimed that it was easy to understand. One stated, “I feel like it is intuitive because people play SIM games so… it [is] pretty self-explanatory.” Another said, “You know, it seems pretty straightforward.” However, others expressed confusion.
There were two primary gaps in the informants’ understanding of computational simulation models. First, several participants did not understand the concept of simulation itself, believing that the video demonstration showed the movement of real children in real time. One informant exclaimed, “So each of those blue dots is a kid? … That can’t be right, there are many more girls than boys!” Another asked, “So this is BMI percentile over time meaning – from when you started interviewing them? You followed a kid for 5 years?”
Second, most participants did not understand how computational simulation models are developed. Many believed that creating a computational simulation model required data collected from an entire population. For instance, one participant said, “But it will take a lot of time and energy to indicate the BMI for every single person to be able to show a very accurate, detailed approach… it will take two people and an entire summer to get 800 stores.”
How policymakers envision using computational simulation models
The overwhelming response of stakeholders was that computational simulation modeling could serve as a useful tool for them. Most informants had positive initial reactions after watching the video demonstration: “I think it’s really cool!” “That’s neat to look at, to watch.” “Everyone likes pictures and graphs.”
The participants described many potential uses for computational simulation modeling in their obesity prevention work. These fell into four primary categories:
-
Applying for grants and funding:
This would be extremely useful to me… our main funder is the federal office on women’s health and… they are very interested in more population-level changes and they ask us all the time what policies we’re influencing and what our research base is and what kind of evidence that we have to support that.
-
Efficient and inexpensive method for testing the impact of programs and policies:
For example, if I had this in that meeting with that guy who wanted to rezone… I would want him to be able to understand why we feel it’s important that he [rezone the city]. Using this [model]… he can understand and he can see, you know, the impact that his store could potentially have in his neighborhood.
-
Providing additional evidence for programs and policies:
You’ll really help their life a lot if you helped us…we need to be able to predict food deserts. So when a store closes, we do it now but it’s extremely cumbersome and time-consuming…. We rewind the entire map to be able to say what is the impact on the neighborhood with the store closure…. and [if] a store opens, we have to continue to recalculate every single time…
-
Visualizing data:
For me, maps are incredibly useful… particularly in the urban environment, to see the concentration of certain things and the depletion of certain [things]…like the concentration of corner stores and the lack of access.
In addition to those four general uses, every participant noted at least one specific question that they want a childhood obesity computational simulation model to answer. These questions were in one of three categories: questions meant to increase understanding of obesity and its contributing factors; questions about the impact of policies; or questions about the effectiveness of interventions. An example of one proposed question from each of the categories follows:
Increase understanding: How far do most kids travel to get to a recreation center or other recreational opportunities, and is that linked to health outcomes?
Policy impact: How does changing the stock requirements of corner stores for WIC and/or SNAP affect food deserts? Does it improve food access for residents or create more food deserts?
Intervention effectiveness: Are the up-front costs of the B’More Fit program worth it in terms of helping prevent costs of poor birth outcomes?
Policymakers’ concerns about using computational simulation models
Informants had several concerns about the use of computational simulation models. One common concern was the quality of the data used to support a model’s results. Many informants wanted reassurance that the data were of an acceptable quality so that they could feel confident in using a model’s results to inform their policies and programs. They explained that the data needed to be accurate, inclusive (of multiple subgroups, such as different income levels and racial breakdowns), and comprehensive. One participant said:
I have a hard time imagining how it would be useful to me unless you were going to increase the scale of interviews dramatically…. there is saying what is statistically likely and representative and there’s what’s overwhelming. Overwhelming is always – if you can do overwhelming, that’s best.
Informants were also concerned about the relevance of the model’s input data to their specific constituency. One informant, for example, said that he felt uncomfortable using a model’s results to inform policy unless these results were based on data that were specific to his own region of the city.
Other concerns included the time required to develop the model (a policymaker might need the information from the model faster than the researchers can produce it; one informant explained, “Sometimes things… in government… are like, ‘We need this now!”’); the validity of the specific measurements used in the model (for instance, one participant questioned the use of BMI, noting that it is a controversial measurement of obesity: “Well, let me just say I have my own issues around BMI…”); and the potential difficulty of policymakers and other stakeholders to understand the model (“For me, I’m okay with it. My concern is for people who are not working on their dissertation or not professional”).
Designing a computational simulation model most useful to policymakers
All of the informants emphasized the importance of a good graphical user interface for computational simulation models in childhood obesity policies and practices. They provided several recommendations for key elements of a visual display based on the visual display in the video demonstration during the interview. First, multiple participants highlighted the need for data transparency in the user interface; they suggested having an easily visible display of the data used to support the results. One informant, for example, said, “I think one thing that people are gonna want to see is an additional tab that shows methodology.” Others recommended including a list of research papers used to validate each result. Additionally, there was a suggestion to contextualize the results:
Yeah, there needs to be a better way to communicate that, so if it is BMI percentile, then have it color coded so that green is your healthy range, yellow is kind of danger range, red’s a bad range… [so] you could look at this and immediately know what’s good or bad.
A few informants recommended providing simple but comprehensive explanations to accompany the visual display to enhance understanding of the model, clearly detailing what is shown in the user interface. “I guess maybe some helpful information…for different audiences… [For example], here’s the map of Baltimore and here’s what it is now, and here’s what we want it to be; or here’s the goal: we want to increase our yellow dots by 7%.” Two other suggestions for the development of a graphical user interface were to use both graphs and bullet points to demonstrate each result, and to give the user the ability to see specific regions of interest on the map.
Participants also recommended incorporating a means of gathering regular feedback from policymakers and topic experts about the computational simulation model throughout the development process, noting that this is especially important because that sort of knowledge is not in the literature. One informant stated:
I’d say thinking about…what that…feasibility cap is for each of the interventions would be important, and I know we talked about this but urban farms, like, there are never going to be that many urban farms… so I think that’s something that’s, maybe, just, I don’t know if you’re going to find data on each thing or if it’s better to send an e-check to each one with stakeholders and be like does this even make sense…
Similarly, others highlighted the value of feedback from community groups and the public. One informant suggested a public forum: “So what would be the process for people submitting feedback or submitting other potential interventions… set it up as a public commentary?”
Informants differed in their opinions about the scope and scale of obesity-related computational simulation models. One informant said that a computational simulation model would be most useful for policymakers if it focused solely on obesity—rather than trying to include too many other public health concerns. Others found the flexibility and ability of computational simulation models to incorporate multiple health issues to be a benefit, and wanted to see them expanded.
A summary of the in-depth interview results is presented in Table 2.
Table 2.
Summary of Results
| Research question | Themes—brief summary | Sample representative quotes | |
|---|---|---|---|
| (1) How well do Baltimore City policymakers understand computational simulation modeling? | Easy to understand | “I feel like it is intuitive because people play SIM games so… it [is] pretty selfexplanatory” | |
| Confusion regarding the concept of simulation | “So this is BMI percentile over time meaning – from when you started interviewing them? You followed a kid for 5 years?” | ||
| Confusion about how a simulation model is developed | “But it will take a lot of time and energy to indicate the BMI for every single person to be able to show a very accurate, detailed approach… it will take two people and an entire summer to get 800 stores” | ||
| (2) How do they envision its utility in their work? | Uses for simulation models in obesity policy | Applying for grants and funding | “This would be extremely useful to me… our main funder is the federal office on women’s health and… they are very interested in more population-level changes and they ask us all the time what policies we’re influencing and what our research base is and what kind of evidence that we have to support that” |
| Efficient and inexpensive method for testing impact of programs and policies | “For example, if I had this in that meeting with that guy who wanted to rezone… I would want him to be able to understand why we feel it’s important that he [rezone the city]. Using this [model]… he can understand and he can see, you know, the impact that his store could potentially have in his neighborhood” | ||
| Providing additional evidence for programs and policies | “You’ll really help their life a lot if you helped us…we need to be able to predict food deserts. So when a store closes, we do it now but it’s extremely cumbersome and time-consuming…. We rewind the entire map to be able to say what is the impact on the neighborhood with the store closure…. and [if] a store opens, we have to continue to recalculate every single time…” | ||
| Visualizing data | “For me, maps are incredibly useful… particularly in the urban environment, to see the concentration of certain things and the depletion of certain [things]…like the concentration of corner stores and the lack of access” | ||
| Questions informants would like to ask a model—3 primary categories | Increase understanding of obesity and its contributing factors | “How far do most kids travel to get to a recreation center or other recreational opportunities, and is that linked to health outcomes?” | |
| See the impact of policies on communities | “How does changing the stock requirements of corner stores for WIC and/or SNAP affect food deserts? Does it improve food access for residents or create more food deserts?” | ||
| Assess effectiveness of interventions | “Are the up-front costs of the B’More Fit program worth it in terms of helping prevent costs of poor birth outcomes?” | ||
| (3) What are their doubts and concerns about utilizing computational simulation modeling? | Data need to be high quality, accurate, inclusive, comprehensive, and relevant to the constituency | “I have a hard time imagining how it would be useful to me unless you were going to increase the scale of interviews dramatically…. there is saying what is statistically likely and representative and there’s what’s overwhelming. Overwhelming is always – if you can do overwhelming, that’s best” | |
| Time to develop a model may not be fast enough for policymakers | “Sometimes things… in government… are like, “We need this now!”” | ||
| Validity of selected model inputs may be controversial (i.e., BMI) | “Well, let me just say I have my own issues around BMI…” | ||
| Model may be difficult for stakeholders to understand | “For me, I’m okay with it. My concern is for people who are not working on their dissertation or not professional” | ||
| (4) How can the model itself be designed to be most useful to policymakers? | Develop a good graphical user interface | “Yeah, there needs to be a better way to communicate that, so if it is BMI percentile, then have it color coded so that green is your healthy range, yellow is kind of danger range, red’s a bad range… [so] you could look at this and immediately know what’s good or bad” | |
| Keep data transparent in the user interface | “I think one thing that people are gonna want to see is an additional tab that shows methodology” | ||
| Provide comprehensive explanations about the model to accompany the visual display | “I guess maybe some helpful information…for different audiences… [For example], here’s the map of Baltimore and here’s what it is now, and here’s what we want it to be; or here’s the goal: we want to increase our yellow dots by 7%” | ||
| Incorporate feedback from policymakers and topic experts while developing the model | “I’d say thinking about…what that…feasibility cap is for each of the interventions would be important, and I know we talked about this but urban farms, like, there are never going to be that many urban farms… so I think that’s something that’s, maybe, just, I don’t know if you’re going to find data on each thing or if it’s better to send an e-check to each one with stakeholders and be like does this even make sense…” | ||
| Get feedback from public/community groups | “So what would be the process for people submitting feedback or submitting other potential interventions… set it up as a public commentary?” | ||
Discussion
Here, we assess the perspectives of Baltimore City policymakers in government and non-profit sectors regarding the utility of computational simulation modeling to inform local obesity-related programs and policies. These findings contribute to the growing body of research on systems science use in health policy, as well as the broader field of translating public health research into policy [23, 24].
Valuable tool for childhood obesity prevention policy
Computational simulation modeling can identify beneficial policies and interventions in a variety of public health settings and has strong potential to inform obesity prevention [2–8, 28]. Our results show that policy stakeholders agree with this: all of the informants offered positive feedback about incorporating computational simulation modeling into obesity-related policies and programs. They primarily saw its utility in supporting funding applications, piloting programs, adding to the evidence base for policies, and providing data visualization. The areas they identified reflect the need for innovative approaches to support obesity prevention efforts [4].
Computational simulation modeling is also a useful tool for addressing a diverse set of priorities [8–10]. Participants suggested a variety of inputs, outputs, and specific policy questions they would like to see a computational simulation model answer, based on their individual priorities—all of which can be tested in the model with the goal of finding win–win solutions.
Many of the informants pointed to the visualization of the map as a key benefit of the computational simulation model. This is a use of computational simulation modeling in public health that has not been emphasized in the literature. In exploring what type of user interface and visual display would be most useful for policymakers, researchers can turn to human-data interaction, a field that aims to optimize the usability of data and computer interfaces [30]. Principles from this field—for example, using artists rather than researchers to create data displays—can be used to help design a computational simulation model’s visual display [30].
Limited understanding of computational simulation models
Most of the informants were confused by the computational simulation model and had questions about how it worked. This highlights a need to make a simple user interface and provide a standardized explanation to accompany it, as suggested by the informants. Formal training sessions with policy stakeholders, which has been done in some cases, may also contribute to improved understanding [21]. Legislative support staff and advocacy organization members often serve as important sources of information for legislators [26, 27, 31], so including these groups in the training sessions is important. Moving forward, building policymakers’ capacity to understand and properly utilize the model will be important to inform meaningful programs and policies.
Addressing data concerns
The recurring theme of data—making it transparent and assuring its quality and relevance—must be addressed in future uses of computational simulation modeling in obesity-related policy. Informants wanted to see the data and come up with their own interpretations about data validity before believing the results. This is understandable as a poorly designed computational simulation model may unintentionally misinform obesity prevention efforts. There are numerous examples of well-intentioned obesity-related policies and programs that have led to undesired consequences [32]. Further, the quality of data in obesity research ranges widely [33]. As a result, computational simulation models should be carefully validated prior to use in obesity prevention. For policymakers, the consequences of designing a policy or program based on an inaccurate or misleading model can be dire, especially for elected officials who may be voted out of office. It is helpful to understand that policymakers view data through this critical lens—it suggests that learning what kinds of data policymakers consider relevant and trustworthy is important in designing a computational simulation model that is useful to them. Modelers and systems scientists need to be transparent with their data inputs and play a key role in educating policymakers on how to interpret model results.
Participatory approach to model design
Informants recommended gathering feedback from both policy stakeholders and the general public when designing a computational simulation model for public health policy. Our results suggest that engaging these stakeholders during model development, rather than presenting them with a completed product, makes the model more useful and trustworthy to them. Engaging the public is also important, as they are affected by these policies, so should have a way to express their concerns [34]. Increasing collaboration between researchers and policymakers will ultimately lead to a better understanding of one another’s work and in turn to increased use of public health evidence in policy [27, 35].
Limitations
Qualitative data studies cannot control for all the biases and limitations of researchers and participants involved. In our study, eight different researchers conducted the interviews, contributing to increased variation. Additionally, the interviewers did not have a thorough understanding of computational simulation models, limiting their ability to correct false assumptions informants made about the model. This was also, however, a strength, as it reduced bias in their questioning. Future interviewers should receive in-depth training about computational simulation modeling and use standardized descriptions when discussing it with informants. Several informants spoke at length about their work experiences, sometimes leaving little time to discuss computational simulation modeling. Further, two of the interviews had a second interviewee present. This may have affected responses, making them more or less likely to agree with one another rather than offer their true thoughts.
Another limitation of this study was the informants’ lack of understanding of computational simulation modeling. This prevented them from being as critical of computational simulation models as they might have been. Future work should provide informants with a more detailed overview of computational simulation models to improve their level of understanding prior to the interview.
The visual demonstration of the computational simulation model shown during interviews was not the actual model. The video was created to demonstrate what a potential user interface could look like, and to enhance understanding of a computational simulation model as it was a new concept for most policymakers. Showing informants this specific video demonstration of a model likely affected their interpretation of a computational simulation model’s value and utility. In future research, different types of possible user interfaces should be used so that policymakers are not biased by one visualization.
Finally, in-depth interviews are only one type of formative research. Additional research methods should be used to further explore policymakers’ perceptions of computational simulation models, including surveys with directed questions to allow for quantitative evaluation and focus groups to allow for stimulating new ideas and discussion amongst participants.
Conclusion
Our formative research highlights the perceptions of Baltimore City policymakers regarding the use of computational simulation models in childhood obesity policies and programs. Policymakers appear to be excited to use these models to inform obesity prevention policies and programs. Visualization and feedback are valued. Data used in the model should be transparent and of high quality. Finally, policymakers’ understanding of the model inputs and how to interpret the model outputs is key to using it effectively.
Acknowledgements
We acknowledge all stakeholders who participated in the Policy Working Group. We also thank the following students, staff, and volunteers: Andrew Seiden, Naomi Rapp, Stacy Nam, Jenny Brooks, Kripa Rajagopalan, and Harmony Farner. This project was supported by Grant Number U54HD070725 from Eunice Kennedy Shriver National Institute of Child Health & Human Development (NICHD). The project was co-funded by NICHD and Office of Behavioral and Social Sciences Research (OBSSR). The content is solely the responsibility of the authors and does not represent the official views of NICHD or OBSSR. Additional funding was supported by Grant Number U48DP005045 and 1U48DP000040, SIP 14-027 from the Centers for Disease Control and Prevention.
Biography
Leah Seifu MD, MPH, graduated from Harvard University with a bachelor’s degree in Human Evolutionary Biology and a minor in Global Health and Health Policy in 2011. She worked as a Clinical Research Coordinator at the World Trade Center Health Program of Mount Sinai in New York City. In 2012, she began medical school at the University of Pennsylvania and completed her MPH at Johns Hopkins School of Public Health in 2015. She graduated from medical school in 2017 and is now completing her pediatrics residency at the Children’s Hospital of Philadelphia. Leah’s primary interests include child health, early childhood development, nutrition, and global health.
Cara Ruggiero RD, LDN, studied Dietetics at the University of Delaware and completed her dietetic internship at University of Maryland Medical Center, focusing her staff relief in pediatrics. She has a background working in obesity and food access research at Johns Hopkins School of Public Health in the Center for Human Nutrition and the Global Obesity Prevention Center. Cara is now a doctoral student at Pennsylvania State University Childhood Obesity Research Center. She is dedicated to focusing her career on childhood obesity in low-income communities and hopes to design studies that combine her clinical foundation with public health solutions.
Marie Ferguson MSPH, is research faculty at the Global Obesity Prevention Center (GOPC). She joined the GOPC in 2015 after graduating from Johns Hopkins Bloomberg School of Public Health with her MSPH in Health Education and Health Communication. As research associate, she is responsible for coordinating and managing Systems Science Core modeling projects. Marie is primarily interested in applying computational modeling approaches to advance programs and policies that address obesity and promote an equitable, sustainable, and healthy food system.
Yeeli Mui PhD, earned her doctorate degree at Johns Hopkins School of Public Health. Mui’s research focuses on improving the neighborhood built and social context to one that fosters a culture of healthy eating and living. Her dissertation used geospatial longitudinal data to investigate the role of neighborhood crime and abandoned homes in an urban food system. Currently, Mui is a Postdoctoral Associate at University at Buffalo in the Community of Global Health Equity where she is aiming to better understand and address food inequities in the Global South.
Bruce Y. Lee MD, MBA is associate professor of International Health at the Johns Hopkins Bloomberg School of Public Health, Executive Director of the Global Obesity Prevention Center (GOPC) at Johns Hopkins and Director of Operations Research at the International Vaccine Access Center (IVAC) as well as associate professor at the Johns Hopkins Carey Business School. He has over 15 years of experience in industry and academia in systems science and developing and implementing mathematical and computational methods, models, and tools to assist decision-making in public health and medicine.
Joel Gittelsohn PhD, MSc, Professor, Department of International Health, Johns Hopkins University, is a medical anthropologist who specializes in the use of qualitative and quantitative information to design, implement, and evaluate health and nutrition intervention programs. Dr. Gittelsohn integrates qualitative and quantitative approaches to better understand culture-based beliefs and behaviors regarding dietary patterns, and how these factors influence the success or failure of dietary and lifestyle modification strategies. He has worked on chronic disease interventions among the White Mountain and San Carlos Apache, the Ojibwa-Cree, African Americans, and children and adults in the Republic of the Marshall Islands.
References
- 1.Centers for Disease Control and Prevention. Childhood Obesity Facts 2015. http://www.cdc.gov/obesity/data/childhood.html. Accessed 15 Aug 2016.
- 2.Bures RM, Mabry PL, Orleans CT, Esposito L. Systems science: a tool for understanding obesity. Am J Public Health 2014;104(7):1156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gittelsohn J, Mui Y, Adam A, et al. Incorporating systems science principles into the development of obesity prevention interventions: principles, benefits, and challenges. Curr Obes Rep 2015;4(2):174–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee BY, Bartsch SM, Mui Y, et al. A systems approach to obesity. Nutr Rev 2017;75(Suppl. 1):94–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hennessy E, Ornstein JT, Economos CD, et al. Designing an agent-based model for childhood obesity interventions: a case study of child obesity180. Prev Chronic Dis 2016;13:150414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mabry PL, Bures RM. Systems science for obesity-related research questions: an introduction to the theme issue. Am J Public Health 2014;104(7):1157–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Steeves EA, Martins PA, Gittelsohn J. Changing the food environment for obesity prevention: key gaps and future directions. Curr Obes Rep 2014;3(4):451–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Luke DA, Stamatakis KA. Systems science methods in public health: dynamics, networks, and agents. Annu Rev Public Health 2012;33:357–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Macal C, North M. Tutorial on agent-based modelling and simulation. J Simul 2010;4:151–62. [Google Scholar]
- 10.Maglio PP, Mabry PL. Agent-based models and systems science approaches to public health. Am J Prev Med 2011;40(3):392–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee BY, Ferguson MC, Hertenstein DL, et al. Simulating the impact of sugar-sweetened beverage warning labels in three cities. Am J Prev Med 2017. 10.1016/j.amepre.2017.11.003. [DOI] [PMC free article] [PubMed]
- 12.Lee BY, Adam A, Zenkov E, et al. Modeling the economic and health impact of increasing children’s physical activity in the United States. Health Aff 2017;36(5):902–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Powell-Wiley TM, Wong MS, Adu-Brimpong J, et al. Simulating the impact of crime on African American women’s physical activity and obesity. J Obes 2017;25:2149–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Levy DT, Bauer JE, Lee HR. Simulation modeling and tobacco control: creating more robust public health policies. Am J Public Health 2006;96(3):494–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Homer J, Wile K, Yarnoff B, et al. Using simulation to compare established and emerging interventions to reduce cardiovascular disease risk in the United States. Prev Chronic Dis 2014;11:E195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ferencik R, Minyard K. Systems thinking in injury prevention: an innovative model for informing state and local policies. West J Emerg Med 2011;12(3):273–4. [PMC free article] [PubMed] [Google Scholar]
- 17.Lee BY, Wong KF, Bartsch SM, et al. The Regional Healthcare Ecosystem Analyst (RHEA): a simulation modeling tool to assist infectious disease control in a health system. J Am Med Inform Assoc 2013;20(e1):e139–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee BY, Brown ST, Cooley P, et al. Simulating school closure strategies to mitigate an influenza epidemic. J Public Health Manag Pract 2010;16(3):252–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guariguata L, Guell C, Samuels TA, et al. Systems science for caribbean health: the development and piloting of a model for guiding policy on diabetes in the Caribbean. Health Res Policy Syst 2016;14:79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gauvreau CL, Fitzgerald NR, Memon S, et al. The onco-sim model: development and use for better decision-making in canadian cancer control. Curr Oncol 2017;24(6):401–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Powell KE, Kibbe DL, Ferencik R, et al. Systems thinking and simulation modeling to inform childhood obesity policy and practice. Public Health Rep 2017;132(Suppl. 2):33S–8S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gittelsohn J, Mui Y, Lin S, et al. Simulating the impact of an urban farm tax credit policy in a low income urban setting. Harvard Heal Policy Rev 2015;15(1):30–3. [Google Scholar]
- 23.Brownson RC, Fielding JE, Maylahn CM. Evidence-based decision making to improve public health practice. Front Public Health Serv Syst Res 2013;2(2). [Google Scholar]
- 24.Lavis JN, Oxman AD, Lewin S, Fretheim A. Support tools for evidence-informed health policymaking. Health Res Policy Syst 2009;7(Suppl. 1):I1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li Y, Kong N, Lawley M, et al. Advancing the use of evidence-based decision-making in local health departments with systems science methodologies. Am J Public Health 2015;105(Suppl. 2):S217–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dodson EA, Geary NA, Brownson RC. State legislators’ sources and use of information: bridging the gap between research and policy. Health Educ Res 2015;30(6):840–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brownson RC, Royer CR, Ewing R, McBridge TD. Researchers and policymakers: travelers in parallel universes. Am J Prev Med 2006;30(2):164–72. [DOI] [PubMed] [Google Scholar]
- 28.Skinner AC, Foster EM. Systems science and childhood obesity: a systematic review and new directions. J Obes 2013;2013:129193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Saldaña JM. The coding manual for qualitative researchers 3rd ed. Los Angeles: Sage; 2009. [Google Scholar]
- 30.Mortier R, Haddadi H, Henderson T, et al. Challenges and opportunities in human-data interaction. In: Proceedings of DE2013: Open Digital—The Fourth Annual Digital Economy All Hands Meeting. 2013. http://www.eecs.qmul.ac.uk/~hamed/papers/hdi2013.pdf. [Google Scholar]
- 31.Tabak RG, Eyler AA, Dodson EA, Brownson RC. Accessing evidence to inform public health policy: a study to enhance advocacy. Public Health 2015;129(6):698–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Brown AW, Allison DB. Unintended consequences of obesity-targeted health policy. Virtual Mentor 2013;15(4):339–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Richardson MB, Williams MS, Fontaine KR, Allison DB. The development of scientific evidence for health policies for obesity: why and how? Int J Obes 2017;41(6):840–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Oxman AD, Lewin S, Lavis JN, Fretheim A. SUPPORT Tools for evidence-informed health policymaking 15: engaging the public in evidence-informed policymaking. Health Res Policy Syst 2009;7(Suppl. 1):S15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Atkinson JM, Wells R, Page A, et al. Applications of system dynamics modeling to support health policy. Public Health Res Pract 2015;25(3):e2531531. [DOI] [PubMed] [Google Scholar]