Summary
The purpose of this study was to identify changes in the competence of healthcare providers who underwent training courses on the management of burns incidents. Theoretical and practical simulation training courses were conducted for 305 healthcare providers from emergency and trauma departments of general hospitals in Vietnam. Pre- and post-tests were conducted using questionnaires and with simulated practical skill evaluation by burns specialists. Results showed a significant improvement in knowledge of emergency management of burns incidents, with an increase in percentage of correct answers from 48.2% to 71.6% (p < .01). There was an average increase from 10.5% to 95.1% for the correct calculation of total body surface area involvement, and from 33.8% to 67.2% for using the Parkland formula. Increases in knowledge of resuscitation and management of inhalation injury were also noted (p < .01). For the management of major burns incidents, sufficient knowledge of the command system increased from 58.4% to 81.9%. A better understanding was gained of the missions of the Emergency Medical Team, triage and air evacuation after training (p < .001). Emergency practical skills such as CPR, ET intubation, splinting of bone fractures, burn wound dressing and using emergency medical devices also improved remarkably (p < .001) after practical simulation training. In conclusion, these results indicate that a significant improvement in the capabilities and competence of medical staff in the emergency management of burn injuries can be achieved by conducting training courses with combined theory components and practical simulation models.
Keywords: mass burn incident, training course, knowledge, practical skills
Abstract
Le but de cet étude était d’évaluer les changements de compétence des professionnels de santé ayant suivi une formation à la prise en charge des brûlés en situation de catastrophe. Une formation théorique et pratique (simulation) a été réalisée au profit de 305 professionnels de santé de services d’urgence et de traumatologie vietnamiens. Des questionnaires ont été remplis avant et après formation et les simulations ont été évaluées par des brûlologues. Les bonnes réponses aux questionnaires passent de 48,2 à 71,6% après formation (p<0,01). L’exactitude de l’évaluation de la SB est passé de 10,5 à 95,1%, l’adéquation du remplissage (Parkland) de 33,8 à 67,2%. La prise en charge de l’inhalation de fumées a aussi été améliorée (p<0,01). Pour ce qui est de la catastrophe, les connaissances sur les échelons de commandement étaient correctes dans 58,4% des cas avant, 81,9% après. De même, la compréhension du rôle de l’équipe médicale, du triage et de l’évacuation aéroportée s’est améliorée (p<0,001). L’amélioration est nette aussi (p<0,001) concernant les gestes d’urgences comme le massage cardiaque, l’intubation trachéale, l’immobilisation des fractures, les pansements de brûlure et l’utilisation du matériel. Cette étude montre qu’une nette amélioration des compétences des équipes dans la prise en charge en urgence des brûlés peut être améliorée au moyen d’une formation mixte théorique et pratique.
Introduction
The medical management of major burns incidents is more difficult than the management of other types of trauma.
The reasons for this are unforeseen occurring accidents, a potentially large number of patients with severe cutaneous burn injuries, inhalation injuries and concomitant trauma at the same time.
Thus, there is an immediate demand for a large amount of medications, equipment and medical professionals.1,2,3
In addition, it is important to note that healthcare providers who participate in the pre-hospital and/or inpatient hospital phase of mass burn injury management must have sufficient knowledge of and practical skills in emergency care, triage and transportation of these critical patients.4,5
Continuing medical education (CME) is the most common model for updating knowledge, skills and competence among healthcare providers.
Theoretical and practical knowledge, as well as experience, can be improved and maintained through training in a simulated environment.6,7 In addition, practical simulation training is an effective method for improving the clinical skills of healthcare providers in both pre-hospital and in-patient phases of emergency management of mass casualty incidents.8,9,10
Despite significant efforts, limited knowledge and practical skills in medical response to disasters involving mass burn incidents continue to be reported.11,12,13,14
Similar to other developing countries, recent reports in Vietnam indicate the limited knowledge of healthcare providers as far as emergency management of mass burn injuries is concerned.15,16 In order to improve the situation, training courses have been conducted.
This study attempted to evaluate changes in knowledge and emergency practical skills for the management of burns incidents amongst healthcare providers who had taken part in training courses.
Materials and methods
Between August and October 2016, three training courses were conducted for 305 healthcare providers including physicians and nurses working in emergency and trauma departments of district and provincial general hospitals in Vietnam. The educational curriculum included 8 hours of lectures in theory and 4 hours of practice on mannequins. Materials were designed by burns specialists at the National Institute of Burns. Pre- and post-tests were conducted using questionnaires and with simulated practical examination evaluated by the burns specialists.
The test contents included basic knowledge of burn extent estimation, fluid resuscitation using the Parkland formula, manifestation and emergency management of inhalation injury, and knowledge of mass burn injury management including the command system, missions of the emergency medical team (EMT), triage, appropriate methods of fluid resuscitation and air evacuation. Overall knowledge level was defined as percentage of correct answers. Simulated emergency practical techniques such as basic cardiopulmonary resuscitation (CPR), endotracheal (ET) intubation, peripheral intravenous access, splinting of bone fracture(s), burn wound dressing and the use of emergency medical devices (defibrillator, infusion pump, monitor, basic mechanical ventilator) were included in the simulation training on mannequins, and the outcomes were evaluated by burns specialists.
Data was calculated as percentage of correct answers, tabulated and analyzed. Paired t-tests of preand post-training courses were applied using Stata 11.0 software. P value ≤ .05 was considered as the significant level.
Results
Of 305 healthcare providers, 155 (50.8%) worked at provincial hospitals and 174 participants were physicians, accounting for 57.1%. There was a predominance of males (n=198, 64.9%) and 51.8% (n=158) participants had less than 5 years of working experience (Table I).
Table I. Characteristics of participants (n=305).
Knowledge of emergency burns management was significantly improved after the training courses. Percentage of correct calculation of burn extent and required fluid resuscitation using the Parkland formula increased from 10.5% to 95.1% and from 33.8% to 67.2% respectively (p < .001). Moreover, there was a significant gain in knowledge of evaluation of fluid resuscitation (from 14.8% to 82%; p < .001) and the diagnosis of inhalation injuries and emergency management (from 49.2% to 86.9%; p < .001) (Table II).
Table II. Knowledge of burn emergency management (n= 305).
Regarding mass burn injury management, Table III shows that there was a significant improvement of all contents. Sufficient understanding of the command system had increased from 58.4% to 81.9%. Mission of burn EMT was also better understood after the training courses (from 90.2% to 100%; p < .001). In addition, increased knowledge of triage, fluid resuscitation and air evacuation was also recorded (p < .001).
Table III. Knowledge of major burns incidents (n= 305).
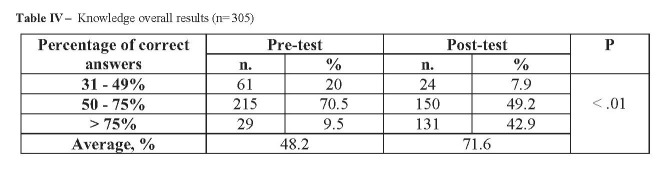
Overall results for participant knowledge are indicated in Table IV. A significant change in percentage of correct answers was recorded (from 48.2% to 71.6%; p < .01). Participants with more than 75% correct answers had increased from 9.5% to 42.9% (p < .001). Meanwhile, the rate of those with less than 50% correct answers had significantly decreased, from 20% to 7.9% (p < .001).
Table IV. Knowledge overall results (n= 305).
The results of simulated practical skill evaluations are shown in Table V. Before simulation training, CPR was correctly performed by 44.9% of participants: after training this rate increased significantly to 91.8% (p < .001). Successful endotracheal intubation rate increased from 38% to 82% (p < .001). Incidence of correct splinting for bone fracture( s) increased from 47.5% to 81.3%. The same situation was also recorded for burn wound dressing and peripheral intravenous access (from 24.6% to 68.5% and from 33.6% to 60.3% respectively, p < .001). Correctly using emergency medical devices (defibrillator, monitor, infusion pumps and mechanical ventilator) also improved (from 33.8% to 64.9%, p < .001).
Table V. Results of practical skills evaluation (n= 305).
Discussion
Despite extensive efforts, healthcare providers may not be adequately prepared for disasters. Most reports in the literature indicate that healthcare providers and medical supporters need further training on emergency disaster management.5,11,17,18 For example, a survey by Berhanu et al. showed that about 25% of participants did not understand the basic steps of “ABC” in first aid management of trauma. About a third had inadequate knowledge of the disaster response cycle. In addition, only 20.6% of the respondents had been trained in disaster-related topics in the two years prior to the survey.19 Chokshi and colleagues conducted an online survey, involving members of the American Pediatric Surgical Association, on experience, perceived preparation, responsibility attitudes, willingness and readiness to take part in a disaster response. Results indicated that 77% of respondents certainly felt responsible for helping out during a disaster but only 24% felt definitely prepared for disaster response. Moreover, most felt they needed additional training. 20 In 2018, Naser and Saleem conducted a survey of healthcare professionals, which indicated that only one third of the participants had sufficient knowledge of disaster planning. A total of 41% of respondents had never attended a training course. Only 13.5% had participated in triage exercises.21 In 2015, Hodge et al. reported from their study that nearly half of nurses (44.6%) rated themselves as unprepared for a disaster.22 Moreover, in 2018, a systematic review by Labrague and co-workers on preparedness for disasters showed that nurses were insufficiently prepared and were not confident they could respond effectively to disasters.23
CME plays an important role in updating the knowledge and practical skills of medical staff, not only for their normal working day but also for mass casualty incidents. CME assists medical staff in understanding, being ready for and feeling confident about mass injury management procedures.24 It is also noted that the development of a standardized, accessible simulation training platform system can reduce medical errors and stress levels in medical practices.25,26,27 Simulation is also considered to be a positive training and education method for medical staff. It provides opportunities to facilitate assessment, treatment and implementation of procedures and devices under realistic conditions.1,8,28 Classroom training and simulation can overcome the problem of “dead‐document” phenomenon or “paper‐plan syndrome”.29 It is also noted that simulation learning involves theory, and practical skills can be applied and integrated with already existing skills. The simulation creates experiences and helps participants to gain a better understanding of the clinical presentation of actual disease or injury.7,9
In fact, the effectiveness of such training courses has been reported worldwide. O’Brien and colleagues demonstrated an improvement in three aspects, namely disaster planning, community linkages and collaborations, and emergency response exercises.30 Works by Idrose and co-workers indicated that classroom training and simulation effectively improved knowledge of disaster planning at low cost and were relatively easy to conduct. There was a mean gain from 47.3 (18.8%) to 84.0 (18.7%) in the post‐test (p < 0.05), and all levels of participants could be grouped together for training.31 Classroom training and simulation can overcome the problem of “dead‐document” phenomenon or “paper‐plan syndrome”.
In 2012, a report by Vincent et al. showed that the mannequin-based simulation model improved understanding of mass casualty triage among healthcare providers from Asia Pacific regions.32 In 2006, Pryor et al. evaluated the change in perceptions of responding to weapons of mass destruction events using the tabletop/real-time-exercise format. There was a consistent improvement in self-rated capabilities after course completion for all 21 capability statements.33 Sahu & Lata also indicated multiple areas where simulation appeared to be useful for training physicians in emergency departments. The standardization of such simulation training could improve overall patient care during times of high demand, and even when the availability of senior staff is limited.34
Regarding the management of burns and major burn incidents, current reports show insufficient teaching in burns management and inadequate skills of medical staff in airway management, CPR, triage, and assessing and managing burns victims.35 Numerous surveys have indicated that, before training courses, many healthcare providers may not be ready or feel confident about medical responses in the event of a burns disaster.36,37,38,39 Our previous survey also indicated limitations, with an overall rate of sufficient knowledge of 39.7% correct answers for nurses and 45.4% for physicians.15,16 The same situation was reported by Kut et al..40 In 2007, Wetta-Hall et al. conducted a continuing education program on management of multiple burn incidents for healthcare practitioners. The percentage of correct responses increased from 30% to 65%. In addition, 64% of participants felt they were able to manage multiple burn casualties after the training program. 41,42 Based on the surveyed demand, in 2015 McWilliam et al. conducted a training program on burn emergency management using video conference with positive outcomes.39 Kua Phek Hui et al (2016) conducted an emergency burns management training course for 274 healthcare providers at a paediatric trauma centre in Singapore using the European guidelines. The post-test results indicated a significant improvement in knowledge.43 Our posttraining results also demonstrated an improvement in the knowledge, practical skills and self-confidence of participants regarding the management of mass burns injuries.
It is also important to note that the training program should be repeated to maintain perception and practical skills.29,44 Schenker and colleagues, in 2006, evaluated results of victim triage using the START protocol at a fire simulation scene with 130 victims. All the participants had been trained in the past but training had not been repeated before the drill. The rate of correct triage was only 78%, and this fell further to 62% when the status of victims changed during the triage process.45
Conclusion
Our results showed that conducting training courses that combine theory with practical simulations leads to a significant improvement in the capabilities and competence of medical staff regarding the emergency management of major burn incidents.
Acknowledgments
Acknowledgements.We are grateful to staff at the National Institute of Burns, Hanoi, for helping us to collect data.
References
- 1.Haberal M. Guidelines for dealing with disaster involving large numbers of intensive burns. Burns. 2006;32:933–939. doi: 10.1016/j.burns.2006.08.026. [DOI] [PubMed] [Google Scholar]
- 2.Kim SJ, Kim CH, Shin SD, Lee SC. Incidence and mortality rate of disasters and mass casualty incidents in Korea: A population-based cross-sectional study, 2000–2009. J Korean Med Sci. 2013;28:658–666. doi: 10.3346/jkms.2013.28.5.658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ngim RCK. Burns mass disasters in Singapore – a three-decade review with implications for future planning. Singapore Med J. 1994;35:47–49. [PubMed] [Google Scholar]
- 4.Atiyeh B, Gunn WS, Dibo S. Primary triage of mass burn casualties with associated severe traumatic injuries. Ann Burns Fire Disasters. 2013;26(1):48–52. [PMC free article] [PubMed] [Google Scholar]
- 5.Baack S, Alfred D. Nurses’ preparedness and perceived competence in managing disasters. J Nurs Scholarsh. 2013;45(3):281–287. doi: 10.1111/jnu.12029. [DOI] [PubMed] [Google Scholar]
- 6.Abelsson A, Lundberg L. Trauma simulation in pre-hospital emergency care. Trauma Nurs. 2018;25(3):201–204. doi: 10.1097/JTN.0000000000000370. [DOI] [PubMed] [Google Scholar]
- 7.Steinemann S, Berg B, Skinner A, DiTulio A. In situ, multidisciplinary, simulation-based teamwork training improves early trauma care. J Surg Educ. 2011;68(6):472–477. doi: 10.1016/j.jsurg.2011.05.009. https://www.ncbi.nlm.nih.gov/pubmed/22000533 . [DOI] [PubMed] [Google Scholar]
- 8.Abelsson A, Rystedt I, Suserud BO, Lindwall L. Mapping the use of simulation in prehospital care - a literature review. Scand J Trauma Resusc Emerg Med. 2014;28(22):22. doi: 10.1186/1757-7241-22-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Abelsson A, Rystedt I, Suserud BO, Lindwall L. Learning by simulation in prehospital emergency care - an integrative literature review. Scand J Caring Sci. 2016;30(2):234–240. doi: 10.1111/scs.12252. [DOI] [PubMed] [Google Scholar]
- 10.Seynaeve G, Archer F, Fisher J, Lueger-Schuster B. International standards and guidelines on education and training for the multi-disciplinary health response to major events that threaten the health status of a community. Prehosp Disaster Med. 2004;19(2):S17–S30. [PubMed] [Google Scholar]
- 11.Gowing JR, Walker KN, Elmer SL, Cummings EA. Disaster preparedness among health professionals and support staff: what is effective? An integrative literature review. Prehosp Disaster Med. 2017;32(3):321–328. doi: 10.1017/S1049023X1700019X. [DOI] [PubMed] [Google Scholar]
- 12.Hammond JS, Ward CG. Transfers from emergency room to burn center: errors in burn size estimate. Journal of Trauma. 1987;27(10):1161–1165. doi: 10.1097/00005373-198710000-00011. [DOI] [PubMed] [Google Scholar]
- 13.Rea S, Kuthubutheen J, Fowler B, Wood FF. Burn first aid in Western Australia – Do healthcare workers have the knowledge? Burns. 2005;31:1029–1034. doi: 10.1016/j.burns.2005.05.010. [DOI] [PubMed] [Google Scholar]
- 14.Wong K, Turner PS, Boppana A, Nugent Z. Preparation for the next major incident: are we ready? Emerg Med J. 2006;23:709–712. doi: 10.1136/emj.2005.034025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lam NN, Huong HTX, Tuan CA. Knowledge on emergency management for burn and mass burn injuries amongst physicians working at emergency and trauma departments. Ann Burns Fire Disasters. 2018;3(2):138–143. [PMC free article] [PubMed] [Google Scholar]
- 16.Lam NN, Huong HTX, Tuan CA. Nurse knowledge of emergency management for burn and mass burn injuries. Ann Burns Fire Disasters. 2018;31(3):246–250. [PMC free article] [PubMed] [Google Scholar]
- 17.Madge SN, Kersey J, Murray G, Murray JR. Are we training junior doctors to respond to major incident? A survey of doctors in the Wesses region. Emerg Med J. 2004;21:577–579. doi: 10.1136/emj.2002.004606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Robison JL. Army nurses’ knowledge base for determining triage categories in a mass casualty. Mil Med. 2002;167(10):812–816. [PubMed] [Google Scholar]
- 19.Berhanu N, Abrha H, Ejigu Y, Woldemichael K. Knowledge, experiences and training needs of health professionals about disaster preparedness and response in Southwest Ethiopia: a cross sectional study. Ethiop J Health Sci. 2016;26(5):415–426. doi: 10.4314/ejhs.v26i5.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chokshi NK, Behar S, Nager AL, Dorey F, Upperman JS. Disaster management among pediatric surgeons: preparedness, training and involvement. Am J Disaster Med. 2008;3(1):5–14. [PubMed] [Google Scholar]
- 21.Naser WN, Saleem HB. Emergency and disaster management training; knowledge and attitude of Yemeni health professionals-a cross-sectional study. BMC Emerg Med. 2018;18(1):23. doi: 10.1186/s12873-018-0174-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hodge AJ, Miller EL, Skaggs MKD. Nursing self-perceptions of emergency preparedness at a rural hospital. J Emerg Nurs, Advanced Online Publication. 2015;43(1):10–14. doi: 10.1016/j.jen.2015.07.012. [DOI] [PubMed] [Google Scholar]
- 23.Labrague LJ, Hammad K, Gloe DS, McEnroe-Petitte DM. Disaster preparedness among nurses: a systematic review of literature. Int Nurs Rev. 2018;65(1):41–53. doi: 10.1111/inr.12369. [DOI] [PubMed] [Google Scholar]
- 24.Daily E, Padjen P, Birnbaum M. A review of competencies developed for disaster healthcare providers: limitations of current processes and applicability. Prehosp Disaster Med. 2010;25(5):387–395. doi: 10.1017/s1049023x00008438. [DOI] [PubMed] [Google Scholar]
- 25.Chiu M, Polivka BJ, Stanley SA. Evaluation of a disaster-surge training for public health nurses. Public Health Nurs. 2012;29(2):136–142. doi: 10.1111/j.1525-1446.2011.00984.x. [DOI] [PubMed] [Google Scholar]
- 26.Linde AS. The need for pre-hospital simulation training platforms in battlefield medicine. J Trauma Rehabil. 2018;1 [Google Scholar]
- 27.Pham PK, Behar SM, Berg BM, Upperman JM, Nager AL. Pediatric online disaster preparedness training for medical and nonmedical personnel: a multi-level modeling analysis. Prehosp Disaster Med. 2018;33(4):349–354. doi: 10.1017/S1049023X18000596. [DOI] [PubMed] [Google Scholar]
- 28.Abatemarco A, Beckley J, Borjan M, Robson M. Assessing and improving bioterrorism preparedness among first responders: a pilot study. J Environl Health. 2007;69(6):16–123. [PubMed] [Google Scholar]
- 29.Hansoti B, Kellogg DS, Aberle SJ, Broccoli MC. Preparing emergency physicians for acute disaster response: a review of current training opportunities in the US. Prehosp Disaster Med. 2016;31(6):643–647. doi: 10.1017/S1049023X16000820. [DOI] [PubMed] [Google Scholar]
- 30.O’Brien C, Selod S, Lamb SV. A national initiative to train longterm care staff for disaster response and recovery. J Public Health Manag Pract. 2009;15(2 Suppl):S20–S24. doi: 10.1097/01.PHH.0000345981.57422.90. [DOI] [PubMed] [Google Scholar]
- 31.Idrose SM, Adnan WA, Villa GF, Abdullah AH. The use of classroom training and simulation in the training of medical responders for airport disaster. Emerg Med J. 2007;24(1):7–11. doi: 10.1136/emj.2006.036202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vincent DS, Berg BW, Ikegami K. Mass-casualty triage training for international healthcare workers in the Asia-Pacific region using manikin-based simulations. Prehosp Disaster Med. 2009;24(3):206–213. doi: 10.1017/s1049023x00006828. [DOI] [PubMed] [Google Scholar]
- 33.Pryor E, Heck E, Norman L, Weiner B. Integrated decision-making in response to weapons of mass destruction incidents: development and initial evaluation of a course for healthcare professionals. Prehosp Disaster Med. 2006;21(1):24–30. doi: 10.1017/s1049023x00003289. [DOI] [PubMed] [Google Scholar]
- 34.Sahu S, Lata I. Simulation in resuscitation teaching and training, an evidence-based practice review. J Emerg Trauma Shock. 2010;3(4):378–384. doi: 10.4103/0974-2700.70758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Leek WE. Reliability of the primary triage process after the Voledam fire disaster. 12th Congress of the International Society for Burn Injury, Yokohama, Japan, 2004 [Google Scholar]
- 36.Allison K. The UK pre-hospital management of burn patients: current practice and the need for a standard approach. Burns. 2002;28:135–142. doi: 10.1016/s0305-4179(01)00083-3. [DOI] [PubMed] [Google Scholar]
- 37.Egro FM, Estela CM. The need for burn teaching: a cross-sectional study to assess burn teaching in the United Kingdom. Burns. 2013;40(1):173–174. doi: 10.1016/j.burns.2013.10.001. [DOI] [PubMed] [Google Scholar]
- 38.Lam NN, Huong HTX, Tuan CA. Mass burn injuries: an analysis of characteristics and outcomes in a developing country. Ann Burns Fire Disasters. 2017;30(3):210–213. [PMC free article] [PubMed] [Google Scholar]
- 39.McWilliam T, Hendricks J, Twigg D, Wood F. Burns education for non-burn specialist clinicians in Western Australia. Burns. 2015;41:301–307. doi: 10.1016/j.burns.2014.06.015. [DOI] [PubMed] [Google Scholar]
- 40.Kut A, Tokalak I, Basaran O, Moray G, Haberal MA. Knowledge, attitude and behavior of occupational physicians related to burn cases: a cross–sectional survey in Turkey. Burns. 2005;31:850–854. doi: 10.1016/j.burns.2005.04.009. [DOI] [PubMed] [Google Scholar]
- 41.Wetta-Hall R, Berg-Copas GM, Cusick Jost J, Jost G. Preparing for burn disasters: predictors of improved perceptions of competency after mass burn care training. Prehosp Disaster Med. 2007;22(5):448–453. doi: 10.1017/s1049023x00005197. [DOI] [PubMed] [Google Scholar]
- 42.Wetta-Hall R, Jost JC, Jost G, Praheswari Y, Berg-Copas GM. Preparing for burn disasters: evaluation of a continuing education training course for pre-hospital and hospital professionals in Kansas. J Burn Care Res. 2007;28(1):97–104. doi: 10.1097/BCR.0B013E31802Cb815. [DOI] [PubMed] [Google Scholar]
- 43.Kua Phek Hui J, Allen JC, Mok WL. Attitude of first aid for paediatric burns: pilot survey of developed city state. Burns. 2016;42(4):926–937. doi: 10.1016/j.burns.2016.02.011. [DOI] [PubMed] [Google Scholar]
- 44.Kearns RD, Ortiz-Pujols SM, Craig CK, Gusler JR. Advanced burn life support for day-to-day burn injury management and disaster preparedness: stakeholder experiences and student perceptions following 56 advanced burn life support courses. J Burn Care Res. 2015;36(4):455–464. doi: 10.1097/BCR.0000000000000155. [DOI] [PubMed] [Google Scholar]
- 45.Schenker JD, Goldstein S, Braun J, Werner A. Triage accuracy at a multiple casualty incident disaster drill: The Emergency Medical Service, Fire Department of New York City experience. J Burn Care Res. 2006;27(5):570–575. doi: 10.1097/01.BCR.0000235450.12988.27. [DOI] [PubMed] [Google Scholar]