Abstract
De Garengeot's hernia is a rare entity defined as the presence of the appendix within the femoral hernia sac. Although appendicitis is a common surgical emergency, appendix herniation into the groin results in a complex symptoms and signs, which make it difficult to diagnose clinically. We report a case of a 72-year-old male who had De Garengeot's hernia. Ultrasound and contrast-enhanced CT revealed a typical radiological feature of femoral hernia with the appendix herniating within femoral hernia sac. Surgical management of De Garengeot's hernia is controversial, and it is tailored according to the patient clinical situation and surgeon's preference. To the best of our knowledge, this is the first case that combines both CT and ultrasound findings with postoperative findings.
Keywords: De garengeot's hernia, Femoral hernia, Groin lump, Amyand hernia, Appendicitis, Hernia
Introduction
Appendicitis is a common surgical emergency case which requires instant diagnosis and management; however atypical presentation is common, and its complications can be fatal.1
De Garengeot's hernia is defined as the presence of the appendix within the femoral hernia sac [8].
It is a rare entity with a right-sided preponderance for hernia due to the normal anatomical location of the appendix. Its underlying predisposing factors can be related to the abnormal position of the appendix, low lying cecum, and increased intra-abdominal pressure [2], [3].
Patients usually present with a painful right groin lump [8]. Ultrasound and CT are commonly performed and shows an inflamed appendix herniating through the femoral hernia [6]. Appendectomy is carried through the femoral hernia sac followed by herniorrhaphy with mesh [1].
Case presentation
A 72 year-old male presented to emergency department with 5 days history of right groin swelling and a 1-day history of acute pain at that region. The patient had undergone laparotomy in 1980 for perforated duodenal ulcer. The patient had no other relevant previous medical or surgical history or history of trauma.
On examination, a 3 × 6 cm firm irreducible tender right groin swelling with no overlying skin changes noted. The patient was otherwise clinically stable with normal vitals. Abdominal examination revealed an upper midline scar and a 1 × 1 cm small reducible umbilical hernia. His lab findings (CBC, creatinine, and PT, PTT, and urea electrolyte) were within normal ranges. A provisional diagnosis of right femoral hernia was given and a bedside ultrasound followed by CT was done to confirm the content of the hernia and rule out any other abdominal pathology prior surgery.
Imaging findings
US
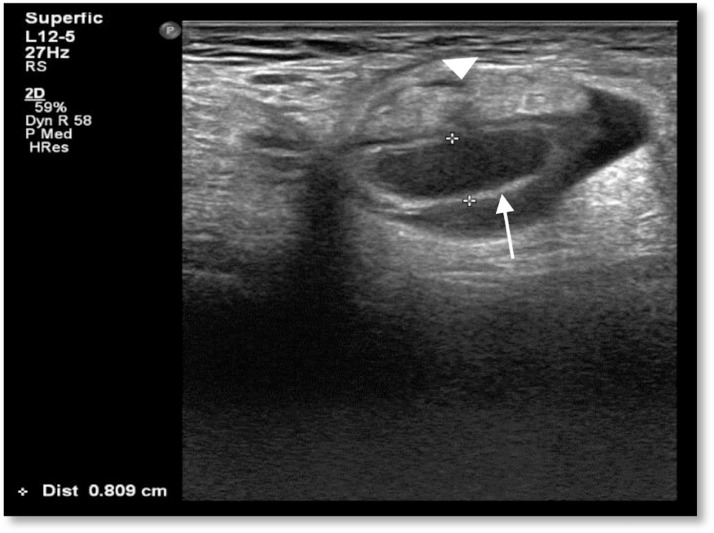
High-frequency linear array ultrasound probe (5-12 MHz) was used to scan the right groin and it showed a noncompressible blind ending tubular cystic mass with a diameter of 0.8 cm seen herniating through right lower abdominal defect with an adjacent hyperechoic omental fat (Fig. 1). The relation of the herniating structures to the femoral vessels could not be established due to probe tenderness and limited field of view.
Fig. 1.
Ultrasound of the right groin showing a blind ending tubular structure herniating through right lower abdominal defect (white arrow) with adjacent omental fat (white arrow head).
CT advised for further evaluation of intraabdominal and pelvic structures, to rule out complications and for surgical planning.
CT
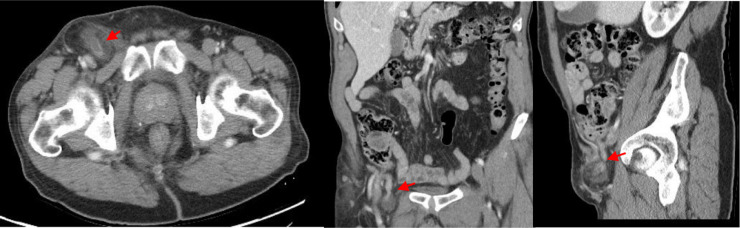
Contrast-enhanced CT examination of the abdomen was done using a 64-detector row scanner (GE optima 660) with 350 mg OMNIPAQUE/100 mL injection administered intravenously. Images revealed herniation of omental fat and a blind ending tubular structure through a narrowed neck defect, medial to the common femoral vessels. Careful evaluation in reformatted coronal and sagittal images showed herniated edematous appendix with adjacent fat stranding. The hernial sac was measuring 5.2 × 3.4 × 5 cm in the 3 orthogonal dimensions. The appendix tip was measuring 0.9 cm with no defect in its enhancing mucosa. Femoral vein demonstrates subtle compression anteromedially due to the hernia sac mass effect (Fig. 2).
Fig. 2.
Axial, coronal, and sagittal CECT images showing a right femoral hernia sac (red arrow) passing inferior to the inguinal ligament and medial to the femoral vessels containing inflamed appendix with adjacent fat stranding.
An impression of acute appendicitis (herniating through femoral defect) with necrotic omental fat were suggested.
The patient was admitted in the hospital with a diagnosis of right femoral hernia containing acutely inflamed appendix and surgery was planned for appendicectomy and herniorrhaphy.
In our patient; an infrainguinal incision was performed. The femoral hernia was found out and was opened. An inflamed congested appendix within the sac was reveled, subsequently appendectomy performed and the hernia was repaired via hernioplasty using McVay technique.
The postoperative course was uneventful and the patient was discharged after 7 days. Afterward, the patient was followed up after 4 weeks in the surgery clinic, the wound was clean and healing as expected (Fig. 3).
Fig. 3.
(A, B) showing the intraoperative findings of congested inflamed appendix (black arrow) with omentum (black arrow head) as content of femoral hernia.
Discussion and conclusion
Femoral hernia containing appendix accounts for only 0.9% of all femoral hernias. De Garengeot's hernia is defined as the presence of the vermiform appendix within the femoral hernia sac. It was first described by French surgeon, Rene Jacques Croissant De Garengeot, in 1731 [3], [4]. Female-to-male incidence ratio equals 5:1 and a mean age of 70 years [3].
Two theories have been described as an etiological factors predisposing to De Garengeot's hernia; the first is that the appendix may be in an abnormal anatomical position. The second theory suggests that an anatomically large caecum forces the appendix into the pelvis [3], [2]. The risk factors include increased intra-abdominal pressure, smoking, age, and connective tissue disease [3].
Majority of patients present with tender groin lump similar to our patient with less than 3% of them being painless [5]. Other symptoms include fever, abdominal pain, and vomiting [2].
Laboratory tests often show leukocytosis and elevated CRP [3]. However, these findings were absent in our case.
Abdominal radiograph is nonspecific but can be performed initially to rule out bowel obstruction [3]. Sonography can be performed in young and pregnant patient [6]. The best diagnostic imaging modality is CT with sensitivity of 100% and a specificity of 98.9% in the diagnosis of acute appendicitis and identifying any associated complications such as small bowel obstruction and strangulation [4], [6]. CT can provide definite preoperative diagnosis and it remains the best way to differentiate Amyand and De Garengeot hernia [2] (Table 1).
Table 1.
The difference between De Garengeot's hernia and Amyand hernia
| De Garengeot's hernia | Amyand hernia | |
|---|---|---|
| Appendix is herniating as | Femoral hernia | Inguinal hernia |
| Appearance on CT | The appendix is herniating through the femoral ring just medial to the common femoral vein. | In direct inguinal hernia, the herniating appendix will be seen medial to the inferior epigastric vessels. In indirect inguinal hernia, the herniating appendix will be seen lateral and superior to the inferior epigastric vessels. |
| Common in | Females | Males |
Note [9].
The definitive treatment of De Garengeot's hernia is surgical appendectomy and femoral hernia repair performed together [7]. Appendectomy can be achieved through the hernial sac if technically feasible or via traditional McBurney incision [8]. Simple herniorrhaphy and avoidance of mesh utilization is preferred in the presence of infection or inflammation [8].
Footnotes
Patient consent: obtained.
Contributor Information
Shareefa Abdulghaffar, Email: sabdulghaffar@dha.gov.ae.
Muna Almulla, Email: maaalmulla@dha.gov.ae.
Priyank Gupta, Email: Pgupta@dha.gov.ae.
Ahmed Bedair Mohamed, Email: ABMohamed@dha.gov.ae.
References
- 1.Salkade P.R., Chung A.Y.F., Law Y.M. De Garengeot's hernia: an unusual right groin mass due to acute appendicitis in an incarcerated femoral hernia. Hong Kong Med J. 2012;18:442. http://www.ncbi.nlm.nih.gov/pubmed/23018075 [PubMed] [Google Scholar]
- 2.Ardeleanu V., Chicos S., Tutunaru D., Georgescu C. A rare case of acute abdomen: Garengeot hernia. Chirurgia. 2013;108:896. http://www.ncbi.nlm.nih.gov/pubmed/24331333 [PubMed] [Google Scholar]
- 3.Garcia-Amador Cristina, De la Plaza Roberto, Arteaga Vladimir, Lopez-Marcano Aylhin, Ramia Jose. Garengeot's hernia: two case reports with CT diagnosis and literature review. Open Med. 2016;11:343–349. doi: 10.1515/med-2016-0065. http://www.degruyter.com/doi/10.1515/med-2016-0065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leite T.F., Chagas C.A., Pires L.A., Cisne R., Babinski M.A. De Garengeot's hernia in an 82-year-old man: a case report and clinical significance. J Surg Case Rep. 2016;2016(7) doi: 10.1093/jscr/rjw120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ahmed K., Bashar K., McHugh T.J., McHugh S.M., Kavanagh E. Appendicitis in De Garengeot's hernia presenting as a nontender inguinal mass: case report and review of the literature. Case Rep Surg. 2014;2014 doi: 10.1155/2014/932638. http://www.ncbi.nlm.nih.gov/pubmed/24716081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Allen B.C., Kirsch J., Szomstein S. Case 187: De Garengeot hernia. Radiology. 2012;265 doi: 10.1148/radiol.12102051. [DOI] [PubMed] [Google Scholar]
- 7.Tanrıkulu C.S., Tanrıkulu Y., Akkapulu N. De Garengeot's hernia: a case of acute appendicitis in a femoral hernia sac. Ulus Travma Acil Cerrahi Derg. 2013;19:380. doi: 10.5505/tjtes.2013.37043. http://www.ncbi.nlm.nih.gov/pubmed/23884684 [DOI] [PubMed] [Google Scholar]
- 8.Erdas E., Sias L., Licheri S. De Garengeot hernia with acute appendicitis. G Chir. 2013;34:86. http://www.ncbi.nlm.nih.gov/pubmed/23578413 [PubMed] [Google Scholar]
- 9.Burkhardt J.H., Arshanskiy Y., Munson J.L., Scholz F.J. Diagnosis of inguinal region hernias with axial CT: the lateral crescent sign and other key findings. RadioGraphics. 2011;31:E12. doi: 10.1148/rg.312105129. [DOI] [PubMed] [Google Scholar]