Abstract
Introduction
The proportion of mobility scooter users in the United States continues to rise. However, these devices impart a substantial yet underappreciated risk of serious injury – namely, fractures – on users.
Methods
The purpose of this cross-sectional, retrospective study was to use the National Electronic Injury Surveillance System (NEISS) to quantify the national burden of these device-associated fractures between 2004 and 2017, analyzing in two-year intervals. We also projected estimates to 2025, and described the demographic characteristics of those injured.
Results
We found that national estimates of device-associated fractures increased significantly between the 2004–2005 (N = 2583; C.I. 1851 - 3316) and 2016–2017 (N = 6553; C.I. 5026 - 8081) periods (p < 0.001). A linear regression model (R2 = 0.89; P = 0.002) was applied to project 9824 such fractures (C.I. 8273–11,328) in the 2024–2025 period. Injured patients were commonly over age 65 (63.5%; C.I. 57.7%–69.4%) and white (61.4%; C.I. 50.7% - 72.1). Fractures often occurred at home (28.6%; C.I. 22.0%–35.3%) or in public (26.0%; C.I. 21.1%–30.9%).
Conclusion
Our study suggests that osteoarthritic patients relying on mobility scooters to manage pain during ambulation should be considered candidates for total joint replacement procedures. This may help minimize the growing economic and health burden of mobility scooter fractures.
Keywords: Mobility scooter, Fracture, Epidemiology, Trends, Burden, Total joint replacement, Osteoarthritis, Surgical candidate, Arthroplasty
1. Introduction
Mobility scooter use has risen substantially in the United States, in parallel with an aging population, an increasing prevalence of obesity, and other risk factors for hip and knee osteoarthritis.1, 2, 3, 4, 5 Patients primarily begin incorporating these devices into their daily lives when they can no longer ambulate effectively or without pain; the majority of users report having trouble performing tasks both at home and related to their occupations.2 Mobility scooter users are most frequently older, non-white, female adults who are obese and have multiple comorbidities.1,6 Importantly, users’ ability to engage in social activities is often dependent on their environment and the infrastructure in place that may facilitate device accessibility.7, 8, 9
Despite their ubiquity, significant concerns regarding the safety of mobility scooters remain at the forefront of debate.10 Specifically, users may be more at risk for experiencing a fall that leads to significant injury.11 For example, fractures of the upper and lower extremities make up roughly half of all mobility scooter injuries, and the risk for injury in general is heightened among novice users.11, 12, 13 Other studies have shown that about 15% of mobility scooter injuries can be classified as “severe trauma,” with the rare but real potential consequence of death.14,15 Given these risks, it is imperative that efforts are undertaken to better characterize the trends in health burden associated with and expected to result from an increasing propensity for patients to use mobility scooters.
In this study, we reported national estimates and demographic characteristics of patients presenting to emergency departments in the United States between 2004 and 2017 with fractures related to mobility scooter use. In addition, we projected scooter-associated fracture estimates between 2017 and 2025. We hypothesized that the total estimate of fractures associated with mobility scooter use has been increasing over time given the annual rise in device use and obesity prevalence.
2. Methods
2.1. Data source
This cross-sectional descriptive epidemiological study identified cases of fractures associated with mobility scooter use in the Consumer Product Safety Commission's (CPSC) National Electronic Injury Surveillance System (NEISS). The CPSC webpage provides publicly available data collection methodologies and general information pertaining to this nationally representative probability sample of hospital emergency departments, which is further stratified by both hospital size and geographic location.16, 17, 18 The NEISS sample includes data entered daily from injuries presenting to approximately 100 designated hospital emergency departments, termed “the sampling frame.” This serves as a probability sample of all U.S. hospitals with emergency departments.
The sampling frame is classified by five strata based on total emergency department visits (EDVs): strata one through four represent hospitals with less than or equal to 16,830 EDVs, 16,831 to 28,150 EDVs, 28,151 to 41,130 EDVs, and greater than or equal to 41,130 EDVs, respectively; a fifth stratum is assigned to emergency departments at children's hospitals. Based on these strata, weighted estimates are assigned to presenting cases such that national estimates and sampling errors for queried injuries may be derived. These weighted estimates incorporate annually adjusted ratios ensuring both that all sampled hospitals implemented proper data collection methodologies, as well as that estimates and sample errors remain accurate despite variation in EDVs within a given year.
Variables included in the NEISS database include: the date of treatment; the case record number; the age, gender, race and ethnicity of the patient; the injury diagnosis; the body part affected by the injury; disposition (treated and released, admitted, etc.); the product involved (if any) in the injury; the location where the injury occurred; whether fire or motor vehicles were involved in the injury; whether the injury was work-related; whether the injury was intentionally inflicted; a narrative of the incident and scenario leading to the injury.
In this study, each yearly sample in the NEISS database was queried between 2004 and 2017 for all injuries classified as fractures and associated with mobility scooter use (Product Code: 1744). Case narratives were then individually analyzed to ensure that the injury occurred while using the cart, as opposed to a non-user being struck by a cart; data prior to 2004 was omitted due to inaccuracies related to identifying users versus non-users in the narrative sections of the NEISS database. Following exclusion criteria from the narrative sections, 668 unique cases of fractures associated with mobility scooter use were observed in the NEISS database, yielding a total estimate of 28,984 total national cases presenting to United States emergency departments.
Data was analyzed in two-year intervals to ensure sufficient statistical power and stable estimates. National estimates, standard errors, and 95% confidence intervals were derived using calculated survey estimates. All statistical analyses were performed using Stata/IC 15.1 (StataCorp, College Station, TX).19 Significance of trends in the total national survey estimates were determined using adjusted Wald tests. P values < 0.05 (two-sided) were considered significant.
2.2. Sources of funding
This study received no external funding support, and was exempt from IRB review given the use of deidentified, publicly available data on a government website.
3. Results
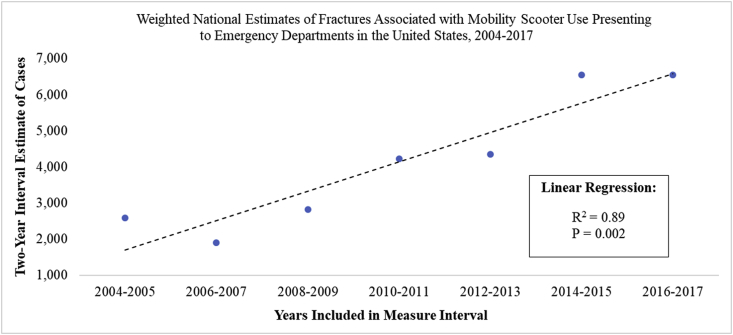
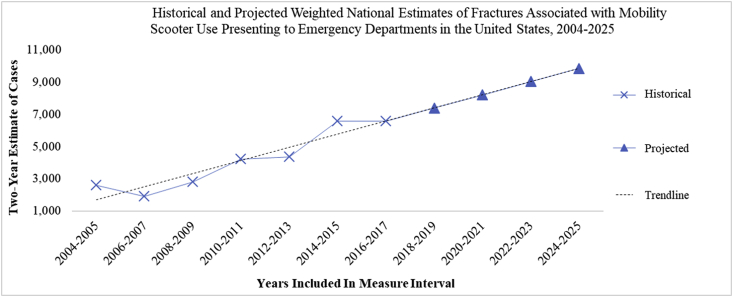
Trends in the estimated national number of fractures associated with mobility scooter use presenting to emergency departments in the United States in two-year intervals between 2004 and 2017 are depicted in Table 1. There was a significant increase in the national estimate of fractures associated with mobility scooter use between the 2004–2005 (N = 2583; C.I. 1851 - 3316) and 2016–2017 (N = 6553; C.I. 5026 - 8081) periods (p < 0.001). Fig. 1 uses a linear regression model (R2 = 0.89; P = 0.002) to illustrate a steady increase in the estimate of fractures associated with mobility scooter use presenting to United States emergency departments across time. Data from this model was extrapolated to project an additional 8 years into the future to the year 2025 (Fig. 2). The number of fractures associated with mobility scooter use is projected to increase from 6553 in the 2016–2017 period to 9824 (C.I. 8273–11,328) in the 2024–2025 period.
Table 1.
Weighted national estimates of fractures associated with mobility scooter use presenting to emergency departments in the United States, 2004–2017.
| Years | National Estimate of Cases | Standard Error | 95% Confidence Interval | ||||
|---|---|---|---|---|---|---|---|
| 2004 | – | 2005 | 2583 | 367 | 1851 | – | 3316 |
| 2006 | – | 2007 | 1906 | 300 | 1308 | – | 2504 |
| 2008 | – | 2009 | 2816 | 548 | 1722 | – | 3909 |
| 2010 | – | 2011 | 4224 | 518 | 3190 | – | 5258 |
| 2012 | – | 2013 | 4351 | 443 | 3467 | – | 5235 |
| 2014 | – | 2015 | 6551 | 892 | 4771 | – | 8330 |
| 2016 | – | 2017 | 6553 | 765 | 5026 | – | 8081 |
Fig. 1.
This graph demonstrates the increased trend in fractures associated with mobility scooter use across two-year intervals using a linear regression model (R2 = 0.89, P = 0.002), at a rate of about 812 additional cases in each consecutive interval period. The blue, filled circles represent the estimates previously shown in Table 1. The linear regression is demonstrated using the dashed, black colored line.
Fig. 2.
This figure extends the regression model from Fig. 1 to the 2024–2025 interval period, to demonstrate that the national estimate of cases would approach 10,000 in said period. The blue crosses represent historical estimates, which are identical to those plotted and described in Table 1 and Fig. 1. The blue, filled triangles represent our projected estimate of cases. The linear regression is demonstrated using the dashed, black colored line. The blue line connecting both historical and projected estimates is meant to illustrate goodness-of-fit with respect to our model.
The demographic characteristics of the overall population of patients presenting to a United States emergency department with a fracture associated with mobility scooter use between 2004 and 2017 are shown in Table 2. Fractures most often occurred in the lower extremity (36.9%; C.I. 32.5%–41.3%) or trunk (36.9%; C.I. 31.4%–42.5%), with just under one-quarter occurring in the upper extremity (22.3%; C.I. 17.6%–26.9%) and a statistically insignificant portion involving the head and neck. The vast majority of presenting patients were over the age of 65 (63.5%; C.I. 57.7%–69.4%) and non-Hispanic white (61.4%; C.I. 50.7% - 72.1). There was no significant difference between the proportion of males (47.5%; C.I. 42.9%–52.0%) versus females (52.5%; C.I. 48.0%–57.1%). Most frequently, patients were either treated and released (54.5%; C.I. 47.7%–61.4%) or admitted to the hospital (39.0%; C.I. 31.7%–46.2%). Fractures commonly occurred at home (28.6%; C.I. 22.0%–35.3%) or in public (26.0%; C.I. 21.1%–30.9%), though it is notable that about one-third of cases occurred in an unknown location (31.3%; C.I. 23.1%–39.4%).
Table 2.
Overall demographics of patients presenting to emergency departments in the United States with fractures associated with mobility scooter use, 2004–2017.
| Demographic Variable | Percentage | Standard Error | 95% Confidence Interval | ||
|---|---|---|---|---|---|
| Anatomical Location of Fracture | |||||
| Head and Necka | 3.9% | ||||
| Upper Extremity | 22.3% | 2.3% | 17.6% | – | 26.9% |
| Lower Extremity | 36.9% | 2.2% | 32.5% | – | 41.3% |
| Trunk (Including Hip, Spine, Ribs) | 36.9% | 2.8% | 31.4% | – | 42.5% |
| Age | |||||
| 0–18 Yearsa | 2.6% | ||||
| 19–64 Years | 33.9% | 3.0% | 27.9% | – | 39.9% |
| 65 Years and Older | 63.5% | 2.9% | 57.7% | – | 69.4% |
| Sex | |||||
| Male | 47.5% | 2.3% | 42.9% | – | 52.0% |
| Female | 52.5% | 2.3% | 48.0% | – | 57.1% |
| Race | |||||
| White | 61.4% | 5.4% | 50.7% | – | 72.1% |
| Black | 4.5% | 1.3% | 2.0% | – | 7.0% |
| Othera | 0.5% | ||||
| Hispanica | 2.3% | ||||
| Race Not Specified | 31.1% | 6.0% | 19.0% | – | 43.2% |
| Disposition | |||||
| Treated and Released | 54.5% | 3.4% | 47.7% | – | 61.4% |
| Treated and Transferred | 5.1% | 1.2% | 2.7% | – | 7.5% |
| Treated and Admitted | 39.0% | 3.6% | 31.7% | – | 46.2% |
| Location | |||||
| Unknown | 31.3% | 4.1% | 23.1% | – | 39.4% |
| Home | 28.6% | 3.3% | 22.0% | – | 35.3% |
| Street | 12.7% | 2.3% | 8.1% | – | 17.3% |
| Public | 26.0% | 2.5% | 21.1% | – | 30.9% |
| Sportsa | 1.2% | ||||
The estimate is considered to be potentially unstable due to the number of unweighted cases from the sample frame totaling <20, the weighted national estimate totaling <1200, or coefficient of variation >33%. Therefore, no standard errors or confidence intervals are provided; the unstable percentage estimate is provided for reference purposes only. Variable results with sample frame totals <20 cases or percentages <0.1% were omitted from this table, resulting in percentage totals not necessarily summing to 100%.
4. Discussion
In this study, we found that the national number of fractures associated with mobility scooter use presenting to US emergency departments has increased significantly over time; in the 2004–2005 period, about 1200 cases presented per year, while in the 2016–2017 period, this value rose to nearly 3300 cases per year. We found that annual estimates of fractures in mobility scooter users are expected to increase over time, projected to reach about 5000 cases per year by 2025. Lastly, the demographic characteristics of presenting patients indicate significant risk to the trunk and extremities, especially for an elderly population most vulnerable to the consequences of severe injuries such as fractures.
These findings implore clinicians and researchers to identify treatment regimens that not only alleviate patients’ pain, but also restore their ability to ambulate. By striving to help patients achieve independence from mobility scooters, clinicians can help minimize exposure to a significant and increasing source of injury risk. Foremost, patients should receive appropriate safety training prior to commencing use of a mobility scooter. Another potential means for mitigating mobility scooter-related risk may be through the use of total joint arthroplasty (TJA), as osteoarthritis is the leading cause of mobility scooter use in the United States. Nearly 15.2% of individuals over the age of 65 who use a mobility scooter require the device directly due to pain from osteoarthritis.2 Given that osteoarthritis is the most common indication for TJA, patients that use a mobility scooter to manage osteoarthritic pain should be considered candidates for TJA since they are at an increased risk for scooter-related injuries (e.g. fractures).
The potential health burden that TJA could alleviate for eligible surgical candidates using mobility scooters would likely prove to be impressive given the successful functional outcomes of the procedure. For example, Walker et al. showed that patients who underwent total knee replacements for osteoarthritis had an average increase in ambulation of about 80%.20 Dalury et al. also demonstrated that following TJA, about 75% of individuals previously using a walking aid (including wheelchairs) no longer required them.21 A study by McAuley et al. demonstrated that up to 85% of patients with limited pre-operative range of motion undergoing total knee replacement were able to walk with less pain and without the use of a wheelchair postoperatively.22 The benefits of TJA for individuals using a mobility scooter, especially due to osteoarthritis, merits consideration for those of acceptable medical risk.
Even when considering the demographic most commonly affected by fractures related to mobility scooter use –individuals age 65 years and older – there is tremendous potential for restoration of independent ambulation and reduced injury risk. Gell et al. showed that 815,000 adults 65 years and older (2.3% of adults in this age category) used a mobility scooter in 2011.1 As previously referenced, it is expected that approximately 15% of these users required the scooter due to pain or immobility from osteoarthritis. If this cohort had elected to undergo TJA surgery, about 100,000 patients would be expected to achieve device independence. This would significantly minimize the at-risk population for fractures associated with mobility scooter use while simultaneously alleviating pain and advancing patients towards more healthful activity levels.
This study has several limitations related to the case collection methodologies and overall structure of the NEISS sample frame. Most importantly, the database only reports injuries presenting to emergency departments. Fractures that were first diagnosed or treated outside of the emergency department, such as at an urgent care clinic or an inpatient setting, are not captured by the present study. Therefore, we consider our findings to represent conservative national estimates of mobility scooter fracture burden. Second, the NEISS database does not distinguish between injuries caused while physically using mobility scooters, versus those occurring to a bystander (for example, someone who was struck by a scooter in public). Efforts were made using the narrative section of the database to exclude such entries from analysis, though it cannot be ruled out that such cases were unintentionally included.
Lastly, the data does not contain important demographic variables or cost data, which would have allowed for analysis pertaining to how factors such as BMI might affect risk or severity of injury, as well as the national cost burden of fractures related to mobility scooter use. Given the wide variety of fractures and missing information about subsequent surgical or nonsurgical treatment approaches, as well as uncertainty regarding the prevalence of regular scooter usage by individuals, cost multipliers could not reliably be employed to derive estimates of economic burden.
Mobility scooters have become increasingly popular in the United States. These mobility assistive devices impart significant freedom and improvement in quality of life to those recovering from surgery or unable to ambulate independently for various reasons. However, dependence on scooters comes with risk: injuries from the use of mobility scooters abound, from simple lacerations to severe fractures and even death. While often an excellent short-term option for mobility, clinicians should help patients develop a long-term goal of independence from the scooters to minimize individual injury risk. This is especially true when the reason for long-term mobility scooter use is due to a condition such as osteoarthritis of the hip and knee, which is treatable through surgical intervention. Patients who rely on mobility scooters to manage joint pain during ambulation should be considered candidates for TJA. In doing so, the growing economic and health burden of mobility scooter injuries may be more effectively curtailed.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.jor.2019.03.011.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Gell N.M., Wallace R.B., Lacroix A.Z., Mroz T.M., Patel K.V. Mobility device use in older adults and incidence of falls and worry about falling: findings from the 2011–2012 national health and aging trends study. J Am Geriatr Soc. 2015;63(5):853–859. doi: 10.1111/jgs.13393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kaye H.S., Kang T., LaPlante M.P. vol. 14. 2000. (Mobility Device Use in the united states). [Google Scholar]
- 3.Ogden C.L., Carroll M.D., Fryar C.D., Flegal K.M. 2015. Prevalence of Obesity Among Adults and Youth: United States, 2011-2014. [PubMed] [Google Scholar]
- 4.Flegal K.M., Kruszon-Moran D., Carroll M.D., Fryar C.D., Ogden C.L. Trends in obesity among adults in the United States, 2005 to 2014. J Am Med Assoc. 2016;315(21):2284–2291. doi: 10.1001/jama.2016.6458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ortman J.M., Velkoff V.A., Hogan H. 2014. An Aging Nation: The Older Population in the united states. [Google Scholar]
- 6.LaPlante M.P., Kaye H.S. Demographics and trends in wheeled mobility equipment use and accessibility in the community. Assist Technol. 2010;22(1):3–17. doi: 10.1080/10400430903501413. [DOI] [PubMed] [Google Scholar]
- 7.Bigonnesse C., Mahmood A., Chaudhury H., Mortenson W.B., Miller W.C., Martin Ginis K.A. The role of neighborhood physical environment on mobility and social participation among people using mobility assistive technology. Disability & Society. 2018:1–28. [Google Scholar]
- 8.Fomiatti R., Richmond J., Moir L., Millsteed J. A systematic review of the impact of powered mobility devices on older adults' activity engagement. Phys Occup Ther Geriatr. 2013;31(4):297–309. [Google Scholar]
- 9.Salminen A., Brandt Å., Samuelsson K., Töytäri O., Malmivaara A. Mobility devices to promote activity and participation: a systematic review. J Rehabil Med. 2009;41(9):697–706. doi: 10.2340/16501977-0427. [DOI] [PubMed] [Google Scholar]
- 10.Mortenson W.B., Kim J. Scoping review of mobility scooter-related research studies. J Rehabil Res Dev. 2016;53(5) doi: 10.1682/JRRD.2015.05.0084. [DOI] [PubMed] [Google Scholar]
- 11.Cassell E., Clapperton A. Consumer product-related injury (2): injury related to the use of motorised mobility scooters. Hospital. 2004;5 doi: 10.1080/17457300.2015.1047857. [DOI] [PubMed] [Google Scholar]
- 12.Murphy C.G., Murphy I.G., O'Rourke K.S., O'Shea K. Motorised mobility scooters; upper limb fractures in elderly novice users. Clin Cases Miner Bone Metabol. 2014;11(2):132. [PMC free article] [PubMed] [Google Scholar]
- 13.Gibson K., Ozanne-Smith J., Clapperton A., Kitching F., Cassell E. Monash University, Australian Competition and Consumer Commission, Monash University Accident Research Centre.Google Scholar; Melbourne, Australia: 2011. Targeted Study of Injury Data Involving Motorised Mobility Scooters. [Google Scholar]
- 14.Kitching F.A., Ozanne-Smith J., Gibson K., Clapperton A., Cassell E. Deaths of older australians related to their use of motorised mobility scooters. Int J Inj Control Saf Promot. 2016;23(4):346–350. doi: 10.1080/17457300.2015.1047857. [DOI] [PubMed] [Google Scholar]
- 15.Leijdesdorff H.A., Krijnen P., Schipper I. Accidents involving a motorized mobility scooter: a growing problem. Ned Tijdschr Geneeskd. 2014;158:A7858. [PubMed] [Google Scholar]
- 16.CPSC U.S. 2000. NEISS, the National Electronic in Jury Surveillance System: A Tool for Researchers.https://www.cpsc.gov/cgibin/NEISSQuery/home.aspx 1:03:23 AM. [Google Scholar]
- 17.Schroeder T., Ault K. US Consumer Product Safety Commission; Washington, DC: 2001. The NEISS Sample: Design and Implementation.https://www.cpsc.gov/s3fs-public/2001d010-6b6.pdf 1:09:47 AM. [Google Scholar]
- 18.US Consumer Product Safety Commission . 2017. National Electronic Injury Surveillance System (NEISS) Coding Manual 2017.https://www.cpsc.gov/s3fs-public/2017NEISSCodingManualCPSConlyNontrauma.pdf 12:56:54 AM. [Google Scholar]
- 19.StataCorp L.P. StataCorp LP; College Station, TX, USA: 2018. Stata/IC 15.1 for Windows. 10:14:54 PM. [Google Scholar]
- 20.Walker D.J., Heslop P.S., Chandler C., Pinder I.M. Measured ambulation and self‐reported health status following total joint replacement for the osteoarthritic knee. Rheumatology. 2002;41(7):755–758. doi: 10.1093/rheumatology/41.7.755. [DOI] [PubMed] [Google Scholar]
- 21.Dalury D.F., Ewald F.C., Christie M.J., Scott R.D. Total knee arthroplasty in a group of patients less than 45 years of age. J Arthroplast. 1995;10(5):598–602. doi: 10.1016/s0883-5403(05)80202-5. [DOI] [PubMed] [Google Scholar]
- 22.McAuley J.P., Harrer M.F., Ammeen D., Engh G.A. Outcome of knee arthroplasty in patients with poor preoperative range of motion. Clin Orthop Relat Res. 2002;404:203–207. doi: 10.1097/00003086-200211000-00033. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.