Abstract
Despite a significant reduction in tuberculosis (TB) mortality over the past decade, TB remains a leading cause of death worldwide. Food insecurity—through pathways such as malnutrition, mental health impact, and high-risk health behaviors—affects the risk of TB disease, treatment failure, and mortality. We searched the literature for studies reporting on the links between food insecurity and TB. In contrast to the well-documented interactions between food insecurity and HIV/AIDS, we found that the association between food insecurity and TB remains largely understudied—this is especially true with regard to non-nutritional correlations. Mental health and behavioral linkages between TB and food insecurity deserve further attention. An improved understanding of the pathways through which food insecurity impacts TB is crucial to inform evidence-based integration of interventions such as psychological counseling, psychiatric care, harm reduction programs, and efforts to address social determinants of disease within current TB programs.
Keywords: food insecurity, high-risk behavior, malnutrition, mental health, tuberculosis
Tuberculosis (TB) remains a leading cause of mortality worldwide, killing more people in 2016 than HIV and malaria [1]. Many risk factors modify the clinical course of TB, including food insecurity. Food security is the condition in which all people, at all times, have physical, social, and economic access to sufficient safe and nutritious food that meets their dietary needs for a healthy life. Food insecurity is the converse of that—a lack of availability or access to food of sufficient quality and quantity [2].
Although the term food insecurity may invoke “hunger” or “malnutrition,” these terms are not synonymous. Hunger is the uncomfortable sensation caused by a lack of food. It may be a consequence of food insecurity, and it may result in malnutrition over time. Malnutrition results from a diet in which nutrient inadequacies cause health problems, often classified by degree of stunting, wasting, and protein-energy malnutrition. Malnutrition and hunger are the most obvious sequelae of food insecurity, but these are just 1 part of a larger paradigm of food insecurity’s association with ill health. A significant proportion of patients with TB, especially in resource-poor settings, are food insecure. The African Food Security Network (AFSUN) 2008–2009 survey of patients with HIV/TB in 11 southern African cities showed that only 10% of patients with TB resided in food-secure households [3].
Weiser et al. have devised a conceptual framework to better comprehend the complex links between food insecurity and HIV/AIDS. They identified 3 main pathways—nutritional, mental health, and behavioral—through which food insecurity is associated with higher risk of HIV acquisition, transmission, morbidity, and mortality [4]. It could be extrapolated that food insecurity also impacts TB through these 3 main pathways; however, a TB-specific framework for food insecurity has yet to be established. In this paper, we apply Weiser et al.’s conceptual framework as a means to explore and review the literature on the relationship between each of the proposed food insecurity pathways and TB, with the goals of understanding the extent of what is known about this relationship and highlighting gaps to be addressed by future research.
METHODS
We conducted a literature search, limited to the English language, to identify studies on the relationship between food insecurity and tuberculosis. Six databases (PubMed, Embase, Web of Science Core Collection, MEDLINE, CABI, and BIOSIS Previews) were searched, from all years through January 2019, using a combination of search terms related to food insecurity, its various pathways (nutritional, mental health, behavioral), and tuberculosis (Supplementary Data).
Results
Article Selection
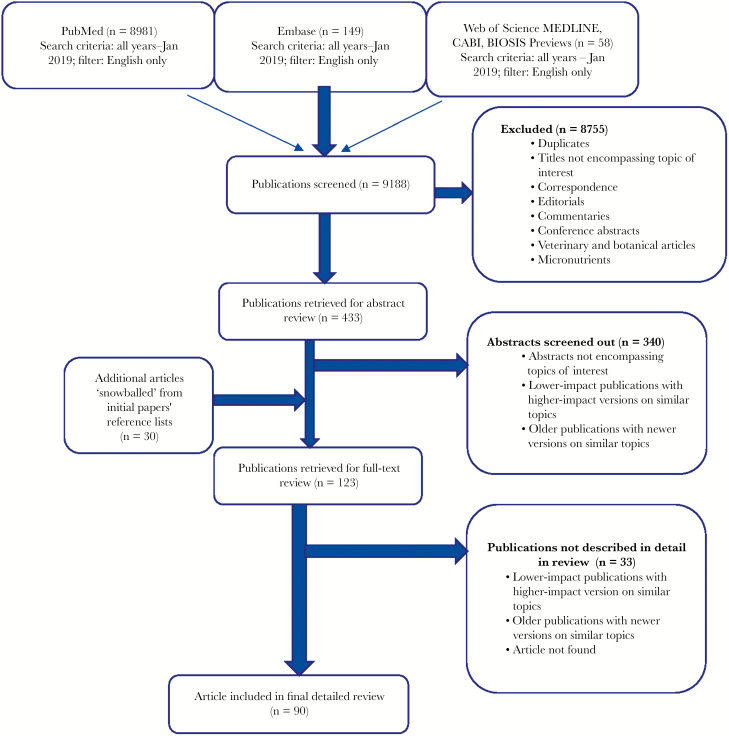
The search resulted in 9188 publications screened; 433 publications that contained description or assessment of various combinations of food insecurity, nutrition, mental health, high-risk behavior, and TB were retrieved for abstract review. For full-text review, we included any paper including both the food security and TB terms. We otherwise prioritized original research articles, meta-analyses, and systematic reviews. Where multiple papers with similar findings existed (this was especially true in the area of malnutrition and TB, micronutrients and TB, mental health and TB, substance use and TB), we used newer publications in preference to older ones; for subjects for which there were few original research papers (eg, mental health side effects of TB medications), we included case reports. Using these criteria and screening out abstracts not encompassing topics of interest, a total of 123 articles, including those additionally mined from reference lists, were selected for full-text review. Finally, using the criteria above again, these were narrowed down to 90 articles to be included in this narrative review. Although briefly discussed, studies on micronutrients were excluded from the detailed individual discussion (Figure 1). Throughout our search, we found no studies that explicitly examined a relationship between food insecurity and TB through mental health or behavioral pathways.
Figure 1.
Literature search strategy and overview of results.
Food Insecurity, Nutrition, and Tuberculosis
Food insecurity can result in malnutrition in individuals with TB and has been widely studied. In a matched case–control study of patients with pulmonary TB in Ethiopia, for example, household food shortage was an independent risk factor for active pulmonary TB (odds ratio [OR], 2.38; 95% confidence interval [CI], 1.52–3.73) [5]. Multiple forms of malnutrition—undernutrition, protein-energy malnutrition, micronutrient deficiency, and overweight/obesity—have been associated with TB. TB causes weight loss, and low body mass index (BMI)—a surrogate for undernutrition—is a risk factor for TB infection [6]. Historically, the disease was referred to as “consumption” and “phthisis” because of the severe weight loss its patients experience [7]. Physicians have also long noted that food insecurity heightens the risk of developing active TB [7]. Cochrane, a physician and prisoner during World War II, noted how, in 1945, the incidence of TB was higher in patients who did not receive sufficient amounts of food [8]. Another prisoner of war, Leyton, compared TB incidence among British and Russian prisoners during World War II; he noted that British prisoners had a lower TB incidence rate (1.2%) compared with Russian prisoners (15%–20%). Although both groups had similar types and amounts of manual labor, living conditions, and clothing, only the British prisoners received weekly Red Cross rations [9].
Significant weight loss associated with TB may also predispose patients to an increased risk of treatment-related side effects such as hepatotoxicity [10]. In a study of adult patients receiving treatment for multidrug-resistant TB (MDR-TB) in Latvia, underweight patients (BMI < 18.5 kg/m2) were significantly more likely to have clinical evidence of advanced disease and had a greater risk of experiencing ≥3 side effects (adjusted OR [AOR], 1.5; 95% confidence interval [CI], 1.1–2.1) and death (AHR, 1.9; 95% CI, 1.1–3.5) compared with patients who were normal or overweight [11]. In a South Korean population, low BMI (<18.5 kg/m2) was an independent risk factor for failure to achieve sputum culture conversion within 3 months among patients with MDR-TB [12]. Furthermore, a systematic review of 6 cohort studies showed an inverse relationship between BMI and TB incidence for the BMI range 18.5–30 kg/m2, with a 14% reduction in TB incidence for every unit increase in BMI [13].
In both human and animal studies, protein-energy malnutrition has been associated with impaired cell-mediated immunity, a principal host defense against TB. Children with kwashiorkor have been shown to have a negative tuberculin skin test (TST) response after Bacillus Calmette-Guérin vaccination [14], adult TB patients with protein malnutrition were less likely to be TST-positive after tuberculin testing [15], and mice with protein calorie malnutrition rapidly succumbed to infection with Mycobacterium tuberculosis compared with well-nourished controls, whereas restoration of a full-protein diet reversed this susceptibility to infection [16].
Micronutrient deficiencies are prevalent in populations with TB [17–23]. The literature describing the association between these deficiencies and TB is mostly observational and therefore cannot confirm the directionality of the relationship; only studies on vitamin D deficiency have been sufficiently rigorous to suggest it as a risk factor for TB infection. A 2016 Cochrane review on macronutrient and micronutrient supplementation, including vitamin D, was inconclusive as to whether it had a positive benefit on TB outcomes [24].
Food insecurity is often thought of only in relationship to underweight, but it has importantly been associated with diabetes mellitus (DM) in some populations [25], which in turn is associated with a 3-fold increased risk of TB [25]. A systematic review of 13 observational studies (n = 1 786 212 participants) with 17 698 TB cases found that, irrespective of study design and population, DM increased risk of TB (relative risk [RR], 3.11; 95% CI, 2.27–4.26) [26]. Although the negative impacts of undernutrition in TB are undisputed, the impacts of being overweight and obese—which are associated with DM—remain less clear cut. Some studies have shown that overweight and obesity are protective, whereas others have demonstrated an opposite association. For instance, a large study in a rural Chinese population found a positive association between elevated BMI and TB risk: BMI ≥28.0 kg/m2 was independently associated with interferon gamma release assay (IGRA) positivity (AOR, 1.17; 95% CI, 1.04–1.33) [27]. Conversely, a large prospective study in TB household contacts in Peru found that overweight (BMI > 25 kg/m2) household contacts had lower risk of developing pulmonary TB disease (hazard ratio [HR], 0.48; 95% CI, 0.37–0.64) than those with normal BMI (BMI ≥ 18.5–25kg/m2) [28].
It remains unclear (and largely unstudied) whether and exactly how food insecurity may be part of the association between TB and DM, warranting more research in this area, especially as the incidence of DM continues to rise at alarming rates in high–TB prevalence settings.
Food Insecurity, Mental Health, and Tuberculosis
An association between various aspects of food insecurity and mental health disorders is well established. A global analysis of 149 countries found that there was a dose–response association between food insecurity and poor mental health, independent of socioeconomic status [29]. In Latin America and the Caribbean, cumulative life exposure to hunger was associated with high rates of depression in women (OR, 2.23; 95% CI, 1.77–2.82) [30]. In India and South Africa, a survey of 1300 households showed that the number of missed meals due to lack of resources increased depression in adults [31], whereas in Tanzania, a cross-sectional study of 449 female caretakers found that food insecurity among these women was significantly associated with anxiety and depression [32]. In a study of 2494 Indian women, the presence of a common mental disorder (depression and anxiety) was associated with experience of hunger in the past 3 months (OR, 2.7; 95% CI, 1.6–4.6) [33]. In Afghanistan, 1 study of 1172 women found an independent association between food shortage experience and post-traumatic stress disorder (PTSD), irrespective of traumatic events experienced during armed conflict (OR 1.86, 95% CI, 1.07–2.23) [34]. A systematic review of qualitative and quantitative studies on the linkages between food insecurity and mental health in low-income settings found that food insecurity was associated with stress, shame, anxiety, and depression [35], and another systematic review assessing longitudinal relationships between food insecurity and poor mental health confirmed a bidirectional association [36].
Poor mental health has also been proposed as a risk factor for TB [37]; however, there is a paucity of studies specifically investigating the impact of mental illness on incident TB. One such study is a Korean nationwide population-based cohort of 32 372 individuals with depression, which demonstrated a dose–response relationship between baseline depression and incident TB risk (HR, 2.63; 95% CI, 1.74–3.96). The authors hypothesized that the association was due to a reduction in cellular immunity (known to be associated with depression), as well as malnutrition, smoking, and alcohol abuse [38]. A number of studies have suggested that TB-associated stigma, which can give rise to internalized feelings of shame, disgust, and guilt in patients with TB [39], may contribute to depression [40], TB diagnosis and treatment delays, and TB treatment nonadherence [41–44]. One study on the impact of TB-associated stigma and depressive symptoms on medication adherence in TB patients in central China revealed that patients with medium (OR, 1.54; 95% CI, 1.08–2.21) or high (OR, 5.32; 95% CI, 3.34–8.46) self-perceived stigma or patients with mild (OR, 1.92; 95% CI, 1.34–2.75) or severe (OR, 3.67; 95% CI, 2.04–6.61) depressive symptoms had a higher likelihood of having low adherence than those with low stigma or without depressive symptoms [45].
Conversely, it has been proposed that M. tuberculosis infection and/or disease reactivation may precipitate depression as a result of the inflammatory response and/or dysregulation of the hypothalamic–pituitary–adrenal axis [37]. Finally, TB patients on therapy may experience adverse psychiatric events. Specifically, neuropsychiatric disturbances (ranging from mild behavioral disturbances to frank psychosis) have been reported with the firstline agent isoniazid [46–48] and with the second-line agents ethionamide [48, 49] and cycloserine [50], adding to the complexity of the association.
Several studies have shown high prevalence of comorbid mental illness and TB. In different regions of the world, depression [51–55], anxiety [51, 53, 55], somatoform symptoms [51], and PTSD [56] are significantly prevalent in patients with TB.
TB patients with untreated mental health disorders are more likely to have suboptimal adherence to treatment [42], with a snowball effect on increased drug resistance [57], treatment failure, and, eventually, mortality [58]. Among 23 TB patients in Northern Russia who presented late for care, hopelessness was found to be a major contributor to delayed TB diagnosis [59], which may result in poor outcomes. A retrospective study of all patients involuntarily detained for TB treatment in New York City from 2002 to 2009 found that mental illness (OR, 5.80; 95% CI, 1.18–28.51) and substance abuse (OR, 9.25; 95% CI, 2.81–30.39) were some of the strongest independent predictors of likelihood of delayed completion of TB treatment due to nonadherence [60]. In Ethiopia, untreated depression was independently associated with TB treatment interruption (adjusted RR [ARR], 9.09; 95% CI, 6.72–12.30) and death (ARR, 2.99; 95% CI, 1.54–5.78) [61]. A retrospective study of 671 patients with MDR TB in Peru found that having a psychiatric disorder (depression being the most common in this cohort) predicted death after treatment loss to follow-up [62], and another prospective study from the same country showed that comorbid TB and depression are significantly associated with poor outcomes, including poor treatment adherence and mortality, when compared with TB without depression (HR, 3.54; 95% CI, 1.43–8.75) [63].
Despite this plethora of studies demonstrating a strong association between food insecurity and mental health, and separately between mental health and TB, we found no studies exploring the possible relationships between TB and food insecurity through a pathway of mental health.
Food Insecurity, Health-Related Behavior, Substance Use, and Tuberculosis
Food insecurity places individuals and families in a precarious situation that can influence their decision-making and tolerance of risk, which can have important health implications. An analysis of the 1999 National Survey of America’s Families (NSAF) revealed that food insecurity was independently associated with postponing needed medical care (AOR, 1.74; 95% CI, 1.38–2.21), postponing medications (AOR, 2.15; 95% CI, 1.62–2.85), increased emergency department use (AOR, 1.39; 95% CI, 1.17–1.66), and hospitalizations (AOR, 1.42; 95% CI, 1.09–1.85) [64].
Several studies support the concept that food insecurity negatively affects treatment adherence in TB patients. Qualitative studies of TB patients in Southern Ethiopia and Papua New Guinea found that various aspects of food insecurity (eg, lack of adequate food, concern about daily food production and shortage) significantly contribute to TB treatment nonadherence [65, 66]. A qualitative study in Swaziland found that some food-insecure patients stopped TB treatment because it increased their appetites when they were already food scarce [67]. Similarly, in a review of 44 qualitative studies on treatment adherence, 7 studies mentioned that the quality of food accessible by patients impacted treatment adherence; in 5 of these studies, patients cited stopping medication or leaving the hospital when they could not access food [44]. Among the factors that negatively impact treatment adherence, medication side effects are commonly reported by patients as a reason for TB therapy discontinuation [68, 69]. Although concomitant food and medication intake might reduce some gastrointestinal side effects (such as nausea and vomiting) associated with many TB medications [70], it is generally recommended that anti-TB medication be taken in a fasting state [70] or with antacids in those with gastrointestinal upset [71], because several studies have shown that food significantly reduces the bioavailability of many firstline anti-TB medications [70, 71], which in turn may lead to treatment failure.
Substance use disorder has also been linked with food insecurity. Observational studies have shown illicit drug and excessive alcohol use to be prevalent among food-insecure individuals [72]. A survey of 144 injection drug users in Canada found that they were 2.5 to 6 times more likely than non–injection drug users to report experiencing food insecurity, and the odds of sharing injection equipment (ie, needles, water, cookers, and filters) were increased for food-insecure individuals [73]. In South Africa, a study investigating food insecurity and postpartum depression in 249 women found that food insecurity was independently associated with hazardous drinking of alcohol, whereby each additional point on the Household Food Insecurity Access Scale was associated with a 4% increased risk of hazardous drinking (ARR, 1.04; 95% CI, 1.00–1.09) [74]. Another study of 2172 individuals in the same country showed that poverty-related stressors including insufficient food were associated with alcohol and drug use [75].
In turn, alcohol and intravenous drug use have strong associations with primary and active TB, respectively. People with alcohol use disorder have reduced numbers and impaired function of lymphocytes and macrophages, which are needed to combat M. tuberculosis [72]. In a cohort of individuals with alcohol use disorders who were followed prospectively for 8 years, the TB incidence was 464/100 000 person-years, which was 9 times the age-matched incidence among the general population in New York [76]. Similarly, Lonroth et al. showed that consumption of more than 40 g/d of alcohol or a diagnosis of alcohol use disorder was associated with a nearly 3-fold higher risk of tuberculosis (RR, 2.94; 95% CI, 1.89–4.59) compared with no alcohol consumption or alcohol consumption below the specified thresholds [77]. Subsequently, Rehm et al. estimated that 10% of active TB cases globally were attributable to alcohol use (>40 g/d) or alcohol use disorder [72]. A more recent meta-analysis supported these findings, showing that alcohol use (RR, 1.35; 95% CI, 1.09–1.68) and alcohol-related problems (RR, 3.33; 95% CI, 2.14–5.19), were associated with increased risk of TB in a dose–response fashion, and that alcohol use caused 22.02 incident TB cases (95% CI, 19.70–40.77) per 100 000 people in 2014 [78].
Illicit drug use, intravenous or otherwise, increases the risk of latent and active TB. This increased risk may occur through increased exposure to TB via the environment, through high-risk behavior, the direct effect of drugs (opiates in particular) on the immune system, or through HIV-induced immunosuppression [79]. A national surveillance data analysis of 2826 HIV/TB cases in Spain found injection drug use to be an independent predictor of TB among people with AIDS (OR, 1.4; 95% CI, 1.2–1.6) [80], whereas another multinational study of 7838 AIDS cases found that injection drug use, and not CD4+ count, predicted risk for TB among patients with CD4+ counts ≥300 cells/μL (OR, 2.12; 95% CI, 1.07–4.21) [81].
Substance use has been shown to be highly prevalent in certain TB populations; a large cross-sectional study of 153 268 TB patients conducted in the United States found that the prevalence of substance abuse—self-reported excess alcohol intake, injection, or no-injection drug use 1 year before the diagnosis of TB—was 18.7%, and that positive sputum smear was positively associated with substance abuse (OR, 1.8; 99% CI, 1.7–1.9) [82]. In Mexico, a study of 1020 people who inject drugs found that the high prevalence of latent TB (67%) among this population was associated with increasing years of injection (AOR, 1.20/5 years; 95% CI, 1.07–1.34) [83].
An association also exists between smoking tobacco and TB. A study examining the relationship between food insecurity and smoking in Nepal showed that smoking was independently associated with higher household food insecurity than not smoking [84]. Similarly, in the United States, smoking prevalence was higher among low-income families who were food insecure compared with low-income families who were food secure [85]. A recent study of 4563 adults showed that developing food insecurity was independently associated with lower likelihood of stopping smoking among smokers (AOR, 0.66; 95% CI, 0.46–0.94) and with higher likelihood of starting smoking among nonsmokers (AOR, 3.77; 95% CI, 1.25–11.32) [86].
Several systemic reviews have demonstrated that smoking increases the risk of TB infection and disease [87–89]. A recent study using data from the National Health and Nutrition Examination Survey (NHANES) found that current smoking was associated with latent TB infection (AOR, 2.31; 95% CI, 1.17– 4.55) [90], and a China-based study of 210 008 individuals showed a positive association between smoking history and TB infection (OR, 1.34; 95% CI, 1.21–1.49), with a significant dose–response relationship between duration of smoking and Quantiferon-TB Gold positivity [91]. A meta-analysis by Patra et al. found that while BMI <18.5 kg/m2, tobacco smoking, alcohol use, and type 2 diabetes each individually increased the risk of active TB, their compound effect tripled or quadrupled this risk [92].
Studies have shown that individuals with substance use disorders present late for TB treatment [93, 94] and have difficulty adhering to TB treatment [44, 95], thereby increasing their risk of treatment failure [72], drug resistance [72], and mortality. For instance, in a study of 96 South African patients, illicit marijuana or mandrax (a sedative) use during treatment was the strongest risk factor for failure to complete treatment for MDR-TB (AOR, 17.9; 95% CI, 4.7–68.5) [96], and in Peru, substance use (HR, 2.96; 95% CI, 1.56–5.62) was significantly associated with treatment loss to follow-up among 671 patients with MDR-TB [62]. Similar findings were seen in Brazil, where alcoholism (OR, 2.94; 95% CI, 1.08–7.99) and substance use disorder (OR, 12.25; 95% CI, 3.04–49.26) were significantly associated with loss to follow-up from TB treatment [97]. In Poland, a study of 2025 TB patients from 2001–2010 found that alcohol abuse increased the rate of unsuccessful TB treatment by 84% (AOR, 1.84; 95% CI, 1.26–2.68) [98]. In a large study of 16 345 TB patients undergoing therapy for active TB in Hong Kong from 2001–2003, smoking was associated with more extensive lung disease, poor treatment outcomes (AOR, 0.72; 95% CI, 0.64–0.82 for treatment success), and higher relapse risk (AHR, 1.63; 95% CI, 1.29–2.06) among successful treatment completers [99]. Notably, smoking accounted for 16.7% of unsuccessful treatment outcomes in this study, with the key contributor being loss to follow-up in current smokers and death in ex-smokers [99].
With regards to mortality among those with TB, a large case–control study of 43 000 adult male deaths and 35 000 controls in India found that smokers had a 4-fold increase in risk of death from TB compared with nonsmokers [100], whereas a recent meta-analysis showed that alcohol consumption caused 2.35 deaths (95% CI, 2.05–4.79) per 100 000 people from tuberculosis in 2014 (78). Another study of 715 TB patients in Iran found that drug use (opium is the most common drug used in this part of Iran; AOR, 7.8; 95% CI, 2.4–5.5) and smoking (AOR, 12.9; 95% CI, 3.9–27.3) were major risk factors for death in TB patients (101). Similarly, substance use disorder was an independent predictor of poor survival (AHR, 3.79; 95% CI, 2.07–6.93) in a study of 426 patients with drug-resistant TB in Malaysia [102].
Despite the clear associations between food insecurity and high-risk behavior, and between certain high-risk behaviors—especially substance use—and TB, we did not find studies more deeply exploring the potential association of food insecurity and TB through the lens of behavioral health.
Interventions to Palliate Food Insecurity in the TB Population
The bidirectional relationship between nutritional deficiencies and TB infection, disease progression, and poor treatment outcomes suggests that food supplements may be of value in curtailing TB-associated morbidity and mortality [103]. A 2016 Cochrane systematic review and meta-analysis of nutritional supplements, however, suggested that there was insufficient evidence to support this approach for the improvement of TB outcomes [24]. Social protection programs have also been of interest, given the exorbitant socioeconomic costs associated with TB disease and treatment. Associated social isolation, reduced income, and increased expenditure can take a toll on entire households and negatively impact TB control via delayed diagnosis and treatment initiation, as well as subpar adherence to and completion of treatment [104].
Several studies have shown a positive impact of social interventions such as food assistance and cash transfers on anti-TB treatment adherence and completion, as well as alleviation of food insecurity. A literature review of 10 studies examining the impact of food assistance on TB treatment adherence and completion found that in the majority of cases, food provision improved adherence and treatment completion [105]. In Haiti, patients with TB who were given financial aid and incentives to attend clinics in addition to free medical care had lower rates of persistent pulmonary symptoms and mortality and higher rates of cure and resumptions of prior livelihood compared with those who only received free medical care [106]. Similarly, a study in homeless Russian patients with TB disease found that food provision resulted in higher treatment adherence and completion rates [107]. In Singapore, a grocery voucher incentive scheme for low-income TB patients on directly observed therapy resulted in statistically significantly higher treatment completion rates compared with those of patients not receiving vouchers [108]. A review of cash transfer schemes in the TB patient population suggested a positive impact on household food security and improved health care access, but no effect on adult malnutrition [109]. However, in Timor-Leste, in a randomized controlled trial of patients with TB receiving either nutritious and culturally appropriate meals or nutritional advice alone, food supplementation did not improve treatment adherence or outcomes [110]. A recent meta-analysis found some evidence that cash transfer interventions improve treatment outcomes in patients with active pulmonary tuberculosis in low- and middle-income countries, although the overall quality of the evidence in terms of research study design was low [111].
Discussion
Globally, 821 million people suffer from chronic food deprivation, and the situation has been worsening in South America and in most regions of the African continent [112]. Food insecurity has a substantial impact on health for populations; in the United States, for example, 1 study estimated the health-related costs of food insecurity to be US$160 billion [113]. Meanwhile, TB continues to be a major cause of morbidity and mortality globally, and its association with access to food and nutrition has been acknowledged for a long time [7–9].
In this narrative review of the literature, we found that while the relationship between the nutritional pathway of food insecurity—specifically undernutrition—and TB has been well studied, other potential pathways through which food insecurity may impact TB risk and TB outcomes have largely been under-researched. As a consequence of the well-defined bidirectional link between food insecurity, undernutrition, and TB, the World Health Organization’s End TB Strategy recommends assessment of nutritional status and dietary counseling for patients with TB [114] and has compiled TB-specific nutritional care guidelines [115]. Similarly, many TB programs incorporate nutritional supplementation and/or food incentives to not only improve nutritional status but also improve treatment adherence and completion. It remains unclear, however, if food assistance alone is sufficient to solve the problem of food insecurity that often coexists with TB, perhaps because providing food is a temporary solution to a more profound problem. For example, Garg et al. demonstrated that baseline maternal depression in low-income families was significantly associated with continued household food insecurity even after receiving supplemental nutrition assistance [116]. In select studies, social protection interventions such as cash transfers, food vouchers, and microfinance schemes have been shown to be an effective short-term intervention to improve treatment adherence and completion in TB treatment; however, longitudinal interventional studies are required to demonstrate the long-term impact of these interventions on both food insecurity and TB-associated mortality.
Beyond malnutrition, food insecurity has several other downstream health consequences, including mental health disruption and high-risk health behaviors. We have shown that although food insecurity and TB are each independently associated with poor mental health, mental illness as an intermediary in the relationship between food insecurity and TB is poorly described. There is a similar dearth of research on how food insecurity may be linked to TB disease and outcomes through high-risk health behavior and substance use. This is in stark contrast to the well-researched association between food insecurity and HIV/AIDS. Food insecurity has been shown to increase the risk of HIV transmission. In people living with HIV/AIDS, food insecurity has been associated with poorer adherence to antiretroviral therapy (ART), impaired viral suppression, higher rates of unprotected sex [117], lower CD4 count [118], higher incidence of opportunistic infections [119], and increased mortality [120]. Food insecurity has also been associated with depression and poor mental health in people living with HIV/AIDS, which in turn are associated with higher risk of HIV transmission and lower rates of ART use and adherence [121]. We hypothesize that food insecurity is part of a negative cycle within households that leads to increased TB disease and poor outcomes through nutritional, mental health, and behavioral pathways. In their work, Weiser et al. highlight that such pathways for food insecurity may have immunological or inflammatory mediators [4, 122].
Furthermore, just as food insecurity resulting in undernutrition is associated with higher risk of TB disease and poor outcomes [6, 11, 12, 123], TB (and other forms of ill-health) may worsen household food insecurity, particularly by rendering the patient unable to contribute the household finances. A 2014 systematic review found that on average 60% of the financial cost of TB in low- and middle-income countries comes from income loss, with only 20% from medical costs [124]. In the review, the authors found that patients often must cover health care and transportation costs, even in countries with free TB care. For some patients, these costs may plunge a household into abject poverty, which in turn predisposes the household members to poor mental health and high-risk behavior for survival’s sake.
Finally, it is also important to note that the stigma associated with substance use in patients with TB might contribute to even poorer outcomes because it may discourage patients with substance use disorder to seek treatment, may cause reluctance in resource allocation by policy-makers, and may dissuade primary care providers to screen for and treat substance use disorder [125]. However, despite the challenges, successful co-treatment of TB and substance use has been documented in several studies [126–128], and substance use should not preclude access to TB treatment.
Limitations
Our intention to perform a meta-analysis was limited by the paucity of high-quality studies. Of the 90 studies included in this review, there were only 12 systematic reviews and/or meta-analyses and no randomized control trials. The remainder of the studies consisted of cohort retrospective and prospective, cross-sectional, case–control, and narrative reviews, the majority of which pertained to the nutritional pathway and independent associations between mental health, high-risk behavior, and TB; none linked food security through mental health or high-risk behaviors as a risk factor for TB infection, disease, or poor outcomes.
Conclusions
Food insecurity is associated with TB. Through a malnutrition pathway, it has a bidirectional relationship, which increases the risk of progression from latent to active disease, may contribute to incident TB disease, and may result in suboptimal adherence to treatment and consequent poor outcomes. However, food insecurity is more than malnutrition and has been demonstrated to have multiple pathways to ill health, many of which also have linkages to TB. This review shows a paucity of research on how non-nutritional pathways may link food insecurity and TB, as well as a need for further quantification and exploration of these relationships, specifically mental health and behavioral pathways and their mediators. Longitudinal studies are required to assess the extent and relative importance of causative pathways in the relationship, to explore the current conceptual model, to understand the directions and mechanisms of the pathways, and to design and test interventions to interrupt negative interactions and improve outcomes and reduce TB incidence.
Supplementary Data
Supplementary materials are available at Open Forum Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Acknowledgments
We would to thank Cara Guenther for her research and writing on an early iteration of a portion of this paper.
Financial support. The authors declare no sources of funding support.
Potential conflicts of interest. All authors: no reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. World Health Organization. 10 facts on tuberculosis. http://www.who.int/features/factfiles/tuberculosis/en/. 2018. Accessed 2 October 2018. [Google Scholar]
- 2. International Food Policy Research Institute. Food security. http://www.ifpri.org/topic/food-security. Accessed 2 October 2018.
- 3. Caesar M, Crush J. The triple burden of HIV, TB and Food insecurity. In: Frayne B , Crush J , McCordic C, eds. Food and Nutrition Security in Southern African Cities. London: Taylor & Francis; 2017: 135–155. [Google Scholar]
- 4. Weiser SD, Young SL, Cohen CR, et al. Conceptual framework for understanding the bidirectional links between food insecurity and HIV/AIDS. Am J Clin Nutr 2011; 94:1729–39S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Berhe G, Enquselassie F, Aseffa A. Assessment of risk factors for development of active pulmonary tuberculosis in northern part of Ethiopia: a matched case control study. Ethiop Med J 2013; 51:227–37. [PubMed] [Google Scholar]
- 6. Schwenk A, Macallan DC. Tuberculosis, malnutrition and wasting. Curr Opin Clin Nutr Metab Care 2000; 3:285–91. [DOI] [PubMed] [Google Scholar]
- 7. Gauss H. Nutrition and tuberculosis. Nutr Rev 1936; 5:97–98. [Google Scholar]
- 8. Cochrane AL. Tuberculosis among prisoners of war in Germany. Br Med J 1945; 2:656–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Leyton P. The effects of slow starvation. Lancet 1946; 132:73–79. [PubMed] [Google Scholar]
- 10. Warmelink I, ten Hacken NH, van der Werf TS, van Altena R. Weight loss during tuberculosis treatment is an important risk factor for drug-induced hepatotoxicity. Br J Nutr 2011; 105:400–8. [DOI] [PubMed] [Google Scholar]
- 11. Podewils LJ, Holtz T, Riekstina V, et al. Impact of malnutrition on clinical presentation, clinical course, and mortality in MDR-TB patients. Epidemiol Infect 2011; 139:113–20. [DOI] [PubMed] [Google Scholar]
- 12. Park HO, Kim SH, Moon SH, et al. Association between body mass index and sputum culture conversion among South Korean patients with multidrug resistant tuberculosis in a tuberculosis referral hospital. Infect Chemother 2016; 48:317–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lönnroth K, Williams BG, Cegielski P, Dye C. A consistent log-linear relationship between tuberculosis incidence and body mass index. Int J Epidemiol 2010; 39:149–55. [DOI] [PubMed] [Google Scholar]
- 14. Satyanarayana K, Bhaskaram P, Seshu VC, Reddy V. Influence of nutrition on postvaccinial tuberculin sensitivity. Am J Clin Nutr 1980; 33:2334–7. [DOI] [PubMed] [Google Scholar]
- 15. Pelly TF, Santillan CF, Gilman RH, et al. Tuberculosis skin testing, anergy and protein malnutrition in Peru. Int J Tuberc Lung Dis 2005; 9:977–84. [PMC free article] [PubMed] [Google Scholar]
- 16. Chan J, Tian Y, Tanaka KE, et al. Effects of protein calorie malnutrition on tuberculosis in mice. Proc Natl Acad Sci U S A 1996; 93:14857–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Pakasi TA, Karyadi E, Wibowo Y, et al. Vitamin A deficiency and other factors associated with severe tuberculosis in Timor and rote Islands, East Nusa Tenggara Province, Indonesia. Eur J Clin Nutr 2009; 63:1130–5. [DOI] [PubMed] [Google Scholar]
- 18. Zeng J, Wu G, Yang W, et al. A serum vitamin D level <25nmol/L pose high tuberculosis risk: a meta-analysis. Cardona P-J, ed. PLoS One 2015; 10:e0126014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Pareek M, Innes J, Sridhar S, et al. Vitamin D deficiency and TB disease phenotype. Thorax 2015; 70:1171–80. [DOI] [PubMed] [Google Scholar]
- 20. Tukvadze N, Sanikidze E, Kipiani M, et al. High-dose vitamin D3 in adults with pulmonary tuberculosis: a double-blind randomized controlled trial. Am J Clin Nutr 2015; 102:1059–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Nnoaham KE, Clarke A. Low serum vitamin D levels and tuberculosis: a systematic review and meta-analysis. Int J Epidemiol 2008; 37:113–9. [DOI] [PubMed] [Google Scholar]
- 22. Centner CM, Carrara H, Harrison TB, et al. Sensory polyneuropathy in human immunodeficiency virus-infected patients receiving tuberculosis treatment. Int J Tuberc Lung Dis 2014; 18:27–33. [DOI] [PubMed] [Google Scholar]
- 23. Lamsal M, Gautam N, Bhatta N, et al. Evaluation of lipid peroxidation product, nitrite and antioxidant levels in newly diagnosed and two months follow-up patients with pulmonary tuberculosis. Southeast Asian J Trop Med Public Health 2007; 38:695–703. [PubMed] [Google Scholar]
- 24. Grobler L, Nagpal S, Sudarsanam TDSD. Nutritional supplements for people being treated for active tuberculosis. Cochrane Database Syst Rev 2011; (8): CD006086. [DOI] [PubMed] [Google Scholar]
- 25. Silverman J, Krieger J, Kiefer M, et al. The relationship between food insecurity and depression, diabetes distress and medication adherence among low-income patients with poorly-controlled diabetes. J Gen Intern Med 2015; 30:1476–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Jeon CY, Murray MB. Diabetes mellitus increases the risk of active tuberculosis: a systematic review of 13 observational studies. PLoS Med 2008; 5:e152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Zhang H, Li X, Xin H, et al. Association of body mass index with the tuberculosis infection: a population-based study among 17796 adults in rural China. Sci Rep 2017; 7:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Aibana O, Acharya X, Huang CC, et al. Nutritional status and tuberculosis risk in adult and pediatric household contacts. PLoS One 2016; 11:e0166333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Jones AD. Food insecurity and mental health status: a global analysis of 149 countries. Am J Prev Med 2017; 53:264–73. [DOI] [PubMed] [Google Scholar]
- 30. Alvarado BE, Zunzunegui MV, Béland F, et al. Social and gender inequalities in depressive symptoms among urban older adults of Latin America and the Caribbean. J Gerontol B Psychol Sci Soc Sci 2007; 62:S226–36. [DOI] [PubMed] [Google Scholar]
- 31. Deaton A, Case A. Health and wealth among the poor: India and South Africa compared. AER Pap Proc 2005; 95(2):229–33. [DOI] [PubMed] [Google Scholar]
- 32. Hadley C, Patil CL. Food insecurity in rural Tanzania is associated with maternal anxiety and depression. Am J Hum Biol 2006; 18:359–68. [DOI] [PubMed] [Google Scholar]
- 33. Patel V, Kirkwood BR, Pednekar S, et al. Gender disadvantage and reproductive health risk factors for common mental disorders in women: a community survey in India. Arch Gen Psychiatry 2006; 63:404–13. [DOI] [PubMed] [Google Scholar]
- 34. Seino K, Takano T, Mashal T, et al. Prevalence of and factors influencing posttraumatic stress disorder among mothers of children under five in Kabul, Afghanistan, after decades of armed conflicts. Health Qual Life Outcomes 2008; 6:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Weaver LJ, Hadley C. Moving beyond hunger and nutrition: a systematic review of the evidence linking food insecurity and mental health in developing countries. Ecol Food Nutr 2009; 48:263–84. [DOI] [PubMed] [Google Scholar]
- 36. Bruening M, Dinour LM, Chavez JBR. Food insecurity and emotional health in the USA: a systematic narrative review of longitudinal research. Public Health Nutr 2017; 20:3200–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Sweetland AC, Kritski A, Oquendo MA, et al. Addressing the tuberculosis-depression syndemic to end the tuberculosis epidemic. Int J Tuberc Lung Dis 2017; 21:852–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Oh KH, Choi H, Kim EJ, et al. Depression and risk of tuberculosis: a nationwide population-based cohort study. Int J Tuberc Lung Dis 2017; 21:804–9. [DOI] [PubMed] [Google Scholar]
- 39. Courtwright A, Turner AN. Tuberculosis and stigmatization: pathways and interventions. Public Health Rep 2010; 125(Suppl 4):34–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Acha J, Sweetland A, Guerra D, et al. Psychosocial support groups for patients with multidrug-resistant tuberculosis: five years of experience. Glob Public Health 2007; 2:404–17. [DOI] [PubMed] [Google Scholar]
- 41. Buregyeya E, Kulane A, Colebunders R, et al. Tuberculosis knowledge, attitudes and health-seeking behaviour in rural Uganda. Int J Tuberc Lung Dis 2011; 15:938–42. [DOI] [PubMed] [Google Scholar]
- 42. Pachi A, Bratis D, Moussas G, Tselebis A. Psychiatric morbidity and other factors affecting treatment adherence in pulmonary tuberculosis patients. Tuberc Res Treat 2013; 2013:489865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Chang SH, Cataldo JK. A systematic review of global cultural variations in knowledge, attitudes and health responses to tuberculosis stigma. Int J Tuberc Lung Dis 2014; 18:168–73, i–iv. [DOI] [PubMed] [Google Scholar]
- 44. Munro SA, Lewin SA, Smith HJ, et al. Patient adherence to tuberculosis treatment: a systematic review of qualitative research. PLoS Med 2007; 4:e238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Yan S, Zhang S, Tong Y, et al. Nonadherence to antituberculosis medications: the impact of stigma and depressive symptoms. Am J Trop Med Hyg 2018; 98:262–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Jackson SL. Psychosis due to isoniazid. Br Med J 1957; 2:743–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Duggal HS, Nizamie SH. Novel antipsychotic drugs and INH-related psychosis. Aust N Z J Psychiatry 2000; 34:343–4. [DOI] [PubMed] [Google Scholar]
- 48. Holdiness MR. Neurological manifestations and toxicities of the antituberculosis drugs. A review. Med Toxicol 1987; 2:33–51. [DOI] [PubMed] [Google Scholar]
- 49. Lansdown FS, Beran M, Litwak T. Psychotoxic reaction during ethionamide therapy. Am Rev Respir Dis 1967; 95:1053–5. [DOI] [PubMed] [Google Scholar]
- 50. Simeon J, Fink M, Itil TM, Ponce D. d-Cycloserine therapy of psychosis by symptom provocation. Compr Psychiatry 1970; 11:80–8. [DOI] [PubMed] [Google Scholar]
- 51. de Araújo GS, Pereira SM, dos Santos DN, et al. Common mental disorders associated with tuberculosis: a matched case-control study. PLoS One 2014; 9:e99551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Koyanagi A, Vancampfort D, Carvalho AF, et al. Depression comorbid with tuberculosis and its impact on health status: cross-sectional analysis of community-based data from 48 low- and middle-income countries. BMC Med 2017; 15:209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Deribew A, Tesfaye M, Hailmichael Y, et al. Common mental disorders in TB / HIV co-infected patients in Ethiopia. 2010; 10:201. [DOI] [PMC free article] [PubMed]
- 54. Naidoo P, Mwaba K. Helplessness, depression, and social support among people being treated for tuberculosis in South Africa. Soc Behav Pers 2010; 38:1323–34. [Google Scholar]
- 55. Husain MO, Dearman SP, Chaudhry IB, et al. The relationship between anxiety, depression and illness perception in tuberculosis patients in Pakistan. Clin Pract Epidemiol Ment Health 2008; 4:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Peltzer K, Naidoo P, Matseke G, et al. Prevalence of post-traumatic stress symptoms and associated factors in tuberculosis (TB), TB retreatment and/or TB-HIV co-infected primary public health-care patients in three districts in South Africa. Psychol Health Med 2013; 18:387–97. [DOI] [PubMed] [Google Scholar]
- 57. Johnson J, Kagal A, Bharadwaj R. Factors associated with drug resistance in pulmonary tuberculosis. Indian J Chest Dis Allied Sci 2003; 45:105–9. [PubMed] [Google Scholar]
- 58. Duarte EC, Bierrenbach AL, Barbosa da Silva J Jr, et al. Factors associated with deaths among pulmonary tuberculosis patients: a case-control study with secondary data. J Epidemiol Community Health 2009; 63:233–8. [DOI] [PubMed] [Google Scholar]
- 59. Kuznetsov VN, Grjibovski AM, Mariandyshev AO, et al. Hopelessness as a basis for tuberculosis diagnostic delay in the Arkhangelsk region: a grounded theory study. BMC Public Health 2013; 13:712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Pursnani S, Srivastava S, Ali S, et al. Risk factors for and outcomes of detention of patients with TB in New York City. An update: 2002–2009. Chest 2014; 145:95–100. [DOI] [PubMed] [Google Scholar]
- 61. Ambaw F, Mayston R, Hanlon C, et al. Untreated depression and tuberculosis treatment outcomes, quality of life and disability, Ethiopia. Bull World Health Organ 2018; 96:243–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Franke MF, Appleton SC, Bayona J, et al. Risk factors and mortality associated with default from multidrug-resistant tuberculosis treatment. Clin Infect Dis 2008; 46:1844–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Ugarte-Gil C, Ruiz P, Zamudio C, et al. Association of major depressive episode with negative outcomes of tuberculosis treatment. PLoS One 2013; 8:e69514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Kushel MB, Gupta R, Gee L, Haas JS. Housing instability and food insecurity as barriers to health care among low-income Americans. J Gen Intern Med 2006; 21:71–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Gugssa Boru C, Shimels T, Bilal AI. Factors contributing to non-adherence with treatment among TB patients in Sodo Woreda, Gurage Zone, Southern Ethiopia: a qualitative study. J Infect Public Health 2017; 10:527–33. [DOI] [PubMed] [Google Scholar]
- 66. Diefenbach-Elstob T, Plummer D, Dowi R, et al. The social determinants of tuberculosis treatment adherence in a remote region of Papua New Guinea. BMC Public Health 2017; 17(1):70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Escott S, Newell J. Don’t forget the bigger picture: the impact of societal issues on a community-based TB programme, Swaziland. J Health Organ Manag 2007; 21:506–18. [DOI] [PubMed] [Google Scholar]
- 68. Sebastian MS, Bothamley GH. Tuberculosis preventive therapy: perspective from a multi-ethnic community. Respir Med 2000; 94:648–53. [DOI] [PubMed] [Google Scholar]
- 69. Watkins RE, Rouse CR, Plant AJ. Tuberculosis treatment delivery in Bali: a qualitative study of clinic staff perceptions. Int J Tuberc Lung Dis 2004; 8:218–25. [PubMed] [Google Scholar]
- 70. Kupparam A, Kumar H, Chandrasekaran V, et al. Food significantly reduces plasma concentrations of first line anti tuberculosis drugs. Indian J Med Res 2017; 145:530–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Lin MY, Lin SJ, Chan LC, Lu YC. Impact of food and antacids on the pharmacokinetics of anti-tuberculosis drugs: systematic review and meta-analysis. Int J Tuberc Lung Dis 2010; 14:806–18. [PubMed] [Google Scholar]
- 72. Rehm J, Samokhvalov AV, Neuman MG, et al. The association between alcohol use, alcohol use disorders and tuberculosis (TB). A systematic review. BMC Public Health 2009; 9:450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Strike C, Rudzinski K, Patterson J, Millson M. Frequent food insecurity among injection drug users: correlates and concerns. BMC Public Health 2012; 12:1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Dewing S, Tomlinson M, le Roux IM, et al. Food insecurity and its association with co-occurring postnatal depression, hazardous drinking, and suicidality among women in peri-urban South Africa. J Affect Disord 2013; 150:460–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Kalichman SC, Simbayi LC, Kagee A, et al. Associations of poverty, substance use, and HIV transmission risk behaviors in three South African communities. Soc Sci Med 2006; 62:1641–9. [DOI] [PubMed] [Google Scholar]
- 76. Friedman LN, Williams MT, Singh TP, Frieden TR. Tuberculosis, AIDS, and death among substance abusers on welfare in New York City. N Engl J Med 1996; 334:828–33. [DOI] [PubMed] [Google Scholar]
- 77. Lönnroth K, Williams BG, Stadlin S, et al. Alcohol use as a risk factor for tuberculosis – a systematic review. BMC Public Health. 2008; 12:289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Imtiaz S, Shield KD, Roerecke M, et al. Alcohol consumption as a risk factor for tuberculosis: meta-analyses and burden of disease. Eur Respir J 2017; 50:1700216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Deiss RG, Rodwell TC, Garfein RS. Tuberculosis and illicit drug use: review and update. Clin Infect Dis 2009; 48:545–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Godoy P, Castilla J, Rullan JV. Incidence and risk factors of the association of AIDS and tuberculosis in Spain [in Spanish]. Med Clin (Barc) 1998; 110:205–8. [PubMed] [Google Scholar]
- 81. Podlekareva D, Mocroft A, Dragsted UB, et al. ; EuroSIDA Study Group Factors associated with the development of opportunistic infections in HIV-1-infected adults with high CD4+ cell counts: a EuroSIDA study. J Infect Dis 2006; 194:633–41. [DOI] [PubMed] [Google Scholar]
- 82. Oeltmann JE, Kammerer JS, Pevzner ES, Moonan PK. Tuberculosis and substance abuse in the United States, 1997–2006. Arch Intern Med 2009; 169:189–97. [DOI] [PubMed] [Google Scholar]
- 83. Garfein RS, Lozada R, Liu L, et al. High prevalence of latent tuberculosis infection among injection drug users in Tijuana, Mexico. Int J Tuberc Lung Dis 2009; 13:626–32. [PMC free article] [PubMed] [Google Scholar]
- 84. Sreeramareddy CT, Ramakrishnareddy N. Association of adult tobacco use with household food access insecurity: results from Nepal demographic and health survey, 2011. BMC Public Health 2017; 18(1):48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Armour BS, Pitts MM, Lee C-W. Cigarette smoking and food insecurity among low-income families in the United States, 2001. Am J Heal Promot 2008; 22:386–92. [DOI] [PubMed] [Google Scholar]
- 86. Kim-mozeleski JE, Seligman HK, Yen IH, et al. Changes in food insecurity and smoking status over time: analysis of the 2003 and 2015 panel study of income dynamics. Am J Heal Promot 2018; 21:890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Bates MN, Khalakdina A, Pai M, et al. Risk of tuberculosis from exposure to tobacco smoke: a systematic review and meta-analysis. Arch Intern Med 2007; 167:335–42. [DOI] [PubMed] [Google Scholar]
- 88. Slama K, Chiang CY, Enarson DA, et al. Tobacco and tuberculosis: a qualitative systematic review and meta-analysis. Int J Tuberc Lung Dis 2007; 11:1049–61. [PubMed] [Google Scholar]
- 89. Lin HH, Ezzati M, Murray M. Tobacco smoke, indoor air pollution and tuberculosis: a systematic review and meta-analysis. PLoS Med 2007; 4:e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Lindsay RP, Shin SS, Garfein RS, et al. The Association between active and passive smoking and latent tuberculosis infection in adults and children in the united states: results from NHANES. PLoS One 2014; 9:e93137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Zhang H, Xin H, Li X, et al. A dose-response relationship of smoking with tuberculosis infection: a cross-sectional study among 21008 rural residents in China. PLoS One 2017; 12:e0175183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Patra J, Jha P, Rehm J, Suraweera W. Tobacco smoking, alcohol drinking, diabetes, low body mass index and the risk of self-reported symptoms of active tuberculosis: individual participant data (IPD) meta-analyses of 72,684 individuals in 14 high tuberculosis burden countries. PLoS One 2014; 9:e96433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Díez M, Bleda MJ, Alcaide J, et al. ; Multicentre Project for Tuberculosis Research Study Group Determinants of patient delay among tuberculosis cases in Spain. Eur J Public Health 2004; 14:151–5. [DOI] [PubMed] [Google Scholar]
- 94. Storla DG, Yimer S, Bjune GA. A systematic review of delay in the diagnosis and treatment of tuberculosis. BMC Public Health 2008; 8:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Pablos-Méndez A, Knirsch CA, Barr RG, et al. Nonadherence in tuberculosis treatment: predictors and consequences in New York City. Am J Med 1997; 102:164–70. [DOI] [PubMed] [Google Scholar]
- 96. Holtz TH, Lancaster J, Laserson KF, et al. Risk factors associated with default from multidrug-resistant tuberculosis treatment, South Africa, 1999-2001. Int J Tuberc Lung Dis 2006; 10:649–55. [PubMed] [Google Scholar]
- 97. Silva MR, Pereira JC, Costa RR, et al. Drug addiction and alcoholism as predictors for tuberculosis treatment default in Brazil: a prospective cohort study. Epidemiol Infect 2017; 145:3516–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Przybylski G, Dąbrowska A, Trzcińska H. Alcoholism and other socio-demographic risk factors for adverse TB-drug reactions and unsuccessful tuberculosis treatment – data from ten years ‘ observation at the Regional Centre of Pulmonology, Bydgoszcz, Poland. Med Sci Monit 2014; 20:444–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Leung CC, Yew WW, Chan CK, et al. Smoking adversely affects treatment response, outcome and relapse in tuberculosis. Eur Respir J 2015; 45:738–45. [DOI] [PubMed] [Google Scholar]
- 100. Gajalakshmi V, Peto R, Kanaka TS, Jha P. Smoking and mortality from tuberculosis and other diseases in India: retrospective study of 43000 adult male deaths and 35000 controls. Lancet 2003; 362:507–15. [DOI] [PubMed] [Google Scholar]
- 101. Alavi-Naini R, Moghtaderi A, Metanat M, et al. Factors associated with mortality in tuberculosis patients. J Res Med Sci 2013; 18:52–5. [PMC free article] [PubMed] [Google Scholar]
- 102. Shariff N, Shah S, Kamaludin F. Predictors of death among drug-resistant tuberculosis patients in Kuala Lumpur, Malaysia: a retrospective cohort study from 2009 to 2013. J Glob Antimicrob Resist 2016; 6:102–7. [DOI] [PubMed] [Google Scholar]
- 103. Boccia D, Hargreaves J, Lönnroth K, et al. Cash transfer and microfinance interventions for tuberculosis control: review of the impact evidence and policy implications. Int J Tuberc Lung Dis 2011; 15(Suppl 2):S37–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Grede N, Claros JM, de Pee S, Bloem M. Is there a need to mitigate the social and financial consequences of tuberculosis at the individual and household level? AIDS Behav 2014; 18(Suppl 5):S542–53. [DOI] [PubMed] [Google Scholar]
- 105. de Pee S, Grede N, Mehra D, Bloem MW. The enabling effect of food assistance in improving adherence and/or treatment completion for antiretroviral therapy and tuberculosis treatment: a literature review. AIDS Behav 2014; 18(Suppl 5):S531–41. [DOI] [PubMed] [Google Scholar]
- 106. Farmer P, Robin S, Ramilus SL, Kim JY. Tuberculosis, poverty, and “compliance”: lessons from rural Haiti. Semin Respir Infect 1991; 6:254–60. [PubMed] [Google Scholar]
- 107. Gärden B, Samarina A, Stavchanskaya I, et al. Food incentives improve adherence to tuberculosis drug treatment among homeless patients in Russia. Scand J Caring Sci 2013; 27:117–22. [DOI] [PubMed] [Google Scholar]
- 108. Chua APG, Lim LKY, Ng H, et al. Outcome of a grocery voucher incentive scheme for low-income tuberculosis patients on directly observed therapy in Singapore. Singapore Med J 2015;56:274–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Boccia D, Hargreaves J, Lonnroth K, et al. Cash transfer and microfinance interventions for tuberculosis: review of the impact evidence. Int J Tuberc Lung Dis 2011; 15(Suppl 2):37–49. [DOI] [PMC free article] [PubMed]
- 110. Martins N, Morris P, Kelly PM. Food incentives to improve completion of tuberculosis treatment: randomised controlled trial in Dili, Timor-Leste. BMJ 2009; 339:b4248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Richterman A, Steer-Massaro J, Jarolimova J, et al. Cash interventions to improve clinical outcomes for pulmonary tuberculosis: systematic review and meta-analysis. Bull World Health Organ 2018; 96:471–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. FAO, IFAD, UNICEF, WFP, WHO. The State of Food Security and Nutrition in the World 2018. Building Climate Resilience for Food Security and Nutrition. Rome: Food and Agriculture Organization of the United Nations (FAO); 2018. [Google Scholar]
- 113. Cook J, Poblacion A.. 2016 Hunger Report: Estimating the Health-Related Costs of Food Insecurity and Hunger. Washington, DC: Bread for the World Institute; 2016. [Google Scholar]
- 114. World Health Organization. Implementing the End TB Strategy: the essentials 2015. http://www.who.int/tb/publications/2015/end_tb_essential.pdf?ua=1. Accessed 18 March 2019.
- 115. World Health Organization. Guideline: nutritional care and support for patients with tuberculosis.2013. http://apps.who.int/iris/bitstream/handle/10665/94836/9789241506410_eng.pdf?sequence=1. Accessed 18 March 2019.
- 116. Garg A, Toy S, Tripodis Y, et al. Influence of maternal depression on household food insecurity for low-income families. Acad Pediatr 2015; 15:305–10. [DOI] [PubMed] [Google Scholar]
- 117. Anema A, Vogenthaler N, Frongillo EA, et al. Food insecurity and HIV/AIDS: current knowledge, gaps, and research priorities. Curr HIV/AIDS Rep 2009; 6:224–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Semba RD, Darnton-Hill I, de Pee S. Addressing tuberculosis in the context of malnutrition and HIV coinfection. Food Nutr Bull 2010; 31:S345–64. [PubMed] [Google Scholar]
- 119. Weiser SD, Tsai AC, Gupta R, et al. Food insecurity is associated with morbidity and patterns of healthcare utilization among HIV-infected individuals in a resource-poor setting. AIDS 2012; 26:67–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Weiser SD, Fernandes KA, Brandson EK, et al. The association between food insecurity and mortality among HIV-infected individuals on HAART. J Acquir Immune Defic Syndr 2009; 52:342–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Weiser SD, Wolfe WR, Bangsberg DR. The HIV epidemic among individuals with mental illness in the United States. Curr Infect Dis Rep 2004; 6:404–10. [DOI] [PubMed] [Google Scholar]
- 122. Weiser SD, Palar K, Hatcher AM, et al. Food Insecurity and Health - a conceptual framework. In: Ivers LC, ed. Food Insecurity and Public Health. 2015: p23–50. [Google Scholar]
- 123. Lönnroth K, Glaziou P, Weil D, et al. Beyond UHC: monitoring health and social protection coverage in the context of tuberculosis care and prevention. PLoS Med 2014; 11:e1001693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Tanimura T, Jaramillo E, Weil D, et al. Financial burden for tuberculosis patients in low- and middle-income countries: a systematic review. Eur Respir J 2014; 43:1763–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Yang LH, Wong LY, Grivel MM, Hasin DS. Stigma and substance use disorders: an international phenomenon. Curr Opin Psychiatry 2017; 30:378–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Gourevitch MN, Wasserman W, Panero MS, Selwyn PA. Successful adherence to observed prophylaxis and treatment of tuberculosis among drug users in a methadone program. J Addict Dis 1996; 15:93–104. [DOI] [PubMed] [Google Scholar]
- 127. Batki SL, Gruber VA, Bradley JM, et al. A controlled trial of methadone treatment combined with directly observed isoniazid for tuberculosis prevention in injection drug users. Drug Alcohol Depend 2002; 66:283–93. [DOI] [PubMed] [Google Scholar]
- 128. O’Connor PG, Shi JM, Henry S, et al. Tuberculosis chemoprophylaxis using a liquid isoniazid-methadone admixture for drug users in methadone maintenance. Addiction 1999; 94:1071–5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.