Abstract
Background
Human resources for health (HRH) are the cornerstone of health systems, enabling the improvement of health service coverage. The systematic fortification of healthcare in Myanmar has accelerated since a new ruling party took office. Since 2006, Myanmar has been listed as one of the 57 crisis countries facing critical health workforce shortages. Therefore, this study aimed to assess the current situation of HRH in the public health sector where major healthcare services are provided to the people of Myanmar.
Methods
A cross-sectional study was conducted from January to May 2017 by collecting secondary data from the official statistic of the Ministry of Health and Sports (MoHS), official reports, press-releases, and presentations of Government officials. The data were collected using a formatted excel spreadsheet. A descriptive analysis was applied and the density ratio per 1,000 population for medical doctors and health workers was calculated.
Findings
In total, 16,292 medical doctors and 36,054 nurses working at 1,134 hospitals were under the management of MoHS in 2016. The finding revealed that 13 out of 15 States and Regions were below the WHO recommended minimum number of 1 per 1,000 population for medical doctor. The distribution of medical doctors per 1,000 population in the public sector showed a gradually decreasing trend since 2006. Urban and rural medical doctor ratios observed wide disparities.
Interpretation
The HRH shortage occurred in almost all State and Regions of Myanmar, including major cities. Wide disparities of HRH were found in urban and rural areas. The Myanmar government needs to consider the proper cost-effective HRH supply-chain management systems and retention strategies. The projection of health workforce, distribution of workforce by equity, effective management, and health information systems should be strengthened.
Keywords: Public health, Health profession
1. Introduction
Human resources for health (HRH) are the cornerstone of health systems [1], enabling improvements of health service coverage to allow people to enjoy their right to be healthy [2, 3]. The quality of healthcare is also facilitated by HRH good management [3, 4]. The global demand for an available, accessible, acceptable, and high quality health workforce is higher than ever [2, 5] since the World Health Organization (WHO) first assessed the crisis of health workforce shortage more than ten years ago in the World Health Report 2006 [5].
In post-millennium development goals, progress towards universal health coverage and sustainable development goals (SDGs), particularly in low- and middle-income countries, rests with resilient health workers in health systems which respond quickly and flexibly to the current context. Although WHO forecast 18 million more health workers needed in low- and middle-income countries by 2030 to achieve SDGs, it is not only about numbers [6]. The availability, accessibility, acceptability, and quality of health workforces are equally important [7]. In response to this, WHO proposed a new Global Strategy on Human Resources for Health: Workforce 2030 to inform countries that appropriate, sustainable, and cost-effective strategies to eliminate needs-based shortages in the health workforce are the way forward.
Since a new ruling party took office in April 2016, the systematic fortification of healthcare in Myanmar has accelerated. A new National Health Plan (NHP)[2017–2021] was launched, with a goal to establish basic essential packages of health services throughout the country by 2020. Since the World Health Report, 2006, Myanmar has been listed as one of the 57 crisis countries facing critical health workforce shortages [5]. However, efforts have been made to move out of crisis mode, as recent data indicate an increase in the health workforce in all cadres of health professionals [8, 9].
In Myanmar, the number of people training as health professionals is increasing every year, along with government recruitment of health professionals. In total, five medical universities for doctors, two for dental surgeons, two for pharmacists, two for medical technicians, two for nursing, one for health assistants, as well as other training schools for midwives and nurses are producing new graduate health professionals every year [10]. However, the voluntary attrition (resignation and absenteeism) rate was higher than the involuntary attrition (death or retirement) rate among health professionals, especially among medical doctors in Myanmar [11], making retention of medical doctors a challenge.
Myanmar is short of human resources for health, mainly due to a mismatch between supply and demand for health professionals. Unequal distribution of health professionals, and increasing need for health professionals due to population growth and increasing life expectancy remain challenging for Myanmar. Working in the public health sector is unattractive to health professionals due to long working hours, heavy burden of workload, unfavourable working environment, and low remuneration [12, 13].
Many young professionals seek a job in the private sector, and humanitarian organizations such as United Nations agencies, WHO, and non-governmental organizations within the country. Migration of health professionals from Myanmar to other countries is also another issue to be tackled. However, there is little known about the current situation, such as total number HRH in public sectors by profession, and distributions of health professionals by region. Therefore, this study aimed to assess the current situation for HRH in the public health sector, which is the main provider of healthcare services in Myanmar.
2. Materials and methods
2.1. Data source
A cross-sectional study was conducted from January to May 2017 by collecting secondary data from the Planning Division, Department of Medical Services, and Department of Public Health at the Ministry of Health and Sports, Nay Pyi Taw, Myanmar. The data were also gathered from the official statistics of MoHS, official reports, press-releases, and presentations from Government officials. The data were collected using a formatted excel spreadsheet. The collected data included 1) public health facilities, 2) total health workforce by profession, 3) the distribution of health workforce by States/Regions, 4) population density by urban and rural area, and 5) government health expenditures. Rural and urban areas are defined according to the Myanmar government official definitions, which were provided by Ministry of Home Affairs in Myanmar [14]. According to definition, the urban area should be met more than 20 criteria such as having at least 5,000 inhabitants or/and at least 1,000 households, availability of transportation, electricity, safe drinking water, waste and sewage management system/space, hospital, school, market, post services, religious/cultural and leisure places, the presence of agricultural and/or commercial/industrial production or services, etc.
2.2. Statistical analysis
A descriptive analysis was applied to calculate the density ratio per 1,000 population for medical doctors and health workforces (HWF). Before the analysis, a desk review was conducted. Tables and figures were prepared using Microsoft excel 2013. The total number are listed in the table. The density ratio per 1,000 population was illustrated and prepared using Microsoft excel 2013.
2.3. Ethics considerations
This study was conducted using secondary official data from the Myanmar government. The permission to access and use the data were obtained from Department of Public Health, Ministry of Health and Sports, Myanmar [Ref. PaKaYa/PaKa-AKhaKa(Kha)/2018 (413)]. The primary data collection process was not included. In addition, personal and patient information were not included in this study.
3. Results
Table 1 shows the total number of health workforce in the public sector by the union territory and 14 States/Regions including medical doctor and HWF per 1,000 population. In total, 16,292 medical doctors, 36,054 nurses, 715 dentists, 503 dental nurses, 184 pharmacists, 2,156 health assistants, 1,867 lady health visitors, 12,295 midwives, 2,465 public health supervisors (Grade I), and 11,484 public health supervisors (Grade II) were working for the public sector in Myanmar as of October 2016. Medical doctors per 1,000 population was highest in Kayah State while the lowest in Sagaing Region. Moreover, HWF per 1,000 population was the highest in Chin State while the lowest in Rakhine State.
Table 1.
Total number∗ of health workforce at public sector by the Union Territory and 14 States/Regions.
| Region/State | Doctors | Nurse | Dentist | Dental Nurse | Pharmacists | Health assistant | Lady health visitor | Midwife | Public health staff-I | Public health staff-II | Doctor: Population (Per 1000) | HWF: Population (per 1000) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Kachin | 631 | 1,470 | 34 | 27 | 7 | 80 | 75 | 438 | 118 | 408 | 0.41 | 1.96 |
| Kayah | 332 | 653 | 14 | 11 | 3 | 32 | 35 | 185 | 70 | 167 | 1.23 | 5.05 |
| Kayin | 362 | 841 | 20 | 12 | 4 | 64 | 58 | 368 | 96 | 427 | 0.32 | 1.58 |
| Chin | 390 | 841 | 20 | 10 | 2 | 81 | 63 | 371 | 68 | 468 | 1.14 | 5.73 |
| Sagaing | 1,317 | 3,219 | 69 | 49 | 22 | 256 | 173 | 1,477 | 298 | 1,544 | 0.18 | 1.39 |
| Tanintharyi | 396 | 983 | 20 | 13 | 3 | 62 | 59 | 351 | 96 | 342 | 0.4 | 1.89 |
| Bago | 1,033 | 2,439 | 49 | 37 | 16 | 212 | 197 | 1,279 | 251 | 1,102 | 0.23 | 1.32 |
| Magway | 928 | 2,174 | 48 | 38 | 15 | 196 | 179 | 1,270 | 226 | 1,267 | 0.31 | 1.67 |
| Mandalay | 2,071 | 5,157 | 94 | 57 | 28 | 170 | 195 | 1,172 | 249 | 1,223 | 0.35 | 1.29 |
| Mon | 492 | 1,081 | 21 | 15 | 7 | 76 | 79 | 507 | 86 | 427 | 0.26 | 1.32 |
| Rakhine | 660 | 1,468 | 34 | 23 | 6 | 129 | 106 | 742 | 158 | 750 | 0.25 | 1.05 |
| Shan | 1,622 | 3,566 | 94 | 63 | 18 | 253 | 213 | 1,343 | 324 | 1,268 | 0.35 | 1.53 |
| Ayeyawady | 1,168 | 2,967 | 62 | 38 | 14 | 250 | 194 | 1,626 | 255 | 1,387 | 0.22 | 1.3 |
| Yangon | 3,900 | 6,818 | 105 | 99 | 22 | 253 | 200 | 895 | 144 | 636 | 0.74 | 1.33 |
| Nay Pyi Taw | 990 | 2,377 | 31 | 11 | 17 | 42 | 41 | 271 | 26 | 68 | 0.6 | 1.62 |
| Total | 16,292 | 36,054 | 715 | 503 | 184 | 2,156 | 1,867 | 12,295 | 2,465 | 11,484 | 0.37 | 1.47 |
Source: Planning Division, Department of Medical Services, Ministry of Health and Sports, Myanmar.
As of October 2016, HWF: Health workforce.
The highest numbers of doctors, nurses, dentists, and dental nurses were working in Yangon Region (3,900 doctors, 6,818 nurses, 105 dentists, and 99 dental nurses) whereas the highest number of pharmacists were found to be in Mandalay Region (28 pharmacists). The lowest numbers of doctors, nurses, and dentists were employed in Kayah State (332 doctors, 653 nurses, and 14 dentists) while the lowest numbers of dental nurses and pharmacists were employed in Chin State (10 dental nurses and 2 pharmacists). The highest numbers of health assistants and public health supervisors (Grade II) were working in Sagaing Region [256 health assistants and 1,544 public health supervisors (Grade II)], while the highest numbers of women health visitors and public health supervisors (Grade I) worked in Shan State [213 women health visitors and 324 public health supervisors (Grade I)]. The highest number of midwives was served in Ayeyarwady Region (1,626 midwives). The lowest numbers of health assistants, women health visitors, and midwives were employed in Kayah State (32 health assistants, 35 lady health visitors, and 185 midwives) whereas the lowest numbers of public health supervisors (Grade I) and public health supervisors (Grade II) were employed in Nay Pyi Taw Union Territory [26 public health supervisors (Grade I) and 68 public health supervisors (Grade II)].
Table 2 presents the total healthcare facilities for the public sector. In total, 1,134 hospitals provide healthcare services under the management of MoHS, while 68 hospitals are managed by other ministries. In rural areas, sub-rural health centres and station hospitals are the smallest unit of health facilities, which provides primary healthcare and curative health services to the community. The station hospital usually has a 16 to 25 bed capacity for inpatient services. In total, 9,152 sub-rural health centres and 746 Station hospitals are in service across the country. Tertiary level care is offered at 38 national hospitals, which are mainly located at major cities in Myanmar. In total, 28 traditional hospitals and 210 traditional clinics provide services to the community under the management of MoHS where treatment for patients is provided mainly by Myanmar traditional medicine practitioners.
Table 2.
Healthcare facilities in Myanmar.
| Public health facility | Number∗ |
|---|---|
| Hospitals | |
| National hospitals | 38 |
| 500-bedded hospitals | 9 |
| 300-bedded hospitals | 1 |
| 200-bedded hospitals | 30 |
| 150-bedded hospitals | 2 |
| 100-bedded hospitals | 41 |
| 50-bedded hospitals | 115 |
| 25-bedded hospitals | 149 |
| 16-bedded hospitals | 10 |
| Station hospitals | 746 |
| Other∗∗ | 6 |
| Total hospitals under MoHS | 1,134 |
| Hospital under other Ministries | 68 |
| Health centers | |
| Rural/Urban health centers | 1,778 |
| Sub-rural health centers | 8,396 |
| School health teams | 80 |
| Maternal and child health centers | 348 |
| Traditional medicine | |
| Hospitals | 22 |
| Clinics | 210 |
Source: Department of Public Health, Department of Medical Services, Department of Traditional Medicine, Ministry of Health and Sports, Myanmar.
As of October 2016.
Drug treatment hospital (3), Infectious diseases hospital (1), Eye specialty hospital (1), and Dental hospital (1).
The distribution of healthcare facilities by State/Regions is shown in Table 3. The highest number of hospitals and health centers located at Sagaing Region while the lowest at Kayah State that relies on the number of townships/area coverage. Moreover, highest number of doctors and nurses concentrated in Yangon and Mandalay Regions were due to higher number of tertiary level hospitals with higher number of available beds in these regions. Similarly, traditional hospitals were concentrated at Magway Region while traditional clinics were found at Mandalay Region.
Table 3.
Total number# of healthcare facilities at public sector by the Union Territory and 14 States/Regions.
| Region/State | Health facilities under Ministry of Health and Sports |
Hospital under other ministries | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hospital |
Health centers |
Traditional medicine |
|||||||||||
| National hospitals | 200-500 bedded | 50-150 bedded | 16-25 bedded | Other∗ | Total | RHC | Sub RHC | School health team | MCH** clinic | Hospital | Clinic | ||
| Kachin State | 2 | 7 | 47 | 1 | 58 | 63 | 287 | 2 | 19 | 2 | 10 | 1 | |
| Kayah State | 1 | 1 | 15 | 2 | 17 | 29 | 116 | 1 | 6 | 2 | 5 | 2 | |
| Kayin State | 1 | 5 | 31 | 3 | 37 | 62 | 263 | 1 | 8 | 1 | 8 | 3 | |
| Chin State | 2 | 6 | 21 | - | 29 | 74 | 317 | 2 | 9 | 1 | 7 | - | |
| Sagaing Region | 4 | 17 | 118 | 6 | 139 | 236 | 1,136 | 5 | 40 | 4 | 19 | 6 | |
| Tanintharyi Region | 2 | 4 | 32 | 5 | 38 | 49 | 244 | 2 | 12 | 2 | 7 | 5 | |
| Bago Region | 3 | 13 | 93 | 7 | 109 | 189 | 843 | 5 | 35 | 2 | 22 | 7 | |
| Magway Region | 1 | 3 | 11 | 83 | 7 | 98 | 183 | 871 | 6 | 33 | 4 | 19 | 7 |
| Mandalay Region | 11 | 3 | 19 | 72 | 9 | 108 | 158 | 742 | 11 | 33 | 3 | 23 | 9 |
| Mon State | 2 | 6 | 33 | 2 | 41 | 66 | 302 | 4 | 15 | 2 | 11 | 2 | |
| Rakhine State | 2 | 12 | 51 | 2 | 65 | 121 | 558 | 4 | 18 | 1 | 11 | 2 | |
| Yangon Region | 18 | 5 | 13 | 47 | 11 | 83 | 88 | 426 | 21 | 22 | 1 | 20 | 11 |
| Shan State | 2 | 3 | 24 | 135 | 10 | 164 | 198 | 861 | 6 | 52 | 1 | 20 | 10 |
| Ayeyawady Region | 6 | 12 | 107 | 1 | 125 | 241 | 1,264 | 9 | 42 | 1 | 25 | 1 | |
| Nay Pyi Taw | 6 | 1 | 7 | 8 | 2 | 23 | 21 | 166 | 1 | 4 | 1 | 3 | 2 |
| Total | 38 | 40 | 157 | 893 | 68 | 1,134 | 1,778 | 8,396 | 80 | 348 | 28 | 210 | 68 |
Drug treatment hospital (3), Infectious diseases hospital (1), Eye specialty hospital (1), and Dental hospital (1); ∗∗Maternal and child health clinic.
As of October 2017.
Table 4 shows government health expenditure as a percentage of gross domestic product (GDP) and general government expenditure. An increasing trend was observed for government health expenditure year by year. The expenditure was increased 2.5 times from 2011-2012 financial year to 2015–2016 financial year. In the financial year 2011–2012, the government spent 1.05 % of general government expenditure, which was 0.21% of GDP. The remarkably increased was observed in 2012–2013 financial year that was 1.77 %.
Table 4.
Government health expenditure as percentage of GDP and general government expenditure (2011–2016).
| Financial year | Government health expenditure as % of gross domestic product | Government health expenditure as % of general government expenditures |
|---|---|---|
| 2011–12 | 0·21 | 1·05 |
| 2012–13 | 0·76 | 2·82 |
| 2013–14 | 0·89 | 3·15 |
| 2014–15 | 0·99 | 3·38 |
| 2015–16 | -# | 3·65 |
Data unavailable.
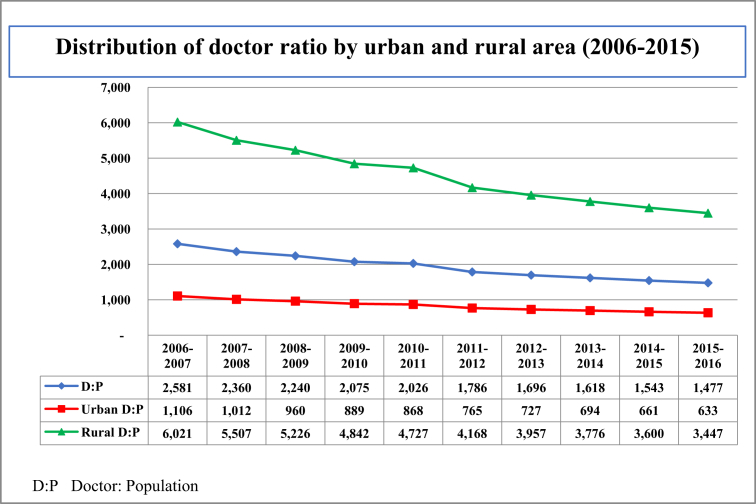
Fig. 1 shows the distribution of doctor ratio by urban and rural area from 2006 to 2015. Overall trend of the distribution of doctor ratio was decreasing for both urban and rural areas. In the financial year of 2006–2007, the ratio was one doctor per 2,581 population and that decreased to one doctor per 1,477 population in the financial year 2015–2016. However, the doctor ratio of urban and rural show wide disparity. In urban area, one doctor needs to cover 633 population while it was 3,447 population in rural area in the financial year 2015–2016.
Fig. 1.
Distribution of doctor ratio by urban and rural area.
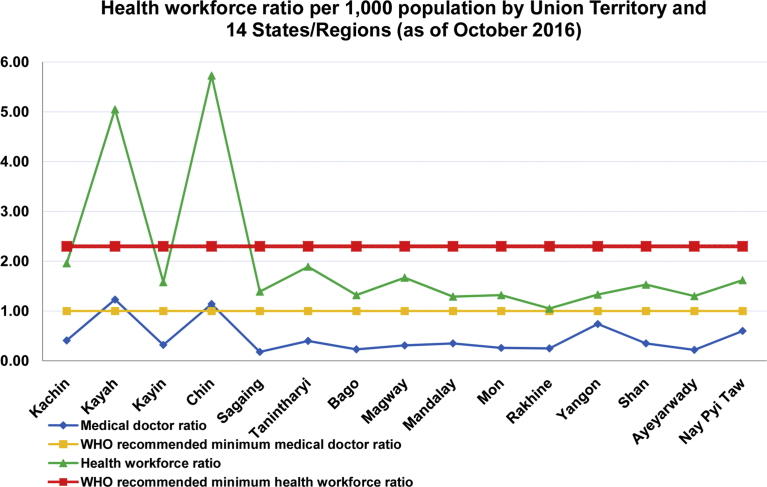
Fig. 2 represents the health workforce ratio per 1,000 population by the Union Territory and 14 States/Regions compared with the WHO recommended minimum ratio. Almost all of the Regions of Myanmar were lower than the WHO recommended minimum threshold for medical doctors and health workforce except Kayah State and Chin State; here, population is low due to geographical isolation and relatively undeveloped modes of transportation. The medical doctor ratio was lowest at Sagaing Region while Yangon Region was the highest.
Fig. 2.
Health workforce ratio per 1,000 population by the Union Territory and 14 States/Regions.
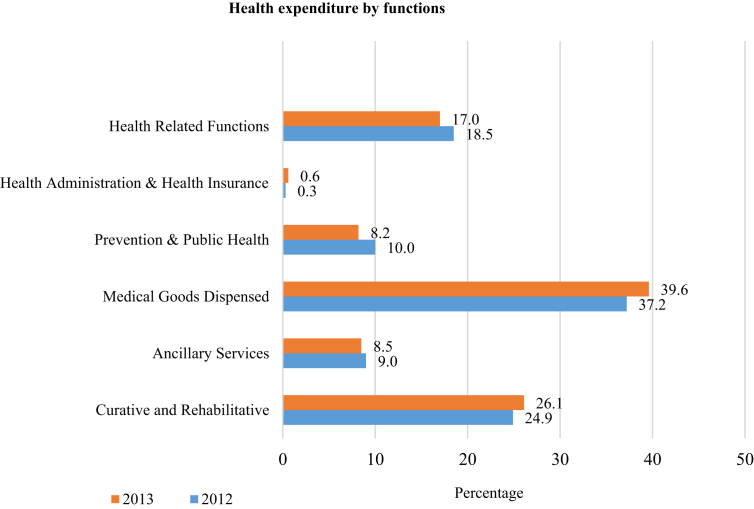
Fig. 3 shows the health expenditure of MoHS by functions comparing 2012 and 2013. Slight increases can be found in three functioning sectors: the curative and rehabilitative sector, health administration and health insurance sector, and medical goods dispensing sector. The largest portion of the total MoHS health expenditure went to medical goods dispensing sector. The expenditure of curative and rehabilitative sector was slightly increased from 24.9% in 2012 to 26.1% in 2013. The expenditure of three other functioning sectors slightly decreased. The expenditure in preventive and public health sector and in ancillary services sector dropped. But the expenditure in and health-related functions sector remained the same.
Fig. 3.
Health expenditure by functions. Source: National Health Accounts, Myanmar (2012–2013).
4. Discussion
To the best of our knowledge, this is the first study to report the human resources for health density ratio of health professionals by State and Region of Myanmar. The finding revealed that 13 out of 15 States and Regions were below the WHO recommended minimum number of 1 per 1,000 population of medical doctor [12]. Moreover, the distribution of medical doctor ratio at public sectors showed a gradually decreasing trend since 2006. The medical doctor ratio of urban and rural areas showed wide disparities.
The HRH shortage occurred in almost all State and Regions of Myanmar, including major cities and the capital city. This might be due to insufficient recruitment and increased attrition, resulting from many underlying factors. For example, few medical doctors applied for public sector jobs due to lower remuneration, unstable policy, and uneven workload. Meanwhile, Myanmar is also facing a brain drain of health professionals to places where better working conditions and remuneration are offered [11, 15].
In the past decade, positive signs of health workforce fortification were observed, such as increased recruitment of doctors, nurses, and public health supervisors [16]. At the same time, the training of medical professionals and retention strategies were also addressed [17]. For instance, new medical university and nursing/midwifery schools were established during these years to increase the production of doctors and nurses/midwives to meet demand. In addition, access to international health professional examinations, increased overseas training, and compensation for those working in hard-to-reach areas have also been implemented. Although output of health professionals has been sustainably increased, it was difficult to suddenly increase the recruitment of new graduates to work in the public health sector due to limited government budget allocation for recruitment and lack of harmonized human resources (HR) plans within the government [18].
Furthermore, the number of institutions still needs to improve to meet the standard level for the whole population. Myanmar has no private medical schools yet, as the legal regulations for private medical schools have yet to be developed. Although the number of health professionals increased in every cadre in recent years, the minimum standard level has not yet been met. In parallel to increases in the production and recruitment of health professionals, the government has upgraded hospitals and developed rural health centres without reflecting HRH priorities and projections during recent decades. Many hospitals were upgraded and established with or without the standard organizational set-up because health workforce recruitment was not sufficient. Consequently, some station hospitals cannot function well, and others are not functioning at all. Possibly due to inadequate HRH information, an HRH mismatch between production/recruitment and deployment has been in evidence. The Myanmar government needs to improve current information systems, and these reforms should be based on systematic evidence rather than ad hoc needs [19].
Limitations in institutional capacity restrict the amount of specialist training and other clinical skill based training, which may be one of the factors responsible for the attrition rate. Under current policy, two years of government service are required before medical doctors are allowed to take an entrance examination for clinical-based master degree specialties training, and at least one year of government service for other masters and postgraduate training. Most of the specialty training accepts only small proportion of total examinees. Moreover, there is no regulation in choice of subjects, which leads to an imbalance of specialties.
In 2006–2007, the ratio was one medical doctor per 2,581 population, which increased to 1,477 in 2015–2016. However, the wide disparity of this ratio was observed in urban and rural areas. In urban areas, there was one medical doctor per 633 population, while, in rural areas there was one per 3,447 population in 2015–2016. This may be due to mismanagement and inadequate institutional development plans resulting in ineffective utilization of resources, which increase unnecessary workload and creates and unfavourable working environment. For example, medical doctors in the public sector have to work 24-hour duty for 5–15 days in addition to day duty on office days, depending on available workforce. Those who work for station level hospitals have to work 24-hour emergency on-duty every day. For nurses, a morning, afternoon, and nightshift system usually applied in public hospitals in Myanmar. However, nurses also work night duty for 6–12 days. Such long working hours and irregular work shifts lead to physical and mental health problems [20], medical errors [21, 22], and poor quality of care that affects patient satisfaction [23].
Ineffective utilization of resources also contributes to disparities between urban and rural areas [24]. In rural areas, the basic healthcare staff need to cover health services including public health interventions and disease control programs for the areas they are assigned, regardless of geographic isolation, difficulties in transportation, and heavy workload due to parallel programs. It is not only due to shortage of HRH, but also unfavourable working environments, although the government provides double salary for civil servants working in hard-to-reach areas. There is no standardized incentive for the health professionals apart from salary. Even staff housing is insufficient for all healthcare workers in health facilities. The government needs to consider this disparity urgently to maintain an adequate health workforce for healthcare coverage. A regular rotation plan, increased production of local workforce, compulsory services in rural areas and the provision of an enabling environment, as well as fairness of policy, may solve this problem.
The study finding also showed the small number of the pharmacists and other allied health professionals working for the public sector in Myanmar. As a consequence, health professionals need to handle multiple job descriptions rather than that of their own specific job, which increased workload. For example, nurses have to take care of maintenance of medical equipment and pharmacy management with doctors. In Myanmar, allotment of health professionals was managed by MoHS based on their desired applications, which causes imbalances between urban and rural areas because of ineffective use of rules for appointments to rural areas, especially hard-to-reach areas.
Moreover, nowadays, the liberalization of government regarding resignation from the civil services enables people to easily leave. Although there have been no changes in the regulation of resignation, the ministry has allowed easier resignation from the civil service since 2016, which had a significant impact on the attrition rate, leading to shortage of workforce in the public sector. The remaining health workforce was further pressured, job dissatisfaction increased, with the extra workload and stress eventually forcing more staff to resign [25]. Our findings also show a decreasing trend of medical doctor ratio yearly. The ministry needs to create a stable system and transparent human resources management policies, especially for rural and hard-to-reach areas.
The ministry is attempting to fulfil the HRH gap in rural areas by capacity building and recruitment of more basic health staff. This might help to improve primary healthcare in rural areas to an extent. However, retention strategies, career development of basic health staff, and quality of care are other important dimensions to be addressed. The ministry also needs to consider HRH issues more, with a special focus on fulfilling the Basic Essential Package of Health Services at township level, and rural areas in line with Myanmar NHP (2017–2021).
Myanmar healthcare mostly relies on the public sector, and the number of health facilities in the private sector still needs to improve to increase healthcare coverage and improve quality of care. However, private sectors also have a shortage of health professionals for full-time service and must share the health workforce from the public sector. Although hospitals under MoHS have their own organizational structure, private hospitals have not yet developed a standardized structure. Other government ministries and the armed forces have their own health facilities. Armed forces also produce health professionals for healthcare at their hospitals and clinics. They also take care of civilians, especially during their tour of rural areas and support healthcare in areas affected by disaster.
In line with reforms implemented since 2011, government expenditure on health has increased notably year upon year. The government spent most of the budget on medical goods, and curative and rehabilitative services represented the second largest utilization of budget. While government expenditure on health is limited, allocation within the health sector for human resource development is still limited due to the priority given to the procurement of medicines and medical equipment. Insufficient government health expenditure is a barrier for further development of HRH. To achieve and maintain better health workforce performance, physiological needs must be fulfilled and an enabling environment is required. Skill trainings and quality of care also need more investment to become more effective. Not only insufficient expenditure, but also parallel aids/funds for health programs affect HRH distribution and overload the health workforce. This study could not explore job dissatisfaction and turnover intentions due to the nature of the secondary data.
5. Conclusion
In conclusion, HRH shortages occur across almost all State and Regions of Myanmar including major cities. Wide disparities of HRH are found in urban and rural areas. The Myanmar government needs to consider a proper cost-effective HRH supply-chain management system and retention strategies. The projection of the health workforce, distribution of workforce by equity and effective management, and health information systems should all be strengthened. For improvement of specialties, specialist training entrance policy should be revised for enhancement of training capacity. Increased production and recruitment for support health professionals such as pharmacists, medical technicians, bioengineers, dieticians, and other health allied professionals should also be planned to reduce unnecessary workload of existing health professionals. The role and responsibilities of each professional and their career pathway should be clear and well defined.
Collaboration with the private sector, other ministries, and professional and international organizations also needs attention for skilling up, training, and improvement of healthcare services. The provision of enabling working and living conditions for the health workforce may improve motivation. Transparency of policy on HR and policy adherence are also important. Providing opportunities to participate in decision making at each level, and a bottom-up approach, is also a good way to improve HR management in a more realistic way.
Declarations
Author Contribution Statement
Yu Mon Saw, Thet Mon Than, Moe Khaing, Nyeing Aye Tun, Thu Nandar Saw: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data, Contributed reagents, materials, analysis tools or data; Wrote the paper.
Yamin Thaung, Sandar Aung, Laura Wen-Shuan Shiao, Ei Mon Win: Performed the experiments; Analyzed and interpreted the data, Contributed reagents, materials, analysis tools or data; Wrote the paper.
Shigemi Iriyama, Hla Hla Win, Kayako Sakisaka, Masamine Jimba, Nobuyuki Hamajima: Conceived and designed the experiments; Analyzed and interpreted the data, Contributed reagents, materials, analysis tools or data; Wrote the paper.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Competing interest statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Acknowledgements
The authors would like to thank staff from Planning Division, Department of Medical Services, Department of Traditional Medicine, and Department of Public Health, Ministry of Health and Sports, Nay Pyi Taw, Myanmar for their support during the data collection.
References
- 1.Anyangwe S.C., Mtonga C. Inequities in the global health workforce: the greatest impediment to health in Sub-Saharan Africa. Int. J. Environ. Res. Public Health. 2007;4:93–100. doi: 10.3390/ijerph2007040002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO . Global Strategy on Human Resources for Health: Workforce 2030. World Health Organization; Geneva: 2016. Background; pp. 10–14. [Google Scholar]
- 3.Campbell J., Buchan J., Cometto G., David B., Dussault G., Fogstad H., Fronteira I., Lozano R., Nyonator F., Pablos-Méndez A., Quain E.E., Starrs A., Tangcharoensathien V. Human resources for health and universal health coverage: fostering equity and effective coverage. Bull. World Health Organ. 2013;91:853–863. doi: 10.2471/BLT.13.118729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ramadevi D., Gunasekaran A., Roy M., Rai B.K., Senthilkumar S.A. Human resource management in a healthcare environment: framework and case study. Guilsborough. 2016;48:387–393. [Google Scholar]
- 5.WHO . The World Health Report 2006: Working Together for Health. World Health Organization; Geneva: 2006. Overview: why the workforce is important; pp. xv–xix. [Google Scholar]
- 6.WHO . Health Workforce Requirement for Universal Health Coverage and the Sustainable Development Goals. WHO; Geneva: 2016. Executive summary; pp. 6–7. [Google Scholar]
- 7.Ministry of Health . Health in Myanmar 2014. Ministry of Health; Nay Pyi Taw, Myanmar: 2014. Health manpower development; p. 143. [Google Scholar]
- 8.WHO . World Health Organization; Geneva: 2013. A Universal Truth: No Health without a Workforce. [Google Scholar]
- 9.Sein T.T., Myint P., Tin N., Win H., Aye S.S., Sein T. The Republic of the Union of Myanmar; Health System Review. WHO Regional Office for the Western Pacific; Manila: 2014. Health workforce trend; pp. 92–95. [Google Scholar]
- 10.Ministry of Health . Newsletter Volume 1 No. 2. Ministry of Health and Sports; Nay Pyi Taw, Myanmar: 2016. Number of medical students attending in medical universities under Department of Human Resources for Health in the year of 2015-2016; p. 21. (In Burmese) [Google Scholar]
- 11.Htun N.M.M., Reyer J.A., Yamamoto E., Yoshida Y., Hamajima N. Trends in attrition among medical teaching staff at universities in Myanmar 2009-2013. Nagoya J. Med. Sci. 2016;78:27–40. PMID:27019526. [PMC free article] [PubMed] [Google Scholar]
- 12.Myint P., Sein T.T. World Health Organization; 2015. Myanmar Health Systems in Transition Policy Notes Series, Policy Notes #1; what Are the Challenges Facing Myanmar in Progressing towards Universal Health Coverage. [Google Scholar]
- 13.WHO. Health . World Health Statistics 2009. World Health Organization; Geneva: 2009. workforce, infrastructure and essential medicine; p. 95. [Google Scholar]
- 14.Ministry of Labor, Immigration and Population. Census Atlas Myanmar – the 2014 Myanmar Population and Housing Census. Ministry of Labor, Immigration and Population, Myanmar. Available at: http://themimu.info/sites/themimu.info/files/documents/Census_Atlas_Myanmar_the_2014_Myanmar_Population_and_Housing_Census.pdf [access on 22 January 2019].
- 15.Win, M.T. The great medical brain drain. Frontier Myanmar. Available at https://frontiermyanmar.net/en/the-great-medical-brain-drain. Accessed 27 March 2018.
- 16.The Global New Light of Myanmar. 2017, April 29. http://www.burmalibrary.org/docs23/GNLM2017-04-29-red.pdf/ Five more ministries hold press conference on one year performance. Retrieved from. [Google Scholar]
- 17.Ministry of Health and Sports . Myanmar National Health Plan (2017-2021) Ministry of Health and Sports; Nay Pyi Taw, Myanmar: 2017. Human resources for health; pp. 10–11. [Google Scholar]
- 18.Kanchanachitra C., Lindelow M., Johnston T., Hanvoravongchai P., Lorenzo F.M., Huong N.L., Wilopo S.A., dela Rosa J.F. Human resources for health in southeast Asia: shortages, distributional challenges, and international trade in health services. Lancet. 2011;377:769–781. doi: 10.1016/S0140-6736(10)62035-1. [DOI] [PubMed] [Google Scholar]
- 19.WHO . Global Strategy on Human Resources for Health: Workforce 2030. World Health Organization; Geneva: 2016. Objective 4: strengthen data on human resources for health for monitoring and accountability of national and regional strategies, and the Global Strategy; pp. 33–38. [Google Scholar]
- 20.Holden R.J., Scanlon M.C., Patel N.R., Kaushal R., Escoto K.H., Brown R.L., Alper S.J., Arnold J.M.,, Shalaby T.M., Murkowski K., Karsh B.T. A human factors framework and study of the effect of nursing workload on patient safety and employee quality of working life. BMJ Qual. Saf. 2011;20:15–24. doi: 10.1136/bmjqs.2008.028381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lockley S.W., Barger L.K., Ayas N.T., Rothschild J.M., Czeisler C.A., Landrigan C.P., Harvard Work Hours, Health. Safety Group Effects of health care provider work hours and sleep deprivation on safety and performance. Joint Comm. J. Qual. Patient Saf. 2007;33:7–18. doi: 10.1016/s1553-7250(07)33109-7. [DOI] [PubMed] [Google Scholar]
- 22.Barger L.K., Lockley S.W., Rajaratnam S.M., Landrigan C.P. Neurobehavioral, health, and safety consequences associated with shift work in safety-sensitive professions. Curr. Neurol. Neurosci. Rep. 2009;9:155–164. doi: 10.1007/s11910-009-0024-7. [DOI] [PubMed] [Google Scholar]
- 23.Bradley S., Kamwendo F., Chipeta E., Chimwaza W., de Pinho H., McAuliffe E. Too few staff, too many patients: a qualitative study of the impact on obstetric care providers and on quality of care in Malawi. BMC Pregnancy Childbirth. 2015;15:65. doi: 10.1186/s12884-015-0492-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lu J.R., Chiang T.L. Developing the adequate supply of health services: taiwan’s path to universal health coverage. Soc. Sci. Med. 2018;198:7–13. doi: 10.1016/j.socscimed.2017.12.017. [DOI] [PubMed] [Google Scholar]
- 25.Bonenberger M., Aikins M., Akweongo P., Wyss K. The effects of health worker motivation and job satisfaction on turnover intention in Ghana: a cross-sectional study. Hum. Resour. Health. 2014;12:43. doi: 10.1186/1478-4491-12-43. [DOI] [PMC free article] [PubMed] [Google Scholar]