Abstract
Michelle Remme and colleagues argue that if costs to users are considered and their financing is right, self care interventions for sexual and reproductive health can improve equity and efficiency
Globally, most of the 4.3 billion people of reproductive age in the world will lack access to adequate sexual and reproductive health services at some time in their life.1 Despite progress towards universal health coverage, the unmet need for sexual and reproductive health interventions is substantial and requires urgent attention and innovative solutions. For decades, self care products, such as the contraceptive pill, condoms, and sanitary products, have had a considerable effect on health and society.2 Technological developments have made self care products increasingly accessible, with a growing range of self administered medicines, diagnostic tests, devices, and apps.
Self care interventions include self awareness interventions for health promotion; self testing, screening, and diagnosis for disease prevention; and self management for better treatment outcomes.3 In sexual and reproductive health, tools are available for fertility management (ovulation predictors, pregnancy tests, and phone based apps), contraception (vaginal barrier methods, oral emergency contraception, and self administered medical abortion), and diagnosis of sexually transmitted infections (self tests for HIV and tests on self samples for human papillomavirus).2
Self care can increase people’s engagement with and autonomy over their health and provide an opportunity for health systems to improve equitable access to healthcare, quality of care, and financial protection for users (fig 1). Self care could improve the efficiency of healthcare delivery by including users as lay health workers, thereby increasing people’s access to essential health services. Self care could also increase the use of preventive services and adoption of preventive behaviours, improve adherence to treatment, and reduce the need for healthcare services.5
Fig 1.
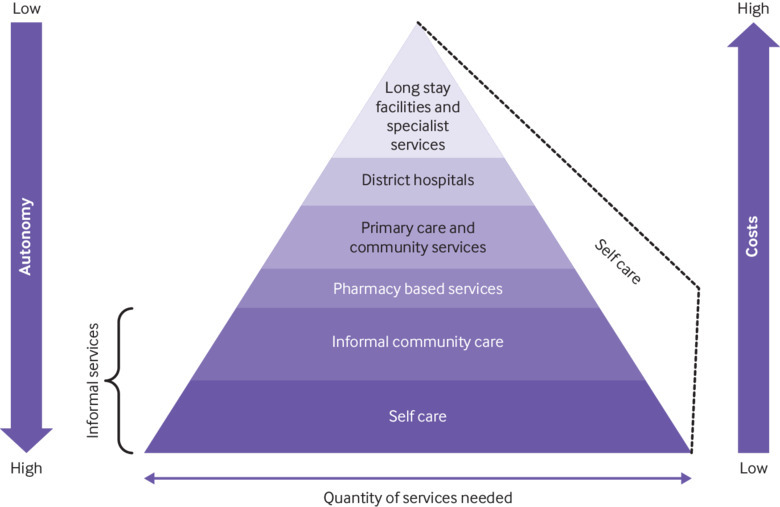
Self care within the healthcare pyramid. Adapted from Shidhaye et al4
Vulnerable and marginalised populations could gain access to sexual and reproductive health services that they would otherwise not be able to access through health providers because of stigma, discrimination, distance, or cost. However, self care could introduce or worsen vulnerabilities if it allows governments to avoid their responsibility to provide good quality healthcare. Moreover, shifting control to individuals may unintentionally shift the financial burden to the users and increase out-of-pocket expenditure.
This article aims to identify the main economic considerations of self care for sexual and reproductive health and rights in the context of universal health coverage. We consider how the use of self care interventions could affect how much societies pay to deliver interventions and produce health outcomes, and how self care interventions affect who accesses and pays for these interventions.
Costs and efficiency
Self care interventions could enable health systems to get “more health for the money,” through technical and productive efficiency gains.6 Technical efficiency would improve if self care interventions were implemented at lower costs than care provided by the healthcare system and produced the same level and quality of health outcomes. Healthcare provision would be shifted to users, patients, or their care givers and fewer health system resources would be required. Such interventions would clearly be worth prioritising over provider based alternatives.
Some self care interventions, such as home pregnancy testing, self abortion, self injection of hormonal contraceptives, and HIV self testing, have reduced costs for users. The costs are lower because the time spent seeking care at healthcare facilities and the resulting losses in productivity and income have decreased (table 1).7 8 9 10 11 In Burkina Faso, Uganda, and Senegal, non-medical client costs were lowest for women who used self injected contraceptives compared with those who used community and facility administration.7 In Malawi, people who self tested for HIV did not incur financial costs, need a family member to accompany them, or have to take time off work.8
Table 1.
Implications of sexual and reproductive health self care interventions for efficiency, financing and access
| Consideration | Evidence | |
|---|---|---|
| Costs, resources, use, and efficiency | Patient/user costs (research/information seeking, transport, lost income, financial cost of commodity/intervention, informal fees) | Use of self injecting hormonal contraceptives by women in Burkina Faso, Uganda, and Senegal had lower direct non-medical costs (travel and time costs) than community and facility based delivery7 |
| HIV self testing reduced client non-medical costs in Malawi 8 and travel costs, clinical costs, or time away from work in Tanzanian men compared with testing by healthcare providers9 | ||
| Home pregnancy test in the US saved workers’ time, and avoided clinic visits and time off work (if test was negative)10 | ||
| Health system costs (direct healthcare utilisation, indirect costs over the life course) | Self administered misoprostol for very early medical abortion had significantly lower time and costs for hospital observation and follow-up, while no differences in outcomes were found between the self administration and hospital administration groups in China11 | |
| Direct health provider costs of HIV self testing in Malawi were comparable with costs of facility based testing.8 Modelling suggested modest healthcare cost savings where a generalised epidemic exists and in a low income country12 | ||
| Self sampling for HPV testing cost more to deliver in France and the Netherlands than a “recall” intervention or conventional cytology screening (because of extra medical consultation fees, postal fees, and costs of the self sampling device), but it also had higher participation and detection rates resulting in similar or lower costs for each extra woman screened and each cervical lesion detected13 14 | ||
| Emergency contraception saved costs in modelling studies that compared spending on emergency contraception with spending on direct medical care for abortions and unintended pregnancies in Australia, Canada, and the US.15 In the US, expansion of access to emergency contraception also reduced immediate health system costs by shifting provision from hospital emergency departments to pharmacies16 | ||
| Better health outcomes at the same, lower, or acceptable higher costs (allocation efficiency) | Internet based STI self sampling cost more but was more effective at detecting STIs than clinic based sampling in the US.17 A US study that considered medical costs averted by the prevention of pelvic inflammatory disease and complications of untreated chlamydia infection estimated that the self administered intervention would be less costly and more effective than the health provider administered intervention18 | |
| HIV self testing had higher use and detection rates in multiple settings.19 However, in Malawi, self testing was less cost effective for each individual identified with HIV than health provider testing8 | ||
| Financing | User or patient out-of-pocket payments (part of the cost of the commodity or intervention paid by the user) | Demand for emergency contraception in Scotland and Spain was not affected by price and did not change when it was made available free of charge, suggesting non-financial barriers may prevent access20 |
| Respondents in the US would be willing to pay for self tests for chlamydia and gonorrhoea if they became available on the market, regardless of their age and insurance coverage21 | ||
| Subsidised public financing (domestic or external assistance) | Use of HIV self testing may need to be subsidised because the price people were willing to pay for test kits was lower than the market price in all income settings22 | |
| For condoms and contraceptives, mixed public subsidies, social marketing, and commercial provision was the most sustainable and effective way to increase coverage23 without negatively affecting equity in a multicountry study in Bangladesh, Ghana, Kenya, Indonesia, and Morocco24 | ||
| The success of national screening programmes may require government financing to include HPV self sampling as an option, as done in the Netherlands13 | ||
| Access, use, and equity | Improved access for marginalised, at risk, and vulnerable groups | HIV self testing increased use and frequency of testing in Australia, Hong Kong, Kenya, and the US19 It had a wider reach among those who may not otherwise test, including men who have sex with men in Canada19 25 |
| Studies in North America and Europe reported increased uptake of HPV testing where self sampling was offered, particularly among poor, hard to reach, and high risk populations13 26 | ||
| Self injection of hormonal contraceptive could increase access in remote areas in Uganda, where women have relatively less education and access to health information and services27 | ||
| Better access for rich people because of information or technological requirements for use | M-health self awareness interventions for sexual and reproductive health increased access to sexual and reproductive health information in men, improved couple communication and service uptake in studies in developing countries (mostly sub-Saharan Africa).28 For women, self care interventions using mobile technologies for health promotion increased access by avoiding the need for husband’s permission or financial support for transport and clinic attendance28 | |
| Demand for and supply of financial incentives to increase use | Cash payments on condition of remaining free of STIs reduced the prevalence of STIs in Tanzania and Lesotho when the amount was large enough29 |
HPV=human papillomavirus, STI=sexually transmitted infection.
Evidence also suggests that self care interventions could reduce costs for the health system.16 Self administered misoprostol for very early medical abortion can substantially lower costs of hospital observation and follow-up, with no effect on outcomes.11 Modelling of HIV self testing shows that it could reduce costs in the long run compared with testing by a healthcare provider.12 Lower healthcare utilisation (especially hospital use) and total costs were also found for self management interventions for chronic diseases, particularly for cardiovascular and respiratory problems.5
Self care could also improve productive efficiency if it results in better outcomes for the same or acceptably higher costs than care provided by healthcare facilities because of greater use, earlier diagnosis, better links to care, or fewer complications. For example, the use of self samples to test for sexually transmitted infections among women in the US was more costly than clinic testing but also more effective at detecting infections (chlamydia, gonorrhoea, trichomonas), making the cost per diagnosis potentially lower.17 Modelling showed that after screening validity and medical costs averted were taken into account, self sampling was less costly and clinically superior to clinic based sampling for chlamydia.18
It is therefore particularly important to consider future medical costs when assessing the cost effectiveness of self care interventions for family planning and self diagnosis of sexually transmitted infections.15 Given that self sampling for sexually transmitted infections and HIV self testing have higher rates of use and detection, the total costs of screening and treatment may increase because more people will need care in the short term.13 14 However, in the long term, the benefits of early diagnosis and prevention would reduce treatment costs because infections and morbidity and mortality would be reduced.19 However, evidence suggests that self sampling for sexually transmitted infections and HIV self testing may not be cost effective in settings where the prevalence of these infections is high. In these cases, symptomatic testing by a healthcare provider may produce more cases at a lower cost per case than population based self administered screening.8 30 Importantly, in the case of positive test results, linkage to care (for example, for confirmatory testing and treatment) are still an important concern both for self testing and testing by a healthcare provider.19 31
Evidence on the cost effectiveness of self care interventions for sexual and reproductive health highlights the importance of the perspective taken.8 32 Focusing on health system costs and excluding user costs could lead to misleading conclusions on whether self care provides value for money for society. For example, self injection of hormonal contraception in Uganda saved costs for society because of savings in women’s time and travel costs.32 However, from a healthcare perspective, it was more costly than facility based provision of contraception (although still probably cost effective).
Reviews of self management interventions for chronic diseases suggest that these interventions generally cost more, lead to better outcomes, and are cost effective (see appendix on bmj.com). Although these interventions improved efficiency by shifting tasks to patients, their effectiveness often depended on complementary support from the health system.
Studies on the efficiency of self care for sexual and reproductive health have only been done on a few interventions in a few settings. The findings vary depending on epidemiological factors and assumptions on linkage to care. Studies funded by the pharmaceutical industry estimate large cost savings from self medication,33 but they may underestimate the costs of unintended consequences, improper use, and inadequate health provider support.
Financing
Evidence is lacking on how self care is being financed. Possible sources of financing include out-of-pocket payments by users or patients, governments, donors, third party payers (for example, insurance companies, employers), or the private sector.6 Products available over the counter without a prescription or through mobile technologies are probably directly paid by users or subsidised by governments or not-for-profit organisations. In countries with social health insurance, some self care interventions may be partly covered by insurance providers. Private for-profit sources may finance m-health interventions (healthcare supported by mobile devices), which are provided free or at discounted prices because of the use of commercial advertising. 34
The main concern about financing is the shift in costs away from the health system to users. Out-of-pocket expenditure could increase or decrease depending on the relative cost of the facility based care, the price of self care products, and who pays for them. If cost savings for the user from seeking healthcare are more than the price of self care commodities, out-of-pocket payments could be reduced. This could contribute to reducing catastrophic health expenditure, particularly in poorer countries where the poorest households spend up to 10 times more of their income on sexual and reproductive health services than the richest households.35
If self care products cost users more than provider based care, they could increase out-of-pocket expenditure or decrease demand. According to economic theory, people demand health services if their benefits outweigh their costs.36 Because of the nature of self care interventions, people expect such interventions to provide them with immediate or direct benefits. However, these benefits may not outweigh their costs, particularly if individuals pay a large share of the costs themselves and the intervention is for an infectious disease or a health condition with substantial future healthcare costs. To account for these external effects, public subsidies are required to increase demand. For example, although indirect financial costs and travel are important barriers to facility based testing, the average price users are willing to pay for HIV self tests is lower than their end user price in all settings (table 1).9 21 22 It may be reasonably argued therefore that interventions started in health facilities and shifted to home settings should maintain the same source of financing, as seen with government financing of self collected samples for human papillomavirus (HPV) testing.26
However, the experience of initial subsidies of condoms and contraceptives highlights the need for a complementary approach across public, social marketing, and commercial sectors to ensure a sustainable supply of commodities and the best access for all people.37 Universal health coverage is not about providing access to all interventions for free, but about ensuring equitable and sustainable access to an essential package of good quality care. Since the supply (and financing) of contraceptives by the private sector may not have increased inequality in contraceptive use,24 different financing models could be used that include public subsidy for the poorest people while allowing commodities to be commercially marketed to wealthier people.23
External assistance has had an important role in financing self care interventions for sexual and reproductive health in low and middle income countries.38 Donor funds, however, are decreasing, requiring a greater reliance on domestic funds and a greater prioritisation of health in government budgets. This makes it all the more important to identify mixed domestic financing approaches for self care interventions to ensure that all needs are met.
Access, uptake, and equity
Access for everyone to high quality essential health services is the cornerstone of universal health coverage. However, access to and use of sexual and reproductive health interventions are constrained because of financial barriers as well as sociocultural, gender, and geographical factors.39 Self care interventions could help overcome these barriers, particularly for vulnerable groups and those that are hard to reach and who do not often engage with the health system.27
For example, m-health or internet based interventions that provide sexual and reproductive health information or testing for sexually transmitted infections have been found to increase men’s access to sexual and reproductive health services in all income settings (table 1).25 28 They are a new way to reach men, who are often put off by waiting times and user fees.28 For women, m-health interventions increased access to health promotion and avoided the need for spousal permission or financial support.28
Modelling studies suggest that HIV self testing could extend the reach and frequency of testing because of its convenience, privacy, and confidentiality.9 12 19 This has been the case for testing for couples and subgroups of men who have sex with men.19 25 Similarly, HPV self sampling could improve access for women who are hard to reach because of cultural perceptions of the virus and sexual behaviour.13
However, some self care interventions may make inequities worse if they increase access only for people who are socioeconomically better off. Health can be seen as a capital stock that individuals and societies can invest in throughout life.36 Similarly, the life course approach of the World Health Organization seeks to improve the functional ability of people and recognises that intervening at an earlier stage in life can show benefits at later stages.40 This approach is relevant when considering the demand for self care—who is most likely to use self care interventions, whether subsidised or not, and how this use is influenced by immediate and future benefits to the individual.
Men’s use of m-health self care interventions reflects their greater access to and ability to pay for mobile technologies, and higher mobile phone literacy.25 28 Reviews of self care e-health interventions for chronic diseases highlight that their use was restricted to people and community organisations with the means to pay for the electronic equipment; disadvantaged communities and elderly people were less likely to use these interventions (see appendix on bmj.com). Reducing these inequities of access by adapting the interventions may erode efficiency gains.
Relying on self care interventions to improve efficiency and empower users could unintentionally reduce choice of and access to complementary health services linked to diagnosis and care for poor and disadvantaged people. In the US, for example, home pregnancy tests have become the usual method for pregnancy testing, and testing through a healthcare provider may therefore be less accessible. This limits the choice of women who may prefer to use a healthcare provide or may need more support. Lack of insurance coverage to access care or age may further limit women’s choice.10
Conversely, free access to self care interventions may not necessarily lead to increased use if non-financial barriers prevent their use. For example, in Scotland and Spain, making emergency contraception available over the counter without prescription was more effective at meeting unmet demand than making it available free of charge with a prescription.20
Since financial and non-financial barriers to access are often connected, people designing self care interventions for sexual and reproductive health should consider behavioural economics. By using financial incentives, use could be increased and barriers overcome. Financial incentives have been used to create demand for and improve the supply of good quality healthcare. For example, for prevention of HIV infection, cash payments were given for negative test results for sexually transmitted infections, and they were effective in reducing the incidence of HIV infection when the financial incentives were large enough.29 Similarly, interventions that offer incentives to providers to promote self management (for asthma and diabetes) can improve quality of care (see appendix on bmj.com).
Conclusion
Self care interventions can increase individual choice and autonomy over sexual and reproductive health. Availability of self care interventions together with healthcare services may help make the health system more efficient and more targeted. Information on their costs, cost effectiveness, and financing, however, is limited. Most studies are from high income settings and lessons were drawn from non-communicable diseases. Some interventions rely on the internet or postal delivery, which is not feasible in settings with limited resources. More research is needed on how self care interventions that reduce costs and improve sexual and reproductive health outcomes and rights can be effectively delivered in these settings, whether they have harmful unintended consequences, and how they can be equitably financed.
Although self care often means self financed, data suggest that self care could reduce indirect user or patient costs and the risk of financial hardship for a household. For self care interventions to be sustainably financed, a combination of government subsidies, private financing, insurance coverage, and partial out-of-pocket payments will need to be considered, based on need and ability to pay. In the long run, the health system is still accountable for the outcomes from the use of self care and it should closely monitor the economic consequences of self care for households and governments.
Self care interventions could also contain health system costs if they maintain diagnostic accuracy, use, and quality of care. Importantly, in some cases, self care interventions have improved access and linkage to care and health outcomes. For most self care interventions to be safe and improve access, health systems will need to provide different levels of support. Otherwise, they may simply promote fragmented consumerist healthcare and undermine person centred healthcare.
While efficiency is an important objective of any health system, equity must be integral to the economic assessment of self care in terms of costs, benefits, and financing. Globally, the social geography of illness is increasingly the social geography of deprivation. A compelling argument exists for including self care as part of an integrated health system and allowing people who can manage their health to do so. Health system resources can then be focused on people who most need help—and who health systems are still failing.
Key messages.
Self care interventions may save money for users and the healthcare system, and recommendations on integrating self care tools into health systems should be based on the effect on society not just the healthcare system
Costs, benefits, and financing of self care need to be considered to determine the equity and efficiency of self care
Self care interventions must be supported by other health system interventions so that people who are less able to manage their own care are not excluded
•Mixed financing, including public subsidy, private sector financing, and direct user payment, is needed, especially for interventions that require little support from healthcare providers
Web Extra.
Extra material supplied by the author
Appendix: Summary of review articles
Contributors and sources: MR, MN and PA conceived the study. MR, LV and FG reviewed the literature. MR drafted the manuscript. All authors revised the manuscript. MR is study guarantor.
Competing interests: All authors have read and understood BMJ policy on declaration of interests and have no relevant interests to declare.
Provenance and peer review: Commissioned; externally peer reviewed.
This article is part of a series proposed by the UNDP/UNFPA/Unicef/WHO/World Bank Special Programme for Human Reproduction (HRP) and commissioned by The BMJ. The BMJ retained full editorial control over external peer review, editing, and publication of these articles. Open access fees are funded by HRP.
References
- 1. Starrs AM, Ezeh AC, Barker G, et al. Accelerate progress-sexual and reproductive health and rights for all: report of the Guttmacher-Lancet Commission. Lancet 2018;391:2642-92. 10.1016/S0140-6736(18)30293-9 [DOI] [PubMed] [Google Scholar]
- 2. Murray M. Women’s self care: products and practices. PATH, 2017. [Google Scholar]
- 3. Narasimhan M, Allotey P, Hardon A. Self care interventions to advance health and well-being: a conceptual framework to inform normative guidance. BMJ 2019;365:l688 10.1136/bmj.l688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Shidhaye R, Lund C, Chisholm D. Health care platform interventions. mental, neurological, and substance use disorders: disease control priorities. Vol 4, 3rd ed The International Bank for Reconstruction and Development/The World Bank, 2016. [Google Scholar]
- 5. Panagioti M, Richardson G, Small N, et al. Self-management support interventions to reduce health care utilisation without compromising outcomes: a systematic review and meta-analysis. BMC Health Serv Res 2014;14:356. 10.1186/1472-6963-14-356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. World Health Organization World health report: health systems financing: The path to universal coverage. WHO, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Di Giorgio L, Mvundura M, Tumusiime J, et al. Costs of administering injectable contraceptives through health workers and self-injection: evidence from Burkina Faso, Uganda, and Senegal. Contraception 2018;98:389-95. 10.1016/j.contraception.2018.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Maheswaran H, Petrou S, MacPherson P, et al. Cost and quality of life analysis of HIV self-testing and facility-based HIV testing and counselling in Blantyre, Malawi. BMC Med 2016;14:34. 10.1186/s12916-016-0577-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Jennings L, Conserve DF, Merrill J, et al. Perceived cost advantages and disadvantages of purchasing hiv self-testing kits among urban Tanzanian men: an inductive content analysis. J AIDS Clin Res 2017;8. 10.4172/2155-6113.1000725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Childerhose JE, Macdonald ME. Health consumption as work: the home pregnancy test as a domesticated health tool. Soc Sci Med 2013;86:1-8. 10.1016/j.socscimed.2013.02.035 [DOI] [PubMed] [Google Scholar]
- 11. Li C-L, Song LP, Tang SY, et al. Efficacy, safety, and acceptability of low-dose mifepristone and self-administered misoprostol for ultra-early medical abortion: a randomized controlled trial. Reprod Sci 2017;24:731-7. 10.1177/1933719116669055 [DOI] [PubMed] [Google Scholar]
- 12. Cambiano V, Ford D, Mabugu T, et al. Assessment of the potential impact and cost-effectiveness of self-testing for HIV in low-income countries. J Infect Dis 2015;212:570-7. 10.1093/infdis/jiv040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Madzima TR, Vahabi M, Lofters A. Emerging role of HPV self-sampling in cervical cancer screening for hard-to-reach women: Focused literature review. Can Fam Physician 2017;63:597-601. [PMC free article] [PubMed] [Google Scholar]
- 14. Haguenoer K, Sengchanh S, Gaudy-Graffin C, et al. Vaginal self-sampling is a cost-effective way to increase participation in a cervical cancer screening programme: a randomised trial. Br J Cancer 2014;111:2187-96. 10.1038/bjc.2014.510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Trussell J, Calabretto H. Cost savings from use of emergency contraceptive pills in Australia. Aust N Z J Obstet Gynaecol 2005;45:308-11. 10.1111/j.1479-828X.2005.00417.x [DOI] [PubMed] [Google Scholar]
- 16. Gross T, Lafortune J, Low C. What happens the morning after? The costs and benefits of expanding access to emergency contraception. J Policy Anal Manage 2014;33:70-93. 10.1002/pam.21731 [DOI] [PubMed] [Google Scholar]
- 17. Blake DR, Spielberg F, Levy V, et al. Could home sexually transmitted infection specimen collection with e-prescription be a cost-effective strategy for clinical trials and clinical care? Sex Transm Dis 2015;42:13-9. 10.1097/OLQ.0000000000000221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Huang W, Gaydos CA, Barnes MR, Jett-Goheen M, Blake DR. Cost-effectiveness analysis of Chlamydia trachomatis screening via internet-based self-collected swabs compared with clinic-based sample collection. Sex Transm Dis 2011;38:815-20. 10.1097/OLQ.0b013e31821b0f50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Johnson CC, Kennedy C, Fonner V, et al. Examining the effects of HIV self-testing compared to standard HIV testing services: a systematic review and meta-analysis. J Int AIDS Soc 2017;20:21594. 10.7448/IAS.20.1.21594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Trilla C, Senosiain R, Calaf J, Espinós JJ. Effect of changes to cost and availability of emergency contraception on users’ profiles in an emergency department in Catalunya. Eur J Contracept Reprod Health Care 2014;19:259-65. 10.3109/13625187.2014.913787 [DOI] [PubMed] [Google Scholar]
- 21. Pearson WS, Kreisel K, Peterman TA, et al. Improving STD service delivery: would American patients and providers use self-tests for gonorrhea and chlamydia? Prev Med 2018;115:26-30. 10.1016/j.ypmed.2018.08.007 [DOI] [PubMed] [Google Scholar]
- 22. Stevens DR, Vrana CJ, Dlin RE, Korte JE. A global review of HIV self-testing: themes and implications. AIDS Behav 2018;22:497-512. 10.1007/s10461-017-1707-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hanson K, Kumaranayake L, Thomas I. Ends versus means: the role of markets in expanding access to contraceptives. Health Policy Plan 2001;16:125-36. 10.1093/heapol/16.2.125 [DOI] [PubMed] [Google Scholar]
- 24. Agha S, Do M. Does an expansion in private sector contraceptive supply increase inequality in modern contraceptive use? Health Policy Plan 2008;23:465-75. 10.1093/heapol/czn035 [DOI] [PubMed] [Google Scholar]
- 25. Gilbert M, Hottes TS, Kerr T, et al. Factors associated with intention to use internet-based testing for sexually transmitted infections among men who have sex with men. J Med Internet Res 2013;15:e254. 10.2196/jmir.2888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Gupta S, Palmer C, Bik EM, et al. Self-sampling for human papillomavirus testing: increased cervical cancer screening participation and incorporation in international screening programs. Front Public Health 2018;6:77. 10.3389/fpubh.2018.00077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Cover J, Namagembe A, Tumusiime J, Lim J, Drake JK, Mbonye AK. A prospective cohort study of the feasibility and acceptability of depot medroxyprogesterone acetate administered subcutaneously through self-injection. Contraception 2017;95:306-11. 10.1016/j.contraception.2016.10.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Jennings L, Gagliardi L. Influence of mHealth interventions on gender relations in developing countries: a systematic literature review. Int J Equity Health 2013;12:85. 10.1186/1475-9276-12-85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Björkman Nyqvist M, Corno L, de Walque D, Svensson J. Incentivizing safer sexual behavior: evidence from a lottery experiment on HIV prevention. Am Econ J Appl Econ 2018;10:287-314 10.1257/app.20160469. [DOI] [Google Scholar]
- 30. van Valkengoed IG, Postma MJ, Morré SA, et al. Cost effectiveness analysis of a population based screening programme for asymptomatic Chlamydia trachomatis infections in women by means of home obtained urine specimens. Sex Transm Infect 2001;77:276-82. 10.1136/sti.77.4.276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Fajardo-Bernal L, Aponte-Gonzalez J, Vigil P, et al. Home-based versus clinic-based specimen collection in the management of Chlamydia trachomatis and Neisseria gonorrhoeae infections. Cochrane Database Syst Rev 2015;(9):CD011317. 10.1002/14651858.CD011317.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Di Giorgio L, Mvundura M, Tumusiime J, Morozoff C, Cover J, Drake JK. Is contraceptive self-injection cost-effective compared to contraceptive injections from facility-based health workers? Evidence from Uganda. Contraception 2018;98:396-404. 10.1016/j.contraception.2018.07.137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Self care: better daily health for individuals and societies. A global policy blueprint. Bayer, 2018. [Google Scholar]
- 34. Mangone ER, Lebrun V, Muessig KE. Mobile phone apps for the prevention of unintended pregnancy: a systematic review and content analysis. JMIR Mhealth Uhealth 2016;4:e6. 10.2196/mhealth.4846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Haghparast-Bidgoli H, Pulkki-Brännström AM, Lafort Y, et al. Inequity in costs of seeking sexual and reproductive health services in India and Kenya. Int J Equity Health 2015;14:84. 10.1186/s12939-015-0216-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Grossman M. On the concept of health capital and the demand for health. J Polit Econ 1972;80:223-55 10.1086/259880. [DOI] [Google Scholar]
- 37. Chapman S, Jafa K, Longfield K, et al. Condom social marketing in sub-Saharan Africa and the Total market approach. Sex Health 2012;9:44-50. 10.1071/SH10165 [DOI] [PubMed] [Google Scholar]
- 38. Grollman C, Arregoces L, Martínez-Álvarez M, Pitt C, Mills A, Borghi J. 11 years of tracking aid to reproductive, maternal, newborn, and child health: estimates and analysis for 2003-13 from the Countdown to 2015. Lancet Glob Health 2017;5:e104-14. 10.1016/S2214-109X(16)30304-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Wulifan JK, Brenner S, Jahn A, De Allegri M. A scoping review on determinants of unmet need for family planning among women of reproductive age in low and middle income countries. BMC Womens Health 2016;16:2. 10.1186/s12905-015-0281-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Kuruvilla S, Sadana R, Montesinos EV, et al. A life-course approach to health: synergy with sustainable development goals. Bull World Health Organ 2018;96:42-50. 10.2471/BLT.17.198358 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix: Summary of review articles


