Abstract
The robotic surgical system has been applied in liver surgery. However, controversies concerns exist regarding a variety of factors including the safety, feasibility, efficacy, and cost-effectiveness of robotic surgery. To promote the development of robotic hepatectomy, this study aimed to evaluate the current status of robotic hepatectomy and provide sixty experts’ consensus and recommendations to promote its development. Based on the World Health Organization Handbook for Guideline Development, a Consensus Steering Group and a Consensus Development Group were established to determine the topics, prepare evidence-based documents, and generate recommendations. The GRADE Grid method and Delphi vote were used to formulate the recommendations. A total of 22 topics were prepared analyzed and widely discussed during the 4 meetings. Based on the published articles and expert panel opinion, 7 recommendations were generated by the GRADE method using an evidence-based method, which focused on the safety, feasibility, indication, techniques and cost-effectiveness of hepatectomy. Given that the current evidences were low to very low as evaluated by the GRADE method, further randomized-controlled trials are needed in the future to validate these recommendations.
Keywords: Minimally invasive surgery, Robotic hepatectomy, Laparoscopic hepatectomy, Hepatectomy resection, Consensus statement
Core tip: The robotic surgical system has been applied in liver surgery. Liver surgeons are also attempting to gradually expand the indications of robotic hepatectomy. To promote the development and standardization of robotic hepatectomy, we identified a group of robotic surgeon experts to provide clinical statements. Based on the published articles and expert panel opinion, 7 recommendations were generated by the GRADE method using an evidence-based method and focused on the safety, feasibility, indication, techniques and cost-effectiveness of hepatectomy. Since the current evidences were low to very low as evaluated by the GRADE method, further randomized controlled trials are needed in the future to validate these recommendations.
INTRODUCTION
In 1987, Mouret performed the first laparoscopic cholecystectomy, which started the era of minimally invasive hepatobiliary surgery[1]. In the 1990s, the use of laparoscopic hepatectomy for benign and malignant tumors was independently reported by Katkhouda, Reich, and others[2,3]. After decades of development, the application of laparoscopic techniques in hepatectomy has become more mature. In 2008, the first consensus guidelines for laparoscopic hepatectomy were published in Louisville, signifying the gradual standardization of minimally invasive hepatectomy[4]. Meanwhile, with the advancement of technology, robot-assisted laparoscopic surgical systems have also continuously evolved. In 1997, Himpens et al[5] successfully performed robotic cholecystectomy, and this new type of laparoscopic surgical systems began to be implemented in clinical practice. In 2000, the new generation da Vinci robotic surgical system was officially approved by the United States Food and Drug Administration and was then gradually accepted by surgeons. Robot-assisted laparoscopic surgical systems possess advantages, such as providing a clear, stable, and magnified field of vision, flexibility, it is ergonomic, and has a tremor filter. Specifically, the flexibility and the clear and stable vision have overcome the major disadvantages of conventional laparoscopy. However, the absence of tactile feedback, high cost of mainstream models, and the lack of available surgical instruments, also limit its clinical development and application.
In 2003, Giulianotti et al[6-11] reported for the first time the application of robot-assisted laparoscopic system in segmental hepatic resection. Since then, countries such as the United States, Europe, China, South Korea, Singapore, Russia, India, and Brazil have reported their own experience on robotic hepatectomy. For example, in China, the Da Vinci robot-assisted laparoscopic surgical system has completed 26765 operations in mainland China as of 2017, which is more than 5 times the number of completed cases in 2014 (4982 operations). The annual growth rate is approximately 45%, with robotic hepatobiliary surgery accounting for approximately 10% of the total number of robotic operations.
Meanwhile, liver surgeons are also attempting to gradually expand the indications of robotic hepatectomy. The earliest cases of robotic hepatectomy included wedge hepatectomy, hemihepatectomy, and extended hemihepatectomy. Some surgeons also utilized robotic hepatectomy to perform segmental resection of posterosuperior segments, liver donor hepatectomy, and the associating liver partition with portal vein ligation for staged hepatectomy[12-16]. However, due to the complexity of the techniques involved in liver surgery, the implementation and popularization of minimally invasive hepatectomy, including robotic hepatectomy, has remained challenging. In 2014, a nationwide survey on hepatectomy conducted by the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) showed that minimally-invasive hepatectomy accounted for 17.9% of all hepatectomy cases in the United States, of which robotic hepatectomy merely accounted for 5.3% of minimally invasive hepatectomy cases[17]. According to the statistics reported by the Italian National Survey Study Group, between January 1, 1995 and February 28, 2012, the proportion of minimally-invasive hepatectomy was approximately 10.3%[18]. A retrospective analysis of a large surgical oncology program conducted by the University of Pittsburgh Medical Center between 2009 and 2014 (1236 surgeries were analyzed, including 157 robotic liver surgeries) showed that the conversion rate was 3.1%, overall incidence rate of complications was 18.6%, and 90-day mortality rate was 1.1%. Among cases of perioperative mortality, 91% were from robotic hepatobiliary procedures. For robotic liver/bile duct procedures, the incidence of complications was 26.1%, mortality rate was 3.2%, and conversion rate was 7.6%, which were all above the overall mean values of robotic procedures[19]. Buchs et al[20] analyzed 884 cases of robotic surgery performed at the University of Illinois Hospital between April 2007 and June 2010 and found that hepatectomy was considered as an advanced robotic procedure, and multivariate analysis showed that advanced procedure was a factor significantly associated with a higher risk for complications.
Although most reports to date show that robotic hepatectomy are safe, feasible and effective, the majority of these studies are case reports and case series from high-volume centers. There are relatively few case-control studies with large sample sizes, and high-quality randomized controlled studies are lacking[6,11,21-56]. According to the findings of current studies, the effectiveness of robotic hepatectomy is essentially identical to that of open surgery and traditional laparoscopic hepatectomy. However, conclusions on operative time, intraoperative blood loss, conversion rate, incidence of postoperative complications, and overall cost-benefit ratio remain divided in different reports, with the main controversy surrounding the application of certain procedure modalities. These factors severely limit the application of robotic hepatectomy[6,21,23,24,31,32,36,37,39,42,57]. Some researchers have pointed out that it is undesirable to simply increase economic expenses and aggressively apply robot-assisted laparoscopic surgical system for procedures such as living-donor hepatectomy while therapeutic efficacy is not improved[58-61]. Other opinions point out that as a developing and advancing surgical technology,robotic surgery will become effective enough to allow us to correct any complications with its own techniques[62].
To promote the development and standardization of robotic hepatectomy and improve patient safety, we identified a group of robotic surgeon experts (based on the number of robotic liver surgeries and published papers to screen experts with international influence) to provide clinical statements related to robotic surgery. We searched the online databases for published articles related to robotic surgery; with evidence-based methods. All evidences were graded using the GRADE system and upgraded or downgraded after integrating experts’ opinions until a final consensus was reached.
METHODS
We referred to the World Health Organization Handbook for Guideline Development and established the Consensus Steering Group, consisting of five experts in the field from all around the world, with the following missions: To (1) approve the use of PICOs (population, intervention, comparator, outcomes); (2) supervise the literature search and systematic reviews; (3) check the grade of the evidence; (4) draft the final recommendations using a modified Delphi approach; and (5) approve the publication of the consensus. The Consensus Development Group is a multidisciplinary group of 30 experts, including clinicians, methodologists, and economists, with the following missions: To (1) define the scope of the consensus, draft the PICOs; (2) grade the quality of the evidence; (3) draft preliminary recommendations; (4) write the draft consensus; and (5) publish and promote the consensus. The Consensus Secretary Group is responsible for conducting systematic reviews and investigation of patients’ views and preferences, along with the Chinese GRADE Center, for providing methodological support. All members of the Consensus Steering Group and the Consensus Secretary Group were required to disclose potential conflicts of interest, which were reviewed by the chairs. No relevant conflicts of interest were noted.
We have held 4 meetings until now on questions focusing on hepato-pancreato-biliary minimally invasive surgery, in Beijing (April, 2017), Lanzhou (October, 2017), Beijing (April, 2018), and Hong Kong (October, 2018) involving more than 60 clinical experts. Finally, we formulated sixteen PICO questions for the consensus. Published articles and conference abstracts were identified from PubMed, Embase, the Cochrane Library. Additionally, we used the GRADE approach to rate the quality of evidence and the strength of recommendation. The experts in the Consensus Development Group voted on the recommendations according to the quality of evidence, patients’ views and preferences, and economic evaluation. The GRADE Grid method and Delphi vote were used to formulate the recommendations. Three rounds of voting were conducted. When 70% of the experts approved a recommendation, a consensus was assumed to have been reached.
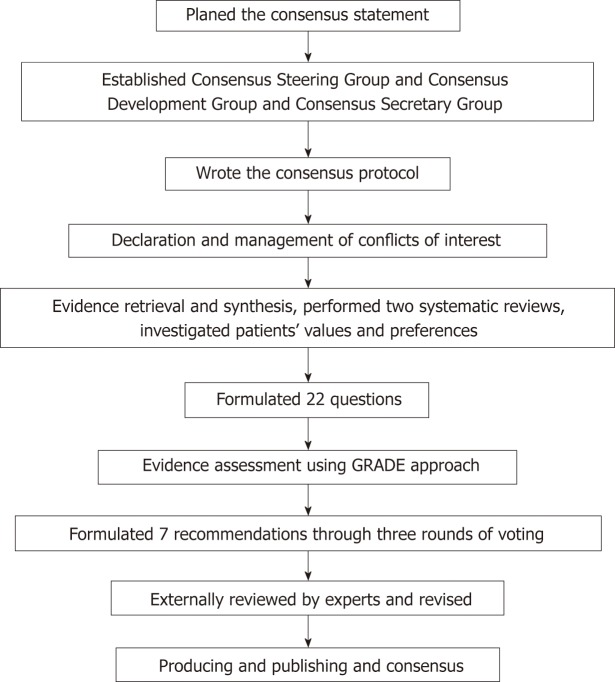
The formulated recommendations were submitted to 24 experts, who have a broad clinical experience in hepatobiliary minimally invasive surgery. The external reviewers were not involved in the development of the consensus. The Consensus Steering Group discussed the external reviews in a meeting and revised the recommendations based on this feedback (Table 1). The Consensus Steering Group plans to update the guideline again before 2022. A flow chart describes the process of the consensus development (Figure 1)
Table 1.
2018 International statement on robotic hepatectomy
| Recommendation | Grade | |
| 1 | RH is as safe and feasible as traditional OH. RH has longer operative time, less intraoperative blood loss, LOS, lower complication rate and lower severe complication rate. The intraoperative blood loss of RH is comparable to that of OH. | 2C |
| 2 | RH has similar effectiveness for liver malignancy lesion compared to OH. Regarding the oncological outcome there is no significant difference in the radical resection rate, overall survival rate and recurrence rate between RH and OH. | 2D |
| 3 | As a minimally invasive surgery, RH is as safe and feasible as traditional LH. RH has longer operative time, more intraoperative blood loss, and higher cost. RH has similar overall complication rate and LOS compared to OH. Conversion rate of RH would decrease with the experience accumulation. | 2D |
| 4 | As minimally invasive surgery, RH has similar effectiveness for liver malignancy disease compared to LH. Regarding the oncological outcome there is no significant difference in the radical resection rate, overall survival rate and recurrence rate between RH and LH. | 2D |
| 5 | For minor hepatectomy, RH as safe and feasible as LH and OH. RH has longer operative time than LH for minor hepatectomy. The intraoperative blood loss, overall postoperative complication rate and overall cost of robotic minor hepatectomy are comparable to that of laparoscopic minor hepatectomy. | 2D |
| 6 | For major hepatectomy, RH as safe and feasible as LH and OH. RH has longer operative time than LH for major hepatectomy. The intraoperative blood loss, overall postoperative complication rate and overall cost of robotic major hepatectomy are comparable to that of laparoscopic major hepatectomy. There is no significant difference in the operative time, intraoperative blood loss and complication rate between RH and OH for minor hepatectomy. | 2D |
| 7 | Robotic liver donor hepatectomy could be an alternative. The procedure should only be performed by experienced surgeons, and the true benefits of robotic donor hepatectomy need further investigation in the future. | 2D |
RH: Robotic hepatectomy; OH: Open hepatectomy; LH: Laparoscopic hepatectomy; LOS: Length of hospital stay.
Figure 1.
Flow chart describes the process of the consensus development.
Recommendation 1: Robotic hepatectomy is as safe and feasible as traditional open hepatectomy. Robotic hepatectomy has longer operative time, less intraoperative blood loss, less length of hospital stays, lower complication rate and lower severe complication rate. The intraoperative blood loss of robotic hepatectomy is comparable to that of open hepatectomy. The level of evidence: low. Level of recommendation: Weak (Grade 2C)
Although the volume of minimally-invasive hepatectomy has been increasing each year since the minimally-invasive technique was applied in hepatectomy in the 1990s, in the United States and Italy, minimally-invasive hepatectomy merely accounts for 17.9% and 10.3% of hepatectomy cases, respectively[17,18]. When subjected to the technical limitations of conventional laparoscopy, from the perspective of operative difficulty, most procedures are still mainly focused on the less complex minimally invasive wedge resection/segmentectomy (44.9%) and minimally-invasive left lateral sectionectomy (20.3%)[63,64]. The robot-assisted laparoscopic systems overcome the disadvantages of conventional laparoscopy by providing flexibility and sharp field of vision, but the lack of feedback and high cost have also led to some controversies regarding their applications. Compared with open hepatectomy, robotic hepatectomy is characterized by longer operative time, less intraoperative blood loss, lower blood transfusion rate, less length of hospital stays (LOS), and lower complication rate[32,36,44,65,66].
Wong et al[23] reported a meta-analysis of 7 retrospective, case-control studies on robotic and open hepatectomy conducted between 2013 and 2016. The analysis evaluated the intraoperative and short-term postoperative outcome in 329 cases of robotic hepatectomy and 426 cases of open hepatectomy in Italy, the United States, Switzerland, and China. The results revealed that compared with open hepatectomy: Regarding intraoperative parameters, robotic hepatectomy had a longer operative time [mean difference (MD) = 61.47 min; 95% confidence interval (CI): 7.03, 115.91], but there were no significant differences in intraoperative blood loss (MD = 220.44 mL; 95%CI: -447.47, 6.58), blood transfusion rate [risk ratio (RR) = 0.78; 95%CI: 0.33, 1.83], and Pringle maneuver usage (RR= 0.98; 95%CI: 0.09, 11.34). The mean conversion rate of patients in the robotic surgery group in these studies was 4.4%; regarding short-term postoperative outcome, robotic hepatectomy led to shorter LOS (MD = -2.57 d; 95%CI: -3.31, -1.82), lower overall complications rate (RR = 0.63; 95%CI: 0.46, 0.86), and lower major (Clavien-Dindo grade III or higher[67]) complication rate (RR = 0.45; 95%CI: 0.22, 0.94).
Although it was previously believed that high cost is a major disadvantage of robotic hepatectomy, only a few reports have compared the cost of the 2 approaches and the conclusions are inconsistent. To date, the report with the largest sample size is published by Sham et al[65], who compared the cost of robotic hepatectomy (n = 71) and open hepatectomy (n = 88); their study was conducted in at a single center between 2011 and 2015. The results showed that although the perioperative costs were higher in the robotic surgery group (6026 vs 5479$, P = 0.047), the postoperative costs were lower (68570 vs 13425$, P < 0.001), and the total cost was lower (14754 vs 18998$, P < 0.001).
Daskalaki et al[32] compared patients admitted to a single center between 2009 and 2013 and found that compared with the conventional open hepatectomy (n = 55), the total cost of the robotic group (n = 68) was slightly lower (36040$ vs 39924$, T-Stat = -0.79). In contrast, Xu et al[68] compared the efficacy of robotic hepatectomy and open hepatectomy for the treatment of hilar cholangiocarcinoma in a single center between 2009 and 2012, and the results showed that compared with open hepatectomy (n = 32), the surgical costs were higher in the robotic group (n = 10) (272427$ ± 21316$ vs 15282$ ± 5957$, P = 0.018).
Recommendation 2: Robotic hepatectomy has similar effectiveness for liver malignancy lesion compared to open hepatectomy. Regarding the oncological outcome there is no significant difference in the radical resection rate, overall survival rate and recurrence rate between robotic hepatectomy and open hepatectomy. Level of recommendation: Very low. Level of recommendation: Weak (Grade 2D)
Open hepatectomy is currently the standard for surgical treatment of liver cancer. There is yet to be a large-scale randomized controlled trial comparing the efficacy of robotic hepatectomy and open hepatectomy in malignant tumors, and most studies have been retrospective, case-control studies. Hepatocellular carcinoma is the most common primary malignant tumor of the liver.
In 2013, Lai et al[69] reported that among patients with hepatocellular carcinoma who received robotic hepatectomy, the R0 resection rate was 93%. After a median follow up of 14 mo, the 2-year overall and disease-free survival was 94%, and 74%, respectively. In the most recent single-center study published by Wang et al[66] in 2018, the follow-up results in patients newly diagnosed with hepatocellular carcinoma who underwent robotic hepatectomy (n = 63) and open hepatectomy (n =177) between June 2013 and July 2016 showed that the 2 approaches had no significant differences with regard to the R0 resection rate (93.7% vs 96%, P = 0.56), overall recurrence rate (27% vs 37.3%, P = 0.140), and survival time (760.47 ± 317.94 vs 686.89 ± 271.81 d, P = 0.115). The follow-up data showed that the robotic and open hepatectomy groups had no significant differences in the 1-year, 2-year, and 3-year disease-free survival (72.5%, 64.3%, 61.6% vs 77.8%, 71.9%, 71.9%, P = 0.325) and overall survival (95.4%, 92.3%, 92.3% vs 100%, 97.7%, 97.7%, P = 0.137). Regarding patients with hepatocellular carcinoma and negative resection margins, the follow-up study published by Chen et al[31] in 2017 evaluated patients with newly diagnosed hepatocellular carcinoma with negative margin (R0 resection) after undergoing robotic hepatectomy (n = 81) and open hepatectomy (n = 81) at a single center between January 2012 and October 2015. The results showed that the robotic and open hepatectomy groups had no significant differences in the 1-year, 2-year, and 3-year disease-free survival (91.5%, 84.3%, 72.2% vs 79.2%, 73.0%, 58%, P = 0.062) and overall survival (100%, 97.8%, 92.6% vs 100%, 98.4%, 92.6%, P = 0.431).
Recommendation 3: As a minimally invasive surgery, robotic hepatectomy is as safe and feasible as traditional laparoscopic hepatectomy. Robotic hepatectomy has longer operative time, more intraoperative blood loss, and higher cost. Robotic hepatectomy has similar overall complication rate and length of hospital stays compared to open hepatectomy. Conversion rate of robotic hepatectomy would decrease with the experience accumulation. Level of evidence: Very low. Level of recommendation: Weak (Grade 2D)
Data from the ACS NSQIP showed that between 2000 and 2011, robotic liver surgery accounted for 7.4% of all minimally invasive liver surgeries[70]. In 2010, Berber et al[56] from the Cleveland Clinic in the United States was the first to compare robotic hepatectomy (n = 9) and conventional laparoscopic hepatectomy (n = 23) at single center. The results showed that the two groups had no significant differences in operative time (259 ± 28 vs 234 ± 17 min, P = 0.6), intraoperative blood loss (136 ± 61 vs 155±54 mL), and resection margin (11±8 vs. 14 ± 10 mm). Guan et al[71] reported a meta-analysis of 13 retrospective, case-control studies on robotic and laparoscopic hepatectomy conducted between 2010 and 2017. The analysis evaluated the intraoperative and short-term outcome in 435 cases of robotic hepatectomy and 503 cases of conventional laparoscopic hepatectomy in Italy, China, France, the United States, Korea, Germany, and Belgium. The results showed that compared with conventional laparoscopic hepatectomy: (1) Intraoperative parameters indicated that robotic hepatectomy had a longer operative time (MD = 65.49 min; 95%CI: 42.00, 88.98) and increased intraoperative blood loss (MD = 69.88 mL; 95%CI: -27.11, 112.65), but there were no significant differences in blood transfusion rate [odds ratio (OR) = 0.96; 95%CI: 0.47, 1.97] and conversion rate (OR=0.75; 95%CI: 0.45, 1.25); (2) there were no statistically significant differences in the overall complication rate (OR = 0.80; 95%CI: 0.56, 1.14), major complication rate (Clavien-Dindo grade III or higher[67]) (OR = 1.0; 95%CI: 0.49, 2.06), R1 resection rate (OR = 1.03; 95%CI: 0.41, 2.55), and LOS (MD = 0.12 d; 95%CI: -0.52, 0.77); (3) the overall hospital cost of robotic hepatectomy was higher than that in the laparoscopic group (MD = 4.24, 95%CI: 3.08, 5.39); (4) subgroup analysis on robotic hepatectomy and conventional laparoscopic hepatectomy conducted after 2010 showed that the robotic group had a lower conversion rate (OR = 0.34; 95%CI: 0.13, 0.87), and there were no statistically significant differences in operative time and intraoperative blood loss.
The meta-analyses published by Qiu et al[72] and Montalti et al[73] had also drawn similar conclusions. In addition, the meta-analysis published by Hu et al[74] in 2018 that analyzed the efficacy of robotic surgery in liver tumors also obtained similar conclusions. The analysis also found that the robotic group had a longer postoperative fasting time (weighted MD = 1.2, 95%CI: 0.24, 2.17), but the two groups showed no significant difference postoperative mortality (OR = 0.67, 95%CI: 0.16, 2.83). Subgroup analyses in some studies had suggested that the robotic group may be superior to conventional laparoscopic surgery when used for major hepatectomy[46] or tumors localized in the superior and posterior segments[61]. In 2018, Marino et al[75] compared laparoscopic right hepatectomy (n = 20) and robotic right hepatectomy (n = 14) and found that the robotic group had shorter operative time than the laparoscopic group (425 ± 139 vs 565.18 ± 183.73 min, P = 0.022), whereas intraoperative blood loss, postoperative complications, LOS, and surgical costs were not significantly different between the groups.
Although the flexibility and the clarity and stability of the visual fields are more superior in the robotic laparoscopic surgical system than in conventional laparoscopic surgery, minimally-invasive hepatectomy is still currently predominated by conventional laparoscopy[17,18]. Studies have indicated that compared with conventional laparoscopic hepatectomy, robotic hepatectomy has a longer operative time, increased intraoperative blood loss, and a higher cost, whereas no significant differences are observed with regard to blood transfusion rate, R0 resection rate, LOS, overall complication rate, and severe complication rate between the two groups. With the accumulation of surgical experience, the conversion rate of the robotic group gradually decreases.
Recommendation 4: As minimally invasive surgery, robotic hepatectomy has similar effectiveness for liver malignancy disease compared to laparoscopic hepatectomy. Regarding the oncological outcome there is no significant difference in the radical resection rate, overall survival rate and recurrence rate between robotic hepatectomy and laparoscopic hepatectomy. Level of evidence: Very low. Level of recommendation: Weak (Grade 2D)
Khan et al[76] evaluated the long-term oncologic outcomes of patients undergoing robotic liver surgery (n = 61) for primary hepatobiliary malignancies between 2006 and 2016 and showed that the R0 resection rates of hepatocellular carcinoma, intrahepatic cholangiocarcinoma, and gallbladder carcinoma were 94%, 68%, and 81.8%, respectively. The median follow-up time was 75 mo (95%CI: 36,113), 5-year overall survival and disease-free survival were 56% and 38%, respectively, and the 3-year survival rates of hepatocellular carcinoma, intrahepatic cholangiocarcinoma, and gallbladder cancer were 94%, 65%, and 49%, respectively.
Hu et al[77] published a meta-analysis of 17 retrospective, case-control studies on robotic and laparoscopic hepatectomy conducted between 2010 and 2017. The analysis evaluated the intraoperative and short-term outcomes in 487 cases of robotic hepatectomy and 902 cases of conventional laparoscopic hepatectomy in Italy, China, France, the United States, Korea, Germany, and Belgium. The results showed that compared with conventional laparoscopic hepatectomy, there was no significant difference in R0 resection rate (OR = 2.20, 95%CI: 0.78, 6.23) and R1 resection rate (OR = 1.10, 95%CI: 0.45, 2.73) between two groups. The meta-analyses published by Qiu et al[72], Guan et al[71] and Montalti et al[73] had also drawn similar conclusion. As there are few comparative studies on long-term prognosis, there is no meta-analysis report on the long-term prognosis of robotic hepatectomy and laparoscopic hepatectomy. Lai et al[39] reported a single-center study evaluating the long-term prognosis of patients with liver cancer treated with robotic hepatectomy (n = 100) and conventional laparoscopic hepatectomy (n = 35) and found that compared with conventional laparoscopic surgery, the robotic hepatectomy for liver cancer had no statistically significant differences in R0 resection rate (96% vs 91.4%, P = 0.72), 5-year overall survival (65% vs 48%, P = 0.28), and 5-year disease-free survival (42% vs 38%, P = 0.65). The report from Troisi[49] evaluated the long-term prognosis of patients with colorectal cancer liver metastases who underwent robotic hepatectomy (n = 24) and conventional laparoscopic hepatectomy (n = 108), and the results showed that the 1-year and 3-year disease-free survival rates were 79% and 62% in the robotic group and 81% and 41% in the open hepatectomy group.
Recommendation 5: For minor hepatectomy, robotic hepatectomy as safe and feasible as laparoscopic hepatectomy and open hepatectomy. Robotic hepatectomy has longer operative time than laparoscopic hepatectomy for minor hepatectomy. The intraoperative blood loss, overall postoperative complication rate and overall cost of robotic minor hepatectomy are comparable to that of laparoscopic minor hepatectomy. Level of evidence: Very low. Level of recommendation: Weak (Grade 2D)
Based on the published articles, the minimally-invasive hepatectomy is mainly used in minor hepatectomy, which includes resections of the left lateral lobes and local liver lesions. Tsilimigras et al[27] systematically reviewed 31 comparative studies between 2008 and 2017 that included a total of 1148 patients and found that robotic minor hepatectomy accounted for 72.7% of all robotic hepatectomy cases, with a mean operative time of 242.2 ± 89 min, intraoperative blood loss of 317.1 ± 331 mL, conversion rate of 8.1%, mean postoperative hospital stay of 6.1 ± 2.9 d, and incidence of postoperative complications of 14.8%. The meta-analysis published by Guan et al[71] included 5 retrospective, case-control studies on robotic and laparoscopic liver surgeries conducted between 2010 and 2017, including 95 cases of robotic minor hepatectomy and 163 cases of conventional laparoscopic minor hepatectomy. The evaluation of intraoperative and short-term postoperative outcomes showed that compared with conventional laparoscopic minor hepatectomy, robotic minor hepatectomy had a longer operative time (MD = 50.29 min; 95%CI: 10.52, 90.05), but there were no significant differences in perioperative outcomes such as intraoperative blood loss and complications. Laparoscopic hepatectomy is currently recommended for left lateral segmentectomy[78]. Salloum et al[79] published a single-center study comparing robotic left lateral segmentectomy (n = 16) and laparoscopic left lateral segmentectomy (n = 80) and showed that the 2 groups had no statistically significant differences in operative time (190 vs 162 min, P = 0.10), intraoperative blood loss (247±239 vs 206 ± 205 mL, P =0.50), overall complication rate (12% vs 11%, P = 0.77), LOS (7 ± 8 vs 6 ± 4 d, P = 0.74), and total cost (5522€ vs 6035€, P = 0.70).
Recommendation 6: For major hepatectomy, robotic hepatectomy as safe and feasible as laparoscopic hepatectomy and open hepatectomy. Robotic hepatectomy has longer operative time than laparoscopic hepatectomy for major hepatectomy. The intraoperative blood loss, overall postoperative complication rate and overall cost of robotic major hepatectomy are comparable to that of laparoscopic major hepatectomy. There is no significant difference in the operative time, intraoperative blood loss and complication rate between robotic hepatectomy and open hepatectomy for minor hepatectomy. Level of evidence: Very low. Level of recommendation: Weak (Grade 2D)
Nguyen et al[64] reviewed the current status of laparoscopic hepatectomy in 127 studies worldwide. Based on the definition of major hepatectomy stated in the Fukuoka Declaration[78], they found that major hepatectomy accounted for 17.3% of all laparoscopic hepatectomy cases. In view of the disadvantages of conventional laparoscopy such as limited flexibility, fulcrum effect, and poor visual field stability, it is believed that robotic hepatectomy may compensate the limitations of conventional laparoscopic surgery in major hepatectomy, such as hemi-hepatectomy and extended hepatectomy, which require precise dissection of the porta hepatis[80]. Tsilimigras et al[27] systematically reviewed 31 comparative studies between 2008 and 2017 and found that robotic major hepatectomy (n = 115) accounted for 27.3% of all robotic hepatectomy cases, with a mean operative time of 403.4 ± 107.5 min, intraoperative blood loss of 543.4 ± 371 mL, conversion rate of 8.6%, mean LOS of 10.5 ± 4.8 d, and complication rate of 17%.
Giulianotti et al[81] reviewed 24 cases of right hepatectomy conducted by a single surgical team between 2005 and 2010. The results showed that the mean operative time was 337 min, mean intraoperative blood loss was 457 mL, blood transfusion rate was 12.5%, conversion rate was approximately 4.2%, and incidence rate of postoperative complications was 25%. No perioperative mortality occurred, and the perioperative outcome was similar to that of laparoscopic hepatectomy conducted during the same period. Spampinato et al[48] compared robotic hemi-hepatectomy (n = 25) and laparoscopic hemi-hepatectomy (n = 25) in their study, which conducted in 2 centers in Italy and Belgium between 2009 and 2012. The results showed that the 2 groups had no statistically significant differences in operative time (430 vs 360 min, P = 0.070), intraoperative blood loss (250 vs 400 mL, P = 0.95), conversion rate (4% vs 4%, P =1), overall complication rate (16% vs 36%, P = 0.2), R0 resection rate in malignant tumors (100% vs 91%, P = 0.49), and LOS (8 vs 7 d, P = 0.48). According to the definitions of minimally-invasive major hepatectomy in the Fukuoka Declaration[78] and Louisville Declaration[4], when considering the difficulty of the surgery, resections of lesions in the superior posterior segments of the liver should also be classified as major hepatectomy. Patriti et al[44] compared the efficacy of robotic hepatectomy (n = 19) and open hepatectomy for the resection of liver segments 6 and 7 in 2 centers in Italy. Compared with open hepatectomy, robotic hepatectomy had a longer operative time (303 ± 132.3 vs 233.9 ± 81 min, P = 0.002). There were no statistically significant differences with regard to the volume of intraoperative blood loss (376.3 ± 410 vs 457.5 ± 365.5 mL, P = 0.40), overall complication rate (15.8% vs 13%, P = 0.70), severe complications rate (5.3% vs 1.4%, P = 0.80), and LOS (6.7 ± 3 vs 7.9 ± 4.4 d, P = 0.60).
Recommendation 7: Robotic liver donor hepatectomy could be an alternative. The procedure should only be performed by experienced surgeons, and the true benefits of robotic donor hepatectomy need further investigation in the future. Level of evidence: Very low. Level of recommendation: Weak (Grade 2D)
In 2012, Giulianotti et al[16] reported for the first robotic living-donor hepatectomy of the right inferior lobe. Compared with conventional laparoscopic surgery, the robotic surgical system provided a magnified and stable 3D field of vision with higher accuracy in intraoperative suture during the living-donor hepatectomy[82]. At present, countries such as Italy, South Korea, China, and India have carried out robotic living-donor hepatectomy, but no report has been published on robotic liver transplantation[6,16,83-86].
The only comparative study on robotic living-donor hepatectomy and standard open living-donor hepatectomy was published by Chen et al[83], which was a retrospective, case-control study on 13 cases of robotic hepatectomy and 54 cases of open hepatectomy conducted at a single center between May 2013 and August 2015. The results showed that the robotic group had a longer operative time (596 vs 383 min, P < 0.001), reduced dosage of postoperative analgesics (0.58 vs 0.84 ng/kg, P = 0.03), and a higher postoperative cost (13436$ vs 5019.1$, P < 0.001), but there were no significant differences in intraoperative blood loss, LOS, and overall complications. No open conversion was required in the robotic group. Even though robotic living-donor hepatectomy is considered safe and feasible based on published case and case series reports and comparative studies, it does not show significant superiority in therapeutic efficacy compared with open and conventional laparoscopic approaches. Although robotic living-donor hepatectomy is technically safe and feasible, critics have pointed out that minimally-invasive surgery for living-donor hepatectomy cannot be truly considered as “minimally-invasive surgery”, as it merely moves the midline incision to the lower abdomen at the cost of increasing 3 to 5 small incisions for port sites. Therefore, it should be considered as “minimal incision surgery”[59]. Furthermore, the complex anatomy of the liver, together with the absence of inflow control and the need for a short ischemic time, may result in a higher risk for both donor and graft safety[60].
ACKNOWLEDGEMENTS
We thank all the external reviewers for giving responses to the consensus; and all Members of the Consensus Secretary Group: Guo-Dong Zhao, Sai Chou, Zi-Zeng Wang, Kong-Yuan Wei, Wen-Bo Tang.
Footnotes
Conflict-of-interest statement: The authors declare no conflict of interest in the development of consensus.
Manuscript source: Unsolicited manuscript
Peer-review started: February 1, 2019
First decision: February 13, 2019
Article in press: March 12, 2019
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report classification
Grade A (Excellent): A, A
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Apisarnthanarax S, Goldaracena N, Snowdon VK, Ward J S-Editor: Yan JP L-Editor: A E-Editor: Song H
Contributor Information
Rong Liu, Second Department of Hepatopancreatobiliary Surgery, Chinese People’s Liberation Army (PLA) General Hospital, Beijing 100853, China. liurong@301hospital.com.cn.
Go Wakabayashi, Center for Advanced Treatment of Hepatobiliary and Pancreatic Diseases, Ageo Central General Hospital, Ageo 362-8588, Japan.
Hong-Jin Kim, Department of Surgery, Yeungnam University Hospital, Daegu 705-703, South Korea.
Gi-Hong Choi, Division of Hepatobiliary Pancreatic Surgery, Department of Surgery, Yonsei University College of Medicine, Seoul 03722, South Korea.
Anusak Yiengpruksawan, Minimally Invasive Surgery Division, Department of Surgery, Faculty of Medicine, Siriraj Hospital, Mahidol University, Bangkok 10700, Thailand.
Yuman Fong, Department of Surgery, City of Hope Medical Center, Duarte, CA 91010, United States.
Jin He, Department of Surgery, the Johns Hopkins Hospital, Baltimore, MD 21287, United States.
Ugo Boggi, Division of General and Transplant Surgery, Pisa University Hospital, Pisa 56124, Italy.
Roberto I Troisi, Department of Clinical Medicine and Surgery, Federico II University, Naples 80131, Italy.
Mikhail Efanov, Department of Hepato-Pancreato-Biliary Surgery, Moscow Clinical Scientific Center, Moscow 11123, Russia.
Daniel Azoulay, Hepato-Biliary Center, Paul Brousse University Hospital, Villejuif 94000, France; Hepato-Biliary Center, Tel Hashomer University Hospital, Tel Aviv, Israel.
Fabrizio Panaro, Department of Surgery/Division of HBP Surgery and Transplantation, Montpellier University Hospital—School of Medicine, Montpellier 34000, France.
Patrick Pessaux, Head of the Hepato-biliary and pancreatic surgical unit, Nouvel Hôpital Civil, Strasbourg Cedex 67091, France.
Xiao-Ying Wang, Department of Liver Surgery and Transplantation, Liver Cancer Institute, Zhongshan Hospital, Fudan University, Shanghai 200032, China.
Ji-Ye Zhu, Department of Hepatobiliary Surgery, Peking University People’s Hospital, Beijing 100044, China.
Shao-Geng Zhang, Department of Hepatobiliary Surgery, 302 Hospital of Chinese PLA, Beijing 100039, China.
Chuan-Dong Sun, Department of Hepatobiliary and Pancreatic Surgery, the Affiliated Hospital of Qingdao University, Qingdao 266071, Shandong Province, China.
Zheng Wu, Department of Hepatobiliary Surgery, the First Affiliated Hospital of Xi’an Jiaotong University, Xi’an 710061, Shaanxi Province, China.
Kai-Shan Tao, Department of Hepatobiliary Surgery, Xijing Hospital, the Fourth Military Medical University, Xi’an 710032, Shaanxi Province, China.
Ke-Hu Yang, Evidence Based Medicine Center, School of Basic Medical Sciences, Lanzhou University, Lanzhou 730000, Gansu Province, China.
Jia Fan, Department of Liver Surgery and Transplantation, Liver Cancer Institute, Zhongshan Hospital, Fudan University, Shanghai 200032, China.
Xiao-Ping Chen, Hepatic Surgery Center, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan 430030, Hubei Province, China.
References
- 1.Litynski GS. Profiles in laparoscopy: Mouret, Dubois, and Perissat: The laparoscopic breakthrough in Europe (1987-1988) JSLS. 1999;3:163–167. [PMC free article] [PubMed] [Google Scholar]
- 2.Reich H, McGlynn F, DeCaprio J, Budin R. Laparoscopic excision of benign liver lesions. Obstet Gynecol. 1991;78:956–958. [PubMed] [Google Scholar]
- 3.Katkhouda N, Fabiani P, Benizri E, Mouiel J. Laser resection of a liver hydatid cyst under videolaparoscopy. Br J Surg. 1992;79:560–561. doi: 10.1002/bjs.1800790628. [DOI] [PubMed] [Google Scholar]
- 4.Buell JF, Cherqui D, Geller DA, O'Rourke N, Iannitti D, Dagher I, Koffron AJ, Thomas M, Gayet B, Han HS, Wakabayashi G, Belli G, Kaneko H, Ker CG, Scatton O, Laurent A, Abdalla EK, Chaudhury P, Dutson E, Gamblin C, D’Angelica M, Nagorney D, Testa G, Labow D, Manas D, Poon RT, Nelson H, Martin R, Clary B, Pinson WC, Martinie J, Vauthey JN, Goldstein R, Roayaie S, Barlet D, Espat J, Abecassis M, Rees M, Fong Y, McMasters KM, Broelsch C, Busuttil R, Belghiti J, Strasberg S, Chari RS World Consensus Conference on Laparoscopic Surgery. The international position on laparoscopic liver surgery: The Louisville Statement, 2008. Ann Surg. 2009;250:825–830. doi: 10.1097/sla.0b013e3181b3b2d8. [DOI] [PubMed] [Google Scholar]
- 5.Himpens J, Leman G, Cadiere GB. Telesurgical laparoscopic cholecystectomy. Surg Endosc. 1998;12:1091. doi: 10.1007/s004649900788. [DOI] [PubMed] [Google Scholar]
- 6.Choi GH, Chong JU, Han DH, Choi JS, Lee WJ. Robotic hepatectomy: The Korean experience and perspective. Hepatobiliary Surg Nutr. 2017;6:230–238. doi: 10.21037/hbsn.2017.01.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schraibman V, de Vasconcellos Macedo AL, Okazaki S, Mauro FC, Epstein MG, Goldman SM, Lustosa S, Matos D. Surgical treatment of hiatus hernia and gastroesophageal reflux disease in complex cases using robotic-assisted laparoscopic surgery: A prospective study/consistent experience in a single institution. J Robot Surg. 2011;5:29–33. doi: 10.1007/s11701-010-0235-6. [DOI] [PubMed] [Google Scholar]
- 8.Efanov M, Alikhanov R, Cvircun V, Kazakov L, Melekhina O, Kim P, Vankovich A, Khatkov L. Radical Robot-Assisted Liver Resection for Alveolar Echinococcosis. CRSLS. 2015:e2015.00021. [Google Scholar]
- 9.Goja S, Singh MK, Vohra V, Soin AS. Robotic Left Hepatectomy: A Case Report (First Reported Case of Robotic Hepatectomy in India) Indian J Surg. 2015;77:338–340. doi: 10.1007/s12262-015-1307-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Giulianotti PC, Coratti A, Angelini M, Sbrana F, Cecconi S, Balestracci T, Caravaglios G. Robotics in general surgery: Personal experience in a large community hospital. Arch Surg. 2003;138:777–784. doi: 10.1001/archsurg.138.7.777. [DOI] [PubMed] [Google Scholar]
- 11.Kam JH, Goh BK, Chan CY, Wong JS, Lee SY, Cheow PC, Chung AY, Ooi LL. Robotic hepatectomy: Initial experience of a single institution in Singapore. Singapore Med J. 2016;57:209–214. doi: 10.11622/smedj.2016024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Choi SB, Park JS, Kim JK, Hyung WJ, Kim KS, Yoon DS, Lee WJ, Kim BR. Early experiences of robotic-assisted laparoscopic liver resection. Yonsei Med J. 2008;49:632–638. doi: 10.3349/ymj.2008.49.4.632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Croner RS, Perrakis A, Brunner M, Matzel KE, Hohenberger W. Pioneering Robotic Liver Surgery in Germany: First Experiences with Liver Malignancies. Front Surg. 2015;2:18. doi: 10.3389/fsurg.2015.00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Quijano Y, Vicente E, Ielpo B, Duran H, Diaz E, Fabra I, Malave L, Ferri V, Plaza C, Lindemann JL, D'Andrea V, Caruso R. Hepatobilio-pancreatic robotic surgery: Initial experience from a single center institute. J Robot Surg. 2017;11:355–365. doi: 10.1007/s11701-016-0663-z. [DOI] [PubMed] [Google Scholar]
- 15.Vicente E, Quijano Y, Ielpo B, Fabra I. First ALPPS procedure using a total robotic approach. Surg Oncol. 2016;25:457. doi: 10.1016/j.suronc.2015.10.001. [DOI] [PubMed] [Google Scholar]
- 16.Giulianotti PC, Tzvetanov I, Jeon H, Bianco F, Spaggiari M, Oberholzer J, Benedetti E. Robot-assisted right lobe donor hepatectomy. Transpl Int. 2012;25:e5–e9. doi: 10.1111/j.1432-2277.2011.01373.x. [DOI] [PubMed] [Google Scholar]
- 17.Stiles ZE, Behrman SW, Glazer ES, Deneve JL, Dong L, Wan JY, Dickson PV. Predictors and implications of unplanned conversion during minimally invasive hepatectomy: An analysis of the ACS-NSQIP database. HPB (Oxford) 2017;19:957–965. doi: 10.1016/j.hpb.2017.06.012. [DOI] [PubMed] [Google Scholar]
- 18.Aldrighetti L, Belli G, Boni L, Cillo U, Ettorre G, De Carlis L, Pinna A, Casciola L, Calise F Italian Group of Minimally Invasive Liver Surgery (I GO MILS) Italian experience in minimally invasive liver surgery: A national survey. Updates Surg. 2015;67:129–140. doi: 10.1007/s13304-015-0307-2. [DOI] [PubMed] [Google Scholar]
- 19.King JC, Zeh HJ, 3rd, Zureikat AH, Celebrezze J, Holtzman MP, Stang ML, Tsung A, Bartlett DL, Hogg ME. Safety in Numbers: Progressive Implementation of a Robotics Program in an Academic Surgical Oncology Practice. Surg Innov. 2016;23:407–414. doi: 10.1177/1553350616646479. [DOI] [PubMed] [Google Scholar]
- 20.Buchs NC, Addeo P, Bianco FM, Gorodner V, Ayloo SM, Elli EF, Oberholzer J, Benedetti E, Giulianotti PC. Perioperative risk assessment in robotic general surgery: Lessons learned from 884 cases at a single institution. Arch Surg. 2012;147:701–708. doi: 10.1001/archsurg.2012.496. [DOI] [PubMed] [Google Scholar]
- 21.Wu CY, Chen PD, Lee CY, Liang JT, Wu YM. Robotic-assisted right posterior segmentectomies for liver lesions: Single-center experience of an evolutional method in left semi-lateral position. J Robot Surg. 2019;13:231–237. doi: 10.1007/s11701-018-0842-1. [DOI] [PubMed] [Google Scholar]
- 22.Marino MV, Gulotta G, Komorowski AL. Fully robotic left hepatectomy for malignant tumor: Technique and initial results. Updates Surg. 2018 doi: 10.1007/s13304-018-0560-2. [DOI] [PubMed] [Google Scholar]
- 23.Wong DJ, Wong MJ, Choi GH, Wu YM, Lai PB, Goh BKP. Systematic review and meta-analysis of robotic versus open hepatectomy. ANZ J Surg. 2019;89:165–170. doi: 10.1111/ans.14690. [DOI] [PubMed] [Google Scholar]
- 24.Goh BKP, Lee LS, Lee SY, Chow PKH, Chan CY, Chiow AKH. Initial experience with robotic hepatectomy in Singapore: Analysis of 48 resections in 43 consecutive patients. ANZ J Surg. 2019;89:201–205. doi: 10.1111/ans.14417. [DOI] [PubMed] [Google Scholar]
- 25.Pesi B, Moraldi L, Bartolini I, Tofani F, Guerra F, Annecchiarico M, Coratti A. Pringle maneuver in robotic liver surgery: Preliminary study. Minerva Chir. 2018;73:482–487. doi: 10.23736/S0026-4733.18.07599-5. [DOI] [PubMed] [Google Scholar]
- 26.Alfano MS, Molfino S, Benedicenti S, Molteni B, Porsio P, Arici E, Gheza F, Botticini M, Portolani N, Baiocchi GL. Intraoperative ICG-based imaging of liver neoplasms: A simple yet powerful tool. Preliminary results. Surg Endosc. 2019;33:126–134. doi: 10.1007/s00464-018-6282-1. [DOI] [PubMed] [Google Scholar]
- 27.Tsilimigras DI, Moris D, Vagios S, Merath K, Pawlik TM. Safety and oncologic outcomes of robotic liver resections: A systematic review. J Surg Oncol. 2018;117:1517–1530. doi: 10.1002/jso.25018. [DOI] [PubMed] [Google Scholar]
- 28.Chen JC, Huang CY, Wang JC, Zhang YJ, Xu L, Chen MS, Zhou ZG. Robot-assisted laparoscopic partial hepatic caudate lobectomy. Minim Invasive Ther Allied Technol. 2018;27:1–6. doi: 10.1080/13645706.2018.1521434. [DOI] [PubMed] [Google Scholar]
- 29.O’Connor VV, Vuong B, Yang ST, DiFronzo A. Robotic Minor Hepatectomy Offers a Favorable Learning Curve and May Result in Superior Perioperative Outcomes Compared with Laparoscopic Approach. Am Surg. 2017;83:1085–1088. [PubMed] [Google Scholar]
- 30.Morel P, Jung M, Cornateanu S, Buehler L, Majno P, Toso C, Buchs NC, Rubbia-Brandt L, Hagen ME. Robotic versus open liver resections: A case-matched comparison. Int J Med Robot. 2017:13. doi: 10.1002/rcs.1800. [DOI] [PubMed] [Google Scholar]
- 31.Chen PD, Wu CY, Hu RH, Chou WH, Lai HS, Liang JT, Lee PH, Wu YM. Robotic Versus Open Hepatectomy for Hepatocellular Carcinoma: A Matched Comparison. Ann Surg Oncol. 2017;24:1021–1028. doi: 10.1245/s10434-016-5638-9. [DOI] [PubMed] [Google Scholar]
- 32.Daskalaki D, Gonzalez-Heredia R, Brown M, Bianco FM, Tzvetanov I, Davis M, Kim J, Benedetti E, Giulianotti PC. Financial Impact of the Robotic Approach in Liver Surgery: A Comparative Study of Clinical Outcomes and Costs Between the Robotic and Open Technique in a Single Institution. J Laparoendosc Adv Surg Tech A. 2017;27:375–382. doi: 10.1089/lap.2016.0576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chen PD, Wu CY, Hu RH, Chen CN, Yuan RH, Liang JT, Lai HS, Wu YM. Robotic major hepatectomy: Is there a learning curve? Surgery. 2017;161:642–649. doi: 10.1016/j.surg.2016.09.025. [DOI] [PubMed] [Google Scholar]
- 34.Salloum C, Lim C, Lahat E, Gavara CG, Levesque E, Compagnon P, Azoulay D. Robotic-Assisted Versus Laparoscopic Left Lateral Sectionectomy: Analysis of Surgical Outcomes and Costs by a Propensity Score Matched Cohort Study. World J Surg. 2017;41:516–524. doi: 10.1007/s00268-016-3736-2. [DOI] [PubMed] [Google Scholar]
- 35.Lee KF, Fong AK, Chong CC, Cheung SY, Wong J, Lai PB. Robotic Liver Resection For Primary Hepatolithiasis: Is It Beneficial? World J Surg. 2016;40:2490–2496. doi: 10.1007/s00268-016-3528-8. [DOI] [PubMed] [Google Scholar]
- 36.Kingham TP, Leung U, Kuk D, Gönen M, D'Angelica MI, Allen PJ, DeMatteo RP, Laudone VP, Jarnagin WR, Fong Y. Robotic Liver Resection: A Case-Matched Comparison. World J Surg. 2016;40:1422–1428. doi: 10.1007/s00268-016-3446-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Montalti R, Scuderi V, Patriti A, Vivarelli M, Troisi RI. Robotic versus laparoscopic resections of posterosuperior segments of the liver: A propensity score-matched comparison. Surg Endosc. 2016;30:1004–1013. doi: 10.1007/s00464-015-4284-9. [DOI] [PubMed] [Google Scholar]
- 38.Lee KF, Cheung YS, Chong CC, Wong J, Fong AK, Lai PB. Laparoscopic and robotic hepatectomy: Experience from a single centre. ANZ J Surg. 2016;86:122–126. doi: 10.1111/ans.13339. [DOI] [PubMed] [Google Scholar]
- 39.Lai EC, Tang CN. Long-term Survival Analysis of Robotic Versus Conventional Laparoscopic Hepatectomy for Hepatocellular Carcinoma: A Comparative Study. Surg Laparosc Endosc Percutan Tech. 2016;26:162–166. doi: 10.1097/SLE.0000000000000254. [DOI] [PubMed] [Google Scholar]
- 40.Boggi U, Caniglia F, Vistoli F, Costa F, Pieroni E, Perrone VG. Laparoscopic robot-assisted resection of tumors located in posterosuperior liver segments. Updates Surg. 2015;67:177–183. doi: 10.1007/s13304-015-0304-5. [DOI] [PubMed] [Google Scholar]
- 41.Felli E, Santoro R, Colasanti M, Vennarecci G, Lepiane P, Ettorre GM. Robotic liver surgery: Preliminary experience in a tertiary hepato-biliary unit. Updates Surg. 2015;67:27–32. doi: 10.1007/s13304-015-0285-4. [DOI] [PubMed] [Google Scholar]
- 42.Jackson NR, Hauch A, Hu T, Buell JF, Slakey DP, Kandil E. The safety and efficacy of approaches to liver resection: A meta-analysis. JSLS. 2015;19:e2014.00186. doi: 10.4293/JSLS.2014.00186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kim SR, Kim KH. Robotic liver resection: A single surgeon's experience. Hepatogastroenterology. 2014;61:2062–2067. [PubMed] [Google Scholar]
- 44.Patriti A, Cipriani F, Ratti F, Bartoli A, Ceccarelli G, Casciola L, Aldrighetti L. Robot-assisted versus open liver resection in the right posterior section. JSLS. 2014;18:pii: e2014.00040. doi: 10.4293/JSLS.2014.00040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wu YM, Hu RH, Lai HS, Lee PH. Robotic-assisted minimally invasive liver resection. Asian J Surg. 2014;37:53–57. doi: 10.1016/j.asjsur.2014.01.015. [DOI] [PubMed] [Google Scholar]
- 46.Tsung A, Geller DA, Sukato DC, Sabbaghian S, Tohme S, Steel J, Marsh W, Reddy SK, Bartlett DL. Robotic versus laparoscopic hepatectomy: A matched comparison. Ann Surg. 2014;259:549–555. doi: 10.1097/SLA.0000000000000250. [DOI] [PubMed] [Google Scholar]
- 47.Yu YD, Kim KH, Jung DH, Namkoong JM, Yoon SY, Jung SW, Lee SK, Lee SG. Robotic versus laparoscopic liver resection: A comparative study from a single center. Langenbecks Arch Surg. 2014;399:1039–1045. doi: 10.1007/s00423-014-1238-y. [DOI] [PubMed] [Google Scholar]
- 48.Spampinato MG, Coratti A, Bianco L, Caniglia F, Laurenzi A, Puleo F, Ettorre GM, Boggi U. Perioperative outcomes of laparoscopic and robot-assisted major hepatectomies: An Italian multi-institutional comparative study. Surg Endosc. 2014;28:2973–2979. doi: 10.1007/s00464-014-3560-4. [DOI] [PubMed] [Google Scholar]
- 49.Troisi RI, Patriti A, Montalti R, Casciola L. Robot assistance in liver surgery: A real advantage over a fully laparoscopic approach? Results of a comparative bi-institutional analysis. Int J Med Robot. 2013;9:160–166. doi: 10.1002/rcs.1495. [DOI] [PubMed] [Google Scholar]
- 50.Kandil E, Noureldine SI, Saggi B, Buell JF. Robotic liver resection: Initial experience with three-arm robotic and single-port robotic technique. JSLS. 2013;17:56–62. doi: 10.4293/108680812X13517013317671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Packiam V, Bartlett DL, Tohme S, Reddy S, Marsh JW, Geller DA, Tsung A. Minimally invasive liver resection: Robotic versus laparoscopic left lateral sectionectomy. J Gastrointest Surg. 2012;16:2233–2238. doi: 10.1007/s11605-012-2040-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Patriti A, Ceribelli C, Ceccarelli G, Bartoli A, Bellochi R, Casciola L. Non-cirrhotic liver tolerance to intermittent inflow occlusion during laparoscopic liver resection. Updates Surg. 2012;64:87–93. doi: 10.1007/s13304-012-0144-5. [DOI] [PubMed] [Google Scholar]
- 53.Lai EC, Tang CN, Li MK. Robot-assisted laparoscopic hemi-hepatectomy: Technique and surgical outcomes. Int J Surg. 2012;10:11–15. doi: 10.1016/j.ijsu.2011.10.005. [DOI] [PubMed] [Google Scholar]
- 54.Lai EC, Tang CN, Yang GP, Li MK. Multimodality laparoscopic liver resection for hepatic malignancy--from conventional total laparoscopic approach to robot-assisted laparoscopic approach. Int J Surg. 2011;9:324–328. doi: 10.1016/j.ijsu.2011.02.004. [DOI] [PubMed] [Google Scholar]
- 55.Giulianotti PC, Coratti A, Sbrana F, Addeo P, Bianco FM, Buchs NC, Annechiarico M, Benedetti E. Robotic liver surgery: Results for 70 resections. Surgery. 2011;149:29–39. doi: 10.1016/j.surg.2010.04.002. [DOI] [PubMed] [Google Scholar]
- 56.Berber E, Akyildiz HY, Aucejo F, Gunasekaran G, Chalikonda S, Fung J. Robotic versus laparoscopic resection of liver tumours. HPB (Oxford) 2010;12:583–586. doi: 10.1111/j.1477-2574.2010.00234.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Di Benedetto F, Magistri P, Halazun KJ. Use of robotics in liver donor right hepatectomy. Hepatobiliary Surg Nutr. 2018;7:231–232. doi: 10.21037/hbsn.2018.03.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Cooper M. Just because you can doesn't mean you should...because many of us really can't! Arch Surg. 2011;146:850. doi: 10.1001/archsurg.2011.130. [DOI] [PubMed] [Google Scholar]
- 59.Kim SH, Lee SD, Kim YK, Park SJ. Pushing the frontiers of living donor right hepatectomy. World J Gastroenterol. 2014;20:18061–18069. doi: 10.3748/wjg.v20.i48.18061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Magistri P, Tarantino G, Ballarin R, Coratti A, Di Benedetto F. Robotic liver donor right hepatectomy: A pure, minimally invasive approach. Liver Transpl. 2017;23:857–858. doi: 10.1002/lt.24767. [DOI] [PubMed] [Google Scholar]
- 61.Tranchart H, Ceribelli C, Ferretti S, Dagher I, Patriti A. Traditional versus robot-assisted full laparoscopic liver resection: A matched-pair comparative study. World J Surg. 2014;38:2904–2909. doi: 10.1007/s00268-014-2679-8. [DOI] [PubMed] [Google Scholar]
- 62.Krawczyk M. Modern surgeons: Still a Master of His Trade or Just an Operator of Medical Equipment? Ann Surg. 2017;266:703–705. doi: 10.1097/SLA.0000000000002364. [DOI] [PubMed] [Google Scholar]
- 63.Ban D, Tanabe M, Ito H, Otsuka Y, Nitta H, Abe Y, Hasegawa Y, Katagiri T, Takagi C, Itano O, Kaneko H, Wakabayashi G. A novel difficulty scoring system for laparoscopic liver resection. J Hepatobiliary Pancreat Sci. 2014;21:745–753. doi: 10.1002/jhbp.166. [DOI] [PubMed] [Google Scholar]
- 64.Nguyen KT, Gamblin TC, Geller DA. World review of laparoscopic liver resection-2,804 patients. Ann Surg. 2009;250:831–841. doi: 10.1097/SLA.0b013e3181b0c4df. [DOI] [PubMed] [Google Scholar]
- 65.Sham JG, Richards MK, Seo YD, Pillarisetty VG, Yeung RS, Park JO. Efficacy and cost of robotic hepatectomy: Is the robot cost-prohibitive? J Robot Surg. 2016;10:307–313. doi: 10.1007/s11701-016-0598-4. [DOI] [PubMed] [Google Scholar]
- 66.Wang WH, Kuo KK, Wang SN, Lee KT. Oncological and surgical result of hepatoma after robot surgery. Surg Endosc. 2018;32:3918–3924. doi: 10.1007/s00464-018-6131-2. [DOI] [PubMed] [Google Scholar]
- 67.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Xu Y, Wang H, Ji W, Tang M, Li H, Leng J, Meng X, Dong J. Robotic radical resection for hilar cholangiocarcinoma: Perioperative and long-term outcomes of an initial series. Surg Endosc. 2016;30:3060–3070. doi: 10.1007/s00464-016-4925-7. [DOI] [PubMed] [Google Scholar]
- 69.Lai EC, Yang GP, Tang CN. Robot-assisted laparoscopic liver resection for hepatocellular carcinoma: Short-term outcome. Am J Surg. 2013;205:697–702. doi: 10.1016/j.amjsurg.2012.08.015. [DOI] [PubMed] [Google Scholar]
- 70.Ejaz A, Sachs T, He J, Spolverato G, Hirose K, Ahuja N, Wolfgang CL, Makary MA, Weiss M, Pawlik TM. A comparison of open and minimally invasive surgery for hepatic and pancreatic resections using the Nationwide Inpatient Sample. Surgery. 2014;156:538–547. doi: 10.1016/j.surg.2014.03.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Guan R, Chen Y, Yang K, Ma D, Gong X, Shen B, Peng C. Clinical efficacy of robot-assisted versus laparoscopic liver resection: A meta analysis. Asian J Surg. 2019;42:19–31. doi: 10.1016/j.asjsur.2018.05.008. [DOI] [PubMed] [Google Scholar]
- 72.Qiu J, Chen S, Chengyou D. A systematic review of robotic-assisted liver resection and meta-analysis of robotic versus laparoscopic hepatectomy for hepatic neoplasms. Surg Endosc. 2016;30:862–875. doi: 10.1007/s00464-015-4306-7. [DOI] [PubMed] [Google Scholar]
- 73.Montalti R, Berardi G, Patriti A, Vivarelli M, Troisi RI. Outcomes of robotic vs laparoscopic hepatectomy: A systematic review and meta-analysis. World J Gastroenterol. 2015;21:8441–8451. doi: 10.3748/wjg.v21.i27.8441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hu HJ, Wu ZR, Jin YW, Ma WJ, Yang Q, Wang JK, Liu F, Li FY. Minimally invasive surgery for hilar cholangiocarcinoma: State of art and future perspectives. ANZ J Surg. 2018 doi: 10.1111/ans.14765. [DOI] [PubMed] [Google Scholar]
- 75.Marino MV, Shabat G, Guarrasi D, Gulotta G, Komorowski AL. Comparative Study of the Initial Experience in Performing Robotic and Laparoscopic Right Hepatectomy with Technical Description of the Robotic Technique. Dig Surg. 2018 doi: 10.1159/000487686. [DOI] [PubMed] [Google Scholar]
- 76.Khan S, Beard RE, Kingham PT, Fong Y, Boerner T, Martinie JB, Vrochides D, Buell JF, Berber E, Kahramangil B, Troisi RI, Vanlander A, Molinari M, Tsung A. Long-Term Oncologic Outcomes Following Robotic Liver Resections for Primary Hepatobiliary Malignancies: A Multicenter Study. Ann Surg Oncol. 2018;25:2652–2660. doi: 10.1245/s10434-018-6629-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Hu L, Yao L, Li X, Jin P, Yang K, Guo T. Effectiveness and safety of robotic-assisted versus laparoscopic hepatectomy for liver neoplasms: A meta-analysis of retrospective studies. Asian J Surg. 2018;41:401–416. doi: 10.1016/j.asjsur.2017.07.001. [DOI] [PubMed] [Google Scholar]
- 78.Wakabayashi G, Cherqui D, Geller DA, Buell JF, Kaneko H, Han HS, Asbun H, OʼRourke N, Tanabe M, Koffron AJ, Tsung A, Soubrane O, Machado MA, Gayet B, Troisi RI, Pessaux P, Van Dam RM, Scatton O, Abu Hilal M, Belli G, Kwon CH, Edwin B, Choi GH, Aldrighetti LA, Cai X, Cleary S, Chen KH, Schön MR, Sugioka A, Tang CN, Herman P, Pekolj J, Chen XP, Dagher I, Jarnagin W, Yamamoto M, Strong R, Jagannath P, Lo CM, Clavien PA, Kokudo N, Barkun J, Strasberg SM. Recommendations for laparoscopic liver resection: A report from the second international consensus conference held in Morioka. Ann Surg. 2015;261:619–629. doi: 10.1097/SLA.0000000000001184. [DOI] [PubMed] [Google Scholar]
- 79.Salloum C, Lahat E, Lim C, Hentati H, Compagnon P, Pascal G, Azoulay D. Minimally invasive left lateral sectionectomy robot vs laparoscopy. HPB. 2016;18:e234. [Google Scholar]
- 80.Choi GH, Choi SH, Kim SH, Hwang HK, Kang CM, Choi JS, Lee WJ. Robotic liver resection: Technique and results of 30 consecutive procedures. Surg Endosc. 2012;26:2247–2258. doi: 10.1007/s00464-012-2168-9. [DOI] [PubMed] [Google Scholar]
- 81.Giulianotti PC, Sbrana F, Coratti A, Bianco FM, Addeo P, Buchs NC, Ayloo SM, Benedetti E. Totally robotic right hepatectomy: Surgical technique and outcomes. Arch Surg. 2011;146:844–850. doi: 10.1001/archsurg.2011.145. [DOI] [PubMed] [Google Scholar]
- 82.Levi Sandri GB, de Werra E, Mascianà G, Guerra F, Spoletini G, Lai Q. The use of robotic surgery in abdominal organ transplantation: A literature review. Clin Transplant. 2017:31. doi: 10.1111/ctr.12856. [DOI] [PubMed] [Google Scholar]
- 83.Chen PD, Wu CY, Hu RH, Ho CM, Lee PH, Lai HS, Lin MT, Wu YM. Robotic liver donor right hepatectomy: A pure, minimally invasive approach. Liver Transpl. 2016;22:1509–1518. doi: 10.1002/lt.24522. [DOI] [PubMed] [Google Scholar]
- 84.Mujeeb A, Mohan N, Karkra S, Dhaliwal M, Raghunathan V, Goyal D, Mohanka R, Rastogi A, Balachandran M, Goja S, Kolar P, Bhangui P, Vohra V, Gupta N, Jolly A, Kumar P, Soin AS. Liver transplantation in india-where are we? Single team experience of 131 pediatric living related liver transplants. J Clin Exp Hepatol. 2014;4:S79–S80. [Google Scholar]
- 85.Liao MH, Yang JY, Wu H, Zeng Y. Robot-assisted Living-donor Left Lateral Sectionectomy. Chin Med J (Engl) 2017;130:874–876. doi: 10.4103/0366-6999.202745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Dimitrakopoulos SK, Andriotis A, Koliantzaki SG, Sorras KD, Saltamavros A, Sidiropoulou AN, Papageorgiou E, Bonas A, Oikonomopoulos N, Sidiropoulos NK. 175 historical retrospection of laparoscopic surgery. Maturitas. 2012;71:S69. [Google Scholar]