Abstract
Objective:
Over the last ten years, there has been a dramatic increase in published randomized controlled trials (RCTs) of brief mindfulness training (from single-session inductions to multi-session interventions lasting up to two weeks), with some preliminary indications that these training programs may improve mental health outcomes, such as negative affectivity. This meta-analysis aimed to evaluate whether brief mindfulness training reliably reduces negative affectivity.
Method:
PubMed, PsycINFO, and the Mindfulness Research Monthly Newsletter were systematically searched for brief mindfulness intervention RCTs assessing negative affectivity outcomes (e.g., depression, rumination, anxiety, stress). 65 RCTs, including 5,489 participants predominantly without experience in meditation (64.64% female, mean age = 24.62), qualified for the meta-analytic review.
Results:
The meta-analysis revealed a small but significant effect of brief mindfulness training on reducing negative affectivity compared to control programs (g=.21, p<.001). The overall effect size was significantly moderated by participant characteristics: community samples (g=.41, p<.001) produced larger training effects compared to student samples (g=.14, p=.001) (Qbetween p=.03). No significant effect size differences were found between clinical and non-clinical samples. However, when accounting for publication bias, the overall effect size of brief mindfulness training programs on negative affectivity was significantly reduced (g=.04).
Conclusions:
Brief mindfulness training programs are increasingly popular approaches for reducing negative affectivity. This meta-analysis indicates that brief mindfulness training modestly reduces negative affectivity. Quantitative analyses indicated the presence of publication bias (i.e., unpublished null effect studies), highlighting the need to continue rigorous evaluation of brief mindfulness interventions.
Keywords: mindfulness interventions, negative affectivity, anxiety, depression, meta-analysis
There has been an exponential increase in randomized controlled trials (RCTs) of mindfulness interventions in recent years (Creswell, 2017). While all mindfulness interventions train participants to bring nonjudgmental awareness to the present moment (Bishop et al., 2004), they vary widely in training duration. Many mindfulness RCTs have utilized 8–10 week interventions, such as the 8-week Mindfulness-Based Stress Reduction (MBSR) program, but there has also been a surge of published studies describing brief mindfulness interventions, from single-session inductions to multi-session training programs lasting two weeks or less (e.g., Zeidan et al., 2010a, b; Creswell et al., 2014; see Figure 1). While there have been numerous meta-analytic reviews of longer-term mindfulness training programs (e.g., MBSR) showing that these programs reliably reduce negative affectivity compared to control groups (see Khoury et al., 2015), there are no meta-analytic reviews evaluating the effects of brief mindfulness interventions. This meta-analysis evaluates whether brief mindfulness training decreases negative affectivity in populations new to meditation.
Figure 1. Number of brief mindfulness training RCTs published per year.
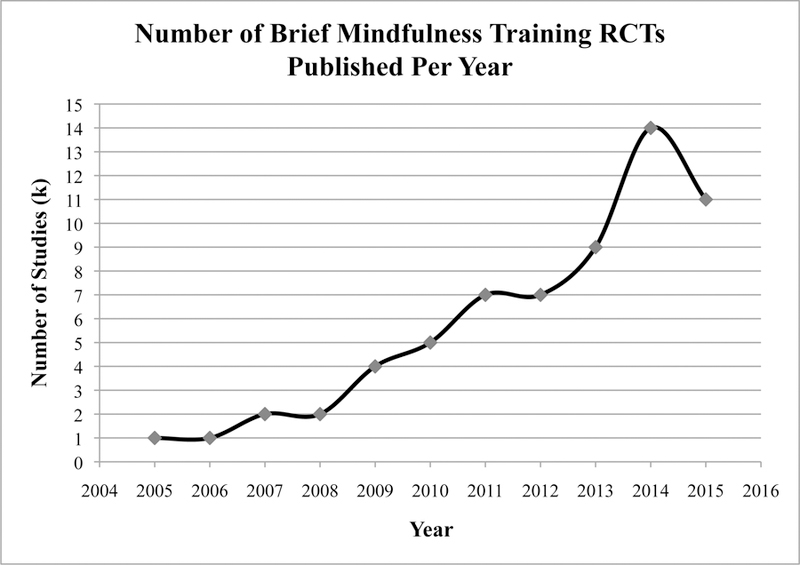
Number of brief mindfulness training studies published per year, beginning with the first brief mindfulness training study published in 2005.
Brief mindfulness training interventions have taken a number of forms, ranging from two-week programs (e.g., 10 minutes of guided at-home practice for 14 days: Cavanagh et al., 2013) to shorter, one-week interventions (e.g., two focused breathing inductions separated by seven days of at-home daily practice: Banks et al., 2015) to single-session inductions that are often lab-based (e.g., five minutes of guided mindfulness practice: Wells & Roussis, 2014). This meta-analysis examines the full range of brief mindfulness interventions and tests whether length of training moderates their efficacy.
Understanding the effects of brief mindfulness interventions is important and timely because brief training approaches (via downloadable Smartphone mindfulness applications or internet streamed audios, for example) are increasingly popular worldwide (Creswell, 2017; Wahbeh, Svalina, & Oken, 2014). And indeed, initial well-controlled RCTs of brief mindfulness training suggest immediate benefits of these programs. For example, in a non-clinical sample exposed to a negative mood induction, Broderick (2005) found that an 8-minute guided mindfulness exercise reduced negative affectivity compared to control exercises. In another non-clinical sample, Zeidan and colleagues (2010b) found that a 3-day intervention (20 minutes of guided practice per day) lowered negative affectivity at post-treatment compared to sham meditation or no training. Despite these promising indications, it is unclear how reliable these effects are across studies and time.
This meta-analysis focuses on the effects of brief mindfulness training programs on reducing measures of negative affectivity, a dimension of subjective distress (Watson & Clark, 1984) that encompasses the experience of negative emotions (e.g., fear, anxiety, disgust) and mood states related to depression (e.g., sadness) (Eysenck, 1970; Gotlib, 1984; Watson, Clark, & Carey, 1988; Zurawski & Smith, 1987). Specifically, negative affectivity is operationalized as any emotional state that is aversive, negative, uncomfortable, or unpleasant, such as anxiety, worry, depression, fear, or anger (Carmody & Baer, 2009; Drapeau, Marchand, & Beaulieu-Pre’vost, 2011; Keng, Smoski, & Robins, 2011; Ridner, 2004). We selected negative affectivity as the outcome of interest in this meta-analysis for several reasons. First, measures of negative affectivity are clinically important; they have been shown to robustly predict clinical symptomatology (Coyne, Thompson, & Racioppo, 2001; Kvaal, Ulstein, Nordhus, & Engedal, 2005, Rush, Carmody, & Reimitz, 2000), including anxiety and depressive symptoms (Headey, Kelley, & Wearing, 1993, Watson, Clark, & Carey, 1988). Second, negative affectivity is one of the most commonly measured outcomes in the mindfulness training literature, with longer-term mindfulness interventions (e.g., MBSR) showing reliable and large effects on reducing negative affectivity compared to control groups (g’s=.62-.80: Baer, 2003; Khoury, Sharma, Rush, & Fournier, 2015). It is also the most commonly measured outcome variable (to our knowledge) in the brief mindfulness interventions literature. In this review, negative affectivity was measured most often via self-report (91 measures) and less often via performance-based measures (2 measures), with the majority of outcomes assessing state-level negative affectivity changes (68 outcomes) (for a full list of negative affectivity outcome measures used in this meta-analysis, see Supplementary Table 1). Finally, negative affectivity is a theoretically relevant outcome in the mindfulness literature. By fostering awareness and nonreactivity toward momentary affective experiences, mindfulness alters how one relates to negative affect; unpleasant and stressful experiences are allowed to arise and pass without interference (Brown, Ryan, & Creswell, 2007; Lindsay & Creswell, 2017).
To examine whether brief mindfulness training reduces negative affectivity, we reviewed published RCTs that assessed the efficacy of brief mindfulness training against a control condition (active or no training) in adults predominantly without prior meditation experience (in a small number of studies, fewer than 5% of participants reported meditation experience). This meta-analysis first presents overall results across all eligible RCTs (N=65). It was predicted that brief mindfulness interventions, relative to control groups, would significantly reduce negative affectivity at post-treatment.
A second aim of this meta-analysis was to empirically evaluate whether study factors or participant characteristics moderated the strength of mindfulness intervention effects on negative affectivity. Previous meta-analyses of longer-term mindfulness training RCTs indicate that intervention duration can moderate the effects of mindfulness training programs, with longer durations of training producing larger mindfulness effects (Khoury et al., 2015; Spijkerman, Pots, & Bohlmeijer, 2016). Given the range of training durations in brief mindfulness interventions (from 5-minute inductions to 2 week programs), this meta-analysis evaluates intervention duration as a moderator. It was hypothesized that there would be a moderating role of intervention duration, such that longer interventions would show larger effects on reducing negative affectivity compared to very brief (e.g., induction) interventions. Regarding participant characteristics, although previous meta-analyses suggest that 8-week mindfulness-based interventions are equally effective for clinical (e.g., physical disease or mental disorder) and nonclinical populations (i.e., students or community volunteers with no clinical diagnoses), some have hypothesized that nonclinical samples are generally likely to show smaller mindfulness training effects due to floor effects. Specifically, with fewer clinical symptoms (e.g., depression and anxiety) at baseline, nonclinical samples have a smaller window for improvement in negative affectivity compared to clinical samples (Carmody & Baer, 2009; Spijkerman et al., 2016). Thus, we explored the hypotheses that clinical status and population type would moderate mindfulness training effects on negative affectivity. Specifically, nonclinical samples were expected to show smaller mindfulness training effects than clinical samples. Community populations were expected to show larger mindfulness training effects than college students, given that community participants are likely more motivated to participate (and to be adherent) to mindfulness intervention programs. Finally, although we had no formal predictions that other participant and study factors would moderate brief mindfulness training effects (age, type of control program, study quality, type of mindfulness exercises, and outcome assessment type and timing)1, these moderators were nonetheless tested in this meta-analysis.
Finally, results are presented from a subsample of RCTs (N=46) that measure negative affectivity in response to a distress paradigm (i.e., tasks designed to trigger a negative affective response). We contrast these “negative affect reactivity studies” with studies measuring changes in negative affectivity from pre- to post-intervention (in the absence of a distress paradigm). We expected brief mindfulness training effects to be more pronounced in these negative affect reactivity studies compared to studies that measure negative affectivity without inducing distress. This expectation borrows logic from the stress-buffering theory; mindfulness may be more effective for lowering negative affectivity in high stress contexts where there is more room for intervention-related improvement (Arch & Craske, 2006; Creswell & Lindsay, 2014).
Methods
This meta-analysis was conducted using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Moher, Liberati, Tetzlaff, Altman, & Group, 2009). Methods and inclusion criteria were specified in advance and documented in a study protocol by the authors of this review.
Search and Selection
The following databases were searched for primary studies between February and May of 2015: PubMed, PsycINFO, and the Mindfulness Research Monthly Newsletter (Black, 2010).
Specifically, the following were used as search terms in the PubMed and PsycINFO databases: ‘mindfulness’ AND ‘brief,’ ‘induction,’ OR ‘short term’. Additional studies were identified from references of relevant studies and review articles retrieved from the database searches.
Figure 2 depicts the study selection process for this meta-analysis. Studies were included if they met the following criteria:
Figure 2. Flowchart of study selection.
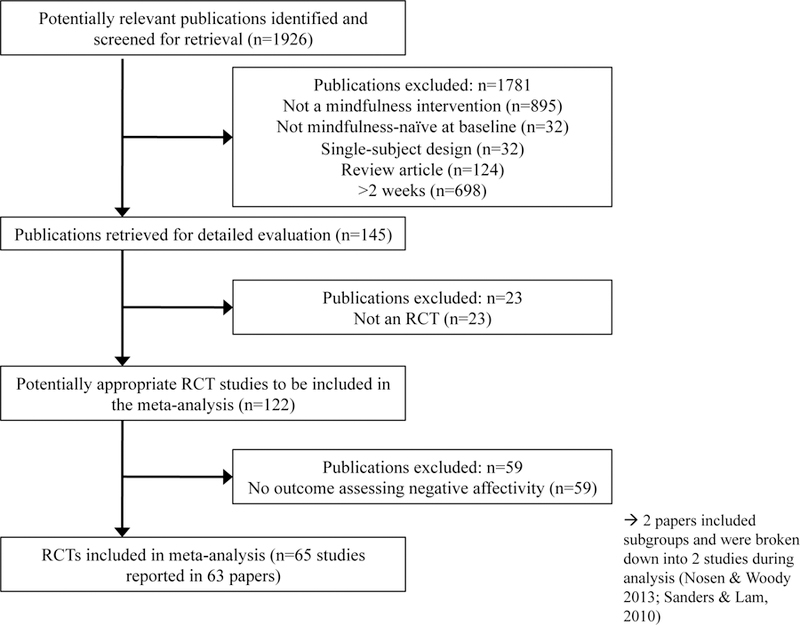
Study selection process for this meta-analysis.
offered a primarily mindfulness meditation-based induction or intervention that aimed to promote nonjudgmental awareness of the present moment (Creswell, 2017) and lasted no longer than 2 weeks2. Studies described as mindfulness-related interventions involving compassion, lovingkindness, Zen, or Buddhist meditation, or those that included mindfulness as part of a multi-component intervention (e.g., Acceptance and Commitment Therapy, Cognitive Behavioral Stress Management, Integrative Body-Mind Therapy) were excluded in order to directly evaluate the impact of mindfulness training without the confounding effects of other intervention elements;
included no more than 5% of participants who reported meditation experience (to assess the effects of brief mindfulness training in a primarily mindfulness-naïve population);
randomly assigned participants to a mindfulness or control condition and used a between-subjects design;
had more than one participant enrolled in the intervention or induction;
included at least one outcome directly measuring negative affectivity. Eligible outcomes measured state or trait negative emotional distress or reactivity (e.g., anger, anxiety, depression, distress, irritability, sadness, shame, stress). Measures that assessed distress or reactivity in response to negative cognitions were included, but cognitive outcomes and tasks without an affective element were not included.
In total, 63 published papers (describing 65 RCTs) met the criteria for inclusion in this meta-analysis. Studies were not excluded based on the clinical status of participants.
Data Abstraction
Information was extracted from each selected study on: (1) characteristics of the study participants (including age, percentage of female participants, ethnicity, whether the sample comprised college students or community adults, and clinical status); (2) type of mindfulness intervention (whether the intervention was an induction or a training program, its duration, and program details); (3) type of control (active or no training); (4) the particular outcome measure assessing negative affectivity and its type (state or trait).
In an effort to reduce reporting bias, all negative affectivity outcomes mentioned in the study’s methods section were included in the database, even if statistical results were not reported for that outcome. When no numerical data was reported on the outcome of interest but figures were included (e.g., bar graphs), group means and SD/SEs were estimated from ruler measurements. When sufficient data was not reported to enable the calculation of an effect size, we contacted the study authors for data. In cases where we were not able to reach authors for data, we coded an F statistic of 0.01 for non-significant effects and missing outcomes, and when Ns per study condition were not obtained, we split Ns evenly between groups (or favored the control group when total Ns were odd).
The coding verification procedure went as follows: A detailed coding manual was developed (and available by request from the authors), and coding reliability was established by two independent coders on several studies (coding agreement was 92.86%). All studies were coded by M.C.S., and a second judge (E.K.L) resolved uncertain coding decisions.
Numerical data were extracted for pre- and post-intervention time points and the coded moderator variables. All data were entered and analyzed using the software program, Comprehensive Meta Analysis Version 3 (CMA; Borenstein, Hedges, Higgins, & Rothstein, 2014). This program allows data entry in various formats based on how the authors reported them. Our preference was to use descriptive statistics (e.g., means and SDs) whenever possible, as opposed to using inferential statistics. The CMA database is available for research purposes by request.
Validity Assessment
Publication bias was evaluated first with a rank correlation test (to test for publication bias in general), then by investigating the extent of publication bias with trim-and-fill methods, and finally by creating funnel plots to visualize the bias. Specifically, Begg’s rank correlation test (Begg and Mazumdar, 1994) is a statistical analogue to the funnel plot and provides a quantitative estimate (using Kendall’s τ) of the relative skewness of the distribution of studies observed in the funnel plot by relating study sample size with each study’s observed effect size (a significant correlation indicates greater publication bias). The trim-and-fill technique described by Duval and Tweedie (2000) evaluated the presence and impact of missing studies shown in the funnel plot, whether they were to the left or to the right of the mean overall effect size (i.e., missing studies with smaller or larger than average effect sizes) using fixed effect models. Specifically, the funnel plot visually assesses publication bias by graphing the effect size estimate of each study against its standard error (with less symmetrical funnel plots indicating greater risk of publication bias).
Study quality was assessed using the Delphi list criteria (Verhagen et al., 1998). This list contains 9 criteria that assess the quality of an RCT: 1) randomization performed, 2) treatment allocation concealed, 3) groups similar at baseline, 4) eligibility criteria specified, 5) outcome assessor blinded3, 6) care provider blinded4, 7) participant blinded, 8) descriptive statistics reported, and 9) intent-to-treat analyses. For each criterion clearly mentioned by a study in the published report, the study receives one point, and if not mentioned, the criterion category receives 0 points, resulting in a Delphi score from 0–9.
Study Characteristics (Moderators)
Length of training:
Length of the mindfulness intervention was coded in two ways. First, an intervention was categorized as either a mindfulness induction (one practice session; e.g., 10 minutes of mindful breathing) or mindfulness training (more than one practice session; e.g., 2 weeks of daily practice). Second, meta-regressions were conducted to look at the moderating role of intervention duration, as measured in minutes, number of sessions, and number of days the training spanned.
Study Population:
The moderating effects of three sample characteristics were tested. First, study population was categorized as comprising either a student or community sample (and if the sample was recruited from both types of populations, the dominant type was favored based on the mean age of the sample, with the cut-off for students at less than 22 years). The average age of the study sample was analyzed with a meta-regression analysis. Clinical status was coded as either nonclinical (i.e., lacking a mental or physical health diagnosis) or clinical (i.e., diagnosed with a disorder or medical condition like Generalized Anxiety Disorder or chronic pain). Additionally, clinical status was analyzed as a moderator separately in student vs. community samples.
Study Quality:
Study quality (i.e., Delphi score) was analyzed continuously in a meta-regression analysis, consistent with previous meta-analyses (Khoury et al., 2013; Spijkerman et al., 2016). Study quality was also analyzed individually in student vs. community samples to explore whether it differed in these two study types and whether it explained potential effect size differences between populations.
Control Type:
Consistent with other mindfulness intervention meta-analyses that tested control condition type as a moderator (Grossman, Niemann, Schmidt, & Walach, 2004; Zoogman, Goldberg, Hoyt, & Miller, 2015), control type was categorized as either “active” or “no training” and evaluated as a moderator. “Active” control conditions included both well-matched (i.e., the control group closely resembled the intervention in duration and amount of required activity; e.g., sham meditation, muscle relaxation) and not well-matched (i.e., the control group participated in some kind of activity that did not match the experimental intervention in terms of duration or rigor; e.g., using usual coping skills) types. In “no training” control conditions, participants did not engage in activity during the time the experimental group received treatment. Larger mindfulness training effects in relation to no training versus active control programs may indicate that active comparisons more accurately account for general or non-specific intervention effects.
Mindfulness Exercise Type:
To compare efficacy among the different mindfulness training exercises used in the selected studies, we coded interventions as instructing: focused breathing, body scan, multiple mindfulness exercises in a single intervention, or “other,” a category that collapses studies where mindfulness instructions were applied to a task (e.g., the raisin-eating exercise: Heppner et al., 2008, Hong et al., 2012; alcohol and smoking cue inductions: Murphy & MacKillop, 2014, Bowen & Marlatt, 2009, Rogojanski et al., 2011) and studies of mindfulness interventions that could not be placed in any of the other three categories (e.g., reading statements mindfully: Huffziger & Kuehner, 2009, Sauer & Baer, 2012, Wahl et al., 2012; learning mindfulness strategies: Chen et al., 2013, Cruess et al., 2015, Singer & Dobson, 2007).
Negative Affectivity Assessment:
Aspects of negative affectivity related to study design and assessment were analyzed in two moderator analyses. To test for the stability of mindfulness training effects, we coded the timing of negative affectivity outcome assessment (whether the outcome was measured immediately post-intervention, within 1 day of the intervention, or 1 day or longer post-intervention). Second, negative affectivity outcomes were categorized as measuring state- or trait-level effects, with the expectation that state negative affectivity would be more malleable in brief mindfulness training studies.
Negative Affect Reactivity Studies:
Within the subsample of negative affect reactivity studies, we assessed whether the timing of the distress paradigm (before, during, after, or both before and after the mindfulness intervention) moderated the brief training effect within these studies so as to compare efficacy across different study designs.
Quantitative Data Synthesis
Due to the heterogeneity across studies from different study designs, such as the differing number of comparison or control groups (1–3) and type of outcome measures (see Supplementary Table 1), we used a random effects model (and in the case of multiple control comparisons to the intervention, a summary effect was computed; Raudenbush, 1994; Shadish & Keith, 1994). Effect directions (see Supplementary Table 1) were typically determined by the measure’s original citation, but when the scale was created specifically for the study, we relied on the author’s interpretation of the effect. Reductions in negative affectivity from pre- to post-training were coded as positive effect directions5.
Effect sizes were calculated in one of two ways: 1) based on pre- and post-intervention values in both the mindfulness and control groups or 2) using only post-intervention data if no pre-intervention data was collected and only post-intervention data was reported. Hedges’ g, the unit for effect size, and its 95% confidence interval (Hedges & Olkin, 1985) were calculated with random-effects models using pre-to-post mean changes and post-only mean differences between groups using the following formula:
Effect sizes (g) were interpreted such that ~0.2 was a small effect, ~0.5 was a medium effect, and ~0.8 was a large effect (Cohen, 1988). A pre-post correlation of 0.6 was used, which is a conservative estimate consistent with previous meta-analyses (Segerstrom & Miller, 2004). Each individual RCT functioned as the unit of analysis, such that each study contributed one effect size in each analysis, and in cases where multiple negative affectivity outcomes were reported in a single RCT, an aggregate effect size was automatically computed; exceptions are noted in the tables. These exceptions consist of studies that included multiple intervention and/or control groups in a single RCT, although the most common study design included one intervention and one control group. In studies where there were multiple mindfulness intervention conditions, an aggregate effect was calculated for all intervention conditions compared to the control condition for each negative affectivity outcome. In studies where there were multiple control conditions, a summary effect for the mindfulness intervention versus all control conditions was calculated.
After the overall negative affectivity effect size was computed (which includes all negative affectivity outcomes), Cochran’s Q was used to evaluate heterogeneity between studies (i.e., whether the observed effect size was influenced by characteristics that vary among studies, such as study design quality and sample characteristics). Given a statistically significant Q, we planned to run moderator analyses and meta-regressions under the assumption that they would explain the heterogeneity across studies.
Results
Primary meta-analytic findings are listed in Table 1. First, we describe the overall negative affectivity effect (Table 1), followed by additional moderator analyses and meta-regressions (Tables 1a-1d) to explore whether the coded moderators explained heterogeneity of the overall effect size. Second, results from the subgroup analysis of studies that included a distress paradigm are presented (Tables 2-2a).
Table 1.
Overall Effects on Negative Affectivity Outcomes.
| Negative Affectivity Outcome | k | N | Effect Size (Hedges’ g) | 95% CI | Q | I2 |
|---|---|---|---|---|---|---|
| All outcomes | 65 | 5489 | 0.208* | 0.124–0.292 | 136.23* | 53.02 |
Note.
p<.001
k=number of studies; N=total participants; 95% CI=95% confidence interval around mean estimate; Q=a standardized metric for heterogeneity of effect sizes around the mean effect size; I2=an estimate of the proportion of observed variability that reflects real effect size variability. N=6 studies had outcomes coded for no effect: Cropley et al., 2007; Ellett et al., 2008; Nosen & Woody, 2013; Ramsey & Jones, 2015; Zabelina, 2011; Zeidan et al., 2010a.
Table 1a.
Moderator Results.
| Moderator Variable | k | N | Effect Size (Hedges’ g) | 95% CI | QWithin | QBetween |
|---|---|---|---|---|---|---|
| Mindfulness Intervention | 1.365 | |||||
| Type Induction | 54+ | 4607 | 0.220*** | 0.122–0.317 | 128.389*** | |
| Training | 14 | 961 | 0.122 | −0.009–0.253 | 13.456 | |
| Population Type | 4.789* | |||||
| Community | 19 | 1160 | 0.402*** | 0.177–0.628 | 58.296*** | |
| Student | 46 | 4329 | 0.136** | 0.057–0.214 | 67.457* | |
| Clinical Status | 1.183 | |||||
| Clinical | 11 | 732 | 0.329** | 0.091–0.567 | 21.198* | |
| Non-Clinical | 54 | 4757 | 0.188*** | 0.098–0.278 | 113.312*** | |
| Control Type | 2.494 | |||||
| Active | 78+ | 5198 | 0.173*** | 0.103–0.243 | 114.574** | |
| No Training | 17+ | 1285 | 0.422** | 0.121–0.722 | 99.020*** | |
| Mindfulness Training Exercise | 12.487** | |||||
| Focused Breathing | 21+ | 1899 | 0.159** | 0.055–0.264 | 24.626 | |
| Multiple Exercises | 12 | 1053 | 0.255* | 0.031–0.479 | 31.512** | |
| Body Scan | 8+ | 588 | −0.089 | −0.256–0.077 | 7.251 | |
| Other | 27 | 2028 | 0.304*** | 0.147–0.461 | 68.139*** | |
| Negative Affectivity Outcome | 1.661 | |||||
| State | 59+ | 4811 | 0.233*** | 0.138–0.327 | 134.062*** | |
| Trait | 18+ | 1296 | 0.136* | 0.022–0.249 | 16.055 | |
| Time Point | 2.746 | |||||
| Immediately Post-Intervention | 77+ | 6218 | 0.286*** | 0.191–0.381 | 238.164*** | |
| Within 1 Day Post-Intervention | 23+ | 1483 | 0.175* | 0.023–0.328 | 40.814** | |
| 1 Day+ Post-Intervention | 5+ | 439 | 0.077 | −0.219–0.374 | 9.304 |
Note.
p<.05
p<.01
p<.001
k=number of studies; N=total participants; 95% CI=95% confidence interval around mean estimate. k+ refers to the analyses where independence was violated by one or more studies being split into multiple studies based on having multiple conditions. These studies were split into multiple studies: Control Type (Arch & Craske, 2006; Broderick, 2005; Cassin et al., 2011; Cruess et al., 2015; Heppner et al., 2008; Hilt & Pollack, 2012; Hong et al., 2012; Hooper et al., 2011; Huffziger & Kuehner, 2009; Johnson et al., 2015; Keng et al., 2013; Kuehner et al., 2009; Laurent et al., 2014; Lee & Orsillo, 2014; Liu et al., 2012; Luethcke et al., 2011; Murphy & MacKillop, 2014; Nosen & Woody, 2013; Ortner & Zelazo, 2014; Ramos Diaz et al., 2014; Shikatani et al., 2014; Singer & Dobson, 2007; Ussher et al., 2009; Villa & Hilt, 2014; Vinci et al., 2014; Wells & Roussis, 2014; Zeidan et al., 2010b), Intervention Type (Ainsworth et al., 2013, 2015; Bonamo et al., 2014), Type of Mindfulness Training Exercise (Ainsworth et al., 2013, 2015; Bonamo et al., 2014), Time Point (Ainsworth et al., 2015; Alberts & Thewissen, 2011; Arch & Craske, 2006; Atkinson & Wade, 2012; Banks et al., 2015; Bowen & Marlatt, 2009; Broderick, 2005; Cropley et al., 2007; Cruess et al., 2015; Erisman & Roemer, 2010; Hilt & Pollak, 2012; Huffziger & Kuehner, 2009; Keng et al., 2013; Kuehner, 2009; Laurent et al., 2014; Marchiori & Papies, 2013; McClintock & Anderson, 2013; Ramos Diaz et al., 2014; Sauer & Baer, 2012; Shikatani et al., 2014; Ussher et al., 2009; Villa & Hilt, 2014; Vinci et al., 2014; Wahl et al., 2012).
Table 2.
Overall Effects on Negative Affect Reactivity Studies.
| Negative Affectivity Outcome | k | N | Effect Size (Hedges’ g) | 95% CI | Q | I2 |
|---|---|---|---|---|---|---|
| All outcomes | 65 | 3810 | 0.245*** | 0.138–0.352 | 109.615*** | 58.947 |
Note.
p<.001
k=number of studies; N=total participants; 95% CI=95% confidence interval around mean estimate; Q=a standardized metric for heterogeneity of effect sizes around the mean effect size; I2=an estimate of the proportion of observed variability that reflects real effect size variability.
Table 2a.
Timing of Distress Paradigm Moderator Analysis.
| Moderator Variable | k | N | Effect Size (Hedges’ g) | 95% CI | QWithin | QBetween |
|---|---|---|---|---|---|---|
| Timing of Distress Paradigm | 0.762 | |||||
| Before Intervention | 10 | 863 | 0.257*** | 0.116–0.397 | 5.820 | |
| After Intervention | 19 | 1832 | 0.262** | 0.077–0.447 | 58.337*** | |
| During Intervention | 7 | 484 | 0.148 | −0.098–0.394 | 10.507 | |
| Before & After Intervention | 11 | 631 | 0.294 | −0.007–0.596 | 32.933*** |
Note.
p<.05
p<.01
p<.001
k=number of studies; N=total participants; 95% CI=95% confidence interval around mean estimate.
Sample Characteristics
5,489 individuals participated in the N=65 independent RCT studies (3,548 were female6,7), and these participants had an average age of 24.62 years (SD=7.77)8. Of the 35 RCTs reporting ethnicity (3,697 participants), 68.97% were Caucasian. Most participants in these studies were categorized as nonclinical (N=4,757) and fewer had clinical diagnoses (N=732).
Sample sizes ranged from 17 to 411 participants, and the average sample size was 84 participants. Studies were drawn from 14 countries, with the United States as the most common setting (N=33).
Overall Effects on Negative Affectivity
As predicted, there was a small, positive effect of brief mindfulness interventions on reducing negative affectivity in the 65 RCTs (Hedges’ g=.21 [.12,.29], p<.001). There was significant heterogeneity in the overall effect size estimate among these 65 studies (Qwithin=136.230, p<.001), so subsequent analyses were conducted with the coded moderator variables to help explain this heterogeneity (Tables 1a-d).
Moderator Effects and Meta-Regressions
Length of Training:
Contrary to predictions, length of training (i.e., whether the mindfulness intervention was one session (g=.22) or longer (g=.12)) did not significantly moderate brief mindfulness intervention effects (see Table 1a). Similarly, meta-regressions showed that the duration of the mindfulness program (in minutes, sessions, or days) did not significantly moderate the overall negative affectivity effect (see Table 1b).
Table 1b.
Meta-Regression Results.
| Regression Variable | k | N | β | 95% CI | Qmodel | Qresidual |
|---|---|---|---|---|---|---|
| Mean Age | 62 | 5320 | 0.0091 | −0.002–0.020 | 2.55 | 128.69*** |
| Duration (minutes) | 61 | 4679 | −0.0006 | −0.003–0.001 | 0.36 | 120.94*** |
| Duration (sessions) | 65 | 5489 | −0.0003 | −0.035–0.034 | 0 | 136.22*** |
| Duration (days) | 65 | 5489 | −0.0087 | −0.036–0.019 | 0.39 | 135.68*** |
| Delphi Score | 65 | 5489 | 0.0674 | −0.008–0.142 | 3.07 | 132.78*** |
| Community | 62 | 5320 | 0.0091 | −0.002–0.020 | 2.55 | 128.69*** |
| Student | 46 | 4329 | 0.0202 | −0.050–0.090 | 0.32 | 67.34* |
Note.
p<.05
p<.01
p<.001
k=number of studies; N=total participants; 95% CI=95% confidence interval around mean estimate; β = slope coefficient. N=3 studies did not report the mean age of their samples or described age more broadly, and were excluded from these analyses (Arch & Craske, 2006; Heppner et al., 2008; Ortner & Zelazo, 2014). N=4 studies did not report the length of the mindfulness induction in minutes, and were excluded from these analyses (Bonamo et al., 2014, Luethcke et al., 2011, Hong et al., 2012, Hulsheger et al., 2013).
Study Population:
Consistent with predictions, the study population type significantly moderated the overall negative affectivity effect (Qbetween p=.03). Specifically, community samples (g=.40) had larger mindfulness intervention effects on reducing negative affectivity relative to student samples (g=.14) (see Table 1a). While clinical status did not significantly moderate the overall effect of mindfulness interventions on negative affectivity, clinical populations showed modestly larger effect sizes (g=.33) than nonclinical populations (g=.19) (see Table 1a). Within community versus student samples alone, clinical status did not significantly moderate the brief mindfulness training effect for these subgroups (see Table 1c). Study sample age did not significantly moderate the overall negative affectivity effect (see Table 1b).
Table 1c.
Subgroup Moderator Results.
| Subgroup | k | N | Effect Size (Hedges’ g) | 95% CI | QWithin | QBetween |
|---|---|---|---|---|---|---|
| Community | 0.037 | |||||
| Clinical | 10 | 525 | 0.390** | 0.128–0.652 | 17.356* | |
| Non-Clinical | 9 | 635 | 0.425* | 0.036–0.814 | 41.010*** | |
| Student | 0.818 | |||||
| Clinical | 1 | 207 | 0.002 | −0.293–0.296 | 0 | |
| Non-Clinical | 45 | 4122 | 0.143** | 0.061–0.225 | 67.017* |
Note.
p<.05
p<.01
p<.001
k=number of studies; N=total participants; 95% CI=95% confidence interval around mean estimate
Study Quality:
When evaluated in a meta-regression analysis, study quality did not significantly moderate the overall negative affectivity effect (see Table 1b). However, within studies using community samples, study quality did moderate the mindfulness training effect (β=.26, p=.03), such that higher quality studies produced larger mindfulness training effects on negative affectivity (see Table 1d); in studies using student samples, study quality was not a significant moderator.
Control Type:
The type of control program (active comparison programs: g=.17; no-training: g=.42) did not significantly moderate the overall effect of mindfulness interventions on negative affectivity, although these effect sizes suggest a smaller overall effect of mindfulness training when compared to other active programs (see Table 1a).
Mindfulness Exercise Type:
The type of mindfulness training exercise (Table 1a) significantly moderated the overall training effect (Qbetween p=.006), with studies instructing multiple types of mindfulness exercises in a single intervention (g=.26) and other types of mindfulness exercises (e.g., mindfulness applied to a task) (g=.30) producing stronger effects compared to studies instructing focused breathing (g=.16) or a body scan (g=−.09), suggesting that instructing mindfulness exercises beyond body scans and focused breathing might be maximally effective.
Negative Affectivity Assessment:
The timing of outcome assessment did not significantly moderate the overall effect (see Table 1a), although effect sizes tended to decrease over time. Outcomes assessed immediately post-intervention showed the largest effect (g=.29), followed by those assessed later that same day (g=.18), and outcomes assessed 1 day or longer post-intervention showed very small effects (g=.08), suggesting that brief mindfulness training effects on negative affectivity may fade with time. Second, whether an outcome measured state or trait negative affectivity did not significantly moderate the overall brief mindfulness training effect (see Table 1a), although state measures (g=.23) produced somewhat larger training effects than trait measures (g=.14).
Negative Affect Reactivity Studies
In the subsample of 46 RCTs that used a distress paradigm to measure negative affect reactivity, a small significant effect of brief mindfulness training was present (Hedges’ g=.27 [.14,.35], p<.001), which, consistent with predictions, was larger than the effect observed in studies that did not use a distress paradigm (Hedges’ g=.10 [−.01, .22], p=.08). There was significant heterogeneity within this reactivity study effect (Table 2). Although the timing of the distress paradigm did not significantly moderate the overall effect within these studies (Table 2a), studies that administered distress paradigms before (g=.26), after (g=.26), as well as both before and after mindfulness training (g=.29) had comparable negative reactivity effects, whereas studies that administered a distress paradigm during the intervention produced a smaller effect (g=.15).
Publication Bias Assessment
To evaluate the potential of publication bias in this brief mindfulness training literature, funnel plots visually depict the distribution of study effect sizes against their standard errors (open circles in Figure 3). Begg’s rank correlation test (Begg & Mazumdar, 1994) indicated a significant association between sample size and observed effect size for studies with negative affectivity outcomes (Kendall’s τ = .40, p <.001), indicating a risk for publication bias in this brief mindfulness training literature. To explore the nature of publication bias, trim-and-fill analyses (Duval & Tweedie, 2000) estimated the potential for missing studies to the left and right of the mean effect size and then filled these studies on the funnel plots (filled-in circles in Figure 3). The trim-and-fill analysis indicated no studies to be missing on the right side (positive mindfulness training effects) whereas 18 study effect sizes were estimated to be missing on the left side (negative or null mindfulness training effects) (Figure 3). By filling in these missing negative effect studies, the trim-and-fill analysis estimates the brief mindfulness training effect size on negative affectivity outcomes to be much more modest and not significantly different from zero (adjusted effect size of training on negative affectivity for potentially missing studies: Hedges’ g=.04 [−.01, .09]).
Figure 3. Funnel plot evaluating publication bias among negative affectivity outcome studies.
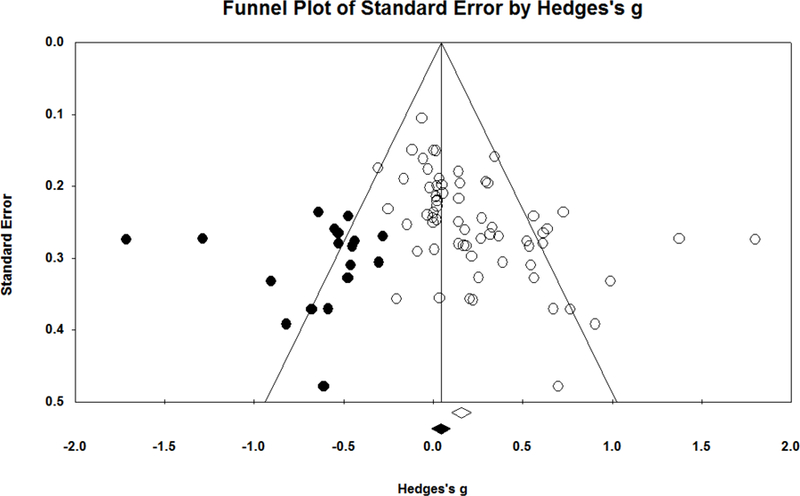
Each funnel plot displays a scatterplot of studies (with open circles) as a function of the study effect size (Hedges’ g) by its standard error. Filled circles are estimates of potentially missing studies from the trim-and-fill analysis, with the filled diamond and vertical line indicating the estimated population effect size after the trim-and-fill procedure.
Discussion
This is the first meta-analysis to examine the effects of brief mindfulness meditation training on negative affectivity outcomes, with the aim of assessing the overall magnitude of the effect of brief mindfulness interventions across studies. The results show that brief mindfulness training programs have an immediate and significant (albeit small) effect on decreasing negative affectivity in both nonclinical and clinical samples. However, since the majority of studies in this meta-analysis sampled from nonclinical populations, the efficacy of brief mindfulness training on reducing negative affectivity in clinical populations requires further evaluation. Overall, brief mindfulness interventions may be effective for reducing negative affectivity by activating attention regulation (Ainsworth et al., 2013; Dickenson et al., 2013) and emotion regulation skills (e.g., decreasing mind-wandering and rumination: Rahl et al., 2016, Chiesa & Serretti, 2009; increasing the tolerance for negative emotional content and arousal: Lutz et al., 2013).
Importantly, analyses also reveal the potential for publication bias in this meta-analysis (i.e., null results might not have been published), suggesting caution in inferring that brief mindfulness training programs reliably reduce negative affectivity. Specifically, trim-and-fill analyses estimated that some studies with negative effects may have been conducted but not published (Figure 3), and including these hypothetical studies reduces the overall effect size to nearly zero.
The possible existence of numerous unpublished brief mindfulness training studies combined with the significant heterogeneity among published studies included in this meta-analysis suggests the likelihood of important boundary conditions on the putative benefits of brief mindfulness training programs on reducing negative affectivity. To this end, this meta-analysis explored several moderating factors that begin to identify contexts when brief mindfulness training effects may be present (e.g., in community samples; immediately post-intervention; in interventions that include multiple mindfulness exercises), but these factors need to be carefully evaluated in future RCTs. Specifically, this meta-analysis indicates that brief mindfulness training programs had significantly larger negative affectivity reduction effects among community adult populations compared to college students. One potential explanation is that there may be higher motivation among community members to seek out and engage with brief mindfulness training programs. For example, older community adults exhibit more positive help-seeking attitudes than younger adults (Mackenzie et al., 2008). This finding supports the notion that particular populations may benefit more from brief mindfulness interventions than others (Creswell & Lindsay, 2014).
The literature on brief mindfulness training shows that studies thus far have mainly sampled from nonclinical populations (approximately 87% of the participants included in this meta-analysis were drawn from nonclinical populations). Although the few studies drawn from clinical populations (k=11; N=732) showed a significant effect of brief mindfulness interventions on reducing negative affectivity in this meta-analysis (g=.33), it is important for future research to further evaluate the efficacy of brief mindfulness interventions in clinical populations, particularly in light of evidence suggesting that individuals with clinical diagnoses have more difficulty practicing mindfulness effectively for the first time compared to nonclinical individuals (Vitalia & Răban-Motounu, 2014). Moreover, the studies included in this meta-analysis did not assess clinical outcomes. Still, brief mindfulness practices are widely used for managing negative affect (Arch & Craske, 2006; Sears & Kraus, 2009; Vinci et al., 2014), an important outcome for mental health professionals (Sauer-Zavala et al., 2012). More research is needed to test whether brief mindfulness interventions may have clinically meaningful effects, and to address the problem of publication bias that limits support for recommending brief mindfulness interventions as an evidence-based treatment for negative affectivity.
Surprisingly, this meta-analysis did not indicate that training duration (which ranged from one session to two weeks of mindfulness training) moderated the overall effect; instead, very brief mindfulness interventions had comparable effects to multi-day brief mindfulness interventions. Moreover, moderator analyses suggest that brief mindfulness training effects on negative affectivity tend to fade with time (see Table 1a) across all lengths of training. Thus, in contrast to more intensive 8-week mindfulness interventions that promote more stable benefits over time (e.g., Bowen et al., 2014; Kuyken et al., 2015), it’s likely that brief mindfulness interventions of up to two weeks have acute, but not long-term, benefits for reducing negative affectivity. Future research directly comparing the effects of inductions, brief trainings, and standard 8-week interventions with multiple post-intervention assessments would inform this question.
Within the 46 negative affect reactivity studies, the timing of the distress paradigm in relation to mindfulness training did not significantly moderate the overall effect. The effects of mindfulness were equally strong when practiced before or after a distress task, as well as when there were multiple distress tasks with mindfulness practice in between, potentially serving two roles: reducing negative affect in response to distress (acting as a distress inoculation) and promoting recovery from distress (with distress potentially increasing participants’ motivation to engage in mindfulness). A recent review of acceptance and mindfulness-based interventions (Levin, Luoma, & Haeger, 2015) concluded that these interventions may reduce the relationship between initial negative affect (e.g., depression) and further reactivity. The present meta-analysis supports and extends these findings, suggesting that mindfulness practice may reduce both the magnitude of initial negative reactivity and the ongoing reactivity toward that primary negative emotional experience (thus facilitating recovery). For example, Arch and Craske (2006) showed that practicing mindfulness between aversive task blocks increased the willingness to be exposed to aversive stimuli, and noted that mindfulness seemed to reduce reactivity and facilitate recovery. Similarly, Erisman and Roemer (2010) measured negative affectivity in response to negative film clips before and twice after a mindfulness induction and found that mindfulness lowered self-reported negative affectivity directly following the film clips (but had no effect when negative affectivity was assessed at a more distal post-induction time point). These results suggest that mindfulness may facilitate emotion regulation by reducing initial reactivity to emotionally threatening stimuli, which reduces the later need for recovery. More research is needed to understand when brief mindfulness training is most effective and the mechanisms through which it impacts affective reactivity and recovery processes over time.
This review is the first systematic meta-analysis of brief mindfulness meditation training, addressing an important gap in the mindfulness intervention literature. Nonetheless, this review has several limitations. First, given the potential for unpublished brief mindfulness training studies with null results, our decision not to seek out and include unpublished studies could be viewed as a limitation. On the other hand, while including unpublished studies may reduce the risk of publication bias, their inclusion can introduce other sources of bias (Higgins & Green, 2011), including the possibility of critical methodological mistakes and unreliable results not addressed through peer-review (Chalmers et al., 1987).
Second, most outcomes were self-reported (except two that were performance-based), a method of data collection that is biased by many factors as it is difficult to introspect about higher-order cognitive processes (Nisbett & Wilson, 1977). To improve reporting on negative affectivity, future studies might implement validated behavioral measures of negative affectivity in addition to self-report measures (e.g., Paced Auditory Serial Addition Task, a behavioral measure of distress tolerance: Lejuez, Kahler, & Brown, 2003). Additionally, Ecological Momentary Assessment (EMA) methods (Shiffman et al., 2008), which collect real-time data in daily life, are an increasing popular way to reduce memory bias by measuring affective experiences in response to daily life events (for recent mindfulness training studies using EMA methods, see Huffziger et al., 2013; Mrazek et al., 2013; Ruscio, Muench, Brede, MacIntyre, & Waters, 2016; Ruscio, Muench, Brede, & Waters, 2016).
Third, the immediacy of post-training outcome assessments in most studies is not informative about the lasting effects – if any – of brief mindfulness training on negative affectivity and its impact on daily life functioning; thus, negative affectivity should be measured at more distal time points and in daily life in future research.
Finally, the studies in this meta-analysis were categorized as having relatively low (Buffart et al., 2012) methodological quality overall (mean Delphi score = 3.23, SD = 1.09), which may be attributed to a lack of clarity in reporting study design characteristics. To improve study quality, future reports should not only explicitly describe their study designs (e.g., participant blinding is particularly important; Bergeron, Almgren-Doré, & Dandeneau, 2016), but also adhere to guidelines for conducting high quality RCTs (e.g., CONSORT; Rennie, 2001).
Several more directions for future research emerge from the findings presented in this meta-analysis. In light of the finding that community adults show larger mindfulness effects than college students, future studies might assess subjects’ baseline motivation for participating.
Perhaps mindfulness is less effective for those driven by external motivation (e.g., monetary compensation or, for college students specifically, course credit); thus, researchers might study the moderating role of motivation. In line with general recommendations in the field (Davidson, 2010; MacCoon et al., 2012) and in light of the finding that mindfulness training showed smaller effects when compared to active rather than no training controls (see Table 1a), it is important for future studies to use well-matched active control programs (e.g., sham meditation, used in Zeidan et al., 2010b). Active control programs more effectively control for non-specific treatment factors, an approach that enables studies to test the unique effects of the “active ingredients” of mindfulness training (Chiesa & Serretti, 2009). Otherwise, mindfulness-specific factors are mixed with non-specific effects of undergoing an intervention (Karlsson & Bergmark, 2015). Another direction for future research is the opportunity to conduct a meta-analytic review assessing brief mindfulness training effects on cognitive outcomes (e.g., working memory, attention), a growing area of literature. In this review alone, 14 out of 66 RCTs measured cognitive outcomes in addition to negative affectivity (e.g., N-back performance; Johnson et al., 2015). This type of review might also inform mindfulness mechanisms (e.g., meditation training may first evoke attentional and meta-cognitive skills or states (Bishop et al., 2004) which then affect emotional health over time (Wells, 2002).
Overall, this meta-analytic review suggests caution in implementing brief mindfulness training programs for reducing negative affectivity, given the potential presence of publication bias. While brief mindfulness programs are rapidly growing in popularity, more rigorous research is needed to evaluate their presumed benefits. This meta-analysis provides some initial clues about populations that may particularly benefit (e.g., community adults), formats for brief mindfulness training (e.g., multiple types of mindfulness exercises in a single program), and study design approaches (e.g., measuring negative affectivity using state measures) that may be important for determining when we are likely to see benefits, evidence that we think will help the field advance in understanding brief mindfulness intervention effects in the coming years.
Supplementary Material
Public Health Significance.
This meta-analysis shows that brief mindfulness interventions lasting up to two weeks are potentially effective for reducing negative affectivity among people with no prior meditation experience. The presence of publication bias in this literature indicates that more published studies are needed to evaluate whether this effect is reliable and robust.
Acknowledgements:
This work was conducted at Carnegie Mellon University.
Footnotes
We did not pursue other demographic factors such as sex, ethnicity, and socioeconomic status (SES) as moderators because there is little indication in the literature for sex differences in mindfulness training effects (Khoury et al., 2013; Zoogman et al., 2015) and limited information was available for determining SES and ethnicity from the included studies.
Studies that did not explicitly refer to the intervention or induction as “mindfulness” but were primarily focused on training or inducing the two key components of mindfulness (awareness and acceptance; Bishop et al., 2004) were included.
By “outcome assessor” we are referring to the experimenter.
Since we were not examining a medical intervention that required a doctor or care provider, by “care provider” we are referring to the person who delivered the mindfulness intervention program (in most cases, mindfulness instructions were pre-recorded) and whether they were blind to condition.
Two outcomes measured distress tolerance (Sauer & Baer, 2012) and psychological detachment (Hülsheger et al., 2015); in these cases, an increase in these outcomes from pre- to post-training was coded as a positive effect direction.
4 studies did not report the number of female participants (Cavanagh et al., 2013; Droit Volet et al. 2014; Ortner & Zelazo, 2014; Wells & Roussis, 2014).
N female and mean age should be interpreted cautiously, as several studies only reported these statistics prior to dropouts and exclusions.
3 studies either a) did not report mean or median age (Heppner et al. 2008, Ortner & Zelazo, 2014) or b) described age more broadly (Arch & Craske, 2006).
References
References marked with an asterisk indicate studies included in the meta-analysis.
- *Adams CE, Benitez L, Kinsaul J, Apperson McVay M, Barbry A, Thibodeaux A, & Copeland AL (2013). Effects of brief mindfulness instructions on reactions to body image stimuli among female smokers: an experimental study. Nicotine & Tobacco Research: Official Journal of the Society for Research on Nicotine and Tobacco, 15(2), 376–384. 10.1093/ntr/nts133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Ainsworth B, Eddershaw R, Meron D, Baldwin DS, & Garner M (2013). The effect of focused attention and open monitoring meditation on attention network function in healthy volunteers. Psychiatry Research, 210(3), 1226–1231. 10.1016/j.psychres.2013.09.002 [DOI] [PubMed] [Google Scholar]
- *Ainsworth B, Marshall JE, Meron D, Baldwin DS, Chadwick P, Munafò MR, & Garner M (2015). Evaluating psychological interventions in a novel experimental human model of anxiety. Journal of Psychiatric Research, 63, 117–122. 10.1016/j.jpsychires.2015.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Alberts HJEM, & Thewissen R (2011). The Effect of a Brief Mindfulness Intervention on Memory for Positively and Negatively Valenced Stimuli. Mindfulness, 2(2), 73–77. 10.1007/s12671-011-0044-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Arch JJ, & Craske MG (2006). Mechanisms of mindfulness: emotion regulation following a focused breathing induction. Behaviour Research and Therapy, 44(12), 1849–1858. 10.1016/j.brat.2005.12.007 [DOI] [PubMed] [Google Scholar]
- *Atkinson MJ, & Wade TD (2012). Impact of metacognitive acceptance on body dissatisfaction and negative affect: engagement and efficacy. Journal of Consulting and Clinical Psychology, 80(3), 416–425. 10.1037/a0028263 [DOI] [PubMed] [Google Scholar]
- Baer RA (2003). Mindfulness Training as a Clinical Intervention: A Conceptual and Empirical Review. Clinical Psychology: Science and Practice, 10(2), 125–143. 10.1093/clipsy.bpg015 [DOI] [Google Scholar]
- *Banks JB, Welhaf MS, & Srour A (2015). The protective effects of brief mindfulness meditation training. Consciousness and Cognition, 33, 277–285. 10.1016/j.concog.2015.01.016 [DOI] [PubMed] [Google Scholar]
- Begg CB, & Mazumdar M (1994). Operating Characteristics of a Rank Correlation Test for Publication Bias. Biometrics, 50(4), 1088–1101. [PubMed] [Google Scholar]
- Bergeron CM, Almgren-Doré I, & Dandeneau S (2016). “Letting Go” (Implicitly): Priming Mindfulness Mitigates the Effects of a Moderate Social Stressor. Frontiers in Psychology, 7 10.3389/fpsyg.2016.00872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishop SR, Lau M, Shapiro S, Carlson L, Anderson ND, Carmody J, … Devins G (2004). Mindfulness: A Proposed Operational Definition. Clinical Psychology: Science and Practice, 11(3), 230–241. 10.1093/clipsy.bph077 [DOI] [Google Scholar]
- Black DS (2010). Mindfulness Research Monthly. Mindfulness Research Monthly [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Bonamo KK, Legerski J-P, & Thomas KB (2014). The Influence of a Brief Mindfulness Exercise on Encoding of Novel Words in Female College Students. Mindfulness, 6(3), 535–544. 10.1007/s12671-014-0285-3 [DOI] [Google Scholar]
- Borenstein M, Hedges L, Higgins J, & Rothstein H (2014). Comprehensive Meta-Analysis Version 3 Englewood NJ: Biostat. [Google Scholar]
- *Bowen S, & Marlatt A (2009). Surfing the urge: brief mindfulness-based intervention for college student smokers. Psychology of Addictive Behaviors: Journal of the Society of Psychologists in Addictive Behaviors, 23(4), 666–671. 10.1037/a0017127 [DOI] [PubMed] [Google Scholar]
- Bowen S, Witkiewitz K, Clifasefi SL, Grow J, Chawla N, Hsu SH, … Larimer ME (2014). Relative Efficacy of Mindfulness-Based Relapse Prevention, Standard Relapse Prevention, and Treatment as Usual for Substance Use Disorders: A Randomized Clinical Trial. JAMA Psychiatry, 71(5), 547–556. 10.1001/jamapsychiatry.2013.4546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Broderick PC (2005). Mindfulness and Coping with Dysphoric Mood: Contrasts with Rumination and Distraction. Cognitive Therapy and Research, 29(5), 501–510. 10.1007/s10608-005-3888-0 [DOI] [Google Scholar]
- Brown KW, Ryan RM, & Creswell JD (2007). Mindfulness: Theoretical Foundations and Evidence for its Salutary Effects. Psychological Inquiry, 18(4), 211–237. 10.1080/10478400701598298 [DOI] [Google Scholar]
- Buffart LM, van Uffelen JG, Riphagen II, Brug J, van Mechelen W, Brown WJ, & Chinapaw MJ (2012). Physical and psychosocial benefits of yoga in cancer patients and survivors, a systematic review and meta-analysis of randomized controlled trials. BMC Cancer, 12, 559 10.1186/1471-2407-12-559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmody J, & Baer RA (2009). How Long Does a Mindfulness-Based Stress Reduction Program Need to Be? A Review of Class Contact Hours and Effect Sizes for Psychological Distress. Journal of Clinical Psychology, 65(6), 627–638. 10.1002/jclp.20555 [DOI] [PubMed] [Google Scholar]
- *Cassin SE, & Rector NA (2011). Mindfulness and the Attenuation of Post-Event Processing in Social Phobia: An Experimental Investigation. Cognitive Behaviour Therapy, 40(4), 267–278. [DOI] [PubMed] [Google Scholar]
- *Cavanagh K, Strauss C, Cicconi F, Griffiths N, Wyper A, & Jones F (2013). A randomised controlled trial of a brief online mindfulness-based intervention. Behaviour Research and Therapy, 51(9), 573–578. 10.1016/j.brat.2013.06.003 [DOI] [PubMed] [Google Scholar]
- Chalmers TC, Levin H, Sacks HS, Reitman D, Berrier J, & Nagalingam R (1987). Meta-analysis of clinical trials as a scientific discipline. I: Control of bias and comparison with large co-operative trials. Statistics in Medicine, 6(3), 315–328. [DOI] [PubMed] [Google Scholar]
- *Chen Y, Yang X, Wang L, & Zhang X (2013). A randomized controlled trial of the effects of brief mindfulness meditation on anxiety symptoms and systolic blood pressure in Chinese nursing students. Nurse Education Today, 33(10), 1166–1172. 10.1016/j.nedt.2012.11.014 [DOI] [PubMed] [Google Scholar]
- Chiesa A, & Serretti A (2009). Mindfulness-based stress reduction for stress management in healthy people: a review and meta-analysis. Journal of Alternative and Complementary Medicine (New York, N.Y.), 15(5), 593–600. 10.1089/acm.2008.0495 [DOI] [PubMed] [Google Scholar]
- Cohen J (1988). Statistical Power Analysis for the Behavioral Sciences (2 edition). Hillsdale, N.J: Routledge. [Google Scholar]
- Coyne JC, Thompson R, & Racioppo MW (2001). Validity and efficiency of screening for history of depression by self-report. Psychological Assessment, 13(2), 163–170. [PubMed] [Google Scholar]
- Creswell JD (2017). Mindfulness Interventions. Annual Review of Psychology, 68(1), 491–516. 10.1146/annurev-psych-042716-051139 [DOI] [PubMed] [Google Scholar]
- Creswell JD, & Lindsay EK (2014). How Does Mindfulness Training Affect Health? A Mindfulness Stress Buffering Account. Current Directions in Psychological Science, 23(6), 401–407. 10.1177/0963721414547415 [DOI] [Google Scholar]
- *Creswell JD, Pacilio LE, Lindsay EK, & Brown KW (2014). Brief mindfulness meditation training alters psychological and neuroendocrine responses to social evaluative stress. Psychoneuroendocrinology, 44, 1–12. 10.1016/j.psyneuen.2014.02.007 [DOI] [PubMed] [Google Scholar]
- *Cropley M, Ussher M, & Charitou E (2007). Acute effects of a guided relaxation routine (body scan) on tobacco withdrawal symptoms and cravings in abstinent smokers. Addiction (Abingdon, England), 102(6), 989–993. 10.1111/j.1360-0443.2007.01832.x [DOI] [PubMed] [Google Scholar]
- *Cruess DG, Finitsis DJ, Smith A-L, Goshe BM, Burnham K, Burbridge C, & O’Leary K (2015). Brief stress management reduces acute distress and buffers physiological response to a social stress test. International Journal of Stress Management, 22(3), 270–286. 10.1037/a0039130 [DOI] [Google Scholar]
- Davidson RJ (2010). Empirical explorations of mindfulness: Conceptual and methodological conundrums. Emotion (Washington, D.C.), 10(1), 8–11. 10.1037/a0018480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickenson J, Berkman ET, Arch J, & Lieberman MD (2013). Neural correlates of focused attention during a brief mindfulness induction. Social Cognitive and Affective Neuroscience, 8(1), 40–47. 10.1093/scan/nss030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drapeau A, Marchand A, & Beaulieu-Pre’vost D (2011). Epidemiology of psychological distress. In mental illnesses — understanding, prediction and control. In Mental Illnesses - Understanding, Prediction and Control (pp. 105–134). InTech. [Google Scholar]
- *Droit-Volet S, Fanget M, & Dambrun M (2015). Mindfulness meditation and relaxation training increases time sensitivity. Consciousness and Cognition, 31, 86–97. 10.1016/j.concog.2014.10.007 [DOI] [PubMed] [Google Scholar]
- Duval S, & Tweedie R (2000). Trim and Fill: A Simple Funnel-Plot–Based Method of Testing and Adjusting for Publication Bias in Meta-Analysis. Biometrics, 56(2), 455–463. 10.1111/j.0006-341X.2000.00455.x [DOI] [PubMed] [Google Scholar]
- *Ellett L, Freeman D, & Garety PA (2008). The psychological effect of an urban environment on individuals with persecutory delusions: the Camberwell walk study. Schizophrenia Research, 99(1–3), 77–84. 10.1016/j.schres.2007.10.027 [DOI] [PubMed] [Google Scholar]
- *Erisman SM, & Roemer L (2010). A preliminary investigation of the effects of experimentally induced mindfulness on emotional responding to film clips. Emotion (Washington, D.C.), 10(1), 72–82. 10.1037/a0017162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eysenck SB (1970). Junior Eysenck personality inventory University of London Press. [Google Scholar]
- Gotlib IH (1984). Depression and general psychopathology in university students. Journal of Abnormal Psychology, 93(1), 19–30. 10.1037/0021-843X.93.1.19 [DOI] [PubMed] [Google Scholar]
- Grossman P, Niemann L, Schmidt S, & Walach H (2004). Mindfulness-based stress reduction and health benefits: A meta-analysis. Journal of Psychosomatic Research, 57(1), 35–43. 10.1016/S0022-3999(03)00573-7 [DOI] [PubMed] [Google Scholar]
- Headey B, Kelley J, & Wearing A (1993). Dimensions of mental health: Life satisfaction, positive affect, anxiety and depression. Social Indicators Research, 29(1), 63–82. 10.1007/BF01136197 [DOI] [Google Scholar]
- Hedges LV, & Olkin I (1985). Statistical Methods for Meta-Analysis (1 edition). Orlando: Academic Press. [Google Scholar]
- *Heppner WL, Kernis MH, Lakey CE, Campbell WK, Goldman BM, Davis PJ, & Cascio EV (2008). Mindfulness as a means of reducing aggressive behavior: dispositional and situational evidence. Aggressive Behavior, 34(5), 486–496. 10.1002/ab.20258 [DOI] [PubMed] [Google Scholar]
- Higgins JPT, & Green S (Eds.). (2011). Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated March 2011] The Cochrane Collaboration. [Google Scholar]
- *Hilt LM, & Pollak SD (2012). Getting out of rumination: comparison of three brief interventions in a sample of youth. Journal of Abnormal Child Psychology, 40(7), 1157–1165. 10.1007/s10802-012-9638-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Hong PY, Lishner DA, & Han KH (2012). Mindfulness and Eating: An Experiment Examining the Effect of Mindful Raisin Eating on the Enjoyment of Sampled Food. Mindfulness, 5(1), 80–87. 10.1007/s12671-012-0154-x [DOI] [Google Scholar]
- *Hooper N, Davies N, Davies L, & McHugh L (2011). Comparing thought suppression and mindfulness as coping techniques for spider fear. Consciousness and Cognition, 20(4), 1824–1830. 10.1016/j.concog.2011.05.013 [DOI] [PubMed] [Google Scholar]
- *Huffziger S, & Kuehner C (2009). Rumination, distraction, and mindful self-focus in depressed patients. Behaviour Research and Therapy, 47(3), 224–230. 10.1016/j.brat.2008.12.005 [DOI] [PubMed] [Google Scholar]
- Huffziger S, Ebner-Priemer U, Eisenbach C, Koudela S, Reinhard I, Zamoscik V, … Kuehner C (2013). Induced ruminative and mindful attention in everyday life: An experimental ambulatory assessment study. Journal of Behavior Therapy and Experimental Psychiatry, 44(3), 322–328. 10.1016/j.jbtep.2013.01.007 [DOI] [PubMed] [Google Scholar]
- *Hülsheger UR, Alberts HJEM, Feinholdt A, & Lang JWB (2013). Benefits of mindfulness at work: the role of mindfulness in emotion regulation, emotional exhaustion, and job satisfaction. The Journal of Applied Psychology, 98(2), 310–325. 10.1037/a0031313 [DOI] [PubMed] [Google Scholar]
- *Hülsheger UR, Feinholdt A, & Nübold A (2015). A low-dose mindfulness intervention and recovery from work: Effects on psychological detachment, sleep quality, and sleep duration. Journal of Occupational and Organizational Psychology, 88(3), 464–489. 10.1111/joop.12115 [DOI] [Google Scholar]
- *Johnson S, Gur RM, David Z, & Currier E (2013). One-Session Mindfulness Meditation: A Randomized Controlled Study of Effects on Cognition and Mood. Mindfulness, 6(1), 88–98. 10.1007/s12671-013-0234-6 [DOI] [Google Scholar]
- Karlsson P, & Bergmark A (2015). Compared with what? An analysis of control-group types in Cochrane and Campbell reviews of psychosocial treatment efficacy with substance use disorders. Addiction, 110(3), 420–428. 10.1111/add.12799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keng S, Robins CJ, Smoski MJ, Dagenbach J, & Leary MR (2013). Reappraisal and mindfulness: A comparison of subjective effects and cognitive costs. Behaviour Research and Therapy, 51(12), 899–904. 10.1016/j.brat.2013.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keng S, Smoski MJ, & Robins CJ (2011). Effects of Mindfulness on Psychological Health: A Review of Empirical Studies. Clinical Psychology Review, 31(6), 1041–1056. 10.1016/j.cpr.2011.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khoury B, Sharma M, Rush SE, & Fournier C (2015). Mindfulness-based stress reduction for healthy individuals: A meta-analysis. Journal of Psychosomatic Research, 78(6), 519–528. 10.1016/j.jpsychores.2015.03.009 [DOI] [PubMed] [Google Scholar]
- *Kiken LG, & Shook NJ (2011). Looking Up: Mindfulness Increases Positive Judgments and Reduces Negativity Bias. Social Psychological and Personality Science, 2(4), 425–431. 10.1177/1948550610396585 [DOI] [Google Scholar]
- *Kuehner C, Huffziger S, & Liebsch K (2009). Rumination, distraction and mindful self-focus: effects on mood, dysfunctional attitudes and cortisol stress response. Psychological Medicine, 39(2), 219–228. 10.1017/S0033291708003553 [DOI] [PubMed] [Google Scholar]
- Kuyken W, Hayes R, Barrett B, Byng R, Dalgleish T, Kessler D, … Byford S (2015). Effectiveness and cost-effectiveness of mindfulness-based cognitive therapy compared with maintenance antidepressant treatment in the prevention of depressive relapse or recurrence (PREVENT): a randomised controlled trial. The Lancet, 386(9988), 63–73. 10.1016/S0140-6736(14)62222-4 [DOI] [PubMed] [Google Scholar]
- *Laurent HK, Laurent SM, Nelson B, Wright DB, & Sanchez M-ADA (2014). Dispositional Mindfulness Moderates the Effect of a Brief Mindfulness Induction on Physiological Stress Responses. Mindfulness, 6(5), 1192–1200. 10.1007/s12671-014-0377-0 [DOI] [Google Scholar]
- *Lee JK, & Orsillo SM (2014). Investigating cognitive flexibility as a potential mechanism of mindfulness in Generalized Anxiety Disorder. Journal of Behavior Therapy and Experimental Psychiatry, 45(1), 208–216. 10.1016/j.jbtep.2013.10.008 [DOI] [PubMed] [Google Scholar]
- Lejuez C, Kahler C, & Brown R (2003). A modified computer version of the Paced Auditory Serial Addition Task (PASAT) as a laboratory-based stressor. The Behavior Therapist, 26(4), 290–293. [Google Scholar]
- Levin ME, Luoma JB, & Haeger JA (2015). Decoupling as a Mechanism of Change in Mindfulness and Acceptance: A Literature Review. Behavior Modification, 39(6), 870–911. 10.1177/0145445515603707 [DOI] [PubMed] [Google Scholar]
- Liehr P, & Diaz N (2010). A Pilot Study Examining the Effect of Mindfulness on Depression and Anxiety for Minority Children. Archives of Psychiatric Nursing, 24(1), 69–71. 10.1016/j.apnu.2009.10.001 [DOI] [PubMed] [Google Scholar]
- Lindsay EK, & Creswell JD (2017). Mechanisms of mindfulness training: Monitor and Acceptance Theory (MAT). Clinical Psychology Review, 51, 48–59. 10.1016/j.cpr.2016.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X, Wang S, Chang S, Chen W, & Si M (2013). Effect of brief mindfulness intervention on tolerance and distress of pain induced by cold-pressor task. Stress and Health: Journal of the International Society for the Investigation of Stress, 29(3), 199–204. 10.1002/smi.2446 [DOI] [PubMed] [Google Scholar]
- *Long EC, & Christian MS (2015). Mindfulness buffers retaliatory responses to injustice: A regulatory approach. The Journal of Applied Psychology, 100(5), 1409–1422. 10.1037/apl0000019 [DOI] [PubMed] [Google Scholar]
- *Luethcke CA, McDaniel L, & Becker CB (2011). A comparison of mindfulness, nonjudgmental, and cognitive dissonance-based approaches to mirror exposure. Body Image, 8(3), 251–258. 10.1016/j.bodyim.2011.03.006 [DOI] [PubMed] [Google Scholar]
- Lutz J, Herwig U, Opialla S, Hittmeyer A, Jäncke L, Rufer M, … Brühl AB (2014). Mindfulness and emotion regulation—an fMRI study. Social Cognitive and Affective Neuroscience, 9(6), 776–785. 10.1093/scan/nst043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacCoon DG, Imel ZE, Rosenkranz MA, Sheftel JG, Weng HY, Sullivan JC, … Lutz A (2012). The validation of an active control intervention for Mindfulness Based Stress Reduction (MBSR). Behaviour Research and Therapy, 50(1), 3–12. 10.1016/j.brat.2011.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackenzie CS, Scott T, Mather A, & Sareen J (2008). Older Adults’ Help-Seeking Attitudes and Treatment Beliefs Concerning Mental Health Problems. The American Journal of Geriatric Psychiatry, 16(12), 1010–1019. 10.1097/JGP.0b013e31818cd3be. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Marchiori D, & Papies EK (2014). A brief mindfulness intervention reduces unhealthy eating when hungry, but not the portion size effect. Appetite, 75, 40–45. 10.1016/j.appet.2013.12.009 [DOI] [PubMed] [Google Scholar]
- *McClintock AS, & Anderson T (2013). The Application of Mindfulness for Interpersonal Dependency: Effects of a Brief Intervention. Mindfulness, 6(2), 243–252. 10.1007/s12671-013-0253-3 [DOI] [Google Scholar]
- *Mirams L, Poliakoff E, Brown RJ, & Lloyd DM (2013). Brief body-scan meditation practice improves somatosensory perceptual decision making. Consciousness and Cognition, 22, 348–359. [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, & Group TP (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLOS Medicine, 6(7), e1000097 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mrazek MD, Franklin MS, Phillips DT, Baird B, & Schooler JW (2013). Mindfulness training improves working memory capacity and GRE performance while reducing mind wandering. Psychological Science, 24(5), 776–781. 10.1177/0956797612459659 [DOI] [PubMed] [Google Scholar]
- *Murphy CM, & MacKillop J (2014). Mindfulness as a strategy for coping with cue-elicited cravings for alcohol: an experimental examination. Alcoholism, Clinical and Experimental Research, 38(4), 1134–1142. 10.1111/acer.12322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nisbett RE, & Wilson TD (1977). Telling more than we can know: Verbal reports on mental processes. Psychological Review, 84(3), 231–259. 10.1037/0033-295X.84.3.231 [DOI] [Google Scholar]
- *Nosen E, & Woody SR (2013). Brief psycho-education affects circadian variability in nicotine craving during cessation. Drug & Alcohol Dependence, 132(1), 283–289. 10.1016/j.drugalcdep.2013.02.017 [DOI] [PubMed] [Google Scholar]
- *Ortner M, & Zelazo PD (2014). Responsiveness to a mindfulness manipulation predicts affect regarding an anger-provoking situation. Canadian Journal of Behavioural Science / Revue Canadienne Des Sciences Du Comportement, 46(2), 117–124. 10.1037/a0029664 [DOI] [Google Scholar]
- *Pepping CA, Davis PJ, & O’Donovan A (2015). The Association between State Attachment Security and State Mindfulness. PLoS ONE, 10(3). 10.1371/journal.pone.0116779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Prins B, Decuypere A, & Van Damme S (2014). Effects of mindfulness and distraction on pain depend upon individual differences in pain catastrophizing: An experimental study. European Journal of Pain, 18(9), 1307–1315. 10.1002/j.1532-2149.2014.491.x [DOI] [PubMed] [Google Scholar]
- Rahl HA, Lindsay EK, Pacilio LE, Brown KW, & Creswell JD (2017). Brief mindfulness meditation training reduces mind wandering: The critical role of acceptance. Emotion (Washington, D.C.), 17(2), 224–230. 10.1037/emo0000250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Ramos Díaz NS, Jiménez Jiménez O, & Lopes PN (2014). The role of mindfulness in coping with recollections of acute stressors: a laboratory study. Psicothema, 26(4), 505–510. 10.7334/psicothema2014.71 [DOI] [PubMed] [Google Scholar]
- *Ramsey AT, & Jones EE (2015). Minding the interpersonal gap: Mindfulness-based interventions in the prevention of ostracism. Consciousness and Cognition, 31, 24–34. 10.1016/j.concog.2014.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raudenbush SW (1994). Random effects models. In Cooper H and Hedges LV (eds.), Handbook of Research Synthesis (pp. 301–322). New York: Russell Sage Foundation. [Google Scholar]
- Rennie D (2001). CONSORT revised--improving the reporting of randomized trials. JAMA, 285(15), 2006–2007. [DOI] [PubMed] [Google Scholar]
- *Reynolds LM, Lin YS, Zhou E, & Consedine NS (2015). Does a brief state mindfulness induction moderate disgust-driven social avoidance and decision-making? An experimental investigation. Journal of Behavioral Medicine, 38(1), 98–109. 10.1007/s10865-014-9582-5 [DOI] [PubMed] [Google Scholar]
- Ridner SH (2004). Psychological distress: concept analysis. Journal of Advanced Nursing, 45(5), 536–545. [DOI] [PubMed] [Google Scholar]
- *Rogojanski J, Vettese LC, & Antony MM (2010). Coping with Cigarette Cravings: Comparison of Suppression Versus Mindfulness-Based Strategies. Mindfulness, 2(1), 14–26. 10.1007/s12671-010-0038-x [DOI] [Google Scholar]
- Ruscio AC, Muench C, Brede E, MacIntyre J, & Waters AJ (2016). Administration and Assessment of Brief Mindfulness Practice in the Field: a Feasibility Study Using Ecological Momentary Assessment. Mindfulness, 7(4), 988–999. 10.1007/s12671-016-0538-4 [DOI] [Google Scholar]
- Ruscio AC, Muench C, Brede E, & Waters AJ (2016). Effect of Brief Mindfulness Practice on Self-Reported Affect, Craving, and Smoking: A Pilot Randomized Controlled Trial Using Ecological Momentary Assessment. Nicotine & Tobacco Research, 18(1), 64–73. 10.1093/ntr/ntv074 [DOI] [PubMed] [Google Scholar]
- Rush J, Carmody T, & Reimitz PE (2000). The Inventory of Depressive Symptomatology (IDS)”: Clinician (IDS-C) and Self-Report (IDS-SR) ratings of depressive symptoms. International Journal of Methods in Psychiatric Research, 9, 45–59. [Google Scholar]
- *Sanders WA, & Lam DH (2010). Ruminative and mindful self-focused processing modes and their impact on problem solving in dysphoric individuals. Behaviour Research and Therapy, 48, 747–753. [DOI] [PubMed] [Google Scholar]
- *Sauer SE, & Baer RA (2012). Ruminative and mindful self-focused attention in borderline personality disorder. Personality Disorders: Theory, Research, and Treatment, 3(4), 433–441. 10.1037/a0025465 [DOI] [PubMed] [Google Scholar]
- Sauer-Zavala S, Boswell JF, Gallagher MW, Bentley KH, Ametaj A, & Barlow DH (2012). The Role of Negative Affectivity and Negative Reactivity to Emotions in Predicting Outcomes in the Unified Protocol for the Transdiagnostic Treatment of Emotional Disorders. Behaviour Research and Therapy, 50(9), 551–557. 10.1016/j.brat.2012.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sears S, & Kraus S (2009). I think therefore I om: cognitive distortions and coping style as mediators for the effects of mindfulness meditation on anxiety, positive and negative affect, and hope. Journal of Clinical Psychology, 65(6), 561–573. 10.1002/jclp.20543 [DOI] [PubMed] [Google Scholar]
- Segerstrom SC, & Miller GE (2004). Psychological stress and the human immune system: a meta-analytic study of 30 years of inquiry. Psychological Bulletin, 130(4), 601–630. 10.1037/0033-2909.130.4.601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shadish WR, & Keith C (1994). Combining estimates of effect size. In Cooper H & Hedges LV (Eds.), The handbook of research synthesis (pp. 261–281). New York, NY, US: Russell Sage Foundation. [Google Scholar]
- Shiffman S, Stone AA, & Hufford MR (2008). Ecological Momentary Assessment. Annual Review of Clinical Psychology, 4(1), 1–32. 10.1146/annurev.clinpsy.3.022806.091415 [DOI] [PubMed] [Google Scholar]
- *Shikatani B, Antony MM, Kuo JR, & Cassin SE (2014). The impact of cognitive restructuring and mindfulness strategies on postevent processing and affect in social anxiety disorder. Journal of Anxiety Disorders, 28(6), 570–579. 10.1016/j.janxdis.2014.05.012 [DOI] [PubMed] [Google Scholar]
- *Singer AR, & Dobson KS (2007). An experimental investigation of the cognitive vulnerability to depression. Behaviour Research and Therapy, 45(3), 563–575. 10.1016/j.brat.2006.05.007 [DOI] [PubMed] [Google Scholar]
- Spijkerman MPJ, Pots WTM, & Bohlmeijer ET (2016). Effectiveness of online mindfulness-based interventions in improving mental health: A review and meta-analysis of randomised controlled trials. Clinical Psychology Review, 45, 102–114. 10.1016/j.cpr.2016.03.009 [DOI] [PubMed] [Google Scholar]
- *Ussher M, Cropley M, Playle S, Mohidin R, & West R (2009). Effect of isometric exercise and body scanning on cigarette cravings and withdrawal symptoms. Addiction (Abingdon, England), 104(7), 1251–1257. 10.1111/j.1360-0443.2009.02605.x [DOI] [PubMed] [Google Scholar]
- Verhagen AP, de Vet HC, de Bie RA, Kessels AG, Boers M, Bouter LM, & Knipschild PG (1998). The Delphi list: a criteria list for quality assessment of randomized clinical trials for conducting systematic reviews developed by Delphi consensus. Journal of Clinical Epidemiology, 51(12), 1235–1241. [DOI] [PubMed] [Google Scholar]
- *Verplanken B, & Fisher N (2013). Habitual Worrying and Benefits of Mindfulness. Mindfulness, 5(5), 566–573. 10.1007/s12671-013-0211-0 [DOI] [Google Scholar]
- *Villa CD, & Hilt LM (2014). Brief Instruction in Mindfulness and Relaxation Reduce Rumination Differently for Men and Women. International Journal of Cognitive Therapy, 7(4), 320–333. 10.1521/ijct_2014_07_02 [DOI] [Google Scholar]
- *Vinci C, Peltier MR, Shah S, Kinsaul J, Waldo K, McVay MA, & Copeland AL (2014). Effects of a brief mindfulness intervention on negative affect and urge to drink among college student drinkers. Behaviour Research and Therapy, 59, 82–93. 10.1016/j.brat.2014.05.012 [DOI] [PubMed] [Google Scholar]
- Vitalia IL, & Răban-Motounu N (2014). Immediate Body Experience and Reflexive Awareness. Journal of Experiential Psychotherapy/Revista de PSIHOterapie Experientiala, 17(1). [Google Scholar]
- Wahbeh H, Svalina MN, & Oken BS (2014). Group, One-on-One, or Internet? Preferences for Mindfulness Meditation Delivery Format and their Predictors. Open Medicine Journal, 1, 66–74. 10.2174/1874220301401010066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Wahl K, Huelle JO, Zurowski B, & Kordon A (2012). Managing Obsessive Thoughts During Brief Exposure: An Experimental Study Comparing Mindfulness-Based Strategies and Distraction in Obsessive–Compulsive Disorder. Cognitive Therapy and Research, 37(4). 10.1007/s10608-012-9503-2 [DOI] [Google Scholar]
- *Watford TS, & Stafford J (2015). The impact of mindfulness on emotion dysregulation and psychophysiological reactivity under emotional provocation. Psychology of Consciousness: Theory, Research, and Practice, 2(1), 90–109. 10.1037/cns0000039 [DOI] [Google Scholar]
- Watson D, & Clark LA (1984). Negative affectivity: The disposition to experience aversive emotional states. Psychological Bulletin, 96(3), 465–490. 10.1037/0033-2909.96.3.465 [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, & Carey G (1988). Positive and negative affectivity and their relation to anxiety and depressive disorders. Journal of Abnormal Psychology, 97(3), 346–353. 10.1037/0021-843X.97.3.346 [DOI] [PubMed] [Google Scholar]
- Wells A (2002). GAD, Meta-cognition, and Mindfulness: An Information Processing Analysis. Clinical Psychology: Science and Practice, 9(1), 95–100. 10.1093/clipsy.9.1.95 [DOI] [Google Scholar]
- *Wells A, & Roussis P (2014). Refraining from intrusive thoughts is strategy dependent: a comment on Sugiura, et al. And a preliminary informal test of detached mindfulness, acceptance, and other strategies. Psychological Reports, 115(2). 10.2466/02.PR0.115c21z9 [DOI] [PubMed] [Google Scholar]
- *Yusainy C, & Lawrence C (2015). Brief mindfulness induction could reduce aggression after depletion. Consciousness and Cognition, 33, 125–134. 10.1016/j.concog.2014.12.008 [DOI] [PubMed] [Google Scholar]
- *Zabelina DLR (2011). Manipulating Mindfulness Benefits Creative Elaboration at High Levels of Neuroticism. Empirical Studies of the Arts, 29(2), 243–255. 10.2190/EM.29.2.g [DOI] [Google Scholar]
- Zeidan F, Johnson SK, Diamond BJ, David Z, & Goolkasian P (2010a). Mindfulness meditation improves cognition: evidence of brief mental training. Consciousness and Cognition, 19(2), 597–605. 10.1016/j.concog.2010.03.014 [DOI] [PubMed] [Google Scholar]
- *Zeidan F, Johnson SK, Gordon NS, & Goolkasian P (2010b). Effects of brief and sham mindfulness meditation on mood and cardiovascular variables. Journal of Alternative and Complementary Medicine (New York, N.Y.), 16(8), 867–873. 10.1089/acm.2009.0321 [DOI] [PubMed] [Google Scholar]
- Zoogman S, Goldberg SB, Hoyt WT, & Miller L (2015). Mindfulness Interventions with Youth: A Meta-Analysis. Mindfulness, 6(2), 290–302. 10.1007/s12671-013-0260-4 [DOI] [Google Scholar]
- Zurawski RM, & Smith TW (1987). Assessing irrational beliefs and emotional distress: Evidence and implications of limited discriminant validity. Journal of Counseling Psychology, 34(2), 224–227. 10.1037/0022-0167.34.2.224 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


