Abstract
The Barratt Impulsiveness Scale (BIS-11) is the most widely administered trait impulsiveness questionnaire. Recently a shorter, unidimensional version of the instrument was developed for adults (BIS-Brief). While psychometric characteristics of the BIS-Brief support its use among adults, it also may be more appropriate youth samples than the complete BIS-11 because it less burdensome and omits items about activities not usually encountered by children and adolescents. This manuscript describes a test of psychometric characteristics of the BIS-Brief among youth. To measure a sufficiently wide range of scores, analyses were conducted based on secondary data analysis of datasets pooled from 3 distinct youth cohorts aged 10–17: healthy controls (Control; n = 356); those who had a family history of substance use disorder (FH+; n = 302); and psychiatric inpatients (Patients; n = 322). Model fit for the BIS-Brief was good but varied somewhat depending on the respondent cohort. There was a strong correlation between test and re-test BIS-Brief both within a single day and at 6 months, and also a strong correlation between BIS-Brief and BIS-11 scores. Concurrent validity was supported by correlation with questionnaire measures, which tended to be more robustly associated with BIS-Brief than behavioral measures. Both BIS-Brief and BIS-11 forms were similarly associated with other convergent measures. In conclusion, the BIS-Brief is a shorter version of the BIS-11 that reduces participant burden and with psychometric properties that support its use among youth populations.
Keywords: impulsiveness, adolescent, child, substance use, inpatient
A Test of the Psychometric Characteristics of the BIS-Brief Among Three Groups of Youth
The Barratt Impulsiveness Scale version 11 (BIS-11) is one of the most commonly used self-report forms for measuring impulsive personality traits (Patton, Stanford, & Barratt, 1995). In developing the current 30-item BIS-11, a factor analytic study of the 34-item BIS-10 was conducted in undergraduates (from Baylor University; Waco, TX), psychiatric inpatients with a substance use disorder, psychiatric patients treated for conditions other than substance use disorder, and incarcerated men. These four samples were used to generate a sufficiently wide range of scores (Patton et al., 1995). As a result of these factor analyses, 4 items were omitted for the BIS-11 and 3 distinct second-order factors were identified via principal components analysis: Attentional Impulsiveness, Motor Impulsiveness, and Non-Planning Impulsiveness (Patton et al., 1995).
On the 50th anniversary of the initial BIS (Barratt, 1959), a review was published (Stanford et al., 2009) that reported updated tests of the BIS-11’s psychometric properties (i.e., internal consistency, test-retest reliability, and concurrent validity tests) in total and second-order factors scores in college students (n = 1,178) and adults from the community (n = 399). The review also discussed clinical and personality studies that used the BIS-11. Despite sound psychometric properties of the second-order factors (Patton et al., 1995; Stanford et al., 2009) and a broad appreciation for the multi-faceted nature of the impulsivity construct (Cyders & Coskunpinar, 2011; de Wit, 2009; Dougherty, Mathias, & Marsh, 2003; Lane, Cherek, Rhoades, Pietras, & Tcheremissine, 2003; Ledgerwood, Alessi, Phoenix, & Petry, 2009; Reynolds, Pendfold, & Patak, 2008), the review noted that most research has focused on the BIS-11 total score as a single measure of impulsiveness.
BIS-Brief
Because most research has focused on the BIS-11 total score as a single measure of impulsiveness, an 8-item, unidimensional version of the Barratt Impulsiveness Scale was recently developed and described (Steinberg, Sharp, Stanford, & Tharp, 2013). This version was identified based on a confirmatory multidimensional item response theory (IRT) test of responses to BIS-11 by 1,178 college students. There was satisfactory model fit when testing the sum of BIS-11 items 1, 2, 5, 8, 9, 12, 14, and 19. In the same paper (Steinberg et al., 2013), construct validity of the new BIS-Brief scale scores were tested by differentiating scores of normal adults and a clinical sample of adults with a history of Borderline Personality Disorder or Domestic Violence. Given its satisfactory psychometric properties, the BIS-Brief was subsequently introduced. It was not intended to replace the BIS-11, but an alternative for researchers focused on impulsivity as a unitary construct and in settings where a brief instrument (e.g., large-scale epidemiological studies or in clinical settings) would be more feasible to administer (Steinberg et al., 2013).
These differences in the length and content may make the BIS-Brief more suitable for clinical administration among children and adolescents than the BIS-11. Although the BIS-11 is widely used to test youth (Krishnan-Sarin et al., 2007; Stanford, Greve, Boudreaux, Mathias, & Brumbelow, 1996), it contains several items (e.g., I plan for job security; Item 13) not relevant to most youth. In contrast, the 8-items of the BIS-Brief are all statements pertinent to youth (e.g., item 19 I act on the spur of the moment). Thus, the BIS-Brief might be preferable to the BIS-11 for children and adolescents and preliminary evidence from the original BIS-Brief paper support this application of the instrument. Significant correlations were found between BIS-Brief (and BIS-11) and measures of aggression among both adolescents and young adults (Buss Perry Aggression Questionnaire r’s =.36 to .53; n = 92; ages 13–22; M = 16.7 years; Steinberg et al., 2013). However, further tests among younger than adult populations are needed.
The current study was designed to extend development of the BIS-Brief by further testing its psychometric properties among children and adolescents. We aimed to examine descriptive statistics of the BIS-Brief, along with model fit, test-retest reliability, and association with self-report and behavioral measures of similar constructs among youth. This study is based on a secondary data analysis of three groups of youth: healthy controls (Controls Group), youth with a family history of substance use disorder (FH+ Group), and youth who had recently received inpatient psychiatric care (Patient Group). The groups were sampled to generate a broad range of BIS-Brief scores similar to the process used for the BIS-11 (Patton et al., 1995). Based on previous research (Steinberg et al., 2013), we expected to find satisfactory model fit, test-retest reliability, and associations with self-report measures.
Methods
The BIS-Brief and its relationship with other self-report and behavioral measures was tested in a secondary data analysis of responses by youth. Measures and the respondent cohorts are described below.
Barratt Impulsiveness Scale (BIS-11)
The BIS-11 (Patton, Stanford, & Barratt, 1995; Stanford et al., 2009) is a 30-item self-report measure of impulsive personality traits. For this questionnaire, the frequency of common impulsive (e.g., “I do things without thinking”) or non-impulsive (“I am self-controlled”) behavioral traits are rated on a scale from 1 = Rarely/Never to 4 = Almost Always/Always. Responses across all items are summed to a total score of 30 to 120 points, with higher scores indicating more impulsiveness. Scores on the BIS-11reflect good test-retest reliability (Spearman’s Rho = 0.83) and internal consistency (Cronbach’s α = .83; Stanford et al., 2009).
BIS-Brief.
The BIS-Brief score is the sum of scores from 8 items from the BIS-11 (items 1, 2, 5, 8, 9, 12, 14, and 19), which Steinberg and colleagues (2013) identified as reflecting a unidimensional measure of impulsiveness. In the original study, scores on the BIS-Brief reflected acceptable internal consistency (Cronbach’s α = .78), construct validity was demonstrated by higher BIS-Brief scores among those with Borderline Personality Disorder, and concurrent validity was reflected in significant correlation with measures of aggression (Steinberg et al., 2013). In the present study, youth completed the full 30-item BIS-11 as part of a larger battery, and BIS-Brief scores were computed from this instrument.
Self-Report Measures
Sensation Seeking Scale-Child (SSS-C).
The SSS-C (Russo et al., 1993) was used to assess youth self-ratings of their sensation seeking. In this 26-item self-report measure respondents chose between two opposite statements to determine the tendency to select varied, novel, complex, and intense situations and experiences. For example, “I would like to try jumping from a plane with a parachute” versus “I would never try jumping from a plane with a parachute”. Scores on the SSS-C reportedly demonstrate acceptable internal consistency (Cronbach’s α = .83), split-half reliability (r = .85), while construct validity is supported by a higher SSS-C scores in clinical compared to nonclinical respondents (Russo et al., 1993).
Life History of Aggression (LHA).
The LHA (Coccaro, Berman, & Kavoussi, 1997) is an interview for assessing participation in 11 types of aggressive behaviors (e.g., Temper Tantrums, Physical Assault, etc.). Each LHA item is scored on a 6-point scale (0 = No Events, 1 = One Event, 2 = A Few Events, 3 = Several Events, 4 = Many Events, and 5 = So Many Events they Cannot be Counted). Items scores are summed (range of possible scores is 0–55); higher total scores reflect greater life history of aggressive acts. Internal consistency is generally high for scores on the LHA (Cronbach’s α = .87) and concurrent validity was demonstrated by strong correlations with the Overt Aggression Scale and the Buss-Durkee Hostility Inventory (Coccaro et al., 1997).
Suicide Ideation Questionnaire Junior (SIQ-JR).
The SIQ-JR (Reynolds, 1988) is a 15-item questionnaire for measuring thoughts of suicide among child and adolescent age samples. Items are rated on a 7-point scale ranging from 0 =“I never had this thought” to 6 = a thought occurred “Almost every day”, with higher scores reflecting more frequent suicidal thoughts. SIQ-JR scores show high internal consistency (Cronbach’s α = .94; Reynolds, 1988) and concurrent validity was demonstrated in scores with strong correlations with self-reported depression, anxiety, hopelessness (Reynolds, 1988), and suicide attempts (Reynolds & Mazza, 1999).
Inventory of Callous-Unemotional Traits (ICU).
The ICU (Kimonis et al., 2008) is a 24-item questionnaire for assessing self-ratings of affective and interpersonal styles related to severe conduct problems. Items are rated on a 4-point scale (0 = Not at all True, 1 = Somewhat True, 2 = Very True, and 3 = Definitely True; range of scores 0 −72) and higher scores reflect more callous unemotional traits. ICU scores demonstrate substantial internal consistency (Cronbach’s α = .81; Kimonis et al., 2008) and concurrent validity was demonstrated in scores with strong correlations with self-reported delinquency, school misconduct, and aggression (Kimonis et al., 2008; Ray, Frick, Thornton, Steinberg, & Cauffman, 2015)
Youth Self-Report (YSR).
The YSR is the child self-report form from the Achenbach System of Empirically Based Assessment (ASEBA; Achenbach & Rescorla, 2001), which characterizes self-assessment of experiences across emotional and behavior problems. The YSR includes 112 statements about difficulties in the last 6 months, which are rated on a 3-point scale (0 = Not True, 1 = Somewhat or Sometimes True, or 2 = Very True or Often True). Item responses are summed to yield syndrome scales categorized into domains of Internalizing (i.e., Anxious/Depressed, Withdrawn/Depressed, and Somatic Complaints) and Externalizing (Rule Breaking Behavior and Aggressive Behavior). Raw scores on all scales were converted to gender-and age-normed T-scores using the ASEBA Assessment Data Manager (ASEBA; Burlington, VT). YSR scores are among the most well-validated in assessment of child and adolescent behavior (Achenbach & Rescorla, 2001), with good internal consistency (Cronbach’s α ranges from .71 to .89) and concurrent validity (e.g., Ebesutani et al., 2010).
Conners 3rd Edition (Conners3).
The Conners3 (Conners, 2008) is a self-report questionnaire of child psychopathology. The 39 items are rated on a 4-point scale (0 = Not True at All, 1 = Just a Little True, 2 = Pretty Much True, and 3 = Very Much True) and scored for content scales of Inattention, Hyperactivity, Learning Problems, Family Relations, and Defiance/Aggression. Raw scores are converted to t-scores based on gender and age norms (Conners, 2008). These content scale scores reflect good internal consistency (Cronbach’s α ranges from .92 to .97) and concurrent validity is supported by significant correlation of Conners3 scores with measures of attention, inhibition, aggressive behavior, and social problems (Conners, 2008).
Behavioral Measures
Immediate Memory Task (IMT).
The IMT (Dougherty, Marsh, & Mathias, 2002) tests erroneous responding to stimuli before information processing is complete − a form of response initiation impulsivity. In this computerized task, participants respond to target stimuli (consecutive matching 5-digit numbers) and avoid responding to non-targets, some of which were very similar to the target (matching on 4 of the 5 digits). The proportion of responses for the similar non-targets divided by response rates to target stimuli (IMT Ratio) is interpreted as the measures of response initiation impulsivity (Dougherty et al., 2002). This ratio method is useful for addressing conditions when participants adopt a conservative response strategy, responding to few stimuli, to avoid commission errors (Tannock et al., 1989).
GoStop Impulsivity Paradigm (GoStop).
The GoStop (Dougherty, Mathias, Marsh, & Jagar, 2005) tests failure to withhold an already initiated response, a form of response disinhibition. In this task, participants respond to target “go” stimuli (black consecutive matching numbers), but withhold responding to “stop” cues (consecutive matching number that change color from black to red 50, 150, 250, or 350 msec after the “go” stimulus) that are rapidly displayed on a computer monitor. The proportion of responses for the “stop” cues at the 150 msec interval divided by response rates to “go” stimuli (GoStop Ratio) is interpreted as a measure of response inhibition impulsivity (Dougherty, Marsh-Richard, Hatzis, Nouvion, & Mathias, 2008).
Two Choice Impulsivity Paradigm (TCIP).
The TCIP (Dougherty et al., 2005) tests preference for smaller-more-immediate rewards versus larger-more-delayed rewards. In this computerized task, participants make a series of 50 choices between 5-cent rewards delivered after experiencing a 5-second delay and a 15-cent reward after a 15-second delay (Dougherty et al., 2005). The proportion of responses for the smaller-more-immediate rewards (Proportion Short) is interpreted as consequence sensitivity impulsivity (Dougherty et al., 2005).
Delay Discounting.
Similar to the TCIP, the Delay Discounting task (Kirby, 2009; Kirby, Petry, & Bickel, 1999) assesses choices between smaller-immediate versus larger-delayed monetary choices. In this task, 27 choices are made about differing hypothetical delays for reward, for example, “Would you prefer $20 today or $55 in 7 days?” An average discount rate estimate (k) based on the hyperbolic discounting function of Mazur (1987) is estimated for each participant based on the pattern of choices across all 27 trials. Possible values of k range from 0.00016 (choosing all delayed options) to 0.25 (choosing all immediate options).
Balloon Analogue Risk Task – Youth (BART-Y).
The BART-Y tests risk taking propensity (Lejuez et al., 2002, Lejuez et al., 2007). In this computerized test, participants earn points by inflating a representation of a balloon on a computer screen, but risk losing these earnings if the balloon explodes. Balloons explode after an average of 64 pumps, and participants can stop responding any time before this point to save the points accrued for that trial. The average number of pumps on balloon trials without explosions was the measure of risk taking, with more pumps indicating higher levels of risk-taking (Lejuez et al., 2002, Lejuez et al., 2007).
Performance and Effort Rating.
The Adaptive Visual Analog Scales (AVAS; Marsh-Richard, Hatzis, Mathias, Venditti, & Dougherty, 2009) was used to measure self-perceived performance and effort across the behavioral tasks. This computerized visual analog scale involved marking point on a line (range 1–100%) reflecting the degree of agreement with the following statements: Performance -”Relative to other people your age, how well do you think you did on today’s computer tasks?” and Effort – “Relative to other people your age, how hard did you try on today’s computer tasks?” The Higher ratings reflect perception of better performance and greater effort than peers (Marsh-Richard et al., 2009).
Respondent Cohorts
For the current study, analyses were conducted based on a non-duplicative re-analysis of data pooled from groups of youth completing studies of youth personality, clinical history, and behavior. Participants were paid approximately $10/hour for completing study procedures, and the study protocols was approved by our local Institutional Review Board. A description of each study cohort follows.
Control Group.
The Control group was composed of 356 (n = 152 boys and 204 girls) youth (ages 10–17 years) recruited from the community, who were in good health. Controls were respondents to advertisements for healthy, well-adjusted youth. Absence of psychiatric disorder or major adjustment disorder was tested in separate interviews of the youth participant and the caregiver using psychiatric diagnostic interviews (KSADS-PL; Kiddie-Schedule for Affective Disorders and Schizophrenia for School Age Children-Present and Lifetime Version; Kaufman et al., 1997). Additionally, a subset of these youth (n = 81) had the additional inclusion criterion of no parent, sibling, or grandparent with substance use disorder.
FH+ Group.
The FH+ group was composed of 302 youth (n = 151 boys and 151 girls) (ages 10–12 years) recruited from the community, who had a family history of substance use disorder, but who had not initiated regular substance use themselves. The family history included at least a father with a substance use diagnosis (assessed using the Family History Assessment Module; Janca et al., 1992) and could also include a mother, sibling, or grandparent with a substance use disorder. Absence of regular substance use by youth was verified using the Drug History Questionnaire (DHQ; Dougherty et al., 2013), as well as breathalyzer (AlcoTest® 7110 MKIII C device; Draeger Safety Inc., Durango, CO) and urine drug analyses (Panel/Dip Drugs of Abuse Testing Device; Redwood Biotech, Santa Rosa, CA). FH+ group included those with psychiatric diagnoses, the proportion with disorder were: 29% Attention Deficit Hyperactivity Disorder; 9% Oppositional Defiant Disorder; 16 % Anxiety Disorder; and 1% Conduct Disorder. These DSM-IV diagnoses were made by a board-certified child and adolescent psychiatrist based responses to the KSADS-PL (Kaufman et al., 1997) administered in full, separately to the adolescent and a parent/caregiver. Only Substance Use Disorder was exclusionary because this cohort was drawn from a larger study testing impulsivity in youth prior to regular substance use onset (Dougherty et al., 2015).
Patient Group.
The Patient group was composed of 322 (n = 159 boys and 163 girls) adolescents (ages 12 – 17 years) who had recently received inpatient psychiatric care. Patients were enrolled during their inpatient stay and were assessed approximately 2 weeks after discharge from care. Patients had a median of 2 psychiatric diagnoses; rates were: 56% Depressive Disorder; 47% Disruptive Behavior Disorders; 46% Attention Deficit Hyperactivity Disorder; 32 % Anxiety Disorder; 26% Substance Use Disorder; 10% Bipolar Disorder; and 6% Eating Disorder. These DSM-IV diagnoses were made by a board-certified child and adolescent psychiatrist based review of their medical record and the full KSADS-PL (Kaufman et al., 1997) administered separately to both the adolescent and a parent/caregiver.
Data Analyses
Descriptive statistics were computed for BIS-Brief scores, including: average, standard deviation, 95% confidence interval of the mean, skewness, and kurtosis. A p-value was computed using the skewness and kurtosis test for normality (Royston, 1991). The distribution of the sum of the 8-items in the BIS-Brief (Steinberg et al., 2013) and model fit statistics were examined separately by cohort using a graded response model under the Item Response Theory (IRT) paradigm. An IRT approach allowed us to test the goodness of fit of an existing instrument in new populations. A good model fit is supported by M2* p values > .05 (Cai & Hansen, 2013; Eagle, 2015), root mean square error of approximation (RMSEA) < .08 (Reise & Revicki, 2014), Tucker-Lewis Index > 0.9 (Bentler & Bonett, 1980), or comparative fit index scores > 0.95 (Bentler, 1990). Model fit statistics were calculated using the M2* function from the R mirt package (version 3.1.3; Chalmers, 2012).
The association of BIS-Brief scores were retested both within a single day and 6 months interval. The test-retest comparisons of the BIS-Brief scores were first examined using the Pearson product-moment correlation. Then, paired-samples t-tests were conducted to examine differences between the two BIS-Brief scores. Finally, to account for variations in the amount of time between the two tests, a linear regression model was used with the second BIS-Brief score as the response variable and the first BIS-Brief score, time between the two tests and the interaction between the first BIS-Brief score, and the time between two tests as the explanatory variables. Based on this linear regression model, the agreement between the two BIS-Brief scores for a given value of time between two tests was assessed by testing the null hypotheses that the intercept is 0 and the slope is 1.
Correlation coefficients and corresponding 95% confidence intervals were used to test the relationship of BIS-Brief scores with questionnaire and behavioral measures to determine concurrent validity. The same tests were conducted to test the relationship with the BIS-11 to provide a frame of reference for interpreting the magnitude of relationships observed with the BIS-Brief.
Results
Central Tendency and Model Fit
Across all participants, the omnibus mean of BIS-Brief scores was 17.43 (SD = 4.92). There were no significant gender differences in BIS-Brief scores (boys n = 462, M = 17.42, SD = 4.67; girls n = 518, M = 17.45, SD = 5.14; t978 = 0.09, p = .928). There was also step-wise increase in BIS-Brief scores from Control, to FH+, and to the Patient groups (F2,977 = 224.90, p < .001; see Table 1, top panel). The distribution of the BIS-Brief scores was approximately normal for all groups (all p ≥ 0.05). Generally, the model fit was acceptable for each population tested (Table 1, bottom panel). Graded response models for the FH+ and Patients had acceptable to adequate fit across the various model fit indices, except for the Tucker-Lewis Index for the Patient group. While the Control group achieved good fit on the comparative fit index and RMSEA, it was marginal on M2* statistic and Tucker-Lewis Index. Range restriction may be why the Control group had a less robust fit than the FH+ and Patient groups.
Table 1.
Distribution of BIS-Brief Scores and Model Fit Statistics
| Control Group n = 356 | FH+ Group n = 302 | Patient Group n = 322 | |
|---|---|---|---|
| Mean | 14.87 | 16.35 | 21.29 |
| Standard Deviation | 3.55 | 4.27 | 4.42 |
| 95% CI of the mean | 14.80 to 15.23 | 15.87 to 16.84 | 20.80 to 21.34 |
| Skewness | .33 | .33 | -.15 |
| Kurtosis | .04 | -.12 | -.31 |
| p-value* | 0.05 | 0.06 | 0.24 |
| M2* (4) | 10.66 | 5.75 | 6.04 |
| M2* (4) p-value | 0.03 | 0.20 | 0.20 |
| RMSEA | 0.07 | 0.04 | 0.04 |
| 90% CI of RMSEA | 0.02 to 0.12 | 0.0 to 0.1 | 0.0 to 0.1 |
| Tucker-Lewis Index | 0.87 | 0.93 | 0.88 |
| Comparative Fit Index | 0.96 | 0.98 | 0.96 |
Note. RMSEA = root mean square error of approximation.
p-value computed using the skewness and kurtosis test for normality (Royston, 1991).
Reliability and Stability
There was a strong linear relationship between BIS-Brief scores collected twice within a single day (r = 0.74, 95% CI = 0.68–0.79; p < .001; n = 303; see Figure 1, left panel). The magnitude of this correlation was similar to the long-term stability of responses assessed at 6-months (r = 0.72, 95% CI = 0.68–0.76; p < .001; n = 591; see Figure 1, right panel). This second BIS-Brief was collected from 591 adolescents about 6 months after the initial assessment (M = 6.33 months, SD = 0.58). Omnibus mean scores for this second BIS-Brief was 17.91 (SD = 5.06), which was significantly lower than the first assessment (t590 = 2.51, p = .012). There was a negative relationship between time and agreement between the two BIS-Brief scores; after adjusting for days between the first and second assessments (range: 133 to 240 days) stability decreased with increasing time (at 130 days: intercept [95% CI] = 0.40 [−3.49, 4.30], slope [95% CI] = 0.93 [0.72, 1.14]; at 180 days: intercept [95% CI] = 3.98 [2.73, 5.24], slope [95% CI] =0.76 [0.69, 0.82]; and at 240 days: intercept [95% CI] = 8.28 [5.06, 11.49], slope [95% CI] = 0.55 [0.38, 0.72]).
Figure 1.
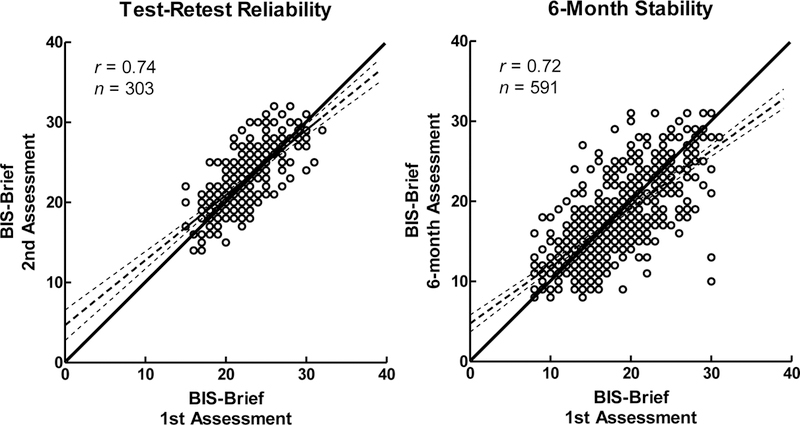
Scatterplot of Test-Retest Reliability within a Single Day (left panel) and Stability Across 6 Months (right panel).
Lines: Solid = 45%, large dashes = linear trend; small dashes = 95% confidence interval.
BIS-Brief and Concurrent Validity – Questionnaires
As expected, BIS-11 scores and BIS-Brief scores were strongly related. Average BIS-11 across the groups were 66.11 (SD = 11.83). There was a significant positive linear relationship between BIS-Brief and BIS-11 scores (r = 0.88, 95% CI = 0.86–0.89, p < .001; see Figure 2). There were significant relationship between BIS-Brief and BIS-11 subscale scores (Attentional r = 0.77, 95% CI = 0.74–0.79, p < .001; Motor r = 0.58, 95% CI = 0.54–0.62, p < .001; and NonPlanning r = 0.76, 95% CI = 0.73–0.78, p < .001).
Figure 2.
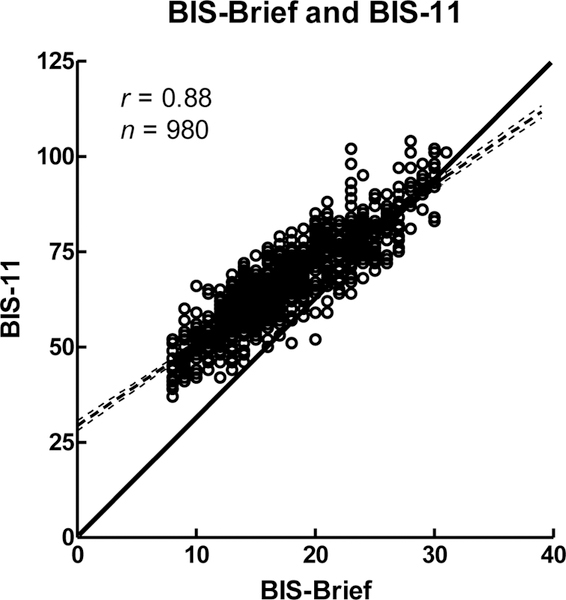
Scatterplot of BIS-Brief Total Scores by BIS-11 Total Scores.
Lines: Solid = 45%, large dashes = linear trend; small dashes = 95% confidence interval.
Table 2 shows correlations of BIS-Brief with other convergent measures and with BIS-11 scores as a referent. Higher BIS-Brief scores were positively related with higher scores on measures of aggression (LHA and Conners3), inattention and hyperactivity (Conners3), externalizing (ASEBA), callous unemotional traits (ICU), and learning problems (ASEBA). More moderate positive correlations were observed for sensation seeking (SSS), suicidal ideation (SIQ Jr), internalizing (ASEBA), and problems with family relations (Conners3). The magnitude of correlations with convergent measures was similar for the BIS-Brief and BIS-11 scores.
Table 2.
Correlations between BIS-Brief and BIS-11 Scores and Self-Report Convergent Validity Measures
| BIS-11 |
BIS-Brief |
||
|---|---|---|---|
| Questionnaire/Scale | Mean (SD) | r [95% CI] p, n | r [95% CI] p, n |
| Sensation Seeking Scale | 10.72 (4.75) |
.24 [.14, .33] < .001; 383 |
.29 [.19, .38] < .001; 383 |
| Life History of Aggression | 11.86 (11.49) |
.57 [.52, .61] < .001; 893 |
.58 [.54, .62] < .001; 893 |
| Suicide Ideation Questionnaire JR | 17.86 (20.18) |
.34 [.25, .42] < .001; 437 |
.37 [.29, .45] < .001; 437 |
| Inventory of Callous Unemotional Traits | 19.81 (7.81) |
.44 [.36, .52] < .001; 400 |
.45 [.37, .53] < .001; 400 |
| ASEBA Youth Self-Report | |||
| Externalizing | 44.99 (10.00) |
.47 [.39, .54] < .001; 446 |
.48 [.40, .55] < .001; 446 |
| Internalizing | 48.41 (10.18) |
.39 [.30, .46] < .001; 446 |
.30 [.21, .38] < .001; 446 |
| Conners3 | |||
| Inattention | 54.19 (13.38) |
.63 [.57, .69] < .001; 401 |
.57 [.50, .64] < .001; 401 |
| Hyperactivity | 55.07 (12.62) |
.62 [.55, .67] < .001; 401 |
.59 [.52, .65] < .001; 401 |
| Learning Problems | 53.01 (12.20) |
.50 [.42, .57] < .001; 401 |
.45 [.37, .53] < .001; 401 |
| Family Relations | 49.02 (9.34) |
.36 [.28, .45] < .001; 401 |
.36 [.27, .44] < .001; 401 |
| Defiance/Aggression | 51.13 (12.10) |
.48 [.40, .55] < .001; 401 |
.47 [.39, .54] < .001; 401 |
Note. ASEBA = Achenbach System of Empirically Based Assessment; Conners3 = Conners 3rd Edition.
BIS-Brief and Concurrent Validity – Behavioral Measures
Like the questionnaires, there were non-zero correlations between the BIS-Brief and behavioral measures (Table 3). Except for the measure of risk taking (BART-Y), behavioral measures were significantly, positively associated with the BIS-Brief score. The magnitude of the correlations was smaller than for the questionnaire measures and somewhat smaller for the BIS-Brief than BIS-11 scores. Finally, when asked to rate their performance on the behavioral measures (AVAS), respondents’ judgment of how well they performed (Performance) and how much effort they exerted on the behavioral tasks (Effort), both decreased with high BIS-Brief scores.
Table 3.
Correlations between BIS-Brief and BIS-11 Scores and Performance-Based Construct Validity Measures
| BIS-11 |
BIS-Brief |
||
|---|---|---|---|
| Mean (SD) |
r [95% CI] p, n | r [95% CI] p, n | |
| IMT Ratio | 62.60 (17.61) |
.14 [.08, .20] < .001; 974 |
.12 [.06, .18] < .001; 974 |
| GoStop Ratio | 48.66 (25.53) |
.14 [.08, .20] < .001; 976 |
.10 [.04, .16] .002; 976 |
| TCIP Proportion Short | 0.30 (0.23) |
.16 [.10, .22] < .001; 977 |
.12 [.05, .18] < .001; 977 |
| Delay Discounting, Average K | .05 (0.60) |
.12 [.02, .22] .02; 383 |
.11 [.01, .21] .03; 383 |
| BART-Y Adjusted Average Pumps | 32.48 (13.26) |
-.02 [−.12, .08] .88; 381 |
-.01 [−.11, .09] .88; 381 |
| AVAS Performance | 63.82 (22.34) |
-.34 [−.40, −.28] < .001; 860 |
-.35 [−.40, −.29] < .001; 860 |
| AVAS Effort | 76.76 (23.17) |
-.15 [−.21, −.08] < .001; 860 |
-.16 [−.22, −.09] < .001; 860 |
Note. AVAS = Adaptive Visual Analog Scales; BART-Y = Balloon Analogue Risk Task – Youth; GoStop = GoStop Impulsivity Paradigm; IMT = Immediate Memory Task; TCIP = Two Choice Impulsivity Paradigm.
Age, Puberty, and BIS-Brief
There was a positive relationship between BIS-Brief score and age (r = 0.15; 95% CI = 0.09–0.21; p < .001); for every 1-year increase in age (between subjects), BIS-Brief score increased by 0.36 points (t978= 5.17, p < 0.001). There was also a positive relationship between the BIS-Brief score and pubertal development (r = 0.27; 95% CI = 0.21–0.33; p < .001). For every 1-unit increase in the Pubertal Development Scale (PDS; Petersen, Crockett, Richards, & Boxer, 1988) score, there was a 0.81-point increase in BIS-Brief scores (t817= 8.06, p < 0.001). When considering both explanatory variables simultaneously, a significant relationship of BIS-Brief scores with PDS remained after adjusting for age: for every 1-unit increase in PDS, there was a 0.38-point increase in BIS-Brief scores (t816= 2.78, p < 0.001). Similar relationship were observed for BIS-11 scores with age (r = 0.15; 95% CI = 0.09–0.22; p < .001) and pubertal development (r = 0.27; 95% CI = 0.21–0.33; p < .001).
Discussion
This study tested psychometric characteristics of the BIS-Brief among youth. Generally, average scores were similar to those reported with adult samples. In addition, BIS-Brief scores increased both with age and pubertal development. Model fit for the BIS-Brief ranged from acceptable to good, depending on the respondent cohort (Control, FH+, or Patients). There was a strong relationship between BIS-Brief scores when administered twice within a single day and 6 months later, as well as strong correlations between BIS-Brief and BIS-11 scores. Concurrent validity was supported by correlations with other questionnaire scores, which tended to be more robustly associated with BIS-Brief than behavioral measures. The BIS-Brief and BIS-11 both showed similar associations with convergent measures.
Descriptive Statistics and Developmental Context
The average BIS-Brief score was 17.43, but varied widely by respondent cohort. As anticipated, scores significantly increased with risk and functional impairment: healthy control respondents had the lowest self-reported impulsiveness, youth at risk for substance use because of their family history (FH+) had significantly higher BIS-Brief scores than controls, and adolescents already impacted by psychiatric disorder (Patients) had the highest average levels of self-reported impulsiveness. Compared to previous reports of BIS-Brief scores, our youth samples scored slightly higher in impulsiveness. For instance, our adolescent healthy controls had a BIS-Brief mean score of 14.87 (SD = 3.55), compared to the mean score of 13.49 (SD = 3.09) in healthy adults reported by Steinberg and colleagues (2013). This same pattern was observed with the BIS-11 were our groups had higher scores than the Steinberg study. Similarly, our Patient sample had a slightly higher average BIS-Brief score (M = 21.29; SD = 4.42) than was reported for mixed groups of adolescent and young adult inpatients (M = 20.57, SD = 5.19, N = 92; Steinberg et al., 2013) and incarcerated adults or prisoners mandated to substance abuse treatment or inpatient treatment (M = 18.76, SD = 4.20; N = 1,920; Fields et al., 2015). This small increase in self-reported impulsiveness may be explained by the younger age of our samples.
Cross-sectionally, we observed an increase in BIS-Brief scores with both increasing age and increasing pubertal development, even after accounting for age. The magnitude of this effect was modest: at this rate (i.e., BIS-Brief +0.36 points/year), it would take about 13.6 years of development to result in a full standard deviation increase in impulsiveness. This implies that over time, our samples could be on a trajectory to become even more disparate from the previously reported means. However, social neuroscience theories of development suggest this trend may reverse by later adolescence or early adulthood. For instance, the Dual Systems Model (Steinberg, 2008) suggests that early adolescence is accompanied by markedly increased sensitivity to incentives, novelty, and sensation seeking, which more gradually comes under restraint of cognitive control systems later in adolescence. These two processes are suggested to be the result of separate neural systems (for review see Leshem, 2016) and their interaction may account for adolescents’ engagement in risky behaviors (Steinberg, 2008). The BIS-Brief may be influenced by the combined developmental effects of these two systems. Given that the average age of the current sample is 13 years, our respondents were tested at the developmental stage predicted to show a rise in risky behaviors, consistent with the observed positive relationship of BIS-Brief scores with age and pubertal development. However, how the construct measured by the BIS-Brief corresponds to concepts of the Dual Systems Model remains to be determined.
The social neuroscience research on development of risk, reward, and impulsiveness have primarily been studied using neuroscience and/or imaging techniques on “neurotypical” youth (Bjork & Pardini, 2015; p. 59). Extending these concepts to account for atypical developmental patterns may elucidate why impulsive, disruptive behaviors are concentrated in subgroups of adolescents. Large-scale longitudinal studies of individual differences in healthy youth and those with behavioral disorders are needed, to account for changes in brain maturation and “real-world” behaviors (Bjork & Pardini, 2015; p. 61). For such studies, participant burden is a concern; therefore, brief measures of impulsiveness, like the BIS-Brief or other complementary measures of impulsive behaviors (short version UPPS-P Impulsive Behavior Scale; Cyders, Littlefield, Coffee, & Karyadi, 2013) could be valuable in such contexts. From our experience in the preparation of an application for the Adolescent Cognitive Development Study (ABCD; National Institutes of Health, 2015), it was clear that the consortia sought to select instruments that were brief/low-burden, repeatable, and psychometrically sound for adolescent behavioral risk. Given the psychometric properties of the BIS-Brief observed in the current study, it meets these criteria.
Model Fit
Model fit was generally supported for the groups we tested, although they varied in the proportion of fit criteria met. The FH+ sample had good model fit across all statistical tests, supporting use of the BIS-Brief for youth (ages 10–12) at risk for substance use development. The adolescent Patient group (12–17 years) similarly showed good model fit on all scales except for the Tucker-Lewis Index, which was marginally close to the recommended cut-off (BIS-Brief score .88, cut-off > 0.9). Finally, the Control group had good fit for RMSEA and Comparative Fit Index criteria, but not M2* p-value (score .03, cut-off > 0.5) and Tucker-Lewis Index (score .87, cut-off > 0.9), although the latter was marginally near the recommended cut-off. This pattern of scores supports use of the BIS-Brief to measure self-reported impulsiveness in youth from ages 10–17 and in mixed groups of adolescents, with confidence in the accuracy of assessment increasing for “at-risk” or “affected” populations of youth.
Of our three samples, the Control group was most similar to the undergraduate student sample used for the first BIS-Brief publication (Steinberg et al., 2013). Since then, tests of fit for the 8-item BIS-Brief have had mixed results; acceptable fit was found for at least some metrics among adult low-and high-risk alcohol users (Morean et al., 2014), but not among adult smokers who were treatment seekers (Morean et al., 2014), or adult prisoners and those adjudicated to substance abuse treatment (Fields et al., 2015). To address these mixed results, Morean and colleagues (2014) propose a repository of data for larger-scale analyses. If the research community embraces this solution, differential fit across divergent homogenous subsamples must be addressed within the larger heterogeneous population.
Concurrent Validity
There was substantial similarity between the BIS-11 and BIS-Brief scores correlations with other self-report and performance-based measures. Generally, the magnitude of correlations were within a few percentage points (Median difference in r = .03 for self-report measures and .01 for performance-based measures), and neither was consistently larger in association than the other. In examining the pattern of association with self-report, there were large correlations with measures of aggression and symptoms of ADHD and moderate correlations with sensation seeking, internalizing, and suicidal ideation. This pattern is consistent with earlier reports of the BIS-Brief (Steinberg et al., 2013) and BIS-11 (Stanford et al., 2009). In contrast, the magnitude of correlations of the BIS-Brief with behavioral measures of impulsivity was small (r’s < .14) and similar in strength to previous BIS-11 results in college students and healthy adults from the community (Stanford et al., 2009). The less robust relationships with performance-based measures might reflect differences between trait measures like the BIS-Brief and the more state-sensitive performance-based measures (e.g., Cyders & Coskunpinar, 2011; Lane et al., 2003; Ledgerwood et al., 2009; Marsh, Dougherty, Mathias, Moeller, & Hicks, 2002; Reynolds et al., 2008).
Limitations
Interpretation of these results must be considered within the limitations of this study. Clearer interpretation of the age/pubertal relationship would be evident had a longitudinal design been used. While adequate, the sample size was on the lower end for a test of model fit, and not all participants completed all measures used for tests of concurrent validity. Model fit did vary somewhat by group; thus, our results might not generalize to adolescent samples with different characteristics than our three groups. Additionally, respondents were between ages 10 and 17 years, and thus our findings may not generalize to younger or older populations. Further, this study relied exclusively on self-report and youth performance measures; reports from other observers or official records (e.g., disciplinary citations) would be useful for testing concurrent validity. Finally, this report is a post-hoc reanalysis, and was not originally collected with the intent to test predictive validity for health consequences of impulsiveness.
Conclusions
The BIS-Brief is a shorter version of the BIS-11 instrument; it reduces participant burden and omits items related to activities not typically encountered in adolescence. The psychometric properties of the BIS-Brief in the samples we tested support its use among certain adolescent populations.
Public Significance Statement.
The BIS-Brief is a shorter version of the BIS-11; it reduces participant burden and omits items about activities not typically encountered in adolescence. The psychometric properties of the BIS-Brief support its use among certain adolescent populations.
Acknowledgments
Research reported in this publication was supported by the National Institutes of Health [award numbers R01DA026868; R01DA033997; R01MH077684; and R01MH081181; and T32DA031115]. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Dr. Donald M. Dougherty also gratefully acknowledges support from a research endowment, the William and Marguerite Wurzbach Distinguished Professor. Dr. Ashley Acheson gratefully acknowledged support from the Arkansas Biosciences Institute.
Footnotes
There are no conflicts of interest to declare.
Contributor Information
Charles W. Mathias, Department of Psychiatry, The University of Texas Health Science Center at San Antonio.
Matthew S. Stanford, Hope and Healing Center
Yuanyuan Liang, Department of Epidemiology & Biostatistics, The University of Texas Health Science Center at San Antonio, Department of Epidemiology & Public Health, University of Maryland School of Medicine..
Martin Goros, Department of Epidemiology & Biostatistics, The University of Texas Health Science Center at San Antonio..
Nora E. Charles, Department of Psychiatry, The University of Texas Health Science Center at San Antonio, Department of Psychology, The University of Southern Mississippi.
Arielle H. Sheftall, Department of Psychiatry, The University of Texas Health Science Center at San Antonio, Research Institute at Nationwide Children’s Hospital and the Department of Pediatrics, The Ohio State University College of Medicine.
Jillian Mullen, Department of Psychiatry, The University of Texas Health Science Center at San Antonio, EASL International Liver Foundation; Geneva, CH. Ashley Acheson is now at the Department of Psychiatry and Behavioral Sciences, University of Arkansas for Medical Sciences..
Nathalie Hill-Kapturczak, Department of Psychiatry, The University of Texas Health Science Center at San Antonio..
Ashley Acheson, Department of Psychiatry, The University of Texas Health Science Center at San Antonio..
Rene L. Olvera, Department of Psychiatry, The University of Texas Health Science Center at San Antonio.
Donald M. Dougherty, Department of Psychiatry, The University of Texas Health Science Center at San Antonio.
References
- Achenbach TM, & Rescorla LA (2001). Manual for the ASEBA school-aged forms & profiles Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families. [Google Scholar]
- Barratt ES (1959). Anxiety and impulsiveness related to psychomotor efficiency. Perceptual and Motor Skills, 9, 191–198. [Google Scholar]
- Bentler PM (1990). Comparative fit indexes in structural models. Psychological Bulletin, 107, 237–246. [DOI] [PubMed] [Google Scholar]
- Bentler PM, & Bonett DG (1980). Significance tests and goodness of fit in the analyses of covariance structures. Psychological Bulletin, 88, 588–606. [Google Scholar]
- Bjork JM, & Pardini DA (2015). Who are those “risk-taking adolescents”? Individual differences in developmental neuroimaging research. Developmental Cognitive Neuroscience, 11, 56–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buss AH, & Perry MP (1992). The aggression questionnaire. Journal of Personality and Social Psychology, 63, 452–459. [DOI] [PubMed] [Google Scholar]
- Cai L, & Hansen M (2013). Limited-information goodness-of-fit testing of hierarchical item factor models. British Journal of Mathematical and Statistical Psychology, 66, 245–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chalmers RP (2012). mirt: A multidimensional item response theory package for the R environment. Journal of Statistical Software, 48, 1–29. [Google Scholar]
- Coccaro EF, Berman ME, & Kavoussi RJ (1997). Assessment of life history of aggression: Development and psychometric characteristics. Psychiatry Research, 73, 147–157. [DOI] [PubMed] [Google Scholar]
- Conners CK (2008). Conners 3rd Edition North Tonawanda, NY: Multi-Health Systems, Inc. [Google Scholar]
- Cyders MA, & Coskunpinar A (2011). Measurement of constructs using self-report and behavioral lab tasks: Is there overlap in nomothetic span and construct representation for impulsivity? Clinical Psychology Review, 31, 965–982. [DOI] [PubMed] [Google Scholar]
- Cyders MA, Littlefield AK, Coffee S & Karyadi KA (2014). Examination of a short English version of the UPPS-P Impulsive Behavior Scale. Addictive Behaviors, 39, 1372–1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Wit H (2009). Impulsivity as a determinant and consequence of drug use: A review of underlying processes. Addiction Biology, 14, 22–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dougherty DM, Lake SL Mathias CW, Ryan SR, Bray BC, Charles NE, & Acheson A (2015). Behavioral impulsivity and risk-taking trajectories across early adolescence in youths with and without family histories of alcohol and drug use disorders. Alcoholism: Clinical and Experimental Research, 39, 1501–1509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dougherty DM, Marsh DM, & Mathias CW (2002). Immediate and Delayed Memory Tasks: A computerized measure of memory, attention, and impulsivity. Behavior Research Methods, Instruments, and Computers, 34, 391–398. [DOI] [PubMed] [Google Scholar]
- Dougherty DM, Marsh-Richard DM, Hatzis ES, Nouvion SO, & Mathias CW (2008). A test of alcohol dose effects on multiple behavioral measures of impulsivity. Drug and Alcohol Dependence, 96, 111–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dougherty DM, Mathias CW, Dawes MA, Furr RM, Charles NE, Liguori A, Shannon EE, & Acheson A (2013). Impulsivity, attention, memory, and decision-making among adolescent marijuana users. Psychopharmacology, 226, 307–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dougherty DM, Mathias CW, & Marsh DM (2003). Laboratory measures of impulsivity. In Coccaro EF (Ed.), Aggression: Psychiatric Assessment and Treatment. Medical Psychiatric Series No. 22 (pp. 247–265). New York: Marcel Dekker Publishers. [Google Scholar]
- Dougherty DM, Mathias CW, Marsh DM, & Jagar AA (2005). Laboratory behavioral measures of impulsivity. Behavior Research Methods, Instruments, and Computers, 37, 82–90. [DOI] [PubMed] [Google Scholar]
- Eagle MM (2015). Assessing differential item functioning across clinical and community samples in the Miller Forensic Assessment of Symptoms Test (unpublished doctoral dissertation) University of Houston, TX: Retrieved from https://repositories.tdl.org/uh-ir/bitstream/handle/10657/1149/EAGLE-DISSERTATION-2015.pdf?sequence=1&isAllowed=y [Google Scholar]
- Ebesutani C, Bernstein A, Nakamura BJ, Chorpita BF, Higa-McMillan CK, & Weisz JR (2010). Concurrent validity of the Child Behavior Checklist DSM-Oriented Scales: Correspondence with DSM diagnoses and comparison to Syndrome Scales. Journal of Psychopathology and Behavioral Assessment, 32, 373–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fields S, Edens JF, Smith ST, Rulseh A, Donnellan MB, Ruiz MA, McDermott BE, & Douglas KS (2015). Examining the psychometric properties of the Barratt Impulsiveness Scale-Brief Form in justice-involved samples. Psychological Assessment, 27, 1211–1218. [DOI] [PubMed] [Google Scholar]
- Janca A, Bucholz K, & Janca I (1992). Family History Assessment Module St. Louis: Washington University School of Medicine. [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, & Ryan N (1997). Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry, 36, 980–988. [DOI] [PubMed] [Google Scholar]
- Kirby KN (2009). One-year temporal stability of delay-discount rates. Psychonomic Bulletin & Review, 16, 457–462. [DOI] [PubMed] [Google Scholar]
- Kirby KN, Petry NM, & Bickel WK (1999). Heroin addicts have higher discount rates for delayed rewards than non-drug-using controls. Journal of Experimental Psychology: General, 128, 78–87. [DOI] [PubMed] [Google Scholar]
- Kimonis ER, Frick PJ, Skeem JL, Marsee MA, Cruise K, Munoz LC, Aucoin KJ, & Morris AS (2008). Assessing callous-unemotional traits in adolescent offenders: Validation of the Inventory of Callous-Unemotional Traits. International Journal of Law and Psychiatry, 31, 241–252. [DOI] [PubMed] [Google Scholar]
- Krishnan-Sarin S, Reynolds B, Duhig AM, Smith A, Liss T, McFetridge A, Cavallo DA, Carroll KM, & Potenza MN (2007). Behavioral impulsivity predicts treatment outcome in a smoking cessation program for adolescent smokers. Drug and Alcohol Dependence, 88, 79–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lane SD, Cherek DR, Rhoades HM, Pietras CJ, & Tcheremissine OV (2003). Relationships among laboratory and psychometric measures of impulsivity: Implications in substance abuse and dependence. Addictive Disorders and Their Treatment, 2, 33–40. [Google Scholar]
- Ledgerwood DM, Alessi SM, Phoenix N, & Petry NM (2009). Behavioral assessment of impulsivity in pathological gamblers with and without substance use disorder histories versus healthy controls. Drug and Alcohol Dependence, 105, 89–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lejuez CW, Aklin W, Daughters S, Zvolensky M, Kahler C, & Gwadz M (2007). Reliability and validity of the youth version of the Balloon Analogue Risk Task (BART-Y) in the assessment of risk-taking behavior among inner-city adolescents. Journal of Clinical Child and Adolescent Psychology, 36, 106–111. [DOI] [PubMed] [Google Scholar]
- Lejuez CW, Read JP, Kahler CW, Richards JB, Ramsey SE, Stuart GL, Strong DR, & Brown RA (2002). Evaluation of a behavioral measure of risk taking: the Balloon Analogue Risk Task (BART). Journal of Experimental Psychology: Applied, 8, 75–84. [DOI] [PubMed] [Google Scholar]
- Leshem R (2016). Using dual process models to examine impulisivity throughout neural maturation. Developmental Neuropsychology, 1–2, 125–143. [DOI] [PubMed] [Google Scholar]
- Marsh DM, Dougherty DM, Mathias CW, Moeller FG, & Hicks LR (2002). Comparisons of women with high and low trait impulsivity using behavioral models of response-disinhibition and reward-choice. Personality and Individual Differences, 33, 1291–1310. [Google Scholar]
- Marsh-Richard DM, Hatzis ES, Mathias CW, Venditti N, & Dougherty DM (2009). The Adaptive Visual Analog Scales (AVAS): A modifiable software program for the creation, administration, and scoring of visual analog scales. Behavior Research Methods, 41, 99–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazur JE (1987). An adjusting procedure for studying delayed reinforcement. In Commons MD, Mazure JE, Nevin JA, and Rachlin H (Eds.), Quantitative analysis of behavior: Vol 5 The effect of delay and of intervening events on reinforcement value (pp. 55–73). Hillsdale, NJ.: Erlbaum. [Google Scholar]
- Morean ME, DeMartini KS, Leeman RF, Pearlson GD, Anticevic A, Krishnan-Sarin S, Krystal JH, & O’Malley SS (2014). Psychometrically improved, abbreviated versions of three classic measures of impulsivity and self-control. Psychological Assessment, 26, 1003–1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institutes of Health. (2015). Adolescent Brain Cognitive Development (ABCD) Study -Research Project Sites (U01) -RFA-DA-15–015 Retrieved from https://grants.nih.gov/grants/guide/rfa-files/RFA-DA-15-015.html
- Patton JH, Stanford MS, & Barratt ES (1995). Factor structure of the Barratt Impulsiveness Scale. Journal of Clinical Psychology, 51, 768–774. [DOI] [PubMed] [Google Scholar]
- Petersen AC, Crockett L, Richards M, & Boxer A (1988). A self-report measure of pubertal status: Reliability, validity, and initial norms. Journal of Youth and Adolescence, 17, 117–133. [DOI] [PubMed] [Google Scholar]
- Ray JV, Frick PJ, Thornton LC, Steinberg L, & Cauffman E (2015). Positive and negative item wording and its influence on the assessment of Callous-Unemotional Traits. Psychological Assessment, 28, 394–404. [DOI] [PubMed] [Google Scholar]
- Reise SP, & Revicki DA (2014). Chapter 8: Handbook of item response theory modeling: Applications to typical performance assessment (1st ed). New York: Routledge. [Google Scholar]
- Reynolds W (1988). Suicidal Ideation Questionnaire: Professional Manual Odessa, FL: Psychological Assessment Resources. [Google Scholar]
- Reynolds W, & Mazza J (1999). Assessment of suicidal ideation in inner-city children and young adolescents: Reliability and validity of the Suicidal Ideation Questionnaire-JR. School Psychology Review, 28, 17–30. [Google Scholar]
- Reynolds B, Pendfold RB, & Patak M (2008). Dimensions of impulsive behavior in adolescents: laboratory behavioral assessments. Experimental and Clinical Psychopharmacology, 16, 124–131. [DOI] [PubMed] [Google Scholar]
- Royston P (1991). sg3.5: Comment on sg3.4 and an improved D’Agostino test. Stata Technical Bulletin, 3, 23–24. [Google Scholar]
- Russo M, Stokes G, Lahey B, Christ M, McBurnett K, Loeber R, Stouthamer-Loeber M, & Green S (1993). A sensation seeking scale for children: Further refinement and psychometric development. Journal of Psychopathology and Behavioral Assessment, 15, 69–86. [Google Scholar]
- Stanford MS, Greve KW, Boudreaux JK, Mathias CW, & Brumbelow JL (1996). Impulsiveness and risk-taking behavior: Comparison of high school and college students using the Barratt Impulsiveness Scale. Personality and Individual Differences, 21, 1073–1075. [Google Scholar]
- Stanford MS, Houston RJ, Mathias CW, Villemarette-Pittman NR, Helfritz LE, & Conklin SM (2003). Characterizing aggressive behavior. Assessment, 10, 183–190. [DOI] [PubMed] [Google Scholar]
- Stanford MS, Mathias CW, Dougherty DM, Lake SL, Anderson NE, & Patton JH (2009). Fifty years of the Barratt Impulsiveness Scale: An update and review. Personality and Individual Difference, 47, 385–395. [Google Scholar]
- Steinberg L (2008). A social neuroscience perspective on adolescent risk-taking. Developmental Review, 28, 78–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg L, Sharp C, Stanford MS, & Tharp AT (2013). New tricks for an old measure: The development of the Barratt Impulsiveness Scale-Brief (BIS Brief). Psychological Assessment, 25, 216–226. [DOI] [PubMed] [Google Scholar]
- Tannock R, Schachar R, Carr RP, Chajczyk D, & Logan GD (1989). Effects of methylphenidate on inhibitory control in hyperactive children. Journal of Abnormal Child Psychology, 17, 473–491. [DOI] [PubMed] [Google Scholar]


