Abstract
The majority of neonatal cutaneous conditions are benign and self-limited. However, some skin infections and specific birthmarks are serious and require proper management approaches. This study was a prospective survey of 1000 consecutive newborns at a tertiary care center in Northeast Thailand from September 2015 to 2016, which aimed to identify various cutaneous findings in newborns during their first 5 days of life. The authors found that Mongolian spots (66.7%) and sebaceous gland hyperplasia (60.9%) were the 2 most common cutaneous conditions found in the Thai population. Salmon patches were the most frequent vascular birthmarks (36%), followed by infantile hemangiomas (1.1%) and port wine stains (0.7%). Although majority of the neonatal cutaneous conditions are benign and self-limited, there were 8 cases (0.8%) of bullous impetigo in which both systemic and topical antibiotics were promptly prescribed.
Keywords: birthmark, physiologic neonatal skin conditions, newborn skin findings
Introduction
Neonatal cutaneous conditions are dermatological skin manifestations that are present from birth or appear during the first few days of life. These cutaneous findings vary from physiological and transient manifestations caused by the developmental process of the skin and its structures to major significant pathological issues.1-3 The majority of these cutaneous findings are benign and do not require immediate action. However, some skin infections and specific birthmarks are serious and require proper management approaches. In Thailand, the available literature on neonatal skin lesions is scarce, and there are very few reports regarding cutaneous lesions in newborns.4 Therefore, the present study was undertaken to review the pattern of neonatal dermatoses in this part of the country. Our study is a prospective survey of the neonatal cutaneous conditions and birthmarks that occurred during the first 5 days of life at Srinagarind Medical School Hospital, a tertiary care center in northeast Thailand. The data will be applied in the development of future educational resources for both dermatologists and pediatricians.
Material and Methods
A prospective cohort descriptive study was performed in 1000 consecutive newborns delivered at Srinagarind Hospital, Faculty of Medicine, Khon Kaen University (a tertiary care university center in northeast Thailand) over a period of 1 year (September 2015-2016). All neonates in regular postnatal wards who were no more than 120 hours of age were included. Consent forms were signed by the parents. Maternal data, gestational age, sex, general condition, and delivery methods were recorded. At the end of the study, the collected data were analyzed using STATA software version 12 (StataCorp LP). Descriptive statistical methods—means, standard deviations (SDs), medians, and frequencies—were used to analyze the demographic data. Comparisons of categorical variables among the groups were performed using a χ2 test. Values of P < .05 were considered to indicate statistical significance.
Ethical Approvals and Informed Consent
Written informed consent was obtained from all study participants’ parents on enrollment to this study. The study was approved by the institutional review board of the Faculty of Medicine, Khon Kaen University, Thailand (IRB No. #HE581270) before enrolling any participants.
Results
Demographic Data
One thousand consecutive newborns in regular postnatal wards during the study period were examined. The majority of the cases (94.5%) were documented as full-term born infants with a mean gestational age (GA) of 38.2 weeks (SD 1.1). There were 52 cases (5.2%) of preterm (GA < 37 weeks) and 3 cases (0.3%) of postterm (GA > 42 weeks). Minimum and maximum birth weight were 2070 and 4920 g, respectively. The median birth weight was 3100 g. There were a total of 495 female infants and 505 male infants. The mean maternal age was 29.6 years (SD 5.5) with a median age of 31 years. The youngest maternal age was 15 years, while the oldest was 49 years. There were total of 93 cases (9.3%) with underlying maternal diseases and 150 cases (15%) of documented maternal complications during pregnancy. Table 1 shows lists of maternal underlying diseases and complications during pregnancy that occurred during the study period.
Table 1.
List of Variables of Maternal Underlying Diseases and Maternal Complications During the Study Period.
| Maternal Condition | N | Percentage |
|---|---|---|
| Maternal underlying diseases (N = 93) | ||
| Heart disease: arrhythmia, cardiomegaly | 9 | 0.9 |
| Thyroid: hyperthyroid, thyroid nodules | 12 | 1.2 |
| Thalassemia | 25 | 2.5 |
| Asthma | 6 | 0.6 |
| Systemic lupus erythematosus | 8 | 0.8 |
| HIV | 4 | 0.4 |
| Hepatitis B infection | 20 | 2.0 |
| Immune thrombocytopenic purpura | 1 | 0.1 |
| Diabetic mellitus | 4 | 0.4 |
| Epilepsy | 2 | 0.2 |
| Acute lymphoblastic leukemia in remission | 1 | 0.1 |
| Syphilis | 1 | 0.1 |
| Maternal complications during pregnancy (N = 150) | ||
| Preterm labor | 41 | 41.0 |
| Premature rupture of membrane | 12 | 1.2 |
| Gestational diabetic mellitus | 58 | 5.8 |
| Hypertension | 18 | 1.8 |
| Preeclampsia | 6 | 0.6 |
| Anemia requiring blood transfusion | 4 | 0.4 |
| Maternal fever | ||
| Acute pharyngitis | 5 | 0.5 |
| Urinary tract infection | 4 | 0.4 |
| Dengue fever | 2 | 0.2 |
| Influenza infection | 2 | 0.2 |
This study distributed neonatal cutaneous conditions into 4 categories: (1) transient neonatal skin conditions, (2) pigmented birthmarks, (3) vascular birthmarks, and (4) other miscellaneous cutaneous conditions. The 2 most frequent cutaneous findings found in the study were Mongolian spots and sebaceous gland hyperplasia, with 66.7% and 60.9%, respectively. Other cutaneous findings found in this study are described in Table 2.
Table 2.
Neonatal Cutaneous Conditions Found in the Study Population.
| Cutaneous Lesions | Total (N) | Percentage | Distribution of Cutaneous Lesions Categorized by Gestational Maturation |
||
|---|---|---|---|---|---|
| Full-term (Total 945) | Preterm (Total 52) | Postterm (Total 3) | |||
| Transient neonatal skin conditions | |||||
| Transient neonatal pustular melanosis | 1 | 0.1 | 1 | 0 | 0 |
| Erythema toxicum neonatorum | 222 | 22.2 | 220 | 0 | 2 |
| Sebaceous gland hyperplasia | 609 | 60.9 | 607 | 0 | 2 |
| Skin desquamation | 20 | 20.0 | 17 | 0 | 3 |
| Vernix caseosa | 160 | 16.0 | 159 | 0 | 1 |
| Cutis marmorata | 12 | 12.0 | 7 | 5 | 0 |
| Epstein’s pearl | 73 | 73.0 | 71 | 1 | 1 |
| Neonatal acne | 5 | 0.5 | 5 | 0 | 0 |
| Milia | 165 | 16.5 | 140 | 25 | 0 |
| Miliaria | 64 | 64.0 | 62 | 2 | 0 |
| Pigmented birthmarks | |||||
| Mongolian spot | 667 | 66.7 | 663 | 2 | 2 |
| Café au lait spot | 30 | 30.0 | 30 | 0 | 0 |
| Nevus depigmentosus | 5 | 0.5 | 4 | 1 | 0 |
| Congenital melanocytic nevus | 18 | 1.8 | 18 | 0 | 0 |
| Vascular birthmarks | |||||
| Salmon patch (nevus simplex) | 360 | 36 | 346 | 17 | 0 |
| Port wine stain | 7 | 0.7 | 7 | 0 | 0 |
| Infantile hemangiomas | 11 | 1.1 | 6 | 5 | 0 |
| Other miscellaneous cutaneous conditions | |||||
| Aplasia cutis | 2 | 0.2 | 1 | 1 | 0 |
| Sucking blister | 10 | 1.0 | 10 | 0 | 0 |
| Nevus Sebaceous | 12 | 1.2 | 12 | 0 | 0 |
| Epidermal nevus | 4 | 0.4 | 4 | 0 | 0 |
| Bullous impetigo | 8 | 0.8 | 8 | 0 | 0 |
Transient Neonatal Skin Conditions
In the “transient neonatal skin conditions” category: the 3 most common cutaneous findings were sebaceous gland hyperplasia (60.9%), erythema toxicum neonatorum (22.2%), and milia (16.5%). These cutaneous lesions occur temporarily during first few days of life. The data showed variation with regard to the time the findings first occurred. Sebaceous gland hyperplasia and milia were mostly initially seen at birth (day 0), while erythema toxicum neonatorum occurred in the days that followed.
Pigmented Birthmarks
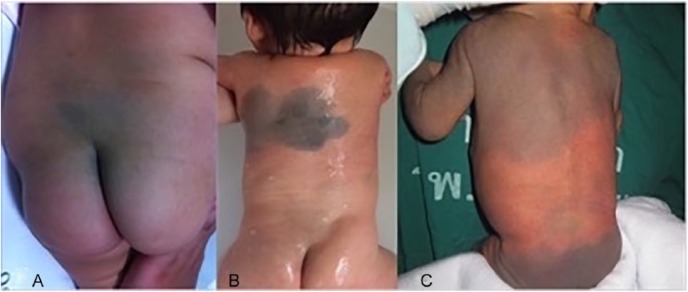
The most common type of pigmented birthmark seen during the study period was Mongolian spots (66.7%). The following most frequent types of pigmented birthmarks were café au lait spots (30%), congenital melanocytic nevus (1.8%), and nevus depigmentosus (0.5%). The majority of Mongolian spots were <5 cm in diameter (305 neonates [45.7%]). Spots between 5 and 10 cm were documented in 274 cases (41%) and >10 cm in diameter in 88 cases (13.2%). Figure 1 shows the clinical presentation of Mongolian spots among the study population.
Figure 1.
Clinical pictures of Mongolian spots on the buttock area (A), back (B), and large extensive area (C) among the study population.
Vascular Birthmarks
The most common type of vascular birthmark during the study period was salmon patch, which was seen in 360 cases (36%). The typical locations of birthmarks were the upper eyelids (18/36, 50%), forehead (9/36, 25%), and nape of the neck (9/36, 25%). There were 7 cases (0.7%) of port wine stain (PWS) and 11 cases (1.1%) of infantile hemangiomas, 5 of which were in preterm infants. Figure 2 shows clinical presentations of salmon patch (Figure 2A), PWS (Figure 2B), and large segmental facial hemangioma in cases of PHACEs (posterior fossa brain malformations, hemangioma, arterial lesions, cardiac abnormalities, and eye abnormalities) syndrome (Figure 2C).
Figure 2.
Clinical presentation of salmon patch (A), port wine stain (B), and large segmental facial hemangioma in PHACEs syndrome (C).
Other Miscellaneous Cutaneous Conditions
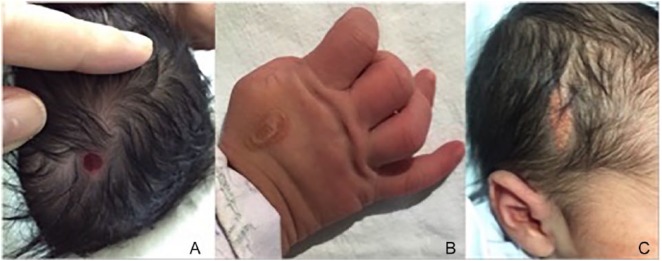
Some uncommon cutaneous findings in this study were aplasia cutis (0.2%; Figure 3A), sucking blister (1%; Figure 3B), nevus sebaceous (1.2%; Figure 3C), and epidermal nevus (0.4%). Bullous impetigo was seen in 8 cases (0.8%). These neonates were all full-term with no maternal risk factors. The treatment given in these cases included topical and systemic antibiotic administration as well as close neonatal monitoring and follow-up. None of these infants developed neonatal sepsis.
Figure 3.
Aplasia cutis presents with an area of scalp defect at birth (A), sucking blister (B) presents as an oval blister on the patient’s hand, which is a result of normal sucking behavior in utero, and nevus sebaceous (C) manifests with an area of hair loss plaque on the scalp at birth. The lesion characteristically has a velvety orange-yellow plaque resulting from hormonal influences from the mother.
Discussion
Neonatal birthmarks and cutaneous conditions in the newborns are the most common problems in general neonatal pediatric practice. The majority of cases are benign cutaneous conditions.5 This study was a statistical and clinical survey of neonatal cutaneous conditions during the first 5 days of life in Thai neonates. The 2 most common cutaneous conditions found in this study were sebaceous gland hyperplasia and Mongolian spots, results which were similar to those of previous studies2,4,6-10 in Asian populations.
Birthmarks and transient skin lesions in newborns and their relationship to maternal factors have been discussed.8,11 The recent study showed significant correlation of the incidence of sebaceous gland hyperplasia that increased with maternal age.12 However, there were no significant differences in illness during the pregnancy, use of drug supplementation in pregnancy, and delivery type in the former publication.8 Our study also gathered data of both maternal underlying diseases and maternal complications during pregnancy, nevertheless no significant correlation of maternal conditions to birthmarks and transient skin lesions in newborns was found in the present study.
The relation between gestational maturity and neonatal cutaneous findings have been described in the literatures.8,13,14 In this study, although the majority of cutaneous findings were seen in full-term infants, there were some types of cutaneous lesions that were more frequently found in preterm infants. These included cutis marmorata (5 out of 12 cases), milia (25 out of 165 cases), salmon patch (6 out of 56 cases), and infantile hemangiomas (5 out of 11 cases). Nevertheless, only milia and sebaceous gland hyperplasia in full-term neonates exhibited a statistical relationship to maturity (P = .01 and .001, respectively). These data are consistent with that of a previous study,6 which showed a highly significant relationship between milia and gestational maturity. Other cutaneous findings related to maturity are shown in Table 3.
Table 3.
Relation of Cutaneous Lesions to Maturity.
| Cutaneous Lesion | Significant Relation With Maturity |
|---|---|
| Milia | P = .001* |
| Miliaria | P = .34 |
| Cutis marmorata | P = .096 |
| Sebaceous gland hyperplasia | P = .0001* |
| Salmon patch | P = .56 |
| Port wine stain | P = .68 |
| Infantile hemangioma | P = .45 |
P < .05.
Salmon patch or nevus simplex was the most commonly found vascular birthmark in this study, which was consistent with the results of other studies from various countries.2,8,15-18 These cutaneous lesions are the result of persistent fetal circulation in newborns. The typical location is usually the upper eyelids, forehead (also called an angel kiss), and nape of neck (also called a stork bite). Most salmon patches disappear within 1 to 2 years, and may present in what is called the “reappearance” phenomenon. Facial lesions may also be accentuated of facial lesions during episodes of crying, breath-holding, straining with defecation, or physical exertion.1,10,15 Because of the differences in natural history, prognosis, and management plan, salmon patches should be distinguished from PWS and infantile hemangiomas.
PWS is a capillary malformation. This cutaneous lesion will not subside by itself. Many cases benefit from early intervention using pulsed dye laser.19 This prevents long-term hypertrophy and nodular proliferation. Moreover, in some cases, PWS may be associated with other anomalies or neurocutaneous syndromes such as Sturge-Weber syndrome, Parker Weber syndrome,20 and Klippel-Trenaunay syndrome. The early detection of PWS may enable prompt management of possible associated anomalies. On the other hand, infantile hemangioma is a form of benign cutaneous vascular tumor in children. This cutaneous lesion has its own characteristics of natural history of growth pattern, which consists of 3 phases: proliferative, involuting, and involuted.21,22 Cutaneous lesions usually occur as preliminary light patches before growing rapidly in the proliferative phase. This pattern can be seen within a few weeks to a few months. Therefore, a diagnosis of infantile hemangioma can be confirmed by following-up on patients’ cutaneous lesions within 1 to 2 months after birth in order to determine if there is proliferative growth. In the majority of cases, infantile hemangioma will regress spontaneously over a period of time. However, there are some problematic hemangiomas that require early treatment.23 The current treatment of choice is oral or topical propranolol, which many studies21,24-26 from around the world have shown to be effective in treating cutaneous lesions.
Mongolian spots refer to macular blue-gray pigmentation that is usually on the sacral area of healthy infants. The lesions represent the collection of melanocytes in the dermal layers, which are believed to arrest in this layer during the embryonal migration from the neural crest to the epidermis.13 This cutaneous finding is commonly seen in Asian, African, and Hispanic populations but is less frequent in Caucasians. Mongolian spots are a type of benign cutaneous lesion with no related anomalies. They usually lessen and/or disappear by the age of 1 to 2 years. However, presentation of large or extensive Mongolian spots may be associated with some serious liposomal storage diseases. Therefore, the occurrence of generalized Mongolian spots in newborns can be a warning sign and possibly enable early detection of these storage diseases.27,28 Although Mongolian spots were the most common cutaneous lesion found in the present study, none of the cases manifested with large or extensive patterns.
Erythema toxicum neonatorum (ETN) is another transient cutaneous condition commonly seen in newborns. The present study found 222 cases (22.2%) of ETN during the study period, similar to the results of many other studies from various regions around the world.8,17,18,29 This benign cutaneous lesion can mimic other cutaneous lesions, such as miliaria pustulosa, neonatal acne, transient neonatal pustular melanosis, and neonatal cephalic pustulosis, as well as some bacterial infections such as impetigo and folliculitis. Differences among these cutaneous findings are summarized in Table 4.
Table 4.
Characteristics of Common Neonatal Pustules During the Early Neonatal Period.
| Characteristics | ETN | TNPM | Neonatal Acne | Neonatal Cephalic Pustulosis |
|---|---|---|---|---|
| Clinical | Multiple tiny pustules erythematous base, blotchy | Multiple tiny pustules on erythematous base with residual hyperpigmented macules and scales | Comedone-like erythematous papules and pustules | Erythematous pustules |
| Location | Face, trunk, extremities | Face, trunk, extremities, can be seen at the palms and soles | Mostly on the face and bilateral cheeks | Characteristically limited to the face |
| Onset | At birth, within 1 week | At birth, within 1 week | Usually after 1 week of age, peak around 2 months of age | Can be seen at birth |
| Pathophysiology | Unknown | Unknown | Stimulation of sebaceous gland by maternal androgen hormone | May associate with Malassezia furfur colonization |
| Stain/smear of the cutaneous lesion | No organism, prominent eosinophils, some neutrophils | No organism, numerous neutrophils, occasional eosinophils | Neutrophils, Malassezia furfur may identify | Neutrophils, Malassezia furfur may identify |
| Prognosis | Excellent, not related to other cutaneous condition; heals without scar | Excellent, not related to other cutaneous conditions; leaves hyperpigmentation for 1-2 weeks then clears completely without scarring | Resolve spontaneously within 1-3 months | Resolve spontaneously within 4-8 weeks |
Abbreviations: ETN, erythema toxicum neonatorum; TNPM, transient neonatal pustular melanosis.
There were 8 cases (0.8%) of bullous impetigo during the study period. This cutaneous lesion can mimic other benign dermatoses, such as miliaria pustulosa, and ETN. Bedside gram staining and the routine monitoring of vital signs are necessary in these cases. Gram staining can confirm a diagnosis of impetigo by revealing gram-positive cocci in cluster pattern. It is noteworthy that bullous impetigo is a form of sub-corneal bacterial infection caused by the exfoliative toxin from Staphylococcus aureus. This cutaneous infection can be more severe if the infection occurs in preterm infants.30 However, the patients in this study with bullous impetigo were full-term and had no serious complications apart from cutaneous infection. All infants were treated with both systemic and topical antibiotics, and there were no cases of subsequent neonatal sepsis. However, pediatricians should be alert to the possibility of clinical sepsis at all times in cases of suspected cutaneous infection. Our study also evaluated maternal risk factors associated with the occurrence of bullous impetigo. However, no related maternal conditions were found (P = .98).
Conclusion
Mongolian spots and sebaceous gland hyperplasia were the 2 most common cutaneous conditions found in the Thai population. Although the majority of the neonatal cutaneous conditions in this study were benign and self-limited, the right diagnosis among various cutaneous conditions is important. This can enable prompt specific action if necessary. Importantly, pediatric dermatologists and pediatricians should be familiar with the various types of birthmarks and become more comfortable discussing disease prevention and cosmetic strategies.
Footnotes
Author Contributions: LT: Contributed to conception and design; contributed to acquisition; drafted manuscript; critically revised manuscript; gave final approval; agrees to be accountable for all aspects of work ensuring integrity and accuracy.
VS: Contributed to acquisition; drafted manuscript; gave final approval; agrees to be accountable for all aspects of work ensuring integrity and accuracy.
PP: Contributed to conception and design; critically revised manuscript; gave final approval; agrees to be accountable for all aspects of work ensuring integrity and accuracy.
LAS: Contributed to conception and design; critically revised manuscript; gave final approval; agrees to be accountable for all aspects of work ensuring integrity and accuracy.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The study was supported by a grant from Khon Kaen University, Faculty of Medicine (Grant Number IN58333).
ORCID iD: Leelawadee Techasatian  https://orcid.org/0000-0003-4668-6792
https://orcid.org/0000-0003-4668-6792
References
- 1. Cordoro KM, Speetzen LS, Koerper MA, Frieden IJ. Physiologic changes in vascular birthmarks during early infancy: mechanisms and clinical implications. J Am Acad Dermatol. 2009;60:669-675. [DOI] [PubMed] [Google Scholar]
- 2. Shih IH, Lin JY, Chen CH, Hong HS. A birthmark survey in 500 newborns: clinical observation in two northern Taiwan medical center nurseries. Chang Gung Med J. 2007;30:220-225. [PubMed] [Google Scholar]
- 3. Schachner L, Ling NS, Press S. A statistical analysis of a pediatric dermatology clinic. Pediatr Dermatol. 1983;1:157-164. [DOI] [PubMed] [Google Scholar]
- 4. Chaithirayanon S, Chunharas A. A survey of birthmarks and cutaneous skin lesions in newborns. J Med Assoc Thai. 2013;96(suppl 1):S49-S53. [PubMed] [Google Scholar]
- 5. Carmona N, Bentz MG, Bhagwat MM, Cabana MD. Newborn skin findings in the nursery. Clin Pediatr (Phila). 2018;57:850-853. [DOI] [PubMed] [Google Scholar]
- 6. Sadana DJ, Sharma YK, Chaudhari ND, Dash K, Rizvi A, Jethani S. A clinical and statistical survey of cutaneous changes in the first 120 hours of life. Indian J Dermatol. 2014;59:552-557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ryan E, Warren L. Birthmarks—identification and management. Aust Fam Physician. 2012;41:274-277. [PubMed] [Google Scholar]
- 8. Boccardi D, Menni S, Ferraroni M, et al. Birthmarks and transient skin lesions in newborns and their relationship to maternal factors: a preliminary report from Northern Italy. Dermatology. 2007;215:53-58. [DOI] [PubMed] [Google Scholar]
- 9. Hidano A, Purwoko R, Jitsukawa K. Statistical survey of skin changes in Japanese neonates. Pediatr Dermatol. 1986;3:140-144. [DOI] [PubMed] [Google Scholar]
- 10. Moosavi Z, Hosseini T. One-year survey of cutaneous lesions in 1000 consecutive Iranian newborns. Pediatr Dermatol. 2006;23:61-63. [DOI] [PubMed] [Google Scholar]
- 11. Ekiz Ö, Gül Ü, Mollamahmutoğlu L, Gönül M. Skin findings in newborns and their relationship with maternal factors: observational research. Ann Dermatol. 2013;25:1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ábrahám R, Meszes A, Gyurkovits Z, Bakki J, Orvos H, Csoma ZR. Cutaneous lesions and disorders in healthy neonates and their relationships with maternal-neonatal factors: a cross-sectional study. World J Pediatr. 2017;13:571-576. [DOI] [PubMed] [Google Scholar]
- 13. McLaughlin MR, O’Connor NR, Ham P. Newborn skin: Part II. Birthmarks. Am Fam Physician. 2008;77:56-60. [PubMed] [Google Scholar]
- 14. Fluhr JW, Darlenski R, Lachmann N, et al. Infant epidermal skin physiology: adaptation after birth. Br J Dermatol. 2012;166:483-490. [DOI] [PubMed] [Google Scholar]
- 15. Haveri FT, Inamadar AC. A cross-sectional prospective study of cutaneous lesions in newborn. ISRN Dermatol. 2014;2014:360590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Sachdeva M, Kaur S, Nagpal M, Dewan SP. Cutaneous lesions in new born. Indian J Dermatol Venereol Leprol. 2002;68:334-337. [PubMed] [Google Scholar]
- 17. Kahana M, Feldman M, Abudi Z, Yurman S. The incidence of birthmarks in Israeli neonates. Int J Dermatol. 1995;34:704-706. [DOI] [PubMed] [Google Scholar]
- 18. Jacobs AH, Walton RG. The incidence of birthmarks in the neonate. Pediatrics. 1976;58:218-222. [PubMed] [Google Scholar]
- 19. Kowalska-Brocka J, Brocki M, Uczniak S, Uczniak K, Kaszuba A, Jurowski P. Sturge-Weber syndrome type II treated with PDL 595 nm laser. Postepy Dermatol Alergol. 2015;32:63-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Esquivel DJR, Manzano EM, Concepción NA, Gutierréz JCL, de Cubas LR. Nodular Proliferation in Parkes Weber Syndrome. Ann Vasc Surg. 2017;38:321.e1-321.e4. [DOI] [PubMed] [Google Scholar]
- 21. Techasatian L, Komwilaisak P, Panombualert S, Uppala R, Jetsrisuparb C. Propranolol was effective in treating cutaneous infantile haemangiomas in Thai children. Acta Paediatr. 2016;105:e257-e262. [DOI] [PubMed] [Google Scholar]
- 22. Techasatian L, Tanming P, Panombualert S, Uppala R, Jetsrisuparb C. Vascular anomalies: the epidemiological profile at Srinagarind Hospital. J Med Assoc Thai. 2015;98(suppl 7):S101-S106. [PubMed] [Google Scholar]
- 23. Price CJ, Lattouf C, Baum B, et al. Propranolol vs corticosteroids for infantile hemangiomas: a multicenter retrospective analysis. Arch Dermatol. 2011;147:1371-1376. [DOI] [PubMed] [Google Scholar]
- 24. Vivas-Colmenares GV, Bernabeu-Wittel J, Alonso-Arroyo V, de Cardenas JAM, Fernandez-Pineda I. Effectiveness of propranolol in the treatment of infantile hemangioma beyond the proliferation phase. Pediatr Dermatol. 2015;32:348-352. [DOI] [PubMed] [Google Scholar]
- 25. Schneider M, Cremer HJ, Ruef P. A retrospective analysis of systemic propranolol for the treatment of complicated infantile haemangiomas. Acta Paediatr. 2014;103:977-983. [DOI] [PubMed] [Google Scholar]
- 26. Drolet BA, Frommelt PC, Chamlin SL, et al. Initiation and use of propranolol for infantile hemangioma: report of a consensus conference. Pediatrics. 2013;131:128-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ashrafi MR, Shabanian R, Mohammadi M, Kavusi S. Extensive Mongolian spots: a clinical sign merits special attention. Pediatr Neurol. 2006;34:143-145. [DOI] [PubMed] [Google Scholar]
- 28. Mimouni-Bloch A, Finezilber Y, Rothschild M, Raas-Rothschild A. Extensive Mongolian spots and lysosomal storage diseases. J Pediatr. 2016;170:333-e1. [DOI] [PubMed] [Google Scholar]
- 29. Nanda A, Kaur S, Bhakoo ON, Dhall K. Survey of cutaneous lesions in Indian newborns. Pediatr Dermatol. 1989;6:39-42. [DOI] [PubMed] [Google Scholar]
- 30. Saida K, Kawasaki K, Hirabayashi K, et al. Exfoliative toxin A staphylococcal scalded skin syndrome in preterm infants. Eur J Pediatr. 2015;174:551-555. [DOI] [PubMed] [Google Scholar]