Abstract
Case summary
It is described a case of a 10-month-old female mixed-breed cat with left ear discharge of approximately 6 days’ duration prior to the admission. Secretions were collected from both ears using a sterile swab for cytological and mycological analysis. A pyogranulomatous inflammatory infiltrate (predominantly characterized by the presence of neutrophils and macrophages) with the presence of cocci, rods and many yeast-like structures were seen on cytological analysis; the fungal culture confirmed the presence of the Sporothrix schenckii complex. Upon diagnosis of fungal otitis due to the S schenckii complex, treatment with oral itraconazole was administered. After 4 weeks of treatment, no S schenckii complex colonies were isolated, and clinical recovery had occurred.
Relevance and novel information
Although rare, clinicians must be aware of atypical presentations of sporotrichosis, as in this case of external otitis. This is of clinical relevance because this infection has been reported in several countries and is defined as a zoonotic disease.
Keywords: Sporothrix schenckii complex, otopathy, fungal infection, zoonotic disease, itraconazole, dermatology
Introduction
Otitis externa is defined as an inflammation of the external ear canal and sometimes the pinna.1–4 It is a common ailment in small animals, occurring in 13–16% of the canine case population;1 however, few data concerning the prevalence and incidence of feline otitis externa have been published.2 The primary causes of this ailment are those that induce otitis externa directly; for example, foreign bodies or ectoparasites are the most common causes of feline external otitis.3,4 Although some allergic cats will have concurrent otitis, the incidence is far lower than in dogs. Additional primary causes include autoimmune diseases, neoplasia and fungal infections.5,6
Fungal infections such as sporotrichosis are more frequently described leading to skin diseases in cats.7,8 Sporotrichosis is a cutaneous mycosis caused by a dimorphic fungus, namely the Sporothrix schenckii complex, which is widely distributed in nature.8 The cutaneous form of feline sporotrichosis is the most commonly reported. The disease usually ranges from a single skin lesion that can progress to multiple skin lesions and fatal systemic involvement. Nodules and ulcers are the most common skin lesions, and respiratory signs and nasal mucosa involvement occur frequently.7–10 The S schenckii complex is a worldwide mycosis and an important zoonotic disease. Although this fungal infection is very common in cats in some geographical areas of the world, sporotrichosis associated with primary cause of external otitis is extremely uncommon. The aim of this report was therefore to describe a case of unusual primary cause of feline external otitis: a case of sporotrichosis.
Case description
A 10-month-old female mixed-breed cat weighing 2.7 kg was referred to a veterinarian with an interest in dermatology in Rio de Janeiro, Brazil with left ear discharge of approximately 6 days’ duration prior to admission. The cat was shaking its head or pawing at the ear. The animal was in good physical health, had been given all annual recommended vaccines and was fed with good-quality cat food. The cat had free outdoor access. The animal’s physiological parameters were normal for the species. Ear examination showed no lesions at the pinna, but at the opening of the external meatus there was visible ulceration, erythema and a dark secretion (Figure 1). Both ears were examined using an otoscope (Welch Allyn Macroview). There were signs of external otitis for only the left ear. Otoscopic examination of the left ear was impaired owing to excessive secretion, although the tympanic membrane was observed as intact, and there was no foreign body, aural polyp or tumor in the canal. Secretion was collected from both ears using a sterile swab for cytological and mycological analysis.
Figure 1.

External meatus of the cat with ulceration, erythema and a dark secretion
A pyogranulomatous inflammatory infiltrate (predominant presence of neutrophils and macrophages) with the presence of cocci, rods and many yeast-like structures were seen on cytology (Figure 2). To rule out other dimorphic fungi that resemble the yeast of the S schenkii complex, a fungal culture was performed. The yeast-like structures observed on cytology did not confirm the diagnosis of sporotrichosis. Therefore, material was collected for fungal culture from the exudative lesion within the external ear canal. The material was transferred to the indicated culture medium (Sabouraud Dextrose Agar) and agar added with chloramphenicol and cycloheximide, and incubated at 25°C. Fungal growth was observed in within 5 days. Microscopically, delicate, septate and conidial pyriform or spherical hyphae were observed and isolated or grouped as flower petals at the end of short conidiophores. This test confirmed the presence of the fungus S schenkii complex.
Figure 2.
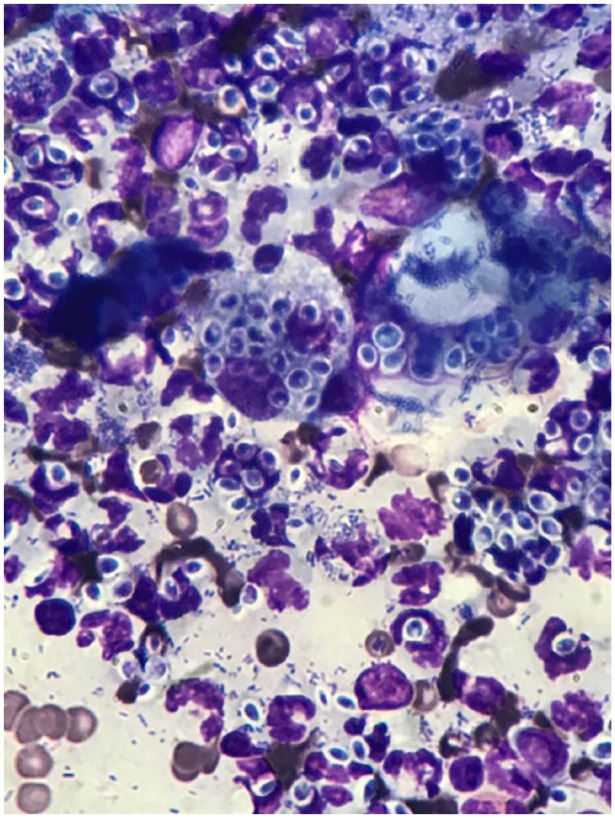
Pyogranulomatous inflammatory infiltrate (predominant presence of neutrophils and macrophages) with the presence of cocci, rods and also many yeast-like structures on cytology
After the cytopathological examination revealed the presence of yeast-like structures, an oral antifungal medication was prescribed: a 4 week course of itraconazole 10 mg/kg q24h. No other oral or topical treatment was administered.
After 30 days of treatment, there was a total regression of the lesions (Figure 3). Additionally, a new cytological examination and culture confirmed negative results for any fungal infection, and the treatment was continued 1 month beyond clinical cure.7
Figure 3.

Total regression of the lesions after 30 days of treatment with itraconazole
Discussion
In cats, the S schenkii complex may produce a wide range of clinical manifestations.7–10 However, involvement of the external auditory meatus is uncommon, even in highly severe or disseminated disease. In general, reports on the isolation of the S schenkii complex from cases of otitis externa in dogs and cats are very rare.11
Sporotrichosis in cats has been reported in several countries, but nowhere has an outbreak of animal sporotrichosis been as large as that seen in Brazil, specifically in Rio de Janeiro.12 Typically, this infection develops after traumatic inoculation of contaminated soil, plants and organic matter into skin or mucosa. Alternatively, infection may occur during animal transmission (cat–cat),10,13 by which a sick cat transmits the disease to a healthy one via traumatic inoculation. Clinically, the skin lesions are characterized by nodules and ulcers that are found at three or more anatomical sites, most commonly on the head.7 The involvement of the external auditory canal of this cat might have been by traumatic inoculation by scratches or even bites from a sick cat.14 In Rio de Janeiro, Brazil, this infection has been described with many atypical presentations,15 as in this case.
Differential diagnoses of external otitis can be based on the observation of a unilateral vs a bilateral problem. All primary causes of unilateral problems, such as a foreign body, aural polyp, neoplasia or trauma (aural hematoma),5 were included in the differential diagnosis of the cat described in this study. Otoscopic evaluation of the external ear canal and tympanic membrane should always be performed in animals presenting with otitis externa.16 Thus, the presence of a foreign body, aural polyp and tumor in the ear canal were ruled out by otoscopy.
To ensure a definitive diagnosis, the cytological evaluation was fundamental in this case. This assay revealed the yeast-like cells that indicated the primary diagnosis of sporotrichosis and the secondary infection with the presence of cocci and rods. Although the definitive diagnosis of feline sporotrichosis is made by fungal culture, cytopathological and histopathological examinations are used routinely because the long culture period may delay onset of treatment.17 In this case, after the cytological evaluation, the treatment was started immediately.
As S schenkii complex organisms are not common agents of external otitis, the disease may easily be misdiagnosed and the results of the treatment can be disappointing. The drug of choice to treat this disease is a systemic antifungal (itraconazole)7 and the drugs recommended for treating ear infections are usually topicals. Until now, there has been no evidence that topical therapy as a sole or adjunct treatment could lead to the cure or even accelerate the cure. As the S schenkii complex is a zoonotic disease, contact with the fungus should be limited and infection-control practices (gloves, hand hygiene) should be carried out. Cats present high zoonotic potential for the transmission of this fungus because their skin lesions contain high numbers of yeast-like cells.13
As the primary cause of the external otitis was the sporotrichosis infection, no other treatment was given and managing the primary disease may have controlled the perpetuating factors (cocci and rods).
Conclusions
Although rare, clinicians must be aware of the atypical presentations of the sporotrichosis fungus, as in this case of external otitis, especially because this infection has been reported in several countries and because it is a zoonotic disease.
Footnotes
Accepted: 15 February 2019
Conflict of interest: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Kuttin ES, Glas I. Mycotic otitis externa in animals. Mycoses 1985; 28: 61–68. [DOI] [PubMed] [Google Scholar]
- 2. Bollez A, de Rooster H, Furcas A, et al. Prevalence of external ear disorders in Belgian stray cats. J Feline Med Surg 2018; 20: 149–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Angus JC. Otic cytology in health and disease. Vet Clin North Am Small Anim Pract 2004; 34: 411–424. [DOI] [PubMed] [Google Scholar]
- 4. Rosser EJ., Jr. Causes of otitis externa. Vet Clin North Am Small Anim Pract 2004; 34: 459–468. [DOI] [PubMed] [Google Scholar]
- 5. Kennis RA. Feline otitis: diagnosis and treatment. Vet Clin Small Anim 2013; 43: 51–56. [DOI] [PubMed] [Google Scholar]
- 6. Nardoni S, Mancianti F, Rum A, et al. Isolation of Malassezia species from healthy cats and cats with otitis. J Feline Med Surg 2005; 7: 141–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gremião IDF, Menezes RC, Schubach TMP, et al. Feline sporotrichosis: epidemiological and clinical aspects. Med Mycol 2015; 53: 15–21. [DOI] [PubMed] [Google Scholar]
- 8. Rippon JW. Sporotrichosis. In: Rippon JW. (ed). Medical mycology: the pathogenic fungi and pathogenic actinomycetes. 2nd ed. Philadelphia, PA: WB Saunders, 1988, pp 325–352. [Google Scholar]
- 9. Scott DW, Miller WH, Griffin CE. Fungal skin diseases. In: Muller and Kirk’s small animal dermatology. 6th ed. Philadelphia, PA: WB Saunders, 2001, pp 386–390. [Google Scholar]
- 10. Boechat JS, Oliveira MME, Almeida-Paes R, et al. Feline sporotrichosis: associations between clinical-epidemiological profiles and phenotypic-genotypic characteristics of the etiological agents in the Rio de Janeiro epizootic area. Mem Inst Oswaldo Cruz 2018; 113: 185–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Dion WM, Speckmann G. Canine otitis externa caused by the fungus Sporothrix schenkii. Can Vet J 1978; 19: 44–45. [PMC free article] [PubMed] [Google Scholar]
- 12. Pereira SA, Gremião IDF, Kitada AAB, et al. The epidemiological scenario of feline sporotrichosis in Rio de Janeiro, State of Rio de Janeiro, Brazil. Rev Soc Bras Med Trop 2014; 47: 392–393. [DOI] [PubMed] [Google Scholar]
- 13. Rodrigues AM, de Hoog GS, de Camargo ZP. Sporothrix species causing outbreaks in animals and humans driven by animal-animal transmission. PLoS Pathog 2016; 12. DOI: 10.1371/journal.ppat.1005638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gremião IDF, Miranda LHM, Reis EG, et al. Zoonotic epidemic of sporotrichosis: cats to human transmission. PLoS Pathog 13. DOI: 10.1371/journal.ppat.1006077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mascarenhas MB, Lopes NL, Pinto TG, et al. Canine sporotrichosis: report of 15 advanced cases. Pesqui Vet Bras 2018; 38: 477–481. [Google Scholar]
- 16. Borio S, Massari F, Abramo F, et al. Proliferative and necrotising otitis externa in a cat without pinnal involvement: video-otoscopic features. J Feline Med Surg 2013; 15: 353–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Jessica N, Sonia RL, Rodrigo C, et al. Diagnostic accuracy assessment of cytopathological examination of feline sporotrichosis. Med Mycol 2015; 53: 880–884. [DOI] [PubMed] [Google Scholar]


